Abstract
Purpose/Background:
Posterior shoulder tightness (PST) has been implicated in the etiology of numerous shoulder disorders. Therefore, clinicians and researchers must have a reliable and valid method for quantifying PST. The purpose of this study was to investigate the interrater reliability, minimal detectable change at the 90% confidence interval (MDC90) and construct validity of an inclinometric measurement designed to quantify PST.
Methods:
Two investigators each performed sidelying PST measurements on the non-dominant shoulder of 45 asymptomatic participants in a blinded repeated measures design. Upon completion of the PST measurements, one rater assessed active internal and external rotation for the validity component of the investigation.
Results:
Interrater reliability using an intraclass correlation coefficient (ICC) model 2,k was good (ICC 5 0.90). The MDC90 indicated that a change of greater than or equal to 9 degrees would be required to be 90% certain that a change in the measurement would not be the result of inter-trial variability or measurement error. Construct validity was evaluated using active internal rotation for convergence and external rotation for discrimination. Construct validity was supported by a good to excellent relationship between PST and internal rotation (r 5 0.88) and by an inverse relationship between PST and external rotation (r 5 20.07).
Conclusion:
The sidelying procedure described in this investigation appears to be a reliable and valid means for quantifying PST when strict measurement protocols are adhered to. An advantage of this procedure lies in the ability to control scapular position to ensure motion is limited to the glenohumeral joint. Moreover, the use of inclinometry provides an absolute angle of tightness that may be used for intersubject comparison, documenting change, and to determine reference values. Clinicians and researchers should consider the MDC values presented when interpreting change values during subsequent measurement sessions.
Keywords: capsule, flexibility, mobility, range of motion
INTRODUCTION
Epidemiological data suggests that up to sixty-seven percent of the general population will experience shoulder pain at some point in their lifetime.1 The shoulder complex ranks third among regions treated by physical therapists in outpatient clinics and has been reported to be a primary location of injury or pain among individuals who participate in weight-training, baseball, football and wrestling.2–6 Although the etiology of shoulder disorders is multifactorial, specific impairments such as inadequate mobility and posterior shoulder tightness (PST) have been associated with common disorders such as labral tears and impingement syndrome in both the general and athletic population.7–12
Throwing athletes, in particular have a predilection for PST owing to repetitive microtrauma at the posterior capsule induced during the follow through phase of the throwing motion.11,13 It has been suggested that the tensile stresses placed on the shoulder during throwing may induce hypertrophy and thickening of the posterioinferior capsule thus producing PST.11,13 Although these capsular changes have been implicated in the etiology of PST, it must be recognized that muscular restrictions may be involved as well. The presence of PST has been identified in throwing athletes with internal impingement syndrome and arthroscopically diagnosed superior labral, anterior to posterior (SLAP) lesions.11 Burkhart et al11 reported that both tennis and baseball players who perform exercises to mitigate PST tend to have a decreased incidence of shoulder problems compared to controls participating in similar sports.
Although common to the overhead athlete, PST has been reported among other subgroups of the population. Tyler et al7 reported increased PST among individuals diagnosed with impingement syndrome when compared to controls. Ticker et al14 reported an association between impingement syndrome and posterior capsular thickening or shortening among patients with a history of shoulder pain who underwent arthroscopy. Additionally, an association between PST and recreational weight-training participation has been reported among asymptomatic individuals when compared to controls suggesting the potential for task specific tissue adaptations.15,16
Clinical recognition of risk or pathology attributed to PST requires a reliable and valid measurement technique that may be used among the heterogeneous population and that is of reasonable expense and availability. Measurement techniques for PST have been reported in the literature using both supine and sidelying procedures as well using varying instruments including inclinometers, goniometers, and tape measures.10,17–21 While these techniques may have utility as a clinical measurement they are not able to discriminate between PST of contractile versus inert tissue. Essentially, the techniques described attempt to isolate glenohumeral horizontal adduction by restricting scapular movement.10,17–19,21 Tyler et al19 first described a sidelying technique for quantifying PST, whereby the scapula is stabilized in retraction while the humerus is passively adducted across the chest, while being maintained at 90 degrees of forward flexion and neutral rotation. The distance from the medial epicondyle to the table is recorded with larger distances implying greater PST. Good intra and interrater reliability of this technique were reported, with intraclass correlation coefficients (ICC) of 0.92 and 0.80 respectively. Myers et al10 assessed the intra and interrater reliability of the sidelying technique using a linear measurement device that recorded the distance between the table and medial epicondyle and reported ICCs 5 0.42-0.83 and 0.69 respectively. A disadvantage of both of the aforementioned sidelying techniques is that PST is not quantified using an absolute value that can be compared between individuals. Other researchers have examined supine measurements performed with either inclinometry or goniometry10,17,18 and reported good intra and inter rater reliability (ICC 5 0.75-0.94); however, a disadvantage of this technique is the inability to visualize a consistent start position of the scapula. A modified sidelying measurement method, performed with the use of an inclinometer, was used for this investigation. This measurement is beneficial because it provides an absolute measurement value which permits intersubject comparison. To the knowledge of the authors, no previously published investigations have reported the interrater reliability, minimal detectable change (MDC90) and validity of a sidelying PST measurement using inclinometry.
The purpose of this study was to investigate the interrater reliability, minimal detectable change (MDC90) and construct validity of an inclinometric measurement technique designed to quantify PST. Construct validity was evaluated using active internal rotation (IR) for convergence given the direct relationship between posterior capsuloligamentous tension and IR.22–24 External rotation (ER) was used for discrimination as biomechanical studies have identified an absence of influence between PST and ER.24 The authors hypothesized that the PST measurement would have good interrater reliability based on the nature of the testing procedures. With regard to validity, it was hypothesized that a strong positive relationship would exist between PST and IR with little or no relationship between PST and ER. Active measurements of IR and ER were used to establish validity since participants were healthy and without injury or neuromuscular impairments therefore soft tissue tightness was the most likely limiting factor for all measurements.
METHODS
Subjects
A convenience sample of forty-five asymptomatic adult participants, 22 men and 23 women, were recruited for this investigation from a local university setting over an18-month time frame. None of the subjects reported history or current participation in overhead sports with the tested upper extremity. Recruitment was based on advertisement throughout the university. Participants who met the study requirements and agreed to participate signed an informed consent form approved by the Institutional Review Board at Nova Southeastern University.
Upon consenting to participate in the study, participants completed a questionnaire to report age, body mass, height, and arm dominance. Exclusion criteria consisted of reported shoulder pain at the time of data collection, recent shoulder surgery for which the participant was still receiving care, or current participation in a rehabilitation program for the non-dominant shoulder. All participants who volunteered met inclusion criteria. One participant was disqualified following the IR measurement as a result of compromised form during repeated attempts. The mean and standard deviation (SD) for the participants age, BMI, body mass, and height were 26.31 years (3.74), 25.17 kg/m2(4.05), 76.72 kg (17.50), and 173.68 cm (9.01) respectively. Testing was performed using the non-dominant arm to account for confounding variables such as humeral retroversion which may be present in the dominant arm and cause a limitation of internal rotation11 independent of PST. The left arm was the non-dominant arm in 40 of the 45 subjects.
Instruments
A standard plinth and Baseline® bubble inclinometer, (model 12-1056, Fabrication Enterprises; White Plains, New York) was used for all measurements. The PST measurement required the use of a velcro strap to secure the inclinometer to the participants' mid-humerus (Figure 1A) during the procedure. A 24 inch bubble level, (model 7724-0, Johnson Level & Tool; Mequon, Wisconsin) anchored to a carpenter's square of similar dimension, (model 45-500, Stanley Works; New Britain, Connecticut) was used during the PST measurement to set the inclinometer at an accurate zero starting point relative to the vertical plane (Figure 1B). The bubble level was used to ensure that the participants' trunk was directly perpendicular to the plinth upon initiating the PST measurement.
Figure 1.
A) Baseline® Bubble Inclinometer attached to Velcro strap b) Setting zero point of inclinometer using bubble level. Once the bubble level is at the zero point(*) the trained assistant turns the inclinometer dial to zero(**).
Procedures
Preparatory Activities
Visual diagrams of the measurement positions and warm-up exercises were presented to participants prior to testing. The purpose of the warm-up was to ensure participant safety and to facilitate consistency of the data being tested. The warm-up required approximately 3 minutes total time and consisted of two supervised exercises including pendulums and standing scapular retractions, neither of which were believed to offer a mobilization effect. The warm-up was repeated between testing sessions for consistency. Each participant was required to perform the same warm-up for consistency; however, to the authors' knowledge there is neither a benefit nor detriment to performing a warm-up.
Measurement of Posterior Shoulder Tightness
Following the warm-up, measurements of the non-dominant extremity were taken using the inclinometer in an intrasession design. Measurements of PST were repeated 2 consecutive times by each rater with a 10 second rest between repetitions and a 3-5 minute rest between raters. The warm-up was repeated following the 3-5 minute rest interval. Once PST measurements were complete, rater 2 performed two consecutive measurements each for IR and ER active range of motion (AROM). Measurements were not randomized to ensure a consistent physiological status of the shoulder structures. The inclinometer was set to a zero value prior to each of the three measurements using a bubble level to ensure accuracy. A trained assistant with approximately 6-months experience using inclinometry recorded measurements from the inclinometer in order to ensure the investigators were blinded to the findings. Measurements were recorded at eye-level to ensure accuracy and were not verbalized to the tester given the potential for measurement bias given a 10-second rest between measurements was used.
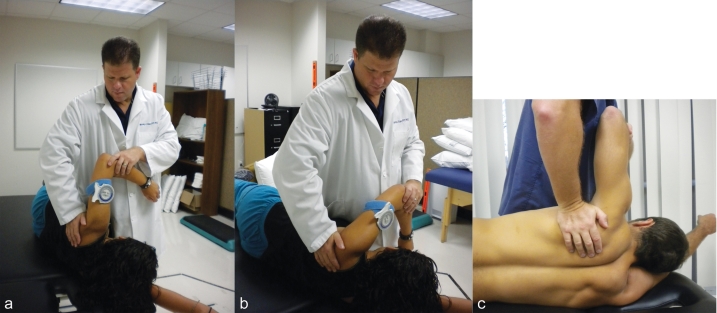
The exact procedure used for measuring PST has previously been investigated for intrarater reliability in the authors lab with ICC (3,k) reported at 0.96.21 Participants were required to lie on their non-tested (dominant arm) side ½ the length of their humerus from the edge of a standard plinth to allow clearance of the forearm past the plinth during horizontal adduction. The non-tested extremity was placed under their head to support a neutral head position. Their trunk was directly perpendicular to the plinth with hips and knees flexed to 45 degrees. The bubble level anchored to the carpenter's square was then used to ensure that their trunk was directly perpendicular to the plinth. The investigator stood facing the participant at the level of their shoulders and grasped the participant's elbow with one hand while passively abducting the humerus to ninety degrees while maintaining zero degrees of rotation at the humerus and approximately ninety degrees of elbow flexion. Humeral positioning was maintained with the initial contact hand while the other hand manually contacted the participant's lateral scapular border and placed it in a fully adducted (retracted) position. The retracted scapular position was maintained by the investigator throughout the test. The position of ninety degrees of humeral coronal abduction with neutral rotation and scapular retraction was the start position of the test (Figures 2A and 2C). Prior to passively lowering the humerus, a verbal cue was given stating “relax your arm and allow me to lower it to the table”. The investigator then passively lowered the humerus into horizontal adduction toward the plinth in the transverse plane maintaining neutral humeral rotation and scapular stabilization in the retracted position (Figure 2B). The movement was ceased once the investigator determined that the scapula or humerus was unable to be further stabilized and/or movement stopped. Once the end point was reached, the investigator directed a trained assistant to record the measurement from the inclinometer to a data collection sheet.
Figure 2.
Posterior shoulder tightness measurement technique. (a) Start position for posterior shoulder tightness measurement. Participants arm is passively positioned in 90° abduction by examiner and scapula is retracted as illustrated. (b) Examiner passively lowers arm across chest into horizontal adduction while manually retracting the scapula through contact with the lateral border. (c) Close up picture illustrating scapular stabilization.
Measurement of Active Internal Rotation
The procedure for measuring IR-AROM followed an established protocol.21,25 The procedure has previously been investigated for intrarater reliability with ICC (3,k) reported at 0.99.21 Participants were positioned prone, with the tested arm supported on the table at 90 degrees of abduction, elbow flexed to 90 degrees and the wrist in neutral (Figure 3). A towel roll was placed directly under each participant's arm to ensure a neutral position of the humerus in the coronal plane without migration into the transverse plane. Additionally, the towel roll was used to provide stabilization. Neutral horizontal positioning of the arm was considered the position where the humerus did not migrate into horizontal adduction or abduction. Neutral horizontal positioning of the humerus ensured that tension in the posterior soft tissues was minimized. Additionally, in the prone position, both the towel roll and table serve to potentially limit compensatory scapular anterior tilt and protraction25 as opposed to the supine position which would require manual stabilization from the investigator. The effect of scapular stabilization on measurement reproducibility is contradictory as IR measurement procedures without stabilization have been reported to possess both higher and lower levels of reproducibility when compared to procedures stabilizing the shoulder and or scapula.26,27 This investigation did not use any manual stabilization during IR measurements. Participants were asked to rotate their arm to their maximum available IR without compromising form and verbal cues were provided as necessary. Although the towel roll was used with an individualized circumference that maintained the humerus in a horizontal neutral, participants were requested to stop movement if they began to exhibit compensatory form and no measurements were recorded with the scapula tilted anteriorly beyond the start position. Once movement ceased the inclinometer was placed on the distal forearm proximal to the radiocarpal joint and the measurement was recorded. Five participants were required to repeat the IR measurement once as a result of compromised form. One participant's results were excluded from further analysis as a result of compromised form on two repeated occasions during the IR measurement.
Figure 3.
Active range of motion measurement for internal rotation. Participant is prone with arm supported on the table in 90 degrees of shoulder abduction and elbow flexed to 90 degrees. A towel roll is placed directly under the arm to provide stabilization and maintain the arm in a neutral position with regard to the transverse plane. Participant actively brings arm back into internal rotation as illustrated above. Examiner places inclinometer on the mid to distal forearm just proximal to the wrist once participant reaches active end-range.
Measurement of Active External Rotation
ER-AROM followed an established protocol (Figure 4).21,25 The procedure has previously been investigated for intrarater reliability with ICC (3,k) reported at 0.97.21 Participants were measured in the supine position with the tested arm supported on the table in 90 degrees of abduction with the elbow flexed to 90 degrees and wrist in neutral. A towel roll was placed directly under each participant's arm to achieve neutral horizontal positioning in the transverse plane, thus preventing the arm from moving into horizontal abduction or adduction. Maintaining neutral horizontal positioning of the humerus ensured that tension in the anterior soft tissue passing over the joint was minimized. Participants were asked to bring their arm back to their maximum available ER motion without compromising form, with verbal cues provided as necessary. Once movement ceased the inclinometer was placed on the distal forearm proximal to the radiocarpal joint and the measurement was recorded.
Figure 4.
Active range of motion measurement for external rotation. Participant is supine with hips and knees flexed to 45 degrees. Tested arm is supported on the table in 90 degrees of abduction, elbow flexed to 90 degrees. A towel roll is placed under the humerus. Participant actively brings arm back into external rotation. Once active end-range is achieved the examiner places inclinometer on the mid to distal forearm just proximal to the wrist.
Data Analysis
Collected data was transferred to SPSS (SPSS Inc, Chicago, Illinois), Version 15.0 for Windows for analysis. Descriptive data including mean measurement angles with standard deviations (SD) were calculated for each rater. The interrater reliability of PST was determined by the intraclass correlation coefficient (ICC) model 2, k. The mean value of 2 measurements was used for the analysis. Model 2, k was used for the interrater analysis to determine if this particular instrument can be used with confidence and reliability among equally trained clinicians.28,29 Our interpretation of the ICC value was based on guidelines offered by Portney and Watkins28, whereas a value of above 0.75 was classified as good and a value of 0.50 to 0.75 would be considered to have moderate to poor reliability. ICC values may be influenced by intersubject variability of scores, as a large ICC may be reported despite poor trial-to-trial consistency if the intersubject variability is too high.28,30 The standard error of measurement (SEM) is not affected by intersubject variability30 and is important for clinical utilization of a measurement procedure; therefore it was reported in conjunction with the ICC's using the formula: SEM 5 SD.28 The MDC was calculated for the interrater measurements using the formula: MDC90 5 1.65 * SEM * to determine the magnitude of change that would exceed the threshold of measurement error at the 90% confidence level.28,31 MDC90 values were rounded to the nearest degree to reflect the smallest unit of measurement on the inclinometer.
A Pearson's correlation coefficient (r) was used for the construct validity component of the investigation. Our interpretation of the r value was based on guidelines offered by Portney and Watkins28, whereas a value of above 0.75 was considered to be a good to excellent relationship. A correlation of 0.00 to 0.25 was considered to have little or no relationship. For the correlation coefficient, the a was considered significant at the .05 level. An a priori power analysis indicated that a sample size of 46 would be needed to obtain 80% power if we estimated an r 5 0.40 with the a2 5 0.05. One participant was excluded from final data analysis secondary to disqualification from study as a result of inability to perform IR without compensation.
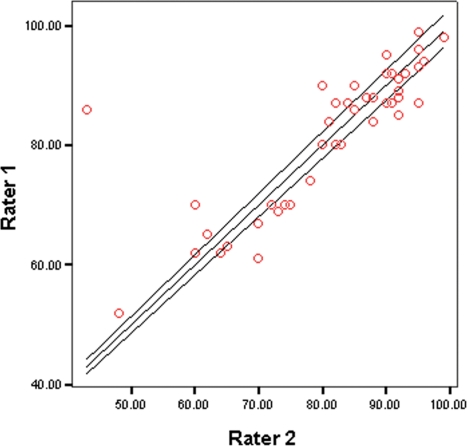
Scatter plots were used to provide a visual illustration of the PST measurements between raters as well as to provide a visual analysis of the relationship between PST and both IR and ER.
RESULTS
Mean angular measurements of PST for the interrater reliability analysis with SD, ICC (95%CI), SEM, and MDC90 are presented in Table 1. The data indicates good interrater reliability for PST (ICC) 5 0.90. The MDC90 for the interrater analysis indicated that a change of equal to or greater than 98 would be required to be 90% certain that the change is not due to inter-trial variability or measurement error.
Table 1.
Interrater Reliability Analysis: Posterior shoulder Tightness measurement.
| Shoulder Test | Rater A Mean angle°(SD) | Rater B Mean angle°(SD) | ICC 2,k (95% CI) | SEM° | MDC°90 |
|---|---|---|---|---|---|
| PST | 81.56(11.74) | 81.24(13.13) | 0.90(0.82-0.94) | 4 | 9 |
Convergent validity using the measurements from rater 2, was supported by a good correlation between PST and internal rotation (r 5 0.88) with p < .001 indicating a significant correlation. Discriminant validity was supported by an inverse correlation between the PST measurement and external rotation (r 5 20.07), with p 5 .673 indicating no significant correlation. Table 2 presents the PST, IR and ER measurements (mean, SD and ranges) obtained by rater 2 for the validity analysis.
Table 2.
Measurement Angles from Rater 2 used for Construct Validity Analysis
| Shoulder Test | Mean Angle°(SD) | Range° | Minimum° | Maximum° |
|---|---|---|---|---|
| PST | 81.24(13.13) | 56 | 43 | 99 |
| Internal Rotation | 80.12(11.30) | 50 | 52 | 102 |
| External Rotation | 100.47(10.27) | 46 | 77 | 123 |
SD= Standard deviation; PST= Posterior Shoulder tightness
The scatterplot (Figure 5) illustrating the PST measurements from rater 1 and 2 illustrate the strong positive correlation. Additionally, a strong positive relationship is illustrated on the scatterplot for the measurements of PST and IR (Figure 6) whereas the measurements for PST and ER (Figure 7) appear random and reflect no linear relationship.
Figure 5.
Scatterplot illustrating a strong positive relationship between measurements of PST for rater 1 and 2.
Figure 6.
Scatterplot illustrating a strong positive relationship between measurements of posterior shoulder tightness (PST) and internal rotation.
Figure 7.
Scatterplot illustrating a random pattern indicating no relationship between measurements of posterior shoulder tightness (PST) and external rotation.
DISCUSSION
This investigation sought to determine the interrater reliability, MDC and construct validity of a measurement procedure designed to quantify PST. Although the posterior capsule and ligamentous structures have been implicated as primary contributors to PST14,22,24 it can not be stated with absolute certainty that they are the only source of PST, therefore, clinicians must appreciate the potential contribution of contractile tissue.33 The term PST collectively encompasses the posterior capsule, posterioinferior glenohumeral ligament as well as the tendinous portion of the posterior rotator cuff and posterior deltoid musculature.14,22,24,32,33 Evidence for contractile tissue contribution may be gathered from the study by Hung et al33, where it was reported that muscle stiffness (change in passive tension per unit change in length) increased in the posterior deltoids, teres minor and infraspinatus when internally rotating the shoulder of patients with limited mobility, whereas muscle stiffness was reduced during external rotation.
Regardless of the soft tissues involved, a reliable and valid measurement technique is necessary for clinicians and researchers to recognize and quantify PST. Clinical measurements isolating PST have been described in the literature;10,17–19,21 however, there is no consensus as to the best method. A procedure that allows the examiner to consistently maintain scapular positioning independent of body morphology while providing an absolute measurement value would be clinically useful.
The inclinometric measurement procedure described and examined in this investigation provided optimal positioning for identifying PST and was developed based on in vivo and in vitro investigations of tissue tension.22–24 It also possessed good construct validity and good interrater reliability that was either comparable to or exceeded the reliability reported in previous studies. Moreover, the investigated procedure provides an absolute value that may be used to document change and be useful for intersubject comparison.
Although the sidelying measurement procedure has been previously described, this investigation is the first to report the interrater reliability, and MDC90 values of this method using inclinometry. Previous researchers have described alternate procedures for quantifying PST with fair to good reliability; however, there is disagreement on what constitutes the optimal position and measurement instrument for assessment. There is, however, a consensus that an optimal technique for quantifying PST requires isolation of true glenohumeral horizontal adduction independent of scapular protraction. Thus, optimal techniques should allow the examiner to maintain scapular retraction throughout the measurement and provide an accurate start position of retraction. Laudner et al17 used a supine method for quantifying PST and reported good intrarater and interrater reliability, ICC 5 0.93 and 0.91 respectively using digital inclinometry in asymptomatic participants. While the reliability values were good and the authors describe a clear reproducible methodology the supine position used may not permit a consistent start position of the scapula. If the scapula is not in full retraction the testers might underestimate PST. Another concern about the Laudner et al17 study, is that although SEM values were reported, the MDC was not reported thus for the reader it is unclear as to how much change would be needed on subsequent sessions to monitor change. Using the SEM value reported from the aforementioned study an MDC90 of 4 degrees was calculated. Lastly, digital inclinometry is costly, thus clinicians may not have this instrument at their disposal for routine use.
Lin and Yang18 used a supine method for quantifying PST among a population with documented shoulder stiffness and reported good inter-rater reliability, ICC 5 0.82 using a bubble inclinometer similar to the one used in the current investigation. Similar to the study by Laudner et al17 the MDC was not reported, however using the data provided the authors of the current study calculated an MDC of 7 degrees. The reliability values were considered good, however were lower than the values identified in the current investigation and in other investigations that used the side lying technique. A factor that may account for the difference is the limited ability to effectively stabilize the scapula in the supine position.
Myers et al10 compared the sidelying and supine methods of quantifying PST using a cohort of 15 healthy males. The interrater reliability of the supine method was reported as ICC 5 0.94, whereas the sidelying method was reported as 0.69. The authors report the use of an electromagnetic tracking device to monitor scapular position; however, measurements for the analysis of the supine method were obtained with a goniometer and sidelying method with a linear measurement method. The reliability of the supine assessment was comparable to values from the current study; however, the sidelying procedure described fell short of the reproducibility reported in the current study. One reason that might explain the higher reliability values in the current investigation was that the investigators in the Myers et al10 study did not use a method to ensure that the participant's trunk was directly perpendicular to the plinth in order to establish an accurate and reproducible starting position prior to taking the measurement. With regard to scapular position, the authors in the Myers et al10 study reported that the sidelying and supine positions produced a comparable ability to stabilize the scapula based on motion analysis with the electromagnetic tracking device. Although the authors report that the supine method is more reliable than the sidelying method, their sample of only 15 participants may be a limitation to the utility of this recommendation.
The sidelying method for quantifying PST has previously been investigated by Tyler et al19 with good interrater reliability, ICC 5 0.80. Advantages of the sidelying technique include a reproducible method of scapular stabilization, which isolates PST and provides a consistent, objectifiable start position. A measurement of the distance between the medial epicondyle and the plinth is thought to quantify PST; however, a disadvantage to this measurement method is that it does not produce a value that could be used for comparison between individuals or to establish normative values due to the varying anthropometric characteristics between individuals. The procedures described in this investigation are similar to the methods originally described by Tyler et al19 with the exception of using an inclinometer for angle measurements as compared to linear measurements. Inclinometry allowed the authors of the current study to obtain an absolute value for the angle of the humerus, which can be used for intersubject comparison. The interrater reliability of the sidelying procedure described in this investigation was good (ICC 5 0.90) and exceeded that of Tyler et al19 which may have been the result of the use of the inclinometer. The authors of the current investigation chose to not measure PST in the supine position as it is difficult to identify a consistent start position of the scapula. Moreover, the authors found it difficult to maintain a fully retracted scapular position during the measurement.
While reproducibility is imperative for any measurement, validity must be established to be certain that a measurement provides accurate information for clinical decision-making.28 Construct validity may be evaluated by determining how well a measurement relates to other tests of the same and different constructs. PST and IR are thought to measure the same construct,22,24 therefore these measurements would be expected to correlate highly or demonstrate convergence. Convergence alone is not a sufficient criterion to determine construct validity. It is also necessary to show that a construct may be differentiated from another construct, thus demonstrating the ability to be discriminant.28 Discriminant validity indicates that different results or poor correlations would be expected from measurements that assess a different construct or characteristic.28 ER should not be markedly affected by tension in the posterior capsuloligamentous or contractile tissues, thus a positive correlation would not be expected when compared to measurements of PST.24,33
Our choice of shoulder motions for the validity component of this investigation was based on both in vitro and in vivo evidence available in the literature. We used IR for our assessment of construct validity as osteokinematic impairments of IR at the glenohumeral joint have been associated with PST.7,11,13,18,19,22,23,33 Gerber et al22 performed surgical shortening of the posterior capsule and reported a significant reduction in internal rotation as a result confirming the association between posterior capsular tension and IR. Harryman et al23 noted a loss of shoulder flexion, horizontal adduction and internal rotation following in vitro tightening of the posterior capsule similar to the results of Gerber et al.22 Tyler et al7,8 indentified an association between PST and internal rotation loss using clinical measurements among subjects with impingement syndrome. Branch et al24 investigated the effect of capsular tension on shoulder rotation in vitro. The study results suggest a direct relationship between IR and tension in the posterior capsuloligamentous tissues, whereas a similar relationship was not found with ER.
The results of the current validity analysis suggest a strong relationship between PST and IR. The mean angle of IR and PST rounded to the nearest degree was 81° and 80° respectively with a statistically significant r 5 0.88. Conversely, there was no correlation between ER and PST (r 5 20.07). Our results were consistent with previous studies that documented a positive association between PST and decreased internal rotation.7,9,10,14,18,19,22,24,32,33 Tyler et al19 reported a good correlation between PST and IR using the sidelying PST measurement method among baseball pitchers and reported r 5 20.61. An inverse correlation was reported based upon their use of a linear measurement whereas a loss of internal rotation correlated with a greater distance measured from the medial epicondyle to the plinth. Laudner et al17 reported a good correlation between IR and PST (r 5 0.72) among baseball pitchers. Lin and Yang18 compared PST to both IR and ER in a symptomatic cohort and reported a moderate to good relationship for IR (r 5 0.69), whereas ER had little or no relationship (r 5 0.25). Hung et al33 described measurements of muscle stiffness using a myotonometer in response to IR and ER among participants with clinically reduced ROM and identified increased stiffness (change in passive tension per unit change in length) of the posterior musculature in response to IR lending support to the possible contribution of contractile tissue to PST.
In regards to measurement error and change scores the MDC has not previously been reported for PST tests documented in the literature, thus, clinicians and researchers previously interpreting change may have relied on individual decisions that did not take into account variability and error. The MDC90 values reported in this investigation indicate that a change greater than or equal to 9° is required over treatment sessions or in research trials to be 90% certain that the change is not due to subject variability or measurement error. The MDC as reported in this investigation is the smallest amount of change that can be considered above the threshold of error,28 however, one must not make the assumption that this change has reached the threshold of clinically meaningful improvement. When interpreting change scores it should be recognized that the MDC is not the same as the minimum clinically important difference (MCID).28 The MCID is the amount of change that is clinically meaningful and is typically associated with an external criterion that indicates when meaningful change has occurred.28 The authors of this manuscript did not calculate the MCID, thus it is uncertain as to the degree of change that would be considered clinically meaningful.
Limitations and Future Research
When considering the results of this study one must recognize potential limitations. This study used only healthy-young asymptomatic participants, thus the results may not correlate with a symptomatic cohort or among individuals of different age groups. In regards to procedures for measuring PST, a 10-second rest period between repetitions one and two for each rater may not be sufficient to avoid rater bias. We attempted to control for this by using a trained assistant who recorded measurements and by blinding raters to the results. Additionally, a limitation of the procedures includes the use of AROM for validating the PST measurement as AROM may be limited as a result of soft tissue restrictions as well as neuromuscular impairments. Although our PST measurement was passive we did not add overpressure thus eliminating the potential for a stretching effect. Moreover, we used healthy-asymptomatic controls with no neuromuscular impairments. Lastly, one must be cautious in their interpretation of the MDC values reported in this investigation as they are not indicative of clinically meaningful change. The MCID would be necessary to determine whether or not a clinically meaningful change occurs in patients or subjects. Future investigations are warranted in order to study this technique on a symptomatic population and on populations of different age ranges, in order to determine if the results are generalizeable to the population.
CONCLUSION
Various procedures and instruments have been described in the literature for quantifying PST, thus it is difficult to state that the method described and investigated in this paper is superior to others. This investigation presents a reproducible and valid measurement protocol for quantifying PST using an inclinometer. The inclinometric procedure outlined in this investigation had a reliability coefficient of 0.90 which is the threshold recommended for tests to be useful in making clinical decisions28 and is a suitable alternative to linear measurements as it allows for intersubject comparison. Clinicians and researchers should consider the MDC values presented (9°) when interpreting change values during subsequent measurement sessions to be certain that the change is not due to intertrial variability or measurement error.
ACKNOWLEDGEMENTS
The authors would like to thank Nova Southeastern University, Department of Physical Therapy for providing facilities for data collection.
REFERENCES
- 1.Luime JJ, Koes BW, Hendriksen IJ, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33(2):73–81 [DOI] [PubMed] [Google Scholar]
- 2.Kolber M, Beekhuizen K, Cheng M, Hellman M. Shoulder Injuries Attributed to Resistance Training: A Brief Review. J Strength Cond Res. 2010;24(6):1696–1704 [DOI] [PubMed] [Google Scholar]
- 3.Di Fabio R, Boissonnault W. Physical therapy and health-related outcomes for pain with common orthopaedic diagnosis. J Orthop Phys Ther. 1998;27:219–230 [DOI] [PubMed] [Google Scholar]
- 4.Kerr Z, Collins C, Comstock R. Epidemiology of weight-training-related injuries presenting to United States emergency departments, 1990 to 2007. Am J Sports Med. 2010;38(4):765–771 [DOI] [PubMed] [Google Scholar]
- 5.Goertzen M, Schoppe K, Lange G, Schulitz KP. Injuries and damage caused by excess stress in bodybuilding and power lifting. Sportverletz Sportschaden. 1989;3:32–36 [DOI] [PubMed] [Google Scholar]
- 6.Bonza JE, Fields SK, Yard EE, Comstock RD. Shoulder Injuries Among United States High School Athletes During the 2005–2006 and 2006–2007 School Years. J Athl Train. 2009;44(1):76–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tyler TF, Nicholas SJ, Roy T, Gleim GW. Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. Am J Sports Med. Sep-Oct 2000;28(5):668–673 [DOI] [PubMed] [Google Scholar]
- 8.Tyler TF, Nicholas SJ, Lee SJ, Mullaney M, McHugh MP. Correction of posterior Shoulder Tightness is Associated With Symptom Resolution in Patients With Internal Impingement. Am J Sports Med. 2010;38(1):114–119 [DOI] [PubMed] [Google Scholar]
- 9.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathological internal impingement. Am J Sports Med. 2006;34:385–391 [DOI] [PubMed] [Google Scholar]
- 10.Myers JB, Oyama S, Wassinger CA, et al. Reliability, Precision, Accuracy, and Validity of Posterior Shoulder Tightness Assessment in Overhead Athletes. Am J Sports Med. 2007;35(11):1922–1930 [DOI] [PubMed] [Google Scholar]
- 11.Burkhart S, Morgan C, Kibler W. The disabled throwing shoulder: spectrum of pathology. Part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404–420 [DOI] [PubMed] [Google Scholar]
- 12.Burkhart S, Morgan C, Kibler W. The disabled thowing shoulder: spectrum of pathology. Part II: evaluation and treatment of SLAP lesions in throwers. Arthroscopy. 2003;19(5):531–539 [DOI] [PubMed] [Google Scholar]
- 13.Burkhart S, Morgan C, Kibler W. Shoulder injuries in overhead athletes: The “dead arm” revisited. Clin Sports Med. 2000;19:125–158 [DOI] [PubMed] [Google Scholar]
- 14.Ticker J, Beim G, JJ W. Recognition and treatment of refractory posterior capsular contracture of the shoulder. Arthroscopy. 2000;16:27–34 [DOI] [PubMed] [Google Scholar]
- 15.Kolber MJ, Beekhuizen K, Cheng MS, Hellman M. Shoulder joint and muscle characteristics in the recreational weight training population. J Strength Cond Res. 2009;23:148–157 [DOI] [PubMed] [Google Scholar]
- 16.Kolber MJ, Corrao M. Shoulder joint and muscle characteristics amoung healthy female recreational weight training participants. J Strength Cond Res. (In press). [DOI] [PubMed] [Google Scholar]
- 17.Laudner K, Stanek J, Meister K. Assessing Posterior Shoulder Contracture: The Reliability and Validity of Measuring Glenohumeral Joint Horizontal J Athl Train. 2006;41(4):375–380 [PMC free article] [PubMed] [Google Scholar]
- 18.Lin JJ, Yang JL. Reliability and validity of shoulder tightness measurement in patients with stiff shoulders. Man Ther. 2006;11:146–152 [DOI] [PubMed] [Google Scholar]
- 19.Tyler TF, Roy T, Nicholas SJ, Gleim GW. Reliability and validity of a new method of measuring posterior shoulder tightness. J Orthop Sports Phys Ther. May 1999;29(5):262–269; discussion 270–264 [DOI] [PubMed] [Google Scholar]
- 20.Warner JJ, Micheli LJ, Arslanian LE, Kennedy J, Kennedy R. Patterns of flexibility, laxity, and strength in normal shoulders and shoulders with instability and impingement. Am J Sports Med. Jul-Aug 1990;18(4):366–375 [DOI] [PubMed] [Google Scholar]
- 21.Kolber MJ, Saltzman S, Beekhuizen K, Cheng MS. The reliability and minimal detectable change of inclinometric shoulder mobility measurements. Physiother Theory Pract. 2009;25:572–581 [DOI] [PubMed] [Google Scholar]
- 22.Gerber C, Werner C, Macy J, Jacob H, RW N. Effect of selective capsulorrhaphy on the passive range of motion of the glenohumeral joint. J Bone Joint Surg Am. 2003;85:48–55 [DOI] [PubMed] [Google Scholar]
- 23.Harryman DT, 2nd, Sidles JA, Clark JM, McQuade KJ, Gibb TD, Matsen FA., 3rd Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. October 1990;72(9):1334–1343 [PubMed] [Google Scholar]
- 24.Branch TP, Lawton RL, Iobst CA, Hutton WC. The role of glenohumeral capsular ligaments in internal and external rotation of the humerus. Am J Sports Med. 1995;23(5):632–638 [DOI] [PubMed] [Google Scholar]
- 25.Clarkson HM, Gilewich GB. Musculoskeletal Assessment. Joint Range of Motion and Manual Muscle Strength. Baltimore, MD: Williams & Wilkins; 1989 [Google Scholar]
- 26.Wilk KE, Reinold MM, Macrina LC, et al. Glenohumeral Internal Rotation Measurements Differ Depending on Stabilization Techniques. Sports Health: A Multidisciplinary Approach. Mar-Apr 2009. 2009;1(2):131–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Awan R, Smith J, Boon AJ. Measuring shoulder internal rotation range of motion: a comparison of 3 techniques. Arch Phys Med Rehabil. September 2002;83(9):1229–1234 [DOI] [PubMed] [Google Scholar]
- 28.Portney L, Watkins M. Foundations of Clinical Research: Applications to Practice. 3rd ed. Upper Saddle River, New Jersey: Pearson Prentice Hall; 2009 [Google Scholar]
- 29.Shrout P, Fleiss J. Intraclass correlation: Uses in assessing rater reliability. Psychol Bull. 1979;86:420–428 [DOI] [PubMed] [Google Scholar]
- 30.Weir J. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19:231–240 [DOI] [PubMed] [Google Scholar]
- 31.Haley S, Fragala-Pinkham M. Interpreting change scores of tests and measures used in physical therapy Phys Ther. 2006;86:735–743 [PubMed] [Google Scholar]
- 32.Bach GH, Goldberg BA. Posterior Capsular Contracture of the Shoulder. J Am Orthop Surg. 2006;14(5):265–277 [DOI] [PubMed] [Google Scholar]
- 33.Hung CJ, Hsieh CL, Yang PL, Lin JJ. Relationships between posterior shoulder muscle stiffness and rotation in patients with stiff shoulder. J Rehabil Med. 2010;42(3):216–220 [DOI] [PubMed] [Google Scholar]