Abstract
Objective
To determine the relationship between napping and cognitive function in preschool-aged children.
Methods
Daytime napping, nighttime sleep and cognitive function were assessed in fifty-nine typically developing children ages 3-5 years, who were enrolled in full-time childcare. Participants wore an actigraphy watch for 7 days to measure sleep and napping patterns, and completed neuropsychological testing emphasizing attention, response control, and vocabulary. Parents of participants completed behavior ratings and sleep logs during the study. Sleep/wake cycles were scored with the Sadeh algorithm.
Results
Children who napped more on weekdays were also more likely to nap during weekends. Weekday napping and nighttime sleep were inversely correlated, such that those who napped more slept less at night, while total weekday sleep remained relatively constant. Weekday napping was significantly (negatively) correlated with vocabulary and auditory attention span, and weekday nighttime sleep was positively correlated with vocabulary. Nighttime sleep was also significantly negatively correlated with performance, such that those who slept less at night made more impulsive errors on a computerized go/no-go test.
Conclusions
Daytime napping is actually negatively correlated with neurocognitive function in preschoolers. Nighttime sleep appears to be more critical for development of cognitive performance. Cessation of napping may serve as a developmental milestone of brain maturation. Children who nap less do not appear to be sleep deprived, especially if they compensate with increased nighttime sleep. An alternative explanation is that children who sleep less at night are sleep deprived and require a nap. A randomized trial of nap restriction would be the next step in understanding the relationship between napping and neurocognitive performance.
Keywords: childhood, attention, sleep, cognition, actigraphy, preschool
The frequency of afternoon naps in children declines between the ages of 2 and 5 years as the biphasic sleep/wake pattern gives rise to a consolidated rest period at night 1-3. Even during infancy, maturation of the sleep/wake cycles is suggested by sleep consolidation. Among premature infants, for example, those with longer, uninterrupted sleep had higher developmental scores on the Bayley-2 Developmental Scales 4. Nevertheless, the role of napping in cognitive development has not been studied in preschoolers. Based on the trends in napping 1-3, it may be speculated that preschool children have an increased diurnal sleep drive and often have difficulty maintaining wakefulness for a full school day, unlike most elementary school aged children. Reduction in nap duration during the preschool years may therefore be a marker for cognitive development. Conversely, nap restriction during the preschool years has the potential to impede developmental progress. Interpretation of nap cessation is challenging, as it may be attributed to cultural or parental choices 5-7; biological variables, such as maturation of chronobiological mechanisms 2; or personality factors such as temperament 8.
A meta-analysis of sleep deprivation studies in adults found that sleep deprivation has profound detrimental effects on cognitive functioning 9. At the same time, daytime naps have been shown to restore wakefulness and promote performance and learning in adults 10-12. Older children with nighttime sleep restriction have been shown to have increased inattentive behaviors 13. Similarly, there is an increased incidence of sleep problems in preschool-aged children with ADHD-like symptoms 14. Nevertheless, at the present time, there are no studies that have directly examined the relationship between the neurocognitive performance and amount of napping among preschool-aged children. As such, there are no clear guidelines to establish when a child “outgrows” the need for a nap. It is also not known what the requirements are in preschoolers for the performance of cognitive tasks, especially those involving attention and cognitive control. This issue is potentially important because if premature nap restriction leads to decreased alertness, there may be an adverse impact on a child’s ability to learn in the classroom.
Since evidence-based guidelines for when naps are developmentally critical have not been established, some early childhood programs have eliminated napping to increase educational learning time 15. This practice has, however, been called into question, as school-aged children who are sleep deprived display difficulty with both attention and emotional regulation 13, 16, 17. Hence, while it is presumed that an adequate amount of sleep is necessary for growth and development 18; it is less clear to what extent naps play a significant role in promoting learning and performance in preschoolers.
The purpose of the present study was to examine the relationship between napping and neurocognitive function in typically developing children ages 3 to 5 years. We hypothesized that the children who napped more would perform better on neurocognitive tests compared to those who napped less. We also hypothesized that nap deprivation was similar to sleep deprivation and would result in similar decrements in cognitive function that have been observed in adult studies.
Methods
Participants
Following approval from the University of Maryland Institutional Review Board, participants were recruited from twenty-two local daycare centers in the greater Baltimore/Washington area. Children were included in the study if they met the following inclusion criteria: 1) age 3-5 years, 2) currently attending preschool, 3) receiving full-time daycare, 3) healthy, and typically developing. Children were excluded if they: 1) were in elementary school, 2) attended part-time daycare, 3) had reports of developmental delays, 4) had chronic medical problems that could interfere with sleep patterns (e.g., asthma, heart disease, reflux, seizures), or 5) were taking any daily medications.
Study Procedures
Flyers were distributed to twenty-two local day care centers after approval by the center director. A member of the research team also visited the centers to answer questions and invite parents to participate. Those parents who expressed interest in the study provided contact information. An initial phone call to the parents screened for medical problems and history of developmental delay. Study methods were explained to the parents as well as risks and benefits to the study. Parents whose children were eligible for the study and who expressed an interest in the study met with a member of the research team in a private room of the day care center. The consent form was reviewed with the parent and after signing the consent form, the child was screened for developmental delays using the Peabody Picture Vocabulary Test-IV (PPVT-IV) 19. If the results of the PPVT-IV were in at least the broad average range (i.e., standard score ≥ 85), and the parent denied the child had any chronic medical problems or was taking any daily medication, the child was scheduled for the study.
For each participant, the study began on a Monday. Children were fitted with an actigraph watch with a hospital band which was worn continuously for seven days (Monday to Monday). Parents were given daily sleep logs to complete while their child was wearing the watch. Parents were also asked to record any nap periods, periods of quiet activities (e.g., solitary independent play, watching television), time the child was in bed (asleep or not), time the child tried to fall asleep, number of arousals during the night, and rise time. When the child was in the child care center, members of the center staff reported nap times to the parents for the logs. Parents were contacted by phone by a member of the research team during the 7-day study period to encourage compliance and to answer any questions from the parents. On Fridays between 8:20 AM and 11:45 AM, children completed a 20-minute screening battery of neuropsychological tests by a evaluator who was blinded to the child’s napping status since parent logs and actigraphy data were collected afterwards.
Actigraphy
Actigraphy was performed using MicroMini Motionlogger Actigraph watches (Ambulatory Monitoring Inc., Ardsley, NY). The watches were programmed for 1-minute recording epochs in zero-crossing mode. Sleep/wake cycles were estimated from actigraphy data using the Action 4 software (Ambulatory Monitoring Inc., Ardsley, NY). Data were scored with the Sadeh scoring algorithm, which has been validated by comparison to polysomnography for this type of actigraph watch 20. The Sadeh algorithm is computed as follows: PS = 7.601 – 0.065MW5 – 1.08NAT – 0.056SD6 – 0.0731ln (ACT), where PS is the probability of sleep, MW5 is the average number of activity counts during the scored epoch and a window of five epochs preceding and following it, NAT is the number of epochs with activity level equal to or higher than 50 but lower than 100 activity counts in a window of 11 minutes, SD6 is the standard deviation of the activity counts during the scored epoch and the five epochs preceding it, and ln(ACT) is the natural logarithm of the number of activity counts during the scored epoch 1. If PS is zero or greater, the specific epoch is scored as sleep; otherwise, it is scored as wake 21. Final scoring was determined by comparison with parent logs (SDC Figure).
Cognitive and Behavioral Measures
Peabody Picture Vocabulary Test, Fourth Edition (PPVT-IV) 19
The PPVT-IV is a measure of single word listening vocabulary and a screening test of verbal ability, as well as an estimate of intellectual functioning. The child is presented four pictures at a time and asked to point to a picture that represents a particular word. Raw score totals scores were used in analyses.
Number Recall (Kaufman Assessment Battery for Children, Second Edition—KABC-II)22
The Number Recall subtest is a measure of auditory attention/verbal span for digit strings forward. Number series were presented orally to the child at a rate of one per second. The child repeated the series back verbatim. Raw score totals were obtained and used in analyses.
Statue (NEPSY-II) 23
The Statue test is a measure of inhibition and motor persistence in which the child is asked to maintain a body position with eyes closed during a 75-second period, and to inhibit the impulse to respond to sound distracters. Thus, motor inhibitory control is an essential component of successful performance on this task. Observations are made every 5 seconds for the presence of body movement, eye opening, and talking. A score of 2 is recorded for each 5-second interval in which there is no movement, eye-opening or talking, and a score of 1 is recorded for each interval in which there is one type of error. Score of 0 is recorded if there are two or more errors during a 5-second epoch. The total score ranges from 0-30. Total raw scores were used as the dependent variable for this task. Performance on the Statue subtest has been shown to be reduced, relative to controls, in preschool children with ADHD 24.
Auditory Continuous Performance Test for Preschoolers (ACPT-P) 25
This measure is a computerized, auditory go/no-go task. Two auditory stimuli (dog bark, bell), are used as target and non-target respectively. Duration of each stimulus is 690 ms, and interstimulus interval is fixed at 5000 msec. A total of 15 targets and 15 non-targets are arranged randomly so that the child is presented 4 targets and 11 non-targets in the first half of the test, and 11 targets and 4 non-targets in the second half of the test. The total time of the test is approximately three minutes. During the test, the child is instructed to place his/her hands on two marks, just in front of the keyboard, and to hit the space bar (marked with a sticker) whenever the dog bark sound is heard. Four variables are obtained: 1) errors of omission; 2) errors of commission; 3) mean response time (calculated as the average response latency for correct hits); and, 4) coefficient of variability, which is calculated as the standard deviation of response times for correct hits, divided by the mean response time for correct hits. Performance on the ACPT-P has been shown to improve between ages 3 and 5 years in typically developing children 25. Preschool children with ADHD show increased errors of omission and increased response variability on the ACPT-P 24.
Behavior Assessment System for Children, Second Edition (BASC-II) 26
The preschool form of the BASC-2 is used for ages 2-5 years, and asks parents to rate a variety of problematic as well as adaptive behaviors for their child, based on a four-point scale of frequency, ranging from “Never” to “Almost Always.” The Hyperactivity and Inattention scales were used in the present study.
Data Analyses
Mean and standard deviations were calculated for napping times based on actigraphy and neuropsychological test results. One-way ANOVA was used to compare napping times for each age group (i.e., 3-year olds, 4-year olds, and 5-year olds). Pairwise differences were assessed using Tukey’s test for honestly significant differences (HSD). Pearson correlations were used to assess relationships between age (in months), daytime napping, nighttime sleep, and total sleep times. Partial correlations (controlling for age) were used to assess relationships between sleep (napping and nighttime sleep) and neurocognitive test results. Significance was set at p < 0.05 (two-tailed).
Results
Sample Characteristics
A total of 59 children (30 girls, 29 boys) ranging from 3 to 5 years old completed the study. The mean age for the sample was 4.3 years (SD = 9.05). The sample included 18 three-year olds (9 girls), 29 four-year olds (14 girls) and 12 five-year olds (7 girls). There were no significant differences in sex distribution at each age (χ2 = 0.57, p = .75). The majority (58%) of the sample was African-American, 22% were Caucasian, 5% were Asian, and 15% were multiracial.
Participant Compliance and Completion of Sleep Data
A total of 64 subjects were initially enrolled in the study. Five children dropped out of the study due to noncompliance with actigraphy. In an additional 5 children, data from the actiwatch could not be downloaded at the end of the study due to watch malfunction. Two of these children repeated the study while the parents of the other three children chose not to repeat the study. Seven children had incomplete actigraph data, such that the actigraph stopped recording after the first 4-5 days. Two of these children repeated the study while the parents of the other children chose not to repeat the study.
Sample characteristics of napping amounts based on actigraphy are listed in Table 1. Throughout the entire week, on average, 3-year olds napped 60 minutes per day, 4-year olds 68 minutes per day, and 5-year olds 21 minutes per day. Overall, both 3-year olds and 4-year olds napped significantly longer than and 5-year olds, but there was no significant difference between 3-year olds and 4-year olds for total napping time.
Table 1.
Weekday and Weekend Napping, and Total Sleep by Age Group
| Age 3a (n = 18) | Age 4b (n = 29) | Age 5c (n =12) | Age-Group Comparisons (Tukey HSD) | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Mean | SD | Mean | SD | Mean | SD | ||
| Weekday Napping | 342 | 191 | 386 | 230 | 116 | 164 | a > c (p = .004), b > c (p < .001) |
| Weekend Napping | 59 | 56 | 88 | 89 | 17 | 33 | b > c (p = .009) |
| Total Napping | 420 | 190 | 473 | 269 | 145 | 85 | a > c (p = .005), b > c (p = .001) |
| Total Sleep | 4021 | 479 | 4018 | 348 | 3886 | 407 | All n.s. |
Note: Means are in minutes. Weekday napping amount is based on five days (Monday through Friday). Weekend napping amount is based on two days (Saturday and Sunday). Total napping and total sleep is over the entire week (Monday through Sunday).
Associations between Napping, Nighttime and Total Sleep
Correlations between napping and other sleep measures are shown online (SDC Table). As expected, weekday napping significantly decreased with age. However, the total sleep time (napping + nighttime sleep) during the week was relatively similar within each age group, suggesting that preschoolers who nap less (during the week) sleep more at night, and vice versa (Figure 1). There was also a tendency for children who nap more during the week to also nap more on weekends (and vice versa).
Figure 1.
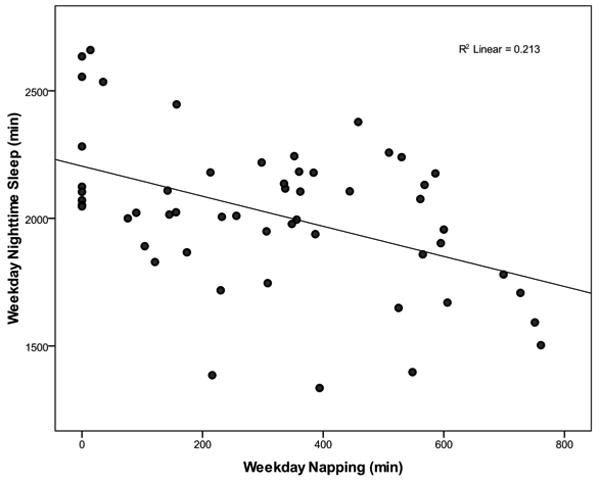
Relationship between weekday napping and nighttime sleep
Group Performance on Behavioral and Cognitive Variables
Age was significantly associated with raw score performance on PPVT-IV vocabulary (r = .66), Number Recall (r = .42), ACPT-P mean response time (r = -.48), and omission errors (r = -.35), all p < .01. In all cases, children performed better (or more efficiently) with increased age. Participant performance by age group on the behavioral measures and cognitive tests are listed in Table 2.
Table 2.
Sample Performance on Cognitive and Behavioral Variables
| Age 3a (n = 18) | Age 4b (n = 29) | Age 5c (n =12) | Group Comparisons (Tukey HSD) | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Mean | SD | Mean | SD | Mean | SD | ||
| PPVT-IV | 65.5 | 17.7 | 78.8 | 19.2 | 103.0 | 16.6 | a < b*,c**; b < c** |
| KABC-II Number Recall | 7.4 | 1.9 | 8.1 | 2.5 | 10.2 | 2.8 | a < c**; b < c* |
| NEPSY-II Statue | 21.0 | 6.8 | 19.3 | 5.9 | 25.2 | 5.5 | b < c** |
| ACPT-P | |||||||
| Omissions | 2.7 | 3.3 | 1.3 | 2.8 | 0.5 | 1.2 | a < c* |
| Commissions | 0.7 | 1.1 | 0.6 | 0.9 | 0.2 | 0.4 | All n.s |
| Mean Response Time | 1778.9 | 883.2 | 1053.7 | 756.2 | 877.7 | 391.5 | a < c**; b < c** |
| Variability | 0.3 | 0.6 | 0.5 | 0.3 | 0.5 | 0.4 | All n.s |
| BASC-II | |||||||
| Attention | 49.9 | 6.7 | 48.9 | 6.2 | 48.4 | 9.8 | All n.s |
| Hyperactivity | 48.0 | 9.7 | 47.5 | 7.3 | 46.8 | 9.5 | All n.s. |
Note: PPVT-IV = Peabody Picture Vocabulary Test-IV; KABC-II = Kaufman Assessment Battery for Children-II; BASC-II = Behavior Assessment System for Children-II. PPVT-IV, Number Recall, Statue, and ACPT-P variables all listed as raw scores. Mean response time and variability are reported in milliseconds. BASC-II scores are T-scores;
p < .05,
p < .01.
Association between Sleep and Cognitive Function
The associations between sleep and cognitive variables are listed in Table 3. After controlling for age, weekday napping was significantly (negatively) correlated with Number Recall (r = -.27, p = .05; Figure 2), and with PPVT-IV (r = -.33, p = .02; Figure 3A), suggesting that greater daytime napping was associated with poorer cognitive performance. The significant relationship between napping and Number Recall (but not PPVT-IV) remained even after controlling for both age and weekday nighttime sleep duration (r = -.32, p = .02). Conversely, weekday napping was not significantly associated with the Statue or ACPT-P tests, or with parent report of behavior problems (BASC-II). After controlling for age, total weekday nighttime sleep was significantly (positively) correlated with PPVT-IV vocabulary (Figure 3B; r =.29, p = .03), such that more nighttime sleep was associated with better vocabulary and vice versa. Total weekday sleep per se (napping plus nighttime) was not significantly correlated with PPVT-IV vocabulary (Figure 3C, r = .08, p = .55). Weekday nighttime sleep was significantly (negatively) correlated with ACPT-P errors of commission (r = -.29, p = .03), such that less nighttime sleep was associated with more impulsive (commission) errors (and vice versa). Because the range of total commission errors in our sample was small (0-3), and because most children in the sample made no commission errors, we also compared average weekday nighttime sleep between those children who made no commission errors (n = 43) and those who made one or more commission errors (n = 17). After controlling for age, those children who made no errors had significantly more weekday nighttime sleep [2083.5 minutes/week] than those who made errors [1768.7 minutes/week; F[(1,53) = 12.2, p = .001]. See Figure 3D. These results did not appear to be influenced by time of testing. As an exploratory analysis, we analyzed the correlation between all cognitive variables and testing time (relative to actual nap time) and found no significant associations (correlations ranged from 0.075 to 0.154). In other words, the nearer the child was tested to his/her actual nap time had no impact on cognitive performance).
Table 3.
Partial Correlation (controlling for age) among Cognitive and Sleep Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Weekday Napping | ||||||||||
| 2. Weekday Night Sleep | -.462*** | |||||||||
| 3. PPVT-IV | -.327** | .291* | ||||||||
| 4. Number Recall | -.265* | -.048 | .125 | |||||||
| 5. Statue | -.183 | .134 | .227 | .007 | ||||||
| 6. Omissions | -.018 | -.051 | -.153 | -.049 | .038 | |||||
| 7. Commissions | .085 | -.290* | -.159 | -.093 | -.120 | .043 | ||||
| 8. Mean Response Time | .004 | -.081 | -.004 | -.146 | .087 | .666*** | .185 | |||
| 9. Variability | -.141 | .113 | .013 | -.089 | -.111 | -.162 | .041 | -.162 | ||
| 10. BASC II Attention | -.172 | .092 | ||||||||
| 11. BASC-II Hyperactivity | .015 | .114 | .736*** |
Note:
p < 0.05,
p < 0.01,
p < 0.001
Figure 2.
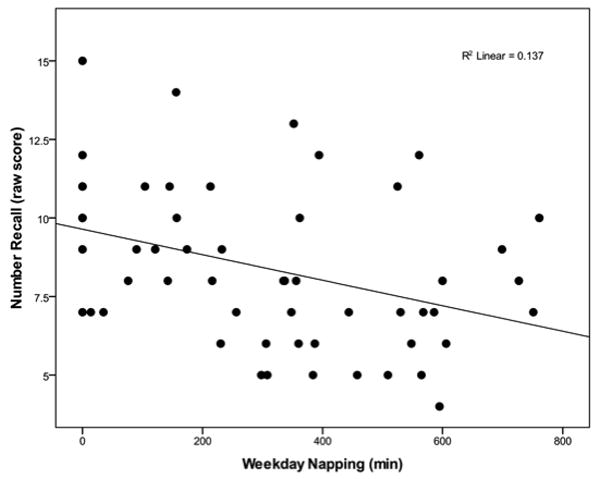
Association between daytime napping and auditory attention (number recall)
Figure 3.
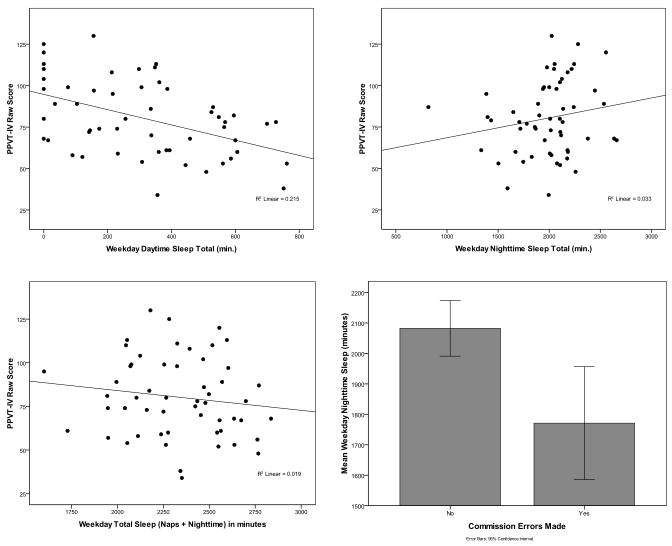
Weekday napping and nighttime sleep and cognitive function
Discussion
Among typically developing preschoolers in full-time daycare, performance on neurocognitive tests decreased with increased napping time. This finding was inconsistent with our initial hypothesis. Additionally, daytime napping was negatively associated with nighttime sleeping such that more weekday napping was associated with less nighttime sleep, and vice versa. Thus, the most parsimonious conclusion from these data is that, among preschoolers (after considering age-related changes), greater nighttime sleep facilitates neurocognitive performance, and reduces the need for daytime napping; while reduced nighttime sleep leads to increased need for daytime naps, and is associated with attentional control problems. The present results also suggest that children who nap less do not experience neurocognitive deficits if they compensate with nighttime sleep since total amount of sleep was the same between children who nap more and those that nap less.
These findings highlight the importance of adequate nighttime sleep for preschoolers. Even after controlling for age, those preschoolers who got more sleep at night (and conversely needed less during the day) performed better cognitively, including increased vocabulary and improved attentional control. Further, the inverse relationship between daytime napping and auditory attention span (Number Recall) was robust, and remained, even after controlling for amount of nighttime sleep. This pattern of findings represents potentially new information about the relationship between daytime and nighttime sleep requirements, and their association with neuropsychological functioning among preschoolers. It might also be hypothesized that naps are less important than nighttime sleep for performance, or that naps interfere with nighttime sleep (which is actually more crucial for cognitive performance).
There are at least three possible interpretations for the overall pattern of findings. First, it is possible that the amount of nighttime sleep may facilitate learning and memory in preschool children. Non-REM sleep, particularly slow wave sleep, is considered to provide consolidation of experience-dependent changes in cortical circuitry 18, thus setting the stage for more efficient consolidation of newly learned material. We speculate that more slow wave sleep occurs during longer periods of nighttime sleep among preschoolers, thus facilitating consolidation of newly learned material. Secondly, it is possible that daytime napping is a marker for brain development, such that children who nap less have more mature brains and therefore perform better on neurocognitive function. The age-related changes in neurocognitive test scores appear to parallel to the age-related changes in napping (i.e., less napping in older children). Therefore, a decline in napping may represent a developmental phenomenon, and may even indicate maturational differences within the same age group. Evidence supporting this interpretation includes the strong relationship between the PPVT-IV vocabulary (thought to be a more global measure of cognitive function) and daytime napping. However, we acknowledge that our conclusion that reduction in napping is a potential marker for cognitive development needs additional confirmation in controlled clinical trials. A third possibility is that naps weaken the sleep drive at night and therefore these children may sleep less at night because their sleep debt is decreased by daytime sleep 27. Alternatively, children who sleep less at night may be partially sleep deficient and require a nap. This partially sleep deficient state may be reflected by poorer performance on testing which was performed prior to naptime. Given that this was an observational study, we cannot determine the cause effect relationship. The best way to determine a cause-effect relationship would be through a randomized trial of nap restriction. Restricting daytime naps in preschoolers who lack the opportunity or ability to increase their nighttime sleep might further impair performance significantly.
The sleep patterns identified in our sample were generally in agreement with other studies which indicate a gradual decline in napping from two to five-year-olds 1-3. In our sample, mean weekday napping time for 4-year-olds was greater than for three year olds, but not significantly so. However, there was a rapid drop-off in napping after age 4 years, such that 5-year-olds napped the least. Despite our speculation that preschoolers have a limited ability to sustain wakefulness, our findings indicate it is an age-related phenomena which may be influenced by the amount of night time sleep. These findings may parallel what is known about brain development in this age range. Between ages 3-6 years, peak growth rates of the anterior corpus callosum and frontal cortex (important for motor, attention, and general cognitive functioning) 28, 29 have been noted. Therefore, these findings may provide support to our hypothesis that napping cessation may represent a marker for brain development.
Of note, in the present sample, weekday napping was inversely correlated with weekday nighttime sleep, such that total daily sleep (including napping and nighttime sleep) was relatively consistent from between ages 3 and 5 years. The difference between children within these age groups was the proportion of napping to total sleep. This pattern is consistent with previous reports that preschoolers who took longer naps had shorter nighttime sleep periods and earlier rise times 30. This finding is striking, and highlights the need to consider the interrelationships between daytime napping and nighttime sleep in preschoolers. Thus, the cognitive and behavioral effects of napping can be best understood by considering the amount of nighttime sleep the child has had (since those who sleep more at night seem to require less napping during the day).
By measuring both weekday and weekend sleep, we were able to examine whether children who slept less during the week, needed to “catch up” on weekends. The present data did not demonstrate such a pattern. Children who napped more during the week were also more likely to nap more on weekends and vice versa. Therefore, less napping during the week did not appear to result in a rebound in sleep since there was not a significant increase in the amount of sleep on weekends for those who did not nap during weekdays.
The current results also suggest that less daytime napping is a different phenomenon in preschoolers than overall sleep deprivation. Possibly, the results may be affected by the increased amount of nighttime sleep in children who nap less. Therefore, children who do not nap may not experience chronic sleep deprivation if they compensate for lack of daytime sleep with increased nighttime sleep. The variability in cognitive findings and the absence of a relationship between behavioral ratings of inattention and hyperactivity and napping may be because the sample was not actually sleep deprived.
Limitations of the study include the observational design and the sampling of children solely from daycare centers. Cause-effect relationships cannot be made with the naturalistic sampling of sleep behaviors. Additionally, conclusions are limited to children in day care settings. It is unclear whether similar patterns would emerge among children not enrolled in full time daycare. Further, although the data acquisition was naturalistic, it is unclear whether parents or daycare providers changed their practices with regard to napping when it was known that a child was wearing an actigraphy watch.
In summary, the present study highlights the interrelatedness of nighttime sleep, daytime napping, and cognitive function among preschoolers. The inverse relationship between daytime and nighttime sleep may play a role in our results which indicate that nighttime sleep was positively correlated with cognitive function. A logical next step in this line of research would be a randomized trial of nap restriction or a trial of modified bedtimes and wake times. These types of studies would enable a better understanding of the relationship between napping and neurocognitive function and reduce other confounding factors, such as parental or cultural choice for determining the amount of naps. Future research is required to expand the assessment of sleep function, as well as the mechanisms of facilitating (or interfering with) cognitive development that are attributable to napping.
Supplementary Material
Acknowledgments
Supported by K12RR023250, P30HD-24061 (Intellectual and Developmental Disabilities Research Center), and NIH HL074441. We also acknowledge the efforts by Natrell Darden for subject recruitment and collection of data.
References
- 1.Iglowstein I, Jenni O, Molinari L, et al. Sleep duration from infancy to adolescence: Reference values and generational rends. Pediatrics. 2003;111(2):302–307. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 2.Webb W, Dinges D. Development of Human Napping. In: Dinges D, B R, editors. Sleep and Alertness: Chronobiological, Behavioral and Medical Aspects of Napping. New York, NY: Raven Press; 1989. pp. 31–51. [Google Scholar]
- 3.Weissbluth M. Naps in children: 6 months-7 years. Sleep. 1995;19(2):82–87. doi: 10.1093/sleep/18.2.82. [DOI] [PubMed] [Google Scholar]
- 4.Gertner S, Greenbaum C, Sadeh A, et al. Sleep-wake patterns in pretemn infants and 6 month’s home environment: Implications for early cognitive development. Early Human Development. 2002;68:93–102. doi: 10.1016/s0378-3782(02)00018-x. [DOI] [PubMed] [Google Scholar]
- 5.Ottaviano S, Giannotti F, Cortesi F, et al. Sleep characteristics in healthy children from birth to 6 years of age in the urban area of Rome. Sleep. 1996;19(1):1–3. [PubMed] [Google Scholar]
- 6.Kohyama J, Shiiki T, Ohinata-Sugimoto J, et al. Potentially harmful sleep habits of 3-year ol children in Japan. J Dev Behav Pediatr. 2002;23(2):67–70. doi: 10.1097/00004703-200204000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Crosby B, LeBourgeois MK, Harsh J. Racial differences in reported napping and nocturnal sleep in 2-to 8-year-old children. Pediatrics. 2005;115(1):225–232. doi: 10.1542/peds.2004-0815D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weissbluth M. Sleep duration, temperament, and Conners’ rating of three-year-old children. J Dev Behav Pediatr. 1984;5(3):120–123. [PubMed] [Google Scholar]
- 9.Pilcher J, Huffcutt A. Effects of sleep deprivation on performance: A meta-analysis. Sleep. 1996;19:318–326. doi: 10.1093/sleep/19.4.318. [DOI] [PubMed] [Google Scholar]
- 10.Dhand R, Sohal H. Good sleep, bad sleep! The role of daytime naps in healthy adults. Current Opinion in Pulmonary Medicine. 2006;12:379–382. doi: 10.1097/01.mcp.0000245703.92311.d0. [DOI] [PubMed] [Google Scholar]
- 11.Hiyashi M, Ito S, Hori T. The effects of a 20-min nap in the mid-afternoon on sleepiness, performance and EEG activity. Int J Psychophysiol. 1999;110:272–279. doi: 10.1016/s0167-8760(99)00009-4. [DOI] [PubMed] [Google Scholar]
- 12.Hiyashi M, Watanabe M, Hori T. Effects of a 20-min nap in the mid-afternoon on mood, performance, and EEG activity. Clin Neurophysiol. 2000;110:272–279. doi: 10.1016/s1388-2457(98)00003-0. [DOI] [PubMed] [Google Scholar]
- 13.Fallone G, Acebo C, Arnedt J, et al. Effects of acute sleep restriction on behavior, sustained attention, and response inhibition in children. Percept Mot Skills. 2001;93(1):213–229. doi: 10.2466/pms.2001.93.1.213. [DOI] [PubMed] [Google Scholar]
- 14.Goodlin-Jones B, Waters S, Anders T. Objective sleep measurement in typically and atypically developing preschool children with ADHD-like profiles. Child Psychiatry Hum Dev. 2009;40:257–268. doi: 10.1007/s10578-009-0124-2. [DOI] [PubMed] [Google Scholar]
- 15.Daniels L, Lewin D. A survey of pre-kindergarten and kindergarten napping policy in the U.S; Associated Professional sleep Societies Conference; Denver. 2005. Abstract. [Google Scholar]
- 16.Lagivne J, Arend R, Rosenbaum D, et al. Sleep and behavioral problems among preschoolers. J Dev Behav Pediatr. 1999;20(3):164–169. doi: 10.1097/00004703-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Sadeh A, Gruber R, Raviv A. Sleep, neurobehavioral functioning, and behavior problems in school-aged children. Chil Dev. 2002;73(2):405–417. doi: 10.1111/1467-8624.00414. [DOI] [PubMed] [Google Scholar]
- 18.Frank M, Issa N, Stryker M. Sleep enhances plasticity in the developing visual cortex. Neuron. 2001;30:275–287. doi: 10.1016/s0896-6273(01)00279-3. [DOI] [PubMed] [Google Scholar]
- 19.Dunn L, Dunn L. Manual: Peabody Picture Vocabulary Test. Fourth Edition. Bloomington, MN: Pearson Assessments; 2007. [Google Scholar]
- 20.Sadeh A, Sharkey K, Carskadon M. Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep. 1994;17(3):201–207. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
- 21.de Souza L, Benedito-Silva A, Pires M, et al. Further validation of actigraphy for sleep studies. Sleep. 2003;26(1):81–85. doi: 10.1093/sleep/26.1.81. [DOI] [PubMed] [Google Scholar]
- 22.Kaufman A, Kaufman N. Kaufman assessment battery for children-II. Circle Pines, MN: American Guidance Service; 2004. [Google Scholar]
- 23.Korkman M, Kirk U, Kemp S. NEPSY-II: A developmental neuropsychological assessment. San Antonio, TX: The Psychological Corporation; 2007. [Google Scholar]
- 24.Mahone E, Pillion J, Hoffman J, et al. Construct validity of the auditory continuous performance test for preschoolers. Developmental Neuropsychology. 2005;27:11–33. doi: 10.1207/s15326942dn2701_2. [DOI] [PubMed] [Google Scholar]
- 25.Mahone EM, Pillion JP, Hiemenz JR. Initial development of an auditory continuous performance test for preschoolers. Journal of Attention Disorders. 2001;5:93–106. [Google Scholar]
- 26.Reynolds C, Kamphaus R. Behavior assessment system for children-2. Circle Pines, MN: American Guuidance Systems, Inc.; 2004. [Google Scholar]
- 27.Stein M, Mendelsohn J, Obermeyer W, et al. Sleep and behavior in school-aged children. Pediatrics. 2001;107(4):e60. doi: 10.1542/peds.107.4.e60. [DOI] [PubMed] [Google Scholar]
- 28.Ding X, Sun Y, Braab H, et al. Evidence of rapid ongoing brain development beyond 2 years of age detected by fiber tracking. Am J Neuroradiol. 2008;29:1261–1265. doi: 10.3174/ajnr.A1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nagy Z, Westerberg H, Klingberg T. Maturation of white matter is associated with the development of cognitive functions during childhood. J Cogn Neurosci. 2004;16:1227–1233. doi: 10.1162/0898929041920441. [DOI] [PubMed] [Google Scholar]
- 30.Acebo C, Sadeh A, Seifer R, et al. Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1 - to 5-year-old children. Sleep. 2005;28(12):1568–1577. doi: 10.1093/sleep/28.12.1568. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


