Abstract
Although under-emphasized, substantial evidence indicates that psychological distress, especially depression, hostility, and anxiety, are risk factors for coronary heart disease (CHD) and affect recovery following major coronary heart disease events. We review several major studies from Ochsner Medical Center demonstrating the high prevalence of psychological distress in CHD patients and the marked benefits that occur following formal cardiac rehabilitation and exercise training programs. These benefits include reductions in psychological stress, improvements in CHD risk factors that accompany high stress, and reduced all-cause mortality. These data support the benefits of exercise training and increased levels of fitness to improve psychological stress and subsequent prognosis.
Keywords: Coronary heart disease, depression, exercise, rehabilitation, stress
Introduction
The major established risk factors for coronary heart disease (CHD) include strong family history, diabetes, dyslipidemia, smoking, and hypertension, as well as metabolic syndrome, obesity, and sedentary lifestyle (1). However, substantial additional evidence indicates that conditions of psychological distress, especially depression, hostility, and anxiety, are also significant CHD risk factors and may adversely affect recovery after major CHD events (2)–(10). Although most of the evidence has focused on the high prevalence of depression in patients with CHD, as well as on depression as a CHD risk factor and as a means of predicting prognosis (2)–(7), substantial evidence has also documented that hostility and anxiety may also increase the risk of major CHD events (2),(8)–(10). In fact, a psychosocial index incorporating many of these adverse behavioral factors has recently been demonstrated to be an independent risk factor for the development of acute myocardial infarction (MI) (11)–(12). In addition, these adverse psychological risk factors have been associated with several standard CHD risk factors (dyslipidemia, hypertension, and obesity), as well as increased inflammatory biomarkers that are associated with CHD events, coronary artery calcification, coronary atherosclerosis, and peripheral vascular disease (13). Current evidence indicates that greater emphasis should be placed on psychological risk factors in the prevention and treatment of CHD.
Background
Although the importance of behavioral and psychological risk factors in the pathogenesis and expression of CHD has been somewhat controversial, we believe that most data support the concept that various psychological risk factors, including depression, anxiety, long-term life stress, hostility, or unexpressed anger, contribute significantly to the pathogenesis of atherosclerosis as well as to the development of major CHD events (Figure 1) (2). As mentioned above, most of the early evidence focused on depression as a significant risk factor, as well as on the poor recovery from depression in CHD patients following major clinical events (2)–(7). However, other psychological factors may also be important (2),(8)–(13). Friedman and Rosenman (14) defined persons who exhibit an emotional syndrome characterized by continuous harrying sense of time, urgency, ambitiousness, aggressiveness, competitive drive, and easily aroused free-floating hostility as having type A behavior, and some studies have demonstrated up to a 4-fold increase in the incidence of major CHD events in these patients (13),(15)–(17). Recently, researchers have focused on the risk of hostility in CHD patients (8), especially younger patients (9), and this psychological risk factor has been linked with metabolic syndrome (MS) and increased risk of mortality (13),(18)–(21). The role of anxiety has probably been the most controversial, although several large-scale studies have suggested a link between anxiety and overall mortality, especially in sudden cardiac death (2),(10),(13). Recently, a large study from Boston demonstrated that a high level of anxiety in CHD patients constituted a strong risk factor for the risk of MI or death (21). In addition, the INTERHEART study, which included nearly 30,000 subjects from over 50 countries, found that psychosocial factors were strong independent risk factors for the development of MI, composing nearly one-third of the population's attributable risk for MI (11)–(12).
Figure 1.
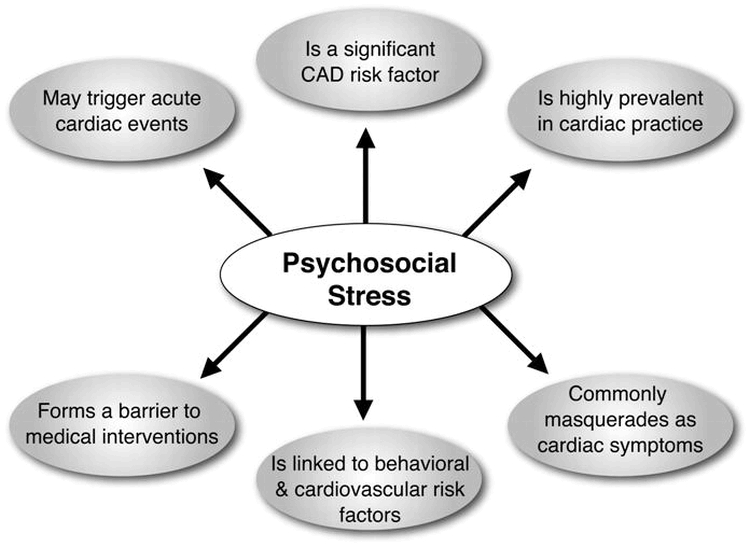
Several reasons that promote interest in the evaluation and treatment of psychosocial stress in medical practices. CAD = coronary artery disease. Adapted with permission from Rozanski A, Blumenthal JA, Davidson KW, et al. J Am Coll Cardiol 2005;45:637–651.
Cardiac Rehabilitation and Exercise Training (CRET)
We and others have published the numerous benefits gained when following the formal, phase II CRET programs in the secondary prevention of CHD (22)–(37). These benefits include marked improvements in exercise capacity and levels of fitness, reductions in obesity indices and risk factors for MS, improvements in plasma lipids (especially high-density lipoprotein cholesterol or HDL-C and triglycerides), inflammation, homocysteine, blood rheology, autonomic function, and parameters of ventricular repolarization dispersion (and, theoretically, the risk of malignant ventricular dysrhythmias). In addition, our CRET studies have also demonstrated that this therapy results in marked improvements in behavioral and psychosocial factors, as well as overall health-related quality of life (QoL) (3)–(10),(13),(38).
Review of Ochsner Studies
Over the past 15 years, we have performed numerous studies assessing behavioral factors with the Kellner Symptom Questionnaire, in which patients respond to 92 questions about how they have felt during the past week, using a yes/no format; this questionnaire has been validated to assess depression, hostility, somatization, and total psychological distress (39)–(40). In addition, our patients have answered the Medical Outcomes Study (MOS) Short Form, which is comprised of 36 short questions, and is validated for total QoL, as well as several individual components (mental health, energy, fatigue, general health, bodily pain, well-being, and functional status) (41).
Over a decade ago, we studied 338 consecutive CHD patients following major CHD events and found that 20% met criteria for depression prior to CRET, and that this percentage dropped dramatically to 12% following the implementation of the CRET program (3). During the same year, we demonstrated that patients with diabetes had a significantly higher prevalence of depression (26% versus 14%) compared with patients without diabetes, yet following the use of the CRET program, both groups had a prevalence of depression of only 9% (4). In a large cohort of 268 elderly ≥65 years of age, the prevalence of depression prior to CRET was 18% and fell to 8% following the CRET program (5). Women have a slightly higher prevalence of depression compared with men (23% versus 18%), and in women the prevalence dropped to 12% following CRET (6). We have demonstrated similar effects of CRET in cohorts of elderly women (7).
In a study of 500 consecutive patients, we demonstrated that hostility was present in 13% of our CHD patients prior to CRET, which fell to only 8% following the formal CRET program (8). Subsequently, we demonstrated that patients <50 years of age had a prevalence of hostility of 28% compared with only 8% prevalence in those ≥65 years; following CRET, the prevalence fell to 15% and 4%, respectively, in the younger and older patients (9).
In another study of 500 patients with CHD, we demonstrated that the prevalence of anxiety was 44%, 20%, and 24%, in patients <55 years (n = 121), 55–70 years (n = 232) and those >70 years (n = 147), respectively (10). Following CRET, the entire cohort had a 56% reduction in the prevalence of anxiety and a nearly 70% reduction in the prevalence of severe anxiety.
Most recently, we studied a large cohort of 635 consecutive patients and specifically compared 104 patients <55 years (mean age 48 +/−6 years) and 260 patients ≥70 years (mean age 75 +/−3 years) to determine the prevalence of psychological risk factors as well as the response to CRET (Figure 2) (13). We demonstrated that depression was slightly more prevalent in the younger cohort (23% versus 19%, p = NS), and that younger patients had a much higher prevalence of anxiety (28% versus 14%; p <0.01) and hostility (13% versus 5%; p <0.01). Following CRET, both younger and older cohorts of patients had marked improvements in depression, hostility, and anxiety (Figures 3–5), but these improvements are even more impressive in the younger patients who had higher baseline prevalence of psychological distress.
Figure 2.
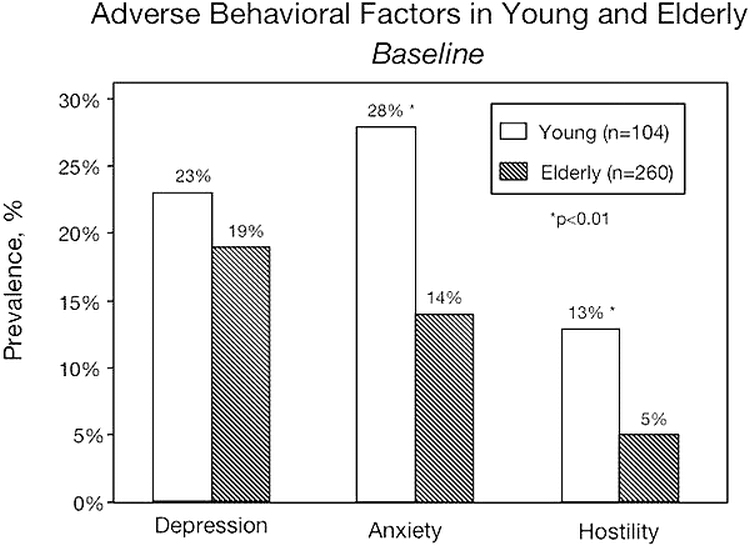
Prevalence of adverse behavioral characteristics in young (mean 48 ± 6 years) and elderly (mean 75 ± 3 years) patients with Coronary Heart Disease. Adapted with permission from Lavie CJ, Milani RV. Arch Intern Med 2006;166:1878–1883.
Figure 3.
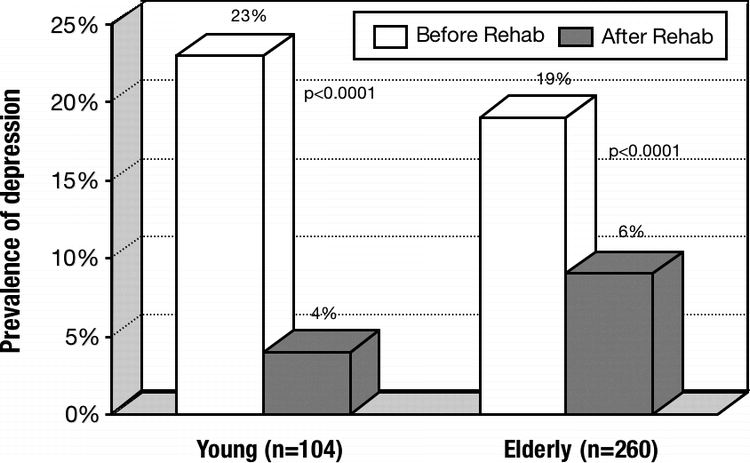
Prevalence of depression before and after rehabilitation in younger and elderly Coronary Heart Disease patients. Data from Lavie CJ, Milani RV. Arch Intern Med 2006;166:1878–1883.
Figure 4.
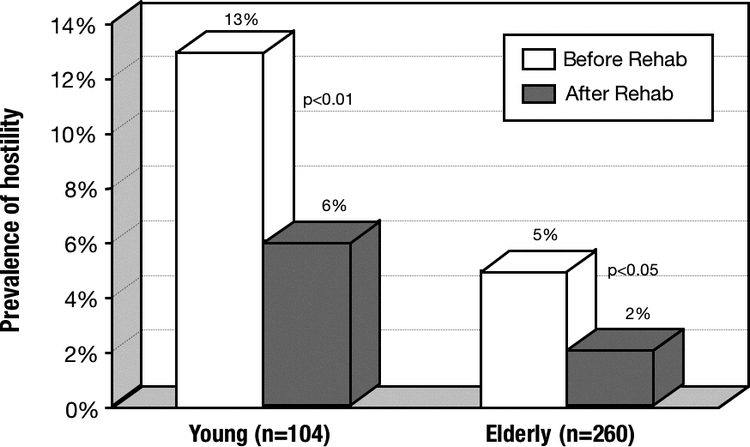
Prevalence of hostility before and after rehabilitation in young and elderly Coronary Heart Disease patients. Data from Lavie CJ, Milani RV. Arch Intern Med 2006;166:1878–1883.
Figure 5.
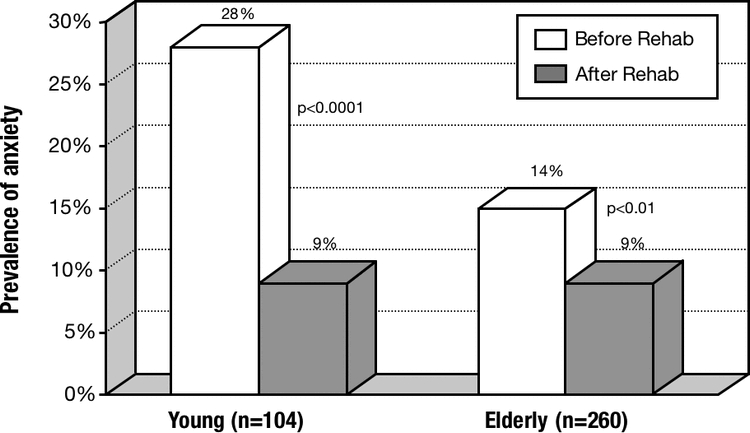
Prevalence of anxiety before and after rehabilitation in young and elderly Coronary Heart Disease patients. Data from Lavie CJ, Milani RV. Arch Intern Med 2006;166:1878–1883.
Recently, we also assessed 500 consecutive patients before and after CRET and utilized a composite Kellner score of Psychological Distress (combined score of depression, hostility, anxiety, and somatization) to compare the highest quintile with the lowest quintile (42). We demonstrated that patients with high distress (HD) were younger and had higher weight, body mass indices, triglycerides, and glycosylated hemoglobin, but had lower levels of exercise capacity and fitness, HDL-C, and total QoL, as well as all six major components of QoL, compared with those with low distress (LD). Following CRET, however, the patients with HD had significant improvements in obesity indices, exercise capacity, HDL-C, and total QoL (and the six components), as well as all four components of distress. Moreover, their improvements were similar to or even greater than those noted in patients with LD, further demonstrating the benefits of CRET in patients with more psychological distress.
Depression and Mortality
Prior studies have demonstrated the increased risk associated with high levels of psychological distress, particularly depression (2)–(7). In a recent study of 522 patients who took part in CRET and 179 patients who did not take part in CRET and served as controls, we noted a 17% prevalence of depression at baseline that fell to 6% following CRET (38). Most importantly, however, those patients who remained depressed following CRET had a 4-fold higher mortality (22% versus 5%; p <0.001) than those who were non-depressed following CRET (Figure 6) (38). Moreover, the control depressed group had a 30% mortality during a mean 3.5-year follow-up compared with an only 8% (p <0.001) mortality in the “active” depressed group who attended CRET (Figure 7). Finally, we noted that those patients who did not improve their exercise capacity maintained a higher prevalence of depression as well as mortality risk, whereas those patients who had either a small or marked improvement in exercise capacity significantly reduced their risk of depression as well as its accompanying high mortality risk (Figure 8). These data suggest that one needs to improve exercise capacity only mildly in order to reduce depression and its high mortality. Although our results were specifically attained in a CHD cohort following major CHD events, we believe that our data are also applicable for depressed patients without known CHD, supporting the potential benefits of exercise training and increased levels of fitness in patients with depression.
Figure 6.
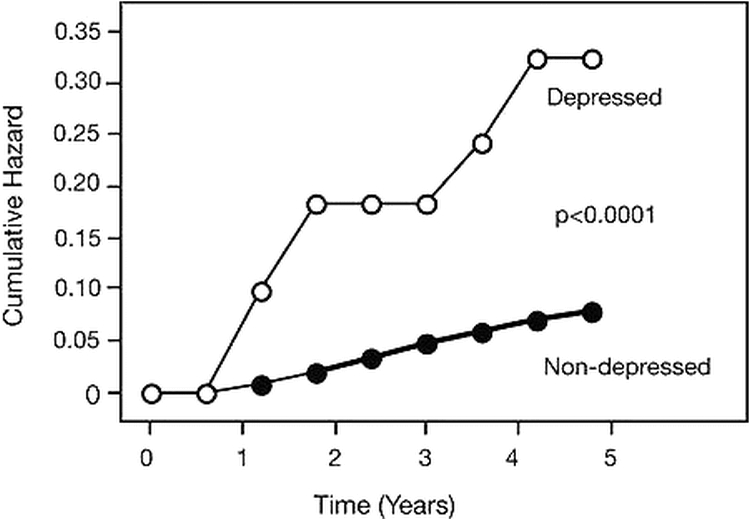
Cumulative hazard curves for mortality in patients who were depressed and non-depressed following formal Cardiac Rehabilitation and Exercise Training. Reproduced with permission from Milani RV, Lavie CJ. Am J Med 2007;120:799–806.
Figure 7.
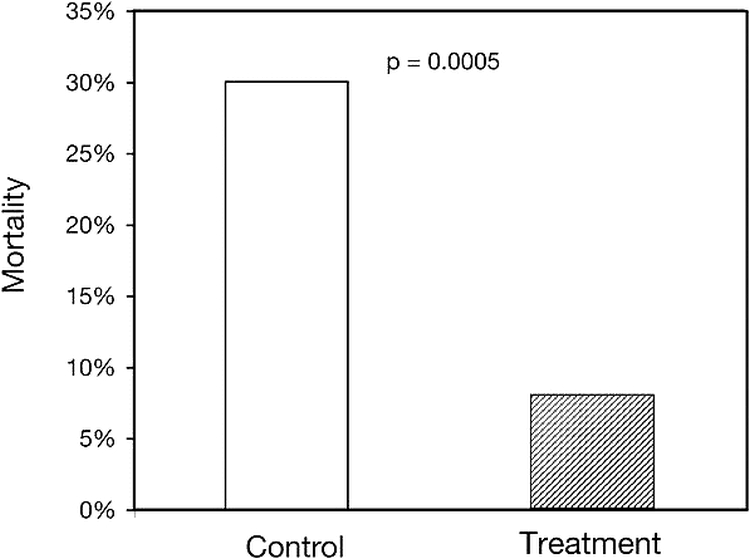
Prevalence of mortality during mean 3.5-year follow-up in control depressed (who did not attend Cardiac Rehabilitation and Exercise Training [CRET]) compared with “active” depressed who attended CRET treatment. Reproduced with permission from Milani RV, Lavie CJ. Am J Med 2007;120:799–806.
Figure 8.
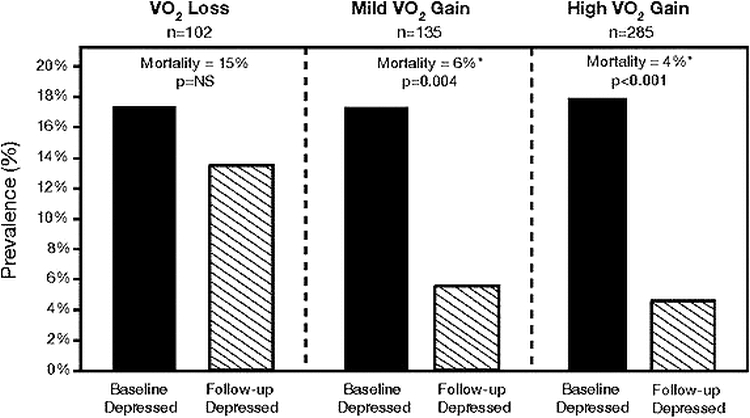
Prevalence of depression and mortality in patients who did not improve exercise capacity (VO2 Loss), those with mild improvements in exercise capacity (Mild VO2 Gain), and those with high improvements in exercise capacity (High VO2 Gain) following Cardiac Rehabilitation and Exercise Training. Reproduced with permission from Milani RV, Lavie CJ. Am J Med 2007;120:799–806.
Conclusion
Numerous studies indicate that psychological risk factors increase the risk of CHD and also affect the impact of recovery following CHD events. We have demonstrated the potential benefits of CRET programs to not only improve most of the established CHD risk factors, but also to dramatically reduce the adverse psychological risk factors, including depression, hostility, anxiety, and total psychological distress, as well as improve QoL in patients with CHD. We believe that our data support the idea that psychological risk factors should be assessed in patients with CHD or high risk; that CRET programs should be routinely utilized as secondary CHD prevention; and, finally, that exercise training and increased levels of fitness should be stressed to improve psychological stress, particularly depression, and to improve the high mortality risk associated with adverse psychological risk.
References
- Lavie C. J., Milani R. V. Cardiac rehabilitation and exercise training programs in metabolic syndrome and diabetes. J Cardiopulm Rehabil. 2005;25:59–66. doi: 10.1097/00008483-200503000-00001. [DOI] [PubMed] [Google Scholar]
- Rozanski A., Blumenthal J. A., Davidson K. W., et al. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637–651. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Milani R. V., Lavie C. J., Cassidy M. M. Effects of cardiac rehabilitation and exercise training programs on depression in patients after major coronary events. Am Heart J. 1996;132:726–732. doi: 10.1016/s0002-8703(96)90304-x. [DOI] [PubMed] [Google Scholar]
- Milani R. V., Lavie C. J. Behavioral differences and effects of cardiac rehabilitation in diabetic patients following cardiac events. Am J Med. 1996;100:517–523. doi: 10.1016/s0002-9343(96)00020-4. [DOI] [PubMed] [Google Scholar]
- Milani R. V., Lavie C. J. Prevalence and effects of cardiac rehabilitation on depression in the elderly with coronary heart disease. Am J Cardiol. 1998;81:1233–1236. doi: 10.1016/s0002-9149(98)00121-0. [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V., Cassidy M. M., et al. Effects of cardiac rehabilitation and exercise training programs in women with depression. Am J Cardiol. 1999;83(10):1480–1483. doi: 10.1016/s0002-9149(99)00127-7. [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V. Benefits of cardiac rehabilitation and exercise training in elderly women. Am J Cardiol 1997;79,664–666. [DOI] [PubMed]
- Lavie C. J., Milani R. V. Effects of cardiac rehabilitation and exercise training programs on coronary patients with high levels of hostility. Mayo Clin Proc. 1999;74:959–966. doi: 10.4065/74.10.959. [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V. Prevalence of hostility in young coronary artery disease patients and effects of cardiac rehabilitation and exercise training. Mayo Clin Proc. 2005;80:335–342. doi: 10.4065/80.3.335. [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V. Prevalence of anxiety in coronary patients with improvement following cardiac rehabilitation and exercise training. Am J Cardiol. 2004;93:336–339. doi: 10.1016/j.amjcard.2003.10.015. [DOI] [PubMed] [Google Scholar]
- Yusuf S., Hawken S., Ounpuu S., et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study) : case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- Rosengren A., Hawken S., Ounpuu S., et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V. Adverse psychological and coronary risk profiles in young patients with coronary artery disease and benefits of formal cardiac rehabilitation. Arch Intern Med. 2006;166:1878–1883. doi: 10.1001/archinte.166.17.1878. [DOI] [PubMed] [Google Scholar]
- Friedman M., Rosenman R. H. Association of specific overt behavior pattern with blood and cardiovascular findings; blood cholesterol level, blood clotting time, incidence of arcus senilis, and clinical coronary artery disease. J Am Med Assoc. 1959;169:1286–1296. doi: 10.1001/jama.1959.03000290012005. [DOI] [PubMed] [Google Scholar]
- Haynes S. G., Feinleib M., Kannel W. B. The relationship of psychosocial factors to coronary heart disease in the Framingham Study. III. Eight-year incidence of coronary heart disease. Am J Epidemiol. 1980;111:37–58. doi: 10.1093/oxfordjournals.aje.a112873. [DOI] [PubMed] [Google Scholar]
- Friedman M., Thoresen C. E., Gill J. J., et al. Alteration of type A behavior and its effect on cardiac recurrences in post myocardial infarction patients: summary results of the recurrent coronary prevention project. Am Heart J. 1986;112:653–665. doi: 10.1016/0002-8703(86)90458-8. [DOI] [PubMed] [Google Scholar]
- Barefoot J. C., Dahlstrom W. G., Williams R. B., Jr Hostility, CHD incidence, and total mortality: a 25-year follow-up study of 255 physicians. Psychosom Med. 1983;45:59–63. doi: 10.1097/00006842-198303000-00008. [DOI] [PubMed] [Google Scholar]
- Todaro J. F., Con A., Niaura R., et al. Combined effect of the metabolic syndrome and hostility on the incidence of myocardial infarction (the Normative Aging Study) Am J Cardiol. 2005;96:221–226. doi: 10.1016/j.amjcard.2005.03.049. [DOI] [PubMed] [Google Scholar]
- Boyle S. H., Williams R. B., Mark D. B., et al. Hostility, age, and mortality in a sample of cardiac patients. Am J Cardiol. 2005;96:64–66. doi: 10.1016/j.amjcard.2005.02.046. [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V. Metabolic syndrome, hostility, and cardiac rehabilitation. Am J Cardiol. 2005;96:1615. doi: 10.1016/j.amjcard.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Shibeshi W. A., Young-Xu Y., Blatt C. M. Anxiety worsens prognosis in patients with coronary artery disease. J Am Coll Cardiol. 2007;49:2021–2027. doi: 10.1016/j.jacc.2007.03.007. [DOI] [PubMed] [Google Scholar]
- Milani R. V., Lavie C. J. Prevalence and profile of metabolic syndrome in patients following acute coronary events and effects of therapeutic lifestyle change with cardiac rehabilitation. Am J Cardiol. 2003;92:50–54. doi: 10.1016/s0002-9149(03)00464-8. [DOI] [PubMed] [Google Scholar]
- Ades P. A. Cardiac rehabilitation and secondary prevention of coronary heart disease. N Engl J Med. 2001;345:892–902. doi: 10.1056/NEJMra001529. [DOI] [PubMed] [Google Scholar]
- Pashkow F. J. Issues in contemporary cardiac rehabilitation: a historical perspective. J Am Coll Cardiol. 1993;21:822–834. doi: 10.1016/0735-1097(93)90116-i. [DOI] [PubMed] [Google Scholar]
- Wenger N. K., Froelicher E. D., Smith L. K., et al. Cardiac Rehabilitation: Clinical Practice Guidleine No.17. Rockville, MD: US Department of Health & Human Services; 1995. AHCPR Publication No. 96-0672. [Google Scholar]
- Williams M. A., Ades P. A., Hamm L. F., et al. Clinical evidence for a health benefit from cardiac rehabilitation: an update. Am Heart J. 2006;152:835–841. doi: 10.1016/j.ahj.2006.05.015. [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V. Effects of cardiac rehabilitation and exercise training on exercise capacity, coronary risk factors, behavioral characteristics, and quality of life in women. Am J Cardiol. 1995;75:340–343. doi: 10.1016/s0002-9149(99)80550-5. [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V. Effects of cardiac rehabilitation, exercise training, and weight reduction on exercise capacity, coronary risk factors, behavioral characteristics, and quality of life in obese coronary patients. Am J Cardiol. 1997;79:397–401. doi: 10.1016/s0002-9149(97)89239-9. [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V., Littman A. B. Benefits of cardiac rehabilitation and exercise training in secondary coronary prevention in the elderly. J Am Coll Cardiol. 1993;22:678–683. doi: 10.1016/0735-1097(93)90176-2. [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V. Patients with high baseline exercise capacity benefit from cardiac rehabilitation and exercise training programs. Am Heart J. 1994;128:1105–1109. doi: 10.1016/0002-8703(94)90740-4. [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V. Effects of nonpharmacologic therapy with cardiac rehabilitation and exercise training in patients with low levels of high-density lipoprotein cholesterol. Am J Cardiol. 1996;78:1286–1289. doi: 10.1016/s0002-9149(96)00614-5. [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V. Effects of cardiac rehabilitation and exercise training on low-density lipoprotein cholesterol in patients with hypertriglyceridemia and coronary artery disease. Am J Cardiol. 1994;74:1192–1195. doi: 10.1016/0002-9149(94)90546-0. [DOI] [PubMed] [Google Scholar]
- Milani R. V., Lavie C. J., Mehra M. R. Reduction in C-reactive protein through cardiac rehabilitation and exercise training. J Am Coll Cardiol. 2004;43:1056–1061. doi: 10.1016/j.jacc.2003.10.041. [DOI] [PubMed] [Google Scholar]
- Ali A., Mehra M. R., Lavie C. J., et al. Modulatory impact of cardiac rehabilitation on hyperhomocysteinemia in patients with coronary artery disease and “normal” lipid levels. Am J Cardiol. 1998;82:1543–1545. doi: 10.1016/s0002-9149(98)00710-3. A8. [DOI] [PubMed] [Google Scholar]
- Church T. S., Lavie C. J., Milani R. V., et al. Improvements in blood rheology after cardiac rehabilitation and exercise training in patients with coronary heart disease. Am Heart J. 2002;143:349–355. doi: 10.1067/mhj.2002.119758. [DOI] [PubMed] [Google Scholar]
- Lucini D., Milani R. V., Costantino G., et al. Effects of cardiac rehabilitation and exercise training on autonomic regulation in patients with coronary artery disease. Am Heart J. 2002;143:977–983. doi: 10.1067/mhj.2002.123117. [DOI] [PubMed] [Google Scholar]
- Kalapura T., Lavie C. J., Jaffrani W., et al. Effects of cardiac rehabilitation and exercise training on indexes of dispersion of ventricular repolarization in patients after acute myocardial infarction. Am J Cardiol. 2003;92:292–294. doi: 10.1016/s0002-9149(03)00628-3. [DOI] [PubMed] [Google Scholar]
- Milani R. V., Lavie C. J. Impact of cardiac rehabilitation on depression and its associated mortality. Am J Med. 2007;120:799–806. doi: 10.1016/j.amjmed.2007.03.026. [DOI] [PubMed] [Google Scholar]
- Kellner R. A symptom questionnaire. J Clin Psychiatry. 1987;48:268–274. [PubMed] [Google Scholar]
- Kellner R., Sheffield B. F. A self-rating scale of distress. Psychol Med. 1973;3:88–100. doi: 10.1017/s0033291700046377. [DOI] [PubMed] [Google Scholar]
- Stewart A. L., Greenfield S., Hays R. D., et al. Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA. 1989;262:907–913. Erratum in: JAMA 1989;262:2542. [PubMed] [Google Scholar]
- Artham S. M., Lavie C. J., Milani R. V. Cardiac rehabilitation programs markedly improve high-risk profiles in coronary patients with high psychological distress. South Med J. In press (2007). [DOI] [PubMed]


