Abstract
Caustic ingestion is a serious medical problem with a variety of clinical presentations and a complicated clinical course. This article reviews the epidemiology and pathophysiology of caustic ingestion as well as the most current approaches to diagnosis and treatment. Finally, a recent case will be presented that highlights the difficulty this problem poses to a medical team.
Keywords: Caustic ingestion, caustic substance, corrosive injury, corrosive substance, endoscopy, esophageal stricture
INTRODUCTION AND EPIDEMIOLOGY
Caustic injury remains an important public health problem in the United States and the world despite various education and regulatory efforts to reduce its occurrence. In the United States, an estimated 5,000 to 15,000 caustic ingestions occur per year.1–3 The age of occurrence of these ingestions shows a bimodal pattern.1 The first peak is seen in children aged 1 to 5 years, with most of these ingestions being accidental, though reports of child abuse have been reported in the literature.1,4,5 The problem of caustic ingestion in children is spreading in developing countries, as these agents become more available, with much of the recent research coming from that part of the world.6 The other peak age for caustic ingestion is seen among adults aged 21 years and older. Most of the ingestions seen in this population are intentional suicide attempts.1,4,5
Caustic ingestions may cause widespread injury to the lips, oral cavity, pharynx, and the upper airway. The effect that these agents have on the esophagus accounts for most of the serious injuries and long-term complications seen among both children and adults.3 Short-term complications include perforation and death. Long-term complications include stricture and increased lifetime risk of esophageal carcinoma.7 In children, 18% to 46% of all caustic ingestions are associated with esophageal burns. This number may be higher in adults who often consume larger amounts of the caustic substance as part of a suicide attempt.7,8 Because of its importance, a large portion of the discussion will be concerned with esophageal injuries.
ETIOLOGIC AGENTS AND TYPES OF INJURIES
The nature of the injury caused by caustic ingestion is determined by a number of factors including the identity of the agent, the amount consumed, the concentration, and the length of time the agent is in contact with a given tissue.5,9
Caustic materials cause tissue injury by chemical reaction. These materials are generally acidic or alkali. Usually, acids with pH less than 3 or bases with pH greater than 11 are of the greatest concern for caustic injury.10 Alkalis contain bases dissolved in water.5 Examples are such agents as sodium hydroxide and potassium hydroxide (for complete list see Table 1). Lye is a general term for alkali found in cleaning products.7 Caustic alkaline materials are also found in drain cleaners, various cleaning agents, hair relaxers, dishwasher detergents, and disk batteries.4,11
Table 1.
Commonly Ingested Caustic/Corrosive Agents
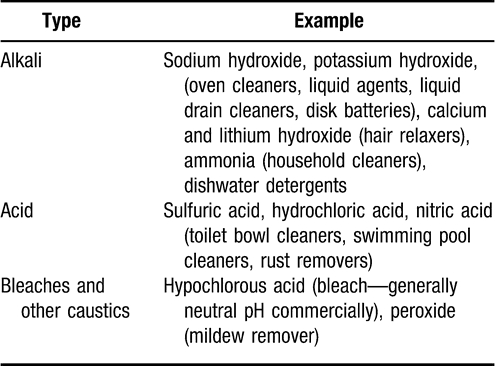
In liquid form, bases are tasteless and denser than water, resulting in pronounced distal injuries1,9 Alkali ingestion causes liquefactive necrosis with diffusion into deeper layers of the injured mucosa. Saponification of fats, denaturation of proteins, and blood vessel thrombosis will occur during the injury process.1,4,5,11 This injury occurs quickly, with a 30% solution of sodium hydroxide being able to produce full thickness injury in 1 second.7 Even lower concentrations can produce extensive injury. A recent animal study from Brazil12 showed that a low concentration solution (1.83%) was able to produce esophageal epithelial necrosis in 1 hour.
Like their liquid counterparts, solid strong alkali substances can produce deep injuries although they tend to adhere to the mucosa of the mouth and esophagus, thus sparing the stomach. Weaker alkalis that are powdered or granular, such as dishwater detergents, tend to injure the upper airway and can cause laryngeal edema and airway compromise.1,8,13
Alkaline disk batteries contain a 45% solution of potassium hydroxide or sodium hydroxide. Their ingestion will result in damage and leakage within 1 hour and in perforation in 8 to 12 hours if they lodge in the esophagus; this event mandates the immediate removal.4,5 If they are ingested and become lodged in the esophagus, an emergency situation arises.
Hair straighteners and relaxers containing calcium or lithium hydroxide are highly alkaline. Despite this, they rarely cause severe injury or sequelae; thus, treatment is largely conservative with overnight observation and management.4
Acids, in contrast to alkali substances, have a poor taste and are irritating, which may lead to a child's choking and gagging. This may predispose the patient to aspirate the caustic material, with subsequent airway compromise.1,4,9 Examples of acids in commercial products include hydrochloric acid, sulfuric acid, and silver nitrate.4,11 They are found in toilet bowl cleaners, swimming pool cleaners, and rust removers.4
Acids are conventionally thought to cause coagulation necrosis that forms an eschar, preventing deep tissue penetration.1,4,11 This eschar is thought to decrease the rate of esophageal burn, though pooling of these agents in the stomach is thought to predispose patients to gastric perforation and stricture.1,9 One recent caustic ingestion series from Israel3 questions this protective eschar theory, showing increased rates of esophageal perforation in patients who ingested acid.
Bleaches such as chloride bleach, peroxide, and mildew remover are also considered caustic esophageal irritants, though pH is typically neutral in commercial preparations.1,5,9 Because of the low concentrations and the neutral pH, bleaches do not cause extensive esophageal damage, though they may cause laryngeal edema and airway compromise in the short-term setting.1
STAGING AND PATHOPHYSIOLOGY
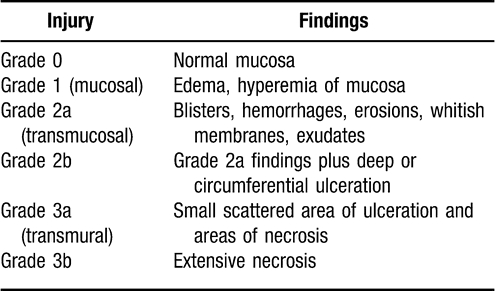
As mentioned above, the esophagus is the site of most long-term sequelae from caustic ingestion. The esophagus is a 10 to 12 cm tube at birth, which increases to from 25 to 30 cm in the adult. It has 3 primary layers. The innermost is the mucosa, consisting of squamous epithelium, lamina propria, and muscularis mucosa. A deeper layer is the submucosa, which consists of fibrous connective tissue with blood vessels, nerves, and numerous mucous glands. Finally, there is a muscular layer divided into inner and outer muscle layers.11 The anatomic layers of the esophagus are of particular importance because most staging systems for injury are based on findings seen on endoscopy that correlate with the depth of injury (see Table 2). Multiple staging systems for injuries are described in the literature, with older systems characterizing injury severity according to different degrees, similar to that used for burns of the skin. The system shown in Table 2 correlates findings seen on endoscopy. Eighty percent of patients with grade 3 burns develop stricture, while only one third of those with grade 2 burns will eventually develop stenosis.7
Table 2.
Injury Staging
Injury to the esophagus is rapid, as described above, for both acids and alkalis, but this acute tissue disintegration and deep tissue penetration may continue for hours.1 Injury progresses within the first week after ingestion, with inflammation and vascular thrombosis. A developing ulcer with fibrin crust will be seen in a few days. Granulation tissue develops between 2 to 4 days and is revealed under shed necrotic tissue by days 15 to 20. This is clinically relevant to healing because collagen deposition may not begin until the second week after injury; thus, the healing tissue will be less strong. This weakness may increase risk during endoscopy performed between 5 to 15 days after injury and may predispose the esophagus to spontaneous rupture during this period.4,14
PRESENTATION AND TREATMENT
After caustic ingestion, patients may present with a combination of many symptoms or none at all depending on the nature of the agent, the specifics of the ingestion (quantity, intent, timing), and what tissues were affected. Patients may have obvious burns to the lips, mouth, and oropharyx. The presence or absence of these lesions does not correlate with the presence of injury to the esophagus or stomach.1,5 Patients with significant laryngeal or epiglottic edema may present with stridor, aphonia, hoarseness, or dyspnea.1 More nonspecific presenting symptoms include nausea, recurrent emesis, hematemesis, dysphagia, odynophagia, and drooling. The presence of abdominal pain or rigidity as well as substernal/chest or back pain may be a sign of severe burn or perforation.1,5,11 Some authors10,14 claim that presentation with 2 or more symptoms may suggest esophageal injury, but there is no 100% accurate sign or group of symptoms that indicates esophageal injury.
The adequacy of the patient's airway must first be addressed. Fiberoptic laryngoscopy can be useful in this regard. If the airway is unstable, intubation under direct visualization is required. “Blind” intubation can lead to bleeding and additional injury and make additional attempts more difficult. If it is impossible to secure the airway through intubation, a surgical airway may be required.1,4,5 When the airway is secured, a thorough physical examination should be completed and a thorough history taken, with particular attention to the timing of the ingestion, identity of the agent, and amount ingested.1,4,5,9 Chest and abdominal radiographs should be obtained to detect free air in the mediastinum (esophageal perforation) or under the diaphragm (gastric perforation) as well as to provide a baseline if aspiration pneumonia develops.5 Furthermore, oral food and fluids should be withheld from the patient, who should, however, receive aggressive hydration. Laboratory results and vital signs should be assessed for signs of acidosis and shock. Induction of emesis should be avoided to prevent further injury as the agent is vomited.11 Neutralization of the caustic material should be avoided because of the potential for causing an exothermic injury, which may worsen an existing injury.1 When the patient is stable, the pH of any unknown liquid or agent should be obtained, and the poison control center should be contacted.4,5,9
Multiple modalities exist to assess the extent of injury to the esophagus, including barium esophagram, technetium-labeled sucralfate, and endoscopy.1 Barium esophagram assesses mild to moderate esophageal burns with a 30% to 60% false-negative rate and is therefore of little use in the short-term setting.1 It is, however, quite useful for following the development of late complications and strictures. Technetium-labeled sucralfate swallow has high sensitivity and specificity but limited ability to show extent of injury. Endoscopy, specifically flexible esophagoscopy, is the most effective method for visualizing the extent of esophageal injury.4 Rigid esophagoscopy may be used but should not be extended beyond the site of caustic burn because of an increased risk of perforation. The flexible endoscope may be advanced past a site of mild injury but should only be stopped at the site of circumferential grade 2 or 3 burns.1,7 Additionally, the flexible esophagoscope provides important information about the stomach and duodenum. Rigid endoscopy is recommended for nasogastric tube placement and airway management.1
The timing of endoscopy and the circumstances for its use, as recommended in the literature, are controversial. In the past, there was a tendency to wait at least 24 hours to allow time for the injury to mature.5 Most authors4,7 are recommending earlier endoscopy and suggesting a wait of only 12 hours and a total wait of no more than 24 hours after ingestion for early assessment and treatment. Endoscopy past 48 hours is discouraged because of progressive wall weakening and increased risk of perforation.1 Most agree that strong alkali ingestion mandates endoscopy, while asymptomatic or questionable ingestions may be observed, according to some sources.1,4
Treatment schemes for caustic injuries vary and no consensus exists. Multiple protocols have been formulated on the basis of documented success in preventing impending complications, though a paucity of randomized trials have assessed any of these interventions. Nasogastric tube placement under endoscopic guidance has been suggested for grade 2b and 3 injuries to stent the injured area and to provide nutritional support.2 Stent placement has shown success in some series,6 though timing and type vary. Stents should be left in place for 14 to 21 days to allow for epithelization.4 Early dilation has been proposed, but has been found to increase rate of perforation.8 Regardless of the intervention, pain control is essential. Antibiotics are often used and have been shown to increase epithelization in animal models though they do not change stricture formation rate or infection rate in numerous series.1,4 Antacids decrease pepsin and acid exposure, which may delay healing of the esophagus, though again, rigorous trials are lacking. Larythrogenic drugs, such as N-acetylcysteine and penicillamine, and mitomycin, an antibiotic and antineoplastic agent, decrease rate of collagen crosslinking and inhibit protein synthesis, respectively, and decrease scarring and stricture formation in animal models.1,5 Data from human trials are lacking.4
Steroids have been a controversial treatment since they were first shown to decrease granulation and stricture formation in animal models.4 Some prospective and retrospective reports have shown that steroids decrease stricture formation in grade 2 injuries in humans.1,9,10 Recent meta-analyses have revealed conflicting results. One recent analysis in 2005 included a total of 10 studies15 in which 572 patients showed no decreased incidence of stricture, with steroids used for second and third-degree (grade 2 and grade 3) burns. In contrast, a meta-analysis of 362 children showed a 40% rate of stricture in the no-steroid group versus a 19% rate of stricture in the steroid-treated group.14
The landmark randomized trial by Anderson et al2 found no difference in the incidence of stricture formation with the use of steroids, though the number of patients in the study was relatively low. A definitive study on the value of steroids is lacking but, if used, most resources suggest the concurrent use of antibiotics.2,4,7 Dosing is controversial and recommendations vary widely.1,8 Side effects of steroids, especially vulnerability to infection, should be considered.2
CASE REPORT
The following case highlights the complexities of treating patients who experience caustic ingestion.
A 2-year-old boy presented to a local hospital after ingesting an unknown amount of hair and grease remover. The patient's past medical and surgical history were unremarkable. The patient underwent intubation at the outside emergency department because of respiratory distress and was transferred to our facility. He had obvious burns to the lips and mouth, though not severe. The patient received flexible endoscopy within the 24 hours following injury. He was found to have erythema and small ulcerations in both the esophagus and stomach. His injuries were deemed grade 2a.
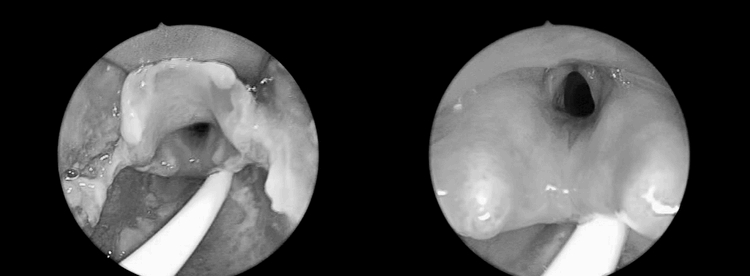
The patient received a nasogastric tube over a guide wire and was given multiple broad spectrum antibiotics without steroids. Our service was consulted to evaluate the patient's upper airway to assess if the patient could be extubated on posttrauma day 4 (Figure 1). As can be seen, the patient's upper airway was grossly edematous with white exudates (grade 2) and we recommended the patient remain intubated. Tube feedings were started and the patient remained afebrile. The patient was finally extubated on posttrauma day 11 after a repeated laryngoscopy/bronchoscopy (Figure 2).
Figure 1. Endoscopic view of the epiglottis and vocal cords 4 days after ingestion.
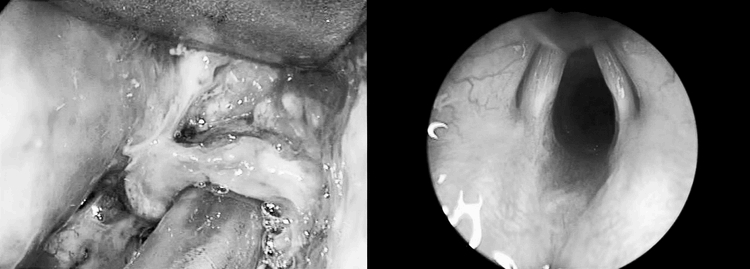
Figure 2. Endoscopic view of the epiglottis and vocal cords 11 days after ingestion.
After extubation the patient had persistent difficulty with secretions. A barium swallow on day 12 revealed mild irregularity and narrowing of the proximal esophagus with normal distention. Most importantly, there was no evidence of a perforation. The patient never tolerated oral intake. He had repeated endoscopy on day 14 with replacement of the nasogastric tube that had been previously removed.
On day 19, during a planned open jejunostomy tube placement, the patient was found to have a walled off area of gastronecrosis and perforation. Throughout his previous stay at the pediatric intensive care unit, he had remained afebrile. The patient's clinical course remained complicated. He was found to have a stricture involving from 15 to 25 cm of his esophagus, and balloon dilations were performed under fluoroscopic guidance 32 days after his initial injury.
This case highlights the unpredictability of these injuries. This is made most apparent by the gastric perforation despite only low-grade findings on initial endoscopy. Furthermore, the patient had a relatively unremarkable barium swallow; yet, he developed an extensive stricture, which currently still requires dilations, despite all the efforts (antibiotics, nasogastric tube, endoscopies) taken by the team providing his medical care. Although the indications and descriptions of standard of care are useful, the unpredictable nature of these injuries continues to trump expectations for patient outcomes and for complications.
COMPLICATIONS
As evidenced by the above case, complications can occur even in “low-grade” injuries, though most long-term sequelae are seen in injuries that are more severe. Esophageal stricture may be seen as early as 3 weeks after ingestion.2,15 It occurs in 10% to 20% of caustic injuries, most commonly at the level of the cricoid cartilage, the region of the aortic arch, and below the left main stem bronchus, as well as the esophageal hiatus, all of which are anatomic regions of narrowing in the esophagus.1,11 Stricture can lead to severe dysphagia, with approximately 80% of strictures causing obstructive symptoms 2 months after their formation.8 Of children ingesting alkalis, 30% will develop esophageal burns; of these, 50% will develop strictures.5 Severe and recalcitrant strictures may require esophageal replacement with colon or jejunum interpositional grafts, while less severe strictures are managed with dilation.1,2,5,11,15 Balloon dilation is the procedure of choice for management of most strictures in children.4 The literature suggests a baseline barium esophagram 3 to 4 weeks after ingestion to establish baseline for future stricture formation.1 Complications of stricture include nutritional compromise, hospitalization, chronic anemia, and repeated dilations.1
Other sequelae may occur that require surgical management. Perforation of the esophagus can lead to tracheoesophageal fistula, mediastinitis, pneumonia, and sepsis, requiring immediate esophagectomy with resultant cervical esophagostomy and gastrostomy.1,4,9,11 Perforation of the stomach or duodenum may lead to peritonitis, shock, and death.4 Such injuries require surgical interventions such as exploratory laparotomy.4,5 Burns to the larynx result in airway loss and strictures; treatment includes tracheostomy and further reconstructive surgeries.16 Some authors1 suggest early reconstruction for grade 3 and some grade 2 injuries to prevent stricture and perforation complications.
Mortality and morbidity for caustic ingestion is most severe for extensive injuries. Transmural burns to the esophagus may be associated with up to 20% mortality.1,9 Injury and stricture formation predispose to esophageal carcinoma, with an estimated increase in risk by a factor of 1000, which continues for 10 to 25 years after injury and requires careful follow-up.1,4,11 Routine screening, however, is not currently recommended.10 Morbid functional complications include nasopharyngeal reflux, hypopharyngeal and laryngeal stenosis, and tongue fixation.1
CONCLUSION
The epidemiology and pathophysiology of caustic ingestion has been thoroughly described in the literature. Despite this, medical teams continue to have difficulty managing the injuries and complications created by this problem. The current available treatment options strive to treat immediate injury and prevent later complications.
Our hope is that this review of literature and this case report demonstrate the unpredictable nature of these injuries as well as the need for more definitive research into treatment. More importantly, we hope it shows the need for treating caustic ingestion on a case by case basis, with great attention given to even low-grade injuries because of the devastating complications that can occur.
REFERENCES
- Schaffer S. B., Hebert A. F. Caustic ingestion. J La State Med Soc. 2000;152(12):590–596. [PubMed] [Google Scholar]
- Anderson K. D., Rouse T. M., Randolph J. G. A controlled trial of corticosteroids in children with corrosive injury of the esophagus. N Engl J Med. 1990;323(10):637–640. doi: 10.1056/NEJM199009063231004. [DOI] [PubMed] [Google Scholar]
- Arévalo-Silva C., Eliashar R., Wohlgelernter J., Elidan J., Gross M. Ingestion of caustic substances: a 15-year experience. Laryngoscope. 2006;116(8):1422–1426. doi: 10.1097/01.mlg.0000225376.83670.4d. [DOI] [PubMed] [Google Scholar]
- Browne J., Thompson J. Caustic ingestion. In: Cummings C. W., Flint P. W., Haughey B. H., Robbins K. T., Thomas J. R., editors. Cummings Otolaryngology: Head & Neck Surgery. 4th ed. St Louis, MO: Elsevier Mosby; 2005. pp. 4330–4341. [Google Scholar]
- Browne J., Thompson J. Caustic ingestion. In: Bluestone C. D., Stool S. E., Kenna M. A., editors. Pediatric Otolaryngology. 4th ed. Philadelphia, PA: WB Saunders Co; 2003. pp. 4330–4342. [Google Scholar]
- Atabek C., Surer I., Demirbag S., Caliskan B., Ozturk H., Cetinkursun S. Increasing tendency in caustic esophageal burns and long-term polytetrafluorethylene stenting in severe cases: 10 years experience. J Pediatr Surg. 2007;42(4):636–640. doi: 10.1016/j.jpedsurg.2006.12.012. [DOI] [PubMed] [Google Scholar]
- Triadefilopolulos G. Caustic ingestion in adults. UpToDate. Available at: www.uptodate.com. Accessed on December 10, 2008.
- Ferry G. D. Caustic esophageal injury in children. UpToDate. January 2008. Available at: www.uptodate.com. Accessed December 15, 2008.
- Friedman E. M. Caustic ingestion and foreign bodies in the aerodigestive tract. In: Bailey B. J., Johnson J. T., Newlands S. D., editors. Head and Neck Surgery—Otolaryngology. 4th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2006. pp. 925–932. [Google Scholar]
- Salzman M., O'Malley R. N. Updates on the evaluation and management of caustic exposures. Emerg Med Clin North Am. 2007;25(2):459–476. doi: 10.1016/j.emc.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Espinola T., Amedee R. Caustic ingestion and esophageal injury. J La State Med Soc. 1993;145(4):121–125. [PubMed] [Google Scholar]
- Mattos G. M., Lopes D. D., Mamede R. C., Ricz H., Mello-Filho F. V., Neto J. B. Effects of time of contact and concentration of caustic agent on generation of injuries. Laryngogscope. 2006;116(3):456–460. doi: 10.1097/01.mlg.0000199935.74009.60. [DOI] [PubMed] [Google Scholar]
- Bertinelli A., Hamill J., Mahadevan M., Miles F. Serious injury from dishwasher powder ingestions in small children. J Paediatr Child Health. 2006;42(3):129–133. doi: 10.1111/j.1440-1754.2006.00811.x. [DOI] [PubMed] [Google Scholar]
- Ramasamy K., Gumaste V. V. Corrosive ingestion in adults. J Clin Gastroenterol. 2003;37(2):119–124. doi: 10.1097/00004836-200308000-00005. [DOI] [PubMed] [Google Scholar]
- Pelclova D., Navratil T. Do corticosteroids prevent oesophageal stricture after corrosive ingestion? Toxicol Rev. 2005;24(2):125–129. doi: 10.2165/00139709-200524020-00006. [DOI] [PubMed] [Google Scholar]
- Ryan F., Witherow H., Mirza J., Ayliffe P. The oral implications of caustic soda ingestion in children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(1):29–34. doi: 10.1016/j.tripleo.2005.04.025. [DOI] [PubMed] [Google Scholar]


