Abstract
Frozen shoulder syndrome, clinically known as adhesive capsulitis, is a painful and debilitating condition affecting up to 5% of the population. Adhesive capsulitis is considered fibrosis of the glenohumeral joint capsule with a chronic inflammatory response. Patients experience pain, limited range of motion, and disability generally lasting anywhere from 1 to 24 months. The purpose of this clinical suggestion is to review the pathophysiolgy of adhesive capsulitis and discuss physical therapy interventions which are supported by evidence, thereby enhancing evidence-based practice.
Keywords: Adhesive capsulitis, physical therapy interventions
The “frozen shoulder” diagnosis has been used for many years in describing shoulder pain and limited motion, and was originally thought to be “periarthritis.” Nevasier was the first to identify the pathology through histological and surgical examination of frozen shoulder patients.1 He concluded that frozen shoulder was not periarthritis, but a “thickening and contraction of the capsule which becomes adherent to the humeral head” that he termed, “adhesive capsulitis.”1 Adhesive capsulitis is characterized by pain, stiffness, and limited function of the glenohumeral joint, which adversely affects the entire upper extremity. Patients typically describe onset of shoulder pain followed by a loss of motion.2 The most common limitations in range of motion are flexion, abduction, and external rotation. Approximately 70% of frozen shoulder patients are women;3 however, males with frozen shoulder are at greater risk for longer recovery and greater disability3–4. Although the exact pathophysiologic cause of this pathology remains elusive, there are two types identified in the literature: idiopathic and secondary adhesive capsulitis.5
Idiopathic (“primary”) adhesive capsulitis occurs spontaneously without a specific precipitating event. Primary adhesive capsulitis results from a chronic inflammatory response with fibroblastic proliferation, which may actually be an abnormal response from the immune system.6 Secondary adhesive ¬capsulitis occurs after a shoulder injury or surgery, or may be associated with another condition such as diabetes, rotator cuff injury, cerebrovascular accident (CVA) or cardiovascular disease, which may prolong recovery and limit outcomes.7 In a profile study of 32 patients with adhesive capsulitis, heart disease and diabetes were more prevalent in those suffering from adhesive capsulitis than a control group.2 In a 1986 study, 19% of older diabetic patients had adhesive capsulitis;8 however, recent estimates place the incidence as high as 71% when patients with pre-diabetes (metabolic syndrome) are included.9 Both Type I and Type II diabetics are susceptible to frozen shoulder;10 unfortunately, diabetics have worse functional outcomes as measured by disability and quality of life questionnaires compared to non-diabetics with frozen shoulder.4 Frozen shoulder is also a common complication following stroke, occurring in 25% of patients within 6 months.11
Frozen shoulder may also be confused with other clinical syndromes; therefore, it is important to have an accurate differential diagnosis to rule out other pathologies. For example, chronic regional pain syndrome (CRPS, formerly known as reflex sympathetic dystrophy) may cause severe limitations in shoulder range of motion similar to those seen with a frozen shoulder; however, CRPS is also associated with swelling and other trophic skin changes in the extremity. Some have speculated, however, that adhesive capsulitis is in-fact a type of “sympathetic dystrophy,” based on decreases in bone mineral density seen in patients with frozen shoulder.12 Shoulder girdle tumors, although rare, may also mimic the symptoms of frozen shoulder.13
Three stages of frozen shoulder have been described in the literature: painful stage, stiffness or “frozen” stage, and recovery or “thawing” stage, with the average length of symptoms lasting 30 months.14 The average range of motion in frozen-stage shoulder patients is 98° of abduction, 117° of flexion, 33° external rotation and 18° of internal rotation with the shoulder abducted to 90°15. While the “stiffness stage” is the longest of the stages, adhesive capsulitis is thought to be reversible in the acute pain stage16. In addition to limited range of motion, shoulder complex muscle imbalances lead to altered shoulder motion. The upper trapezius tends to be more activated than the lower trapezius, creating an imbalance of the scapular stabilizers17 leading to increased elevation and upward rotation of the scapula during elevation of the glenohumeral joint in both the frontal and sagittal planes.15,18 Patients with adhesive capsulitis have higher EMG ratios of upper trapezius to lower trapezius during arm elevation when compared to asymptomatic subjects, indicating a muscular imbalance.17
Patients with frozen shoulder exhibit significant deficits in shoulder kinematics, including increased elevation and upward scapular rotation.15,19 Eventually, patients with adhesive capsulitis develop the characteristic “shrug sign” during glenohumeral joint elevation, where the scapula migrates upward prior to 60 degrees of abduction. This indicates compensation due to lack of capsular extensibility as well as a change in the central nervous system motor patterning due to maladaptive movement. Patients with adhesive capsulitis may also develop adaptive postural deviations such as anterior shoulders or increased thoracic kyphosis as the function of the shoulder complex remains limited and painful.
Adhesive capsulitis is generally related to a shortening and fibrosis of the joint capsule (ligaments) surrounding the shoulder joint. Nevasier1 was among the first to report thickening and contraction of the shoulder capsule as well as inflammatory changes through histologic analysis. The contracture of the shoulder ligaments actually decreases the volume of the capsule, thus limiting range of motion. It is likely that limitations in range of motion and the pain associated with frozen shoulder are not only related to capsular and ligamentous tightness, but also fascial restrictions, muscular tightness, and trigger points within the muscles. Physical therapists can address impairments and limitations associated each of these contributors to the pathology of adhesive capsultis with a variety of treatment methods.
PHYSICAL THERAPY INTERVENTIONS
Levine and colleagues20 showed a 90% success rate with non-operative treatment (oral NSAIDs and standardized physical therapy) over an average of 4 months. As little as 4 weeks of targeted intervention can improve pain and strength in frozen shoulder patients21–22. It has been suggested23 that ‘gentle’ therapy (painfree pendulum and active exercises) is better than ‘intensive’ therapy (passive stretching and manipulation up to and beyond the pain threshold). Unfortunately, frozen shoulder patients often maintain some deficiencies in range of motion even after ‘successful’ treatment.4 In a 15 year follow-up, Farrell24 reported forward elevation range of motion of only 168° and external rotation of 67°.
Jewell and colleagues25 suggested in their meta-¬analysis of physical therapy interventions for frozen shoulder syndrome that joint mobilization and exercise were the most effective interventions. Non-aggressive physical therapy interventions are generally more effective than aggressive or intensive interventions23,26. Physical therapy interventions used with patients with frozen shoulder frequently include modalities, manual techniques, and therapeutic exercise. While some of these interventions have been studied in patients with adhesive capsulitis, it is important to remember that not all clinical interventions have evidence to support their use in specific patient populations. Recall that evidence-based practice is best defined as the use of the best evidence available along with clinical experience while taking into consideration the unique needs of an individual patient.
Modalities.
The rationale for using modalities in patients with adhesive capsulitis includes pain relief and affecting scar tissue (collagen). However, the use of modalities such as ultrasound, massage, iontophoresis, and phonophoresis has not been proven to be beneficial in treatment of patients with adhesive capsulitis.25,27 Interestingly, transcutaneous electrical stimulation (TENS) has been shown to significantly increase range of motion more than heat combined with exercise and manipulation.28 Research also suggests that low-power laser therapy is more effective than a placebo for treatment of patients with adhesive capsulitis.29–30 Recently, deep heating through diathermy combined with stretching was shown to be more effective than superficial heating for treating frozen shoulder patients.31
Passive Motion.
Because adhesive capsulitis involves fibrotic changes to the capsuloligamentous structures, continuous passive motion or dynamic splinting are thought to help elongate collagen fibers. Continuous passive motion (CPM) was recently compared with conventional PT in 57 patients with adhesive capsulitis.32 Both groups improved after 4 weeks of treatment; while there was no significant difference between the groups, the CPM patients had greater reduction in pain levels. Dynamic splinting was also recently evaluated in patients with Stage 2 (“frozen stage”) adhesive capsulitis.33 The authors, Gaspar and Willis, noted better outcomes when physical therapy was combined with the Dynasplint® protocol, although there was no statistically significant difference between standard physical therapy or the Dynasplint alone. The concept of total end-range time (TERT) has also been described in the treatment of patients with adhesive capsulitis, suggesting maintenance of a stretch in the maximally lengthened range of motion for a total of 60 minutes per day34–35.
Manual Techniques.
As stated previously, joint mobilization is an effective intervention for adhesive capsulitis. Several studies have demonstrated the effectiveness of joint mobilization in adhesive capsulitis patients.25,36–37 In particular, posterior glide mobilization was determined to be more effective than anterior glide for improving external rotation range of motion in patients with adhesive capsulitis36 Johnson and colleagues randomly assigned 20 consecutive adhesive capsulitis patients to physical therapy intervention including grade III stretch mobilization with distraction at end range of abduction and external rotation using either an anterior or posterior directed linear translation. After 3 sessions, the posterior mobilization group had significantly improved their external rotation range of motion by 31 degrees versus only 3 degrees in the anterior mobilization group. In addition, high-grade joint mobilization techniques were more effective than low-grade mobilization in improving glenohumeral mobility and reducing disability in a recent randomized controlled trial of treatment of patients with adhesive capsulitis.37
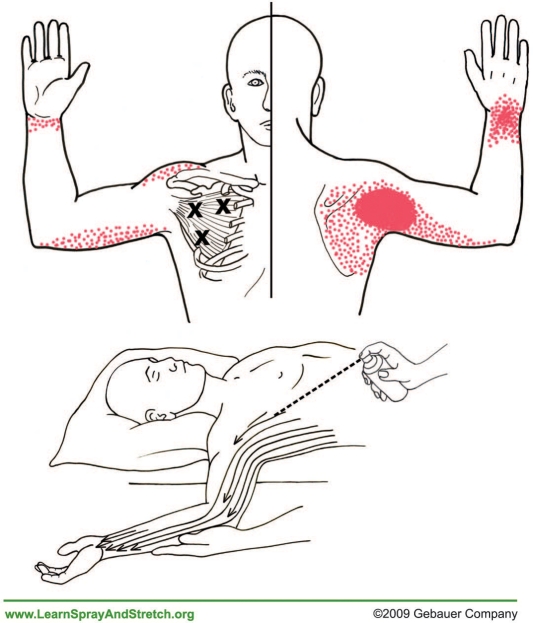
As discussed earlier, myofascial trigger points, focal areas of increased tension within a muscle, may be present in the musculature around the shoulder complex in patients with adhesive capsulitis.38 In Travel and Simons' classic textbook, the authors describe how the subscapularis muscle in particular is referred to as the “Frozen Shoulder” muscle because trigger points in the subscapularis cause limitations in shoulder elevation and external rotation.39 The Spray and Stretch® technique for the subscapularis and latissimus dorsi muscle may be effective at reducing trigger point irritation, pain, and helping to gradually lengthen tight muscles.40 (Figure 1)
Figure 1:
Spray and Stretch® technique for treatment of the subscapularis. (Copyright, Gebauer Company, used with permission.)
Soft Tissue Mobilization.
Soft tissue mobilization and deep friction massage may benefit adhesive capsulitis patients. Deep friction massage using the Cyriax method was shown to be superior to superficial heat and diathermy in treatment of patients with adhesive capsulitis.41 Recently, instrument-assisted soft tissue mobilization (IASTM) as used in such interventions as Graston Technique®, ASTYM®, or guasha has become increasingly popular in physical therapy practice. IASTM reportedly provides strong afferent stimulation and reorganization of collagen, as well as in increase in microcirculation. The inferior glenohumeral capsule and pectoral fascia are often restricted, as well as the insertion of the latissimus dorsi and subscapularis. IASTM may help improve fibroblast proliferation and promote normal collagen alignment,42–43 although no studies have evaluated outcomes of the use of IASTM on patients with adhesive capsulitis. (Figure 2)
Figure 2:
Instrument-assisted Graston Technique® for treatment of the pectoral fascia. (Used with permission, Graston Technique®).
Therapeutic Exercise.
Probably the most com¬monly prescribed therapeutic exercises for adhesive capsulitis are active-assisted range of motion (AAROM) exercises. These typically involve the patient using the uninvolved arm, or using equipment such as rope-and-pulley, wand/T-bar, or exercise balls. Generally, these exercises are performed for flexion, abduction and external rotation ranges of motion which are frequently the most limited. Griggs and colleagues found that physical therapy including 4 self-stretches (passive flexion, horizontal adduction, internal rotation behind the back with the unaffected arm, and external rotation at 0° using a cane) performed at least twice a day produced a satisfactory outcome in 90 percent of stage 2 adhesive capsulitis patients.4 These patients significantly improved in pain, range of motion, and shoulder function; however, the study did not compare the intervention to other types of treatment. Despite this limitation, the authors suggested that more aggressive treatments such as manipulation are rarely necessary.
Resistive exercises typically include strengthening of the scapular stabilizers and rotator cuff, when range of motion has progressed enough for strengthening to be an appropriate intervention. Muscles prone to weakness in a variety of shoulder dysfunctions include the lower trapezius, serratus anterior, and infraspinatus. Patients with adhesive capsulitis have significantly weaker lower trapezius muscles compared to asymptomatic controls.17 It is important that treating therapists facilitate normal movement patterns rather than allowing pathological adaptive patterns to prevail during movement for the sake of completing an exercise. For example, if a patient demonstrates a ‘shrug sign’ while performing resisted abduction, the exercise should be stopped and modified with less resistance or be attempted in an altered position, while cuing of the patient for proper movement patterns. The “Shoulder Sling” exercise can be used to help re-train the initial setting phase of the rotator cuff when initiating abduction. (Figure 3) The Shoulder Sling exercise for a “rotator cuff set” is considered analogous to a “quad set” exercise in the lower extremity. The elastic band creates an “upward and inward” vector of resistance that the patient must push against in a “down and out” vector. This movement simulates the initiation of abduction as well as the depression and stabilization functions of the rotator cuff, which occur prior to and during abduction. Anecdotally, this exercise helps reduce early activation of the upper trapezius during abduction in patients demonstrating a shrug sign.
Figure 3:
“Shoulder Sling” exercise designed to facilitate “setting” of the rotator cuff. Place an elastic loop under the elbow and around the neck and opposite shoulder. Simultaneously depress your shoulder and initiate abduction against the band resistance, pushing your elbow in a “down and out” motion. Do not actually move the arm away from the body. (Used with permission, The Hygenic Corporation).
Rigid and Kinesiological Taping.
Although no studies have been published on the efficacy of taping (such as rigid strapping tape or kinesiological taping [KT]) with patients who have adhesive capsulitis, taping may be helpful in reducing pain and providing tactile cues through proprioceptive and afferent mechanisms. The mechanisms and efficacy of taping applications remain unclear. Because adhesive capsulitis patients often exhibit poor posture and scapular mechanics, KT may provide postural cues and assist with promoting proper scapular motion. (Figure 4)
Figure 4:
Kinesiological Taping Technique: Postural Spider (Used with permission, SpiderTech).
Additional Interventions.
Non-operative treatment may also include injections directly into the glenohumeral joint joint. These injections often contain both a corticosteroid and an anesthetic, and can also include saline to distend the capsule, stretching the fibers. When saline is used to distend the capsule, it is known as “distension arthrography” or “hydroplasty”. Corticosteroid injections have been shown to be as effective as exercise for treating frozen shoulder,45–47 particularly when provided in the early stages of the pathology.16 In their systematic review, Blanchard et al. suggested that corticosteroid injections have a greater effect when compared to physical therapy when utilized within the first 6 weeks of treatment, although these differences diminished over time.48 They noted a moderate effect of corticosteroid injections on pain, external rotation ROM, and disability at 6 weeks, and only small effects after 12 weeks. Distension arthrography is often successfully combined with physical therapy.49–51 In fact, therapeutic exercise, including physical therapy, is more effective when combined with a corticosteroid injection.52–54
Adhesive capsulitis patients not responding to physical therapy are often treated with manipulation under anesthesia (MUA), where the shoulder is forcefully moved by the physician into the full ranges of motion, breaking the adhesions located within of the shoulder capsule. In addition to increased risk of complications from anesthesia, MUA can cause severe damage including labral tears, tendon tears, fractures, and ruptures of the shoulder ligaments.55 Most recently, steroid injections with distention arthrography have been shown to be as effective as MUA and are therefore the recommended course of treatment because of the risks associated with MUA.56
In conclusion, adhesive capsulitis is a challenging condition for both the physical therapist and patient. It is important for clinicians to make an accurate diagnosis and assessment in order to best choose their interventions. By understanding the published evidence related to the rehabilitation of patients with adhesive capsulitis, both therapists and patients will benefit from an integrated, multi-faceted, evidence-based approach to intervention.
REFERENCES
- 1. Nevaiser T. J. Adhesive capsulitis of the shoulder: a study of the pathological findings in periarthritis of the shoulder. J Bone Joint Surg 1945; 27:211–222 [Google Scholar]
- 2. Boyle-Walker K. L., Gabard D. L., Bietsch E., Masek-VanArsdale D. M., Robinson B. L. A profile of patients with adhesive capsulitis. J Hand Ther 1997; 10:222–228 [DOI] [PubMed] [Google Scholar]
- 3. Sheridan M. A., Hannafin J. A. Upper extremity: emphasis on frozen shoulder. Orthop Clin North Am. 2006; 37:531–539 [DOI] [PubMed] [Google Scholar]
- 4. Griggs S. M., Ahn A., Green A. Idiopathic adhesive capsulitis. A prospective functional outcome study of nonoperative treatment. J Bone Joint Surg Am. 2000;82-A:1398–1407 [PubMed] [Google Scholar]
- 5. Lundberg B. J. The frozen shoulder. Clinical and radiographical observations. The effect of manipulation under general anesthesia. Structure and glycosaminoglycan content of the joint capsule. Local bone metabolism. Acta Orthop Scand Suppl. 1969; 119:1–59 [PubMed] [Google Scholar]
- 6. Hand G. C., Athanasou N. A., Matthews T., Carr A. J. The pathology of frozen shoulder. J Bone Joint Surg Br. 2007; 89:928–932 [DOI] [PubMed] [Google Scholar]
- 7. Wolf J. M., Green A. Influence of comorbidity on self-assessment instrument scores of patients with idiopathic adhesive capsulitis. J Bone Joint Surg Am. 2002;84-A:1167–1173 [PubMed] [Google Scholar]
- 8. Pal B., Anderson J., Dick W. C., Griffiths I. D. Limitation of joint mobility and shoulder capsulitis in insulin- and non-insulin-dependent diabetes mellitus. Br J Rheumatol. 1986; 25:147–151 [DOI] [PubMed] [Google Scholar]
- 9. Tighe C. B., Oakley W. S., Jr. The prevalence of a diabetic condition and adhesive capsulitis of the shoulder. South Med J. 2008; 101:591–595 [DOI] [PubMed] [Google Scholar]
- 10. Arkkila P. E., Kantola I. M., Viikari J. S., Ronnemaa T. Shoulder capsulitis in type I and II diabetic patients: association with diabetic complications and related diseases. Ann Rheum Dis. 1996; 55:907–914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bruckner F. E., Nye C. J. A prospective study of adhesive capsulitis of the shoulder (“frozen shoulder”) in a high risk population. Q J Med. 1981; 50:191–204 [PubMed] [Google Scholar]
- 12. Muller L. P., Muller L. A., Happ J., Kerschbaumer F. Frozen shoulder: a sympathetic dystrophy? Arch Orthop Trauma Surg. 2000; 120:84–87 [DOI] [PubMed] [Google Scholar]
- 13. Robinson D., Halperin N., Agar G., Alk D., Rami K. Shoulder girdle neoplasms mimicking frozen shoulder syndrome. J Shoulder Elbow Surg. 2003; 12:451–455 [DOI] [PubMed] [Google Scholar]
- 14. Reeves B. The natural history of the frozen shoulder syndrome. Scand J Rheumatol. 1975; 4:193–196 [DOI] [PubMed] [Google Scholar]
- 15. Rundquist P. J., Anderson D. D., Guanche C. A., Ludewig P. M. Shoulder kinematics in subjects with frozen shoulder. Arch Phys Med Rehabil. 2003; 84:1473–1479 [DOI] [PubMed] [Google Scholar]
- 16. Mao C. Y., Jaw W. C., Cheng H. C. Frozen shoulder: correlation between the response to physical therapy and follow-up shoulder arthrography. Arch Phys Med Rehabil. 1997;78: 857–859 [DOI] [PubMed] [Google Scholar]
- 17. Lin J. J., Wu Y. T., Wang S. F., Chen S. Y. Trapezius muscle imbalance in individuals suffering from frozen shoulder syndrome. Clin Rheumatol. 2005; 24:569–575 [DOI] [PubMed] [Google Scholar]
- 18. Fayad F., et al. Three-dimensional scapular kinematics and scapulohumeral rhythm in patients with glenohumeral osteoarthritis or frozen shoulder. J Biomech. 2008; 41:326–332 [DOI] [PubMed] [Google Scholar]
- 19. Rundquist P. J. Alterations in scapular kinematics in subjects with idiopathic loss of shoulder range of motion. J Orthop Sports Phys Ther. 2007; 37:19–25 [DOI] [PubMed] [Google Scholar]
- 20. Levine W. N., et al. Nonoperative management of idiopathic adhesive capsulitis. J Shoulder Elbow Surg. 2007; 16:569–573 [DOI] [PubMed] [Google Scholar]
- 21. Jurgel J., et al. Shoulder function in patients with frozen shoulder before and after 4-week rehabilitation. Medicina (Kaunas). 2005; 41:30–38 [PubMed] [Google Scholar]
- 22. Sokk J., Gapeyeva H., Ereline J., Kolts I., Paasuke M. Shoulder muscle strength and fatigability in patients with frozen shoulder syndrome: the effect of 4-week individualized rehabilitation. Electromyogr Clin Neurophysiol. 2007; 47:205–213 [PubMed] [Google Scholar]
- 23. Diercks R. L., Stevens M. Gentle thawing of the frozen shoulder: a prospective study of supervised neglect versus intensive physical therapy in seventy-seven patients with frozen shoulder syndrome followed up for two years. J Shoulder Elbow Surg. 2004; 13:499–502 [DOI] [PubMed] [Google Scholar]
- 24. Farrell C. M., Sperling J. W., Cofield R. H. Manipulation for frozen shoulder: long-term results. J Shoulder Elbow Surg. 2005; 14:480–484 [DOI] [PubMed] [Google Scholar]
- 25. Jewell D. V., Riddle D. L., Thacker L. R. Interventions associated with an increased or decreased likelihood of pain reduction and improved function in patients with adhesive capsulitis: a retrospective cohort study. Phys Ther. 2009;89: 419–429 [DOI] [PubMed] [Google Scholar]
- 26. Miller M. D., Wirth M. A., Rockwood C. A., Jr. Thawing the frozen shoulder: the “patient” patient. Orthopedics. 1996; 19:849–853 [DOI] [PubMed] [Google Scholar]
- 27. Dogru H., Basaran S., Sarpel T. Effectiveness of therapeutic ultrasound in adhesive capsulitis. Joint Bone Spine. 2008; 75:445–450 [DOI] [PubMed] [Google Scholar]
- 28. Rizk T. E., Christopher R. P., Pinals R. S., Higgins A. C., Frix R. Adhesive capsulitis (frozen shoulder): a new approach to its management. Arch Phys Med Rehabil. 1983; 64:29–33 [PubMed] [Google Scholar]
- 29. Green S., Buchbinder R., Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003;CD004258, doi:10.1002/14651858.CD004258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stergioulas A. Low-power laser treatment in patients with frozen shoulder: preliminary results. Photomed Laser Surg. 2008; 26:99–105 [DOI] [PubMed] [Google Scholar]
- 31. Leung M. S., Cheing G. L. Effects of deep and superficial heating in the management of frozen shoulder. J Rehabil Med. 2008; 40:145–150 [DOI] [PubMed] [Google Scholar]
- 32. Dundar U., Toktas H., Cakir T., Evcik D., Kavuncu V. Continuous passive motion provides good pain control in patients with adhesive capsulitis. Int J Rehabil Res. 2009; 32:193–198 [DOI] [PubMed] [Google Scholar]
- 33. Gaspar P. D., Willis F. B. Adhesive capsulitis and dynamic splinting: a controlled, cohort study. BMC Musculoskelet Disord. 2009;10:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. McClure P. W., Blackburn L. G., Dusold C. The use of splints in the treatment of joint stiffness: biologic rationale and an algorithm for making clinical decisions. Phys Ther. 1994; 74:1101–1107 [DOI] [PubMed] [Google Scholar]
- 35. McClure P. W., Flowers K. R. Treatment of limited shoulder motion: a case study based on biomechanical considerations. Phys Ther. 1992; 2:929–936 [DOI] [PubMed] [Google Scholar]
- 36. Johnson A. J., Godges J. J., Zimmerman G. J., Ounanian L. L. The effect of anterior versus posterior glide joint mobilization on external rotation range of motion in patients with shoulder adhesive capsulitis. J Orthop Sports Phys Ther. 2007; 37:88–99 [DOI] [PubMed] [Google Scholar]
- 37. Vermeulen H. M., Rozing P. M., Obermann W. R., le Cessie S., Vliet Vlieland T. P. Comparison of high-grade and low-grade mobilization techniques in the management of adhesive capsulitis of the shoulder: randomized controlled trial. Phys Ther. 2006; 86:355–368 [PubMed] [Google Scholar]
- 38. Gerwin R. D. Myofascial pain syndromes in the upper extremity. J Hand Ther. 1997; 10:130–136 [DOI] [PubMed] [Google Scholar]
- 39. Simons D. G., Travell J. G., Simons L. S. Travell & Simons' myofascial pain and dysfunction: the trigger point manual. Volume 1. The upper body. 2nd ed, 1999;596–612 Lippincott Williams & Wilkins [Google Scholar]
- 40. Kostopoulos D., Rizopoulos K. Effect of topical aerosol skin refrigerant (Spray and Stretch technique) on passive and active stretching. J Bodyw Mov Ther. 2008;12:96–104 [DOI] [PubMed] [Google Scholar]
- 41. Guler-Uysal F., Kozanoglu E. Comparison of the early response to two methods of rehabilitation in adhesive capsulitis. Swiss Med Wkly. 2004;134:353–358 [DOI] [PubMed] [Google Scholar]
- 42. Davidson C. J., et al. Rat tendon morphologic and functional changes resulting from soft tissue mobilization. Med Sci Sports Exerc. 1997; 9:313–319 [DOI] [PubMed] [Google Scholar]
- 43. Gehlsen G. M., Ganion L. R., Helfst R. Fibroblast responses to variation in soft tissue mobilization pressure. Med Sci Sports Exerc. 1999; 31:531–535 [DOI] [PubMed] [Google Scholar]
- 44. Page P., Frank C. C., Lardner R. Assessment and treatment of muscle imbalance: The Janda Approach. 2010;191–211 Human Kinetics [Google Scholar]
- 45. Arslan S., Celiker R. Comparison of the efficacy of local corticosteroid injection and physical therapy for the treatment of adhesive capsulitis. Rheumatol Int. 2001; 1:20–23 [DOI] [PubMed] [Google Scholar]
- 46. Dacre J. E., Beeney N., Scott D. L. Injections and physiotherapy for the painful stiff shoulder. Ann Rheum Dis. 1989; 48:322–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ryans I., Montgomery A., Galway R., Kernohan W. G., McKane R. A randomized controlled trial of intra-articular triamcinolone and/or physiotherapy in shoulder capsulitis. Rheumatology (Oxford). 2005; 44:529–535 [DOI] [PubMed] [Google Scholar]
- 48. Blanchard V., Barr S., Cerisola F. L. The effectiveness of corticosteroid injections compared with physiotherapeutic interventions for adhesive capsulitis: a systematic review. Physiotherapy. 2010; 6:95–107 [DOI] [PubMed] [Google Scholar]
- 49. Piotte F., et al. Effects of repeated distension arthrographies combined with a home exercise program among adults with idiopathic adhesive capsulitis of the shoulder. Am J Phys Med Rehabil. 2004; 83:537–546 [DOI] [PubMed] [Google Scholar]
- 50. Buchbinder R., et al. Efficacy and cost-effectiveness of physiotherapy following glenohumeral joint distension for adhesive capsulitis: a randomized trial. Arthritis Rheum. 2007; 57:1027–1037 [DOI] [PubMed] [Google Scholar]
- 51. Callinan N., et al. Effectiveness of hydroplasty and therapeutic exercise for treatment of frozen shoulder. J Hand Ther. 2003; 16:219–224 [DOI] [PubMed] [Google Scholar]
- 52. Bal A., et al. Effectiveness of corticosteroid injection in adhesive capsulitis. Clin Rehabil. 2008; 22:503–512 [DOI] [PubMed] [Google Scholar]
- 53. Carette S., et al. Intraarticular corticosteroids, supervised physiotherapy, or a combination of the two in the treatment of adhesive capsulitis of the shoulder: a placebo-controlled trial. Arthritis Rheum. 2003; 8:829–838 [DOI] [PubMed] [Google Scholar]
- 54. Khan A. A., Mowla A., Shakoor M. A., Rahman M. R. Arthrographic distension of the shoulder joint in the management of frozen shoulder. Mymensingh Med J. 2005; 14:67–70 [PubMed] [Google Scholar]
- 55. Loew M., Heichel T. O., Lehner B. Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. J Shoulder Elbow Surg. 2005; 14:16–21 [DOI] [PubMed] [Google Scholar]
- 56. Jacobs L. G., Smith M. G., Khan S. A., Smith K., Joshi M. Manipulation or intra-articular steroids in the management of adhesive capsulitis of the shoulder? A prospective randomized trial. J Shoulder Elbow Surg. 2009; 18:348–353 [DOI] [PubMed] [Google Scholar]