Gastroduodenal Crohn's disease (GCD) occurs in 0.5–4% of patients with ileocolonic disease, though it occurs very rarely as an isolated entity, and, according to various studies, is frequently difficult to treat with medical and surgical interventions.1 Acute pancreatitis has also been occasionally associated with Crohn's disease, though the exact etiology remains unclear. We report a case of a patient who presented initially with severe episodes of acute pancreatitis, nausea, vomiting, and weight loss and was found to have gastric Crohn's disease. The patient was treated with medical therapy, to which he responded with complete resolution of symptoms, and since then has remained clinically stable.
Case Report
A 50-year-old African-American man presented to our outpatient gastrointestinal clinic with no significant medical history other than a pancreatitis episode two months earlier. During his episode of pancreatitis, the patient was admitted with complaints of nausea, vomiting, and a 15-pound weight loss. Due to his decreased nutritional status, the patient was given parental nutrition via a peripherally inserted central catheter line. Esophagogastroduodenoscopy performed during this admission showed hypertrophic gastric folds and two pyloric channel ulcers (with gastric biopsies negative for Helicobacter pylori), and the patient was placed on omeprazole (Figures 1 and 2). Abdominal ultrasound ruled out gallstones or any ductal dilatation, whereas abdominal computed tomography showed changes consistent with acute pancreatitis, though no pseudocysts or masses were noted. Laboratory examinations were normal for both calcium and triglyceride levels. The patient denied taking any medications before being admitted.
Figure 1.
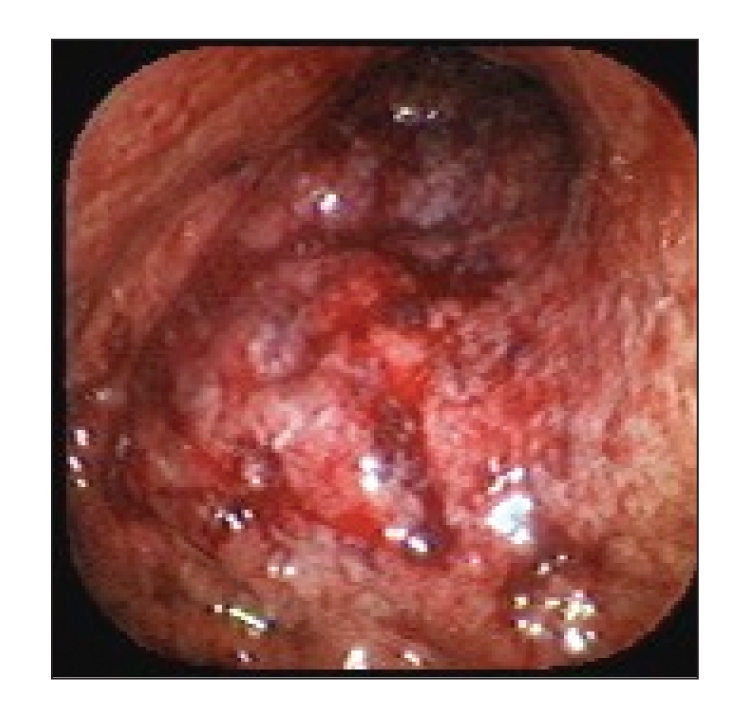
Endoscopic image showing gastric erosions and erythema.
Figure 2.
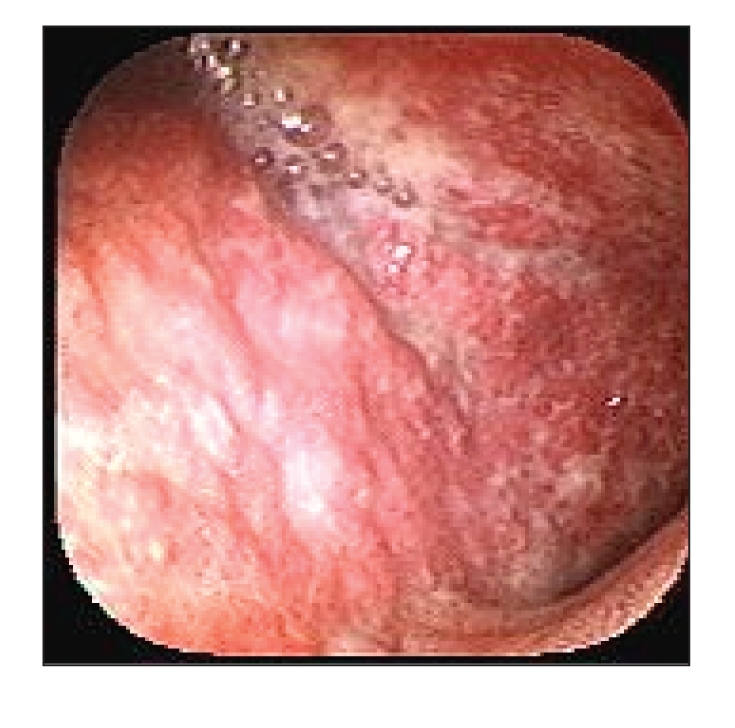
Endoscopic image showing gastric nodularity.
Two months later, on the patient's second visit to the outpatient gastrointestinal clinic, the patient had a lipase level of 1,195 U/L, an amylase level of 187 U/L, a triglyceride level of 31 mg/dL, and a calcium level of 8.8 mg/dL. As further work-up for his weight loss and hypertrophic folds, the patient underwent endoscopic ultrasound (EUS), which revealed diffuse thickening, ulcerations, nodularity, and friability of the gastric mucosa, with thickening of the gastric folds up to 11.8 mm in diameter. Gastric biopsy showed no evidence of malignancy, H. pylori, acid-fast bacillus, or fungi. There was evidence of severe acute and chronic gastritis with superficial aphthous ulcers and granulomas consistent with a diagnosis of GCD (Figures 3 and 4). Subsequent colonoscopy showed no endoscopic or histologic evidence of Crohn's disease in the colon or terminal ileum. Our patient was diagnosed with GCD and started on mesalamine 500 mg daily, omeprazole 20 mg daily, and a taper of prednisone 60 mg. He experienced significant clinical improvement on the prednisone and mesalamine. The patient's amylase and lipase levels continued to decrease and, of note, he was also abstinent from alcohol. When the prednisone was tapered down to 5 mg daily, the patient developed a recurrence of vomiting and weight loss. He was subsequently taken off mesalamine and omeprazole and then restarted on his original dose of prednisone 60 mg daily. The patient was also concomitantly started on 6-mercaptopurine (6-MP) 100 mg daily. Over time, he was tapered off steroids, but he has continued on 6-MP for more than 9 years and has remained clinically asymptomatic during that time.
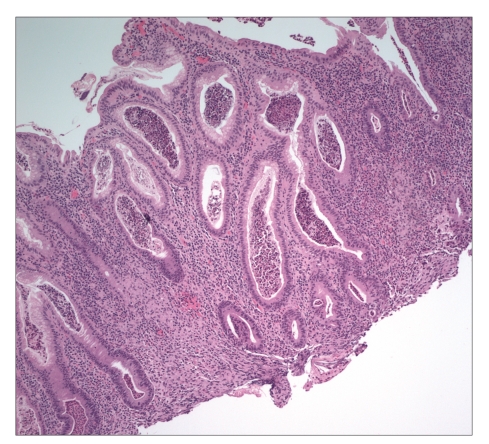
Figure 3.
Light microscopy image of gastric biopsy showing diffuse chronic inflammation, pit microabscesses, and focal poor-formed nonnecrotizing granulomas. No Helicobacter pylori infection was seen with special staining.
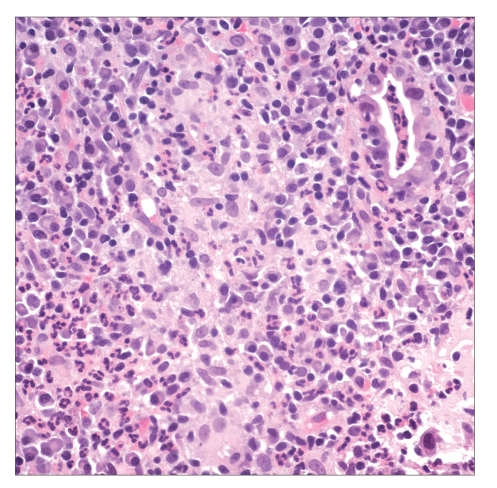
Figure 4.
Light microscopy image showing a high-power photomicrograph of a gastric biopsy revealing poorly formed nonnecrotizing granuloma adjacent to a ruptured gastric pit.
Discussion
Isolated GCD is a rare disorder, as evidenced by the findings that only 1 of 940 Crohn's disease patients from a major Dutch university referral center had isolated proximal Crohn's disease and that the largest case series of isolated GCD published to date consisted of only 7 patients.2 The finding of granulomas on biopsy in isolated GCD is even more rare. Endoscopically, GCD can manifest as mucosal edema, focal or diffuse redness, nodular lesions or erosions, and ulcers.3 In a case series of 49 patients with Crohn's disease with gastroduodenal involvement, more than 75% of the patients had abnormal gastroduodenal biopsies,4 but only 9% of the patients had granulomas. Also worth noting is that when Crohn's disease does involve the upper gastrointestinal tract, concomitant disease nearly always exists in the small bowel or colon. However, there is no evidence of this in our patient.3 Based on our patient's presenting symptoms, histopathology findings on biopsy, EUS findings, and the dramatic response to Crohn's disease treatment and maintenance therapy, the diagnosis of GCD was established. Other disease entities in the differential diagnosis to consider in patients with gastric granulomas include sarcoidosis, granulomatous gastritis, foreign body reaction, vasculitis-associated disease, and Whipple disease.
In an analysis of 89 GCD cases, Nugent and Roy found that most patients with GCD achieved positive results from intermittent corticosteroid therapy.5 Our patient responded very well to proton pump inhibitors and corticosteroids initially, but experienced a reoccurrence of disease symptoms when therapy was tapered, after which he was finally placed on 6-MP. He currently remains on 6-MP and has been asymptomatic for more than 9 years.
Acute pancreatitis has occasionally been associated with Crohn's disease, but whether a causal association exists remains uncertain. In a study of 48 patients with Crohn's disease and pancreatitis, the etiology of the pancreatitis was gallstones (21%), significant alcohol intake (15%), use of purine analogs (13%), duodenal Crohn's involvement (12%), use of other medications (4%) and idiopathic causes (8%).6 Possibilities for the etiology of pancreatitis in our patient included GCD, ethanol or idiopathic.
In summary, we report an unusual patient with isolated GCD with gastric granulomas on biopsy who presented with symptoms of pancreatitis, which completely resolved with medical therapy.
References
- 1.Reynolds HL, Jr, Stellato TA. Crohn's disease of the foregut. Surg Clin North Am. 2001;81:117–135. doi: 10.1016/s0039-6109(05)70276-0. [DOI] [PubMed] [Google Scholar]
- 2.Wagtmans MJ, Verspaget HW, Lamers CB, van Hogezand RA. Clinical aspects of Crohn's disease of the upper gastrointestinal tract: a comparison with distal Crohn's disease. Am J Gastroenterol. 1997;92:1467–1471. [PubMed] [Google Scholar]
- 3.Wagtmans MJ, van Hogezand RA, Griffioen G, Verspaget HW, Lamers CB. Crohn's disease of the upper gastrointestinal tract. Neth J Med. 1997;50:S2–S7. doi: 10.1016/s0300-2977(96)00063-0. [DOI] [PubMed] [Google Scholar]
- 4.Wright CL, Riddell RH. Histology of the stomach and duodenum in Crohn's disease. Am J Surg Pathol. 1998;22:383–390. doi: 10.1097/00000478-199804000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Nugent FW, Roy MA. Duodenal Crohn's disease: an analysis of 89 cases. Am J Gastroenterol. 1989;84:249–254. [PubMed] [Google Scholar]
- 6.Moolsintong P, Loftus EV, Jr, Chari ST, Egan LJ, Tremaine WJ, Sandborn WJ. Acute pancreatitis in patients with Crohn's disease: clinical features and outcomes. Inflamm Bowel Dis. 2005;11:1080–1084. doi: 10.1097/01.mib.0000186485.30623.ad. [DOI] [PubMed] [Google Scholar]