Abstract
A number of sporting and daily activities involve rotation of the spine. The ability to quantify motion of the spine in a clinical setting usually relies on the use of a device to measure angles (goniometer or inclinometer) or visual assessment. Standardized measurement criteria exist for measuring rotation at the cervical and lumbar spine. Little has been written regarding established methods for measuring thoracic spine rotation. Thoracic rotation may be measured in a seated position, half-kneeling position, or quadruped position. Steps should be taken to minimize motion of surrounding segments such as the shoulder and hips, which may improve measurement accuracy. Key words: inclinometer, goniometer, range of motion
INTRODUCTION
Adequate spine rotation is essential for sporting tasks such as golf, throwing sports, tennis, and rowing. Although movement of the vertebrae may be more accurately measured using diagnostic imaging, it is not a plausible clinical method due to cost and potential radiation exposure. A variety of methods have been proposed to measure rotation of the spine,1–8 but there is no consensus regarding a clinical gold standard of spinal motion measurements. Clinical measurements of spine motion may be quantified with a goniometer, inclinometer, or visual assessment. Clinically relevant measurement methods for cervical spine2 and lumbar spine rotation7 have been established and have been shown to have good reliability. Little has been written on standardized assessment of thoracic spine rotation.
In this clinical commentary, we describe five suggested methods of measuring thoracic rotation. Each of the methods attempts to limit or restrain movement from adjacent joints such as the lumbar spine and hips. Variations of these methods have been briefly described in previous literature3–6,9,10 but no manuscript has focused on standardized measurement criteria. Since these methods may be used in athletic performance and rehabilitation settings, standardized criteria for testing should be established. The use of standardized criteria should allow future investigation into the reliability of these techniques.
METHODS
Seated Rotation Technique
The individual is in a seated position with their hips and knees flexed to 90° and their trunk in an upright neutral posture (not flexed, extended, side bent, or rotated) (Figure 1a). A small ball (volleyball, soccer ball) is placed between the knees and the individual is asked to maintain slight pressure on the ball by adducting the hips. The ball is used in an attempt to reduce the contribution of the lower body on spine rotation. A PVC dowel may be placed across the chest with the arms crossed over the bar (Figure 1a). Alternatively, PVC dowel may be placed across the back (Figure 1b), at approximately the inferior border of the scapulae. The individual is asked to place the palmar aspect of their hands on their stomach (interlocking fingers is not necessary). The bar in back position is thought to reduce the contribution from the shoulder joints on spine rotation.
Figure 1.
Seated rotation technique. Hips and knees are at 90°, trunk is upright and neutral, and lower body motion is reduced with a ball held between the knees. a) bar in front position requires the individual to cross their arms across their chest b) bar behind the back position requires the individual to place the palmar aspect of their hands on their stomach, fingers do not need to interlock.
Regardless of bar position (bar front or back), a goniometer is aligned parallel to the ground, at the midpoint between the T1-T2 spinous processes, while using the spine of the scapula as a reference point during rotation (Figure 2). The stationary arm is pointed away from the side of rotation and remains in line with the starting position. The individual is instructed to maximally rotate to one side while the clinician follows this motion with the moving arm of the goniometer. Once the individual reaches end range of motion, the angle of the goniometer is noted.
Figure 2.
Goniometer alignment. Goniometer is aligned parallel to the ground, between the T1-T2 spinous processes, using the spine of the scapula as a reference point. This figure depicts left rotation. The stationary arm is pointed away from the side of rotation (to the right) and remains in line with the starting position. The moving arm follows the spine of the scapula.
Half-Kneeling Rotation Technique
The half-kneeling rotation technique utilizes a lunge position, with one foot on the ground and the contralateral knee and toe in contact with the ground (Figure 3a). This position is also thought to limit the contribution of the lumbar spine and hips, but perhaps not to the same degree as the seated rotation position with bilateral hip flexion. Additionally this position requires a component of lower extremity stability to remain upright. The neutral position of the trunk is the same as the seated rotation technique. PVC dowel position, goniometer alignment, and measurement technique are identical to the seated rotation test. The individual is asked to rotate toward the forward leg (i.e. right leg forward, rotation to the right) (Figure 3b). Once the individual reaches end range of motion, the angle of the goniometer is noted.
Figure 3.
Half-kneeling technique. a) Trunk is upright and neutral and the forward (right) foot is in line with the knee. b) The individual is asked to rotate toward the forward leg (right leg forward, rotation to the right).
Lumbar-Locked Rotation Technique
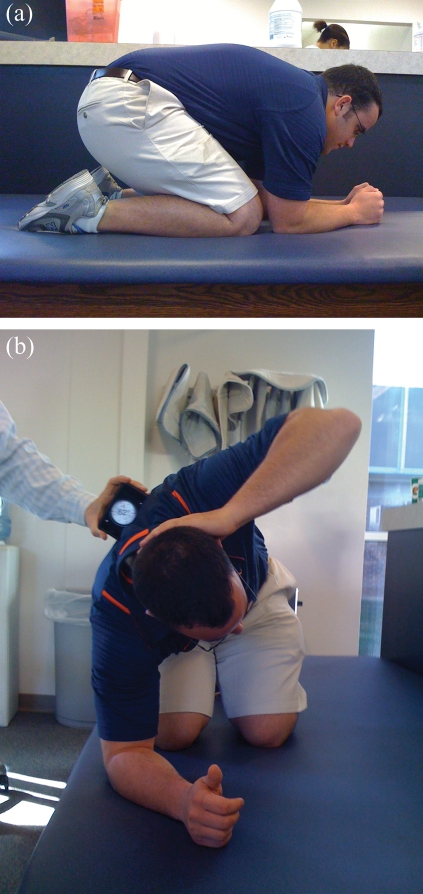
The individual is in a hands and knees position, sitting on heels, while maintaining upper extremity support with the elbows and forearms (Figure 4a). This position is similar to the “prayer position” used in the performance of yoga. Flexion of the hips and lumbar spine is thought to reduce the contribution of the hip, pelvis, and lumbar spine motion during thoracic rotation. An inclinometer (bubble or digital) is positioned between the scapular spines at the T1-T2 level. The individual is instructed to place one hand on the posterior aspect of their neck and rotate the thoracic spine to that side while maintaining the kneeling position (Figure 4b). Once the individual reaches end range, the angle of the inclinometer is recorded.
Figure 4.
Lumbar-locked rotation technique. a) Shoulders and elbows are at 90° while the individual sits back on heels as far as possible. b) Individual places one hand behind head (left), while opposite (right) forearm remains in contact with the ground. Individual is instructed to rotate (left rotation) as far as possible with the head remaining forward relative to the torso.
Common Substitution Patterns
Attempts should be made in all positions to minimize motion of surrounding joints. In the seated rotation testing position individuals may attempt to increase available motion by hiking one hip, not maintaining equal weight bearing on the ischial tuberosities, side bending at the lumbar spine, or internally rotating the opposite hip. This may be recognized by movement of the ball placed between the legs, shifting of the hips, or feet that do not remain flat on the ground. In the half-kneeling position the individual may adduct the hip of the forward leg or attempt to side bend at the lumbar spine to gain additional motion. Side bending of the spine may be recognized if the PVC dowel does not remain parallel to the ground. For both seated rotation and half-kneeling positions, the bar in back is thought to minimize the contribution of the shoulder joints. During the bar in front position shoulder protraction and retraction may contribute to the increased rotation motion relative to the bar in back position. Common substitution patterns during the lumbar-locked position include extension of the trunk, lateral shift of the hips, and shoulder horizontal abduction. This may be recognized if the elbow or forearm does not maintain contact with the ground, a noticeable weight shift occurs at the hips, or if the elbow does not maintain an in line orientation with the spine of the scapula and clavicle.
CONCLUSION
For all rotation measurements it is important to monitor compensatory motions. The use of a PVC dowel behind the back as well as the use of a ball in the seated position are both thought to minimize the contribution of the shoulders and hips on thoracic rotation motion. Understanding and being able to identify common compensatory strategies utilized to gain additional motion is also important. Most individuals will compensate by not maintaining equal weight distribution through the lower extremity. Minimizing motion of surrounding regions may improve measurement accuracy. It should be noted that the reliability for these techniques has not been established. Without reliable measurement techniques, little confidence exists in the results of measurements and intervention effectiveness cannot be evaluated. Future research should determine if these clinical techniques are reliable and determine the measurement error associated with each technique. These techniques do provide clinicians and researchers with specific measurement criteria for clinically relevant techniques which can be used with little equipment and training.
REFERENCES
- 1. Malmström EM, Karlberg M, Melander A, Magnusson M. Zebris versus Myrin: a comparative study between a three-dimensional ultrasound movement analysis and an inclinometer/compass method: intradevice reliability, concurrent validity, intertester comparison, intratester reliability, and intraindividual variability. Spine (Phila Pa 1976). 2003;28:E433–440 [DOI] [PubMed] [Google Scholar]
- 2. Youdas JW, Carey JR, Garrett TR. Reliability of measurements of cervical spine range of motion- Comparision of three methods. Phys Ther. 1991;71:98–104 [DOI] [PubMed] [Google Scholar]
- 3. Hoogenboom BJ, Voight ML, Cook G, Gill L. Using rolling to develop neuromuscular control and coordination of the core and extremities of athletes. N Am J Sports Phys Ther. 2009;4:70–82 [PMC free article] [PubMed] [Google Scholar]
- 4. Kiesel K, Burton L, Cook G. Mobility screening for the core. Athl Ther Today. 2004;9:38–41 [Google Scholar]
- 5. Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry. Philadelphia: FA Davis Company; 1995 [Google Scholar]
- 6. Klein AB, Snyder-Mackler L, Roy SH, DeLuca CJ. Comparison of spinal mobility and isometric trunk extensor forces with electromyographic spectral analysis in identifying low back pain. Phys Ther. 1991;71:445–454 [DOI] [PubMed] [Google Scholar]
- 7. Olson KA, Goehring MT. Intra and inter-rater reliability of a goniometric lower trunk rotation measurement J Back Musculoskelet Rehabil. 2009;22(3):157–164 [DOI] [PubMed] [Google Scholar]
- 8. Magee DJ. Orthopedic Physical Assessment. 4th ed. Philadelphia: Saunders; 2002 [Google Scholar]
- 9. Willems JM, Jull GA, Ng J-F. An in vivo study of the primary and coupled rotations of the thoracic spine. Clin Biomech. 1996;11(6):311–316 [DOI] [PubMed] [Google Scholar]
- 10. Schenkman M, Laub KC, Kuchibhatla M, Ray L, Shinberg M. Measures of shoulder protraction and thoracolumbar rotation. J Orthop Sports Phys Ther. 1997;25(5):329–335 [DOI] [PubMed] [Google Scholar]