A 70-year-old man presented with right-sided epistaxis that had been unrelieved by direct pressure for the past 90 minutes. His medical history was significant for hypertension (blood pressure was 180/100 mmHg on arrival), atrial fibrillation, and coronary artery disease. His current medications are aspirin, warfarin, enalapril, and metoprolol tartrate. On placement of an anterior nasal pack on the right side, the patient began bleeding heavily from the left side.
Epistaxis, or nose bleed, is a common problem, affecting up to 60 million Americans each year. Although most cases of epistaxis are relatively minor and manageable with conservative measures, sometimes the malady can present as a life-threatening problem. The focus of this article is to review the vascular anatomy of the nasal cavity as well as the etiologies and management of epistaxis.
VASCULAR ANATOMY
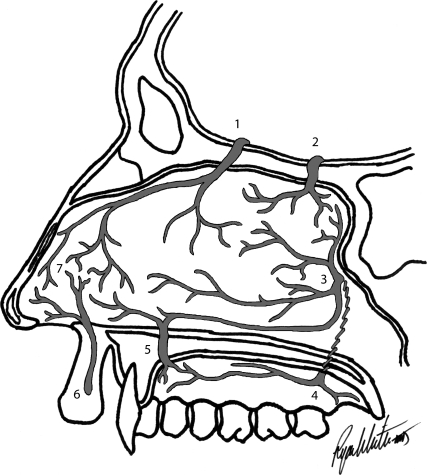
The nasal blood supply comes from both internal and external carotid artery systems (Figure). The external carotid provides arterial flow via the facial and internal maxillary artery (IMA). The facial artery forms the superior labial artery, which supplies the septum and nasal alae. The IMA terminates into 5 branches: the sphenopalatine, pharyngeal, greater palatine, infraorbital, and superior alveolar arteries. Of these 5 branches, only the sphenopalatine, pharyngeal, and greater palatine supply the nasal cavity. The sphenopalatine and its terminal branches supply the septum and middle and inferior turbinate area. The pharyngeal artery also supplies the inferior aspect of the lateral nasal wall, and the greater palatine transverses the greater palatine canal and supplies the anterior aspect of the septum.
Blood supply of the nasal septum: (1) anterior ethmoidal artery, (2) posterior ethmoidal artery, (3) sphenopalatine artery, (4) greater (anterior division) and lesser (posterior division) palatine arteries, (5) greater palatine artery, (6) superior labial artery, and (7) Kiesselbach plexus.
The internal carotid artery supplies the nose via the terminal branches of the ophthalmic artery and the anterior and posterior ethmoid arteries. These arteries branch from the ophthalmic artery within the orbit and descend into the nasal cavity from above, supplying the septum and lateral nasal walls. Of note, 2 anastomotic areas within the nose often provide a source of epistaxis. Woodruff area is located on the inferior aspect of the lateral nasal wall, posterior to the inferior turbinate. It is formed from the anastomoses of the sphenopalatine and pharyngeal arteries. The posterior location makes it a common source for severe, nontraumatic bleeds. Kiesselbach plexus is an anastomosis with branches from both the internal and external carotid artery systems. The anterior ethmoid, greater palatine, sphenopalatine, and superior labial arteries all form a plexus of vessels in the anteroinferior nasal septum. Kiesselbach plexus is the source of the majority of nose bleeds.
ETIOLOGIES
Epistaxis can be divided into local and systemic etiologies. Furthermore, the most common causes of epistaxis will change as the patient ages. One constant among etiologies, though, is that epistaxis increases in frequency during winter months. The decreased humidity along with decreased temperature inhibits nasal humidification. The nasal mucosa is subject to poor local wound healing and is therefore more susceptible to bleeding.1
Local
The most common local causes of epistaxis are trauma, anatomic deformities, inflammatory reactions, and intranasal tumors.
Epistaxis is most commonly encountered in the pediatric population secondary to digital trauma.2 Digital irritation to Kiesselbach plexus is a very common source of anterior septal nose bleeds in children, especially during the winter months. The improper use of topical nasal sprays is another source of epistaxis. Repeated trauma to the epithelium of the septal mucosa from sprays directed medially can cause intermittent epistaxis. Proper counseling and instruction to direct the spray away from the midline septum can alleviate this problem. Trauma from a foreign body can elicit epistaxis. Rhinorrhea may also be present secondary to an associated foreign body reaction or infection. Postsurgical epistaxis is a common phenomenon that is usually amenable to conservative treatments. Lastly, the use of nasal cannula can cause epistaxis secondary to their local irritation as well as effects of nasal drying.
Septal deflections, bony spurs, and fractures are underlying anatomic deformities in the nose that can predispose a patient to epistaxis. Any nasal obstruction leads to a disruption of air flow. The resultant turbulent flow anterior to these obstructions has a drying effect, increasing the opportunity for mucosal disruption and epistaxis. Furthermore, severe deflections/spurs can actually cause local trauma to the lateral nasal wall mucosa.
Any form of inflammatory or granulomatous disease within the nasal cavity can cause bleeding. Common examples include bacterial sinusitis, allergic rhinitis, nasal polyposis, Wegner granulomatosis, tuberculosis, and sarcoidosis.
Finally, suspicion should arise for intranasal neoplasms/vascular malformations involving recurrent nose bleeds, especially unilateral ones, with no known cause. Some examples of intranasal masses that can initially present with epistaxis are inverted papillomas, angiofibromas, aneurysms, encephaloceles, hemangiomas, adenocarcinomas, and esthesioneuroblastomas.
Systemic
The most common systemic causes of epistaxis are hypertension, aberrations in clotting ability, inherited bleeding diatheses, and vascular/cardiovascular diseases.
Although the mechanistic relationship of hypertension and epistaxis is still being debated, the 2 are undeniably associated. Hypertension is the most common associated finding in cases of severe or refractory epistaxis.3
The ability to form clots is essential to the prevention and control of epistaxis. Both medication-induced clotting aberrations and liver dysfunction are common systemic factors influencing epistaxis. Medications commonly associated with epistaxis are aspirin, clopidogrel, nonsteroidal anti-inflammatory drugs, and warfarin. Chronic alcohol ingestion and renal dysfunction with associated uremia uniquely cause platelet dysfunction. In the setting of these specific diseases, liver function tests and platelet counts are generally within normal limits.
The most common inherited bleeding disorders associated with epistaxis are hemophilia A, hemophilia B, and von Willebrand disease. Hemophilia A and B are caused by deficiencies in factor VIII and factor IX, respectively; both are integral components in the coagulation cascade. von Willebrand disease is caused by a qualitative or quantitative deficiency in the von Willebrand factor, a glycoprotein essential to the proper function of factor VIII. Inheritance of these disorders is sex-linked; only males are affected. A preoperative work-up identifying these disorders can potentially prevent life-threatening bleeding during surgery. Desmopressin and cryoprecipitate can be given prophylactically and therapeutically in these situations.
Vascular and cardiovascular diseases such as congestive heart failure, arteriosclerosis, and collagen abnormalities can also be contributing factors to epistaxis. A well-known association between hereditary hemorrhagic telangiectasia and epistaxis has been determined.4 Hereditary hemorrhagic telangiectasia, or Osler-Rendu-Weber disease, has an autosomally dominant inheritance pattern with incomplete penetrance. Its presenting symptom is usually epistaxis secondary to telangiectasias of the nasal mucosa. Genetic mutations involving growth factor-beta result in fragile, injury-prone vessels with deficiencies in elastic tissue and smooth muscle.
MANAGEMENT
The management of epistaxis can be divided into medical therapy, conservative therapy, surgical therapy, and arterial embolization.
Medical Therapy
Medical therapy acts in both a therapeutic and prophylactic manner. Hypertension and other hematologic causes for epistaxis must be identified and corrected initially. Once these conditions are corrected, the majority of bleeds are alleviated with gentle direct pressure in the form of a nose pinch. Furthermore, nasal irrigation with saline and the placement of topical ointment in the nostrils create a humidified nasal environment that can prevent further episodes of epistaxis. If bleeding persists, a topical nasal decongestant for the purpose of vasoconstriction can be used. Care must be taken to not continue topical decongestant use indefinitely as it can become physiologically addictive.
Conservative Therapy
Conservative therapy includes cautery and nasal packing. Nasal cautery can be performed chemically or thermally. Chemical cautery uses topical application of silver nitrate, while Bovie electrocautery is used in thermal cautery. Cautery can be performed at the bedside or in the clinic setting after adequate topical anesthesia if the bleeding site is anterior and therefore visible. More posterior sites may require general anesthesia and an operating room setting.
Nasal packing is performed via anterior or posterior nasal packs. When medical therapy and cautery fail, identification of anterior nasal bleeds is followed by application of an anterior pack. Physician preference and the patient's comfort level determine the choice of packing agent. All packs should be covered in antibiotic ointment and provide ample pressure against the source of bleeding. Packs should be left in place no more than 5 days to prevent toxic shock syndrome or other associated infections. Oral antibiotics should be administered for as long as the packs remain in the nose. After placement of an anterior pack, epistaxis should cease and examination should reveal no active bleeding down the posterior oropharynx. After successful placement of an anterior pack, patients can be sent home and safely managed on an outpatient basis.
If epistaxis begins in the contralateral nose or bleeding down the posterior oropharynx worsens after application of an anterior pack, the addition of a posterior pack may be required. Posterior packs include double-balloon nasal packs as well as Foley catheters. The goal of the posterior pack is to seal the nasopharynx at the choanal entrance and provide a support against which to place an anterior pack. Double-balloon systems provide both an anterior and posterior balloon. When using a Foley catheter, the placement of anterior packing material tightly against the inflated Foley balloon is required. Similar general principles must be followed when using posterior packs to prevent infection. One important difference is that the placement of an anterior/posterior pack requires hospitalization secondary to potential complications. Specifically, placing a pack in the nasopharynx can trigger the nasopulmonary reflex, resulting in apnea and dysrhythmias. Therefore, patients should be monitored in an intensive care unit or with continuous pulse oximetry and telemetry.
Surgical Therapy
Surgical therapy for epistaxis has largely been supplanted by the use of arterial embolization. Procedures used for bleeds that are refractory to medical and conservative therapy include IMA, anterior ethmoid artery, and external carotid artery ligation.
Arterial Embolization
Arterial embolization performed by interventional radiologists is a relatively new technique used to embolize distal branches of the IMA. Under local anesthesia, diagnostic angiograms are performed to assess the vascular anatomy. Brisk bleeds will show up as blushes and can be selectively embolized. Potential complications include transient hemiparesis, facial paralysis, blindness, columellar necrosis, stroke, and death, but these are uncommon when procedures are performed by experienced surgeons. Finally, a general principle is that the more proximal the embolization, the greater the likelihood for postembolization complications.
CONCLUSION
Epistaxis is a problem commonly encountered by otolaryngologists. The majority of cases are easily treated, but some can present as life-threatening. Knowledge of the vascular anatomy is critical to determining the location of the bleed. Once the location is identified, appropriate medical, conservative, or surgical therapy can ensue.
REFERENCES
- 1.Bailey B. J. Head and Neck Surgery–Otolaryngology. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 2.Cummings C. W. Cummings Otolaryngology Head and Neck Surgery. 4th ed. Philadelphia, PA: Elsevier Mosby; 2005. [Google Scholar]
- 3.Guarisco J. L., Graham H. D. 3rd. Epistaxis in children: causes, diagnosis, and treatment. Ear Nose Throat J. 1989;68((7)) [PubMed] [Google Scholar]
- 4.Sharathkumar A. A., Shapiro A. Hereditary haemorrhagic telangiectasia. Haemophilia. 2008;14((6)):1269–1280. doi: 10.1111/j.1365-2516.2008.01774.x. [DOI] [PubMed] [Google Scholar]