Abstract
Retention of fixed partial dentures is mostly dependent upon the bond between metal and cement as well as cement and tooth structure. However, most of the time clinical failure of bond has been observed at metal and cement interface. The treatment of metal surface, prior to luting, plays a crucial role in bonding cement with the metal. This study is conducted to evaluate and compare the effect of different surface preparations on the bond strength of resin-modified glass ionomer cement with nickel–chromium metal ceramic alloy. Fifty caries-free extracted molar teeth were made flat until the dentin of the occlusal surface was exposed. After fabrication of the wax patterns and subsequent castings, the castings were subjected to porcelain firing cycles. The nickel–chromium metal ceramic alloy discs were also divided into five groups and subjected to various surface treatments: (1) Unsandblasted (U), (2) sandblasted (S), (3) sandblasted and treated with 10% aqueous solution of KMnO4 (SK), (4) unsandblasted and roughened with diamond abrasive points (UD) and (5) unsandblasted and roughened with diamond abrasive points and treated with 10% aqueous solution of KMnO4 (UDK). After surface treatments, the castings were cemented using Fuji PLUS encapsulated resin-modified glass ionomer cement. The obtained values of all the groups were subjected to statistical analysis for Tensile and Shear bond strength. Different surface treatments of the metal affects the bond strength values of resin-modified glass ionomer cement when used as luting agent.
Keywords: Surface treatment, Bond strength, Resin-modified glass ionomer cement
Introduction
Era of adhesive dentistry began with the development of acid etching of enamel and later acid etching of dentin to improve the retention of the restoration. The treatment of metal surface, prior to luting, plays a crucial role in bonding adhesive cement with the metal. The bond of luting resin to metal framework is a critical factor and is found to depend upon various factors like, type of alloy and its contents [1], surface treatment of the metal, type of adhesive cement and film thickness of the luting cement. The first important step is the treatment of metal surface being luted. The treatment of surface results in changes in chemistry or alters the surface texture and area thereby increasing mechano-chemical bond between metal and the adhesive cement being used.
Apart from air abrasion, manufacturers and investigators have recommended different acids, acid concentrations and current densities for electrolytic etching of base metal alloys for surface treatment. Chemical bonding employing the deposition of Silica layer [2] or Tin layer [3, 4] were recommended and the use of chemical gel etchants, liquid etchants, immersion into KMnO4 solution and alloy primers were in use [5, 6].
Bond strength can also be affected by the type of luting cement used and the inappropriate treatment of the surfaces of alloys. Wide use of resin modified glass ionomer cement as luting agents is mainly attributed to their low film thickness, higher strength, low solubility, adhesion to tooth structure and restoration, reduced microleakage, long working time, short setting time and low post-cementation sensitivity [7, 8]. So, this study was done to evaluate and compare the effect of different surface preparations on the bond strength of resin-modified glass ionomer cement with nickel–chromium metal ceramic alloy.
Materials and Methods
Fifty freshly extracted, caries free, unrestored human molar teeth were collected. The occlusal surface of each tooth was made flat until the dentin was exposed (Fig. 1), with the help of an extra fine grit flat end tapered diamond abrasive point using a high-speed hand piece and copious water spray after which it was smoothened & polished with 120 grit sandpaper. The teeth were embedded in a self-cure acrylic resin block 3 × 2.8 × 2 cm (height × width × thickness), and the coronal portion of each tooth was kept above the acrylic resin block and care was taken to keep the occlusal surface parallel to the horizontal plane.
Fig. 1.
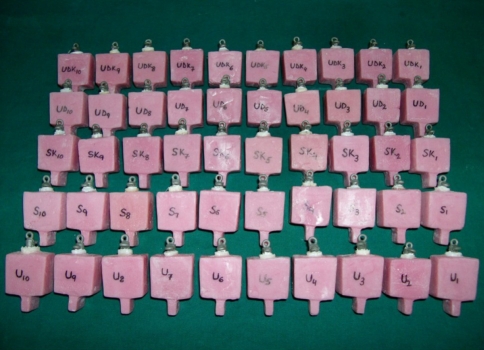
Prepared samples (10 each of Groups U, S, SK, UD, UDK)
The prepared teeth samples were divided into 5 groups randomly by selecting 10 samples for each group. The five groups were designated on the basis of the type of surface treatment of metal as unsandblasted, sandblasted, sandblasted and treated with 10% aqueous solution of KMnO4, unsandblasted and roughened with diamond abrasive points and treated with 10% aqueous solution of KMnO4 and grouped as U, S, SK, UD, UDK respectively.
Fabrication of Wax Pattern
Plastic hollow tubes of diameter 6.5 mm and height 3 mm were cut in the form of discs to eliminate the cylindrical effect of artificial crowns. Fifty wax patterns were fabricated directly over the prepared teeth to avoid errors in film thickness of luting cements. Die-lube was applied on the specimens directly and application of the die spacer was eliminated intentionally to avoid luting film thickness variation. The wax pattern discs for each sample were fabricated following direct wax pattern technique. An inverted ‘U’ shaped wax loop was attached on the occlusal surface of the disc and another was attached perpendicular to it.
Wax patterns were invested and cast in nickel–chromium metal ceramic alloy. Cast discs were retrieved, cleaned of the investment material. Each metallic disc was inspected for casting defects under magnification, and seated on respective teeth to evaluate complete seating. The discs were ultrasonically cleaned of debris in ultrasonic cleaner for 2 min [1, 9].
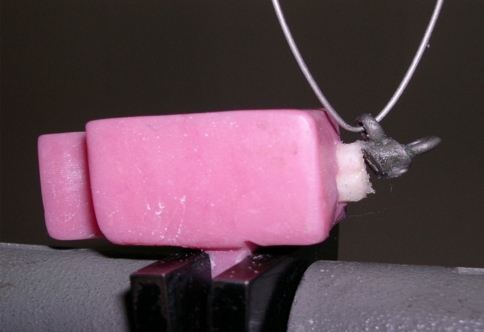
These metallic discs were then subjected to oxidation cycle to simulate porcelain firing on one surface [10]. The nickel–chromium metal ceramic alloy discs were also divided into five groups and subjected to various surface treatments (Fig. 2). All the 50 castings were again ultrasonically cleaned in distilled water for 2 min before cementation [1, 9].
Fig. 2.
Samples with surface treatment (10 each of Group U, S, SK, UD and UDK)
The metallic discs were cemented onto the flat surface of the teeth with GC Fuji PLUS capsules [11] (resin modified glass ionomer luting cement) mixed for 10 s in a capsule mixer (GC) (Fig. 3), according to the manufacturer’s instructions [12]. The specimens were held with firm finger pressure to give as close fit as possible until the resin cement had polymerized. The excess cement was wiped off with cotton pellets and removed with dental explorer (after initial setting). Vaseline was applied at the margins of the cemented specimens to prevent water contamination. Likewise, remaining 49 test specimens were cemented (Fig. 4).
Fig. 3.
Armamentarium for cementation (GC Fuji PLUS capsules and capsule mixer)
Fig. 4.
Cemented discs on teeth mounted on acrylic resin block
The specimens were stored in distilled water for 24 h before testing on Instron testing machine. Five specimens from each group of 10 were tested for tensile strength and the remaining five specimens were tested for shear strength (Figs. 5, 6). Tensile force was applied at a crosshead speed of 1 mm/min in vertical direction & shear force was applied at a crosshead speed of 1 mm/min in horizontal direction. The forces were applied till the disc was dislodged from the tooth.
Fig. 5.
Vertically mounted and dislodged specimen on Instron testing machine
Fig. 6.
Horizontally mounted and dislodged specimen on Instron testing machine
Results
Mean and standard deviation of Tensile bond strength values of samples of different groups revealed that the highest mean vertical force was found for Group UD (3.322 ± 0.4377 MPa) and the least for Group SK (1.217 ± 0.3901 MPa).
Mean and standard deviation of Shear bond strength values of samples of different groups revealed that the highest mean horizontal force was for Group UDK (1.956 ± 0.5944 MPa) and the least for Group U (0.9276 ± 0.3927 MPa).
A Student’s t test was performed on observed values (Table 1) to compare the tensile strength with different surface treatments between all the groups. The results showed statistically non-significant differences on comparing groups; S with UD, S with UDK, UD with UDK. Similarly Student’s t test was performed on observed values (Table 2) to compare shear strength with different surface treatments between all the groups. The results showed statistically non-significant differences on comparing groups; U and SK, S and SK, S and UD, S and UDK, SK and UD, UD and UDK.
Table 1.
Statistical comparison of mean tensile strength values (Student’s t test) of Groups U and S, U and SK, U and UD, U and UDK, S and SK, S and UD, S and UDK, SK and UD, SK and UDK, UD and UDK
| Group | Mean (n = 5) | Standard deviation | |t| value | P-value | Remarks |
|---|---|---|---|---|---|
| U | 2.057 | 0.3290 | 5.65 | 0.0005 | S |
| S | 3.220 | 0.3215 | |||
| U | 2.057 | 0.3290 | 3.68 | 0.0062 | S |
| SK | 1.217 | 0.3901 | |||
| U | 2.057 | 0.3290 | 5.16 | 0.0009 | S |
| UD | 3.322 | 0.4377 | |||
| U | 2.057 | 0.3290 | 4.18 | 0.0031 | S |
| UDK | 2.814 | 0.2358 | |||
| S | 3.220 | 0.3215 | 8.86 | 0.0000 | S |
| SK | 1.217 | 0.3901 | |||
| S | 3.220 | 0.3215 | 0.42 | 0.6867 | NS |
| UD | 3.322 | 0.4377 | |||
| S | 3.220 | 0.3215 | 2.28 | 0.0520 | NS |
| UDK | 2.814 | 0.2358 | |||
| SK | 1.217 | 0.3901 | 8.03 | 0.0000 | S |
| UD | 3.322 | 0.4377 | |||
| SK | 1.217 | 0.3901 | 7.83 | 0.0001 | S |
| UDK | 2.814 | 0.2358 | |||
| UD | 3.322 | 0.4377 | 2.29 | 0.0516 | NS |
| UDK | 2.814 | 0.2358 |
S Significant, NS non significant, S* significant at 5% level of significance
Table 2.
Statistical comparison of mean shear strength values (Student’s t test) of Groups U and S, U and SK, U and UD, U and UDK, S and SK, S and UD, S and UDK, SK and UD, SK and UDK, UD and UDK
| Group | Mean (n = 5) | Standard deviation | |t| value | P-value | Remarks |
|---|---|---|---|---|---|
| U | 0.9276 | 0.3927 | 2.71 | 0.0266 | S* |
| S | 1.694 | 0.4954 | |||
| U | 0.9276 | 0.3927 | 1.15 | 0.2840 | NS |
| SK | 1.190 | 0.3269 | |||
| U | 0.9276 | 0.3927 | 2.59 | 0.0321 | S* |
| UD | 1.438 | 0.1997 | |||
| U | 0.9276 | 0.3927 | 3.23 | 0.0121 | S* |
| UDK | 1.956 | 0.5944 | |||
| S | 1.694 | 0.4954 | 1.90 | 0.0941 | NS |
| SK | 1.190 | 0.3269 | |||
| S | 1.694 | 0.4954 | 1.07 | 0.3151 | NS |
| UD | 1.438 | 0.1997 | |||
| S | 1.694 | 0.4954 | 0.76 | 0.4707 | NS |
| UDK | 1.956 | 0.5944 | |||
| SK | 1.190 | 0.3269 | 1.45 | 0.1857 | NS |
| UD | 1.438 | 0.1997 | |||
| SK | 1.190 | 0.3269 | 2.52 | 0.0355 | S* |
| UDK | 1.956 | 0.5944 | |||
| UD | 1.438 | 0.1997 | 1.85 | 0.1019 | NS |
| UDK | 1.956 | 0.5944 |
S Significant, NS non significant, S* significant at 5% level of significance
One way ANOVA was performed on the tensile bond strength (Table 3) and shear bond strength (Table 4) values of various groups and were found to be significant for both.
Table 3.
Statistical analysis (one way ANOVA) of tensile bond strength values of Groups U, S, SK, UD and UDK
| Source of variance | Degree of freedom | Sum of squares | Mean sum of squares | F-ratio | P-value | Remarks |
|---|---|---|---|---|---|---|
| Between groups | 4 | 15.65 | 3.913 | 32.03 | 0.0000 | S |
| Within groups | 20 | 2.444 | 0.1222 | |||
| Total | 24 | 18.10 |
S Significant, NS non significant, S* significant at 5% level of significance
Table 4.
Statistical analysis (one way ANOVA) of shear bond strength values of Groups U, S, SK, UD and UDK
| Source of variance | Degree of freedom | Sum of squares | Mean sum of squares | F-ratio | P-value | Remarks |
|---|---|---|---|---|---|---|
| Between groups | 4 | 3.279 | 0.8198 | 4.56 | 0.0089 | S |
| Within groups | 20 | 3.599 | 0.1799 | |||
| Total | 24 | 6.878 |
S Significant, NS non significant, S* significant at 5% level of significance
Discussion
The clinical success of a fixed partial denture depends upon the retention of the prosthesis. The retention is achieved by the tenso-frictional resistance and the nature of the luting agent used. Though, the preparation of the tooth structure is a critical factor, the proper selection of a suitable luting agent greatly contributes to the retention of fixed partial dentures.
The development of resin-modified glass ionomer cement, that chemically bonds to dental alloys as well as tooth structure, have simplified the conventional approach for treatment with fixed partial dentures. Improper treatment of metal surface has been cited as the main cause for metal and cement bond failure [9]. Different surface treatments of Gold alloys as well as base metal alloys have been advocated (by manufacturers’ of adhesive cements) and evaluated to enhance bonding with resin cements [13–15].
Resin-modified glass ionomer cements used in the study are basically water-hardening cements, where the water component is replaced by a water/HEMA mixture (hydroxyethylmethacrylate). The reaction is dual-setting i.e. sets partly by an acid–base reaction and partly by polymerization [16].
Most of the evaluations of metal–cement bonding have been based on in-vitro bond strength evaluations. Determination of tensile and shear bond strength values seems to be important mainly because of the involvement of tensile and shear stresses during the dislodgement of prostheses.
Immersion of test samples in 10% aqueous solution of KMnO4 as an oxidizing solution after surface treatment with sandblasting or diamond abrasives, was included in this study to verify the effect on bonding, of resin-modified glass ionomer cement, when applied to an oxidized surface.
Tanaka [17] studied the effect of oxidation of alloy on bond with 4-META resin. Samples of nickel–chromium were subjected to oxidation with 61% HNO3 solution at room temperature for 15 min after treating the surface with:
Suspension of alumina.
Grinding with emery paper.
Etching with 36% HCl.
Oxidation of surface resulted in improvement of bond strength. The study stressed upon the need to roughen the metal surface prior to oxidation.
Tanaka et al. [18] used acidic solution of KMnO4 and dilute H2SO4 for treating nickel–chromium samples. Higher bond strength was obtained for sandblasted samples treated by oxidizing agent.
Coelho et al. [9] achieved better bond strength on using 10% aqueous solution of KMnO4 for 2 min as compared to acidic solution, because aqueous solution of KMnO4 was found to be more innocuous and produced an effective oxide layer.
After surface treatments, the castings were ultrasonically cleaned to remove the debris, as it might weaken the interfacial resin bond. To avoid the variation in proportioning the rate of spatulation, mixing consistency, time lapsed, the capsulated form of Fuji PLUS resin modified glass ionomer luting cement was used to cement all the castings with their respective tooth samples over dentin following manufacturers’ instructions [12].
The cemented samples were then stored in distilled water at room temperature for 24 h [19] to simulate oral environment, as cemented crowns will come in contact with water contents of saliva. As the pH of saliva changes, the solution of KMnO4 can also be made acidic. However, based on the findings of Coelho et al. [9], instead of acidic KMnO4, aqueous KMnO4 was used in this study.
The results in this study showed differences in the bond strength values when nickel–chromium metal ceramic discs were cemented with resin-modified glass ionomer cement, after various surface treatments. Differences within the groups may be due to the film thickness of cement and differences in surface roughness of the metal discs, though uniformity in preparation of samples was maintained.
The increased tensile bond strength with diamond abrasives points may be due to the irregularities in the form of scratches and cuts produced on the surface of the metal discs whereas, the layer of oxides during porcelain firing along with the salts formed by the action of KMnO4 might have resulted in easy debonding of the test samples of Group SK.
The increased shear bond strength may be mainly due to the roughness with diamond abrasives and large surface area for oxide formation. Because of the release of nascent oxygen, even distribution of oxide layer was there in samples treated with diamond abrasives.
Statistical analysis of mean tensile and shear bond strength values of different groups showed statistically significant difference between the groups. This difference between the groups may be due to the difference in the amount of surface roughness caused by various surface treatments. This shows that surface treatment affects the bond strength values and the differences in mean and standard deviation are found to be significant.
The reaction of KMnO4 with nickel and chromium ions with nascent oxygen released by KMnO4 might have resulted in metallic bond of resinous matrix as well as carboxyl group from the glass ionomer cores. The filler particles from unreacted particles of alumino silicate component might also have been responsible for increased tensile and shear bond strengths in these groups.
Limitations
Relatively small sample size was the main limitation of the study.
The intraoral conditions like unlimited thermocycling and repeated occlusal stresses which could lead to fatigue failure of the luting agent were not included in the study [19, 20].
Unidirectional pull of samples for dislodging the nickel–chromium specimens was employed in this study. However it was purposely selected to eliminate the combined effect of multiaxial walls existing in the cylindrical form of artificial crowns.
Finally, the variations can occur in surface roughness of the samples within a group, film thickness of luting cement used [21], the environmental conditions like humidity and temperature [20, 21], which led to variations in magnitude of bond strengths observed in this study though uniform methodology was employed while preparing the samples.
Mechanical mixing of capsules may result in the incorporation of air porosity in the cement, leading to weakening of the bond strength [11].
Conclusion
Within the parameters of this study, following conclusions were drawn.
Diamond abrasives and Potassium permanganate are cost effective methods over sandblasting in the operatory which can be successfully used for surface treatment of nickel–chromium metal ceramic alloy.
Tensile bond strength values are found to be highest for samples which were unsandblasted and roughened with diamond abrasive points and lowest for sandblasted and treated with 10% aqueous solution of KMnO4 samples.
Shear bond strength values are found to be highest for samples which were unsandblasted, roughened with diamond abrasive points and treated with 10% aqueous solution of KMnO4 and lowest for unsandblasted samples.
The Tensile and Shear bond strength values of resin-modified glass ionomer cement were more for sandblasted samples as compared to unsandblasted samples and differed significantly in Groups U, S, SK, UD and UDK.
The Tensile and Shear bond strength values of resin-modified glass ionomer cement were found to be more for sandblasted samples as compared to sandblasted and immersed in potassium permanganate solution and differed significantly in Groups U, S, SK, UD and UDK.
Immersion in aqueous solution of potassium permanganate after having surface roughness, with diamond abrasives, enhances the shear bond strength between metal and resin-modified glass ionomer cement.
The optimum bond strength values for clinical success needs to be ascertained for different alloys as well as different luting agents.
Acknowledgment
The author acknowledges Dr. Anurag Hasti, Mr. Monal Hasti and Dr. Nidhi Gupta for their help during the study.
References
- 1.Rubo JH, Pegoraro LF. Tensile bond strength of a composite resin cement for bonded prosthesis to various dental alloys. J Prosthet Dent. 1995;74:230–234. doi: 10.1016/S0022-3913(05)80128-3. [DOI] [PubMed] [Google Scholar]
- 2.Kolodney H, Puckett AD, Breazeale MS, Patterson KL, Lentz DL. Shear bond strengths of prosthodontic adhesive systems to a nickel–chromium–beryllium alloy. Quintessence Int. 1992;23:65–69. [PubMed] [Google Scholar]
- 3.Rubo JH, Pegoraro LF, Marolato F, Rubo MHM. The effect of tin-electroplating on the bond of four dental alloys to resin cement: an in vitro study. J Prosthet Dent. 1998;80:27–31. doi: 10.1016/S0022-3913(98)70087-3. [DOI] [PubMed] [Google Scholar]
- 4.Imbery TA, Davis RD. Evaluation of tin plating systems for a high-noble alloy. Int J Prosthodont. 1993;6:55–59. [PubMed] [Google Scholar]
- 5.Kohli S, Levine WA, Grisius RJ, Fenster RK. The effect of three different surface treatments on the tensile strength of the resin bond to nickel chromium beryllium alloy. J Prosthet Dent. 1990;63:4–8. doi: 10.1016/0022-3913(90)90255-B. [DOI] [PubMed] [Google Scholar]
- 6.Re GJ, Kaiser DA, Malone WFP. Shear bond strengths and scanning electron microscope evaluation of three different retentive methods for resin-bonded retainers. J Prosthet Dent. 1988;59:568–573. doi: 10.1016/0022-3913(88)90071-6. [DOI] [PubMed] [Google Scholar]
- 7.Anusavice KJ. Phillips science of dental materials. 12. Philadelphia: W.B. Saunders; 2003. [Google Scholar]
- 8.Rosenstiel S, Land MF, Fujimoto J. Contemporary fixed prosthodontics. 3. St. Louis: Mosby; 2001. [Google Scholar]
- 9.Coehlo CMP, Rubo JH, Pegoraro LF. Tensile bond strength of a resinous cement to a nickel chromium alloy modified with five surface treatments. J Prosthet Dent. 1996;76:246–249. doi: 10.1016/S0022-3913(96)90166-3. [DOI] [PubMed] [Google Scholar]
- 10.Campbell SD, Pelletier LB. Thermal cycling distortion of metal ceramics: part I—metal collar width. J Prosthet Dent. 1992;67:603–608. doi: 10.1016/0022-3913(92)90155-4. [DOI] [PubMed] [Google Scholar]
- 11.Nomoto R, Komoriyama M, McCabe JF, Hirano S. Effect of mixing method on the porosity of encapsulated glass ionomer cement. Dent Mater. 2004;20:972–978. doi: 10.1016/j.dental.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 12.GC Fuji PLUS. Product and Instruction manual
- 13.Livaditis GJ. A chemical etching system for creating micromechanical retention in resin bonded retainers. J Prosthet Dent. 1986;86:181–188. doi: 10.1016/0022-3913(86)90468-3. [DOI] [PubMed] [Google Scholar]
- 14.Livaditis GJ, Tate DL. Gold plating etched metal surfaces of resin bonded retainers. J Prosthet Dent. 1988;59(2):153–158. doi: 10.1016/0022-3913(88)90006-6. [DOI] [PubMed] [Google Scholar]
- 15.Tanaka T, Atsuta M, Nakabayashi N, Masuhara E. Surface treatment of gold alloys for adhesion. J Prosthet Dent. 1988;60(3):271–279. doi: 10.1016/0022-3913(88)90267-3. [DOI] [PubMed] [Google Scholar]
- 16.Wilson AD. Resin modified glass ionomer cements. Int J Prosthodont. 1990;3:425–429. [PubMed] [Google Scholar]
- 17.Tanaka T (1981) 4-META opaque resin—a new resin strongly adhesive to nickel–chromium alloy. J Prosthet Dent [DOI] [PubMed]
- 18.Tanaka T, Fujiyama E, Shimizu H, Takaki A, Atsuta M. Surface treatment of nonprecious alloys for adhesion fixed partial dentures. J Prosthet Dent. 1986;55(4):456–462. doi: 10.1016/0022-3913(86)90176-9. [DOI] [PubMed] [Google Scholar]
- 19.Ishijima T, Caputo AA, Mito R. Adhesion of resin to casting alloys. J Prosthet Dent. 1992;67:445–449. doi: 10.1016/0022-3913(92)90070-Q. [DOI] [PubMed] [Google Scholar]
- 20.Ergin S, Gemalmaz D. Retentive properties of five different luting cements on base and noble metal copings. J Prosthet Dent. 2002;88:491–497. doi: 10.1067/mpr.2002.129090. [DOI] [PubMed] [Google Scholar]
- 21.Mota CS, Demarco FF, Camacho GB, Powers JM. Tensile bond strength of four resin luting agents bonded to bovine enamel and dentin. J Prosthet Dent. 2003;89:558–564. doi: 10.1016/S0022-3913(03)00177-X. [DOI] [PubMed] [Google Scholar]