Abstract
Background:
Because newer anticoagulation strategies for total knee replacement present potentially increased risk of neuraxial analgesia, there is movement away from using patient-controlled epidural analgesia (PCEA) for pain control. This concern opens the door for other regional modalities in postoperative analgesia, including the use of extended-release epidural morphine (EREM) combined with a femoral nerve block (FNB).
Methods:
This study was a prospective observational chart review with the use of recent historical controls in patients undergoing unilateral total knee replacement. Outcomes of interest were 0-, 24-, and 48-hour postoperative pain scores using the visual analog scale (VAS); incidence of side effects; and time spent in the postanesthesia care unit (PACU).
Results:
Postoperative pain scores at 24 and 48 hours in the EREM and FNB group (n = 14; 2.6 ± 0.6 and 5.0 ± 0.9, respectively) were comparable to the PCEA group (n = 14; 3.8 ± 0.6 and 4.2 ± 0.9). The PACU time was shorter in the EREM and FNB group (2.4 ± 0.3 hours) compared with PCEA (3.6 ± 0.3 hours, P = .02). No statistically significant difference was found in the incidence of side effects between the 2 groups.
Conclusions:
The VAS scores at 24 and 48 hours indicate that EREM and FNB provide comparable analgesia to PCEA. The trend toward shorter PACU times represents an opportunity for cost-identification analysis. The study data are limited by their observational nature and the small number of patients involved; nevertheless, this study demonstrates a therapeutic equivalence to PCEA that may be more cost effective.
Keywords: Analgesia, extended-release epidural morphine, femoral nerve block, patient-controlled epidural analgesia, total knee arthroplasty
INTRODUCTION
Arthroplasty of the knee has been evolving as a surgical treatment for arthritis for almost 150 years.1-6 Total knee replacements now account for 1% to 2% of all inpatient surgical procedures performed7 and almost 5% of procedures for the population aged 65 to 74 in short-stay hospitals.8 The postoperative pain from this procedure is substantial,9,10 with the possibility of prolonged hospitalization,11 impairment of the rehabilitation process,11 and worse functional outcome.12 The traditional method of perioperative care for this orthopedic procedure consisted of a general anesthetic followed by postoperative parenteral opioids.13,14 However, during the past 20 years, clinical studies have supported a transition to spinal conduction blockade for intraoperative anesthetic management and patient-controlled epidural analgesia (PCEA) for postoperative analgesia.9 This regimen has several benefits, including reduced blood loss,15 decreased incidence of deep venous thrombosis (DVT),16 better postoperative pain control,17 improved range of motion,17 and fewer opioid-related side effects.9,11,14,18 These reported benefits have resulted in some authors considering PCEA the current gold standard for pain control with this procedure.18
Despite the reported decrease in the incidence of postoperative DVT afforded by epidural analgesia,16 this complication remains a significant source of morbidity and mortality during the postoperative course, leading to development of various perioperative anticoagulation regimens.19,20 Initially, anticoagulation for this surgical procedure was managed with anticoagulants such as warfarin, beginning on the night after the procedure with the removal of the epidural catheter up to 36 hours after the first warfarin dose.21 However, to further decrease the incidence of DVT, some orthopedic services now prescribe the first dose of warfarin on the night prior to surgery22 or start treatment with low-molecular-weight heparin (LMWH) on postoperative day 1.19,20 The addition of LMWH has further reduced the incidence of DVT to 25%20 to 33%19 compared with an incidence of 45%20 with the use of warfarin alone. This change in anticoagulation practice necessitates the removal of the epidural catheter on the first postoperative day,21 which may result in ineffective management of postoperative pain.
The evolving approach to perioperative anticoagulation for orthopedic surgery requires changes in our anesthetic practice and in our approach to the management of postoperative pain. Although single-shot femoral nerve block (FNB),23,24 continuous femoral nerve blockade (CFNB),25-27 and extended-release epidural morphine (EREM)28 have been studied for postoperative pain in total knee arthroplasty, the results have been mixed.23-28 Single-shot FNB, when used alone, does not provide satisfactory pain relief in the sciatic distribution, and the resultant analgesia does not extend beyond 24 to 36 hours.23,24 CFNB has been shown in multiple studies to provide adequate postoperative analgesia after unilateral total knee arthroplasty (uTKA), but it is a resource-expensive technique that requires additional training and equipment and may not be practical for all anesthesia providers.25-27 Doses of EREM necessary to provide adequate analgesia for uTKA are higher than those recommended by the Food and Drug Administration (FDA).28 Experience at our institution revealed that EREM alone at FDA-recommended doses did not reliably control postoperative pain for our knee arthroplasty patients. PCEA in combination with single-shot FNB might be a suitable alternative because this strategy provides better pain relief with movement than PCEA alone, but newer anticoagulation regimens are incompatible with an epidural catheter remaining in place for 48 hours.21,29 At our institution, we have examined a hybrid of these techniques, using 7.5- to 15-mg doses of EREM in conjunction with an FNB using 30 mL of 0.375% bupivacaine to provide adequate postoperative analgesia with minimal side effects in a manner that allows the institution of early anticoagulation therapy.
Therefore, we examined a hybrid of these techniques, using a larger dose of EREM in conjunction with FNB with respect to the hybrid's ability to provide adequate post–knee arthroplasty analgesia. The goal of our study was to prospectively compare EREM with FNB to PCEA on pain, postanesthesia care unit (PACU) stay, hospital length of stay, and side effects. No funding for this study was provided from outside our institution.
MATERIALS AND METHODS
The study design was a case-controlled observational study compared with recent institutional historical controls. This study was approved by the institutional review board (IRB) of Ochsner Clinic Foundation prior to inception. The IRB granted approval to waive the need for informed consent. The study's a priori hypothesis involved examination of the analgesic effectiveness of EREM in combination with a single-injection FNB compared with PCEA following total knee arthroplasty. Patients were enrolled between January 1, 2006, and March 31, 2008, and observed throughout their hospital stay. Data collected from these patients included age; gender; body mass index (BMI); 0-, 24-, and 48-hour postoperative pain scores measured by the visual analog scale (VAS) of 0 to 10; postoperative range of motion at 24, 48, and 72 hours; side effects; adverse events; use of additional opioid analgesics; time spent in the PACU; and days spent in the hospital. All cases were drawn from the population of patients undergoing uTKA at a referral care institution. Exclusion criteria included the presence of metastatic bone cancer, Paget disease, narcolepsy, excessive daytime sleepiness, pregnancy, lactation, chronic opioid use, or idiosyncratic/hypersensitive reaction to opioids as documented in the preoperative evaluation.30 Cases were preoperatively selected by reviewing the elective operating room (OR) schedule. The control group was defined as patients who underwent uTKA with spinal anesthesia and received PCEA during the 2006 calendar year. These historical controls were chosen just prior to the change in the orthopedic anticoagulation regimen for this surgical procedure and implementation of EREM and FNB in 2007. Control patients were matched to the study group by age and gender. Sample size was 14 for each group and was determined by the number of patients receiving EREM and FNB during the study period.
Two assessors were assigned the task of screening the OR schedule, anesthesiology billing records, and hospital charts to ensure completeness and accuracy of data collection and management. The primary statistic analyzed was the postoperative VAS score. Secondary data observed were demographic data, PACU times and costs, hospital discharge times, and side effects as specified previously. PACU costs were calculated from fixed and variable hourly rates for routine acuity recovery and displayed as an aggregate sum. Numeric data were analyzed for normalcy of distribution, equal variance, and statistical difference between the 2 groups using analysis of variance (ANOVA) t test and Wilcoxon and Kruskal-Wallis tests as indicated by data distribution. Categorical data were analyzed for independence using Pearson chi square analysis and Fisher exact test. Continuous data are displayed as quantile box plots. Subgroup analysis of the study group was performed regarding doses of EREM and FNB used. Alpha level was set at 0.05 for 2-tailed analysis of data. Statistical analysis was performed with JMP 6.0.0 (SAS Institute Inc, Cary, NC).
RESULTS
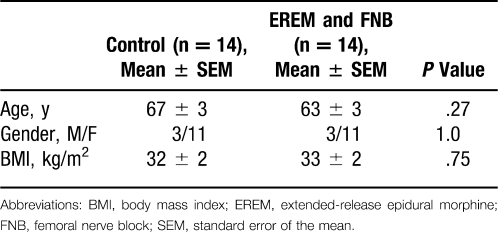
During the study period, 14 patients met criteria for the EREM and FNB (study) group, while 14 patients similarly matched in age and gender from the PCEA sample (control) were identified and paired. No statistical differences were found in the demographic characteristics, such as age, gender, or BMI (Table 1).
Table 1.
Patient Demographics
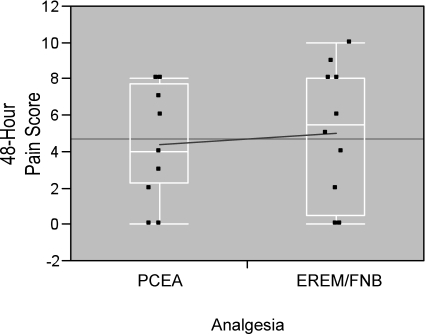
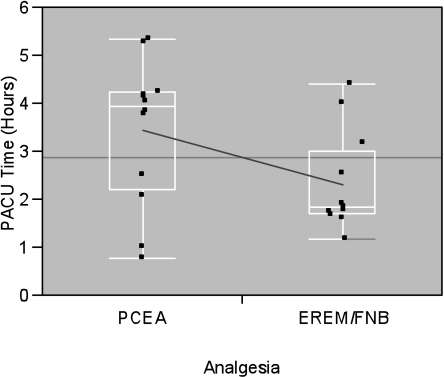
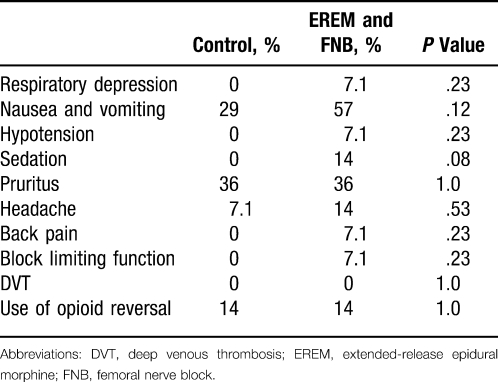
The study group had a higher mean VAS pain score on admission to the PACU (Table 2) and similar VAS pain scores at 24 and 48 hours (Figures 1 and 2). The mean time spent in the PACU was statistically shorter in the study group (Figure 3); however, days spent in the hospital postoperatively were not significantly different between the 2 groups (Table 2). No statistically significant difference was found in the incidence of any reported side effects (Table 3). Range of motion was not analyzed because of insufficient data recorded in the patients' hospital charts.
Table 2.
Pain Scores and Discharge Times
Figure 1.
Quantile box plots of 24-hour visual analog scale scores of control group (patient-controlled epidural analgesia [PCEA]) versus study group (extended-release epidural morphine [EREM] and femoral nerve block [FNB]).
Figure 2.
Quantile box plots of 48-hour visual analog scale scores of control group (patient-controlled epidural analgesia [PCEA]) versus study group (extended-release epidural morphine [EREM] and femoral nerve block [FNB]).
Figure 3.
Quantile box plots of hours spent in the postanesthesia care unit of control group (patient-controlled epidural analgesia [PCEA]) versus study group (extended-release epidural morphine [EREM] and femoral nerve block [FNB]). n, number of patients in each group.
Table 3.
Side Effect Frequency
DISCUSSION
Our data allow a comparison of PCEA and combination epidural morphine and FNB analgesia after knee replacement surgery. They indicate a shorter PACU stay can be achieved with the latter while offering comparable 24- to 48-hour analgesia. The lower VAS score at 24 hours in the EREM and FNB group suggests that this novel technique is effective in the control of postoperative pain in patients who undergo uTKA. The upward trend of the mean VAS score at 48 hours, which was greater in the study group compared with the control group, may be caused by several factors: (1) there was no residual analgesia from FNB, (2) there were diminishing benefits from EREM, and (3) most important, in patients whose postoperative pain was not well controlled at 24 hours, active adjustments were required in their local anesthetic and opioid infusions to improve postoperative analgesia.
The EREM and FNB patients had shorter stays in the PACU, representing a significant opportunity for cost savings. A more predictable PACU stay can allow for more efficient and accurate scheduling of PACU use (Figure 3). The shorter stay by EREM and FNB patients might improve PACU throughput. This in turn may reduce wait times for OR patients seeking PACU admission during periods of high utilization. The phenomenon of ORs waiting for PACU admission, with attendant throughput slowdowns, has been a problem for institutions across the country. The shorter PACU stay itself represents an aggregate cost savings of $991 in use of PACU nursing and other resources (Figure 4). From this series of patients, we project institutional savings of more than $14,000 per year in direct PACU costs; however, the feasibility and cost effectiveness of this new technique are dependent on an individual institution's acquisition costs, labor costs, and scarcity of resources. Also, the reduced utilization of PACU hospital resources may be offset by the cost of EREM.
Figure 4.
Bar graph comparing aggregate hospital postanesthesia care unit (PACU) cost based on time spent in PACU of control group (patient-controlled epidural analgesia [PCEA]) versus study group (extended-release epidural morphine [EREM] and femoral nerve block [FNB]).
The clinical implications of these data are that EREM and FNB may be a comparable method of postoperative analgesia to PCEA.
The observational nature of this study precludes controlling for all variables but does eliminate volunteer and practitioner bias and suggests broad acceptance of this technique. Although the use of historical controls has the potential to introduce a multitude of confounding factors, our controls were from the same institution within a short time frame and with many of the same perioperative personnel. A larger sample size would have provided more accurate confidence intervals and may have allowed some trends in the data to reach statistical significance. Therefore, our study likely lacked the statistical power to detect all but very large side effect or pain score differences. Nevertheless, our data show that EREM and FNB provide analgesia comparable to PCEA, with a potential for institutional cost savings from shorter PACU stays. Although our EREM and FNB patients seemed to have less pain at 24 hours compared with PCEA, further investigation is required to confirm this finding.
Acknowledgments
This article meets the Accreditation Council for Graduate Medical Education competencies for Patient Care, Medical Knowledge, and Systems-Based Practice.
Footnotes
Financial support solely provided by institution.
Presented at the Gulf-Atlantic Anesthesia Residents' Research Conference, April 12, 2008.
The authors acknowledge the assistance of Pat Brandon, RN, for assistance with data collection.
REFERENCES
- 1.Fergusson M. Excision of the knee joint: recovery with a false joint and a useful limb. Med Times Gaz. 1861;1:601. [Google Scholar]
- 2.Campbell W. C. Interposition of Vitallium plates in arthroplasties of the knee: preliminary report. Clin Orthop Relat Res. 1976. pp. 4–6. Oct. [PubMed]
- 3.Walldius B. Arthroplasty of the knee joint using endoprosthesis. Acta Orthop Scand. 1957;24((suppl)):19. doi: 10.3109/ort.1957.28.suppl-24.01. [DOI] [PubMed] [Google Scholar]
- 4.Coventry M. B., Upshaw J. E., Riley L. H., Finerman G. A., Turner R. H. Geometric total knee arthroplasty: I. Conception, design, indications, and surgical technic. Clin Orthop. 1973;94:171–184. [PubMed] [Google Scholar]
- 5.Rand J. A. Patellar resurfacing in total knee arthroplasty. Clin Orthop. 1990;260:110–117. [PubMed] [Google Scholar]
- 6.Laskin R. S., Maruyama Y., Villaneuva M., Bourne R. Deep-dish congruent tibial component use in total knee arthroplasty: a randomized prospective study. Clin Orthop. 2000;380:36–44. doi: 10.1097/00003086-200011000-00006. [DOI] [PubMed] [Google Scholar]
- 7.DeFrances C., Podgornik M. 2004 National Hospital Discharge Survey. Advance Data From Vital and Health Statistics. 2006;371:1–20. [PubMed] [Google Scholar]
- 8.Chartbook on trends in the health of Americans. Health. 2006. pp. 363–365.
- 9.Raj P., Knarr D., Vigdorth E., et al. Comparison of continuous epidural infusion of a local anesthetic and administration of systemic narcotics in the management of pain after total knee replacement surgery. Anesth Analg. 1987;66((5)):401–406. doi: 10.1213/00000539-198705000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Bonica J. Postoperative pain. In: Bonica J., editor. The Management of Pain. 2nd ed. Philadelphia, PA: Lea & Febiger; 1990. pp. 461–480. [Google Scholar]
- 11.Ryu J., Saito S., Yamamoto K., Sano S. Factors influencing the postoperative range of motion in total knee arthroplasty. Bull Hosp Jt Dis. 1993;53((3)):35–40. [PubMed] [Google Scholar]
- 12.Kehlet H. Surgical stress: the role of pain and analgesia. Br J Anaesth. 1989;63((2)):189–195. doi: 10.1093/bja/63.2.189. [DOI] [PubMed] [Google Scholar]
- 13.Ferrante F. M., Orav E. J., Rocco A. G., Gallo J. A statistical model for pain in patient-controlled analgesia and conventional intramuscular opioids regimens. Anesth Analg. 1988;67((5)):457–461. [PubMed] [Google Scholar]
- 14.Liu S. S., Wu C. L. The effect of analgesic technique on patient-reported outcomes including analgesia: a systematic review. Anesth Analg. 2007;105((3)):789–808. doi: 10.1213/01.ane.0000278089.16848.1e. [DOI] [PubMed] [Google Scholar]
- 15.Modig J. Regional anaesthesia and blood loss. Acta Anaesthesiol Scand Suppl. 1988;89:44–48. doi: 10.1111/j.1399-6576.1988.tb02842.x. [DOI] [PubMed] [Google Scholar]
- 16.Modig J., Malmberg P., Karlstrom G. Effect of epidural versus general anesthesia on calf blood flow. Acta Anaesthesiol Scand. 1980;24:305–309. doi: 10.1111/j.1399-6576.1980.tb01553.x. [DOI] [PubMed] [Google Scholar]
- 17.Farag E., Dilger J., Brooks P., Tetzlaff J. E. Epidural analgesia improves early rehabilitation after total knee replacement. J Clin Anesth. 2005;17((4)):281–285. doi: 10.1016/j.jclinane.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Zaric D., Boysen K., Christiansen C., Christiansen J., Stephensen S., Christensen B. A comparison of epidural analgesia with combined continuous femoral-sciatic nerve blocks after total knee replacement. Anesth Analg. 2006;102((4)):1240–1246. doi: 10.1213/01.ane.0000198561.03742.50. [DOI] [PubMed] [Google Scholar]
- 19.Colwell C. W., Jr, Hardwick M. E. Rationale for low-molecular-weight heparin prophylaxis after total knee arthroplasty. Clin Orthop Relat Res. 2006;452:181–185. doi: 10.1097/01.blo.0000238826.63648.c5. [DOI] [PubMed] [Google Scholar]
- 20.Fitzgerald R. H., Jr, Spiro T. E., Trowbridge A. A., et al. Prevention of venous thromboembolic disease following primary total knee arthroplasty: a randomized, multicenter, open-label, parallel-group comparison of enoxaparin and warfarin. J Bone Joint Surg Am. 2001;83-A((6)):900–906. [PubMed] [Google Scholar]
- 21.Horlocker T. T., Wedel D. J., Benzon H., et al. Regional anesthesia in the anticoagulated patient: defining the risks (the second ASRA Consensus Conference on Neuraxial Anesthesia and Anticoagulation) Reg Anesth Pain Med. 2003;28((3)):172–197. doi: 10.1053/rapm.2003.50046. [DOI] [PubMed] [Google Scholar]
- 22.Lenzini P. A., Grice G. R., Milligan P. E., et al. Optimal initial dose adjustment of warfarin in orthopedic patients. Ann Pharmacother. 2007;41((11)):1798–1804. doi: 10.1345/aph.1K197. [DOI] [PubMed] [Google Scholar]
- 23.Wang H., Boctor B., Verner J. The effect of single-injection femoral nerve block on rehabilitation and length of hospital stay after total knee replacement. Reg Anesth Pain Med. 2002;27((20)):139–144. doi: 10.1053/rapm.2002.29253. [DOI] [PubMed] [Google Scholar]
- 24.Sites B. D., Beach M., Gallagher J. D., Jarrett R. A., Sparks M. B., Lundberg C. J. A single injection ultrasound-assisted femoral nerve block provides side effect-sparing analgesia when compared with intrathecal morphine in patients undergoing total knee arthroplasty. Anesth Analg. 2004;99((5)):1539–1543. doi: 10.1213/01.ANE.0000136470.51029.52. [DOI] [PubMed] [Google Scholar]
- 25.Singelyn F. J., Deyaert M., Joris D., Pendeville E., Gouverneur J. M. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg. 1998;87((1)):88–92. doi: 10.1097/00000539-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 26.Capdevila X., Barthelet Y., Biboulet P., Ryckwaert Y., Rubenovitch J., d'Athis F. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology. 1999;91((1)):8–15. doi: 10.1097/00000542-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Barrington M. J., Olive D., Low K., Scott D. A., Brittain J., Choong P. Continuous femoral nerve blockade or epidural analgesia after total knee replacement: a prospective randomized controlled trial. Anesth Analg. 2005;101((6)):1824–1829. doi: 10.1213/01.ANE.0000184113.57416.DD. [DOI] [PubMed] [Google Scholar]
- 28.Hartrick C. T., Martin G., Kantor G., Koncelik J., Manvelian G. Evaluation of a single-dose, extended release epidural morphine formulation for pain after knee arthroplasty. J Bone Joint Surg Am. 2006;88((2)):273–281. doi: 10.2106/JBJS.D.02738. [DOI] [PubMed] [Google Scholar]
- 29.YaDeau J. T., Cahill J. B., Zawadsky M. W., et al. The effects of femoral nerve blockade in conjunction with epidural analgesia after total knee arthroplasty. Anesth Analg. 2005;101((3)):891–895. doi: 10.1213/01.ANE.0000159150.79908.21. [DOI] [PubMed] [Google Scholar]
- 30.Viscusi E. R., Martin G., Hartrick C. T., Singla N., Manvelian G. EREM Study Group. Forty-eight hours of postoperative pain relief after total hip arthroplasty with a novel, extended-release epidural morphine formulation. Anesthesiology. 2005;102((5)):1014–1022. doi: 10.1097/00000542-200505000-00022. [DOI] [PubMed] [Google Scholar]