Abstract
Background
Nearly two thirds of reproductive-aged women in the United States are currently overweight or obese, placing them at elevated risk for adverse health outcomes. This study identifies factors associated with transition in body mass index (BMI) category to overweight or obesity status over a 2-year period among women of reproductive age.
Methods
Data were collected in the Central Pennsylvania Women's Health Study (CePAWHS), a longitudinal cohort study of reproductive-aged women. Participants were 689 women with normal or overweight BMI at baseline who were not pregnant at either baseline or 2-year follow-up. Separate multiple logistic regression analyses were estimated to model adverse change in weight category for women who were normal weight at baseline and to model transition to obesity among women who were overweight at baseline.
Results
Among women of normal weight at baseline, 18% became overweight or obese by follow-up; 25% of women overweight at baseline became obese. In multiple regression analyses, low physical activity at baseline was significantly associated with a 2-fold elevation in the odds of transitioning from normal BMI to overweight/obesity (odds ratio [OR] 2.11, 95% confidence interval [CI] 1.06-4.20), as was having an interim live birth (OR 2.75, 95%CI 1.27-5.95). In contrast, demographics (lower education, younger age) were the only significant predictors of transition from overweight to obesity.
Conclusions
: Meeting physical activity guidelines should be encouraged among normal weight women of reproductive age as well as those who are overweight or obese, as low physical activity is a risk for transitioning from normal to overweight status. Younger overweight women are particularly at risk for transition to obesity.
Introduction
Nearly two thirds of reproductive-aged women in the United States are currently overweight or obese.1 Obesity and overweight status put women at elevated risk for a myriad of adverse health outcomes, including cardiovascular disease, diabetes, kidney disease, and obesity-related cancers.2,3 These women are also more likely to develop pregnancy complications, such as gestational diabetes, hypertensive disorders of pregnancy, and cesarean section delivery.4,5 Transitions from normal weight status to overweight and obesity and from overweight to obesity in midlife have also been associated with adverse health outcomes, including an increased likelihood of developing major chronic physical conditions, such as cancer, coronary heart disease, diabetes, and metabolic syndrome,6–8 as well as higher risks of mental impairment, including cognitive decline and dementia.6,9 Increased risk of mortality overall and due to coronary heart disease, cardiovascular disease, and cancer have also been linked to weight gain among women aged 30–55 years.10 Numerous professional groups, including the Institute of Medicine (IOM)11 and the Centers for Disease Control and Prevention (CDC)12 have stressed the importance of entering pregnancy within the normal weight status and have identified lifestyle counseling and intervention before pregnancy as key strategies for moderating weight and reducing long-term weight gain in women.
Although there is consensus that promotion of healthy weight status among reproductive-aged women is necessary and important,12,13 little is known about the factors that influence the progression from normal weight status to overweight and obesity in this population. Dietary intake and physical activity levels are identified as primary proximate determinants of weight status, and a range of characteristics has been shown to influence these behaviors and, in turn, to affect body weight trajectories among women in their reproductive years. For example, previous research highlights the importance of mental health-related factors, including perceived psychosocial stress14,15 and depression,16 in the development and persistence of adverse health behaviors that affect weight. A number of sociodemographic characteristics, including educational attainment,17 income,18 and race/ethnicity,1 have also been shown to significantly affect weight-related behavior and to increase the prevalence of overweight and obesity over time.
We use data from a longitudinal study of reproductive-aged women to identify predictors of transition in BMI category to overweight or obesity status over a 2-year period. Based on the previous literature and reproductive life stage,1,14–18 the predictors considered include sociodemographics, health behaviors associated with weight, psychosocial factors, and reproductive history. Because baseline weight has been found to be important in previous weight gain research,15,19,20 body mass index (BMI) transitions are examined separately based on initial weight status for two groups of reproductive-aged women: (1) transition to overweight or obese status among women who have a normal BMI at baseline and (2) transition to obesity among women who are overweight at baseline.
Materials and Methods
Study design and sample
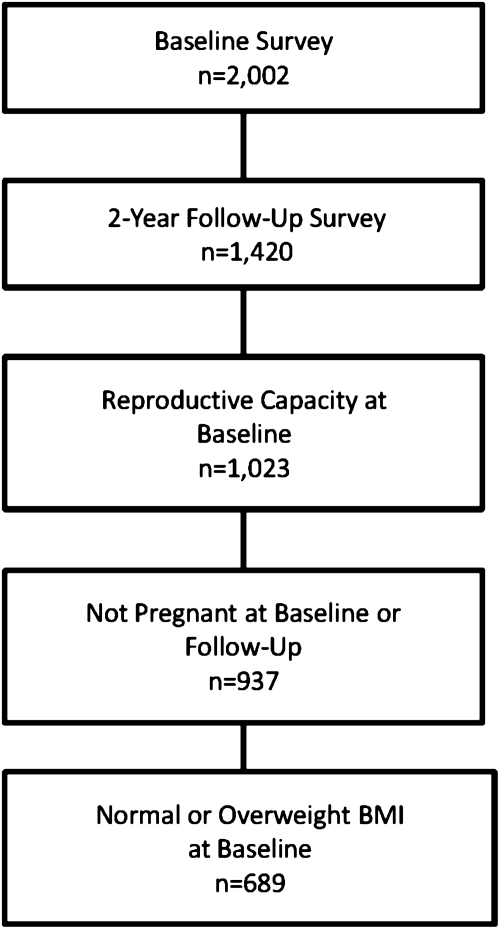
As shown in Figure 1, data come from women who participated in both the baseline and 2-year follow-up (n=1420) waves of the Central Pennsylvania Women's Health Study (CePAWHS). The baseline random-digit dial survey was conducted between September 2004 and March 2005. Participants were reinterviewed at the 2-year anniversary of the baseline interview. All women were between the ages of 18 and 45 at baseline. The baseline sample (n=2002) was highly representative of the target population with regard to sociodemographics.21 Ninety percent of baseline respondents consented to be contacted for follow-up. Among these, a 79% follow-up response rate was attained, with nonresponse due mainly to failure to locate; only 5% of those contacted refused to be interviewed.22 Participants in the follow-up survey were compared to nonparticipants, and women who were older at baseline (aged 35–45), college-educated, married or cohabitating, not in poverty, and non-Hispanic white were more likely to participate in the follow-up survey.21,22 Additional details of the study design, response rates, and sample representativeness have been published previously.21,22 The study was approved by the Institutional Review Board at the Pennsylvania State College of Medicine.
FIG. 1.
Characteristics of the analytic sample, n=689.
Because we were interested in the effect of pregnancy on weight category transitions, the sample is limited to women with reproductive capacity at baseline (n=1023). To ensure that BMI is based on nonpregnant weight, the final analytic sample includes 689 women who were not pregnant at either the baseline or follow-up interview and had normal or overweight BMI at baseline. Because this analysis focuses on those undergoing adverse change in BMI category, we excluded respondents who were obese at baseline, and underweight women were excluded because there were too few for analysis (n=16).
Measures
Dependent variables
BMI (calculated from reported weight and height as weight in kilograms divided by height in meters squared23) was ascertained at both baseline and follow-up so that BMI change could be measured. Self-reported height and weight have been found to accurately represent BMI abstracted from medical records for reproductive-aged women.24 The dependent variables are (1) change in BMI from normal (BMI range 18.5–24.9) at baseline to overweight or obese (BMI ≥25.0) at follow-up and (2) change in BMI from overweight (BMI range 25.0–29.9) at baseline to obese (BMI ≥30.0) at follow-up. Note that there were too few women (n=4) who transitioned from normal weight at baseline to obesity at follow-up for separate analysis of that adverse transition; thus, they are combined with women who became overweight at follow-up. Both dependent variables are scored as dichotomies (i.e., change did occur or change did not occur).
Independent variables
The independent variables were measured in the baseline interview. Sociodemographics include age in years, education level, poverty status, and race/ethnicity. Poverty status is computed based on household income and composition according to federal poverty standards, and in the analyses, those in poverty (<100% of the federal poverty level) and near poverty (between 100% and 200% of the federal poverty level) were grouped together and contrasted with those with higher household incomes. Of respondents in the analytic sample, 11% did not report household income and are, therefore, coded as poverty status unknown. Not reporting income could reflect sensitivity about disclosing this information (which could be present at all income levels) or lack of awareness of the family financial situation. Based on previous research, older age, lower education, lower income, and nonwhite race are expected to be associated with greater weight gain.17
Health behaviors likely to be associated with less risk of weight gain include fruit and vegetable consumption and physical activity levels meeting the guidelines.25,26 Fruit and vegetable intake was dichotomized as either <1 or ≥1 servings per day. Physical activity was categorized as either meeting or not meeting exercise recommendations of 30 minutes of moderate to strenuous physical activity on most, if not all, days of the week. Cigarette smoking increases energy expenditure and reduces appetite and is, therefore, associated with relatively lower body weight.27 Cigarette smoking status was dichotomized as either currently smoking or nonsmoking. The measures of these behaviors are based on the Behavioral Risk Factor Surveillance System (BRFSS) and have been described in additional detail in prior publications.21
Psychosocial factors include the Psychosocial Hassles Scale, a 12-item scale measuring the degree to which common hassles (such as money worries, problems with friends) were perceived as stressful during the past 12 months,28 and Depressive Symptoms, a 6-item scale measuring high risk for psychological distress, particularly depression.29 Both high stress and depressive symptoms are expected to be associated with greater weight gain.14–15,19,30
Reproductive history is relevant to weight gain because pregnancy weight gain may persist postpartum, and successive pregnancies may have a cumulative effect on weight status.11 A covariate is included in our analyses to indicate whether or not the woman had a live birth during the 2-year follow-up period.
Statistical analyses
Bivariate associations between independent and dependent variables were examined using chi-square tests or analysis of variance (ANOVA) (with post-hoc tests if necessary) and logistic regression analysis. Independent variables were examined for multicollinearity. Multiple logistic regression analysis was then used to model adverse change in weight category for two subsamples: women who were normal weight at baseline and women who were overweight at baseline. Variables conceptually regarded as potentially related to weight gain based on previous research were included in the models. All analyses were conducted using SAS version 9.1 statistical software.
Results
Eighteen percent of those who were normal weight at baseline (78 of 435) transitioned to overweight or obese status at follow-up; 25% of those were overweight at baseline (63 of 254) transitioned to obese status at follow-up. Table 1 compares demographic, behavioral, psychosocial, and reproductive characteristics of women in the sample who had normal BMI at baseline with those who were overweight at baseline. The groups were roughly equivalent with respect to many of these characteristics. Women who were overweight at baseline were, however, significantly more likely than normal weight women to report physical activity below the recommended level of 30 minutes or more on most days of the week (80.0% vs. 72.0%, p=0.02).25,26 They were also more likely to experience high levels of stress as measured by the Psychosocial Hassles Scale (52.0% vs. 39.8%, p<0.01) and to report a high level of depressive symptoms (18.9% vs. 13.3%, p=0.05).
Table 1.
Behavioral, Psychosocial, Reproductive, and Demographic Characteristics of Reproductive-Aged Women by Baseline Body Mass Index (n=689)
| |
Normal BMI at baseline (n=435) |
Overweight at baseline (n=254) |
|
||
|---|---|---|---|---|---|
| n | % | n | % | p value for difference | |
| Demographics | |||||
| Age (mean), years | 32.8 | 33.4 | 0.37 | ||
| Race/ethnicity | |||||
| Nonwhite race/ethnicity | 32 | 7.4 | 15 | 5.9 | 0.45 |
| White, non-Hispanic | 400 | 92.0 | 239 | 94.1 | |
| Education | |||||
| ≤High school | 308 | 70.8 | 189 | 74.4 | 0.31 |
| >High school | 127 | 29.2 | 65 | 25.6 | |
| Poverty status | |||||
| In poverty/near poverty | 85 | 19.5 | 55 | 21.7 | 0.26 |
| Not in poverty | 295 | 67.8 | 177 | 69.7 | |
| Unknown | 55 | 12.6 | 22 | 8.7 | |
| Health behaviors | |||||
| Fruit Consumption | |||||
| <1 serving daily | 269 | 61.8 | 146 | 57.5 | 0.26 |
| ≥1 serving daily | 166 | 38.2 | 108 | 42.5 | |
| Vegetable consumption | |||||
| <1 serving daily | 243 | 55.9 | 146 | 57.5 | 0.68 |
| ≥1 serving daily | 192 | 44.1 | 108 | 42.5 | |
| Physical activity level | |||||
| <30 minutes most days | 313 | 72.0 | 203 | 80.0 | 0.02 |
| ≥30 minutes most days | 122 | 28.0 | 51 | 20.1 | |
| Cigarette Smoking | |||||
| Current smoker | 78 | 17.9 | 51 | 20.1 | 0.49 |
| Not current smoker | 357 | 82.1 | 203 | 79.9 | |
| Psychosocial factors | |||||
| Psychosocial Hassles Scale | |||||
| High stress | 173 | 39.8 | 132 | 52.0 | <0.01 |
| Low stress | 262 | 60.2 | 122 | 48.0 | |
| Depressive symptoms | |||||
| High | 58 | 13.3 | 48 | 18.9 | 0.05 |
| Low | 376 | 86.4 | 206 | 81.1 | |
| Interim live birth | 40 | 9.2 | 25 | 9.8 | 0.79 |
Table 2 presents bivariate associations, quantifying the unadjusted association of each independent variable with adverse BMI transition using logistic regression models to generate odds ratios (ORs). At baseline, among women with normal BMI, significant associations were observed between adverse BMI transition and a number of characteristics, including elevated psychosocial stress (OR 1.89, 95% confidence interval [CI] 1.15-3.09) and depressive symptoms (OR 1.93, 95% CI 1.02-3.65), low physical activity level (OR 2.45, 95% CI 1.27-4.71), and experiencing a live birth in the follow-up interval (OR 1.88, 95% CI 1.00-3.55). A different pattern is seen among overweight women such that significant associations are observed only for demographic factors including lower education (OR 2.04, 95% CI 1.10-3.78) and younger age (18–24 years vs. 35–45 years) (OR 2.98, 95% CI 1.31-6.81).
Table 2.
Bivariate Relationships Among Behavioral, Psychosocial, Reproductive, and Demographic Characteristics and Adverse Body Mass Index Category Transition
| |
Normal BMI at baseline (n=435) |
Overweight at baseline (n=254) |
|---|---|---|
| |
Unadjusted OR for overweight or obese transition |
Unadjusted OR for obese transition |
| OR (95% CI) | OR (95% CI) | |
| Demographics | ||
| Age, years | ||
| 18–24 | 1.50 (0.79–2.83) | 2.98 (1.31–6.81) |
| 25–34 | 1.10 (0.63–1.93) | 1.65 (0.87–3.13) |
| 35–45 | Reference | Reference |
| Race/ethnicity | ||
| Nonwhite race/ethnicity | 1.34 (0.56–3.23) | 2.86 (0.99–8.23) |
| White, non-Hispanic | Reference | Reference |
| Education | ||
| ≤High school | 1.18 (0.70–2.00) | 2.04 (1.10–3.78) |
| >High school | Reference | Reference |
| Poverty status | ||
| In poverty/near poverty | 1.17 (0.65–2.13) | 1.64 (0.83–3.21) |
| Poverty unknown | 0.44 (0.17–1.15) | 2.09 (0.82–5.35) |
| Not in poverty | Reference | Reference |
| Health behaviors | ||
| Fruit Consumption | ||
| <1 serving daily | 1.60 (0.94–2.72) | 0.83 (0.47–1.47) |
| ≥1 serving daily | Reference | Reference |
| Vegetable consumption | ||
| <1 serving daily | 1.42 (0.86–2.35) | 1.07 (0.60–1.91) |
| ≥1 serving daily | Reference | Reference |
| Physical activity level | ||
| <30 minutes most days | 2.45 (1.27–4.71) | 1.52 (0.60–2.62) |
| ≥30 minutes most days | Reference | Reference |
| Cigarette smoking | ||
| Not current smoker | 0.67 (0.37–1.22) | 1.45 (0.68–3.09) |
| Current smoker | Reference | Reference |
| Psychosocial factors | ||
| Psychosocial Hassles Scale | ||
| High stress | 1.89 (1.15–3.09) | 1.32 (0.74–2.34) |
| Low stress | Reference | Reference |
| Depressive symptoms | ||
| High | 1.93 (1.02–3.65) | 1.32 (0.66–2.66) |
| Low | Reference | Reference |
| Interim live birth | ||
| Yes | 1.88 (1.00–3.55) | 0.77 (0.30–1.98) |
| No | Reference | Reference |
CI, confidence interval; OR, odds ratio.
Results of multiple logistic regression analysis modeling transition from normal BMI to overweight or obesity at follow-up are shown in Table 3. Controlling for other covariates, physical activity below the recommended level remains independently associated with a 2-fold elevation in the odds of transitioning to overweight/obesity (adjusted OR [AOR] 2.11, 95% CI 1.06-4.20). Women who had a live birth in the interval had over twice the odds of experiencing an adverse BMI transition compared to women who did not have an interval birth (AOR 2.75, 95% CI 1.27-5.95).
Table 3.
Results of Multiple Regression Analyses Modeling Transition from Normal Body Mass Index to Overweight or Obesity Among Reproductive-Aged Women (n=426)
| Adjusted odds ratio | 95% CI | |
|---|---|---|
| Demographics | ||
| Age, years | ||
| 18–24 | 1.01 | 0.48–2.12 |
| 25–34 | 0.79 | 0.43–1.44 |
| 35–45 | Reference | |
| Race/ethnicity | ||
| Nonwhite | 0.91 | 0.34–2.46 |
| White, non-Hispanic | Reference | |
| Education | ||
| ≤High school | 1.16 | 0.63–2.14 |
| >High school | Reference | |
| Poverty status | ||
| In poverty/near poverty | 1.00 | 0.51–1.98 |
| Poverty status unknown | 0.37 | 0.13–1.06 |
| Not in poverty | Reference | |
| Health behaviors | ||
| Fruit consumption | ||
| <1 serving daily | 1.26 | 0.70–2.28 |
| ≥1 serving daily | Reference | |
| Vegetable consumption | ||
| <1 serving daily | 1.28 | 0.74–2.23 |
| ≥1 serving daily | Reference | |
| Physical activity level | ||
| <30 minutes most days | 2.11 | 1.06–4.20 |
| ≥30 minutes most days | Reference | |
| Cigarette smoking | ||
| No | 1.00 | 0.51–2.00 |
| Yes | Reference | |
| Psychosocial factors | ||
| Psychosocial Hassles Scale | ||
| High stress | 1.65 | 0.95–2.88 |
| Low stress | Reference | |
| Depressive symptoms | ||
| High | 1.49 | 0.73–3.06 |
| Low | Reference | |
| Interim birth | ||
| Yes | 2.75 | 1.27–5.95 |
| None | Reference | |
The Hosmer Lemeshow goodness-of-fit test p value was 0.4193 (no misfit detected). The p value for the likelihood ratio test for overall model predictiveness was 0.0137, and c-statistic was 0.68.
Table 4 shows the results of multiple logistic regression analysis modeling transition from overweight status at baseline to obesity. Consistent with the bivariate analyses, in this group demographic factors are most important. Significantly increased risk of transition to obesity is seen for those with lower education (AOR 2.07, 95% CI 1.04-4.12). Women aged 18–24 years (AOR 2.91, 95% CI 1.16-7.32) were more likely than older women to transition from overweight to obesity status. Despite high levels of psychosocial stress and depressive symptoms among overweight women at baseline, neither these nor other independent variables were associated with transition to obesity over the 2-year follow-up period.
Table 4.
Results of Multiple Regression Analyses Modeling Transition from Overweight to Obesity Among Reproductive-Aged Women (n=254)
| Adjusted odds ratio | 95% CI | |
|---|---|---|
| Demographics | ||
| Age, years | ||
| 18–24 | 2.91 | 1.16–7.32 |
| 25–34 | 1.97 | 0.98–3.93 |
| 35–45 | Reference | |
| Race/ethnicity | ||
| Nonwhite | 2.85 | 0.88–9.12 |
| White, non-Hispanic | Reference | |
| Education | ||
| ≤High school | 2.07 | 1.04–4.12 |
| >High school | Reference | |
| Poverty status | ||
| In poverty/near poverty | 1.25 | 0.59–2.64 |
| Poverty status unknown | 1.60 | 0.58–4.42 |
| Not in poverty | Reference | |
| Health behaviors | ||
| Fruit consumption | ||
| <1 serving daily | 0.60 | 0.32–1.14 |
| ≥1 serving daily | Reference | |
| Vegetable consumption | ||
| <1 serving daily | 0.94 | 0.50–1.78 |
| ≥1 serving daily | Reference | |
| Physical activity level | ||
| <30 minutes most days | 1.38 | 0.60–3.18 |
| ≥30 minutes most days | Reference | |
| Cigarette smoking | ||
| No | 1.88 | 0.81–4.34 |
| Yes | Reference | |
| Psychosocial factors | ||
| Psychosocial Hassles Scale | ||
| High stress | 1.47 | 0.78–2.79 |
| Low stress | Reference | |
| Depressive symptoms | ||
| High | 1.02 | 0.46–2.26 |
| Low | Reference | |
| Interim birth | ||
| Yes | 0.38 | 0.12–1.25 |
| None | Reference | |
The Hosmer Lemeshow goodness-of-fit test p value was 0.4114 (no misfit detected). The p value for the likelihood ratio test for overall model predictiveness was 0.0392, and c-statistic was 0.68.
Discussion
This study examined transitions to overweight and obesity among reproductive-aged women. Several predictors of adverse transitions over a 2-year follow-up period were identified. Among women who were in the normal BMI category at baseline, physical activity levels lower than those recommended by the guidelines25,26 more than doubled the odds of becoming overweight, as did experiencing a live birth in the follow-up interval. Among women who were overweight at baseline, only lower educational level and younger age were associated with transition to the obese category. These findings suggest that the determinants of transitioning from normal weight to overweight and from overweight to obesity in the short term among women of reproductive age are not the same, and they illustrate the need to identify the important behavioral and psychological factors that increase women's risk of transitioning to obesity.
The finding that younger women are more likely than older women to transition from overweight to obesity is consistent with previous longitudinal studies of weight gain. For example, Williamson et al.31 examined weight gain and incidence of overweight in a 10-year follow-up of the population-representative cohort of US adults in the First National Health and Nutrition Examination Survey Epidemiologic Follow-up Study. They found that the absolute gain in BMI declined with increasing age, and the incidence of major weight gain was greatest in women and men 25–34 years of age. Younger women in their study who were already overweight at baseline had the highest incidence of major weight gain. In a similar study conducted in Finland, Rissanen et al.32 found that the incidence of substantial weight gain over approximately 5 years was highest among those 20–29 years of age at the baseline assessment. Lewis et al.33 analyzed weight trends among black and white participants in the Coronary Artery Risk Development in Young Adults (CARDIA) study, using linear, mixed-model regression to partition weight gain into gain associated with age and gain associated with secular trends. The largest age-related increases in weight occurred in the youngest age groups for both women and men. The authors hypothesized that physical activity and energy expenditure levels tend to decrease sharply after the teenage years, although caloric intake remains steady, which results in weight gain. Recognition of increased body weight over the early adult years may eventually lead people to cut back on their energy intake, resulting in a return to energy balance by their 30s.33
Whereas some previous research has examined changes in weight or BMI scores over time,14–16,19,34,35 this study examined transition in BMI categories. This may be more clinically relevant, as clinical guidelines use BMI categories to determine who should be screened for diabetes,36 how optimal cardiovascular health is defined,37 and whom and how intensively to counsel about weight loss interventions.38 Moreover, transition into a less favorable BMI category is associated with excess disease risk for hypertension, high cholesterol, diabetes, and obesity-related cancers,6–8 as well as subsequent declines in cognitive functioning.6,9 In terms of preconception health, women who are overweight or obese have increased risk for a myriad of pregnancy complications and adverse outcomes and should be counseled accordingly. Overweight and obese women who become pregnant also need to be counseled about the newest IOM guidelines for the BMI-specific gestational weight gain goals because excessive prenatal weight gain elevates the risk for numerous maternal and infant complications, and it independently predicts short-term and long-term postpartum weight retention.11 Preventing such transitions in BMI categories is, therefore, an important goal,39 and identifying the predictors of such transitions can be used to identify those at risk of a transition to worse BMI status.
Although this study of adverse transition in BMI category has many strengths, including its prospective design, several limitations should be noted. One limitation is reliance on self-reported height and weight for the computation of BMI. To the extent that self-report is biased, misclassification of some respondents' BMI category could occur. In the general U.S. population, there is evidence that self-report underestimates obesity prevalence.40 Among U.S. women, studies show they tend to overreport their height from 0.04 to 2.53 cm and to underreport their weight from 0.56 to <2 kg.41,42 These findings suggest that women may be misclassified into lower BMI categories based on self-reported height and weight; one international estimate is that 8.9% of North American females are categorized too low based on self-report.43 Among women of reproductive-age, however, the target population for this analysis, self-reported height and weight have been found to accurately represent BMI abstracted from medical records.24 Thus, the degree of bias, if any, in BMI classifications in this study is unknown, and future studies based on measured BMI category would be helpful. Future research examining short-term weight change might also consider additional analyses using as the definition of change a defined amount of change in weight, as this would include women who began at the lower end of their weight category and moved to the upper limit of their weight category in the changed category, as well as those who moved into the next category if they had a large increase in weight. Another limitation of the present study is that the dataset did not include weight history or sufficient information about weight gain during past and interim pregnancies to account for these factors in analyses. Also, both the sample and target populations are predominantly white, so finding only marginally significant effects of race/ethnicity for one transition group may reflect insufficient numbers of minority women in the sample. Finally, we have follow-up data over a 2-year time span but cannot examine longer term weight gain.
Our study has several important implications. First, we found that normal weight, reproductive-aged women who are not engaging in recommended levels of physical activity are at risk for becoming overweight or obese. Current U.S. Preventive Services Task Force guidelines recommend that after screening all adults for obesity, intensive counseling should be offered to obese patients about lifestyle modifications, including increasing physical activity.38 However, our findings suggest that engaging in recommended levels of physical activity may offer women protection against transitioning from normal weight to overweight status. Thus, an important public health recommendation may be that this counseling should be extended to nonobese women as a strategy for preventing obesity development among women of childbearing age. Second, adverse BMI transitions are common among normal weight women who experience a live birth. It is important that these women receive counseling about appropriate pregnancy weight gain, strategies for postpartum weight loss, and adopting and maintaining physical activity levels consistent with recommended guidelines. Third, overweight reproductive-aged women with lower educational levels require monitoring for obesity risk. Lower educational levels could be associated with less awareness of the importance of weight status for future health and of the health behaviors that are likely to prevent obesity, such as meeting physical activity guidelines. Fourth, because younger overweight women are at higher risk for transition to obesity in this study and other research,31–33,44 it should not be assumed that younger age is protective. Rather, counseling interventions to promote healthy weight-related behaviors should also target younger women of reproductive age.
Conclusions
Our findings highlight that transition into less favorable weight categories in reproductive-aged women occurs commonly and quickly. Taking the reproductive life stage context into account is an important aspect of monitoring and addressing adverse weight transitions among women, as these transitions will have deleterious effects on women's long-term health and on the risk of adverse pregnancy outcomes if pregnancy occurs. Maintaining recommended physical activity levels should be encouraged among normal weight women of reproductive age as well as those who are overweight or obese, as low physical activity is a risk for transitioning from normal to overweight status.
Acknowledgments
This research was funded, in part, under grant number 4100020719 with the Pennsylvania Department of Health. The Department specifically disclaims responsibility for the analyses, interpretations, or conclusions. C.C. is supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K23 HD051634). J. M.-H. is supported by the NIH Office of Research on Women's Health's Building Interdisciplinary Research Careers in Women's Health career development award, 5 K12 HD05582. The Penn State University Survey Research Center conducted the telephone surveys.
Disclosure Statement
No competing financial interests exist for any of the authors.
References
- 1.Flegal KM. Carroll MD. Ogden CL. Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM. Graubard BI. Williamson DF. Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007;298:2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- 3.Malnick SD. Knobler H. The medical complications of obesity. Q J Med. 2006;99:565–579. doi: 10.1093/qjmed/hcl085. [DOI] [PubMed] [Google Scholar]
- 4.Abenhaim HA. Kinch RA. Morin L. Benjamin A. Usher R. Effect of prepregnancy body mass index categories on obstetrical and neonatal outcomes. Arch Gynecol Obstet. 2007;275:39–43. doi: 10.1007/s00404-006-0219-y. [DOI] [PubMed] [Google Scholar]
- 5.Kaiser PS. Kirby RS. Obesity as a risk factor for cesarean in a low-risk population. Obstet Gynecol. 2001;97:39–43. doi: 10.1016/s0029-7844(00)01078-4. [DOI] [PubMed] [Google Scholar]
- 6.Sun Q. Townsend MK. Okereke OI. Franco OH. Hu FB. Grodstein F. Adiposity and weight change in mid-life in relation to healthy survival after age 70 in women: Prospective cohort study. BMJ. 2009;339:b3796. doi: 10.1136/bmj.b3796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stefanska A. Sypniewska G. Blaszkiesicz B. Ponikowska I. Szternel L. Chojnowski J. Long-term weight gain and metabolic syndrome, adiponectin and C-reactive protein in women aged 50–60 years. Adv Med Sci. 2010;22:1–5. doi: 10.2478/v10039-010-0047-y. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki R. Iwasaki M. Inoue M, et al. Body weight at age 20 years, subsequent weight change and breast cancer risk defined by estrogen and progesterone receptor status—The Japan Public Health Center-based prospective study. Int J Cancer. Nov 9, 2010. [Epub ahead of print] [DOI] [PubMed]
- 9.Beydoun MA. Beydoun HA. Wang Y. Obesity and central obesity as risk factors for incident dementia and its subtypes: A systematic review and meta-analysis. Obes Rev. 2008;9:204–218. doi: 10.1111/j.1467-789X.2008.00473.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manson JE. Willett WC. Stampfer MJ, et al. Body weight and mortality among women. N Engl J Med. 1995;333:677–685. doi: 10.1056/NEJM199509143331101. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine. Weight gain during pregnancy: Reexamining the guidelines. Washington DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 12.Johnson K. Posner SF. Biermann J, et al. Recommendations to improve preconception health and health care—United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep. 2006;55:1–23. [PubMed] [Google Scholar]
- 13.Ashton DM. Lawrence HC., 3rd Adams NL., 3rd Fleischman AR. Surgeon General's Conference on the Prevention of Preterm Birth. Obstet Gynecol. 2009;113:925–930. doi: 10.1097/AOG.0b013e31819bdba3. [DOI] [PubMed] [Google Scholar]
- 14.Roberts C. Troop N. Connan F. Treasure J. Campbell IC. The effects of stress on body weight: Biological and psychological predictors of change in BMI. Obesity (Silver Spring) 2007;15:3045–3055. doi: 10.1038/oby.2007.363. [DOI] [PubMed] [Google Scholar]
- 15.Block JP. He Y. Zaslavsky AM. Ding L. Ayanian JZ. Psychosocial stress and change in weight among US adults. Am J Epidemiol. 2009;170:181–192. doi: 10.1093/aje/kwp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sammel MD. Grisso JA. Freeman EW, et al. Weight gain among women in the late reproductive years. Fam Pract. 2003;20:401–409. doi: 10.1093/fampra/cmg411. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y. Beydoun MA. The obesity epidemic in the United States—Gender, age, socioeconomic, racial/ethnic, and geographic characteristics: A systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 18.Braveman PA. Cubbin C. Egerter S. Williams DR. Pamuk E. Socioeconomic disparities in health in the United States: What the patterns tell us. Am J Public Health. 2010;100(Suppl 1):S186–196. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fowler-Brown AG. Bennett GG. Goodman MS. Wee CC. Corbie-Smith GM. James SA. Psychosocial stress and 13-year BMI change among blacks: The Pitt County Study. Obesity (Silver Spring) 2009;17:2106–2109. doi: 10.1038/oby.2009.130. [DOI] [PubMed] [Google Scholar]
- 20.Purslow LR. Young EH. Wareham NJ, et al. Socioeconomic position and risk of short-term weight gain: Prospective study of 14,619 middle-aged men and women. BMC Public Health. 2008;8:112. doi: 10.1186/1471-2458-8-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weisman CS. Hillemeier MM. Chase GA, et al. Preconceptional health: Risks of adverse pregnancy outcomes by reproductive life stage in the Central Pennsylvania Women's Health Study (CePAWHS) Womens Health Issues. 2006;16:216–224. doi: 10.1016/j.whi.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 22.Weisman CS. Misra DP. Hillemeier MM, et al. Preconception predictors of birth outcomes: Prospective findings from the Central Pennsylvania Women's Health Study. Matern Child Health J. May 27, 2009. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 23.Garrow JS. Webster J. Quetelet's index (w/h2) as a measure of fatness. Int J Obes. 1985;9:147–153. [PubMed] [Google Scholar]
- 24.Huber LRB. Validity of self-reported height and weight in women of reproductive age. Matern Child Health J. 2007;11:137–144. doi: 10.1007/s10995-006-0157-0. [DOI] [PubMed] [Google Scholar]
- 25.American College of Sports Medicine (ACSM) ACSM's guidelines for exercise testing and prescription. 6th. Philadelphia: Lippincott, Williams & Wilkins; 2000. [Google Scholar]
- 26.American College of Obstetricians and Gynecologists (ACOG) Exercise during pregnancy and the postpartum period (Committee Opinion No. 267) Obstet Gynecol. 2002;99:171–173. doi: 10.1016/s0029-7844(01)01749-5. [DOI] [PubMed] [Google Scholar]
- 27.Chiolero A. Faeh D. Paccaud F. Cornuz J. Consequences of smoking for body weight, body fat distribution, and insulin resistance. Am J Clin Nutr. 2008;87:801–809. doi: 10.1093/ajcn/87.4.801. [DOI] [PubMed] [Google Scholar]
- 28.Weisman CS. Hillemeier MM. Downs DS. Chuang CH. Dyer AM. Preconception predictors of weight gain during pregnancy: Prospective findings from the Central Pennsylvania Women's Health Study. Womens Health Issues. 2010;20:126–132. doi: 10.1016/j.whi.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sherbourne CD. Dwight-Johnson M. Klap R. Psychological distress, unmet need, and barriers to mental health care for women. Womens Health Issues. 2001;11:231–243. doi: 10.1016/s1049-3867(01)00086-x. [DOI] [PubMed] [Google Scholar]
- 30.Onyike CU. Crum RM. Lee HB. Lyketsos CG. Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003;158:1139–1147. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- 31.Williamson DF. Kahn HS. Remington PL. Anda RF. The 10-year incidence of overweight and major weight gain in US adults. Arch Intern Med. 1990;150:665–672. [PubMed] [Google Scholar]
- 32.Rissanen A. Heliovaara M. Aromaa A. Overweight and anthropometric changes in adulthood: A prospective study of 17,000 Finns. Int J Obes. 1988;12:391–401. [PubMed] [Google Scholar]
- 33.Lewis CE. Jacobs DR., Jr McCreath H, et al. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Coronary Artery Risk Development in Young Adults. Am J Epidemiol. 2000;151:1172–1181. doi: 10.1093/oxfordjournals.aje.a010167. [DOI] [PubMed] [Google Scholar]
- 34.Schulz M. Kroke A. Liese AD. Hoffmann K. Bergmann MM. Boeing H. Food groups as predictors for short-term weight changes in men and women of the EPIC-Potsdam cohort. J Nutr. 2002;132:1335–1340. doi: 10.1093/jn/132.6.1335. [DOI] [PubMed] [Google Scholar]
- 35.Tiggemann M. Dietary restraint and self-esteem as predictors of weight gain over an 8-year time period. Eat Behav. 2004;5:251–259. doi: 10.1016/j.eatbeh.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 36.American Diabetes Association. Executive summary: Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(Suppl 1):S4–S10. doi: 10.2337/dc10-S004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lloyd-Jones DM. Hong Y. Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association's Strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 38.U.S. Preventive Services Task Force. Screening for obesity in adults. www.ahrq.gov/clinic/uspstf/uspsobes.htm. [Jul 1;2010 ]. www.ahrq.gov/clinic/uspstf/uspsobes.htm
- 39.Files JA. David PS. Frey KA. The patient-centered medical home and preconception care: An opportunity for internists. J Gen Intern Med. 2008;23:1518–1520. doi: 10.1007/s11606-008-0657-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yun S. Zhu BP. Black W. Brownson RC. A comparison of national estimates of obesity prevalence from the Behavioral Risk Factor Surveillance System and the National Health and Nutrition Examination Survey. Int J Obes (Lond) 2006;30:164–170. doi: 10.1038/sj.ijo.0803125. [DOI] [PubMed] [Google Scholar]
- 41.Engstrom JL. Paterson SA. Doherty A. Trabulsi M. Speer KL. Accuracy of self-reported height and weight in women: An integrative review of the literature. J Midwifery Womens Health. 2003;48:338–345. doi: 10.1016/s1526-9523(03)00281-2. [DOI] [PubMed] [Google Scholar]
- 42.Jain RB. Regression models to predict corrected weight, height and obesity prevalence from self-reported data: Data from BRFSS 1999–2007. Int J Obes (Lond) 2010;34:1655–1664. doi: 10.1038/ijo.2010.80. [DOI] [PubMed] [Google Scholar]
- 43.Krul AJ. Daanen HAM. Choi H. Self-reported and measured weight, height and body mass index (BMI) in Italy, the Netherlands, and North America. Eur J Public Health. 2010 doi: 10.1093/eurpub/ckp1228. Advance access. [DOI] [PubMed] [Google Scholar]
- 44.Wane S. van Uffelen JG. Brown W. Determinants of weight gain in young women: A review of the literature. J Womens Health. 2010;19:1327–1340. doi: 10.1089/jwh.2009.1738. [DOI] [PubMed] [Google Scholar]