Abstract
Background
While studies have demonstrated higher medium-term mortality for community-acquired pneumonia (CAP), mortality and costs have not been characterized for health-care-associated pneumonia (HCAP) over a one-year period.
Methods
We conducted a retrospective cohort study to evaluate mortality rates and health-system costs for patients with CAP or HCAP during initial hospitalization and for one year after hospital discharge. We selected 50,758 patients admitted to the Veterans Affairs (VA) health care system between October, 2003 and May, 2007. Main outcome measures included hospital, post-discharge and cumulative mortality rates and cost during initial hospitalization and at 12 months following discharge.
Results
Hospital and one-year HCAP mortality were nearly twice that of CAP. HCAP was an independent predictor for hospital (odds ratio (OR): 1.62, 95% confidence interval (CI): 1.49–1.76) and one-year mortality (OR: 1.99, 95% CI: 1.87–2.11) when controlling for demographics, comorbidities, pneumonia severity and factors associated with multidrug resistant infection including immune suppression, previous antibiotic treatment and aspiration pneumonia. HCAP patients consistently had higher mortality in each stratum of the Charlson-Deyo-Quan comorbidity index. HCAP patients incurred significantly greater cost during the initial hospital stay and in the following 12 months. Demographics and comorbid conditions, particularly aspiration pneumonia, accounted for 19–33% of this difference.
Conclusion
HCAP represents a distinct category of pneumonia with particularly poor survival up to one year after hospital discharge. While comorbidities, pneumonia severity and risk factors for multidrug resistant infection may interact to produce even higher mortality compared to CAP, they alone do not explain the observed differences.
Keywords: PNEUMONIA, HEALTH CARE DISPARITIES, NOSOCOMIAL INFECTION, COMMUNITY-ACQUIRED PNEUMONIA, CAP, HCAP
Introduction
Pneumonia is the leading cause of infectious disease related death, with a financial impact exceeding $8 billion dollars.1, 2 For nearly two decades, it has been recognized that patients previously classified with community-acquired pneumonia (CAP) admitted from a nursing home or those frequently exposed to the health care system suffered a disproportionally higher morbidity and mortality.3 Accordingly, multiple schemes were developed to better identify these patients; in 2005 the American Thoracic Society (ATS) with the Infectious Disease Society of America (IDSA) defined a new category for lower respiratory tract infections termed health-care-associated pneumonia (HCAP).4 HCAP is defined as pneumonia in a non-hospitalized person with at least one of the following characteristics: 1) residing in a nursing home or long-term care facility; 2) being hospitalized within the prior 90 days; 3) receiving intravenous therapy, wound care or intravenous chemotherapy within the prior 30 days; or 4) receiving hemodialysis within the previous 30 days.4
The rising incidence of bacterial resistance to previously effective antibiotics, and the frequent emergence of novel respiratory infections are leading to an increasing prevalence of pneumonia.5 Because of the expanding elderly population, this increase may disproportionately include disease likely to be classified as HCAP. Many studies have demonstrated that HCAP portends a significantly poorer hospital survival than CAP (10% vs. 4%).6–9 After discharge patients with CAP continue to suffer substantial health burden, with one year mortality rates up to 41%.10–12 Yet, little is known regarding post discharge mortality among HCAP patients, and no studies have evaluated the one-year differences in clinical and financial outcomes between these two entities. Moreover, controversy exists regarding the clinical validity of the ATS/IDSA HCAP classification,3 meaning that clinical practice may vary widely, leading to over or under treatment, each with potential to substantially impact patient survival.
The Department of Veterans Affairs (VA) health care system comprises over 150 acute-care hospitals throughout the United States and Puerto Rico. It has a uniform electronic health record and collects encounter-level cost data. The VA system provides a unique opportunity to study the epidemiology of pneumonia with adequate numbers of patients to address the effects of multiple covariates including immune suppression, prior antibiotic use, and aspiration pneumonia, which are related to infection with multidrug resistant pathogens.6, 13, 14 Herein, we evaluated mortality and VA health care cost during the index hospital stay and for one year after discharge among patients admitted to all VA hospitals with pneumonia during the years 2003–2007. In addition, we evaluated the clinical validity of the ATS/IDSA HCAP classification. We hypothesized that the one-year mortality rate and VA costs would be significantly higher for HCAP patients than for CAP patients after controlling for demographic and clinical variables.
Methods
Design, Setting, and Participants
We performed a retrospective analysis of hospital discharge records from all acute-care hospitals in the VA system. This analysis was conducted with approval from the Stanford University institutional review board (approval number 13980).
Definitions
A pneumonia patient was defined as any person admitted to an acute care hospital with an admission and discharge diagnosis of pneumonia (International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 480–483, 485–487.0) or with a discharge diagnosis of pneumonia and an admission diagnosis of decompensated chronic obstructive pulmonary disease (COPD) with acute exacerbation (491.21), asthma (493.9), food/vomitus pneumonitis (507), acute respiratory failure (518.81), acute respiratory distress (518.82), or other respiratory distress/insufficiency (786.09).11 We then applied three exclusion criteria: transfer from another hospital, less than 48 hours of antimicrobial therapy upon hospital admission, and admission within seven days of a prior VA hospital stay.
HCAP was defined according to ATS/IDSA criteria, as pneumonia occurring outside the hospital setting in a patient who had at least one of four criteria: 1) a VA-funded inpatient hospitalization within 90 days prior to the index hospitalization, 2) admission from a VA-funded long-term care stay, 3) VA-funded hemodialysis within the prior 30 days, or 4) VA-funded wound care, intravenous therapy or chemotherapy within prior 30 days. VA-funded care occurs primarily at VA facilities but may be purchased on contract from other institutions.
Following ATS major criteria, we defined severe pneumonia as occurring when a patient received either a diagnosis of shock or invasive mechanical ventilation.15 We defined an intensive care unit (ICU) stay as one that occurred within 72 hours of hospital admission, increasing the likelihood that the ICU admission was due to pneumonia acquired outside the hospital setting. We stratified data by factors previously associated with an increased risk of multidrug resistant infection (MDRI) including immune suppression, aspiration pneumonia (507), and antibiotic use (any class) in the 6 months prior to hospitalization.3,6,13,14 Immune suppression was defined as an admission or discharge diagnosis of neutropenia (288.00) during the index hospitalization, a previous history of HIV-infection (042), a history of any solid organ (v42) or hematopoietic stem cell transplantation (HSCT) (41.0), or prednisone use (>20mg) for greater than 3 weeks in the year prior to hospitalization. While hospitalization in the previous 90 days is also associated with MDRI, we chose not to stratify by this parameter, as it is an integral part of the case definition for HCAP.4, 6,14
Data Sources
Clinical and demographic data came from the VA Medical SAS Inpatient Dataset (“PTF”) and Outpatient Dataset (“OPC”).16 Financial data were drawn from the VA Health Economics Resource Center (HERC) Inpatient and Outpatient Average Cost files, which link to PTF and OPC.17,18 By construction there is a one-to-one match of the HERC data to inpatient stays recorded in PTF.19 Outpatient pharmacy costs, lacking in the HERC data, were extracted from the VA Decision Support System.20 Death during the hospital stay was indicated in the inpatient (PTF) encounter record. One-year mortality was obtained from the VA Beneficiary Identification and Record Locator Subsystem (BIRLS).21 Data from BIRLS and PTF are combined with Medicare data to create the VA Vital Status file. Relative to the National Death Index the VA Vital Status file has 98.3% sensitivity and 97.6% exact agreement with dates.22
Statistical Methods
Outcomes of interest were hospital mortality; one-year mortality among patients discharged from their indexed hospital admission (termed “one-year post-discharge mortality”); and one-year cumulative mortality, which included mortality during or after hospitalization. We extracted clinical, demographic, and cost data for each pneumonia-related inpatient stay having admission and discharge dates between October, 2003 and the end of May, 2007. We selected only the first qualifying event for each individual. To classify comorbid illness we used the enhanced version of the Charlson-Deyo comorbidity index developed by Quan et al., termed the “Charlson-Deyo-Quan (CDQ) comorbidity index.”23 Costs were converted to 2008 dollars using the Consumer Price Index.
We calculated descriptive statistics for demographic, clinical, and cost variables by pneumonia status. Chi-square, log-rank and t-tests were employed as appropriate. We used Kaplan-Meier curves and logistic regression to assess the relation of HCAP and CAP to hospital and 12-month survival controlling for clinical covariates including age, CDQ comorbidity index, ICU admission, pneumonia severity and factors associated with MDRIs. Analyses were carried out in SAS 9.1 (SAS Institute, Cary, NC). We estimated the marginal effect of HCAP on cost using regression analysis with the previously described covariates. Model selection followed standard methods.24, 25 Regression analyses were performed in Stata 11 (StataCorp LP, College Station, TX).
Results
Patient Characteristics
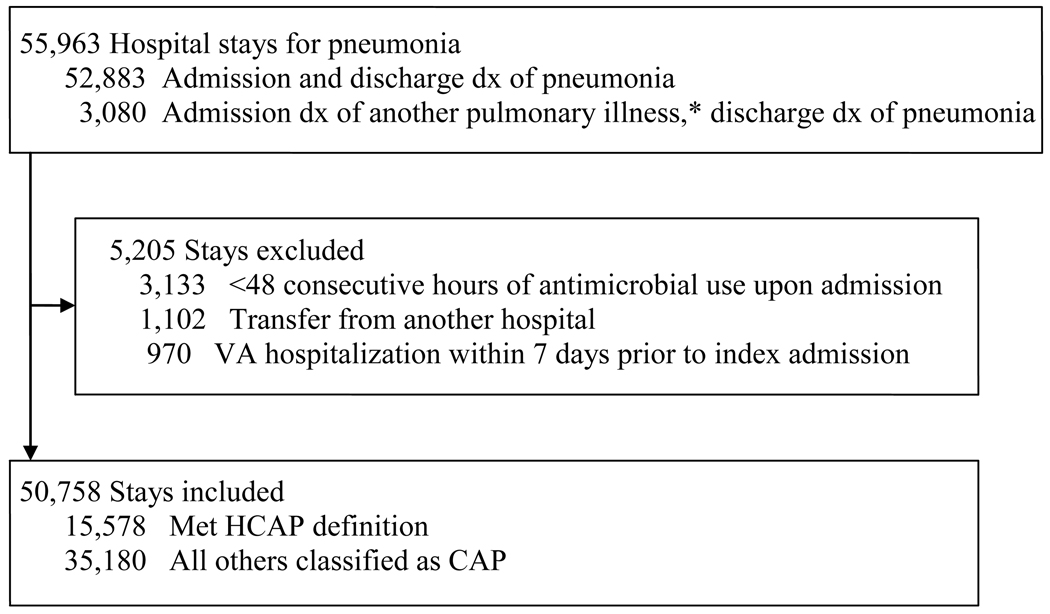
A total of 55,963 patients met entry criteria. After exclusions the final sample numbered 50,758 stays, of which 15,578 (30.7%) qualified as HCAP and 35,180 as CAP (Figure 1). Table 1 presents demographic and clinical characteristics of the study sample. ICU admission and mechanical ventilation were more common among HCAP patients (19.3% and 9.7%, respectively) than CAP patients (15.2% and 7.6%, respectively). The CDQ comorbidity score averaged 3 in HCAP patients and 2.5 among CAP patients.
Figure 1.
Selection of Hospital Stays
* Includes decompensated chronic obstructive pulmonary disease with acute exacerbation (491.21), asthma (493.9), food/vomitus pneumonitis (507), acute respiratory failure (518.81), acute respiratory distress (518.82), or other respiratory distress/insufficiency (786.09).
Table 1.
Patient characteristics by HCAP status †
| CAP patients | HCAP patients | |
|---|---|---|
| (N = 35,180) | (N = 15,578) | |
| Age (years) | 69.2 ± 12.9 | 70.3 ± 12.3 |
| Male gender (%) | 97.0 | 97.4 |
| Comorbidity score* (%) | ||
| 0 | 10.79 | 5.10 |
| 1 | 19.12 | 13.97 |
| 2 | 23.97 | 21.64 |
| 3+ | 46.11 | 59.30 |
| Mean comorbidity score* | 2.5 ± 1.6 | 3.0 ± 1.6 |
| ICU Admission (%) | 15.2 | 19.3 |
| Mechanical ventilation (%) | 7.6 | 9.7 |
| Severe Pneumonia (%) | 6.2 | 8.1 |
| Aspiration Pneumonia (%) | 1.1 | 2.3 |
| Immune Suppression (%) | 7.4 | 20.7 |
| Prior Antibiotics (%) | 28.4 | 58.6 |
Differences between CAP and HCAP were all statistically significant p<.01
Based on Charlson-Deyo-Quan comorbidity index score
Hospital Mortality
Hospital mortality rates were nearly two-fold higher among HCAP patients within every stratum with the exception of patients admitted to the ICU, those with severe pneumonia, immune suppression or aspiration pneumonia (Table 2). Highest hospital mortality was observed among HCAP patients with severe pneumonia (38.2%). After adjustment for demographic and clinical factors, HCAP relative to CAP was an independent predictor of hospital mortality (odds ratio (OR) 1.62; 95% confidence interval (CI): 1.49–1.76).
Table 2.
Hospital and One-Year Mortality by HCAP Status†
| Hospital Mortality (%) |
One-Year Post-discharge Mortality (%) § |
One-Year Cumulative Mortality (%) |
||||
|---|---|---|---|---|---|---|
| Characteristic | CAP | HCAP | CAP | HCAP | CAP | HCAP |
| All patients | 5.0 | 9.9 | 17.0 | 34.4 | 21.2 | 40.9 |
| Age range, y | ||||||
| <50 | 1.2 | 4.2 | 5.0 | 14.5 | 6.1 | 18.0 |
| 50–59 | 2.8 | 6.2 | 10.1 | 27.5 | 12.5 | 31.9 |
| 60–69 | 4.2 | 8.4 | 12.6 | 30.6 | 16.3 | 36.5 |
| 70–79 | 5.7 | 11.0 | 19.1 | 36.5 | 23.8 | 43.4 |
| 80–89 | 7.5 | 13.2 | 26.0 | 43.1 | 31.5 | 50.6 |
| 90+ | 9.4 | 16.3 | 36.7 | 51.4 | 42.7 | 59.3 |
| Sex | ||||||
| Male | 5.1 | 10.1 | 17.3 | 34.8 | 21.5 | 41.4 |
| Female | 2.4 | 4.9 | 7.8 | 19.6 | 10.0 | 23.6 |
| Comorbidity score* | ||||||
| 0 | 3.3 | 8.4 | 8.0 | 18.0 | 10.9 | 24.7 |
| 1 | 4.4 | 9.9 | 14.1 | 31.4 | 17.9 | 38.2 |
| 2 | 5.0 | 9.3 | 16.2 | 33.6 | 20.4 | 39.7 |
| >3 | 5.8 | 10.3 | 20.8 | 36.9 | 25.4 | 43.4 |
| MDRI Risk Factors** | ||||||
| Aspiration Pneumonia | 16.5 | 22.3 | 30.5 | 51.2 | 41.9 | 62.1 |
| Immune Suppression | 9.3 | 13.7 | 26.2 | 42.3 | 32.9 | 50.2 |
| Prior Antibiotics | 4.8 | 10.5 | 18.2 | 36.7 | 22.2 | 43.3 |
| Pneumonia severity# | ||||||
| Less severe Pneumonia | 3.4 | 7.5 | 16.7 | 33.9 | 19.5 | 38.9 |
| Severe Pneumonia | 30.3 | 38.2 | 22.9 | 42.2 | 46.2 | 64.1 |
| ICU status | ||||||
| Non-ICU | 2.9 | 6.6 | 16.4 | 33.2 | 18.8 | 37.6 |
| ICU | 17.2 | 23.9 | 21.0 | 40.6 | 34.6 | 54.8 |
One-year Post Discharge Mortality
A greater than 1.6-fold mortality difference one-year after hospital discharge was observed in all strata with the exception of patients older than 90 years (Table 2). After controlling for demographics, ICU admission, pneumonia severity, immune suppression, aspiration pneumonia, treatment with antibiotics in the 6 months prior to hospital admission and CDQ comorbidity index, HCAP relative to CAP was still associated with increased mortality at one year (OR 1.99, 95% CI: 1.87–2.11).
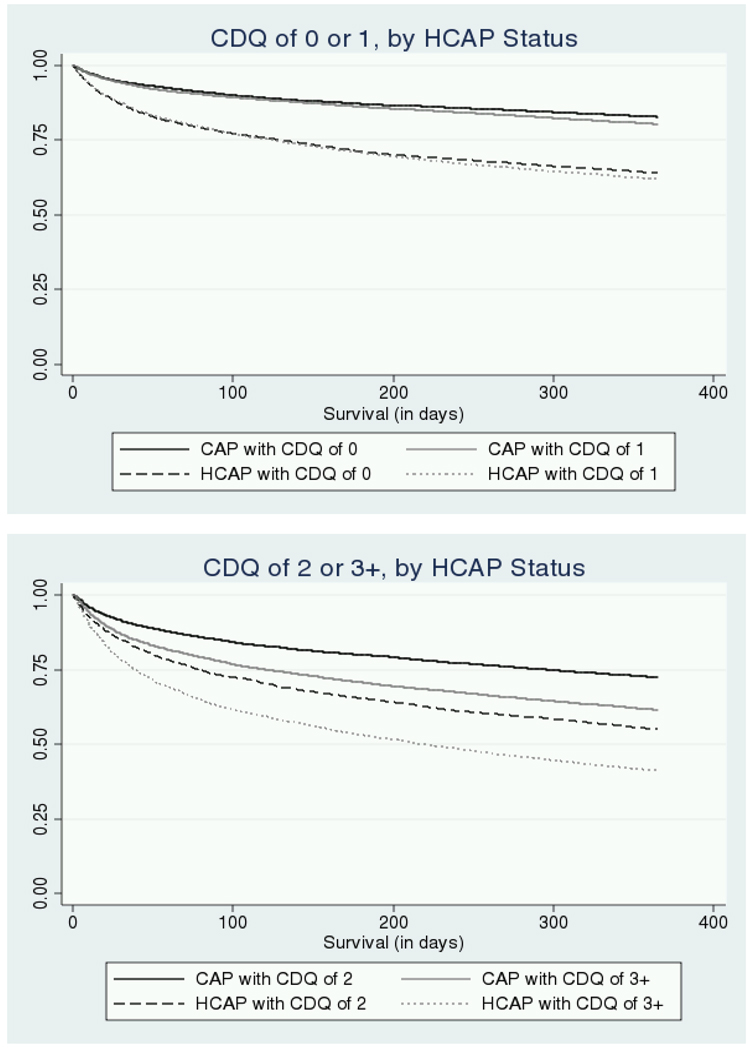
One-year Cumulative Mortality
HCAP patients experienced higher one-year cumulative mortality rates than CAP patients within every stratum (Table 2). Figure 2 presents Kaplan-Meier survival curves by pneumonia category and CDQ comorbidity score. For patients with CDQ comorbidity scores of 2 or more, the survival gap between CAP and HCAP patients begins immediately and widens over time. All HCAP-CAP comparisons were significant (p<.05) by log-rank test.
Figure 2.
Kaplan-Meier Survival Curves by HCAP Status and Comorbidity Score*
Notes: CAP= Community-acquired pneumonia; HCAP=Health-care-associated Pneumonia; CDQ = Charlson-Deyo-Quan comorbidity index score
* All HCAP-CAP comparisons were significant (p<.05) by log-rank test.
Factors associated with Multidrug Resistant Infection
Risk factors associated with MDRIs were more prevalent in HCAP patients (Table 1). When the data was stratified by aspiration pneumonia or immune suppression the mortality difference between HCAP and CAP decreased to 1.4-fold (Table 2). Stratification by prior antibiotic use did not change the 2-fold mortality difference between HCAP and CAP. After hospital discharge, having a history of aspiration pneumonia was associated with some of the highest cumulative one-year mortality rates (62.1%).
Health System Costs
On average HCAP stays were 1.6 days (23%) longer and cost $3,640 (31%) more than CAP stays (for both differences, p<.01, Table 3). In regression analysis, the marginal effect of HCAP was to add $2,809 (25%) to the cost of the initial hospital stay. Among patients alive at discharge, the estimated cost of VA health care in the following year averaged $45,594 for CAP patients and $80,861 for HCAP patients. Controlling for differences in demographics and comorbid conditions, HCAP was associated with additional costs of $23,060 (52%) over that period and reduced the HCAP-CAP difference by 19% in the initial stay and 33% at 12 months among survivors.
Table 3.
VA Cost by HCAP Status and Clinical Characteristic*
| CAP | HCAP | |
|---|---|---|
| Initial Hospital Stay | ||
| LOS (days) | 6.8 ± 12.4 | 8.5 ± 18.1 |
| VA cost | $11,603 ± $39,841 | $15,243 ± $39,794 |
| Marginal effect** | -- | $2,809 |
| First Year after Discharge | ||
| VA cost | $45,594± $151,733 | $80,861 ± $169,321 |
| Marginal effect** | -- | $23,060 |
Mean differences and marginal effects are all statistically significant (p<.01).
Coefficient on HCAP from a regression model controlling for demographic and clinical characteristics.
Discussion
In 50,758 patients treated for pneumonia in the VA, we detected a nearly two-fold overall mortality difference between HCAP and CAP patients up to one year after discharge. This difference, which corroborates and extends prior research showing higher hospital mortality among HCAP than CAP patients,7, 26 persisted after consideration of age, gender, comorbidity score, pneumonia severity, ICU status and factors associated with MDRIs. Our findings lend further support to classifying HCAP as a distinct category of lower respiratory tract infection.
In previous studies hospital mortality among CAP patients ranged from 4.3% to 10%.6–9, 26 While our CAP findings are consistent, the hospital mortality we observed for HCAP patients (9.9%) is lower than results from several earlier, smaller studies (17% to 25%).6, 8, 26, 27 This difference may reflect substantial variability in the definition of HCAP among studies.3 For example, in the study demonstrating the highest hospital mortality, HCAP was expansively defined, including a wide variety of immune suppressed patients.6 As 39% of HCAP patients in this study were immune suppressed, it is not surprising that mortality was particularly high in this cohort. In a prospective study with strictly defined ATS/IDSA HCAP criteria, the 30-day mortality of 10.3% was similar to that observed in the current study.9
Persistence of a mortality difference between HCAP and CAP patients after controlling for comorbidities, pneumonia severity and MDRI risk factors suggests that the difference is related to pneumonia category rather than simply a higher prevalence of comorbidities or more severe illness in one group. While it is not surprising that HCAP patients have a higher mortality, as they are by definition more debilitated by comorbidities, it was unexpected that the nearly two-fold mortality difference decreased only at extremes of illness, age (>90 years old) or comorbidity status (CDQ ≥ 3). The persistence of a mortality difference between HCAP and CAP suggests that the current HCAP/CAP classification is an important discriminator for mortality that diminishes only when other well described risk factors (age, CDQ score) increase mortality for the entire cohort. Thus, while these factors may produce even greater reductions in survival compared to CAP, they alone do not explain the observed mortality differences. Although we are unable to completely elucidate these differences in our administrative database, it may require extensive chart review or prospective study to clarify the relative contribution of these factors.
It has been suggested by previous in-hospital HCAP studies that the difference in part may be related to initial inappropriate antibiotics.6,7 In a retrospective analysis by Micek et al., use of inappropriate antibiotics was more common in HCAP patients and was an independent risk factor for mortality (adjusted OR: 2.19; 95% CI: 1.27–3.78).6 Similarly, we found that the mortality gap between CAP and HCAP decreased after controlling for severe pneumonia, immune suppression and aspiration pneumonia, three factors that have been associated with increased risk for infection with multidrug resistant pathogens. Because patients with MDRIs have a higher risk of initial inappropriate antibiotic therapy this may in part explain some of the mortality differences between pneumonia categories. Unfortunately we were unable to directly evaluate this hypothesis with our data. Alternatively, mortality may differ by differential pneumonia severity, criteria for ICU admission, or prevalence of culture positivity, as observed in smaller prospective analyses.27, 28
Greater costs for HCAP patients were due in part to demographic and clinical differences. Controlling for covariates reduced the HCAP-CAP cost difference by 19% in-hospital and by 33% at one-year. We believe that residual differences are due to the higher mortality rate among HCAP patients coupled with greater intensity and cost of health care services around the time of death.
To our knowledge, this is the first study to characterize the one-year clinical and financial impact of HCAP. The study’s strength lies in our strictly defined HCAP definition and in the large sample size, which allowed us to adjust for multiple covariates in our analysis. However, several study limitations deserve mention. Two are specific to the VA: nearly all patients were male, and analyses could not be stratified by race due to incomplete data. Thus, the external generalizability of our results is uncertain. In addition, the use of ICD-9-CM codes to define disease may have led to misclassification bias, although our inclusion and exclusion criteria and large sample size may have lessened the impact of misclassification. Multiple studies have shown that ICD-9 codes for pneumonia compared with chart review demonstrate moderately high sensitivity for detecting CAP.29–31 Toward this end, the proportion of HCAP patients (30.7%) reported in this study is similar to that reported in a prospective, multicenter, point prevalence study (28%).26 Although we were unable to classify patients in this administrative database by their functional status, an independent risk factor for multidrug resistant pathogens, we did stratify our data by the incidence of aspiration pneumonia.3 Studies have shown that dependency for feeding (a marker of poor functional status) also is a risk factor for aspiration pneumonia.3, 32 Thus, at least one aspect of functional status could be investigated and did correlate with our primary findings. Another potential limitation was our inability to identify patients with “do not resuscitate” orders, which would limit aggressiveness of treatment and may differentially impact survival. In contrast to previous HCAP studies, rates of ICU admission and mechanical ventilation were higher in HCAP than CAP patients, suggesting that a treatment ceiling effect potentially more prevalent in HCAP patients did not substantially bias our results.9, 28
In conclusion, this study supports HCAP as a distinct category by showing it is associated with particularly poor survival up to one year after hospital discharge and that HCAP patients create substantially greater costs for the health care system. The mortality difference between CAP and HCAP persisted after controlling for multiple demographic and clinical factors, including factors associated with MDRIs. HCAP patients admitted to the ICU with severe pneumonia represented a sub-group with particularly high mortality. Knowledge of this disparity may help improve post discharge surveillance and palliative care in patients with low probability for survival. Further study is needed to evaluate whether inappropriate antibiotic use among patients with HCAP contributes to the observed mortality difference between CAP and HCAP.
Acknowledgements
Dr. Mei-Chiung Shih for her careful read of the manuscript.
Funding/Support: JH is funded through a National Institute of Health training grant [T32 HL007948-07]; and AMS, MWS, MH, and GUM received funding from the Cooperative Studies Program of the U.S. Department of Veterans Affairs [CSP 574].
Role of sponsor: The funders had no involvement in the design and conduct of the study; collection, management, analysis and interpretation of the data; or preparation, review or approval of the manuscript.
Abbreviation List
- ATS
American Thoracic Society
- BIRLS
Beneficiary Identification and Record Locator Subsystem
- CAP
Community-acquired pneumonia
- CDQ-index
Charlson-Deyo-Quan comorbidity index
- COPD
Chronic obstructive pulmonary disease
- HERC
Health Economics Resource Center
- HSCT
Hematopoietic stem cell transplant
- IDSA
Infectious Disease Society of America
- HCAP
Health-care-associated pneumonia
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- ICU
Intensive care unit
- MDRI
Multidrug resistant infection
- OPC
Outpatient care file
- PTF
Patient treatment file
- VA
Veterans Affairs
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Institution(s) at which work was performed: Stanford University Medical Center and the Health Economics Resource Center, Veterans Affairs, Palo Alto Health Care System.
Disclosures: None to report.
Author Contributions: Dr. Hsu had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Specific Contributions:
Study concept and design: Hsu, Siroka, Smith, Holodniy, Meduri.
Acquisition of data: Hsu, Siroka, Smith
Analysis and interpretation of data: Hsu, Siroka, Smith, Holodniy, Meduri.
Drafting of manuscript: Hsu, Siroka, Smith, Holodniy, Meduri.
Critical revision of manuscript for important intellectual content: Hsu, Siroka, Smith, Holodniy, Meduri.
Statistical analysis: Siroka, Smith.
Obtaining funding: Smith, Holodniy, Meduri.
Administrative, technical, or material support: Hsu, Siroka, Smith
Study supervision: Holodniy, Meduri.
Conflicts of Interest Statement:
No conflicts exist for any of the authors.
Disclaimer: The views expressed herein are those of the authors and not necessarily those of the Department of Veterans Affairs or Stanford University School of Medicine.
Ethical Approval: The work has been approved by the Department of Veterans Affairs Cooperative Studies Program.
Contributor Information
Andrew M. Siroka, Email: andrew.siroka@va.gov.
Mark W. Smith, Email: mark.smith9@va.gov.
Mark Holodniy, Email: mark.holodniy@va.gov.
G. Umberto Meduri, Email: gmeduri@uthsc.edu.
References
- 1.Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. Natl Vital Stat Rep. 2009;57(14):1–134. [PMID: 19788058] [PubMed] [Google Scholar]
- 2.Niederman MS, McCombs JS, Unger AN, Kumar A, Popovian R. The cost of treating community-acquired pneumonia. Clin Ther. 1998;20(4):820–837. doi: 10.1016/s0149-2918(98)80144-6. [PMID: 9737840] [DOI] [PubMed] [Google Scholar]
- 3.Ewing S, Welte T, Chastre J, Torres A. Rethinking the concepts of community-acquired and health-care-associated pneumonia. Lancet Infect Dis. 2010;10:279–287. doi: 10.1016/S1473-3099(10)70032-3. [DOI] [PubMed] [Google Scholar]
- 4.American Thoracic Society and the Infectious Disease Society of America Documents. Niederman MS, Craven DE Co-chairs. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and health-care-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 5.Mizgerd JP. Lung infection – a public health priority. PLoS Med. 2006;3(2):376. doi: 10.1371/journal.pmed.0030076. Epub 2006 Jan 17. [PMID 16401173] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Micek ST, Kollef KE, Reichley RM, Roubinian N, Kollef MH. Health care-associated pneumonia and community-acquired pneumonia: a single-center experience. Antimicrob Agents Chemother. 2007;51(10):3568–3573. doi: 10.1128/AAC.00851-07. [PMID: 17682100] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. Epidemiology and outcomes of health care–associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005;128(6):3854–3862. doi: 10.1378/chest.128.6.3854. [DOI] [PubMed] [Google Scholar]
- 8.Kothe H, Bauer T, Marre R, Suttorp N, Welte T, Dalhoff K. Outcome of community-acquired pneumonia: influence of age, residence status and antimicrobial treatment. Eur Respir J. 2008;32:139–146. doi: 10.1183/09031936.00092507. [DOI] [PubMed] [Google Scholar]
- 9.Carratalà J, Mykietiuk A, Fernández-Sabé N, et al. Health care–associated pneumonia requiring hospital admission: epidemiology, antibiotic therapy, and clinical outcomes. Arch Intern Med. 2007;167:1393–1399. doi: 10.1001/archinte.167.13.1393. [DOI] [PubMed] [Google Scholar]
- 10.Hedlund J, Hansson L-O. Ortqvist A. Short- and long-term prognosis of middle-aged and elderly patients hospitalized with community-acquired pneumonia: impact of nutritional and inflammatory factors. Scand J Infect Dis. 1995;27(1):32–37. doi: 10.3109/00365549509018970. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan V, Clermont G, Griffin MF, et al. Pneumonia: still the old man's friend? Arch Intern Med. 2003;163(3):317–323. doi: 10.1001/archinte.163.3.317. [PMID: 12578512] [DOI] [PubMed] [Google Scholar]
- 12.Mortensen EM, Kapor WN, Chang CC, Fine MJ. Assessment of mortality after long-term follow-up of patients with community-acquired pneumonia. Clin Infect Dis. 2003;37(12):1617–1624. doi: 10.1086/379712. [PMID: 14689342] [DOI] [PubMed] [Google Scholar]
- 13.El Sohl AA, Pietrantoni C, Bhat A, Bhora M, Berbary E. Indicators of potentially drug-resistant bacteria in severe nursing home-acquired pneumonia. Clin Infect Dis. 2004;39:474–480. doi: 10.1086/422317. [DOI] [PubMed] [Google Scholar]
- 14.Brito V, Niederman MS. Healthcare-associated pneumonia is a heterogeneous disease, and all patients do not need the same broad-spectrum antibiotic therapy as complex nosocomial pneumonia. Curr Opin Infect Dis. 2009;22:316–325. doi: 10.1097/QCO.0b013e328329fa4e. [DOI] [PubMed] [Google Scholar]
- 15.Niederman MS, Mandell LA, Anzueto A, et al. Guidelines for the management of adults with community-acquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001;163:1730–1754. doi: 10.1164/ajrccm.163.7.at1010. [DOI] [PubMed] [Google Scholar]
- 16.VA Information Resource Center (VIReC), U.S. Department of Veterans Affairs. Medical SAS Datasets - description. Hines, Ill: VIReC; 2009. [accessed Mar. 22, 2010]. URL: http://www.virec.research.va.gov/DataSourcesName/Medical-SAS-Datasets/SAS.htm. [Google Scholar]
- 17.Barnett PG, Wagner TH. Using average cost methods to estimate encounter-level costs for medical-surgical stays in the VA. Med Car Res Rev. 2003;60(3 Suppl):15S–36S. doi: 10.1177/1077558703256485. [DOI] [PubMed] [Google Scholar]
- 18.Yu W, Wagner TH, Chen S, Barnett PG. Average cost of VA rehabilitation, mental health, and long-term hospital stays. Med Care Res Rev. 2003;60(3 Suppl):40S–53S. doi: 10.1177/1077558703256724. [DOI] [PubMed] [Google Scholar]
- 19.Wagner TH, Chow A, Barnett PG. HERC's Average Cost Datasets for VA Inpatient Care FY1998 - FY2008. Menlo Park, CA: VA Palo Alto, Health Economics Resource Center; 2009. [Google Scholar]
- 20.Smith MW, Joseph GJ. Pharmacy data in the VA health care system. Med Care Res Rev. 2003;60 3 Suppl:92S–123S. doi: 10.1177/1077558703256726. [DOI] [PubMed] [Google Scholar]
- 21.VA Information Resource Center (VIReC) A Vital Status Files. Hines, Ill.: VIReC; 2009. [accessed Nov. 4, 2009]. URL: http://www.virec.research.va.gov/DataSourcesName/VitalStatus/VitalStatus.htm. [Google Scholar]
- 22.Sohn MW, Arnold N, Maynard C, Hynes DM. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metr. 2006 April 10;4:2. doi: 10.1186/1478-7954-4-2. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 24.Manning WG, Mullahy J. Estimating log models to transform or not to transform? J Health Econ. 2001;20(4):461–494. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 25.Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24(3):465–488. doi: 10.1016/j.jhealeco.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 26.Venditti M, Falcone M, Corrao S, Licata G, Serra P. Outcomes of patients hospitalized with community-acquired, health care-associated, and hospital-acquired pneumonia. Ann Intern Med. 2009;150(1):19–26. doi: 10.7326/0003-4819-150-1-200901060-00005. [PMID: 19124816] [DOI] [PubMed] [Google Scholar]
- 27.Labelle AJ, Arnold H, Reichley RM, Micek ST, Kollef MH. A comparison of culture-positive and culture-negative health-care-associated pneumonia. Chest. 2010;137:1130–1137. doi: 10.1378/chest.09-1652. [DOI] [PubMed] [Google Scholar]
- 28.Rello J, Luján M, Gallego M, et al. Why mortality is increased in health-care-associated pneumonia: lessons from pneumococcal bacteremic pneumonia. Chest. 2010;137:1138–1144. doi: 10.1378/chest.09-2175. [DOI] [PubMed] [Google Scholar]
- 29.van de Garde EM, Oosterheert JJ, Bonten M, Kaplan RC, Leufkens HG. International classification of diseases codes showed modest sensitivity for detecting community-acquired pneumonia. J Clin Epidemiol. 2007;60(8):834–838. doi: 10.1016/j.jclinepi.2006.10.018. [PMID: 17606180] [DOI] [PubMed] [Google Scholar]
- 30.Aronsky D, Haug PJ, Lagor C, Dean NC. Accuracy of administrative data for identifying patients with pneumonia. Am J Med Qual. 2005;20:319–328. doi: 10.1177/1062860605280358. [DOI] [PubMed] [Google Scholar]
- 31.Whittle J, Fine MJ, Joyce DZ, et al. Community-acquired pneumonia: can it be defined with claims data? Am J Med Qual. 1997;12(4):187–193. doi: 10.1177/0885713X9701200404. [DOI] [PubMed] [Google Scholar]
- 32.Langmore SE, Skarupski KA, Park PS, Fries BE. Predictors of aspiration pneumonia in nursing home residents. Dsyphagia. 2002;17(4):298–307. doi: 10.1007/s00455-002-0072-5. [DOI] [PubMed] [Google Scholar]