Abstract
Objective
This study assessed decisional conflict about invasive prenatal testing among women pregnant after infertility.
Methods
We surveyed 180 pregnant women with a history of infertility using a mixed methods cross-sectional design. Difficulty in deciding whether to have prenatal testing was measured using the Decisional Conflict Scale.
Results
A minority of women (31%) chose to have invasive prenatal testing. Most participants (72%) reported low decisional conflict (score <25; mean = 22.1; standard deviation = 23.2; range: 0–100). Half (53%) of the participants said that infertility made the testing decision easier. Qualitative data suggest that infertility makes the decision easier by clarifying relevant values and priorities. Most infertility characteristics studied were not significantly associated with decisional conflict. Variables associated with higher decisional conflict included infertility distress due to rejection of a childfree lifestyle, disagreement with others about testing, and choosing to have invasive testing after having had treatment for infertility.
Conclusions
For some women, infertility may make the invasive prenatal testing decision easier. Women with the greatest need for decisional support were those who have had treatment and choose invasive testing, who disagree with others about their testing choice, or who are particularly distressed about being childless.
Keywords: prenatal testing, infertility, decisional conflict, decision making, genetic counseling
INTRODUCTION
In the United States, 10 to 15% of couples deal with infertility (Chandra and Stephen, 1998). One-third of these couples eventually achieve a successful pregnancy with treatment, whereas 2 to 5% conceive spontaneously each year (Osmanagaoglu et al., 2002; Schmidt, 2006). Current professional guidelines state that all pregnant women should be offered chorionic villus sampling (CVS) or amniocentesis, regardless of age (American College of Obstetricians and Gynecologists, 2007). This newer recommendation and the increasing incidence of infertility predict that far more pregnant women with a history of infertility will be offered invasive prenatal testing (Abma et al., 1997). Yet there is a paucity of research on making decisions about amniocentesis or CVS after a period of infertility. The available studies address testing uptake and not the process of decision making (Meschede et al., 1998; Monni et al., 1999; Elimian et al., 2003; Geipel et al., 2004).
Existing evidence suggests that a history of infertility is relevant to making a decision about whether to undergo CVS or amniocentesis. When deciding whether to have invasive prenatal testing, women report that they consider how hard it was to get pregnant and how likely it is that they will get pregnant again (Moyer et al., 1999). Many couples with a history of infertility report their pregnancies as precious, scarce, and a final or solitary chance to have a baby (Sandelowski et al., 1991; Covington and Burns, 1999; Hjelmstedt et al., 2003a). Infertile couples also have high anxiety about miscarriage, the health of the baby, and the outcome of the delivery (Reading et al., 1989; McMahon et al., 1997; Bernstein et al., 1994; Hjelmstedt et al., 2003a,b).
Given that these pregnancies are characterized by intense desire and high levels of investment, it may be difficult for formerly infertile couples to consider the possible negative outcomes of invasive prenatal testing: pregnancy loss, diagnosis of a fetal abnormality, and pregnancy termination.
The conflict theory of decision making states that decisions have the potential to be particularly difficult if they are appraised by the decision maker as emotionally laden, time-pressured, irreversible, having potential for significant loss, and requiring individual assessment of potential advantages and disadvantages of different courses of action (Janis and Mann, 1977). Many of these factors are inherent in the invasive prenatal testing decision, particularly in the setting of pregnancy after infertility. Difficulty in making an important decision can be conceptualized as decisional conflict (O'Connor, 1993). Identifying individuals who experience high decisional conflict is valuable because interventions such as genetic counseling, group counseling, decision aids, and decisional analysis can each be used to minimize decisional conflict and enhance informed choice (Drake et al., 1999; Kaiser et al., 2002; Bekker et al., 2004; Hunter et al., 2005).
The primary objective of this study was to assess the levels of decisional conflict associated with deciding whether to undergo invasive prenatal testing among women who conceived after infertility. We also aimed to identify factors related to infertility that predict higher decisional conflict. Our selection of variables was guided by the conflict theory of decision making (Janis and Mann, 1977). Based on past research, we hypothesized that higher levels of decisional conflict would be associated with more severe infertility (e.g. longer duration, need for treatment), lower psychological well-being (e.g. higher infertility-related distress, greater perceived infertility severity), and perceived disagreement with valued others about the testing decision.
METHODS
This was a cross-sectional study with data collected through an online questionnaire. The National Human Genome Research Institute, National Institutes of Health Institutional Review Board approved this study. Participants were women who were currently pregnant and met the following inclusion criteria: self-reported history of infertility, defined as taking more than a year to conceive (American Society for Reproductive Medicine, 2008); first pregnancy after period of infertility; offered and decided whether to have invasive prenatal testing; proficient in written English. Women with children were not excluded. Participants were recruited from websites for pregnancy and pregnancy after infertility.
The questionnaire had 77 multiple choice or Likert scale questions and three open-ended questions, included to supplement the quantitative data with women's perceptions of the impact of their infertility history on their decision making. We developed close-ended questions to measure demographics, medical characteristics of infertility such as treatment history and duration of infertility, and test decision.
Perceived severity of infertility was measured by rating three items: perceived difficulty conceiving relative to other women with infertility, perceived difficulty conceiving relative to women without infertility, and perceived likelihood of conceiving again. Participants rated the items on 7-point Likert scales. Higher scores indicate greater perceived severity.
Infertility-related distress was measured using three subscales of the Fertility Problem Inventory: social concern, rejection of childfree lifestyle, and need for parenthood. (Cronbach's α 0.82, 0.88, and 0.82, respectively) (Newton et al., 1999). Participants rated each item on a 6-point Likert scale. In completing this measure, participants were instructed to reflect back on their period of infertility. Higher scores indicate greater infertility-related distress.
Perceived disagreement with test choice was defined as match (mismatch) between subjective norms and test decision. Subjective norms were measured through a series of questions on the opinions of four referents (husband/partner, other infertile women, infertility doctor, and most people who are important to me) about prenatal testing and motivation to comply with the referent's preference. Participants rated each item on a 5-point Likert scale and responses were summed for each referent. Similar scales have been used to measure subjective norms in other studies (Cronbach's α 0.81) (Kim et al., 2003), including among an infertile population (Callan et al., 1998). Lower subjective norm scores represent a perception that the other person does not want the participant to have prenatal testing. To assess perceived disagreement with test choice, we created an interaction variable that combined the subjective norm score and test choice. For women who chose to have testing, lower subjective norm scores indicate a disagreement; conversely, for women who chose not to have testing, higher subjective norm scores indicate a disagreement.
The outcome variable, decisional conflict, was measured using the decisional uncertainty subscale of the Decisional Conflict Scale (Cronbach's α 0.78) (O'Connor, 1995). The overall scale measures ‘uncertainty, selected factors contributing to the uncertainty, and perceptions of effective decision making’ (O'Connor, 1995). The uncertainty subscale specifically assesses uncertainty about the decision, the key component of our outcome variable. The informed and values clarity subscales of the Decisional Conflict Scale measure modifiable factors that can increase decisional uncertainty. These subscales were used to control for sources of decisional conflict that were beyond our research question: lack of information or unclear values. Items were rated on a 5-point Likert scale. Scores above 25 represent high decisional conflict (O'Connor, 1995).
To isolate the relationship between our independent variables and decisional conflict, we controlled for the effects of other variables that have a known or potential relationship, based on clinical experience, with decisional conflict (O'Connor, 1993). These included demographics, time since decision, gestational age, discussion with health care provider(s) including genetic counseling, indication for invasive prenatal testing, test decision, receipt of test results, and the values clarity and informed subscales of the decisional conflict scale. The following confounders had significant bivariate relationships with decisional conflict and were included in the multivariable analysis: age, education, and discussion with multiple health care providers, discussion with a perinatologist, the values clarity subscale of the decisional conflict scale, test decision, and time since decision was made.
The statistical software package SPSS 14.0 (SPSS Inc., Chicago, IL, USA) was used for data analysis. Multivariable linear regression, with decisional conflict as the outcome variable, was used to test the relationship between each independent variable and decisional conflict, while adjusting for the effects of potential confounders.
We hypothesized that the decision-making process may differ for women who did and did not choose invasive prenatal testing. As such, we treated test choice as a modifier of the relationship between the predictor variables and the outcome variable, decisional conflict. If the interaction between the independent variable and the test choice was not significant, the main effect relationship between the independent variable and the decisional conflict was reported.
Brief thematic analysis was used to analyze the qualitative data from the open-ended questions. This involved looking for themes that arose in multiple participants’ responses or were relevant to the study objective and then determining the proportion of participants’ responses encompassed in each theme.
RESULTS
Demographics, basic infertility history, and characteristics of current pregnancy are presented in Table 1. Just over one third (68/180; 38%) of the participants were above 35 years, the historical cut-off point for offering invasive prenatal testing. The frequency of prior miscarriage was higher than in the general population, but comparable to other pregnancy after infertility samples (Klock and Greenfeld, 2000; Hjelmstedt et al., 2003a).
Table 1.
Participant characteristics: demographics, infertility, current pregnancy
| n | % | |
|---|---|---|
| Total (n) | 180 | |
| Age [years, mean (SD)] | 32.6 (4.74) | |
| Marital status | ||
| Married | 172 | 95.7 |
| Divorced or separated | 4 | 2.2 |
| Education | ||
| College graduation or more | 140 | 77.8 |
| Ethnicity | ||
| White | 165 | 91.7 |
| Duration of infertility [months, mean (SD)] | 37.9 (26.7) | |
| Ever had infertility treatment | 159 | 88.3 |
| Have children | 55 | 30.6 |
| History of miscarriage | 80 | 44.4 |
| Number of miscarriages [n, mean (SD)] | 1.66 (1.2) | |
| Current pregnancy conceived with assistance | 133 | 73.9 |
| In vitro fertilization | 48 | 26.7 |
| Ovulation induction | 28 | 15.6 |
| Ovulation induction with IUI | 26 | 14.4 |
| In vitro fertilization with ICSI | 22 | 12.2 |
| Gestational age of current pregnancy [weeks, mean (SD)] | 20.5 (9.4) | |
| Twins or triplets in current pregnancy | 25 | 17.7 |
IUI, intrautierine insemination; ICSI, intracytoplasmic sperm injection.
The majority of women (124/180; 69%) declined invasive prenatal testing. There was a significant bivariate relationship between test choice and decisional conflict; women who chose to have invasive testing had higher decisional conflict [mean = 28.3; standard deviation (SD) = 23.6] than those who declined testing (mean = 17.3; SD = 20.1; p = 0.006). This relationship is partly attributable to interactions between test choice and several of the independent variables (reported below).
The mean decisional conflict score was 22.1 (SD = 23.2), with the majority of women reporting low decisional conflict (129/180; 72%). In open-ended questions, over half (53%) of participants noted that their infertility experience had made their decision easier or that it had not made it more difficult. For example, one participant said ‘infertility made this very clear to my husband and me. We only debated for a few minutes’ (33-year-old woman, 2 years of infertility, declined prenatal testing). A much smaller percentage (6%) of women reported that their infertility experience made their decision more difficult.
Answers to the open-ended questions offered some insight into how infertility may have clarified the testing choice. Some women said that they would accept any baby, because of their infertility experience (47/180; 26%): ‘I think working towards becoming pregnant made the value of the baby's life, whether or not it had defects, what mattered most to me’ (34-year-old woman, 1.7 years of infertility, declined prenatal testing).
Other women noted that infertility had made them unwilling to take on the procedure-related risk of miscarriage (76/180; 42%): ‘After everything we went through it is ABSOLUTELY NOT worth the risk’ (29-year-old woman, 1 year of infertility, declined prenatal testing).
Some participants mentioned that infertility had made them more savvy health care consumers, making it easier to make complicated and difficult decisions. When asked whether there were any ways infertility made the prenatal testing decision easier, one participant said, ‘As a result of my infertility, I was an extremely informed consumer. I had become comfortable with asking medical professionals questions. I also found some reliable websites to do research on.’ (35-year-old woman, 3 years of infertility, had amniocentesis). While this claim was made by only a few women (11/180; 6%), a high level of medical savvy was implicitly evident in many of the qualitative responses.
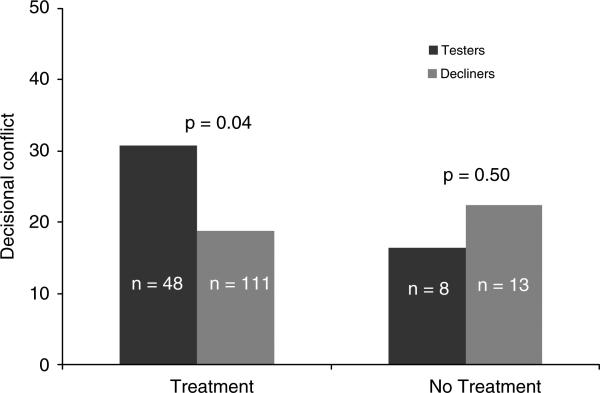
While most of the infertility variables tested were not significantly associated with decisional conflict, a few were (Table 2). There was a significant interaction between infertility treatment and prenatal test choice on decisional conflict. For women who had been treated for infertility, choosing to have testing was associated with higher decisional conflict (Figure 1). Among women who were not treated for infertility, test choice was not significantly associated with decisional conflict. Only a small number of study participants had not been treated for infertility, and thus our ability to make inferences about this group is limited. Other infertility treatment variables such as the type of treatment used to conceive the current pregnancy or number of cycles of treatment were not significantly associated with decisional conflict.
Table 2.
Multivariable linear regression analysis: prediction of decisional conflict by independent variables alone or with test choice as a modifiera
| Interaction with test choice |
Main effect |
||||
|---|---|---|---|---|---|
| Test takers | Test decliners | ||||
| p-Value | Standardized βb | Standardized βb | p-Value | Standardized βc | |
| Medical infertility characteristics | |||||
| Infertility duration | n.s. | — | — | 0.138 | −0.091 |
| Have children | n.s. | — | — | 0.25 | 0.068 |
| Given a diagnosis | n.s. | — | — | 0.457 | 0.044 |
| Miscarriage history | n.s. | — | — | 0.096 | 0.098 |
| Ever had treatment | 0.041 | 0.2056 | −0.0426 | — | — |
| Money spent on tests and treatment | n.s. | — | — | 0.54 | 0.037 |
| Spontaneous versus assisted conception | n.s. | — | — | 0.398 | −0.024 |
| Multiples in current pregnancy | n.s. | — | — | 0.280 | −0.067 |
| Donor egg in current pregnancy | n.s. | — | — | 0.849 | −0.012 |
| Psychological infertility characteristics | |||||
| Perceived severity | |||||
| Versus women without infertility | n.s. | — | — | 0.482 | −0.043 |
| Versus women with infertility | n.s. | — | — | 0.166 | −0.083 |
| Likelihood of getting pregnant again | n.s. | — | — | 0.205 | 0.076 |
| Distress | |||||
| Social concern | n.s. | — | — | 0.303 | −0.061 |
| Rejection of childfree lifestyle | n.s. | — | — | 0.033 | 0.168 |
| Need for parenthood | n.s. | — | — | 0.64 | −0.029 |
| Perceived Disagreementd | |||||
| Husband | 0.007 | 0.346 | −0.0954 | — | — |
| Doctor | 0.003 | 0.248 | −0.154 | — | — |
| Other infertile women | n.s. | — | — | — | — |
| Most people who are important to me | 0.011 | 0.168 | −0.196 | — | — |
n.s., not significant.
Standardized β indicates the strength and direction of the relationship with decisional conflict.
Standardized β for test takers or test decliners shown only if interaction with test choice is significant (p < 0.05).
Standardized β for main effect shown only if interaction with test choice is not significant.
Only interaction is reported because perceived disagreement was measured as an interaction between norms and test choice (see Figure 1 for graphical representation).
Figure 1.
Relationship between infertility treatment and decisional conflict, modified by test choice
There was a significant main effect between one of the dimensions of infertility distress and decisional conflict (Table 2). Distress associated with rejection of a childfree lifestyle was positively correlated with decisional conflict, indicating that women who were more distressed by living without a child had greater difficulty deciding whether to have invasive testing.
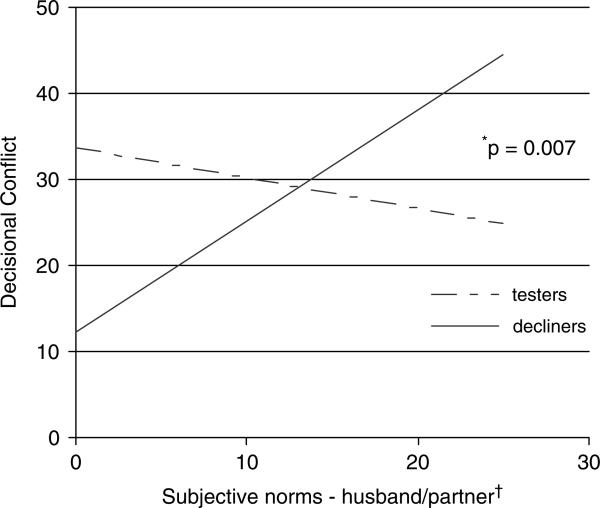
Women who perceived that other people disagreed with their choice about testing reported significantly higher levels of decisional conflict. Perceived disagreement with the test choice was measured using an interaction between subjective norms and test choice. This interaction was significant for husbands/partners, infertility doctors, and ‘most people who are important to me’ (Table 2). It was not significant for ‘other women with infertility’. Higher levels of decisional conflict were reported when the participant perceived that other people disagreed with their decision. For example, women who chose to have testing reported higher decisional conflict if they reported low subjective norm scores, indicating that they perceived their partner did not want them to have testing and thus their test choice was in disagreement with their partner's preference (Figure 2).
Figure 2.
Interaction between subjective norms and test choice: relationship between decisional conflict and perceived disagreement with test choice by husband/partner. *p-Value for interaction between test choice and subjective norms; † Lower subjective norm scores represent a perception that husband/partner does not want the participant to have prenatal testing and/or the participant is not motivated to comply with that opinion. Higher scores indicate that the participant perceives the husband/partner wants her to have prenatal testing and she is motivated to comply with that opinion
DISCUSSION
Most participants declined invasive testing. The 31% uptake rate in our sample is consistent with some studies of invasive prenatal testing uptake in pregnancy after infertility (Meschede et al., 1998; Geipel et al., 2004), and substantially lower than others (Schover et al., 1998; Monni et al., 1999; Elimian et al., 2003). The proportion of individuals in our study who chose to have invasive testing was roughly half that reported in the general prenatal testing literature (60–80%) (French et al., 1992; Tercyak et al., 2001; Bekker et al., 2004; Kaiser et al., 2004; Hunter et al., 2005).
Given the greater level of investment and higher levels of anxiety associated with pregnancies after infertility, we anticipated finding a high level of decisional conflict in this sample. Contrary to these expectations, the majority of women in this study reported low levels of decisional conflict and said that infertility did not make the decision more difficult. This suggests that for many women the decision about whether to undergo invasive prenatal testing may actually be easier after infertility. Indeed, half of participants specifically noted that their infertility history made the decision easier or at least did not make it more difficult.
This raises the question of how the infertility experience helped to clarify the invasive prenatal testing decision. Several of the qualitative themes suggest possible explanations. It seems that infertility helped, or perhaps obligated, women to confront and resolve tensions in underlying values and beliefs, such as willingness to accept a child with disabilities and unwillingness to risk a procedure-related miscarriage (Sapp et al., 2010). The qualitative data suggest that values-clarification may have applied primarily to women who declined invasive testing. By clarifying values around parenting and disability, infertility made the choice not to have testing clearer, but did not make the choice to have testing any easier. This is consistent with our finding that women who chose to have testing reported higher decisional conflict than those who chose to not have testing.
Prior studies also describe infertility as a values-clarifying experience. Sandelowski et al. observed that couples who declined amniocentesis in post-infertility pregnancies did so because their ‘efforts to achieve a viable pregnancy served to change their attitudes toward parenting an impaired child’ (Sandelowski et al., 1991). Studies on pregnancy after infertility have reported that this population is more willing to accept difficult infants and places less importance on the gender of the fetus (Sandelowski et al., 1991; McMahon et al., 1999; Hjelmstedt et al., 2003a). The value shift observed in this study may be part of a larger increase in parenting preparedness, motivation for parenthood, and appreciation for the importance of parenting (Sandelowski et al., 1991; van Balen and Trimbos-Kemper, 1995).
While our participants reported a shift in their willingness to accept difficult or disabled children, little is known about how these families actually do when a child is born with medical problems. Future research investigating parent, child, and family psychological outcomes in post-infertility families with children with disabilities could elucidate an understanding of this phenomenon (Cohen, 1996; Schover et al., 1998).
The qualitative data suggest that the decision may have been easy for some women because their experience with infertility made them adept decision makers and savvy health care consumers. Infertile couples are well practiced at making emotionally laden and medically complex decisions, having done so with each choice to engage in another cycle of infertility treatment (Sandelowski et al., 1991). While values clarification may have helped them determine what to choose, heightened medical literacy, self-awareness, and decision-making skills may have helped women with how to choose.
Although decisional conflict was low for many participants, a subset reported high levels of conflict. These women may benefit from interventions aimed at reducing their conflict, such as values clarification using a decision aid or participating in genetic counseling (O'Connor et al., 2003; Sapp et al., 2010). Many of the independent variables we tested were not significantly associated with decisional conflict; however, the relationships that were significant were in the direction we hypothesized; greater infertility-related distress, having treatment then choosing testing, and disagreement with others about the test choice were all associated with higher decisional conflict.
Our results suggest that a history of infertility treatment coupled with a choice to have invasive testing made it more difficult for women to decide. Women who have had infertility treatment likely experience a greater level of investment and thus attribute greater significance to the potential losses associated with invasive testing. This finding is consistent with those from a prior study suggesting that women who have been through more treatment cycles have higher levels of pregnancy-related anxiety (McMahon et al., 1997).
Of the dimensions of infertility distress we measured, only rejection of a childfree lifestyle was associated with decisional conflict. Perhaps, women who are particularly distressed by the notion of not having a child in their life are more conflicted about whether to have a test that may risk their hard-won chance to finally have a child. Consistent with this finding, studies on pregnancy after infertility have found that higher levels of infertility-related distress are associated with greater anxiety about pregnancy loss (Hjelmstedt et al., 2003a,b).
Our results also reveal that there is a strong social component to difficulty with this decision. The interaction effect between subjective norms and test decision demonstrates that women whose choices were incongruent with other significant people's opinions had more difficulty with the decision. The association between decisional conflict and disagreement with others about the test choice is consistent with the conflict theory of decision making (Janis and Mann, 1977; O'Connor and D'Amico, 1990). Previous studies support the notion that infertile women are particularly conscious of the opinions of others when making choices (Callan et al., 1998; Peddie et al., 2005). It has also been suggested that couples who have been through infertility may be especially sensitive to social pressure and scrutiny (McMahon et al., 1995; Hahn, 2001). Further research is needed to determine whether the relationship between disagreement with others and decisional conflict observed here is particular to women with a history of infertility.
Study limitations
Due to the cross-sectional nature of this study, conclusions cannot be made about the direction or causality of relationships. The study was not designed to make comparisons with populations without infertility. Online recruitment has the potential for selection bias. While studies suggest that most (>80%) women who are dealing with infertility use the Internet for information and support (Haagen et al., 2003), we cannot ascertain whether survey respondents are representative of the general population of women with infertility. We were unable to calculate a response rate. Given that infertility-related distress, decisional conflict, and infertility severity were all measured retrospectively, there is also potential for recall bias. The scope of the study was limited to the women's viewpoint, so the perspective of the fathers regarding decision making was not assessed. Cultural and religious variables were also not included in this study.
Clinical implications
The findings of this study may help obstetricians, reproductive endocrinologists, and genetic counselors identify individuals who are particularly likely to struggle with this decision. Our results suggest that the women who have the greatest need for decisional support are those who disagree with the perceived opinions of others, who have had infertility treatment and choose to have prenatal testing, and those who are especially distressed by the notion of a childfree life. The findings of this study can be used as a guide for clinicians to determine who to help, as well as how to help them. They tell a story of broader decision-making processes and resolution of decisional conflict. The values clarification described by women in this study demonstrates how exploration of values and beliefs can contribute to decision making.
ACKNOWLEDGEMENTS
The authors thank Rajiv Rimal, PhD, for his input into the early study design process. This research was funded by the National Human Genome Research Institute intramural research program, National Institutes of Health.
Footnotes
Paper presented at National Society of Genetic Counselors Annual Education Conference in Kansas City, MO, 15 October 2007.
REFERENCES
- Abma JC, Chandra A, Mosher WD, et al. Fertility, family planning, and women's health: new data from the 1995 National Survey of Family Growth. Vital Health Stat. 1997;23(19):1–114. [PubMed] [Google Scholar]
- ACOG Invasive prenatal testing for aneuploidy. Obstet Gynecol. 2007;110(6):1459–1467. doi: 10.1097/01.AOG.0000291570.63450.44. ACOG Practice Bulletin No. 88, December 2007. [DOI] [PubMed] [Google Scholar]
- ASRM Definitions of infertility and recurrent pregnancy loss. Fertil Steril. 2008;90(5 Suppl):S60–S60. doi: 10.1016/j.fertnstert.2008.08.065. [DOI] [PubMed] [Google Scholar]
- Bekker HL, Hewison J, Thornton JG. Applying decision analysis to facilitate informed decision making about prenatal diagnosis for Down syndrome: a randomised controlled trial. Prenat Diagn. 2004;24(4):265–275. doi: 10.1002/pd.851. [DOI] [PubMed] [Google Scholar]
- Bernstein J, Lewis J, Seibel M. Effect of previous infertility on maternal-fetal attachment, coping styles, and self-concept during pregnancy. J Women's Health. 1994;3(2):125–133. [Google Scholar]
- Callan VJ, Kloske B, Kasma Y, et al. Toward understanding women's decisions to continue or stop in vitro fertilization: the role of social, psychological, and background factors. J In Vitro Fert Embryo Transf. 1998;5(6):363–369. doi: 10.1007/BF01129572. [DOI] [PubMed] [Google Scholar]
- Chandra A, Stephen EH. Impaired fecundity in the United States: 1982–1995. Fam Plann Perspect. 1998;30(1):34–42. [PubMed] [Google Scholar]
- Cohen CB. ‘Give me children or I shall die!’ New reproductive technologies and harm to children. Hastings Cent Rep. 1996;26:19–27. [PubMed] [Google Scholar]
- Covington SN, Burns LH. Pregnancy after infertility. In: Burns LH, Covington SN, editors. Infertility Counseling: A Comprehensive Handbook for Clinicians. Parthenon Publishing Group; New York, NY: 1999. [Google Scholar]
- Drake E, Engler-Todd L, O'Connor A, et al. Development and evaluation of a decision aid about prenatal testing for women of advanced maternal age. J Genet Couns. 1999;8(4):217–233. doi: 10.1023/A:1022998415890. [DOI] [PubMed] [Google Scholar]
- Elimian A, Demsky M, Figueroa R, et al. The influence of IVF, multiple gestation and miscarriage on the acceptance of genetic amniocentesis. Prenat Diagn. 2003;23(6):501–503. doi: 10.1002/pd.633. [DOI] [PubMed] [Google Scholar]
- French BN, Kurczynski TW, Weaver MT, et al. Evaluation of the Health Belief Model and decision making regarding amniocentesis in women of advanced maternal age. Health Educ Q. 1992;19(2):177–186. doi: 10.1177/109019819201900203. [DOI] [PubMed] [Google Scholar]
- Geipel A, Berg C, Katalinic A, et al. Different preferences for prenatal diagnosis in pregnancies following assisted reproduction versus spontaneous conception. Reprod Biomed Online. 2004;8(1):119–124. doi: 10.1016/s1472-6483(10)60506-8. [DOI] [PubMed] [Google Scholar]
- Haagen EC, Tuil W, Hendriks J, et al. Current Internet use and preferences of IVF and ICSI patients. Hum Reprod. 2003;18(10):2073–2078. doi: 10.1093/humrep/deg423. [DOI] [PubMed] [Google Scholar]
- Hahn CS. Review: psychosocial well-being of parents and their children born after assisted reproduction. J Pediatr Psychol. 2001;26(8):525–538. doi: 10.1093/jpepsy/26.8.525. [DOI] [PubMed] [Google Scholar]
- Hjelmstedt A, Widstrom A, Wramsby HM, et al. Patterns of emotional responses to pregnancy, experience of pregnancy and attitudes to parenthood among IVF couples: a longitudinal study. J Psychosom Obstet Gynaecol. 2003a;24(3):153–162. doi: 10.3109/01674820309039669. [DOI] [PubMed] [Google Scholar]
- Hjelmstedt A, Widstrom AM, Wramsby H, et al. Personality factors and emotional responses to pregnancy among IVF couples in early pregnancy: a comparative study. Acta Obstet Gynecol Scand. 2003b;82(2):152–161. doi: 10.1034/j.1600-0412.2003.00040.x. [DOI] [PubMed] [Google Scholar]
- Hunter AG, Cappelli M, Humphreys L, et al. A randomized trial comparing alternative approaches to prenatal diagnosis counseling in advanced maternal age patients. Clin Genet. 2005;67(4):303–313. doi: 10.1111/j.1399-0004.2004.00405.x. [DOI] [PubMed] [Google Scholar]
- Janis IL, Mann L. Decision Making. The Free Press; New York: 1977. [Google Scholar]
- Kaiser AS, Ferris LE, Katz R, et al. Psychological responses to prenatal NTS counseling and the uptake of invasive testing in women of advanced maternal age. Patient Educ Couns. 2004;54(1):45–53. doi: 10.1016/S0738-3991(03)00190-3. [DOI] [PubMed] [Google Scholar]
- Kaiser AS, Ferris LE, Pastuszak AL, et al. The effects of prenatal group genetic counselling on knowledge, anxiety and decisional conflict: issues for nuchal translucency screening. J Obstet Gynaecol. 2002;22(3):246–255. doi: 10.1080/01443610220130508. [DOI] [PubMed] [Google Scholar]
- Kim K, Reicks M, Sjoberg S. Applying the theory of planned behavior to predict dairy product consumption by older adults. J Nutr Educ Behav. 2003;35(6):294–301. doi: 10.1016/s1499-4046(06)60343-6. [DOI] [PubMed] [Google Scholar]
- Klock SC, Greenfeld DA. Psychological status of in vitro fertilization patients during pregnancy: a longitudinal study. Fertil Steril. 2000;73(6):1159–1164. doi: 10.1016/s0015-0282(00)00530-6. [DOI] [PubMed] [Google Scholar]
- McMahon CA, Tennant C, Ungerer J, et al. ’Don't count your chickens’: a comparative study of the experience of pregnancy after IVF conception. J Reprod Infant Psychol. 1999;17(4):345–356. [Google Scholar]
- McMahon CA, Ungerer J, Beaurepaire J, et al. Psychosocial outcomes for parents and children after in vitro fertilization: a review. J Reprod Infant Psychol. 1995;13:1–16. [Google Scholar]
- McMahon CA, Ungerer J, Beaurepaire J, et al. Anxiety during pregnancy and fetal attachment after in-vitro fertilization conception. Hum Reprod. 1997;12(1):176–182. doi: 10.1093/humrep/12.1.176. [DOI] [PubMed] [Google Scholar]
- Meschede D, Lemcke B, Stussel J, et al. Strong preference for non-invasive prenatal diagnosis in women pregnant through intracytoplasmic sperm injection (ICSI). Prenat Diagn. 1998;18(7):700–705. [PubMed] [Google Scholar]
- Monni G, Cau G, Lai R, et al. Intracytoplasmic sperm injection and prenatal invasive diagnosis. Prenat Diagn. 1999;19(4):390. doi: 10.1002/(sici)1097-0223(199904)19:4<390::aid-pd558>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Moyer A, Brown B, Gates E, et al. Decisions about prenatal testing for chromosomal disorders: perceptions of a diverse group of pregnant women. J Womens Health Gend Based Med. 1999;8(4):521–531. doi: 10.1089/jwh.1.1999.8.521. [DOI] [PubMed] [Google Scholar]
- Newton CR, Sherrard W, Glavac I. The fertility problem inventory: measuring perceived infertility-related stress. Fertil Steril. 1999;72(1):54–62. doi: 10.1016/s0015-0282(99)00164-8. [DOI] [PubMed] [Google Scholar]
- O'Connor A. Decisional conflict. In: McFarland GK, McFarlane EA, editors. Nursing Diagnosis and Intervention. 2nd Edn C. V. Mosby; St. Louis: 1993. pp. 468–477. [Google Scholar]
- O'Connor A, D'Amico M. Decisional conflict. In: McFarland GK, Thomas MD, editors. Psychiatric Mental Health Nursing: Application of the Nursing Process. J.B. Lippincott; Philadelphia: 1990. [Google Scholar]
- O'Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15(1):25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- O'Connor AM, Bennett CL, Stacey D, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2003;(2):CD001431. doi: 10.1002/14651858.CD001431. [DOI] [PubMed] [Google Scholar]
- Osmanagaoglu K, Collins J, Kolibianakis E, et al. Spontaneous pregnancies in couples who discontinued intracytoplasmic sperm injection treatment: a 5-year follow-up study. Fertil Steril. 2002;78(3):550–556. doi: 10.1016/s0015-0282(02)03300-9. [DOI] [PubMed] [Google Scholar]
- Peddie VL, van Teijlingen E, Bhattacharya S. A qualitative study of women's decision-making at the end of IVF treatment. Hum Reprod. 2005;20(7):1944–1951. doi: 10.1093/humrep/deh857. [DOI] [PubMed] [Google Scholar]
- Reading AE, Chang LC, Kerin JF. Attitudes and anxiety levels in women conceiving through in vitro fertilization and gamete intrafallopian transfer. Fertil Steril. 1989;52(1):95–99. doi: 10.1016/s0015-0282(16)60796-3. [DOI] [PubMed] [Google Scholar]
- Sandelowski M, Harris BG, Holditch-Davis D. Amniocentesis in the context of infertility. Health Care Women Int. 1991;12(2):167–178. doi: 10.1080/07399339109515938. [DOI] [PubMed] [Google Scholar]
- Sapp JC, Hull SC, Duffer S, et al. Ambivalence toward undergoing invasive prenatal testing: an exploration of its origins. Prenat Diagn. 2010;30(1):77–82. doi: 10.1002/pd.2343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt L. Infertility and assisted reproduction in Denmark. Epidemiology and psychosocial consequences. Dan Med Bull. 2006;53(4):390–417. [PubMed] [Google Scholar]
- Schover LR, Thomas AJ, Falcone T, et al. Attitudes about genetic risk of couples undergoing in-vitro fertilization. Hum Reprod. 1998;13(4):862–866. doi: 10.1093/humrep/13.4.862. [DOI] [PubMed] [Google Scholar]
- Tercyak KP, Johnson SB, Roberts SF, et al. Psychological response to prenatal genetic counseling and amniocentesis. Patient Educ Couns. 2001;43(1):73–84. doi: 10.1016/s0738-3991(00)00146-4. [DOI] [PubMed] [Google Scholar]
- van Balen F, Trimbos-Kemper TC. Involuntary childless couples: their desire to have children and their motives. J Psychosom Obstet Gynecol. 1995;16:137–144. doi: 10.3109/01674829509024462. [DOI] [PubMed] [Google Scholar]