Abstract
Background:
Oral anticoagulant therapy (OAT) is used to prevent/treat thromboembolism. Major bleeding is common in patients on OAT; eg, warfarin increases intracranial hemorrhage (ICH) risk.
Case:
A 71-year-old male on warfarin (to reduce stroke risk) presented at Accident and Emergency Minor Injuries Unit with headache after reportedly sounding ‘drunk’. On triage, the patient appeared lucid and well. However, International Normalized Ratio (INR) was 4.1. Head computed tomography (CT) indicated a large right-sided subdural hematoma. Prothrombin complex concentrate (PCC; Beriplex® P/N, CSL Behring) with vitamin K normalized the INR within minutes of administration. The patient underwent neurosurgery without complications, and was discharged after 5 days, with no residual neurological symptoms.
Conclusions:
ICH patients can present with no neurological signs. In OAT patients with headache, INR must be established; if ≥3.0, normalization of INR and head CT are essential. PCC is the best option to rapidly reverse anticoagulation and correct INR pre-surgery.
Keywords: anticoagulation reversal, Beriplex® P/N, computed tomography, International Normalized Ratio, intracranial hemorrhage, prothrombin complex concentrate
Introduction
Oral anticoagulant therapy (OAT) is prescribed to large numbers of patients for the prevention and treatment of thromboembolic disease.1 In 2001, approximately 500,000 people in the UK took OAT; the vitamin K antagonist warfarin was used in the large majority of these patients.2 Warfarin has a narrow therapeutic index; thrombosis risk increases when the International Normalized Ratio (INR) falls below 2.0 and serious bleeding risk increases when the INR rises above 4.0. As a result, major bleeding is a common problem in people taking OAT, occurring at a rate of 2.4%–8.1% per patient-year.3 Intracranial hemorrhage (ICH) is perhaps the most serious complication of OAT; warfarin therapy increases both the likelihood of suffering ICH and the mortality associated with it.4,5 Intracranial hemorrhage associated with OAT can be divided into the following types: intracerebral/intraparenchymal, subdural/epidural (acuteorchronic), and subarachnoid. Intracerebral hemorrhage accounts for around 70% of OAT-associated ICH, with subdural hematoma making up the bulk of the remainder.5,6
Current therapeutic options for reversal of OAT in patients with major hemorrhage are fresh frozen plasma (FFP), prothrombin complex concentrate (PCC; which includes the vitamin-K dependent coagulation factors II, VII, IX and X) and recombinant factor VIIa, administered in combination with vitamin K.7–10 Although FFP is still often used, PCC offers substantial benefits over FFP and is the ‘gold standard’ therapy.11 Whereas PCC can be rapidly prepared and corrects vitamin K antagonist-induced impairment of hemostasis within 30 minutes of administration, FFP must be thawed and large volumes infused, leading to delayed and often inadequate correction of anticoagulation.12–14 PCC also offers safety advantages over FFP, such as virus reduction/inactivation and a low risk of thrombotic events.13,15,16 FFP is associated with transfusion-related lung injury, allergy/anaphylaxis, hemolysis, and bacterial contamination/sepsis.17 A randomized, multicenter, Phase IIIb trial (NCT00803101) is currently evaluating the efficacy and safety of the PCC Beriplex® P/N compared with FFP in patients taking OAT who require emergency surgery or invasive intervention. This study has the proportion of subjects experiencing a rapid decrease in INR as a primary endpoint and is due to complete in mid-2011.
The case described below highlights that even in the absence of neurological signs, a slow-onset headache in a patient taking OAT might indicate underlying ICH. In this scenario, head computed tomography(CT) is required for differential diagnosis, and administration of PCC can rapidly reverse OAT to enable successful neurosurgery.
Case Report
A 71-year-old white British male (weight: 80 kg, height: 178 cm) presented at night to our Accident and Emergency Minor Injuries Unit with a headache. Although the patient felt he was fine, his son reported that he sounded ‘drunk’ in conversation. The patient had been experiencing intermittent ‘waves’ of headache that had slowly worsened over the preceding five days but were not debilitating. He graded the headache as 8/10 at its worst. Simple analgesia helped with the pain initially, but had become less effective. The headache had a slow onset and was focused around both orbits and the frontal area, with no radiation. No nausea, vomiting, changes in vision, systemic symptoms or deterioration of general health were reported. The patient had no history of falls or head injury. On initial triage by a nurse, the patient was speaking in full sentences, did not appear confused and looked well. He was given two tablets of co-codamol (30/500).
The patient’s medical history included atrial fibrillation, hypertension, glaucoma, gastroesophageal reflux, and hypothyroidism. The patient was taking warfarin (4 mg per day) as part of his regular medication to reduce stroke risk associated with atrial fibrillation. Medication history included ranitidine, bendroflumethiazide, diltiazem, levothyroxine, and no known drug allergies. Review of systems and family history were negative. The patient was an ex-smoker (stopped smoking 20 cigarettes per day 10 years ago) and consumed little alcohol. He was living at home with his wife and stated that he was stressed by her recent admittance to our hospital with fast atrial fibrillation.
On examination, the patient’s vital signs were: blood pressure, 138/82 mmHg; heart rate, 82 beats/min (irregular); respiratory rate, 19 breaths/min; temperature, 35.4 °C; and oxygen saturation, 97% (on air). The patient’s chest was clear, with normal breath sounds. Heart sounds (in rate-controlled atrial fibrillation) were also normal, jugular venous pressure was not raised, and there were no signs of heart failure. The abdomen was soft and not tender. Neurological examination showed power was 5/5 in all limbs, with normal tone, sensation and reflexes. Extraocular movements were normal, with direct and indirect pupil reactions bilaterally. Mini-mental state examination score was 10/10. Cerebellar function was normal and there were no obvious signs of an intracranial bleed. Immediately after examination, the patient vomited. This was most likely due to the codeine given for analgesia rather than indicating raised intracranial pressure because the patient had not vomited up to that point and did not vomit again afterwards. However, considering that the patient was normally fit and healthy, had reportedly sounded ‘drunk’, and was taking warfarin, a possible intracranial bleed was suspected.
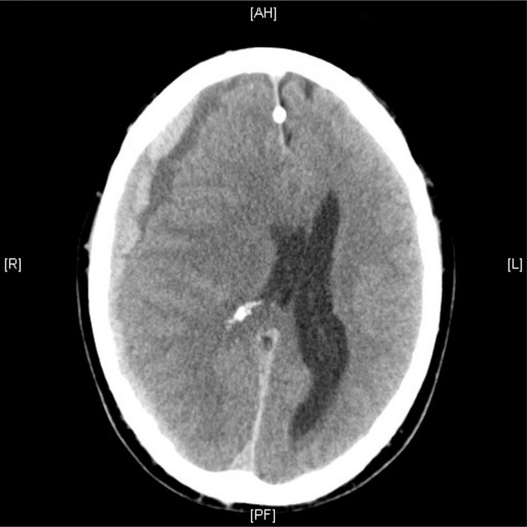
Head CT indicated a large right-sided acute on chronic subdural hematoma (maximum depth, 1.9 cm) occupying the frontal, parietal and temporal convexities, and potentially also a small subarachnoid hemorrhage (Fig. 1). No hydrocephalus or recent infarct were observed. Blood tests at presentation returned an INR of 4.1, a prothrombin time of 51 seconds, and an activated partial thromboplastin time ratio of 1.69.
Figure 1.
Computed tomography indicated a large right-sided acute on chronic subdural hematoma (maximum depth, 1.9 cm) occupying the frontal, parietal and temporal convexities, and a possible small subarachnoid hemorrhage.
Because reversal of warfarin and rapid correction of INR were required before surgery, 10 mg of vitamin K and 40 IU/kg of PCC (Beriplex® P/N; CSL Behring, Marburg, Germany) were administered intravenously. Blood tests subsequently showed an INR of 1.0, at which point the patient underwent emergency transfer to the Neurosurgery Department at King’s College Hospital, London for surgical intervention. The patient was operated on approximately 10 hours after diagnosis of the intracranial bleed and there were no bleeding complications during surgery.
The patient’s outcome was excellent—he was discharged 5 days after surgery, with no residual neurological symptoms apparent.
Discussion
Guidelines from the American College of Emergency Physicians recommend that head CT should be performed in the Emergency Department in patients presenting with a headache if this is accompanied by new abnormal neurological findings or is new, sudden-onset, and severe.18 The case described here, however, demonstrates that patients with large subdural hematomas may present with a slow-onset headache and no neurological symptoms. Without further investigation, such patients might be given analgesic treatment and discharged, with potentially fatal consequences. In patients with a headache who are taking OAT and are therefore at increased risk of major bleeding, it is imperative to establish the INR (even if the patient’s INR record book is up-to-date). If the INR is ≥3.0, the patient should be admitted for normalization of INR and head CT should be performed in order to try and identify a treatable lesion. This is a generalized approach, however, and it is important to be aware that patients with an INR <3.0 may also suffer an ICH. Sound clinical judgment and availability of hospital resources are crucial in delivering effective care on a case-by-case basis.
Before surgery, rapid reduction of the INR is required (normalized INR is ≤1.3). In line with current guidelines, the protocol in our hospital is to use Beriplex® P/N to achieve this and stop bleeding in patients taking OAT. Approximate dosing of Beriplex® P/N can be calculated based on patient bodyweight, the INR before treatment, and the target INR. Resuscitation nurses at our hospital are trained in the administration of Beriplex® P/N—familiarity of nurses and hematology staff with the protocol is key in enabling urgent treatment. Despite this, however, treatment with FFP was initially suggested and approval had to be sought from the on-call hematology consultant before Beriplex® P/N could be given. Once administered, Beriplex® P/N corrected the vitamin K antagonist-induced impairment of hemostasis within minutes, enabling the patient to be transferred and operated on. The neurosurgical team was grateful for our effective pre-transfer care and communication, both being important factors in the successful outcome of this case.
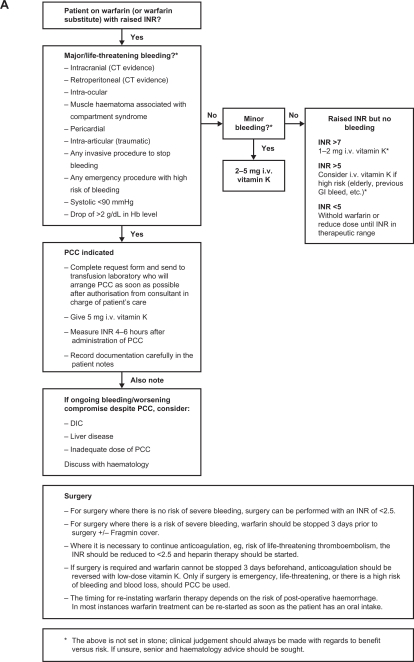
In emergency bleeding situations it is vital that any barriers to early treatment are removed. In this case, administrative barriers prevented earlier use of Beriplex® P/N. This delayed the second INR reading, which is critical for deciding when a patient with major bleeding can be transferred for emergency surgery. Following this case, our hospital implemented a management algorithm to help Accident and Emergency staff in providing PCC for warfarin reversal; this algorithm and the PCC request form are shown in Figure 2. Although this algorithm states to ‘measure INR 4–6 hours after administration of PCC’, it is important to be aware that PCC typically normalizes INR much more quickly than this (ie, within 30 minutes of administration).19 Valuable time could also be saved by training of on-call laboratory staff to accept direct referrals (rather than via the on-call consultant hematologist).
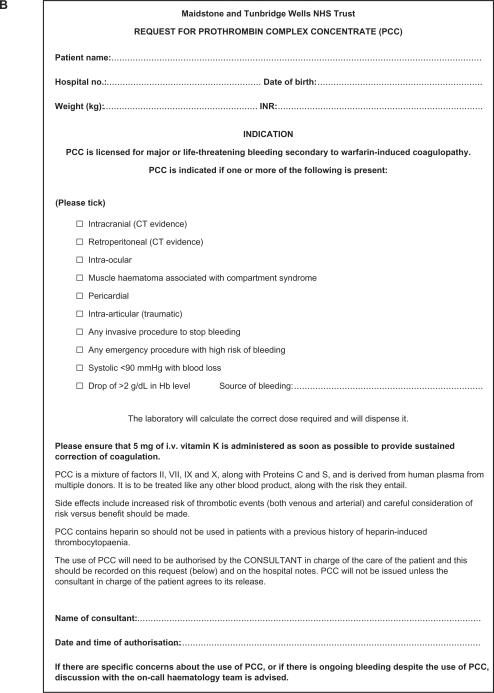
Figure 2.
Management algorithm (A) and prothrombin complex concentrate (PCC) request form (B) implemented at Maidstone and Tunbridge Wells NHS Trust, UK to help Accident and Emergency staff in providing PCC for warfarin reversal.
Abbreviations: CT, computed tomography; DIC, disseminated intravascular coagulation; GI, gastrointestinal; Hb, hemoglobin; INR, International Normalized Ratio; i.v., intravenous; mmHg, millimeters of mercury; NHS, National Health Service; PCC, prothrombin complex concentrate.
Other important factors in enabling early treatment include rapid triage in Accident and Emergency and taking an accurate medical history. The latter is especially important when assessing patients with a headache;18 in this case, ongoing warfarin therapy indicated a possible intracranial bleed. Furthermore, this case highlights the importance of taking a collateral history from a close relative or friend in elderly patients who want to maintain their independence. Neurological evaluation is essential as patients with ICH may decompensate rapidly.
In summary, this case shows that patients with ICH may present with no neurological signs. In patients who are taking OAT, a headache and an elevated INR (≥3.0) might indicate ICH; therefore, normalization of INR and head CT are essential. PCC is widely considered to be the best option for rapid anticoagulation reversal and correction of INR. This enables potentially life-saving neurosurgery to be performed with minimal delay, increasing the likelihood of a positive outcome.
Acknowledgments
The author thanks Meridian HealthComms for editorial assistance provided on behalf of CSL Behring.
Footnotes
Disclosures
Consent was obtained from the patient for publication of this case report. This manuscript has been read and approved by the author. This paper is unique and not under consideration by any other publication and has not been published elsewhere. The author reports no conflicts of interest. The author confirms that they have permission to reproduce any copyrighted material.
References
- 1.Evans G, Luddington R, Baglin T. Beriplex P/N reverses severe warfarin-induced overanticoagulation immediately and completely in patients presenting with major bleeding. Br J Haematol. 2001;115(4):998–1001. doi: 10.1046/j.1365-2141.2001.03214.x. [DOI] [PubMed] [Google Scholar]
- 2.Baglin TP, Cousins D, Keeling DM, Perry DJ, Watson HG. Safety indicators for inpatient and outpatient oral anticoagulant care: [corrected] Recommendations from the British Committee for Standards in Haematology and National Patient Safety Agency. Br J Haematol. 2007;136(1):26–9. doi: 10.1111/j.1365-2141.2006.06379.x. [DOI] [PubMed] [Google Scholar]
- 3.Fitzmaurice DA, Blann AD, Lip GY. Bleeding risks of antithrombotic therapy. BMJ. 2002;325(7368):828–31. doi: 10.1136/bmj.325.7368.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Appelboam R, Thomas EO. Warfarin and intracranial haemorrhage. Blood Rev. 2009;23(1):1–9. doi: 10.1016/j.blre.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 5.Hart RG, Boop BS, Anderson DC. Oral anticoagulants and intracranial hemorrhage. Facts and hypotheses. Stroke. 1995;26(8):1471–7. doi: 10.1161/01.str.26.8.1471. [DOI] [PubMed] [Google Scholar]
- 6.Berwaerts J, Robb OJ, Dykhuizen RS, Webster J. Course, management and outcome of oral-anticoagulant-related intracranial haemorrhages. Scott Med J. 2000;45(4):105–9. doi: 10.1177/003693300004500403. [DOI] [PubMed] [Google Scholar]
- 7.Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133(6 Suppl):160S–98. doi: 10.1378/chest.08-0670. [DOI] [PubMed] [Google Scholar]
- 8.Baglin TP, Keeling DM, Watson HG. Guidelines on oral anticoagulation (warfarin): third edition—2005 update. Br J Haematol. 2006;132(3):277–85. doi: 10.1111/j.1365-2141.2005.05856.x. [DOI] [PubMed] [Google Scholar]
- 9.Hirsh J, Fuster V, Ansell J, Halperin JL. American Heart Association/American College of Cardiology Foundation guide to warfarin therapy. Circulation. 2003;107(12):1692–711. doi: 10.1161/01.CIR.0000063575.17904.4E. [DOI] [PubMed] [Google Scholar]
- 10.Steiner T, Kaste M, Forsting M, et al. Recommendations for the management of intracranial haemorrhage—part I: spontaneous intracerebral haemorrhage. The European Stroke Initiative Writing Committee and the Writing Committee for the EUSI Executive Committee. Cerebrovasc Dis. 2006;22(4):294–316. doi: 10.1159/000094831. [DOI] [PubMed] [Google Scholar]
- 11.Levy JH, Tanaka KA, Dietrich W. Perioperative hemostatic management of patients treated with vitamin K antagonists. Anesthesiology. 2008;109(5):918–26. doi: 10.1097/ALN.0b013e3181895bd8. [DOI] [PubMed] [Google Scholar]
- 12.Lankiewicz MW, Hays J, Friedman KD, Tinkoff G, Blatt PM. Urgent reversal of warfarin with prothrombin complex concentrate. J Thromb Haemost. 2006;4(5):967–70. doi: 10.1111/j.1538-7836.2006.01815.x. [DOI] [PubMed] [Google Scholar]
- 13.Leissinger CA, Blatt PM, Hoots WK, Ewenstein B. Role of prothrombin complex concentrates in reversing warfarin anticoagulation: a review of the literature. Am J Hematol. 2008;83(2):137–43. doi: 10.1002/ajh.21046. [DOI] [PubMed] [Google Scholar]
- 14.Makris M. Optimisation of the prothrombin complex concentrate dose for warfarin reversal. Thrombosis Research. 2005;115(6):451–3. doi: 10.1016/j.thromres.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 15.Samama CM. Prothrombin complex concentrates: a brief review. Eur J Anaesthesiol. 2008;25(10):784–9. doi: 10.1017/S0265021508004675. [DOI] [PubMed] [Google Scholar]
- 16.Vigue B, Ract C, Tremey B, et al. Ultra-rapid management of oral anticoagulant therapy-related surgical intracranial hemorrhage. Intensive Care Med. 2007;33(4):721–5. doi: 10.1007/s00134-007-0528-z. [DOI] [PubMed] [Google Scholar]
- 17.MacLennan S, Williamson LM. Risks of fresh frozen plasma and platelets. J Trauma. 2006;60(6 Suppl):S46–50. doi: 10.1097/01.ta.0000199546.22925.31. [DOI] [PubMed] [Google Scholar]
- 18.Edlow JA, Panagos PD, Godwin SA, Thomas TL, Decker WW. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann Emerg Med. 2008;52(4):407–36. doi: 10.1016/j.annemergmed.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 19.Pabinger-Fasching I. Warfarin-reversal: results of a phase III study with pasteurised, nanofiltrated prothrombin complex concentrate. Thrombosis Research. 2008;122(Suppl 2):S19–22. doi: 10.1016/S0049-3848(08)70005-7. [DOI] [PubMed] [Google Scholar]