Abstract
Nurses often encounter patients with chronic pelvic pain associated with endometriosis, which is a puzzling and problematic gynecologic condition that has continued to plague women and baffle doctors and researchers worldwide since it was first identified by Dr. J. Sampson in the 1920s (Sampson, 1940). Endometriosis is defined as the growth, adhesion and progression of endometrial glands and stroma outside of the uterine cavity, with cellular activity evident in lesions, nodules, cysts or endometriomas (Audebert et al., 1992). Although it typically appears benign on histopathology, endometriosis has been likened to a malignant tumor since the lesions grow, infiltrate and adhere to adjacent tissues and interfere with physiologic processes (Kitawaki et al., 2002; Noble, Simpson, Johns, & Bulun, 1996). Ectopic endometriotic growths respond to cyclic changes of estrogen and proliferate and shed in a manner similar to eutopic endometrium. This cyclic ectopic activity results in internal bleeding, formation of scar tissue, inflammation and sometimes debilitating chronic pain (Kitawaki et al.).
Background
The true prevalence of endometriosis is not known, as diagnostic confirmation is accomplished only by laparoscopy, and unknown numbers of women are either asymptomatic or do not seek treatment for their symptoms (Signorello, Harlow, Cramer, Spiegelman, & Hill, 1997). Endometriosis has been observed in 4 percent (range of 1 percent to 20 percent) of asymptomatic women undergoing laparoscopic tubal ligation (Signorello et al.; Wellbery, 1999). Approximately 20 percent (range of 2 percent to 78 percent) of women undergoing laparoscopic investigation for infertility and 24 percent (range 4 percent to 82 percent) of women investigated for pelvic pain have also been found to have endometriosis (Schenken, 1996; Wellbery). The estimated overall prevalence of endometriosis among symptomatic and asymptomatic women is 10 percent (Wellbery). Endometriosis afflicts women of reproductive age; the average age at first diagnosis is 28. There is no racial or socioeconomic predisposition to the condition; however, there does appear to be a familial correlation in women with severe disease (Dos Reis et al., 1999; Endometriosis Research Center, 2006; Moen & Magnus, 1993; Stefansson et al., 2002).
Endometriosis is thought to be the gynecologic manifestation of systemic pathology representing a range of health problems with underlying hormonal and/or immune disorders. Patients with endometriosis tend to develop additional symptoms such as allergies, fibromyalgia, asthma, eczema, autoimmune inflammatory disease, chronic fatigue syndrome and hypothyroidism (Sinaii, Cleary, Ballweg, Nieman, & Stratton, 2002). However, women with endometriosis have been found not to have a higher risk of thyroid dysfunction (Petta, Arruda, Zantut-Wittman, & Benetti-Pinto, 2007). There is also a higher risk of breast cancer in women diagnosed with endometriosis after age 40, because of their increased exposure to elevated endogenous estrogen (Bertelsen et al., 2007). Increased incidences of hematopoietic malignancies, such as non-Hodgkin’s lymphoma, may result from the altered immune system of a woman with endometriosis (Brinton, Gridley, Persson, Baron, & Bergqvist, 1998). Endometriosis explants have been found on the ovaries, bowel, pelvic cavity, intestines and bladder, as well as skin (scars), lungs, brain and nostrils (Endometriosis Research Center, 2006; Murphy, 2002). Endometriosis has also been observed in men undergoing hormonal therapy, although this is a rare finding (Murphy).
This paper provides a comprehensive review of endometriosis and the plight of patients who experience this disease. We’ll focus on the clinical appearance, chronic nature of the symptoms, pathophysiology and treatment options in order to bring a degree of organization to appreciating this multifaceted condition. Nurses are often the first health professionals patients encounter in settings such as community health clinics, schools, general practitioners’ offices, emergency rooms and surgery units (Cox, Henderson, Andersen, Cagliarini, & Ski, 2003; Cox, Henderson, Wood, & Cagliarini, 2003; Denny, 2004). With increased information, nurses can educate patients about endometriosis, help them cope emotionally and physically with the chronic symptoms they experience and reduce the feelings of helplessness and depression that often accompany it.
What Causes Endometriosis?
The pathophysiology of endometriosis remains unknown, although many theories have been developed to address this issue. The most accepted theories propose four potential causes: (a) retrograde menstruation (Sampson’s theory); (b) coelomic metaplasia; (c) vascular and lymphatic spread and (d) altered immunosurveillance.
Retrograde Menstruation
Sampson’s theory of retrograde menstruation postulates that viable endometrial cells are shed through the fallopian tubes into the peritoneum during menstruation, accumulate in the dependent portions of the pelvis and attach to pelvic walls and organs (Gazvani & Templeton, 2002; Lebovic, Mueller & Taylor, 2001; Sampson, 1940). This theory is most widely accepted, although it’s important to acknowledge that there is disagreement as many women (76 percent to 90 percent) experience a reflux of menstrual fluid into the pelvic cavity but don’t develop endometriosis (Garcia-Velasco, Arici, Zreik, Naftolin, & Mor, 1999; Garcia-Velasco, Mulayim, Kayisli, & Arici, 2002; Lebovic et al., 2001). Also, Sampson’s theory doesn’t explain the occurrence of remote implants of endometriosis, such as in the lung or nose (Murphy, 2002).
Coelomic Metaplasia
During the early weeks of gestation, the reproductive organs are developed from the embryonic germ layers of mesoderm and endoderm. The coelomic metaplasia theory postulates that metaplasia of the multipotential coelomic epithelium is the origin of endometriosis, as peritoneal and endometrial cells are both derived from the same embryonic precursor (Mounsey, Wilgus, & Slawson, 2006; Shaw, 1993). The presence of stress, such as inflammation or irritation from refluxed menstrual tissues, causes the coelomic cells that had differentiated previously into peritoneal cells to transform into endometrial cells, which respond in a cyclic manner (Wellbery, 1999). Many scientists criticize this theory, because it would suggest that higher rates of pleural endometriosis would be expected if this theory was valid.
Vascular and Lymphatic Spread
Vascular and lymphatic spread is associated with endometrial tissue infiltrating the local blood and lymphatic systems and being transported to distant sites in the body. This theory would explain the presence of endometriotic implants in distant and rare locations such as lungs, bone, skin, etc., but doesn’t explain the gravity-dependent location of implants, which accounts for most common presentations (Shaw, 1993).
Altered Immunosurveillance
The three previously mentioned theories have been criticized for being too superficial and limited, because they don’t explain the full scope of the disease. Recently, findings of altered immunosurveillance have been associated with the pathophysiology of endometriosis. A normally functioning immune system in a woman without endometriosis identifies and destroys the misplaced endometrial tissues, preventing their implantation (Dmowski, Gebel, & Braun, 1998). It’s theorized that endometriosis occurs either when the immune system is overwhelmed by the amount of menstrual backflow or when a defective immunosurveillance system allows the lesions to escape immunosurveillance, attach, establish a blood supply and continue to thrive (Braun & Dmowski, 1998; Gazvani & Templeton, 2002). Immune alterations caused by the presence of ectopic endometrial tissue within the pelvic cavity are believed to contribute to the disease process, as illustrated by the high level of irritation, resulting inflammation, locally augmented prostanoid production and high levels of activated peritoneal macrophages (Gazvani & Templeton; Noble et al., 1997; Schenken, 1996; Wellbery, 1999).
Role of Macrophages in Endometriosis
Macrophages are the most abundant type of cell (85 percent) found in the peritoneal fluid of women with no evidence of endometriosis (Gazvani & Templeton, 2002). While macrophage concentrations fluctuate during the menstrual cycle, they are normally elevated during menses (Braun et al., 2002; Gazvani & Templeton; Oral, Olive, & Arici, 1996). Activated macrophages release cytokines, growth factors and prostaglandins during menstruation in women who do not have endometriosis in order to regulate the peritoneal cavity by removing red blood cells, tissue fragments and foreign endometrial cells (Gazvani & Templeton). Women with endometriosis have a higher level of activated peritoneal macrophages (Garcia-Velasco et al., 1999; Gazvani & Templeton; Oral et al.). Therefore, the increased expression of cytokines and growth factors from the macrophages and their effects on the peritoneal environment is associated with the pathophysiology of endometriosis (Berkkanoglu & Arici, 2003; Garcia-Velasco et al., 1999).
Maintenance of Ectopic Endometrial Lesions
Endometrial implants have estrogen receptors (Gazvani & Templeton, 2002; Kitawaki et al., 2002). The lesions respond to cyclic levels of hormones demonstrated by their growth and proliferation as estrogen produced by developing follicles increases. Endometriosis regresses after oophorectomy or menopause, when the levels of estrogen are decreased, but will relapse when a woman is treated with estrogen replacement therapy (Kitawaki et al.; Ulukus, Cakmak, & Arici, 2006). This phenomenon has established endometriosis as a disease that is estrogen-dependent (Bulun et al., 2002).
Prostaglandins, such as PGE2 and PGF2α, are secreted in significantly higher levels from eutopic and ectopic endometrial cells in women with endometriosis (Dmowski et al., 1998; Gazvani & Templeton, 2002). Higher levels of PGE2 increase estrogen biosynthesis (Noble et al., 1997) by creating a positive feedback system favoring continuous estrogen production (Bulun et al., 1999; Bulun, Zeitoun, Takayama, & Sasano, 2000; Gazvani & Templeton; Noble et al.; Ulukus et al., 2006; Zeitoun & Bulun, 1999).
Clinical Appearance of Endometriosis
Signs and Symptoms
The symptoms of endometriosis vary in their presentation and severity; however, the most common symptom is pelvic pain (Schenken, 1996). The pain usually begins one or two days before expected menstruation, may be unilateral or bilateral, and lasts until the end of menses (Schenken; Wellbery, 1999). However, some women may experience a constant, debilitating pain that interferes with their daily lives (Cox, Henderson, Andersen et al., 2003; Denny & Mann, 2007; Jarrell, 2004; Murphy, 2002; Wesselmann & Czakanski, 2001). Curiously, the severity of pain does not correlate well with severity of the condition and, therefore, severe disease may go undiagnosed (Audebert et al., 1992; Murphy; Olive & Pritts, 2001; Schenken). Women with endometriosis may also experience a wide variety of other symptoms including dyspareunia, dysmenorrhea, dyschezia, dysuria, gastrointestinal complaints, rectal bleeding with significant bowel involvement, menstrual dysfunction such as oligomenorrhea or hypermenorrhea, low back pain and infertility (Chopin et al., 2006; Lemaire, 2004; Schenken; Signorello et al., 1997; Wellbery).
Physical Examination
Physicians or nurse practitioners should palpate for endometriosis-related lesions during early menses as the implants are most likely large and tender at this phase of the menstrual cycle (Wellbery, 1999). A common physical finding is cul-de-sac tenderness, with multiple tender nodules palpated along the cul-de-sac or uterosacral ligaments. Adnexal masses or adhesions are palpated bimanually, while deep infiltrated lesions involving the rectovaginal septum are palpated rectovaginally (Schenken, 1996). However, physical findings can vary depending on the location, severity of disease and severity of symptoms and will often appear within normal limits (Wellbery).
Surgical Findings
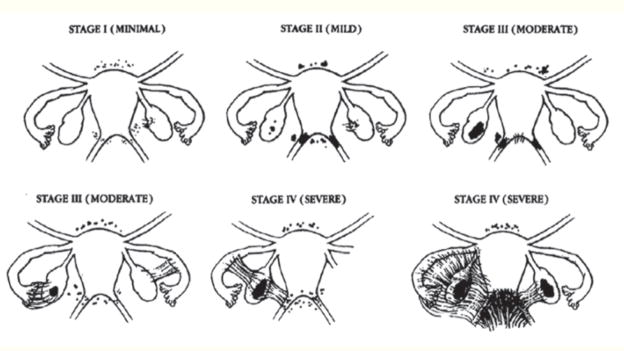
Endometriotic lesions are highly variable in size, shape and color when viewed at laparoscopy (see Figure 1). They can range in size from microscopic measurements to 10 cm endometriomas that obliterate the cul-de-sac. Despite the variability of appearance, endometriosis can be classified into three major categories based on the location within the pelvis: (a) peritoneal, (b) ovarian and (c) deep nodular (Brosens, 1997a) (see Box 1).
Figure 1. Laparoscopic visualization of endometrial lesions (A – F).
(A)Isolated red lesions located on broad ligament. (B)Multiple red lesions adjacent to sigmoid colon. Laparoscopic instrument visualized in the top center portion of image. Lesions visualized directly to left of instrument. (C)Hemorrhagic lesion located on sigmoid colon in the center of the image. (D)Hemorrhagic lesion on broad ligament posterior to round ligament. Lesion is located immediately to right of laparoscopic instrument. (E)Adhesions formed at base of oviduct adjacent to the uterus. Hemorrhagic endometrial lesions located at left of image with filmy adhesions. (F)Filmy adhesions and hemorrhagic lesion located at distal portion of oviduct.
Box 1. Types of Endometriosis.
Peritoneal Endometriosis: This is also known as “superficial endometriosis” and has many appearances ranging from red, vesicular and hemorrhagic; puckered, blue-black powder-like burn patterns; or fibrotic lesions white to black in color. The red lesions are highly vascular, bleed into the peritoneal cavity during menstruation, and are associated with early neoangiogenesis, adhesion formation and inflammation. Dark or white lesions are correlated with higher amounts of fibrosis, decreased vascularity and decreased bleeding. Peritoneal endometriotic implants can change appearance and location and even regress with medical treatment, but often reappear after cessation of treatment and return of the menstrual cycle (Brosens, Puttermans, Campo & Gordts, 2004; Brosens, 1997a, 1997b).
Ovarian Endometriosis: Endometriotic lesions or pseudo uterine cavities on the ovary are most often visualized as dark brown cystic structures. The endometriotic cyst does not invade the ovary, but is most likely formed by attachment of an endometriotic hematoma to the surface of the ovary. The cysts can be completely or partially lined by endometrial-like mucosa and surface epithelium as well as highly vascularized stroma (Brosens et al., 2004). Bleeding or rupture of an ovarian endometrioma can cause an acute abdominal emergency requiring surgery in approximately 5 percent of women with endometriosis (Schenken, 1996).
Deep Nodular Endometriosis: These endometrial lesions can be found in the rectovaginal septum, uterosacral ligaments, utero-ovarian ligaments and muscular wall of pelvic organs. Endometrial glands and stroma invade into adjacent fibromuscular tissue along loose connective tissue, but are arrested at the underlying fat tissue level (Brosens, 1997b).
Diagnosing Endometriosis
Diagnosis of endometriosis is difficult to confirm due to the wide variety of appearances and symptoms, as well as the unreliable correlation between clinical presentation and surgical findings (Wellbery, 1999). Endometriosis should be considered especially if patients present with dysmenorrhea after having previous pain-free menstrual cycles (Schenken, 1996; Wellbery). Diagnostic laparoscopy for visualization and biopsy of lesions remains the gold standard for diagnosis after ruling out other causes of pelvic pain, such as upper genital tract infection, adenomyosis and pelvic inflammatory disease (Barbieri & Missmer, 2002; Brosens, 1997a; Endometriosis Research Center, 2006; Lemaire, 2004; Kang, Chung, Lee, Lee, & Chang, 2006; Schenken), as noninvasive methods for predicting disease prior to surgery are only moderately successful (Eskenazi et al., 2001). It’s important to note that not all endometriosis lesions are visualized at surgery; lesions may be hidden by pelvic organs or adhesions, microscopic or similar in appearance to other malignant or benign lesions such as ovarian cancer, hemangioma or ectopic pregnancy (Brosens, Puttemans, Campo, & Gordts, 2004). Therefore, techniques such as peritoneal fluid aspiration, lysis of adhesive disease, mobilization of adherent structures from the pelvic wall and biopsy of lesions are typically performed to thoroughly examine the cul-de-sac and pelvic organs and confirm the presence of endometriosis (Brosens et al.; Schenken).
Laparoscopy
Diagnosis of endometriosis at laparoscopy is dependent on the skill and experience of the surgeon (Barbieri & Missmer, 2002), thoroughness of examination, preoperative bias or presence of other pelvic pathology (Fauconnier & Chapron, 2005; Schenken, 1996). The surgeon must be knowledgeable about common locations and the variable appearances of the disease. The classification and staging guidelines developed by the American Society of Reproductive Medicine (ASRM) are useful to assist in diagnosing and documenting the location, appearance and extent of endometriotic lesions (ASRM, 1996, 2006; Schenken; Wellbery, 1999).
Imaging Techniques
In theory, imaging techniques such as endorectal ultrasonography, transvaginal ultrasonography, computed tomography (CT) and magnetic resonance imaging (MRI) could be used to confirm the presence of endometriosis preoperatively, but, unfortunately, imaging remains limited in establishing a definitive diagnosis (Schenken, 1996; Wellbery, 1999). Endorectal ultrasonography is a reliable tool but is limited to identifying rectal infiltration associated with deep pelvic endometriosis (Bahr et al., 2006; Bazot et al., 2007). Transvaginal ultrasonography can be used to identify size, shape and location of ovarian (Bazot et al., 2003; Mais et al., 1993) and bladder lesions (Fedele, Bianchi, Raffaelli, & Portugese, 1997) but it may be difficult to distinguish among ovarian endometriomas, cysts, tumors, ectopic pregnancies, tubal cysts or abscesses (Schenken). The usefulness of Doppler ultrasonography for diagnostic purposes is uncertain, as the high variability of endometriosis presentation continues to confound imaging results. MRI can be used to detect up to 82 percent of endometriomas greater than or equal to 1 cm and 50 percent of hemorrhagic lesions less than or equal to 5 mm due to the small implant size and variable appearance (Brosens et al., 2004). CT, MRI and ultrasonography are unfortunately associated with a high rate of false positive diagnoses of structures such as blood vessels, small bowel, corpora lutea, lutein cysts, teratoma, ovarian fibroids, tubal ovarian abscess and carcinoma (Brosens et al.; Schenken). Therefore, these imaging techniques are not specific or sensitive enough to be a cost-effective preoperative diagnostic option (Schenken).
Classifying Endometriosis
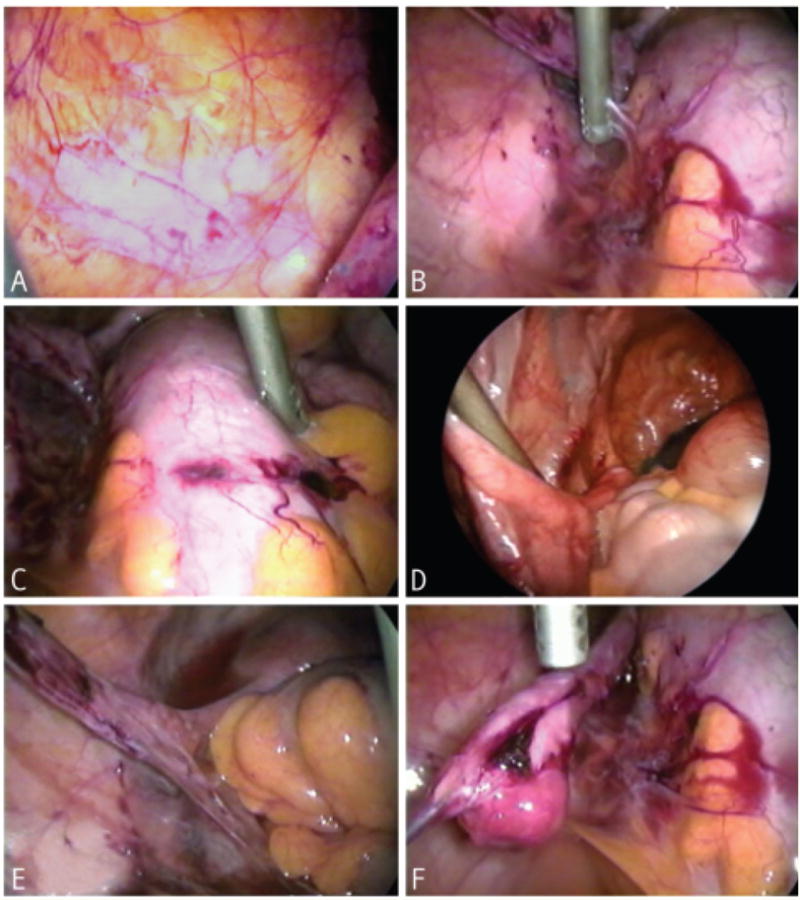
The ASRM has developed classification and staging guidelines to assist with diagnosis, prognosis, treatment, subsequent progress and communication among medical professionals (ASRM, 2006; Wellbery, 1999). In this standardized scheme, endometriosis is classified into four stages as illustrated in Figure 2: Stage I (minimal), Stage II (mild), Stage III (moderate) and Stage IV (severe). Staging is based on the extent of the spread of lesions, density of pelvic adhesions, involvement of pelvic organs and degree of fallopian tube occlusion (ASRM). It’s important to remember that the stage of endometriosis is not reflective of degree of pain, risk of infertility or predictive of the patient’s ability to conceive after therapy (ASRM; Audebert et al., 1992). Women with minimal or mild endometriosis have been found to have high degrees of pain and infertility, while asymptomatic women have been diagnosed with Stage IV on laparoscopy for tubal ligation. The variability in clinical presentation and stage of disease likely reflects of our lack of understanding of the pathophysiology of endometriosis. Until a better understanding of the pathophysiology is achieved, the classification system will not be improved (ASRM; Wellbery).
Figure 2. Schematic classification examples of extent and location of endometriosis.
Adapted from the Revised American Society for Reproductive Medicine Classification of Endometriosis (1996).
Endometriosis and Infertility
An association between endometriosis, pelvic pain and infertility was first suggested in the 1920s by J. Sampson (1940). Theoretically, adhesions, cysts and lesions in the pelvic cavity have the potential to impair folliculogenesis and ovulation, limit fimbrial mobility, inhibit ovum pickup and occlude the fallopian tubes, impeding fertilization or causing dyspareunia, which can limit sexual activity (Barbieri & Missmer, 2002; Dokras & Olive, 1999; Martinez-Roman et al., 1997; Olive & Pritts, 2001). However, many women with little anatomic distortion have been found to experience infertility as well (Burns & Schenken, 1999). Impairment of oocyte fertilization resulting from pituitary-ovarian (Cahill & Hull, 2000) or endometrial dysfunction (Lessey, 2002) may also be factors affecting fertility. Nevertheless, a cause and effect relationship between infertility and endometriosis has not been established (ASRM, 2006; Barbieri & Missmer; Cahill & Hull; Jarrell, 2004; Oral et al., 1996; Schenken, 1996).
Serum levels of estradiol, progesterone, testosterone and androstenedione have been found to be similar between women with and without endometriosis (Pellicer, Albert et al., 1998; Pellicer, Valbuena et al., 1998). However, differences were discovered in the follicular fluid of follicles aspirated for in vitro fertilization, which led to the speculation that oocytes and embryos of endometriosis patients are of decreased ability to be fertilized. Levels of progesterone were increased and positively correlated to the stage of disease, whereas testosterone levels were decreased in the follicular fluid, which may lead to oocyte damage (Pellicer, Valbuena et al.). Women who did not have endometriosis had a fertilization rate of 69 percent compared with 46 percent for women with endometriosis (Cahill, Wardle, Maile, Harlow, & Hull, 1997). It’s also an important observation that fertilization and implantation rates are lower when embryos from patients with endometriosis were transferred back into the same patient, but were higher when patients with severe disease received embryos from ovum donors (Pellicer, Albert et al.; Pellicer, Valbuena et al.).
Chronic Pelvic Pain
Chronic pelvic pain is defined as nonmenstrual pain in the pelvic region lasting six or more months (Butrick, 2007; Howard, 2001; Jarrell, 2004; Wesselman, 2001). Chronic pelvic pain causes neurological changes in the dorsal horn of the spine, resulting in neurogenic inflammation of multiple pelvic viscera, hyperalgesia, dysreflexia, a lower sensory threshold and, therefore, a greater perception of pain (Butrick; Wesselman). Endometriosis is observed in 71 to 87 percent of women with chronic pelvic pain (Ozawa et al., 2006); however, pelvic pain is also commonly associated with other conditions, including interstitial cystitis, irritable bowel syndrome and adhesions. Patients may experience more than one source of pain (Bordman & Jackson, 2006; Fauconnier & Chapron, 2005), which may also radiate to areas such as the perineum, thighs, abdomen and lower back (Wesselman). Therefore, each source of pain must be identified and treated individually (Butrick; Howard).
Women’s Experiences With Endometriosis
For most women living with endometriosis, the road to diagnosis and treatment can be long, painful and frustrating (Ballard, Lowton, & Wright, 2006; Sinaii, Cleary, Younes, Ballweg, & Stratton, 2007). The mean time from onset of symptoms to diagnosis for women with endometriosis in the United States is 11.73±9.05 years; for women in the United Kingdom it’s 7.96±7.92 years (Hadfield, Mardon, Barlow, & Kennedy, 1996). Women may delay seeking medical attention in the mistaken belief that painful symptoms are part of a “normal” menstruation, especially if there is a family history of “difficult periods,” or fears of appearing unable to cope with “female problems” (Ballard et al.). Also, medical professionals who lack knowledge about the severity of pain that women with endometriosis often suffer may trivialize symptoms, attribute pain to being a normal part of menstruation or dismiss symptoms as being imaginary (Ballard et al.; Cox, Henderson, Andersen et al., 2003; Denny, 2004; Huntington & Gilmour, 2005). This failure of validation often delays referrals to gynecologists or other health professionals specializing in chronic pain management. This cascade leads to increased frustration, depression and anger as these women experience a lack of understanding, empathy and caring for their condition (Cox, Henderson, Andersen et al.; Cox, Henderson, Wood et al., 2003).
During this time, patients must live with chronic pain that affects their careers, relationships and feelings of self-worth (Cox, Henderson, Andersen et al., 2003; Denny, 2004; Gao et al., 2006; Huntington & Gilmour, 2005). In addition, women with endometriosis often experience higher incidents of depression (Hodgkiss & Watson, 1994) and emotional distress due to the uncertainty of diagnosis, unpredictability of symptoms and repeated dismissal of their experiences (Lemaire, 2004). Further descriptions of women’s experiences of struggling with endometriosis are described from a qualitative viewpoint in Cox, Henderson, Anderson et al., Huntington and Gilmour (2005).
Treatment Options
Plans of treatment for endometriosis typically start with the least invasive approach and progress to more invasive interventions. However, clinical symptoms, intensity of symptoms, stage of disease, reaction to previous treatment methods and concern for future pregnancy are also taken into consideration. It’s important to note that 10 to 20 percent of women with endometriosis have a recurrence of disease regardless of which treatment they receive. Evidence-based guidelines for the treatment of endometriosis are continually updated and are accessible through the European Society for Human Reproduction & Embryology (ESHRE) Web site or the National Guideline Clearinghouse Web site (see “Get the Facts” box).
Get the Facts.
Endometriosis.org www.endometriosis.org
ESHRE guidelines.endometriosis.org
National Guideline Clearinghouse www.guideline.gov
The Endometriosis Association www.endometriosisassn.org
Medical Treatment
The goal of medical treatment of endometriosis is to reduce the amount of estrogen in the body so that menstruation, resultant internal bleeding and irritation is interrupted or decreased (Wellbery, 1999). Medicinal therapies are highly effective for regression of the majority of implants and the resulting inflammation. However, some endometriotic cysts are enclosed by adhesions and, therefore, have limited vascularity compared with other lesions, which may explain the variance in response to hormonal treatment among implants (Brosens, 1997b). Decreasing the amount of available estrogen decreases the severity of the lesions and accompanying pain, but doesn’t improve pregnancy rates. It’s important to understand that most patients must discontinue medical treatment of endometriosis to achieve a pregnancy. Endometriotic lesions and the associated symptoms unfortunately recur when medical treatment is discontinued and estrogen levels increase during the follicular phase of the menstrual cycle (Schenken, 1996; Wellbery). Box 2 outlines the most common types of medical treatment.
Box 2. Treatments for Endometriosis.
Type of Treatment Combination oral contraceptives (COCs)
Mechanism of Action
Contains progestins and an orally active estrogen, which suppresses gonadotropins via a negative feedback on gonadotropin-releasing hormone (GnRH) in the hypothalamus (Canadian Pharmacists Association [CPA], 2006)
Prevents ovulation (CPA, 2006)
Causes endometrial atrophy (CPA, 2006)
Relieves pain by thinning of endometrial lining and causing regression of the endometriotic implants (Crosignani et al, 2006)
Potential Adverse Effects
Irregular bleeding, weight gain, headache, thrombophlebitis, pulmonary embolism, neuro-occular lesions, cerebral thrombosis and hemorrhage, hypertension, benign liver tumors and gallbladder disease (CPA, 2006; Crosignani et al, 2006)
Treatment Duration and Results
Discontinue after 6 to 12 months or use indefinitely if patient is satisfied with symptom relief and doesn’t want to become pregnant in the near future (ASRM, 2006; Wellbery, 1999)
Alleviates symptoms in approximately 75 percent of patients (ASRM, 2006; Wellbery, 1999)
Type of Treatment Gonadotropin inhibitors: Danazol (Danocrine, Cyclomen)
Mechanism of Action
Synthetic androgen acts as a pituitary gonadotropin inhibitor (CPA, 2006)
Suppresses the mid-cycle surges of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) (CPA, 2006; Wellbery, 1999)
Inhibits enzymes involved with gonadal hormone synthesis (CPA, 2006; Crosignani et al, 2006; Kitawaki et al, 2002)
Competes with steroid receptors at target tissues (CPA, 2006; Crosignani et al, 2006; Kitawaki et al, 2002)
Pain relief is due to a hypo-estrogenic environment, endometrial atrophy and regression of lesions (CPA, 2006; Wellbery, 1999)
Potential Adverse Effects
Headaches, flushing, sweating, atrophic vaginitis, acne, edema, hirsutism, deepening of voice, amenorrhea and weight gain (CPA, 2006; Olive & Pritts, 2001)
Is contraindicated in pregnancy (CPA, 2006)
Treatment Duration and Results
Approximately 6 months due to adverse events, but can be as long as 9 months with Stage IV disease (Crosignani et al, 2006; Wellbery, 1999)
84 to 92 percent of patients responded well to this treatment and experienced beneficial effects of symptom relief up to 6 months after discontinuation of Danazol (Wellbery, 1999)
Type of Treatment GnRH agonists: Leuprolide (Lupron), Gosarelin (Zoladex), Nafarelin (Synarel nasal spray)
Mechanism of Action
A more potent synthetic analog of gonadotropin-releasing hormone
Produces a hypo-estrogenic environment by inhibiting the production of gonadotropins (CPA, 2006; Crosignani et al, 2006, Gambone et al, 2002)
Potential Adverse Effects
Hot flashes, vaginal dryness, emotional lability, loss of libido (Crosignani, 2006)
Mild degree of bone loss during treatment but is reversible (CPA, 2006)
May also prescribe progestins or COC due to osteopenia concerns
Treatment Duration and Results
Treatment limited to 6 months due to decrease in bone mineral density (Crosignani et al, 2006)
Comparable to Danazol with regard to pain relief (90 percent symptom alleviation)
Type of Treatment Progestational agents: Medroxyprogesterone (Depo-Provera)
Mechanism of Action
Has similar inhibitory effects as COCs with regard to suppressing gonadotropins and thinning endometrial tissue (CPA, 2006)
Inhibits angiogenesis of implants (Crosignani, 2006)
Potential Adverse Effects
Weight gain, headache, abdominal discomfort and irregular bleeding (CPA, 2006)
Treatment Duration and Results
Treatment outcomes similar to COCs
Less expensive than Danazol or GnRH analogs (ASRM, 2006; Wellbery, 1999)
Type of Treatment Aromatase inhibitors: Anastrozole (Arimidex), Letrozole (Femara)
Mechanism of Action
Ectopic implants express elevated levels of P450 expression, which converts androgens to estrogens (Takayama et al, 1998)
Decreases the local synthesis of estrogen by inhibiting androgen conversion (Amerstam et al, 2005; Attar & Bulun, 2006; Soysal et al, 2004)
Potential Adverse Effects
Mild headache, nausea, diarrhea, mild hot flashes and increased risk of osteoporosis with long-term use
May also prescribe progestins or COCs due to osteopenia concerns (Attar & Bulun, 2006; Razzi et al, 2004)
Treatment Duration and Results
Treatment limited to 6 months due to decrease in bone mineral density
90 percent of patients experience symptom alleviation during (Ailawadi et al, 2004) and up to 15 months post-treatment (Shippen & West, 2004)
Surgical Treatment
Diagnostic laparoscopy with biopsy of lesions is currently the only accurate method to diagnose endometriosis. Surgical treatment is normally carried out immediately following confirmation of the disease at the time of surgery (ASRM, 2006; Wellbery, 1999). Therefore, surgical treatment occurs prior to medical treatment with most patients (ASRM). Surgical removal of lesions, adhesions and cysts via excision, electrocautery, laser vaporization and restoration of pelvic anatomy is the preferred method of treatment for infertile patients with Stages III–IV endometriosis (ASRM; Schenken, 1996; Wellbery). The recurrence rate of endometriotic lesions after five years is 19 percent with laparoscopic removal of lesions and 10 percent with hysterectomy and bilateral oophorectomy; this is compared with 53.4 percent with medical treatment (ASRM). However, this doesn’t reflect the recurrence rate of pain as many women have a recurrence of pelvic pain (Butrick, 2007). Uterosacral nerve ablation and presacral neurectomy may also be considered to attempt to relieve chronic pelvic pain (Gambone et al., 2002); however, others have found that laparoscopic laser ablation of lesions is more effective for women with minimal to moderate endometriosis (Sutton, Pooley, Jones, Dover, & Haines, 2001).
Ablation of the endometriotic lesions in cases of Stages I–II endometriosis has been associated with an approximately 13 percent increase in pregnancy rates and a significant reduction in pelvic pain for 20 to 36 months after surgery. In cases of Stages III–IV endometriosis without the presence of other fertility issues, the probability of achieving a pregnancy increased 45 percent in the 12 months and 63 percent in the 24 months following surgical treatment (ASRM, 2006; Schenken, 1996). Currently, surgical treatment focuses on diagnosis of endometriosis and removing lesions thought to be the source of pain. The neurologic changes associated with chronic pain are not addressed in this situation and patients often experience a recurrence of pelvic pain (Butrick, 2007).
Combined Surgical and Medical Treatment
Medical treatment before or after surgical excision of endometriosis is theoretically advantageous. Unfortunately, fertility is not enhanced and fertility treatment may be unnecessarily postponed. Initiating medical treatment before surgery decreases endometriotic lesions, reduces vascularity, reduces blood loss and decreases the invasiveness of surgery (Marcoux, Maheux, Berube, & The Canadian Collaborative Group on Endometriosis, 1997; ASRM, 2006). Postoperative medical treatment eliminates lesions that were inoperable due to their location or microscopic size. Women who don’t experience a decrease in pain with surgical or medical treatment and no longer desire a pregnancy have the option of hysterectomy and oophorectomy (Gambone et al., 2002; Seydel, Sickel, Warner, & Sax, 1996). In mild or moderate cases of endometriosis, one ovary may be surgically removed, leaving one ovary to maintain function, although the patient will not experience the same amount of symptom alleviation as with bilateral oophorectomy. Patients who undergo a bilateral oophorectomy should be treated with hormone replacement therapy as the benefits outweigh the risk of endometriosis recurrence (ASRM).
Implications for Nursing Care
Learning about the causes and potential treatments for endometriosis is an important step in remedying the negative experiences many women encounter (Lemaire, 2004). The emotional distress and uncertainty that accompanies endometriosis can be decreased by providing patients with education and support (Lemaire). Education regarding menstrual experiences with endometriosis should start at a premenarchal age through elementary health courses to eliminate the notion that painful menstruation is “normal” (Ballard et al., 2006). It’s also useful to encourage patients to recording symptoms in a diary to help identify any possible cyclic patterns (Lemaire). As well, a complete health history must be taken focusing on specific symptoms such as location, severity, characteristics of pain and how activities of daily living are affected when a patient presents with pelvic pain (Bordman & Jackson, 2006; Howard, 2001).
Therapeutic listening is an important aspect of nursing care; it reflects respect and a trusting rapport with the patient (Alford, 1968; Huntington & Gilmour, 2005), allowing the patient to disclose sensitive issues such as dyspareunia (Denny, 2004).
Nurses can help empower patients by educating them about their condition, including planning their treatment and discussing possible alternative methods of pain control, such as modification to diet and activity levels (Cox, Henderson, Wood et al., 2003; Lemaire, 2004). Neurotransmitters may be altered in a depressive state, affecting the patient’s threshold for pain; therefore, treatment for depression must be addressed as well (Jarrell, 2004). A multidisciplinary approach to treatment with a health care team that includes dietitians, physiotherapists, psychologists and chronic pain specialists is most effective in treating endometriosis on a long-term basis (Howard, 2001). The use of alternative medicinal therapy has not been well-supported for the treatment of endometriosis; however, many women do find relief from symptoms and, therefore, should be encouraged to continue practicing these methods (Lemaire). Nurses can offer much needed emotional support to help patients cope with symptoms and complications (Alford, 1968; Lemaire) by encouraging open discussions as well as by referring patients to local or online support groups such as the Endometriosis Association (see “Get the Facts” box) (Denny, 2004; Huntington & Gilmour, 2005; Lemaire).
Conclusion
Endometriosis remains a troubling and enigmatic gynecologic condition that affects many women. Several theories attempt to explain the unknown pathophysiology of this disease, including retrograde menstruation, coelomic metaplasia, lymphatic/vascular infiltration and immune system dysfunction. Endometriosis has been associated with infertility, but a cause and effect relationship has not been established. The varying signs, symptoms and clinical appearances of the disease combined with the high rates of recurrence make diagnosis and treatment difficult for doctors. Nurses can play a significant role in facilitating diagnosis, providing patient education and emotional support, and alleviating patients’ negative experiences. More research into the etiology of endometriosis is needed to generate a better understanding of this enigmatic condition, so that more successful treatment options may be developed.
Bottom Line.
Endometriosis is a painful condition that affects many women.
It has been associated with infertility, but a cause-and-effect relationship has not been proved.
Nurses can play a significant role in facilitating diagnosis, providing patient education and support, and alleviating patients’ negative experiences.
Acknowledgments
The authors thank Dr. Donna R. Chizen for contributing laparoscopic images of endometrial lesions and John Deptuch for his technical assistance. Funding for this article was provided by the Canadian Institutes of Health Research.
References
- Ailawadi RK, Jobanpufra S, Kataria M, Gurates B, Bulun SE. Treatment of endometriosis and chronic pelvic pain with Letrozole and norethindrone acetate: A pilot study. Fertility and Sterility. 2004;81(2):290–296. doi: 10.1016/j.fertnstert.2003.09.029. [DOI] [PubMed] [Google Scholar]
- Alford D. Nursing care of the patient with endometriosis. Nursing Clinics of North America. 1968;3(2):217–227. [PubMed] [Google Scholar]
- American Society for Reproductive Medicine. Revised American society for reproductive medicine classification of endometriosis: 1996. Fertility and Sterility. 1996;67(5):817–821. doi: 10.1016/s0015-0282(97)81391-x. [DOI] [PubMed] [Google Scholar]
- American Society for Reproductive Medicine. Endometriosis and infertility. Fertility and Sterility. 2006;86(4):156–160. [Google Scholar]
- Attar E, Bulun SE. Aromatase inhibitors: The next generation of therapeutics for endometriosis? Fertility and Sterility. 2006;85(5):1307–1318. doi: 10.1016/j.fertnstert.2005.09.064. [DOI] [PubMed] [Google Scholar]
- Audebert A, Backstrom T, Barlow DH, Benagiano G, Brosens I, Buhler K, et al. Endometriosis 1991: A discussion document. Human Reproduction. 1992;7(3):432–435. doi: 10.1093/oxfordjournals.humrep.a137665. [DOI] [PubMed] [Google Scholar]
- Bahr A, de Parades V, Gadonneix P, Etienney I, Salet-Lizee D, Villet R, et al. Endorectal ultrasonography in predicting rectal wall infiltration in patients with deep pelvic endometriosis: A modern tool for an ancient disease. Diseases of the Colon and Rectum. 2006;49:869–875. doi: 10.1007/s10350-006-0501-x. [DOI] [PubMed] [Google Scholar]
- Ballard K, Lowton K, Wright J. What’s the delay? A qualitative study of women’s experiences of reaching a diagnosis of endometriosis. Fertility and Sterility. 2006;86(5):1296–1301. doi: 10.1016/j.fertnstert.2006.04.054. [DOI] [PubMed] [Google Scholar]
- Barbieri RL, Missmer S. Endometriosis and infertility: A cause-effect relationship? Annals New York Academy of Sciences. 2002;955:23–33. doi: 10.1111/j.1749-6632.2002.tb02762.x. [DOI] [PubMed] [Google Scholar]
- Bazot M, Bornier C, Dubernard G, Roseau G, Cortez A, Darai E. Accuracy of magnetic resonance imaging and rectal endoscopic sonography for the prediction of location of deep pelvic endometriosis. Human Reproduction. 2007;22(5):1457–1463. doi: 10.1093/humrep/dem008. [DOI] [PubMed] [Google Scholar]
- Bazot M, Detchev R, Cortez A, Amouyal P, Uzan S, Darai E. Transvaginal sonography and rectal endoscopic sonography for the assessment of pelvic endometriosis: A preliminary comparison. Human Reproduction. 2003;18(8):1686–1692. doi: 10.1093/humrep/deg314. [DOI] [PubMed] [Google Scholar]
- Berkkanoglu M, Arici A. Immunology and endometriosis. American Journal of Reproductive Immunology. 2003;50:48–59. doi: 10.1034/j.1600-0897.2003.00042.x. [DOI] [PubMed] [Google Scholar]
- Bertelsen L, Mellemkjaer L, Frederiksen K, Kjaer SK, Brinton LA, Sakoda LC, et al. Risk for breast cancer among women with endometriosis. International Journal of Cancer. 2007;120:1372–1375. doi: 10.1002/ijc.22490. [DOI] [PubMed] [Google Scholar]
- Bordman R, Jackson B. Below the belt: Approach to chronic pelvic pain. Canadian Family Physician. 2006;52(12):1556–1562. [PMC free article] [PubMed] [Google Scholar]
- Braun DP, Ding J, Shen J, Shen J, Rana N, Fernandez BB, et al. Relationship between apoptosis and the number of macrophages in eutopic endometrium from women with and without endometriosis. Fertility and Sterility. 2002;78(4):830–835. doi: 10.1016/s0015-0282(02)03334-4. [DOI] [PubMed] [Google Scholar]
- Braun DP, Dmowski WP. Endometriosis: Abnormal endometrium and dysfunctional immune response. Current Opinion in Obstetrics and Gynecology. 1998;10(5):365–369. doi: 10.1097/00001703-199810000-00003. [DOI] [PubMed] [Google Scholar]
- Brinton LA, Gridley G, Persson I, Baron J, Bergqvist A. Cancer risk after a hospital discharge diagnosis of endometriosis. American Journal of Obstetrics and Gynecology. 1998;176(3):572–579. doi: 10.1016/s0002-9378(97)70550-7. [DOI] [PubMed] [Google Scholar]
- Brosens IA. Diagnosis of endometriosis. Seminars in Reproductive Endocrinology. 1997a;15(3):229–233. doi: 10.1055/s-2008-1068752. [DOI] [PubMed] [Google Scholar]
- Brosens IA. Endometriosis: A disease because it is characterized by bleeding. American Journal of Obstetrics and Gynecology. 1997b;176(2):263–267. doi: 10.1016/s0002-9378(97)70482-4. [DOI] [PubMed] [Google Scholar]
- Brosens I, Puttemans P, Campo R, Gordts S. Diagnosis of endometriosis: Pelvic endoscopy and imaging techniques. Best Practice and Research Clinical Obstetrics and Gynaecology. 2004;18(2):285–303. doi: 10.1016/j.bpobgyn.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Bulun SE, Yang S, Fang Z, Gurates B, Tamura M, Sebastian S. Estrogen production and metabolism in endometriosis. Annals New York Academy of Sciences. 2002;955:75–85. doi: 10.1111/j.1749-6632.2002.tb02767.x. [DOI] [PubMed] [Google Scholar]
- Bulun SE, Zeitoun K, Takayama K, Noble L, Michael D, Simpson E, et al. Estrogen production in endometriosis and use of aromatase inhibitors to treat endometriosis. Endocrine-Related Cancer. 1999;6(2):293–301. doi: 10.1677/erc.0.0060293. [DOI] [PubMed] [Google Scholar]
- Bulun SE, Zeitoun KM, Takayama K, Sasano H. Molecular basis for treating endometriosis with aromatase inhibitors. Human Reproduction Update. 2000;6(5):413–418. doi: 10.1093/humupd/6.5.413. [DOI] [PubMed] [Google Scholar]
- Burns WN, Schenken RS. Pathophysiology of endometriosis-associated infertility. Clinical Obstetrics and Gynecology. 1999;42(3):586. doi: 10.1097/00003081-199909000-00014. [DOI] [PubMed] [Google Scholar]
- Butrick CW. Chronic pelvic pain: How many surgeries are enough? Clinical Obstetrics and Gynecology. 2007;50(2):412–424. doi: 10.1097/GRF.0b013e31804b195f. [DOI] [PubMed] [Google Scholar]
- Cahill DJ, Hull MGR. Pituitary-ovarian dysfunction and endometriosis. Human Reproduction. 2000;6(1):56–66. doi: 10.1093/humupd/6.1.56. [DOI] [PubMed] [Google Scholar]
- Cahill DJ, Wardle PG, Maile LA, Harlow CR, Hull MGR. Ovarian dysfunction in endometriosis-associated and unexplained infertility. Journal of Assisted Reproduction and Genetics. 1997;14(10):554–557. doi: 10.1023/A:1022568331845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Pharmacists Association. Compendium of pharmaceuticals and specialties: The Canadian drug reference for health professionals. Ottawa, ON: Author; 2006. [Google Scholar]
- Chopin N, Ballester M, Borghese B, Fauconnier A, Foulot H, Marlartic C, et al. Relation between severity of dysmenorrhea and endometriosis. Acta Obstetricia et Gynecologica Scandinavica. 2006;85:1375–1380. doi: 10.1080/00016340600935490. [DOI] [PubMed] [Google Scholar]
- Cox H, Henderson L, Andersen N, Cagliarini G, Ski C. Focus group study of endometriosis: Struggle, loss and the medical merry-go-round. International Journal of Nursing Practice. 2003;9(1):2–9. doi: 10.1046/j.1440-172x.2003.00396.x. [DOI] [PubMed] [Google Scholar]
- Cox H, Henderson L, Wood R, Cagliarini G. Learning to take charge: Women’s experiences of living with endometriosis. Complementary Therapies in Nursing and Midwifery. 2003;9(2):62–68. doi: 10.1016/S1353-6117(02)00138-5. [DOI] [PubMed] [Google Scholar]
- Crosignani P, Olive D, Bergqvist A, Luciano A. Advances in the management of endometriosis: An update for clinicians. Human Reproduction Update. 2005;12(2):179–189. doi: 10.1093/humupd/dmi049. [DOI] [PubMed] [Google Scholar]
- Denny E. Women’s experience of endometriosis. Journal of Advanced Nursing. 2004;46(6):641–648. doi: 10.1111/j.1365-2648.2004.03055.x. [DOI] [PubMed] [Google Scholar]
- Denny E, Mann CH. Endometriosis-associated dyspareunia: The impact on women’s lives. Journal of Family Planning and Reproductive Health Care. 2007;33(3):189–193. doi: 10.1783/147118907781004831. [DOI] [PubMed] [Google Scholar]
- Dmowski WP, Gebel H, Braun DP. Decreased apoptosis and sensitivity to macrophage mediated cytolysis of endometrial cells in endometriosis. Human Reproduction Update. 1998;4(5):696–701. doi: 10.1093/humupd/4.5.696. [DOI] [PubMed] [Google Scholar]
- Dokras A, Olive DL. Endometriosis and assisted reproductive technologies. Clinical Obstetrics and Gynecology. 1999;42(3):687. doi: 10.1097/00003081-199909000-00020. [DOI] [PubMed] [Google Scholar]
- Dos Reis RM, Silva De Sa MF, De Moura MD, Nogueira AA, Ribeiro JU, Ramos ES, et al. Familial risk among patients with endometriosis. Journal of Assisted Reproduction and Genetics. 1999;16(9):500–503. doi: 10.1023/A:1020559201968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endometriosis Research Center. Endometriosis: An overview. Nurses World Magazine; 2006. Retrieved July 15, 2008, from http://nursesworldmag.com/articles-on-nursing/print-this.cfm/id/27. [Google Scholar]
- Eskenazi B, Warner M, Bonsignore L, Olive D, Samuels S, Vercellini P. Validation study of nonsurgical diagnosis of endometriosis. Fertility and Sterility. 2001;76(5):929–935. doi: 10.1016/s0015-0282(01)02736-4. [DOI] [PubMed] [Google Scholar]
- Fauconnier A, Chapron C. Endometriosis and pelvic pain: Epidemiological evidence of the relationship and implications. Human Reproduction Update. 2005;11(6):595–606. doi: 10.1093/humupd/dmi029. [DOI] [PubMed] [Google Scholar]
- Fedele L, Bianchi S, Raffaelli R, Portugese A. Pre-operative assessment of bladder endometriosis. Human Reproduction. 1997;12:2519–2522. doi: 10.1093/humrep/12.11.2519. [DOI] [PubMed] [Google Scholar]
- Gambone JC, Mittman BS, Munro MG, Scialli AR, Winkel CA the Chronic Pelvic Pain/Endometriosis Working Group. Consensus statement for the management of chronic pelvic pain and endometriosis: Proceedings of an expert-panel consensus process. Fertility and Sterility. 2002;78(5):961–972. doi: 10.1016/s0015-0282(02)04216-4. [DOI] [PubMed] [Google Scholar]
- Gao X, Outley J, Botteman M, Spalding J, Simon JA, Pashos CL. Economic burden of endometriosis. Fertility and Sterility. 2006;86(6):1561–1572. doi: 10.1016/j.fertnstert.2006.06.015. [DOI] [PubMed] [Google Scholar]
- Garcia-Velasco JA, Arici A, Zreik T, Naftolin F, Mor G. Macrophage derived growth factors modulate Fas ligand expression in cultured endometrial stromal cells: A role in endometriosis. Molecular Human Reproduction. 1999;5(7):642–650. doi: 10.1093/molehr/5.7.642. [DOI] [PubMed] [Google Scholar]
- Garcia-Velasco JA, Mulayim N, Kayisli UA, Arici A. Elevated soluble Fas ligand levels may suggest a role for apoptosis in women with endometriosis. Fertility and Sterility. 2002;78(4):855–859. doi: 10.1016/s0015-0282(02)03320-4. [DOI] [PubMed] [Google Scholar]
- Gazvani R, Templeton A. Peritoneal environment, cytokines and angiogenesis in the pathophysiology of endometriosis. Reproduction. 2002;123(2):217–226. doi: 10.1530/rep.0.1230217. [DOI] [PubMed] [Google Scholar]
- Hadfield R, Mardon H, Barlow D, Kennedy S. Delay in diagnosis of endometriosis: A survey of women from the USA and the UK. Human Reproduction. 1996;11(4):878–880. doi: 10.1093/oxfordjournals.humrep.a019270. [DOI] [PubMed] [Google Scholar]
- Hodgkiss AD, Watson JP. Psychiatric morbidity and illness behaviour in women with chronic pelvic pain. Journal of Psychosomatic Research. 1994;38(1):3–9. doi: 10.1016/0022-3999(94)90003-5. [DOI] [PubMed] [Google Scholar]
- Howard FM. Chronic pelvic pain in women. The American Journal of Managed Care. 2001;7(10):1001–1011. [PubMed] [Google Scholar]
- Huntington A, Gilmour JA. A life shaped by pain: Women and endometriosis. Journal of Clinical Nursing. 2005;14(9):1124–1132. doi: 10.1111/j.1365-2702.2005.01231.x. [DOI] [PubMed] [Google Scholar]
- Jarrell J. Myofascial dysfunction in the pelvis. Current Pain and Headache Reports. 2004;8(6):452–456. doi: 10.1007/s11916-004-0066-0. [DOI] [PubMed] [Google Scholar]
- Kang S, Chung HH, Lee H, Lee JY, Chang YS. Impact of diagnostic laparoscopy on the management of chronic pelvic pain. Surgical Endoscopy. 2006;21(6):916–919. doi: 10.1007/s00464-006-9047-1. [DOI] [PubMed] [Google Scholar]
- Kitawaki J, Kado N, Ishihara H, Koshiba H, Kitaoka Y, Honjo H. Endometriosis: The pathophysiology as an estrogen-dependent disease. Journal of Steroid Biochemistry and Molecular Biology. 2002;83(1–5):149–155. doi: 10.1016/s0960-0760(02)00260-1. [DOI] [PubMed] [Google Scholar]
- Lebovic DI, Mueller MD, Taylor RN. Immunobiology of endometriosis. Fertility and Sterility. 2001;75(1):1–10. doi: 10.1016/s0015-0282(00)01630-7. [DOI] [PubMed] [Google Scholar]
- Lemaire GS. More than just menstrual cramps: Symptoms and uncertainty among women with endometriosis. Journal of Obstetric, Gynecologic and Neonatal Nursing. 2004;33(1):71–79. doi: 10.1177/0884217503261085. [DOI] [PubMed] [Google Scholar]
- Lessey BA. Implantation defects in infertile women with endometriosis. Annals of the New York Academy of Sciences. 2002;955:265–280. doi: 10.1111/j.1749-6632.2002.tb02787.x. [DOI] [PubMed] [Google Scholar]
- Mais V, Guerriero S, Ajossa S, Angiolucci M, Paoletti AM, Melis GB. The efficiency of transvaginal ultrasonography in the diagnosis of endometrioma. Fertility and Sterility. 1993;60(5):776–780. doi: 10.1016/s0015-0282(16)56275-x. [DOI] [PubMed] [Google Scholar]
- Marcoux S, Maheux R, Berube S The Canadian Collaborative Group on Endometriosis. Laparoscopic surgery in infertile women with minimal or mild endometriosis. New England Journal of Medicine. 1997;337(4):217–222. doi: 10.1056/NEJM199707243370401. [DOI] [PubMed] [Google Scholar]
- Martinez-Roman S, Balasch J, Creus M, Fabregues F, Carmona F, Vilella R, et al. Immunological factors in endometriosis-associated reproductive failure: studies in fertile and infertile women with and without endometriosis. Human Reproduction. 1997;12(8):1794–1799. doi: 10.1093/humrep/12.8.1794. [DOI] [PubMed] [Google Scholar]
- Moen MH, Magnus P. The familial risk of endometriosis. Acta Obstetricia et Gynecologica Scandinavica. 1993;72(7):560–564. doi: 10.3109/00016349309058164. [DOI] [PubMed] [Google Scholar]
- Mounsey AL, Wilgus A, Slawson DC. Diagnosis and management of endometriosis. American Family Physician. 2006;74(4):594–600. [PubMed] [Google Scholar]
- Murphy AA. Clinical aspects of endometriosis. Annals of the New York Academy of Sciences. 2002;955:1–10. doi: 10.1111/j.1749-6632.2002.tb02760.x. [DOI] [PubMed] [Google Scholar]
- Noble LS, Simpson ER, Johns A, Bulun SE. Aromatase expression in endometriosis. Journal of Clinical Endocrinology and Metabolism. 1996;81(1):174–179. doi: 10.1210/jcem.81.1.8550748. [DOI] [PubMed] [Google Scholar]
- Noble LS, Takayama K, Zeitoun KM, Putman D, Johns A, Hinshelwood M, et al. Prostaglandin E2 stimulates aromatase expression in endometriosis-derived stromal cells. Journal of Clinical Endocrinology and Metabolism. 1997;82(2):600–606. doi: 10.1210/jcem.82.2.3783. [DOI] [PubMed] [Google Scholar]
- Olive DL, Pritts EA. Treatment of endometriosis. New England Journal of Medicine. 2001;345(4):266–275. doi: 10.1056/NEJM200107263450407. [DOI] [PubMed] [Google Scholar]
- Oral E, Olive DL, Arici A. The peritoneal environment in endometriosis. Human Reproduction Update. 1996;2(5):385–398. doi: 10.1093/humupd/2.5.385. [DOI] [PubMed] [Google Scholar]
- Ozawa Y, Murakami T, Terada Y, Yaegashi N, Okamura K, Kuriyama S, et al. Management of the pain associated with endometriosis: An update of the painful problems. Tohoku Journal of Experimental Medicine. 2006;210(3):175–188. doi: 10.1620/tjem.210.175. [DOI] [PubMed] [Google Scholar]
- Pellicer A, Albert C, Mercader A, Bonilla-Musoles F, Remohi J, Simon C. The follicular and endocrine environment in women with endometriosis: Local and systemic cytokine production. Fertility and Sterility. 1998;70(3):425–431. doi: 10.1016/s0015-0282(98)00204-0. [DOI] [PubMed] [Google Scholar]
- Pellicer A, Valbuena D, Bauset C, Albert C, Bonilla-Musoles F, Remohi J, et al. The follicular endocrine environment in stimulated cycles of women with endometriosis: steroid levels and embryo quality. Fertility and Sterility. 1998;69(6):1135–1141. doi: 10.1016/s0015-0282(98)00085-5. [DOI] [PubMed] [Google Scholar]
- Petta CA, Arruda MS, Zantut-Wittmann DE, Benetti-Pinto CL. Thyroid autoimmunity and thyroid dysfunction in women with endometriosis. Human Reproduction. 2007;22(10):2693–2697. doi: 10.1093/humrep/dem267. [DOI] [PubMed] [Google Scholar]
- Razzi S, Fava A, Sartini A, De Simone S, Cobellis L, Petraglia F. Treatment of severe recurrent endometriosis with an aromatase inhibitor in a young ovariectomised woman. BJOG: An International Journal of Obstetrics and Gynecology. 2004;111:182–184. doi: 10.1046/j.1471-0528.2003.00038.x. [DOI] [PubMed] [Google Scholar]
- Sampson JA. The development of the implantation theory for the origin of peritoneal endometriosis. American Journal of Obstetrics and Gynecology. 1940;40:549–557. [Google Scholar]
- Schenken RS. Treatment of human infertility: The special case of endometriosis. In: Adashi EY, Rock JA, Rosenwaks Z, editors. Reproductive endocrinology, surgery, and technology. Vol. 2. Philadelphia: Lippincott-Raven; 1996. pp. 2121–2140. [Google Scholar]
- Seydel AS, Sickel JZ, Warner ED, Sax HC. Extrapelvic endometriosis: Diagnosis and treatment. The American Journal of Surgery. 1996;171:239–241. doi: 10.1016/S0002-9610(97)89557-8. [DOI] [PubMed] [Google Scholar]
- Shaw RW. An atlas of endometriosis. Carnforth, UK: The Parthenon Publishing Group; 1993. [Google Scholar]
- Shippen ER, West WJ. Successful treatment of severe endometriosis in two premenopausal women with an aromatase inhibitor. Fertility and Sterility. 2004;81(5):1395–1398. doi: 10.1016/j.fertnstert.2003.11.027. [DOI] [PubMed] [Google Scholar]
- Signorello LB, Harlow BL, Cramer DW, Spiegelman D, Hill JA. Epidemiologic determinants of endometriosis: A hospital-based case-control study. Annals of Epidemiology. 1997;7(4):267–741. doi: 10.1016/s1047-2797(97)00017-3. [DOI] [PubMed] [Google Scholar]
- Sinaii N, Cleary SD, Ballweg ML, Nieman LK, Stratton P. High rates of autoimmune and endocrine disorders, fibromyalgia, chronic fatigue syndrome and atopic diseases among women with endometriosis: A survey analysis. Human Reproduction. 2002;17(10):2715–2724. doi: 10.1093/humrep/17.10.2715. [DOI] [PubMed] [Google Scholar]
- Sinaii N, Cleary SD, Younes N, Ballweg M, Stratton P. Treatment utilization for endometriosis symptoms: A cross-sectional survey study of lifetime experience. Fertility and Sterility. 2007;87(6):1277–1286. doi: 10.1016/j.fertnstert.2006.11.051. [DOI] [PubMed] [Google Scholar]
- Soysal S, Soysal ME, Ozer S, Gul N, Gezgin T. The effects of post-surgical administration of goserelin plus anastrozole compared to goserelin alone in patients with severe endometriosis: A prospective randomized trial. Human Reproduction. 2004;19(1):160–167. doi: 10.1093/humrep/deh035. [DOI] [PubMed] [Google Scholar]
- Stefansson H, Geirsson RT, Steinthorsdottir V, Jonsson H, Manolescu A, Kong A, et al. Genetic factors contribute to the risk of developing endometriosis. Human Reproduction. 2002;17(3):555–559. doi: 10.1093/humrep/17.3.555. [DOI] [PubMed] [Google Scholar]
- Sutton C, Pooley AS, Jones KD, Dover RW, Haines P. A prospective, randomized, double-blind controlled trial of laparoscopic uterine nerve ablation in the treatment of pelvic pain associated with endometriosis. Gynaecological Endoscopy. 2001;10:217–222. [Google Scholar]
- Takayama K, Zeitoun K, Gunby RT, Sasano H, Carr BR, Bulun SE. Treatment of severe postmenopausal endometriosis with an aromatase inhibitor. Fertility and Sterility. 1998;69(4):709–713. doi: 10.1016/s0015-0282(98)00022-3. [DOI] [PubMed] [Google Scholar]
- Ulukus M, Cakmak H, Arici A. The role of endometrium in endometriosis. Journal of the Society for Gynecologic Investigation. 2006;13(7):467–476. doi: 10.1016/j.jsgi.2006.07.005. [DOI] [PubMed] [Google Scholar]
- Wellbery C. Diagnosis and treatment of endometriosis. American Family Physician. 1999;60(6):1753–1762. [PubMed] [Google Scholar]
- Wesselman U. Neurogenic inflammation and chronic pelvic pain. World Journal of Urology. 2001;19:180–185. doi: 10.1007/s003450100201. [DOI] [PubMed] [Google Scholar]
- Wesselmann U, Czakanski PP. Pelvic pain: A chronic visceral pain syndrome. Current Pain and Headache Reports. 2001;5(1):13–19. doi: 10.1007/s11916-001-0005-2. [DOI] [PubMed] [Google Scholar]
- Zeitoun KM, Bulun SE. Aromatase: A key molecule in the pathophysiology of endometriosis and a therapeutic target. Fertility and Sterility. 1999;72(6):961–969. doi: 10.1016/s0015-0282(99)00393-3. [DOI] [PubMed] [Google Scholar]