Abstract
Objective: The purpose of this study was to determine if dilation and curettage has an effect on future pregnancy outcome.
Methods: Retrospective review of the electronic medical records of all patients who underwent D&C between January 1, 2002, and December 31, 2006, was performed. Patients who had one or more subsequent pregnancies were selected and evaluated for pregnancy outcome. Frequency and incidence of subsequent pregnancy complications were determined by Chi square and Fisher's exact tests and compared to reported statistics.
Results: The incidence of postpartum hemorrhage was significantly higher than previously reported averages (p < 0.0004). We found no difference in the incidence of preterm delivery, preeclampsia, placental abruption, malpresentation, cervical incompetence, first trimester bleeding, and miscarriage when compared with previously reported data. Pregnancy outcomes among patients with a history of cervical dilation and those without were not significantly different.
Conclusion: The current study suggests that dilation and curettage may predispose to postpartum hemorrhage. It is important to consider the effects of surgical management for miscarriage on future pregnancy outcomes.
Keywords: Abortion, curettage, dilation, miscarriage
Introduction
Up to 20% of pregnancies result in spontaneous abortion (1). Dilation and curettage (D&C) has been the traditional treatment throughout most of the 20th and 21st centuries (2). Recently, however, the practice of performing immediate surgical evacuation in stable patients has been questioned due to the risks of the procedure, and due to the success of medical and expectant management. In addition to uterine perforation, hemorrhage, and pelvic infection, D&C with rigid dilators has been associated with cervical trauma (3).
Review of the literature regarding the effect of induced abortion on late pregnancy outcomes yields conflicting results. Some studies have suggested that dilation and curettage may predispose to negative future pregnancy outcomes, including higher rates of spontaneous abortion, incompetent cervix, preterm labor, preterm rupture of membranes, early neonatal death, and ectopic pregnancy (4). Multiple dilation and curettage procedures have even been associated with first trimester bleeding, abnormal presentations, placenta abruption, fetal distress, low birth weight, short gestation, and major malformations in subsequent pregnancies (5). The World Health Organization (WHO) in 1979 reported that second trimester spontaneous pregnancy loss was more common in women who had a history of induced abortion compared to primigravid women (6). Other studies concluded that second trimester dilation and evacuation (D&E) was not a risk factor for midtrimester pregnancy loss or spontaneous preterm birth (6). Overall, few studies are available pertaining to the effect of dilation and curettage on future pregnancy outcome, and it is questionable whether existing studies accounted for all confounding variables, including differences in medical history and demographics.
Expectant management has been shown to be successful in 82%–96% of women. Medical management is considered safe and effective, with success rates as high as 95% (1),(7).
The objective of this study was to determine if a history of dilation and curettage has an effect on future pregnancy outcome. In particular, we sought to determine whether a history of prior dilation and curettage procedures increases the risk for negative late pregnancy outcomes such as preterm labor, cervical insufficiency, or abnormal bleeding.
Methods
Retrospective review of the electronic medical records of all patients who underwent D&C between January 1, 2002 and December 31, 2006 was performed at Ochsner Hospital by a single physician (J.L.B.). Institutional Review Board approval was obtained. Patients who had one or more subsequent pregnancies were selected for participation in the study and evaluated for pregnancy outcome.
Demographic and obstetric characteristics were collected from patient electronic and paper medical records. The demographic information included maternal age, race, gravida, and parity. Antepartum risk factors were noted such as maternal tobacco use, illicit drug use, history of sexually transmitted diseases, history of abnormal pap smears, and history of cervical procedures. Obstetrical data included approximate gestational age at time of D&C, use of mechanical dilation, number of prior D&C procedures, and subsequent pregnancy information, including prenatal complications, gestational age at delivery, and infant birth weight. Prenatal complications were included if they were mentioned in the clinic or delivery record as a diagnosis.
Chi-square and Fisher's exact tests were used to calculate the frequency and incidence of the following pregnancy complications: preterm delivery, preeclampsia, placental abruption, malpresentation at term, postpartum hemorrhage, incompetent cervix (defined as patients with a history of unexplained second trimester loss or cerclage or both), first trimester bleeding, and/or miscarriage. Data were compared to previously recorded incidences in the literature and texts (1),(8)–(13). Pregnancy outcomes were also compared between patients with a history of mechanical dilation and those without.
Results
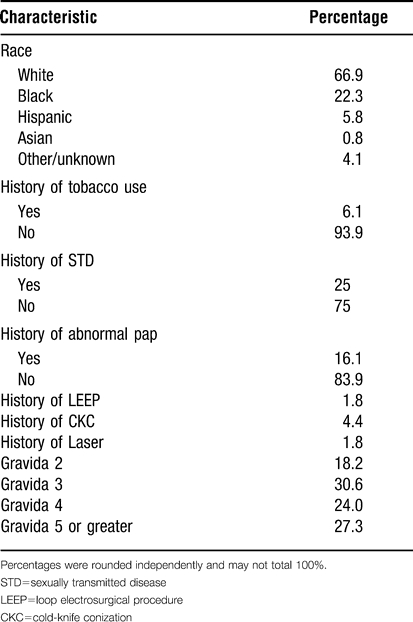
From 411 D&C procedures performed from January 1, 2002 to December 31, 2006, 121 subsequent pregnancies were identified in 99 women. Twin, triplet, and higher-order pregnancies were excluded (n = 7), leaving 114 singleton pregnancies. (Characteristics of study subjects are summarized in Table 1.) The mean gestational age at D&C was 9.23 weeks, ranging from 6–19 weeks. The mean maternal age at D&C was 30.5 years, with the median age 31.25 at time of D&C. The mean maternal age at subsequent delivery was 32.58 years (range 20–45). The median interval from D&C to subsequent delivery was 1.69 years. Of the 99 D&C procedures performed, mechanical dilation was used in 52 (52.52%). No dilation was reported in 41 of the procedures (41.41%). Use of dilation was not confirmed in six (6.06%) of the D&C procedures.
Table 1.
Maternal characteristics.
Of the 114 subsequent pregnancies, 36 (31.58%) had spontaneous vaginal deliveries, one (0.88%) had a vacuum-assisted vaginal delivery, six (5.26%) had forceps-assisted vaginal deliveries, 47 (41.23%) had low transverse cesarean sections, two (1.75%) had classical or low vertical cesarean sections, and 22 (19.30%) aborted before 20 weeks. Ninety two (80.70%) of the pregnancies reached viability. Of the pregnancies reaching viability, 14 (15.22%) delivered before 37 weeks (preterm), and 78 (84.78%) delivered after 37 weeks (term). Of the 92 pregnancies reaching viability, the mean gestational age at delivery was 38.5 weeks (range 30 weeks, 5 days – 41 weeks, 3 days). Excluding seven infants whose birth weight was not available, the mean infant birth weight was 3,308 g, and the median infant birth weight was 3,355 g. Infant birth weights ranged from 1,754 g to 4,760 g.
The frequency and incidence of complications for the 114 subsequent pregnancies is recorded in Table 2. Incidence of pregnancy complications found in the literature is recorded in Table 3.
Table 2.
Frequency and incidence of late pregnancy outcomes (study).
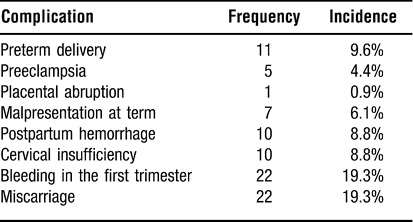
Table 3.
Reported incidence of selected complications.
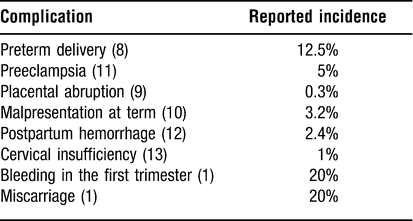
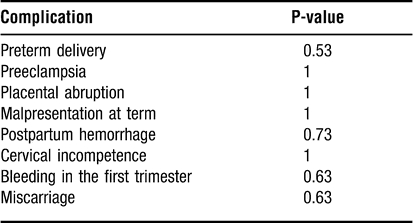
There was a statistically higher incidence of postpartum hemorrhage in our population than previously reported in a large multicenter study (p < 0.0004) (12). We found no statistically significant increase in the incidence of cervical incompetence following D&C. We found no difference in the incidence of preterm delivery, preeclampsia, placental abruption, malpresentation, first trimester bleeding, and miscarriage when compared to overall expected incidences in the literature (1),(8)–(13) (Table 4).
Table 4.
Results of Chi-square or Fisher’s Exact Test comparing incidence of complications among study patients with reported incidences in the literature.
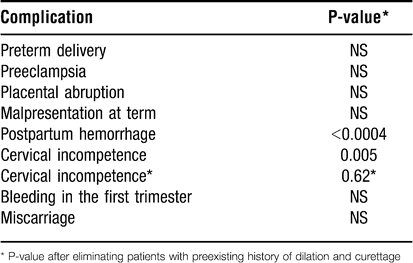
Pregnancy outcomes among patients with a history of cervical dilation did not differ significantly from patients with no history of rigid dilation (Table 5).
Table 5.
Results of Fisher’s Exact Test comparing complications among subsequent pregnancies in women with and without a history of mechanical dilation.
Discussion
The current study suggests that there is a significant increase in postpartum hemorrhage among patients with a history of dilation and curettage. Other studies have also described an increase in abnormal bleeding during pregnancy following a D&C. In a study performed by Harlap and Davies in 1975, women with a history of induced abortion reported an increased frequency of first trimester bleeding compared to women with no prior abortions (14). Linn et al. observed an increase in first trimester bleeding in women with a history of one induced abortion, and an increase in first and third trimester bleeding and placental abruption in women with a history of two or more induced abortions (5). It is known that endomyometrial injury is frequent following D&C; in a study performed by Beuker et al. in 2005, myometrium was observed microscopically among products of conception in 44% and 35% of termination and miscarriage tissues, respectively (15). Levin et al. proposed that curettage itself may increase the risk of subsequent pregnancy loss, and that multiple induced abortions may somehow impair implantation or placentation (16). This study also suggests that uterine curettage may predispose to abnormal bleeding following delivery.
This study does not demonstrate that cervical dilation during D&C predisposes to cervical insufficiency as previously described. Patients with a history of both dilation and curettage had no increase in poor pregnancy outcomes over patients who underwent curettage alone without mechanical dilation. The incidence of cervical incompetence was similar to that reported when patients with preexisting disease were excluded (13). Patients with an incompetent cervix may be at higher risk of requiring a D&C in a subsequent pregnancy secondary to retained placenta or incomplete abortion, which could explain the high incidence of cervical incompetence in this cohort. Other studies have suggested that rigid mechanical dilation, especially above 9 mm, may cause significant cervical trauma. Further research on this topic should be performed to determine at what point dilation becomes significant.
It is important to consider the effects of surgical management for missed and incomplete abortion on future pregnancy outcomes when managing patients. Nonsurgical management is an effective and safe alternative that carries a lower incidence of both short- and medium-term complications in randomized controlled trials (17). A more conservative approach may also decrease healthcare costs due to a reduction in the number of surgical procedures (17). Patient satisfaction should also be considered, and women have expressed high acceptance and satisfaction with conservative management (17). At the least, women should be given the opportunity to choose a treatment option after being informed of all the risks and alternatives. If surgical management is chosen, premedication with cytotec, or preoperative placement of laminaria, could reduce mechanical injury to the cervix and should be considered.
This study has several limitations. First, the sample size was small (n = 114). Second, the study population differs from the general population in terms of demographics. For example, only 33.1% of the patients in the study were nonwhite. Third, the study is retrospective and based on chart review. In addition, a definition of postpartum hemorrhage was not established; patients were determined to have a history of postpartum hemorrhage only if it was mentioned as a diagnosis in their medical record. It is possible that some patients labeled as having a history of postpartum hemorrhage actually did not because a standard definition was not used. Fourth, it is possible that the increased incidence of postpartum hemorrhage in our population is related to the history of spontaneous abortion and not to the actual D&C procedure. A larger, prospective, observational study of patients with a history of first trimester loss with and without D&C may confirm the significance of our findings.
Conclusion
The current study suggests that dilation and curettage may predispose to postpartum hemorrhage. It is important to consider the effects of surgical management for miscarriage on future pregnancy outcomes.
References
- Griebel C. P., Halvorsen J., Golemon T. B., et al. Management of spontaneous abortion. American Family Physician. 2005;72:1243–1250. [PubMed] [Google Scholar]
- Zhang J., Gilles J. M., Barnhart K., et al. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005;353:761–769. doi: 10.1056/NEJMoa044064. [DOI] [PubMed] [Google Scholar]
- Caspi E., Schneider D., Sadovsky G., et al. Diameter of cervical internal os after induction of early abortion by laminaria or rigid dilatation. Am J Obstet Gynecol. 1983;146:106–108. doi: 10.1016/0002-9378(83)90936-5. [DOI] [PubMed] [Google Scholar]
- Madore C., Hawes W. E., Many F., et al. A study on the effects of induced abortion on subsequent pregnancy outcome. Am J Obstet Gynecol. 1981;139:516–521. doi: 10.1016/0002-9378(81)90510-x. [DOI] [PubMed] [Google Scholar]
- Linn S., Schoenbaum S. C., Monson R. R., et al. The relationship between induced abortion and outcome of subsequent pregnancies. Am J Obstet Gynecol. 1983;146:136–140. doi: 10.1016/0002-9378(83)91041-4. [DOI] [PubMed] [Google Scholar]
- Kalish R. B., Chasen S. T., Rosenzweig L. B., et al. Impact of midtrimester dilation and evacuation on subsequent pregnancy outcome. Am J Obstet Gynecol. 2002;187:882–885. doi: 10.1067/mob.2002.127139. [DOI] [PubMed] [Google Scholar]
- Nanda K., Peloggia A., Grimes D., et al. The Cochrane Library, Issue 2, 2007. Oxford: Update Software; Expectant care versus surgical treatment for miscarriage (Cochrane Review) [DOI] [PubMed] [Google Scholar]
- PeriStats. March of Dimes Perinatal Data Center, 2007. http://www.marchofdimes.com/peristats. Accessed 1 May 2007.
- Cunningham F. G., Leveno K. J., Bloom S. L., et al. Obstetrical hemorrhage. In: Cunningham F. G., Leveno K. J., Bloom S. L., et al., editors. Williams Obstetrics, 22nd Edition. New York: McGraw-Hill; 2005. pp. 811–854. [Google Scholar]
- Cunningham F. G., Leveno K. J., Bloom S. L., et al. Normal labor and delivery. In: Cunningham F. G., Leveno K. J., Bloom S. L., et al., editors. Williams Obstetrics, 22nd Edition. New York: McGraw-Hill; 2005. pp. 410–441. [Google Scholar]
- Prevalence and Incidence of Preeclampsia. WrongDiagnosis.com, 2007. http://www.wrongdiagnosis.com/p/preeclampsia/prevalence.htm. Accessed 1 May 2007.
- Lu M., Fridman M., Korst L., et al. Variations in the incidence of postpartum hemorrhage across hospitals in California. Matern Child Health J. 2005;9:297–304. doi: 10.1007/s10995-005-0009-3. [DOI] [PubMed] [Google Scholar]
- Vyas N. A., Vink J. S., Ghidini A., et al. Risk factors for cervical insufficiency after term delivery. Am J Obstet Gynecol. 2006;195:787–791. doi: 10.1016/j.ajog.2006.06.069. [DOI] [PubMed] [Google Scholar]
- Harlap S., Davies A. M. Late sequelae of induced abortion: complications and outcome of pregnancy and labor. Am J Epidemiol. 1975;102:217–224. doi: 10.1093/oxfordjournals.aje.a112150. [DOI] [PubMed] [Google Scholar]
- Beuker J. M., Erwich J. J., Khong T. Y. Is endomyometrial injury during termination of pregnancy or curettage following miscarriage the precursor to placenta accreta? J Clin Pathol. 2005;58:273–275. doi: 10.1136/jcp.2004.020602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin A. A., Schoenbaum S. C., Monson R. R., et al. Association of induced abortion with subsequent pregnancy loss. JAMA. 1980;243:2495–2499. [PubMed] [Google Scholar]
- Tam W. H., Tsui M. H. Y., Lok I. H., et al. Long-term reproductive outcome subsequent to medical versus surgical treatment for miscarriage. Hum Reprod. 2005;20:3355–3359. doi: 10.1093/humrep/dei257. [DOI] [PubMed] [Google Scholar]


