Abstract
Background
The leading cause of injury death among adults in Connecticut (CT), USA is drug poisonings. We analyzed the epidemiology and geographic distribution of opioid-involved accidental drug-involved intoxication deaths (“overdoses”) in CT over an 11-year period.
Methods
We reviewed data from 1997 to 2007 on all adult accidental/undetermined drug intoxication deaths in CT that were referred to the Office of the Chief Medical Examiner (OCME). Regression analyses were conducted to uncover risk factors for fatal opioid-involved intoxications and to compare heroin- to prescription opioid- and methadone-involved deaths. Death locations were mapped to visualize differences in the geographic patterns of overdose by opioid type.
Results
Of the 2900 qualifying deaths, 2231 (77%) involved opioids. Trends over time revealed increases in total opioid-related deaths although heroin-related deaths remained constant. Methadone, oxycodone and fentanyl, the most frequently cited prescription opioids, exhibited significant increases in opioid deaths. Prescription opioid-only deaths were more likely to involve other medications (e.g., benzodiazepines) and to have occurred among residents of a suburban or small town location, compared to heroin-involved or methadone-involved deaths. Heroin-only deaths tended to occur among non-Whites, were more likely to involve alcohol or cocaine and to occur in public locations and large cities.
Conclusions
The epidemiology of fatal opioid overdose in CT exhibits distinct longitudinal, risk factor, and geographic differences by opioid type. Each of these trends has implications for public health and prevention efforts.
Keywords: overdose, opioid, mortality, prescription opioid, heroin
1. Introduction
Opioid drugs are vitally important for the treatment of pain, opioid dependence, and terminal illness but also have the potential to produce physical dependence, abuse, addiction, and overdose. An illegal opioid, heroin, is one of the most common drugs of abuse worldwide, nationally, and in New England(Substance Abuse and Mental Health Services Administration, 2009; UNODC, 2009). As with other states in New England, Connecticut (CT) witnessed a substantial increase in heroin abuse beginning in the early 1970’s with the most recent peak of heroin abuse coinciding with peak purity in 1999(Ciccarone, 2009; Ciccarone et al., 2009). More recently, and consistent with national trends, heroin abuse has been compounded by increasing levels of abuse of prescription opioids, including methadone(Paulozzi, 2006; Paulozzi et al., 2006a; Paulozzi et al., 2006b; Paulozzi et al., 2009; Paulozzi and Ryan, 2006; Spiller et al., 2009).
Vital statistic calculations indicate that as of 2006, mortality due to drug poisoning is the leading cause of injury death among adults in CT(Warner et al., 2009), with unintentional drug poisonings—“overdoses”-- claiming the lives of about one resident per day. Despite these alarming statistics, little is known about the epidemiology of fatal overdose in CT. One reason may be due to the data sources.
Publicly available surveillance sources inadequately track overdoses, and none collects data on events occurring in CT. The Centers for Disease Control and Prevention (CDC) National Violent Death Reporting System does not include drug overdose death as part of its event surveillance. The nearest metropolitan areas that have contributed longitudinal data to SAMHSA’s Drug Abuse Warning Network (DAWN) are Boston and New York City; Providence, Rhode Island, joined DAWN in 2009. Vital statistics available from the CDC rely upon state-reported death certificate data. However, death certificates may lack drug-specific information in the “cause of death” field (e.g., “combined opiate toxicity” cause without information on which opiates were involved) and have limited and sometimes inaccurate reporting of the locations of injury/death and residence. For instance, location of injury may have been recorded as the location where the decedent was pronounced dead (e.g., the hospital), which may differ from the location of injury (e.g., home). Geographic analyses, therefore, would incorrectly attribute deaths to cities, where hospitals are located. In contrast, data available from the CT Office of the Chief Medical Examiner (OCME), like many other state medical examiner databases, provide information on cause and manner of death, other significant medical conditions, extensive toxicological findings of all substances detected in available specimens, and key details on the circumstances of the death, including addresses specifying location of injury and residence. A local and detailed examination of CT overdose deaths using medical examiner data is therefore in order.
Connecticut is similar to other states in the New England region with respect to the geography of drug abuse. The state is a network of suburbs and small town areas, with only 5 cities with populations over 100,000. The cities and even several pockets of small towns have long legacies of heroin use, as “hubs” of distribution along the major interstate highways and the New York-Providence-Boston drug trafficking route (Fox and Leukhardt, 2002; Grund et al., 1995). Anecdotal evidence suggests increases in suburban drug use and, in particular, prescription opioid abuse over the past decade, creating a new demographic of opioid users(Merritt, 2008). Scientific evidence to substantiate these local anecdotes is lacking. Local and regional media have reported on prescription opioid abuse, rising overdose deaths in the suburbs(Calefati 2008; Fox and Leukhardt, 2002), and transitions to heroin use from OxyContin®, a purported “gateway” drug(Inciardi et al., 2009; Levy, 2007), despite evidence to the contrary(Grau et al., 2007).
This study aimed to analyze the epidemiology of opioid-involved accidental intoxication deaths in CT over 11 years (1997–2007) by examining longitudinal trends and geographic differences within this New England state.
2. Methods
2.1 Sample
Data were abstracted from the records of the CT Office of the Chief Medical Examiner (OCME) and included autopsy reports, toxicological analyses, hospital and ambulance case notes and records including information regarding history of substance abuse, medication records, death investigation and death scene reports including photos and detailed documentation of medications or drug paraphernalia found at the death scene, police reports including witness statements and information regarding previous criminal histories, and death certificates which included demographic information. The OCME reviews all accidental deaths that occur among CT residents.
All drug-involved deaths from 1997 to 2007 in CT due to intoxication and determined to be of accidental or undetermined manner by the OCME were eligible for this analysis. Initially, an electronic query of the case files was performed, applying the search terms of ‘toxicity’ or ‘intoxication’ to the cause of death and other significant conditions data fields. Eligible cases were then reviewed individually, with 2005 cases reviewed by hand (microfiche, hard copy, electronic files, as available) at the OCME to clarify discrepancies in the toxicological and address fields. We examined deaths occurring within the age range of 17 to 70. Excluded cases had died out of state (n=20); had a cause of death due to motor vehicle, bicycle or motorcycle accident, drowning, asphyxia, smoke inhalation, or capital punishment; or involved fatal intoxication by carbon monoxide (n=50), caffeine (n=1), cyanide (n=1), water (n=1), or ethylene glycol (an antifreeze, n=1). Alcohol-only intoxication deaths were included in the analysis.
Socio-demographics available in the OCME files included gender and age. We were unable to consider ethnic categories as a covariate in our analyses due to differences in administrative coding of ethnicity over time. Race categories were used instead, dichotomized as White vs. non-White for the multivariable regressions due to low frequencies in the non-White categories. Locations of injury and residence (street address, city, ZIP code) were available for all decedents. When the town/city of injury was the same as the residence, decedents were considered having died in their hometown. When location of injury was noted in the case file or discovered upon investigation as occurring in a public place (e.g., park, restaurant, public bathroom, hotel, street), the injury location was coded as such. The decedent’s residence was coded according to whether or not they lived in one of the 5 cities (Bridgeport, Hartford, New Haven, Stamford, and Waterbury) with a population ≥100,000. Homelessness at the time of death was assigned to decedents for whom a home address was not given and where the case review indicated they were homeless. Homeless decedents were assigned the city of residence corresponding to the location of their last shelter stay or to the location of the event.
Post-mortem toxicology data were available for all but 5 decedents and included drugs and drug metabolites. The OCME routinely autopsies all potential victims of drug overdose and screens them for licit and illicit drugs. Quantitative analyses of drugs and drug metabolites in postmortem blood, body fluids, and liver were performed by a number of validated analytical methods employing gas chromatography-mass spectrometry that permitted detection of heroin or morphine, prescription opioids (as a class and by drug name), cocaine, alcohol, antidepressants (coded as tricyclics, selective serotonin reuptake inhibitors, other antidepressants), and benzodiazepines (as a class and by drug name). Deaths were classified according to whether they were opioid-related and which specific patterns of opioids were involved.
2.2 Geospatial Data
All locations were assigned geographic identifiers (i.e., geocoded) first within ArcGIS (ESRI, Redlands, CA) with a match criterion of ≥ 80%. Unmatched addresses were then reviewed by hand and iteratively re-geocoded until every case had latitude and longitudinal coordinates. Locations that were described but that did not have a street address (e.g., in the woods of a state park, street intersection) were geocoded by hand using GPS Visualizer (www.gpsvisualizer.com/geocoder/) or Google maps. Thereafter, the few remaining addresses were assigned the centroid of the city/town. This analysis aggregated locations to the city/town level. Maps of the location of residence were prepared displaying at the city/town level the rate per 100,000 population of deaths due to any opioid, heroin-only, prescription opioid-only, and methadone-only.
2.3 Statistical Analyses
Descriptive statistics summarized trends over time and for each year. Counts of deaths were those related to any opioid and by the specific opioid type involved in each death and included: heroin as the only opioid, methadone as the only opioid, only prescription opioids other than methadone, or polyopioid. We used Poisson regression methods(Agresti, 2007) to examine longitudinal changes in the number of overdose deaths.
Bivariate statistics (Pearson and Likelihood ratio χ2 tests and nonparametric Mann-Whitney U or Kruskal-Wallace tests) compared (1) opioid to non-opioid related drug intoxication deaths and (2) patterns among opioid-involved deaths involving a single opioid. Thus, analyses reflected how opioid-related deaths differed from other drug-related accidental intoxication deaths and differences in risk factors among opioid users, respectively. Regression covariates were selected based on detected bivariate associations of p<0.10; all analyses controlled for age, gender, and race. Logistic regression assessed factors independently associated with heroin-only deaths and nominal logistic regression compared differences in correlates of fatal opioid overdoses due to heroin-only to those due to patterns of other opioids. Regression analyses controlled for year of death with 2007 as the reference year. We used SAS version 9.2 (Cary, NC) for analyses. Statistical tests of the regression parameters were two-sided, conducted at the alpha=0.05 level. The Yale Human Investigations Committee determined this study to not be human subjects research (defined as research on living humans). In accordance with CT state statute, the research project was reviewed and approved by the Commission on Medicolegal Investigations (http://www.cga.ct.gov/2005/pub/Chap368q.htm#Sec19a-411.htm).
3. Results
There were 9,784 accidental/undetermined deaths in CT during the study period. Applying the case eligibility criteria, there were 2900 drug-involved accidental/undetermined intoxication deaths in Connecticut from 1997 to 2007, inclusive; 2231 (76.9%) of those were opioid-involved. Table 1 differentiates the characteristics of opioid-involved from non-opioid involved drug intoxication deaths. Opioid-related accidental/undetermined intoxication deaths tended to occur among men, to affect those under 44 years of age, to also involve alcohol and benzodiazepines, and were less likely to involve cocaine and antidepressants compared to non-opioid intoxication deaths.
Table 1.
Socio-demographics and concomitant substances involved in accidental drug-involved intoxication deaths and in opioid intoxication deaths by opioid overdose pattern, 1997–2007
| Variable | All accidental drug-involved intoxication deaths [N=2900] |
Accidental opioid intoxication deaths only [N=1975] |
Test statistic (p-value) |
|||||
|---|---|---|---|---|---|---|---|---|
| Non-opioid [N=662] % (N) |
Opioid [N=2238] % (N) |
Heroin-only [N=1195] % (N) |
Prescription opioid- only [N=269] % (N) |
Methadone- only [N=305] % (N) |
Polyopioid [N=206] % (N) |
|||
| Socio-demographics | ||||||||
| Female | 34.4 (228) | 23.7 (531)* | 17.6 (210) | 37.3 (101) | 36.7 (112) | 32.2 (67) | 85.7 (p<0.001) |
|
| Non-white minority | 19.8 (131) | 8.0 (179)* | 9.0 (107) | 2.6 (7) | 8.6 (26) | 9.1 (19) | 12.66 (p<0.001) |
|
| Age group | ||||||||
| 17–24 | 5.4 (36) | 12.0 (268)* | 12.7 (152) | 14.4 (39) | 11.1 (34) | 7.7 (16) | 54.05 | |
| 25–34 | 16.9 (112) | 22.7 (507) | 24.5 (293) | 16.6 (45) | 19.3 (59) | 20.7 (43) | (p<0.001) | |
| 35–44 | 39.6 (262) | 41.2 (922) | 41.8 (500) | 37.6 (102) | 36.7 (112) | 51.0 (106) | ||
| 45–54 | 29.5 (195) | 20.8 (465) | 18.7 (224) | 23.6 (64) | 28.2 (86) | 18.3 (38) | ||
| 55+ | 8.6 (57) | 3.4 (76) | 2.3 (27) | 7.7 (21) | 4.6 (14) | 2.4 (5) | ||
| Homeless | 83.8 (9) | 71.0 (22) | 1.4 (17) | 0.4 (1) | 0.3 (1) | 0 (0) | † | |
| Resided in town/city <100,000‡ |
69.8 (447) | 73.0 (1586) | 70.8 (818) | 87.1 (229) | 69.8 (206) | 72.9 (148) | 30.8 (p<0.001) |
|
| Died in town/city <100,000 population |
68.0 (450) | 69.4 (1553) | 65.8 (786) | 87.0 (234) | 70.5 (215) | 68.9 (142) | 47.0 (p<0.001) |
|
| Died in public place | 17.1 (113) | 16.5 (370) | 19.7 (236) | 8.2 (22) | 10.5 (32) | 18.0 (37) | 30.90 (p<0.001) |
|
| Died in hometown | 85.0 (559) | 83.3 (1864) | 80.8 (965) | 88.5 (238) | 88.5 (270) | 81.1 (167) | 17.16 (p=0.001) |
|
| Concomitant substances | ||||||||
| Cocaine | 48.0 (318) | 26.5 (594)* | 31.5 (377) | 13.3 (36) | 20.7 (63) | 36.1 (75) | 51.5 (p<0.001) |
|
| Alcohol | 20.2 (225) | 34.0 (453)* | 23.9 (286) | 16.6 (45) | 11.5 (35) | 25.5 (53) | 28.28 (p<0.001) |
|
| Any benzodiazepine | 5.1 (34) | 9.0 (202)* | 4.9 (59) | 20.7 (56) | 10.8 (33) | 25.5 (53) | 122.28 (p<0.001) |
|
| Any antidepressant | 8.6 (57) | 1.9 (43)* | 1.3 (15) | 5.2 (14) | 3.5 (11) | 0.5 (1) | 23.0 (p<0.001) |
|
| Tricyclic | 4.2 (28) | 0.6 (13)* | 0.3 (4) | 2.2 (6) | 1.0 (3) | 0 (0) | † | |
| SSRI | 3.6 (24) | 1.3 (28)* | 0.8 (10) | 3.0 (8) | 2.3 (7) | 0.5 (1) | † | |
| Other antidepressant | 1.5 (10) | 0.2 (5)* | 0.1 (1) | 0.4 (1) | 0.7 (2) | 0 (0) | † | |
| Mean (SD) Total number of substances |
† | 1.63 (0.74) | 1.70 (0.87) | 1.48 (0.68) | 3.14 (0.97) | p<0.001 | ||
P<0.001 statistically significant difference in the characteristic comparing opioid to non-opioid involved intoxication deaths;
not estimable;
Due to unknown city of residence and out of state residence, N=2813 for the opioid versus non-opioid comparison and N=1916 for the within opioid comparison.
SSRI= Selective Serotonin Reuptake Inhibitor, SD=standard deviation
Toxicological data were available for 2644 decedents (91.2% of all cases) and for 1975 of the opioid-involved deaths (88.5% of 2231), indicating involvement of specific opioid(s). Opioid cases that lacked complete toxicological data were more likely to be male compared to all other opioid-involved deaths (84% versus 75%, p=0.002) but were not distinguishable from the deaths involving heroin on any demographic or geographic variables. Of the 1975 deaths with complete toxicological information, 1769 involved a single opioid, including heroin (n=1195, 67.6%), methadone (n=305, 17.2%), oxycodone (n=140, 7.9%), fentanyl (n=51, 2.9%), hydrocodone (n=43, 2.4%), and propoxyphene (N=28, 1.6%). Of the 206 polyopioid deaths, over 80% involved use of heroin. The most common combination was heroin and one or more prescription opioid (n=116, 56.3%), followed by heroin and methadone (n=47, 22.8%), methadone and one or more other prescription opioid (n=35, 17%), but rarely heroin, methadone, and one or more other prescription opioid in combination (n=10, 4.8%). Among those who died of polyopioid intoxication, the common prescription opioid classes involved were codeine (n=71, 34.5%), followed by oxycodone (n=42, 20.4%), hydrocodone (n=35, 17%) and propoxyphene (n=23, 11.2%). Other drugs commonly found among opioid-involved decedents included cocaine (n=551, 27.9%) and alcohol (n=419, 21.2%), whereas benzodiazepines (n=201, 10.2%) and antidepressants (n=41, 2.1%) were less often detected.
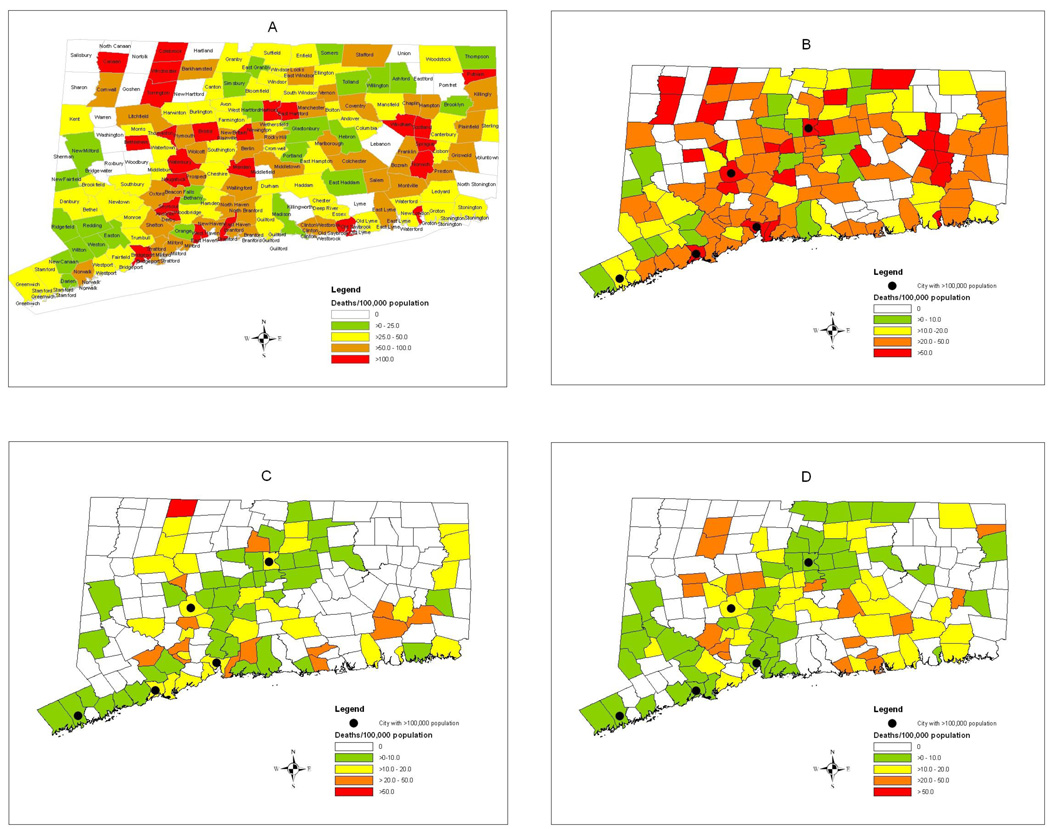
Opioid intoxication deaths occurred throughout the state with no concentrated geographic pattern evident (Figure 1A). Of the 169 CT towns, 148 towns experienced at least one opioid-related death over the 11-year period. However, the pattern differed as a function of the type of opioid. Heroin-only and methadone-only related deaths were more common in cities with populations over 100,000 (Figures 1B, 1C) whereas death related to other prescription opioids were more common in smaller cities and towns (Figure 1D). Therefore, further analysis was conducted dividing opioid-related deaths into four categories: heroin-only, methadone-only, other prescription opioid-only (hereinafter referred to as prescription opioid-only), and polyopioid.
Figure 1.
A–D: Opioid-involved accidental/undetermined deaths per 100,000 population, 1997–2007: residence of decedent aggregated by town. (A) All opioids; (B) Heroin-only; (C) Methadone-only; (D) Deaths dues to single prescription opioids other than methadone.
Bivariate results indicated other notable differences in pattern of opioid deaths (Table 1). Heroin-only decedents were more likely male than female. Prescription opioid-only decedents were more likely to be White than non-White, were more likely residents of small towns (population <100,000) rather than cities (population ≥100,000), and tended to die in their hometowns rather than elsewhere. Methadone only victims were more likely to die in their hometown, but their residence tended to be in larger cities. Deaths occurring in a public place were more likely to have involved heroin only or multiple opioids.
The mean number of substances involved across the opioid overdose patterns suggested that most of the heroin-, methadone- and prescription opioid-only deaths involved only one nonopioid substance (e.g, cocaine, alcohol, antidepressants, or benzodiazepines) whereas for the polyopioid overdoses the number of non-opioids exceeded three (e.g., cocaine, alcohol, and benzodiazepines).
3.1 Longitudinal trends and patterns according to time of death
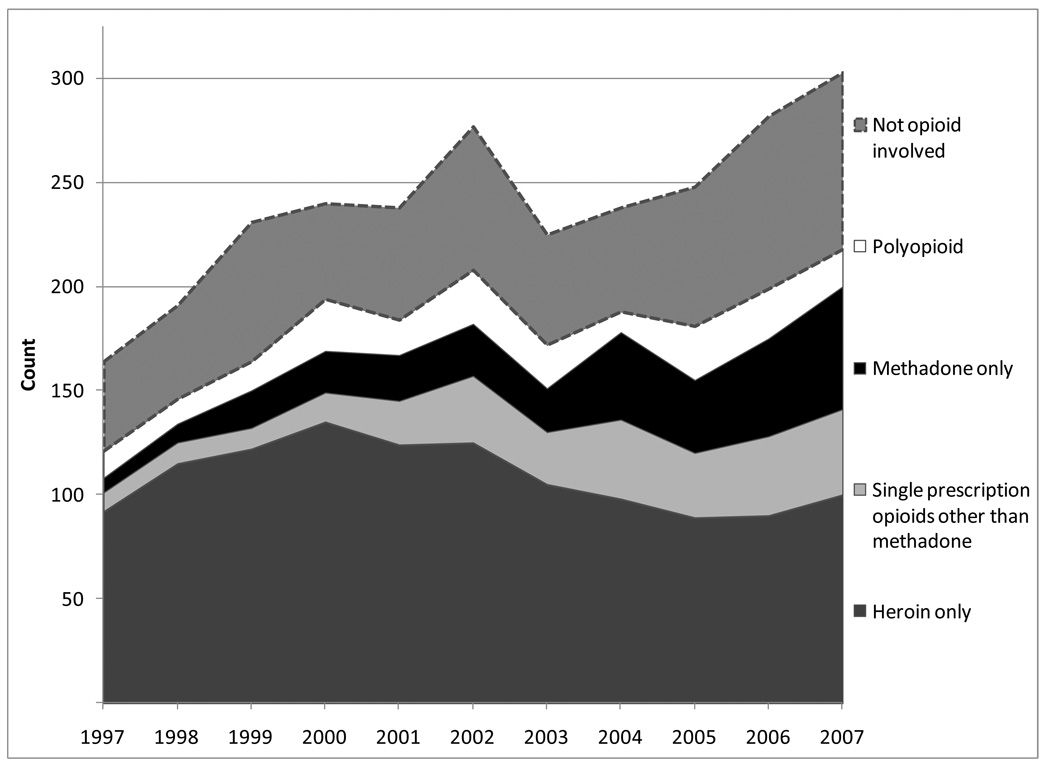
Distinct epidemiologic and longitudinal trends in the opioid accidental intoxication deaths over the 11-year period were also evident in CT (Figure 2).
Figure 2.
Accidental intoxication deaths over time involving specific opioid combinations and not opioid involved
3.1.1 Counts
Comparing 1997 to 2007, the absolute number of opioid overdose deaths increased by 44% (from 168 to 242) (Figure 2). Among the opioid overdose deaths with toxicological data (n=1975 of 2637) there was an increase of 80% over the study period (from 121 to 218). There was no trend in the number of heroin intoxication deaths from 1997 to 2007, which averaged 124.4 per year and ranged from a low of 102 in 1997 to a peak of 160 in 2000. On the other hand, there was a 379% increase in methadone deaths from 14 to 67 (p<0.001). Prescription opioid intoxication deaths increased at an average of 3.9 additional cases per year (p=0.02), rising steadily from 19 in 1997 to 54 in 2000 at a rate of 4% per year (p=0.006) with a statistically significant 28% jump in 2001.
3.1.2 Proportion of deaths due to specific opioids
Although the overall proportion of accidental drug intoxication deaths involving an opioid was unchanged over the study period (linear: 1.87, p=0.17), the relative proportion of the opioids involved in the overdoses changed dramatically (Figure 2). There was a significant reduction in the proportion of accidental/undetermined deaths involving heroin over time (linearly: 56.43, p<0.001), with greater odds of heroin-only deaths occurring in the years 1997–2003 compared to the years 2004–2007 (Figure 2). The proportion of methadone-involved deaths significantly increased over time (linearly: 58.09, p<0.001), with the highest proportions of methadone-only deaths occurring 2003 to 2007. Another increasing trend was deaths involving prescription opioids. Starting in 2001, intoxication deaths involving any prescription opioid increased from previous years, a trend which persisted through 2007 (linearly: 25.14, p<0.001). Specific prescription opioids contributing to this phenomenon were fentanyl (linearly: 34.38, p<0.001; 0.6% to 5.3%) and oxycodone (linearly: 38.34, p<0.001; 1.2% to 8.9%). These time trends persisted even after controlling for confounding variables in multivariable regressions (data available upon request).
Heroin-only deaths (N=1195) were significantly more likely to occur on a Friday (15.6%) or a Saturday (21.0%, χ2: 7.6, p=0.006). Those that involved any prescription opioid (N=428) were more likely to occur on a Monday (16.6%, χ2: 17.15, p=0.009) and prescription opioid-only deaths (N=269) tended to occur during the week (Mondays 17.5%, Wednesdays 16.7%, Thursdays 16.0%, χ2 20.25, p<0.001). Opioid-involved deaths wherein cocaine (N=550) or methadone (N=395) was involved tended to occur at uniform rates throughout the week. Finally, alcohol-involved opioid deaths (N=419) were more likely to occur on a Saturday (23.6%, χ2: 16.09, p=0.01). No monthly or quarterly trends were detected.
3.3 Regression analyses
3.3.1 Heroin-only deaths
Compared to other accidental intoxication deaths, the independent risk factors for heroin-only intoxication death were younger age (17–34 years), male gender, and being White. Heroin-only deaths were less likely to occur among people over the age of 45 and tended not to involve concurrent use of antidepressants, benzodiazepines, cocaine, or alcohol (Table 2). Use of these other substances was more common among other drug-related intoxication victims. Heroin-only decedents were more likely to die in a public place and to reside in a location with ≥ 100,000 population.
Table 2.
Variables independently associated with heroin-only accidental intoxication deaths and with specific opioid pattern compared to heroin-only deaths among opioid-involved decedents*
| All accidental intoxication deaths |
Accidental opioid intoxication deaths Heroin-Only as the Reference Category |
||||
|---|---|---|---|---|---|
| Heroin as only opioid AOR (95% CI) |
Prescription opioid(s) other than methadone only AOR (95% CI) |
Methadone only AOR (95% CI) |
Polyopioids AOR (95% CI) |
||
| Age (ref=35–44) 17–24 | 1.48 (1.10, 1.98) | 0.95 (0.60, 1.51) | 0.84 (0.53, 1.33) | 0.49 (0.27, 0.90) | |
| 25–34 | 1.28 (1.02, 1.60) | 0.80 (0.53, 1.21) | 0.90 (0.62, 1.31) | 0.72 (0.48, 1.08) | |
| 45–54 | 0.73 (0.59, 0.91) | 1.16 (0.79, 1.71) | 1.39 (0.98, 1.97) | 0.73 (0.48, 1.11) | |
| 55+ | 0.40 (0.25, 0.64) | 2.62 (1.31, 5.21) | 1.28 (0.60, 2.74) | 0.86 (0.31, 2.35) | |
| Gender (0=male, 1=female) | 0.45 (0.37, 0.55) | 2.34 (1.69, 3.24) | 2.41 (1.78, 3.26) | 2.22 (1.56, 3.16) | |
| Non-white minority | 0.59 (0.44, 0.79) | 0.51 (0.22, 1.17) | 1.08 (0.65, 1.82) | 1.00 (0.56, 1.76) | |
| Cocaine involvement | 0.71 (0.59, 0.85) | 0.50 (0.34, 0.74) | 0.74 (0.54, 1.04) | 1.34 (0.96, 1.88) | |
| Alcohol involvement | 0.78 (0.64, 0.96) | 0.87 (0.58, 1.30) | 0.61 (0.41, 0.92) | 1.18 (0.81, 1.72) | |
| Antidepressant involvement | 0.20 (0.11, 0.37) | 2.78 (1.21, 6.39) | 1.90 (0.81, 4.45) | 0.35 (0.04, 2.73) | |
| Benzodiazepine involvement | 0.33 (0.24, 0.46) | 5.61 (3.61, 8.74) | 3.04 (1.87, 4.93) | 6.92 (4.47, 10.71) | |
| Resided in a town/city <100,000 population |
0.82 (0.67, 1.00) | 2.14 (1.42, 3.25) | 0.83 (0.60, 1.13) | 1.00 (0.69, 1.44) | |
| Died in hometown | 0.80 (0.61, 1.05) | 1.33 (0.80, 2.22) | 1.47 (0.90, 2.41) | 0.80 (0.50, 1.27) | |
| Died in public place | 1.32 (1.02, 1.70) | 0.50 (0.29, 0.87) | 0.56 (0.34, 0.90) | 0.86 (0.55, 1.37) | |
N=1911 due to missing city of residence and out of CT residence in n=64 decedents. Regressions also adjusted for year of death. AOR=Adjusted Odds Ratio; 95% CI=95% Confidence Interval; Bold values are statistically significant at p<0.05
3.3.2 Prescription opioids-only
Compared to heroin-only decedents, prescription opioid-only cases were more likely to have resided in small towns/cities of < 100,000 people, to have also used one or more antidepressants, and were less likely to have died in a public place (Table 2). Alcohol was as likely to be involved in heroin-only as in prescription opioid-only intoxication deaths. Compared to heroin-only decedents, older age was associated with prescription opioid-only intoxication death (Table 2, Adjusted Odds Ratio (AOR) 2.62 aged 55+).
3.3.3 Methadone-only
Compared to heroin-only decedents, methadone-only decedents were more likely female (AOR 2.41), to involve benzodiazepine(s) (AOR 3.04), but tended not to die in a public place (AOR 0.56) or to involve alcohol (AOR 0.61) (Table 2). Like heroin-only decedents, methadone-only decedents tended to have resided in the large cities of CT.
3.3.4 Polyopioid
Polyopioid decedents were more likely than heroin-only decedents to be older than 25 (AOR 0.49 for 17–24 years), female (AOR 2.22), and to have used one or more benzodiazepine (AOR 6.92) (Table 2). Polyopioid decedents, like heroin-only decedents, were more likely to reside and die in urban settings and to die in a public place.
4. Discussion
In this analysis of CT OCME records of accidental intoxication deaths between 1997 and 2007, more than three-quarters of deaths involved an opioid. Methadone and prescription opioid intoxication led the growth in opioid intoxication deaths and outpaced all other accidental intoxication deaths during the study period. Several of our findings on risk factors for fatal prescription opioid overdose concur with reports from other individual states (Hall et al., 2008; Paulozzi et al., 2009; Shah et al., 2008), including high concomitant use of psychotherapeutic drugs (Hall et al., 2008), greater representation of white and female decedents and an older age distribution compared to illicit drug involved (Paulozzi et al., 2009; Shah et al., 2008) and to methadone involved overdose deaths (Hall et al., 2008; Paulozzi et al., 2009). As in New Mexico (Mueller et al., 2006; Shah et al., 2008) and West Virginia (Hall et al., 2008), prescription opioid (including methadone) only deaths comprised a large proportion of single drug deaths in CT, with the persistent and predominant concern in CT and New Mexico of heroin involved drug overdose deaths. Such similarities in findings between the current study and investigations in other locations of trends and risk factors for prescription opioid deaths suggest that national approaches to overdose prevention may be plausible.
Although elsewhere in the US, opioid overdose deaths are often concentrated in metropolitan areas(Garfield and Drucker, 2001), deaths in CT are clearly spread throughout the state. Uniquely, the geographic pattern of overdose death in CT varied according to opioid type, where prescription opioid deaths predominated in non-public settings of suburban and small town locations while heroin and methadone deaths predominated in urban locations, in both public (heroin) and non-public (methadone) settings. Others have reported geographic trends in substance abuse more generally(McLafferty, 2008), for prescription opioid use and non-medical use(Brownstein et al., ; Havens et al., 2006; Zerzan et al., 2006), and of fatal drug overdose(Dasgupta et al., 2008; Paulozzi, 2006; Paulozzi and Xi, 2008). Our findings add to this discussion the observed differential patterns of opioid overdose deaths in a New England state. Future work to understand why and how observed geographic patterns of opioid overdose arise could contribute to the etiology and better prevention of overdose.
Heroin remains the opioid most commonly involved in CT intoxication deaths. Trends over this period reflect shifts in the local illicit drug market that mirror regional and national trends. Peaks in heroin deaths in 1999 and 2000 coincided with peak heroin purity and an all-time low in price, when Colombian heroin achieved market dominance in the Northeast(Ciccarone, 2009). Since then, purity has plateaued(Ciccarone, 2009), which may have contributed to the decreasing proportion of heroin in opioid intoxication deaths. Heroin-involved deaths disproportionately tended to affect young people who may be newer users, do use a drug whose purity is constantly varying, may not practice harm reduction techniques (e.g., “tasting” the drug first to check strength), and may experience an overdose in the presence of other young users who fail to recognize and respond to its signs. The fact that 71% of fatal heroin overdose victims resided in a small town/city and were more likely to take place on a weekend suggest recreational use that traverses suburban to urban areas. Preventing heroin overdose deaths will require more active involvement of suburban communities in substance abuse prevention, addiction treatment, overdose training and response efforts, and increasing awareness of overdose potential.
Increased availability of prescription opioids has resulted in the rise in prescription opioid overdoses. For instance, availability of oxycodone products in CT increased 561% from 3,180 grams per population in 1997 to 21,033 grams per population in 2006(U.S. Department of Justice). It is possible that the reduction in the proportion of opioid-involved deaths associated with heroin and the increase in prescription opioid-only deaths could have been due to reductions in heroin initiation and experimentation displaced by prescription opioid initiation and experimentation, and/or by transitions to non-injection routes of administration of heroin (cf(Frank, 2000)) that reduce risk of fatal heroin-associated overdoses.
The 2001 increase in prescription opioid overdose deaths we note corresponds to state-level findings that media mentions of prescription opioids rose dramatically starting in early 2001, followed two to six months later by increases in overdose deaths involving prescription opioids(Dasgupta et al., 2009). This suggests that aspects of the social environment — in this case media coverage — may enhance the popularity of certain drugs and possibly foster demand(Fan, 1996; Orcutt and Turner, 1993). The etiology of opioid abuse and overdose death is complex. The fact that the agent of injury is a prescribed medication reduces variabilities in dose and drug quality encountered with heroin, but leaves problems of improper marketing, lax prescribing standards, inadequate safety labeling(James, 2001), prescriber and dispenser medication errors, and lack of patient education about safe medication storage and disposal. Most overdose deaths are preventable. Effective reduction of opioid overdose deaths in CT, as in other areas witnessing high rates of accidental fatal opioid overdose, may therefore require more nuanced, local, and multi-level interventions, such as real-time state prescription monitoring programs, that influence availability of and access to controlled medications.
Retail sales of methadone increased nationally by 1177% from 1997 to 2006 (Manchikanti and Singh, 2008), a trend exemplified in CT. The rise in methadone involved deaths stands in contrast to expanding methadone treatment for narcotic addiction, which has a proven safety record and actually reduces mortality among those in treatment. Increased deaths may reflect sharing of medications among friends, diversion, and doctor shopping. We found that the increase in methadone overdose deaths occurred after the 2001 federal policy change on methadone prescribing for the treatment of pain, suggesting a substantial contribution from methadone prescribed for pain. Medical providers in CT may have turned to methadone as a less expensive, “safer”, well-established, and federally-endorsed pain management option in response to the increases in local diversion and abuse of OxyContin®(Cohn, 2/19/2008). This hypothesis is supported by the observation that methadone deaths began increasing in 2004, three years after the onset of the increases in prescription opioid deaths. Another explanation for the methadone death increases may be changes in off-label prescribing practices(U.S. Government Accountability Office, 2009) especially of high dose formulations of methadone and misconceptions about methadone’s pharmacokinetics. More research on this subject and on the impact of the January 2008 retail distribution restriction(U.S. Government Accountability Office, 2009) on the incidence of methadone associated overdose deaths is clearly needed.
The present analysis is hampered by notable limitations. First, important unmeasured covariates exist including ethnicity, medical history, and the inability to differentiate between prescription to the decedent and diversion and, in the case of methadone, prescription for pain or opioid substitution therapy. Second, approximately 10% of decedents lacked toxicological results at autopsy. One example of how this may have occurred would be if there had been survival time between injury and death, in which case only toxicology results conducted at the time of hospital admittance would have been available for our review. Opioid cases lacking toxicological results resembled heroin-involved decedents across all socio-demographic and geographic variables. Thus, the exclusion of cases with no toxicology results from the reference group of our regression analyses may have resulted in a small but non-differential bias of the reported gender associations. In contrast to previous studies, the fact that all accidental overdose cases are reviewed by the CT OCME suggests that our study reflects generalizable, population-level trends. Access to the CT OCME database is permitted to qualified researchers and state agencies, as outlined in CT state statute. However, because medical examiner data are not collected for the purpose of research, the logistics of preparing these data for analysis are not trivial. Future efforts could explore organizing and coordinating data linkages between state agencies to improve reporting on substance abuse, mental health, prescription opioid prescribing, and overdose trends.
Results from this study suggest an opportunity to target, geographically and epidemiologically, effective interventions to reduce the high rates of accidental opioid intoxication deaths in CT. Such responses may include overdose prevention programs for populations at high risk of fatal overdose (Strang et al., 2003; Wakeman et al., 2009) and expanding access to naloxone -the national standard antidote for reversing opioid overdose in the pre-hospital setting- in the community by training first responders, drug users, prescription opioid users, and other caregivers in overdose recognition, response, and proper administration of naloxone in an overdose situation (Dasgupta et al., 2010; Doe-Simkins et al., 2009; Green et al., 2008; Maxwell et al., 2006; Piper et al., 2007).
Acknowledgements
We thank the staff of the Connecticut Office of the Chief Medical Examiner and especially Nandi Colon for their assistance in conducting this research.
Role of Funding Source
Research for this manuscript was supported by the National Institutes of Health, National Institute on Drug Abuse grant 1F31DA023862-01A1 to TCG. The funding sources had no further involvement in the study design, data collection, analysis, writing, preparation or decision to submit this manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
TCG conceived of the analysis, conducted the data abstraction and statistical analysis, and authored the first manuscript draft; RH guided the research questions and the interpretation of analyses and provided comments to manuscript drafts; LEG assisted with the data abstraction, helped with interpretation of analyses, and provided comments to manuscript drafts; MK and HWC assisted with interpretation of analyses and provided comments to manuscript drafts. All authors contributed to and have approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
References
- Agresti A. An Introduction to Categorical Data Analysis. Hoboken, NJ: John Wiley & Sons; 2007. [Google Scholar]
- Brownstein JS, Green TC, Cassidy TA, Butler SF. Geographic information systems and pharmacoepidemiology: using spatial cluster detection to monitor local patterns of prescription opioid abuse. Pharmacoepidemiol Drug Saf. 19:627–637. doi: 10.1002/pds.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calefati J. Heroin Hits the Suburbs Hard Amid Wave of Drug Abuse by Teens and 20-Somethings. US News and World Report. 2008 [PubMed]
- Ciccarone D. Heroin in brown, black and white: structural factors and medical consequences in the US heroin market. Int J Drug Policy. 2009;20:277–282. doi: 10.1016/j.drugpo.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D, Unick GJ, Kraus A. Impact of South American heroin on the US heroin market 1993&2004. Int J Drug Policy. 2009;20:392–401. doi: 10.1016/j.drugpo.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn A. Team 8 Investigates Methadone prescriptions. 2008. Feb 19, [Google Scholar]
- Dasgupta N, Jonsson Funk M, Brownstein J. Comparing Unintentional Opioid Poisoning Mortality in Metropolitan and Non-Metropolitan Counties, United States, 1999–2003. In: Thomas Y, Richardson TD, Cheung I, editors. Geography and Drug Addiction. Springer Publishers (Collaboration between the National Institute on Drug Abuse and the Association of American Geographers); 2008. [Google Scholar]
- Dasgupta N, Mandl KD, Brownstein JS. Breaking the News or Fueling the Epidemic? Temporal Association between News Media Report Volume and Opioid-Related Mortality. PLoS ONE. 2009;4:e7758. doi: 10.1371/journal.pone.0007758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta N, Sanford C, Albert S, Brason FW. Opioid drug overdoses:A prescription for harm and potential for prevention. Am J Lifestyle Med. 2010:32–37. [Google Scholar]
- Doe-Simkins M, Walley AY, Epstein A, Moyer P. Saved by the nose: bystander-administered intranasal naloxone hydrochloride for opioid overdose. Am J Public Health. 2009;99:788–791. doi: 10.2105/AJPH.2008.146647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan DP. News media framing sets public opinion that drugs is the country's most important problem. Subst Use Misuse. 1996;31:1413–1421. doi: 10.3109/10826089609063984. [DOI] [PubMed] [Google Scholar]
- Fox T, Leukhardt B. Small Town, Big-Time Heroin Use. Hartford, CT: Hartford Courant; 2002. [Google Scholar]
- Frank B. An overview of heroin trends in New York City: past, present and future. The Mount Sinai journal of medicine, New York. 2000;67:340–346. [PubMed] [Google Scholar]
- Garfield J, Drucker E. Fatal overdose trends in major U.S. cities: 1990–1997. Addiction Research and Theory. 2001;9:425–436. [Google Scholar]
- Grau LE, Dasgupta N, Harvey AP, Irwin K, Givens A, Kinzly ML, Heimer R. Illicit use of opioids: is OxyContin a "gateway drug"? The American journal on addictions / American Academy of Psychiatrists in Alcoholism and Addictions. 2007;16:166–173. doi: 10.1080/10550490701375293. [DOI] [PubMed] [Google Scholar]
- Green TC, Heimer R, Grau LE. Distinguishing signs of opioid overdose and indication for naloxone: An evaluation of six overdose training and naloxone distribution programs in the United States. Addiction (Abingdon, England) 2008;103:979–989. doi: 10.1111/j.1360-0443.2008.02182.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grund JP, Heckathorn DD, Broadhead RS, Anthony DL. In eastern Connecticut, IDUs purchase syringes from pharmacies but don't carry syringes. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;10:104–105. doi: 10.1097/00042560-199509000-00016. [DOI] [PubMed] [Google Scholar]
- Hall AJ, Logan JE, Toblin RL, Kaplan JA, Kraner JC, Bixler D, Crosby AE, Paulozzi LJ. Patterns of Abuse Among Unintentional Pharmaceutical Overdose Fatalities. JAMA. 2008;300:2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- Havens JR, Talbert JC, Walker R, Leedham C, Leukefeld CG. Trends in controlled-release oxycodone (OxyContin) prescribing among Medicaid recipients in Kentucky, 1998–2002. J Rural Health. 2006;22:276–278. doi: 10.1111/j.1748-0361.2006.00046.x. [DOI] [PubMed] [Google Scholar]
- Inciardi JA, Surratt HL, Cicero TJ, Beard RA. Prescription opioid abuse and diversion in an urban community: the results of an ultrarapid assessment. Pain medicine (Malden, Mass. 2009;10:537–548. doi: 10.1111/j.1526-4637.2009.00603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James M. FDA, Maker Warn Doctors on OxyContin. ABCNEwscom. 2001. [Google Scholar]
- Levy MS. An exploratory study of OxyContin use among individuals with substance use disorders. J Psychoactive Drugs. 2007;39:271–276. doi: 10.1080/02791072.2007.10400613. [DOI] [PubMed] [Google Scholar]
- Manchikanti L, Singh A. Therapeutic opioids: a ten-year perspective on the complexities and complications of the escalating use, abuse, and nonmedical use of opioids. Pain physician. 2008;11:S63–S88. [PubMed] [Google Scholar]
- Maxwell S, Bigg D, Stanczykiewicz K, Carlberg-Racich S. Prescribing naloxone to actively injecting heroin users: a program to reduce heroin overdose deaths. J Addict Dis. 2006;25:89–96. doi: 10.1300/J069v25n03_11. [DOI] [PubMed] [Google Scholar]
- McLafferty S. Placing Substance Abuse. In: Thomas Y, Richardson D, Cheung I, editors. Geography and Drug Addiction. New York: Springer; 2008. [Google Scholar]
- Merritt G. Heroin moves in to Connecticut Suburbia. Hartford: Hartford Courant; 2008. [Google Scholar]
- Mueller MR, Shah NG, Landen MG. Unintentional prescription drug overdose deaths in New Mexico, 1994–2003. Am J Prev Med. 2006;30:423–429. doi: 10.1016/j.amepre.2005.12.011. [DOI] [PubMed] [Google Scholar]
- Orcutt J, Turner J. Shocking numbers and graphic accounts: quantified images of drug problems in the print media. Social Problems. 1993;40:190–206. [Google Scholar]
- Paulozzi LJ. Opioid analgesic involvement in drug abuse deaths in American metropolitan areas. Am J Pblic Halth. 2006;96:1755–1757. doi: 10.2105/AJPH.2005.071647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulozzi LJ, Ballesteros MF, Stevens JA. Recent trends in mortality from unintentional injury in the United States. J Safety Res. 2006a;37:277–283. doi: 10.1016/j.jsr.2006.02.004. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006b;15:618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Logan JE, Hall AJ, McKinstry E, Kaplan JA, Crosby AE. A comparison of drug overdose deaths involving methadone and other opioid analgesics in West Virginia. Addiction (Abingdon, England) 2009;104:1541–1548. doi: 10.1111/j.1360-0443.2009.02650.x. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Ryan GW. Opioid analgesics and rates of fatal drug poisoning in the United States. Am J Prev med. 2006;31:506–511. doi: 10.1016/j.amepre.2006.08.017. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Xi Y. Recent changes in drug poisoning mortality in the United States by urban-rural status and by drug type. Pharmacoepidemiol Drug Saf. 2008;17:997–1005. doi: 10.1002/pds.1626. [DOI] [PubMed] [Google Scholar]
- Piper TM, Rudenstine S, Stancliff S, Sherman S, Nandi V, Clear A, Galea S. Overdose prevention for injection drug users: lessons learned from naloxone training and distribution programs in New York City. Harm reduction J. 2007;4:3. doi: 10.1186/1477-7517-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah NG, Lathrop SL, Reichard RR, Landen MG. Unintentional drug overdose death trends in New Mexico, USA, 1990–2005: combinations of heroin, cocaine, prescription opioids and alcohol. Addiction (Abingdon, England) 2008;103:126–136. doi: 10.1111/j.1360-0443.2007.02054.x. [DOI] [PubMed] [Google Scholar]
- Spiller H, Lorenz DJ, Bailey EJ, Dart RC. Epidemiological trends in abuse and misuse of prescription opioids. J Addict Dis. 2009;28:130–136. doi: 10.1080/10550880902772431. [DOI] [PubMed] [Google Scholar]
- Strang J, McCambridge J, Best D, Beswick T, Bearn J, Rees S, Gossop M. Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow up study. BMJ (Clinical research ed. 2003;326:959–960. doi: 10.1136/bmj.326.7396.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use and Health: National Findings. . NSDUH Series H-36. Rockville, MD: Office of Applied Studies; 2009. [Google Scholar]
- U.S. Department of Justice. D.E.A., ARCOS: Automation of Reports and Consolidated Orders System. www.deadiversion.usdoj.gov/arcos/index.html.accessed on.
- U.S. Government Accountability Office. Washington, DC: Methadone Associated Overdose Deaths: Factors Contributing to Increased Deaths and Efforts to Prevent Them. 2009
- UNODC. Vienna, Austria: United Nations Office on Drugs and Crime; The World Drug Report. 2009
- Wakeman SE, Bowman SE, McKenzie M, Jeronimo A, Rich JD. Preventing death among the recently incarcerated: an argument for naloxone prescription before release. J Addict Dis. 2009;28:124–129. doi: 10.1080/10550880902772423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner M, Chen LH, Makuc DM. Increase in fatal poisonings involving opioid analgesics in the United States, 1999–2006. NCHS data brief. Hyattsville, MD: National Center for Health Statistics; 2009. [PubMed] [Google Scholar]
- Zerzan JT, Morden NE, Soumerai S, Ross-Degnan D, Roughead E, Zhang F, Simoni-Wastila L, Sullivan SD. Trends and geographic variation of opiate medication use in state Medicaid fee-for-service programs, 1996 to 2002. Medical care. 2006;44:1005–1010. doi: 10.1097/01.mlr.0000228025.04535.25. [DOI] [PubMed] [Google Scholar]