Abstract
Background
Some surgeons consider the abscission of a part of the articular bursa around the point of the input of ganglion's nape (average 1-2 cm diameter) to be very important with excellent results. However, a literature search revealed disagreement as to whether it is essential to repair a bursa defect. This study examined the effectiveness of this method without repairing the articular defect. An attempt was made to identify the anatomical origin of wrist ganglia during the surgical procedure.
Methods
This study evaluated 124 wrist ganglia that had been treated surgically during 2004-2009 using this technique and without repairing the bursa defect (1-2 cm in diameter). The variables studied were age, gender, time from the occurrence till abscission of the ganglia, former surgical interventions, preoperative and postoperative pain, insertion of the ganglion's nape and complications. Sixty-six patients with a mean follow-up of 42 months and minimum 12 months were examined.
Results
At the time of the follow-up, 80.3% had no pain whereas 92.2% showed a remarkable improvement. Seven cases of recurrence (10.6%) were found 2 to 85 months after surgery, of which most appeared during the first year (71.4%). It is important to mention that the majority of the dorsal ganglia (42.8%) originated from the capitate-lunate joint. None of the patients presented with scapholunate or other instability.
Conclusions
This surgical method is a simple and safe with excellent long-term results and a lower recurrence rate compared to other surgical approaches. Overall, repair of the articular bursa is unnecessary.
Keywords: Wrist ganglia, Dorsal, Volar, Excision
The wrist ganglia are the commonest benign soft tissue tumor of the hand. According to some authors, they represent 60% to 70% of all soft tissue tumor of the hand.1) Most of the ganglia are dorsal with only 40% originating from the volar aspect of the wrist.2) The incidence in females is higher than in males3) and most cases (70%) occur in the second to fifth decade of life.4)
Prior treatments of wrist ganglia included massaging with a splint, dubbing with mercure, strapping on a bullet, radiation, suture transfixation and rapture either with the spine of a bible or the examiner's thumb. Current treatments include benign neglect, aspiration with or without methylprednizolone,5) aspiration with an injection of tetradecyl sulfate6) and surgical excision simple or with a capsulectomy.
Angelides and Wallace4) reported that the pedicle of the ganglia penetrate the wrist capsule, particularly over the ligament. Macroscopic studies indicated the presence of a tortuous duct communicating with the scapholunate joint. This duct might function as a valve, allowing the synovial fluid to be pumped into the cyst from the wrist joint. They proposed an excision of the tissue removing the involved segment of the joint capsule and the deep attachments to the scapholunate ligament. According to Angelides and Wallace,4) Razemon,7) the recurrence rate was very low (1-2%). This study examined the results of surgical removal of the ganglia including abscission a part of the bursa without repairing the bursa defect.
METHODS
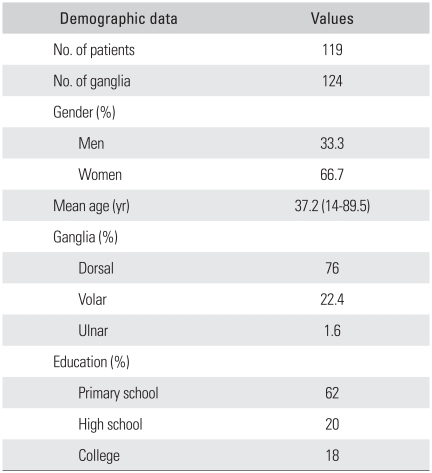
One hundred nineteen patients underwent an excision and capsulectomy of 124 ganglia from 2004-2009 in the Orthopaedic Department of Amalia Hospital in Athens and the Orthopaedic Department of University Hospital of Alexandroupolis. Ninety-four (76%) were dorsal, 28 (22.4%) were volar and two (1.6%) were located at the ulnar aspect of the wrist. The male:female ratio was 2:1. Their ages ranged from 14 to 89.5 years with a mean of 37.2 years. Most patients were between 20-40 years of age (56.5%). In all cases, minor trauma or stress of the ligament (10-50% previous trauma) was noted.4) Only one patient with severe trauma developed a dorsal ganglion 3 months later (Table 1).
Table 1.
Demographic Data of Patients
All patients were operated on und er an axillary block anesthesia. A transverse and longitudinal incision was made over the dorsal ganglia and over the palmar, respectively. The main body of the cyst, a cuff of wrist capsules approximately 1cm around the site of entry of the pedicle and any attachments to the deeper structures were excised. No repair of the capsule defect was made. After suture closure, the wrist was supported on a plaster slab for 10 days. Active mobilization was encouraged after plaster removal.
Fifteen percent of patients underwent surgery due to a recurrence of previously excised ganglia (without capsulectomy) after a period of 6 months to 11 years. All patients were reviewed with a minimum follow-up of one year. Sixty six patients (66 ganglia) could be reviewed for forty two months. Forty six of them were from the dorsal aspect, eighteen were from the volar and only two were from the ulnar aspect. The pre- and postoperative pain were rated using the visual analogue scale (VAS) scale (0-10). The range of action and grip strength were measured. A technological examination was also performed.
RESULTS
Anatomical Study
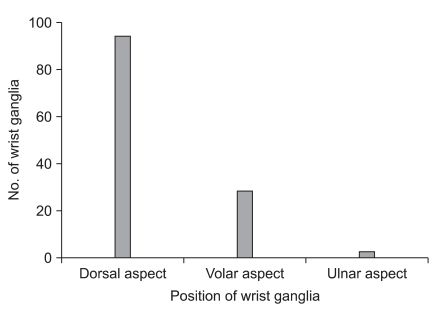
The age and gender distribution of our patients was similar to other studies.4,8,9) The anatomical origin of wrist ganglia was examined during the surgical procedure (Fig. 1) but this was not possible in some cases. The dimensions of the removed cyst were small (0-0.9 cm) in twenty-six cases, medium (1-1.19 cm) in sixty-three cases and large (2.0 cm) in thirty-six cases.
Fig. 1.
Origin of ganglia.
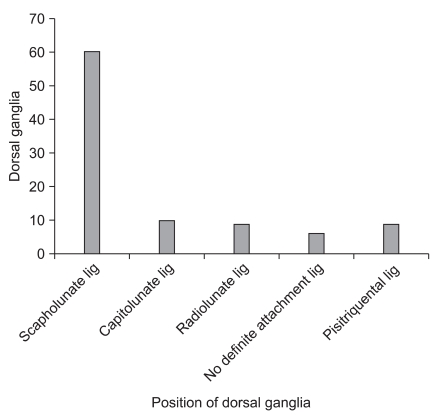
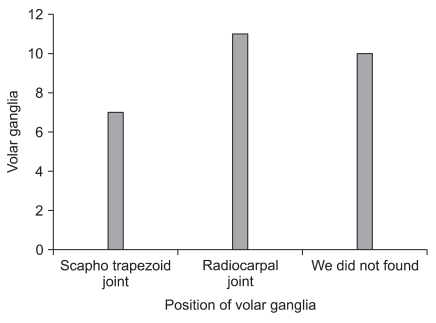
Anatomical analysis of the ninety-four dorsal ganglia showed that the pedicle in sixty of them arose from the scapholunate ligament, ten of them from the capitolunate ligament, nine from the radiolunate and nine from the pisitriquetral ligament. In particular, regarding the pisitriquetral ligament, the two ganglia were from the ulnar aspect and the remaining seven were radiocarpal. Definite attachment of the pedicle could not be found in six cases (Fig. 2). Surprisingly, the volar ganglia originated mostly from the radiocarpal joint but some were derived from the scapho-trapezoid joint. In ten cases, definite attachment of the pedicle could not be found (Fig. 3). In two cases the ganglia appeared from the ulnar aspect of the wrist.
Fig. 2.
Origin of dorsal ganglia. Lig: ligament.
Fig. 3.
Origin of volar ganglia.
These results (for the volar ganglia) are quite different from other studies, which reported 25 to 72 cases from the scapho-trapezoid joint.10) The ganglia were presented for more than 1 and 2 years in 67 and 45 cases, respectively.
Surgical Results
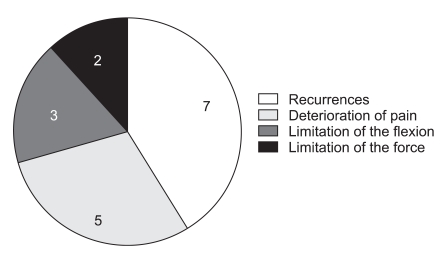
The indications for surgery were 79.8% with persistent pain (range, 7 to 9 according to VAS scale) and the remainder with cosmetic problems. One case had compression of the posterior interosseus nerve on the scapholunate ligament, and one patient had compression of the sensory branch of the ulnar nerve, which improved after the excision but not completely. At the time of the follow-up, 80.3% reported no pain (0 VAS) and 92.2% showed remarkable improvement (VAS, 0-2). The patients did not suffer any serious complications. Deterioration of the pain and a small limitation of wrist flexion (7°) was observed in five (7.8%) and three (4.5%) of the sixty-six cases, respectively. There were also two cases with a limitation of the grip strength (3%). Seven recurrences (10.6%) were noted two to eighty-five months after the surgical excision. Five of them had recurred within the first year (71.4%). The recurrences were five dorsal ganglia and two from the triquetral-pisiform articulation. Sixty percent of the dorsal wrist ganglion arose from the capitate-lunate articulation when they represented only the 10.6% of the dorsal ganglion. Only three patients accepted additional surgery with the same surgical procedure. No patient developed scapholunate or other types of instability after the X-ray examination (Fig. 4).
Fig. 4.
Number of complications.
DISCUSSION
Ganglia have been recognized by physicians since ancient times. Hippocrates described ganglia as containing "mucoid flesh." Through the ages, numerous hypotheses have been proposed to explain their nature. The current hypotheses include retention cysts, herniation of the joint capsule, degenerative cysts and ligament stress with an impaired repair process leading to a mucinous degeneration. Carp and Staut11) support the theory that ganglions arise from mucosus degeneration. This theory was not verified in the present study because 10% of patients were under twenty years of age; a fact that cannot be explained by the theory of mucoid degeneration of the capsule.8,11) Andren and Eiken12) proposed a valnular mechanism allowing the cyst to distend with the synovial fluid. McEvedy2) suggested that a ganglion most likely arises from a bursa and reported that the ganglia proceeds through three stages of development, a stage of formation, a stationary phase and a stage of diminution. Angelides and Wallace4) provided evidence to suggest the presence of a tortuous duct between the main cyst and the scapholunate joint. Further evidence of this apparent communication was provided by their surgical observations in 500 cases, all of which revealed an attachment of the cyst to the scapholunate ligament. Chronic stress in the ligament was suggested to be the reason for this consistent site of origin. However, the area of the capsule excised in these procedures was large. Therefore, this extensive excision might have included some ganglia arising some distance from the scapholunate ligament. In 1989, it was suggested13) that the ganglion is a secondary manifestation of an underlying periscaphoid ligament injury. Cadaveric studies14) showed that moderate rotatory subluxation of the scaphoid was produced when the dorsal radiocarpal ligament over the scapholunate joint and the scapholunate interosseous ligament were excised. It is also reported the presence of rotatory subluxation of the scaphoid, years after excising the ganglion. This study examined whether partial excision of the scapholunate ligament produced any element of carpal instability in any of our patients. No clinical or radiological signs of wrist instability were observed in this study. In any case, it would be prudent to minimize the resection of any scapholunate ligament attachment and obtain preoperative radiographs in any patient undergoing an excision of the wrist ganglion.
In this study, the main reason for surgery was pain (79.8% of our patients). In a previous series, pain was present in only 25-67% of cases6,8) with the exception of the series reported by Clay and Clement (87%).9)
The persistence of pain or a feeling of weakness after surgery was also documented. Improvement was noted in 92.3% of cases but also 3% and 7.8% reported a weaker grip and a limitation of dorsiflexion, respectively. Angelides and Wallace4) reported no persistent symptoms in any of their 346 patients and Clay and Clement9) showed that nine patients of their fifty had a weaker grip.
The recurrence rate appears to be controversial. In most studies,4,15) the recurrence ranged from 0% to 30%. These results appear to have been influenced by the fact that the majority of ganglia are dorsal,10,16) the pedicle of the ganglion was not found and the mean follow-up period. The reference rate was 10.6% with a 7.5% recurrence rate within the first year. The recurrences originated from the lunate capitate ligament in 60% of cases. The two ganglia from the ulnar aspect both recurred. Carp and Staut11) proposed an excision of the cyst, less extensive capsulectomy (0.5 cm2) and closure of the capsule with an absorbable suture with a recurrence rate of 5%.
Most recent studies preferred an arthroscopy resection of wrist ganglia.3,6,17-20) Few studies have compared the effectiveness of an arthroscopy resection with an open excision in a ganglionectomy.20) Most concluded that an arthroscopy resection is a reasonable alternative to an open excision but in some cases, the post operative functional result was better with an open excision.21)
In most studies, the mean follow-up duration was 24-36 months.18-21) Few had a longer follow-up than the present study and they referred to a small group of patients, which may have biased the results.22)
Overall, no treatment is indicated when there are no functional or significant esthetic problems. The presence of functional signs, particularly pain, stiffness, diminution of grasping force, or signs of compression can indicate the need for treatment. Complete surgical excision with a capsulectomy and closure of the defect is certainly the most effective method for obtaining a definitive cure.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Bain GI, Munt J, Turner PC. New advances in wrist arthroscopy. Arthroscopy. 2008;24(3):355–367. doi: 10.1016/j.arthro.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 2.McEvedy BV. The simple ganglion: a review of modes of treatment and an explanation of the frequent failures of surgery. Lancet. 1954;266(6803):135–136. doi: 10.1016/s0140-6736(54)90983-6. [DOI] [PubMed] [Google Scholar]
- 3.Osterman AL, Raphael J. Arthroscopic resection of dorsal ganglion of the wrist. Hand Clin. 1995;11(1):7–12. [PubMed] [Google Scholar]
- 4.Angelides AC, Wallace PF. The dorsal ganglion of the wrist: its pathogenesis, gross and microscopic anatomy, and surgical treatment. J Hand Surg Am. 1976;1(3):228–235. doi: 10.1016/s0363-5023(76)80042-1. [DOI] [PubMed] [Google Scholar]
- 5.Varley GW, Needoff M, Davis TR, Clay NR. Conservative management of wrist ganglia: aspiration versus steroid infiltration. J Hand Surg Br. 1997;22(5):636–637. doi: 10.1016/s0266-7681(97)80363-4. [DOI] [PubMed] [Google Scholar]
- 6.Holm PC, Pandey SD. Treatment of ganglia of the hand and wrist with aspiration and injection of hydrocortisone. Hand. 1973;5(1):63–68. doi: 10.1016/0072-968x(73)90013-2. [DOI] [PubMed] [Google Scholar]
- 7.Razemon JP. Surgical treatment of ganglions of the wrist by partial excision of the joint capsule: report on 303 cases. Ann Chir Main. 1983;2(3):230–243. doi: 10.1016/s0753-9053(83)80005-2. [DOI] [PubMed] [Google Scholar]
- 8.Nelson CL, Sawmiller S, Phalen GS. Ganglions of the wrist and hand. J Bone Joint Surg Am. 1972;54(7):1459–1464. [PubMed] [Google Scholar]
- 9.Clay NR, Clement DA. The treatment of dorsal wrist ganglia by radical excision. J Hand Surg Br. 1988;13(2):187–191. doi: 10.1016/0266-7681_88_90135-0. [DOI] [PubMed] [Google Scholar]
- 10.Gundes H, Cirpici Y, Sarlak A, Muezzinoglu S. Prognosis of wrist ganglion operations. Acta Orthop Belg. 2000;66(4):363–367. [PubMed] [Google Scholar]
- 11.Carp L, Staut AP. A study of ganglion with special reference to treatment. Surg Gynecol Obstet. 1928;47:460–468. [Google Scholar]
- 12.Andren L, Eiken O. Arthrographic studies of wrist ganglions. J Bone Joint Surg Am. 1971;53(2):299–302. [PubMed] [Google Scholar]
- 13.Watson HK, Rogers WD, Ashmead D., 4th Reevaluation of the cause of the wrist ganglion. J Hand Surg Am. 1989;14(5):812–817. doi: 10.1016/s0363-5023(89)80080-2. [DOI] [PubMed] [Google Scholar]
- 14.Ruby LK, An KN, Linscheid RL, Cooney WP, 3rd, Chao EY. The effect of scapholunate ligament section on scapholunate motion. J Hand Surg Am. 1987;12(5 Pt 1):767–771. doi: 10.1016/s0363-5023(87)80065-5. [DOI] [PubMed] [Google Scholar]
- 15.Wright TW, Cooney WP, Ilstrup DM. Anterior wrist ganglion. J Hand Surg Am. 1994;19(6):954–958. doi: 10.1016/0363-5023(94)90095-7. [DOI] [PubMed] [Google Scholar]
- 16.Bienz T, Raphael JS. Arthroscopic resection of the dorsal ganglia of the wrist. Hand Clin. 1999;15(3):429–434. [PubMed] [Google Scholar]
- 17.Dumontier C, Chaumeil G, Chassat R, Nourissat G. Arthroscopic treatment of dorsal wrist ganglia. Chir Main. 2006;25(Suppl 1):S214–S220. doi: 10.1016/j.main.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 18.Mathoulin C, Hoyos A, Pelaez J. Arthroscopic resection of wrist ganglia. Hand Surg. 2004;9(2):159–164. doi: 10.1142/s0218810404002169. [DOI] [PubMed] [Google Scholar]
- 19.Mathoulin C, Massarella M. Therapeutic interest of wrist arthroscopy: about 1000 cases. Chir Main. 2006;25(Suppl 1):S145–S160. doi: 10.1016/j.main.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 20.Rocchi L, Canal A, Fanfani F, Catalano F. Articular ganglia of the volar aspect of the wrist: arthroscopic resection compared with open excision. A prospective randomised study. Scand J Plast Reconstr Surg Hand Surg. 2008;42(5):253–259. doi: 10.1080/02844310802210897. [DOI] [PubMed] [Google Scholar]
- 21.Aydin A, Kabakas F, Erer M, Ozkan T, Tuncer S. Surgical treatment of volar wrist ganglia. Acta Orthop Traumatol Turc. 2003;37(4):309–312. [PubMed] [Google Scholar]
- 22.Petricig P, Pepe E. First choice treatment of the pediatric wrist ganglia. Minerva Pediatr. 2006;58(4):379–383. [PubMed] [Google Scholar]