Abstract
Background
The results after acetabular fracture are primarily related to the quality of the articular reduction. We evaluated the results of internal fixation of posterior wall fractures with using three-step reconstruction.
Methods
Thirty-three patients (mean age at the time of injury, 47.9 years; 28 males and 5 females) were followed for a minimum of 2 years after surgery. The three-step reconstruction included 1) preservation of soft tissues and reduction of the marginally impacted osteochondral (articular) fragments using screws, 2) filling the impacted cancellous void with a bone graft, and 3) reinforcement with buttress-plating. Clinical evaluation was done according to the criteria of D'aubigne and Postel, while the radiological criteria were those of Matta. The associated injuries and complications were evaluated.
Results
The clinical results were excellent in 15 (45.5%) patients and they were good in 5 (15.2%), (i.e., satisfactory in 60.7%), while the radiologic results were excellent in 10 (30.3%) and good in 14 (42.4%) (satisfactory in 72.7%). Heterotopic ossification was common, but this did not require excision, even without prophylactic treatment with indomethacin. Deep infection was the worst complication and this was accompanied by a poor outcome.
Conclusions
This study confirms that three-step reconstruction facilitates accurate and firm reduction of displaced posterior wall fractures of the acetabulum. Therefore, we anticipate less long-term arthrosis in the patients treated this way.
Keywords: Acetabulum, Posterior wall fracture, Reconstruction
Most acetabular fractures involve the posterior wall.1-3) Although such fractures may appear to be simple on plain radiographs, many surgeons face difficulties when reducing the fragments. Most posterior wall fractures are comminuted or they are associated with an impaction injury of the articular surface into the underlying cancellous bone along the margin of the fracture line.4-6) The soft tissues are frequently detached from fragments at the time of injury or during the surgery. In addition, after surgery it is difficult to know the exact quality of the reduction and the shape and congruity of the articular surface of the acetabulum due to its three-dimensionally complex shape and the interfering effect of metals on the radiologic images. Accurate evaluation of the resulting union and the likelihood of future osteoarthritis and differentiating between avascular necrosis (AVN) of the femoral head and true post-traumatic arthritis are also hindered. Therefore, surgeons should make every effort to obtain a stable congruous hip joint with complete union of the fragments during the primary surgery because a second operation is not feasible.
We report here on the medium-term results of internal fixation of posterior wall fractures by three-step reconstruction. The technique includes 1) preservation of the attached soft tissues and repairing the marginally impacted and osteochondral fragments using screws, 2) filling the cancellous bone void using a bone graft, and 3) final reinforcement with buttress-plating.
METHODS
Seventy five patients with posterior wall fractures were treated at our institution from 2004, when our hospital first adopted the picture archiving communication system (PACS), through 2009. Of these, 47 displaced fractures were surgically treated. The surgical indications were femoral head subluxation and > 50% involvement of the posterior wall, a fracture pattern involving the weight-bearing dome with ≥ 2 mm of displacement on the anterior-posterior (AP) and Judet views of the pelvis without extremity traction, and a positive dynamic stress view consistent with hip instability.7) All the radiological data stored in the PACS was reviewed and the final clinical outcomes were evaluated. The 33 patients included in this study were followed up for a minimum of 2 years after surgery.
All the patients were treated by the trauma protocol established at our emergency center and the associated injuries were evaluated immediately after arrival. Our protocol for acetabular fractures includes the AP and two Judet 45° pelvic radiographs8,9) and a 2- and 3-dimensional CT scan of the pelvis. All the fractures were classified by the senior author (HTK) and an orthopedic trauma surgeon (JMA), and all the data on posterior wall fractures of the acetabulum was entered into the orthopedic trauma database. A surgical plan that included the associated injuries to the pelvic ring was created and all the patients were treated by the surgeons (HTK and JMA) using the three-step reconstruction method as described herein.
Twenty-eight patients were male and five were female. The mean patient age at the time of injury was 47.9 years (range, 20 to 67 years). Fourteen fractures involved the right side and 19 involved the left. The causes of injury were road-traffic accidents (14 patients in cars, 5 pedestrians and 3 motorcycle accidents) for 22 patients, falls from a height for 5, being crushed under a heavy cargo for 3, sports-related injuries for 2 and a ferry accident for 1.
The fractures were classified according to the Letournel- Judet system. There were 21 (63.6%) simple posterior wall fractures. Twelve (36.4%) were complex fractures associated with other types of fractures involving both columns in 7, the transverse acetabulum in 3, anterior column in 1 and anterior wall in 1.
Posterior hip dislocation was observed in 5 patients on the initial radiographs; these patients underwent manipulation and application of lower femoral traction as the primary treatment. In 2 of the 5 hips, closed reduction was performed within 6 hours after the injury, 2 were reduced after 6 hours, and 1 was reduced by surgery after failure with closed methods. Four patients had sciatic nerve damage at the time of injury. Nineteen patients underwent surgery for posterior wall fracture within 1 week after injury, 10 underwent surgery between 1 and 2 weeks and 4 underwent surgery after 2 weeks. Twelve patients (37%) had fractures in their extremities (9 lower and 3 upper) that required surgical treatment. Other injuries included 3 to the head (skull fracture with brain hemorrhage), 2 facial injuries and 1 injury in the chest.
Surgical Technique
Three-step reconstruction
1) Reduction of the osteochondral (articular) fragments and fixation with screws: A Kocher-Langenbeck approach8,10) was used. We began by cleaning off the soft tissue-debris between the fracture fragments and carefully preserving the attached capsular soft tissues. The osteochondral free fragments in the hip joint were removed and the extent of marginal impaction was identified by applying gentle traction at the hip joint. The posterior wall fragments and their attached capsular ligaments were reduced and held with a pointed ball spike. Using a ball spike instrument (for maintaining the fragment in its reduced position while creating a pilot hole and drilling the fragment) reduced the necessity of temporary fixation with Kirshner wire. Kirshiner wires were sometimes used provisionally until definitive fixation was performed. When maintaining a marginally impacted and/or osteochondral free fragment in its elevated and reduced position was difficult, 2.0 mm subchondral mini-screws or 2.4 mm (Fig. 1) or 2.7 mm lag screws (Synthes, Paoli, PA, USA; Stryker Leibinger GmbH & Co. KG, Freiburg, Germany), bioabsorbable pegs (Mitek, Raynham, MA, USA) or bioabsorbable screws (Linvatec Biomaterials Ltd, Tampere, Finland), which were countersunk below the cancellous bone surface, were used for stabilization of the fragments. When the fragments were large, two or three 3.5 mm cortical screws were used for firm fixation. The smallest fragments were discarded when they were detached from their soft tissues. After fixation, intrarticular reduction was confirmed with gentle traction at the hip joint and a stability test. Care was taken to confirm that the lag screws that were placed close to the posterior rim were extrarticular.
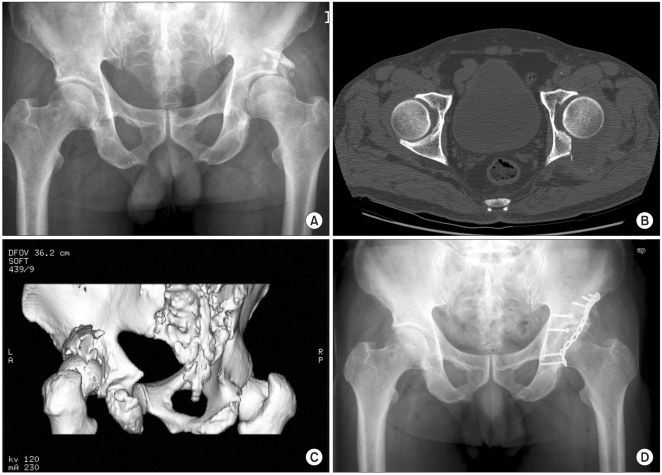
Fig. 1.
(A) Preoperative radiograph and (B) 2-dimensional and (C) 3-dimensional CT scans of a 65-year-old male with posterior wall fracture. After reduction of the osteochondral fragments with an autologous bone graft into the bone void, we performed internal fixation of the fracture with 2.4 mm lag screws and a reconstruction plate. (D) radiograph taken 3 years after surgery, the patient was free of pain with an adequate range of motion.
2) Use of a bone graft to fill the void: The space resulting from the elevated marginal fracture was filled with a bone graft using autologous bone from the greater trochanter.
3) Buttress fixation: The outer surfaces of the reduced fragments were supported with buttress-plating (Fig. 2). The buttress plates (Synthes; Zimmer, Warsaw, IN, USA) were slightly undercontoured so as to provide compression to the posterior wall. The one-third tubular spring plate11) with its tines was placed near the edge of the acetabular rim to securely maintain the fragments.
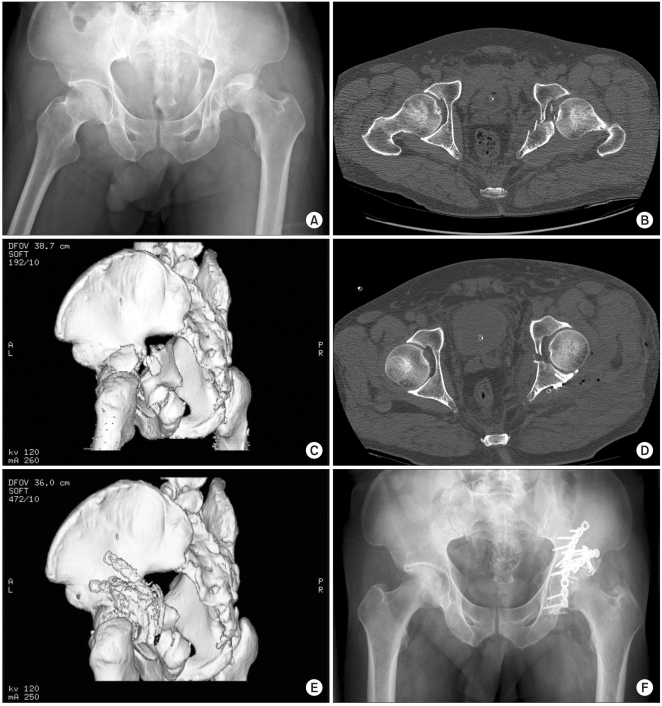
Fig. 2.
(A) Preoperative radiograph and (B) 2-dimensional and (C) 3-dimensional CT scans of a 46-year-old male with posterior wall fracture associated with a transverse acetabular fracture. We performed reduction of the osteochondral fragments with an autologous bone graft and internal fixation of the fractures with 2.0 mm mini-screws, a spring plate and two reconstruction plates. (D) Two-dimensional and (E) 3-dimensional CT scans after surgery show congruous reduction of the posterior wall. (F) Radiograph taken 2 years after surgery, the patient showed excellent functional results.
Clinical Grade
The clinical grade was based on the system of D'aubigne and Postel12) and as modified by Matta.2) The grading system includes pain, gait and range of motion with assigning a maximum of 6 points for each parameter. The 3 parameter values are then added, and the total is classified as excellent (18 points), very good (17 points), good (15 or 16 points), fair (13 or 14 points) or poor (less than 13 points).
Radiologic Grade
The quality of the reduction and the congruency of the hip joint were evaluated using the postoperative radiographs or CT scans. The radiologic criteria after open reduction and internal fixation were based on the gap remaining at the fracture site after reduction: anatomic (0-1 mm), good (2-3 mm), and poor (more than 3 mm).2) The radiologic grade at the last follow-up was based on the criteria of Matta2): excellent (a normal appearing hip joint), good (mild changes with minimal sclerosis and joint narrowing less than 1 mm), fair (intermediate changes with moderate sclerosis and joint narrowing less than 50%), and poor (advanced changes).
Grading of Heterotopic Ossification and AVN
For heterotopic ossification, the classification system of Brooker et al.13) and as modified by Moed and Smith14) was used. For AVN of the femoral head, we used the classification of Ficat and Arlet.15)
RESULTS
Clinical Results
The D'Aubigne and Postel scores at the final follow-up visit were as follows: excellent and very good in 15 patients (45.5%) (Figs. 1 and 2), good in 5 (15.2%), fair in 3 (9.1%), and poor in 10 (30.3%). Fifteen (78.9%) of the 19 patients who had surgery within 1 week showed good/excellent results, 4 (40%) of 10 who underwent surgery between 1 and 2 weeks also had good/excellent results and only 1 (25%) of 4 who had surgery after 2 weeks had good/excellent results.
Radiologic Results
Based on the fracture gap after surgery, 16 (48.5%) patients showed anatomic reduction, 12 (36.4%) showed good reduction and 5 (15.2%) showed poor reduction. According to the radiologic criteria of Matta,2) 10 patients (30.3%) had excellent results, 14 (42.4%) had good results, 4 (12.1%) had fair results and 5 (15.2%) were poor.
Complications
The early postoperative complications after surgery included two deep infections and one superficial infection. These patients had anterior and posterior approaches for both column fractures. Two patients required debridement and metal removal due to deep infection, and they had early post-traumatic arthritis. Of the 4 cases of sciatic nerve palsy that were identified preoperatively, recovery was complete in 2 and partial in 2. For the late complications, we had one patient with stage 4 AVN and one patient with post-traumatic arthritis of the hip joint 2 years after operation; both underwent total hip replacement. Seventeen patients had class I heterotopic ossification, 4 patients had class II heterotopic ossification and one patient had class III heterotopic ossification; therefore, the incidence of grade III and above heterotopic ossification was 3.0%.
DISCUSSION
Several studies1-3,16,17) have found higher rates of poor outcomes and surgical complications for posterior wall fracture of the acetabulum when a surgeon only occasionally performed acetabular fracture surgery. For experienced fracture surgeons, the incidence of fair or poor long-term results has ranged from 19 to 25%,1-3) while this was 55-56% for inexperienced surgeons who only occasionally performed acetabular surgery.16,17) Some authors have reported overall good to excellent results in the range of 74-76%,2,18-21) but in these reports the surgeons' level of expertise was not described. We believe that the severity of the fractures and the time required to become proficient at the surgery were the main reasons for our lower number of good to excellent outcomes and the higher incidence of fair or poor results.
Postoperative radiographs are important for evaluating the initial degree of articular congruency and to anticipate osteoarthritis, which may occur later on.20,22,23) Eighty four point nine percent of our patients showed anatomic or good reduction on the postoperative radiographs. However, according to Matta's radiologic criteria,2) 24 (72.7%) of our 33 patients had good to excellent results 2 years or more after surgery. We observed functional impairment even in some of the patients who showed congruent reduction on the radiographs in the medium term. These patients were relatively old (over 40)18,24) and they had suffered high energy trauma with complex fracture patterns that were difficult to reconstruct.
We believe that displaced posterior wall fractures are best treated through three-step reconstruction, with using a bone graft in the comminuted corticocancellous part to reduce the incidence of malunion and non-union. At present, the 72.7% satisfactory radiologic outcomes surpassed the 60.7% of satisfactory clinical outcomes. We expect that a few patients will develop osteoarthritis as time goes on because a three-step reconstruction was quite effective for accurate reduction of the fragments and to maintain the reduction.
Regarding the filling materials for a bone void, calcium sulfate (or synthetic materials) or a freeze-dried cancellous allograft25) can be used as bone-void filler. Since we experienced progressively collapsed fragment reduction and screw loosening in one patient with nonunion of the fragment, our first choice was autologous bone, either from the greater trochanter or the posterior iliac crest, although an allograft can be used.
The most common complication of acetabular fracture is traumatic osteoarthritis of the hip, with the incidence reported to be between 20 and 50%.2,3,17,26-28) In our study, one patient had post-traumatic osteoarthritis and one patient developed AVN. These patients subsequently underwent total hip replacement. In both cases, there was inadequate reduction of the fracture at the time of surgery due to a comminuted fracture pattern, with posterior or central dislocation of the femoral head along with intraarticular lesions of the acetabular surface and/or the femoral head. Another problem was the delayed reduction of the dislocated femoral head and/or the fracture fragments.
The rate of AVN has been reported to be between 3 and 10%2,26) and the rate is higher for the cases of associated posterior dislocation.8) However, the true rate is difficult to ascertain due to confusing true AVN with true post-traumatic arthritis because their differentiation is difficult with using only simple radiographs. We agree with Matta2) that a malreduced posterior wall or non-union of the comminuted fragments even after a bone graft can cause subsequent wear of the femoral head that resembles AVN.
The incidence of sciatic nerve palsy in acetabular fractures is about 16% and the incidence increases to about 40% when there is posterior dislocation of the femoral head.22) We had four (12.1%) cases of nerve palsy preoperatively, and two of them fully recovered over the following months. We had no case of sciatic nerve palsy that resulted from the surgery, and this has been reported to occur 2 to 6% of the time.2,22)
We believe that early reduction of the fragments with careful handling of the soft tissues can reduce the incidence of heterotopic ossification. One report states that the rate of heterotopic ossification following surgery is 25.6%.22) A majority of our patients developed grade I (51.5%) or II (12.1%) heterotopic ossification without significant functional impairment of the hip even though we did not routinely used indomethacin as prophylactic treatment. One patient (3.0%) had class III heterotopic ossification, but this did not require excision.
In the three infected patients, one had an intraarticular infection with progressive destruction of the hip joint that required multiple debridements, and finally the patient underwent a Girdlestone procedure. One patient had metal removal and multiple debridements. Both had poor clinical outcomes. The other patient had an extraarticular infection. The organism cultured from all three patients was methicillin-resistant Staphylococcus aureus and this was treated with vancomycin. Our infection rate of 9.1% is higher than the 0-3% infection rate reported in other studies2,24,29) where a simple approach was used. The incidence of infection is reported to be higher when an extensive approach was used.16)
The time elapsed after injury is important because it is more difficult to achieve anatomic reduction of the smaller fragments. Surgery is inevitably delayed for severely polytraumatized patients, yet an improved referral system to get these severely injured patients to a specialist and timely surgery are obviously desirable.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Letournel E, Judet R. Fractures of the acetabulum. 2nd ed. Berlin: Springer-Verlag; 1993. [Google Scholar]
- 2.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78(11):1632–1645. [PubMed] [Google Scholar]
- 3.Mayo KA. Open reduction and internal fixation of fractures of the acetabulum: results in 163 fractures. Clin Orthop Relat Res. 1994;(305):31–37. [PubMed] [Google Scholar]
- 4.Brumback RJ, Holt ES, McBride MS, Poka A, Bathon GH, Burgess AR. Acetabular depression fracture accompanying posterior fracture dislocation of the hip. J Orthop Trauma. 1990;4(1):42–48. doi: 10.1097/00005131-199003000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Baumgaertner MR. Fractures of the posterior wall of the acetabulum. J Am Acad Orthop Surg. 1999;7(1):54–65. doi: 10.5435/00124635-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Moed BR, Carr SE, Watson JT. Open reduction and internal fixation of posterior wall fractures of the acetabulum. Clin Orthop Relat Res. 2000;(377):57–67. doi: 10.1097/00003086-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Ebraheim NA, Patil V, Liu J, Sanford CG, Jr, Haman SP. Reconstruction of comminuted posterior wall fractures using the buttress technique: a review of 32 fractures. Int Orthop. 2007;31(5):671–675. doi: 10.1007/s00264-006-0246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Letournel E, Judet R, Elson RA, editors. Fractures of the acetabulum. New York: Springer; 1993. [Google Scholar]
- 9.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. 1964;46(8):1615–1646. [PubMed] [Google Scholar]
- 10.Moed BR. Acetabular fractures: the Kocher-Langenbeck approach. In: Wiss DA, editor. Master techniques in orthopaedic surgery: fractures. Philadelphia: Lippincott-Raven; 1998. pp. 631–656. [Google Scholar]
- 11.Olson SA, Finkemeier CG. Posterior wall fractures. Oper Tech Orthop. 1999;9(3):148–160. [Google Scholar]
- 12.D'aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36(3):451–475. [PubMed] [Google Scholar]
- 13.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1973;55(8):1629–1632. [PubMed] [Google Scholar]
- 14.Moed BR, Smith ST. Three-view radiographic assessment of heterotopic ossification after acetabular fracture surgery. J Orthop Trauma. 1996;10(2):93–98. doi: 10.1097/00005131-199602000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Ficat P, Arlet J. Necrosis of the femoral head. In: Hungerford DS, editor. Ischemia and necrosis of bone. Baltimore: Williams and Wilkins; 1980. pp. 53–74. [Google Scholar]
- 16.Kaempffe FA, Bone LB, Border JR. Open reduction and internal fixation of acetabular fractures: heterotopic ossification and other complications of treatment. J Orthop Trauma. 1991;5(4):439–445. doi: 10.1097/00005131-199112000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Wright R, Barrett K, Christie MJ, Johnson KD. Acetabular fractures: long-term follow-up of open reduction and internal fixation. J Orthop Trauma. 1994;8(5):397–403. doi: 10.1097/00005131-199410000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Kumar A, Shah NA, Kershaw SA, Clayson AD. Operative management of acetabular fractures: a review of 73 fractures. Injury. 2005;36(5):605–612. doi: 10.1016/j.injury.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 19.Chiu FY, Chen CM, Lo WH. Surgical treatment of displaced acetabular fractures: 72 cases followed for 10 (6-14) years. Injury. 2000;31(3):181–185. doi: 10.1016/s0020-1383(99)00277-6. [DOI] [PubMed] [Google Scholar]
- 20.Deo SD, Tavares SP, Pandey RK, El-Saied G, Willett KM, Worlock PH. Operative management of acetabular fractures in Oxford. Injury. 2001;32(7):581–586. doi: 10.1016/s0020-1383(00)00200-x. [DOI] [PubMed] [Google Scholar]
- 21.Petsatodis G, Antonarakos P, Chalidis B, Papadopoulos P, Christoforidis J, Pournaras J. Surgically treated acetabular fractures via a single posterior approach with a follow-up of 2-10 years. Injury. 2007;38(3):334–343. doi: 10.1016/j.injury.2006.09.017. [DOI] [PubMed] [Google Scholar]
- 22.Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum: a meta-analysis. J Bone Joint Surg Br. 2005;87(1):2–9. [PubMed] [Google Scholar]
- 23.Murphy D, Kaliszer M, Rice J, McElwain JP. Outcome after acetabular fracture: prognostic factors and their interrelationships. Injury. 2003;34(7):512–517. doi: 10.1016/s0020-1383(02)00349-2. [DOI] [PubMed] [Google Scholar]
- 24.Liebergall M, Mosheiff R, Low J, Goldvirt M, Matan Y, Segal D. Acetabular fractures: clinical outcome of surgical treatment. Clin Orthop Relat Res. 1999;(366):205–216. [PubMed] [Google Scholar]
- 25.Moed BR, McMichael JC. Outcomes of posterior wall fractures of the acetabulum: surgical technique. J Bone Joint Surg Am. 2008;90(Suppl 2 Pt 1):87–107. doi: 10.2106/JBJS.G.01471. [DOI] [PubMed] [Google Scholar]
- 26.Moed BR, WillsonCarr SE, Watson JT. Results of operative treatment of fractures of the posterior wall of the acetabulum. J Bone Joint Surg Am. 2002;84(5):752–758. doi: 10.2106/00004623-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Johnson EE, Matta JM, Mast JW, Letournel E. Delayed reconstruction of acetabular fractures 21-120 days following injury. Clin Orthop Relat Res. 1994;(305):20–30. [PubMed] [Google Scholar]
- 28.Matta JM, Merritt PO. Displaced acetabular fractures. Clin Orthop Relat Res. 1988;(230):83–97. [PubMed] [Google Scholar]
- 29.Helfet DL, Schmeling GJ. Management of complex acetabular fractures through single nonextensile exposures. Clin Orthop Relat Res. 1994;(305):58–68. [PubMed] [Google Scholar]