Abstract
Objective
This pilot study evaluated the effectiveness of a four-session, caregiver-child Intervention, the Child and Family Traumatic Stress Intervention (CFTSI), to prevent the development of Chronic PTSD provided within 30 days of exposure to a Potentially Traumatic Event (PTE).
Method
One-hundred-seventy-six 7-to-17 year old youth were recruited through telephone screening based on report of one new distressing posttraumatic stress symptom after a PTE. Of those, one-hundred-six youth were randomly assigned to the Intervention (n=53) or a four-session supportive Comparison condition (N=53). Group differences in symptom severity were assessed using repeated measures with mixed effects models of intervention group, time, and the interaction of intervention and time. Logistic regression analyses were performed to assess treatment condition and any subsequent traumas experienced as predictors for Full and Partial PTSD diagnosis at 3 month follow-up. An exploratory chi-square analysis was performed to examine the differences in PTSD symptom criteria B, C, and D at follow-up
Results
At baseline, youth in both groups had similar demographics, past trauma exposures and symptom severity. At follow-up, the Intervention group demonstrated significantly fewer Full and Partial PTSD diagnoses than the Comparison group on a standardized diagnostic measure of PTSD. Also, there was a significant group by time interaction for TSCC Posttraumatic Stress and Anxiety Indices as the CFTSI group had significantly lower posttraumatic and anxiety scores than the Comparison group.
Conclusions
The results suggest that a caregiver-youth, brief preventative early intervention for youth exposed to a PTE is a promising approach to preventing Chronic PTSD.
Keywords: Trauma, prevention, family
Children and adolescents are subject to extremely high rates of maltreatment, victimization, intentional and unintentional injury, and exposure to other potentially traumatic events (PTEs) (Centers for Disease Control and Prevention, 2009; Finkelhor, Ormrod, & Turner, 2009; McCaig & Nghi, 2002; McDonald, Jouriles, Ramisetty-Mikler, Caetano, & Green, 2006). A telephone survey of a nationally representative sample indicates that upwards of 60% of children and adolescents have experienced or witnessed at least one potentially traumatic event (PTE) in the previous year (Finkelhor, et al., 2009). In the United States an estimated 15.5 million children are exposed to domestic violence each year. Another 7 million children were exposed to severe and chronic intrafamilial violence (McDonald, et al., 2006) and an estimated 10 million children and adolescents under the age of 15 were seen in hospital emergency rooms due to injuries in 2000 (McCaig & Nghi, 2002). Although most studies estimate that only 6%–20% of individuals will develop Posttraumatic Stress Disorder (PTSD) after a PTE (Kahana, Feeny, Youngstrom, & Drotar, 2006), the shear number of youth who encounter PTEs in a given year could lead to annual incidence of Full or Partial PTSD that reaches the millions. It is of additional concern that children affected by multiple factors of social adversity are at greater risk for PTSD (Cooley-Quille, Boyd, Frantz, & Walsh, 2001; Overstreet & Braun, 2000; Sharfstein, 2006). A study of elementary and middle school children in a poor urban community reported that 50% screened positive for the full diagnosis of PTSD and 21% for partial PTSD (Horowitz, McKay, & Marshall, 2005). Given the high rates of exposure, there is an urgent need for effective interventions that decrease the risk for posttraumatic disorders. We define Secondary Prevention as an intervention introduced when there are early distressing symptoms that indicate risk for subsequent psychiatric disorder.
At present there is one published randomized controlled study with baseline and outcome data of an early preventative intervention for youth. A modified version of Critical Incident Stress Debriefing was used for youth involved in motor vehicle accidents (MVA), which demonstrated no difference between the intervention and non-intervention groups for PTSD (Stallard, et al., 2006). Also, there is one report in which the provision of psychoeducational information for parents did not improve child outcomes when compared to a no intervention group after exposure to a MVA (Kenardy, Thompson, Le Brocque, & Olsson, 2008). Many agree that the development of PTSD constitutes a “failure of recovery” as the majority of individuals, both adults and youth, exposed to a PTE typically experience transient symptoms and subsequently return to their previous level of functioning (Foa & Meadows, 1997; Rothbaum & Davis, 2003). While multiple non-modifiable factors contribute to suboptimal recovery, it should be possible when providing early interventions to target and optimize protective factors such as social and family support and coping skills shortly after a PTE.
We report the promising findings of a four-session caregiver-child early intervention and secondary prevention model, the Child and Family Traumatic Stress Intervention (CFTSI), for children ages 7–17. We hypothesized that the CFTSI would be a more effective secondary prevention model compared to a four session supportive intervention. (see Table 1)
Table 1.
Comparison Intervention
| Session 1 | Session 2 | Session 3 | Session 4 | |
|---|---|---|---|---|
| Comparison Intervention |
Caregiver Alone
|
Child Alone
|
Child Alone
|
Caregiver and Child
|
The CFTSI focuses on two key risk factors of poor social or familial support and poor coping skills in its effort to prevent chronic PTSD. The CFTSI ameliorates these risks by (1) increasing communication between the affected child and his caregivers about feelings, symptoms and behaviors with the goal of increasing the caregivers’ support of the child and (2) providing specific behavioral skills that are taught both to the caregiver and child to assist in coping with symptoms (See description below, manual available on request).
CFTSI’s focus is informed by findings that indicate the role of family support as a primary protective factor for children exposed to a PTE (Hill, Levermore, Twaite, & Jones, 1996; Kliewer, et al., 2004; Ozer, Best, Lipsey, & Weiss, 2003). This protective factor has also been demonstrated in families where there has been intra-familial abuse, with a decrease in children’s symptoms when the non-offending parent is able to provide support (Boney-McCoy & Finkelhor, 1995; Margolin, 1998; Trickett, 1997). An analysis of the current study’s baseline data of child reports demonstrated that hostile/coercive parenting was a statistically significant predictor of initial child PTSD symptom severity adding further evidence to the salience of caregiver-child relationships (Valentino, Berkowitz, & Stover, 2010).
Optimal support requires communication between caregivers and affected children (Kerr & Stattin, 2000; Kerr, Stattin, & Trost, 1999; Stattin & Kerr, 2000). CFTSI expedites and enhances communication by using well-established PTSD and Mood questionnaires as vehicles for identifying and discussing the child’s difficulties and focusing on understanding and reviewing agreement and discrepancies between reported and observed symptoms of PTSD and Depression. Once symptoms are identified, CFTSI teaches caregivers and youth specific coping skills to manage them. The current study specifically evaluates whether the CFTSI, a protocolized 4-session caregiver-child early intervention, was more effective in preventing the development of Chronic PTSD as compared to an Individual Child, 4-session intervention that provided supportive counseling and psychoeducation (see table 1).
CFTSI DESCRIPTION
Only the adult caregivers and the provider are present for the first session. At its opening, the clinician explains each step in the process and its rationale. A psychoeducational approach is applied with explanations of typical reactions to PTEs and the protective role of family support. Consistent with the focus on the essential role of caregivers, the Posttraumatic Checklist-Civilian version (Weathers, Litz, Huska, & Keane, 1994) is administered. This allows the clinician to integrate an understanding of the caregiver’s psychological status throughout the Intervention. External stressors related to the recent PTE are identified and a plan for managing them is developed. We have found that addressing event related stressors both serves as an engagement tool and permits caregiver’s to more readily focus on the child’s emotional needs. Lastly, the caregivers are administered parent versions of the Trauma History Questionnaire (THQ)(Berkowitz & Stover, 2005), and modified versions of the UCLA Posttraumatic Reaction Index (PTSD-RI) (R. Pynoos, N. Rodriguez, A. M. Steinberg, M. Stuber, & C. Frederick, 1998) and the Mood and Feelings Questionnaire (MFQ) (Angold & Costello, 1987), which will be the central focus of the joint session to follow next. Session one and all subsequent session average an one to one and one half hours in length.
Session Two occurs as close to Session One as possible and the provider meets first with the child alone and then with caregivers and child. The second half of this session is the core component of the CFTSI and lays the groundwork for all subsequent aspects of the Intervention. First, the child is administered the THQ, PTSD-RI and Short MFQ. The clinician, with the child and caregiver/s) facilitates a comparison of the responses as means of improving communication, which is the presumed pre-requisite to enhancing caregiver emotional support. If there is an agreement about symptom severity the parent and child are praised. Discordance is seen as an opportunity to increase communication. The clinician takes a dual approach to improving communication; both helping the child to better inform the parent about symptoms, and the parent to be more aware, receptive, and supportive. Session Two ends with the clinician proposing two areas of concern based on symptom clusters the child and caregivers have identified as most problematic. Together the clinician and family choose two behavioral skill modules as “homework” before the next session. These modules cover 6 topic areas (1) sleep disturbance, (2) depressive withdrawal, (3) oppositionality/tantrums, (4) intrusive thoughts, (5) anxiety, avoidance and phobic reactions and (6) a general overview of traumatic stress symptoms and techniques to manage them. Each module reviews psychoeducation and specific techniques, with separate instructions for the caregiver and child to discuss and practice. The maintenance of routines is emphasized throughout. Specific techniques involve both behavioral and cognitive procedures such as thought replacement methods for intrusive thoughts, breathing retraining for anxiety, behavioral activation for depression and avoidance. The specific elements for addressing each problem area have been borrowed and adapted from well accepted methods from the Traumatic Stress treatment literature.
The caregivers, child, and clinician meet together for Session Three; demonstrating the solution to the child’s difficulties is a family matter. The same symptom surveys are administered with the child responding first and the caregivers offering their perspective on the items. It permits symptom monitoring as well as an examination of which methods of communication and supportive efforts were most successful. Efforts center on adjustments to improve communication efforts and review the effectiveness of the skill modules and other supportive measures. While the skill modules were reviewed during Session Two, they are practiced in Session Three and Four.
Session Four essentially duplicates Session Three with one key difference. The end of the session is used to discuss next steps. Depending on the status of the child, the clinician may suggest a future check-in, evaluation and treatment for an apparent pre-existing psychiatric disorder or a more extensive treatment for PTSD.
METHODS
Participants
One hundred-twelve youth aged 7–17 years exposed to a potentially traumatic event (PTE) who endorsed at least one new and distressing symptom of PTSD on the Posttraumatic Checklist-Civilian (PCL)(Weathers, et al., 1994) within 30 days of the PTE were randomized into the pilot study at the Trauma Section of the Yale Child Study Center. Children were referred for service by police or a forensic sexual abuse program. Children were recruited from a pediatric emergency department (PED) following a record review, by follow up phone call. The study recruitment occurred from 1/1/2005–5/1/2009 with follow-up interviews completed by 9/1/2009.
Procedure
The randomized pilot was conducted within the context of a clinical treatment and service development grant to design early intervention models for youth exposed to a PTE. All screened youth and families were offered services regardless of agreement to participate in the study.
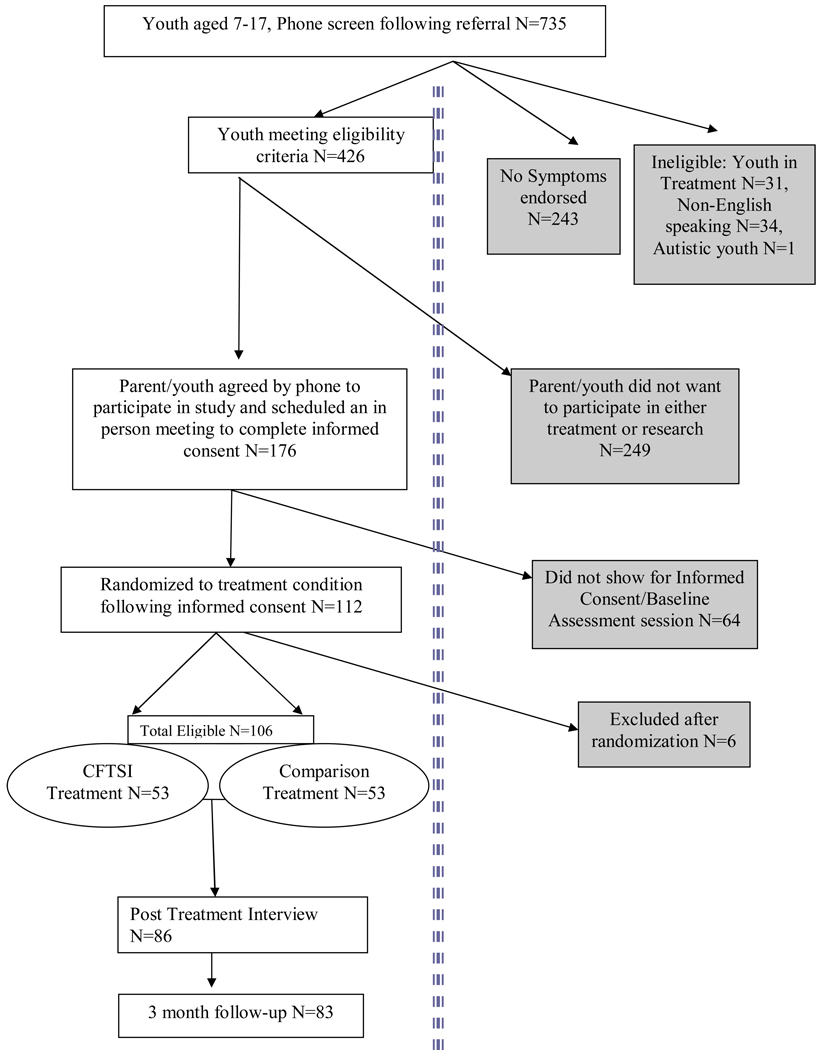
Seven-hundred-thirty-five families were contacted by phone and, if agreeable, screened using the PCL by trained research assistants (RAs). Youth who had one new symptom since the PTE as reported by either the youth or caregiver were further screened for eligibility (N=426). Youth were excluded if: 1) they were receiving counseling or mental health treatment (N=31); 2) they had a developmental delay (e.g. autism) or diagnosed psychotic or bipolar disorder (N=1); 3) non-English speaking caregiver or youth (N=34) or 4) or refused participation in the research study (N=249). If they met inclusion criteria and agreed to participate, an initial appointment was scheduled to complete informed consent (N=176). Sixty-four families scheduled an appointment to enroll but did not attend yielding a total sample of 112 who signed informed consent and were randomized to the two conditions (See figure 1). Six cases were excluded following randomization; three due to the caregiver or child’s ’s inability to complete research measures, two due to inability to follow the CFTSI protocol and one due to the child already receiving other mental health treatment. This resulted in a final sample of 106 participants. There were no differences in the age or gender of the child for those who agreed to participate and those who either refused or didn’t attend. Eighty-two percent of potential cases came from the Pediatric Emergency Department (PED). Of those contacted and screened from the PED, 71% declined participation versus 26% of police and 21% of sexual abuse program referrals. The high rate of refusal from those recruited for the PED was expected, since families were contacted by phone without prior knowledge of the study or expressed desire for mental health follow-up.
Figure 1.
Participant Flow Through Each Phase of Study
Children and their families were randomized to the CFTSI or the Comparison Intervention condition immediately after consent by an RA, using a ten subject block design using number containers, and received baseline measures and the first treatment session at the time of their initial visit. Baseline interviews and the first treatment session occurred within 30 days of a child’s exposure to a PTE, and so youth could not meet criteria for a PTSD diagnosis at that time. Following written informed consent procedures, participants were interviewed using a set of standard measures. Separate interviews were conducted with each child and caregiver by trained RAs who were unblinded. Youth and caregivers in the intervention group received the 4 session CFTSI protocol. Comparison youth received a protocolized psychoeducational (including relaxation training) and supportive 4 session intervention that included an initial meeting with the adult caregiver, two individual child sessions and a fourth feedback session with both (see Table 1). All participants were interviewed by RA at baseline, immediately following their fourth treatment session (4 weeks from baseline) and 3 months post-treatment by research assistants. The intervention was provided by master and doctoral level clinicians. They were divided into two groups and trained in each model. Each group rotated every 6 months. Fidelity to both groups was ensured through weekly group supervision with a developer of each condition who did not rotate. Progress notes were developed for each condition to help supervisors ensure fidelity.
Measures
Trauma History Questionnaire (THQ) was administered at baseline and follow-up to establish the number previous of PTEs as a history of exposure to traumatic events has been shown to be a risk factor for the development of PTSD and therefore a possible confounder if a group difference was found. This questionnaire contains 13 items developed at the Childhood Violent Trauma Center to quickly assess children’s histories of previous traumatic events and the intensity of their reactions. The THQ is a modification of the Traumatic Events Screening Inventory- Child Self-Report and the Parent-Report Revised,(Ghosh-Ippen, et al., 2002) which screens for a range of traumatic events and includes assessments of the impact of the event on the child both at the time of the incident and at present. A Total Trauma History Score was achieved by totaling the number of unique trauma types endorsed by either caregiver or child report (each trauma type was counted once, whether reported by the child, caregiver or both.)
The Parent Behavior Inventory (PBI) was administered at baseline as parenting practice is a focus of the CFTSI and would moderate PTSD outcomes. The PBI is a brief 20-item measure of parenting behavior that contains two independent scales, Supportive/Engaged and Hostile/Coercive. These scales have sufficient content validity, adequate internal consistency (alpha=.81 and .83 respectively) and test-retest reliability (.69 and .74 respectively) (Lovejoy, Weis, O'Hare, & Rubin, 1999).
The Perceived Social Support-Family (PSS-Fa) was administered at baseline, since caregiver support of their child was the hypothesized mechanism of action of the CFTSI and between group differences would confound outcomes. The PSS-Fa is a 20 item measure that was used to assess the child’s perceived emotional support from their family. The measure demonstrated good internal consistency (alpha=.90) and the test retest coefficient=.83.(Procidano & Heller, 1983) Furthermore, Windle & Tutzauer(Windle & Miller-Tutzauer, 1992) tested a four point likert scale resulting in a three factor structure within the PSS. Cronbach alphas for the scales were .93, .87, and .62. Test retest coefficients were .77, .71, and .55.
The UCLA Posttraumatic Stress Disorder Index (PTSD-RI)(R. Pynoos, N. Rodriguez, A. Steinberg, M. Stuber, & C. Frederick, 1998) was administered at baseline by the clinician in each condition and at the 3 month follow up by an RA. The PTSD-RI is an extensively used instrument that was used to assess posttraumatic symptomatology related to subjective distress, as well as PTSD diagnostic criteria B (re-experiencing), C (arousal) and D (avoidance) symptoms and can be used to diagnose full or partial PTSD based on DSM-IV criteria (Steinberg, Brymer, Decker, & Pynoos, 2004).
The Behavior Assessment System for Children, Second Edition- Self Report (BASC-2) was administered at baseline only to assess for symptoms and functioning prior to the current PTE as a potential confounder if there were differences between groups. The BASC-2 is a 139-item measure of the child’s reported symptoms and behaviors in a wide variety of domains (e.g. hyperactivity, aggression, depression, adaptability etc.) (Reynolds & Kamphaus, 2004). It generates T-scores for several scales including Internalizing and Emotional Problems, and has been standardized for children aged 7–18.
The Child Behavior Checklist (CBCL) was administered to caregivers at baseline to assess for pre-existing symptoms and behaviors as a potential confounder if there were differences between groups. The CBCL is a factor analytic derived checklist of child behavior that is administered to parents or guardians(Achenbach & Rescorla, 2001). The CBCL yields age-and gender-normed T-scores for children’s internalizing, externalizing, and total behavior problems. The PTSD Checklist- Civilian Version (PCL-C) was used as the screening tool asked of both a primary caregiver and child. It was also administered to the participant caregiver at baseline. The PCL-C is a 17-item self-report questionnaire designed to assess the 17 PTSD symptoms described in the DSM-IV (Weathers, et al., 1994). The total score on the PCL-C was our index of PTSD symptomatology in caregivers. It has been cross-validated with the Clinician Administered PTSD Scale (Blake, et al., 1995) and is considered to be a valid and reliable screening measure for PTSD (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996).
The Trauma Symptom Checklist for Children (TSCC) was administered at all time points to evaluate posttraumatic symptomatology (Briere, 1996). The scale does not provide a diagnosis, but measures PTSD symptoms, as well as other symptoms found in some traumatized children. Specifically, this 54 item self-report measure consists of two validity scales and six clinical scales. For this study, the Anxiety, Post-traumatic Stress, and Dissociation Indices were analyzed as these indices are associated with the PTSD diagnosis.
Data Analysis
Prior to hypothesis testing, chi-squares and analysis of variance (ANOVA) were run to determine if there were significant group differences at baseline. The potential confounders assessed were ethnicity, age of victim, total trauma history, parental posttraumatic symptoms (PCL), family social support (PSS-Fa), parent behavior (PBI), child adaptive and emotional functioning (BASC/CBCL). Parent behavior toward their child and family support were important baseline considerations given the focus of the CFTSI on increasing familial support and improving parents’ responsiveness to their children following a trauma. If significant group differences existed, these variables would be entered into subsequent multivariate analysis models. To assess potential bias of analysis due to missing data, chi-square and ANOVAs were conducted to compare cases with or without missing data on covariates and baseline measures of the dependent variables as suggested by Hedeker and Gibbons (1997) and Graham (2009).
There were two related outcomes of interest; differences in TSCC symptom severity on the PTS, Anxiety and Dissociation indices, and PTSD diagnosis and severity of symptoms at the 3-month follow-up (F/U). For diagnosis, logistic regression analyses were performed to assess treatment condition and any subsequent traumas experienced as predictors for Full and Partial (meeting two of three criteria) PTSD diagnosis at F/U. For symptom severity, repeated measures with mixed effects models were conducted. Group (CFTSI versus Comparison), time (Baseline, post-treatment, or 3 -month follow-ups), and the interaction of treatment and time (Group × Time) were the primary independent variables of interest. The Group × Time interaction effect, if significant, represents significant differences in change within the groups on symptoms. The Holm-Bonferroni method was used to correct for multiple comparisons (Holm, 1979). To further disentangle the impact of the intervention on PTSD diagnosis we performed exploratory chi-square analysis to examine the differences in PTSD symptom criteria B, C, and D at F/U.
RESULTS
Demographics
One Hundred-six were available for analysis (53 Comparison and 53 CFTSI). Fifteen families attended the baseline session only and did not return for treatment sessions or additional research interviews, 5 did not attend the final session and post interview and 3 did not participate in F/U. There was no significant difference between the CFTSI and Comparison Conditions in the number of dropouts, nor were there significant differences between groups in number of treatment sessions attended (F(1,105)1.12, p=.29) or the number of days between the PTE and beginning the intervention F(1,105)=1.82, p=.18). The mean number of days from session 1 to session 4 was 28.9 SD=12.87.There were no differences between groups for age, ethnicity or PTE type. The mean age of youth in the sample was 12 with 48% males, 32% Caucasian, 37% African American, 22% Hispanic, 7% Multi-ethnic, 2% other ethnicities. The nature of the PTEs that brought participants to the study were: 24% motor vehicle accident (MVA), 18% sexual abuse, 19% witnessing violence, 21% physical assaults, 8% injuries (e.g. sports, cycling), 5% animal bite, and 5% threats of violence (e.g. mugging). The majority of caregivers were females (90%) with only 10% fathers or stepfathers participating. Only non-offending caregivers were permitted to participate.
Additionally, there were no significant differences between groups on number of previous trauma types experienced, parenting behavior, social support, baseline symptom scores on the PCL, PTSD-RI Severity, BASC-II, CBCL or TSCC Indices. There were no differences in the number of new traumas experienced F(1, 81)=.082, p=.78 between baseline and 3-month follow-up with means 1.85 for Comparison and 1.80 for CFTSI.
Cases were coded as either complete or missing data. There were no significant differences between cases with complete or missing data on any of the covariates (e.g. trauma history, parent behavior, social support, BASC or CBCL scores) or baseline measures of the dependent variables (TSCC anxiety, dissociation, and PTS or PTSD partial or full diagnosis). Given the lack of differences and the ability of mixed effects modeling to handle missing data and its comparability to multiple imputations (Raudenbush & Bryk, 2002) mixed effects models were conducted with the full sample of 106 participants. Imputation was not used in this study since baseline interviews took place within 30 days of a PTE and PTSD symptoms often remit on their own making it difficult to impute data appropriately. In addition, there are cautions in the literature regarding use of imputation methods for dichotomous outcomes and missing covariates (Schafer & Graham, 2002; Allison, 2000).
Group Differences in TSCC Symptom Severity Post-Treatment and at Follow-up
There was a significant group by time interaction for TSCC Posttraumatic Stress (F(2,163)= 3.25, p=.04) and Anxiety (F(2,163)=4.89, p=.009) Indices. Youth in the CFTSI group had significantly lower posttraumatic and anxiety scores than comparison youth (see Table 2).
Table 2.
Repeated Measures Models to Compare Groups on TSCC Indices (N=106)
| Outcome Measure | LSMean (SE) |
LSMean (SE) |
LSMean (SE) |
df | F (Group × Time)a |
p |
|---|---|---|---|---|---|---|
| Baseline | Post | 3 Mos | ||||
| PTS | 163 | 3.25* | .04 | |||
| CFTSI | 53. 30(1.34) | 42.97(1.37)+ | 39.74(1.38) | |||
| Comparison | 51.741.29) | 46.12 (1.33) | 42.22(1.37) | |||
| Dissociation | 163 | 1.28 | .28 | |||
| CFTSI | 47.64(1.12) | 42.26(1.12)+ | 41.02(1.13.) | |||
| Comparison | 48.23(1.07) | 45.12(1.09) | 43.54(1.12) | |||
| Anxiety | 163 | 4.89 ** | .009 | |||
| CFTSI | 51.34(1.33) | 40.86(1.36)* | 39.64(1.37) | |||
| Comparison | 50.45(1.29) | 45.49(1.31) | 41.82(1.35) | |||
Note:
p<.10,
p<.05,
p<.01
Group Differences in PTSD Diagnostic Criteria at Follow-up
Logistic regression was performed to examine group differences in PTSD diagnosis at F/U based on child self-reports on the PTSD-RI. Intervention group and total number of trauma types experienced since the baseline interview were simultaneously entered into the models for Full PTSD and then for Full or Partial PTSD. At 3-month follow-up the overall model was significant (X2 (2, 81) = 6.25, p=.04) and accounted for 10.8% of the variance (Nagelkerke R2 = .108). After intervention, the CFTSI group was significantly less likely to have PTSD at F/U (B=−1.063, p=.046) reducing the odds of PTSD by 65% (see Table 3). The overall model assessing Full or Partial PTSD diagnosis at 3-month follow-up was significant (X2 (2, 81) =12.65, p=.002) and accounted for 18.9% of the variance (Nagelkerke R2 = .189). CFTSI reduced the odds of Partial or Full PTSD by 73% (B=−1.32, p=.008) (see Table2). Additionally, there were significant differences between groups at 3-month follow-up in severity of PTSD symptoms on the PTSD-RI (F(2, 81=6.55, p=.01), with means for CFTSI and Comparison 8.70 and 14.74 at F/U respectively.
Table 3.
Logistic Regression Models for PTSD Full Diagnosis and Full or Partial Diagnosis at 3 Month Follow-up (N=82)
| Effect | 3-Month Follow-up | |
|---|---|---|
| B (SE) | Odds Ratio | |
| Full Diagnosis | ||
| Total Traumas | 192(.142) | 1.21 |
| Intervention | −1.06(.534) | .345* |
| Full or Partial Diagnosis | ||
| Total Traumas | 373(.178) | 1.45* |
| Intervention | −1.36(.499) | .268** |
p < .05
p <.01
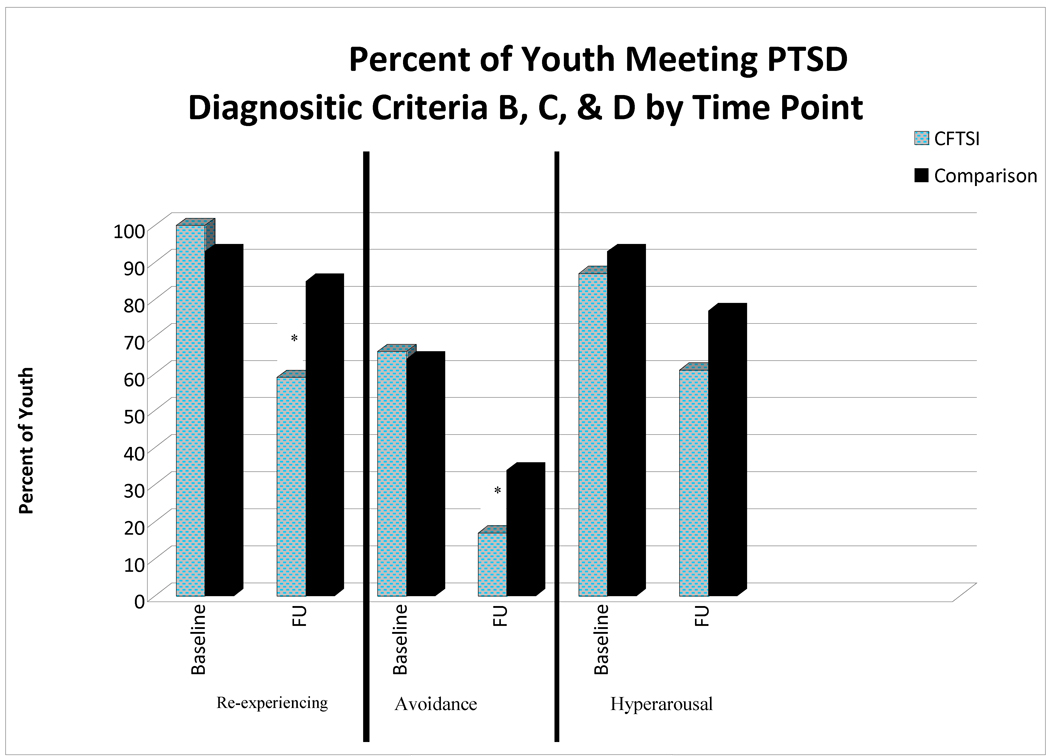
Exploratory Analysis
Chi-square analyses were used to determine which PTSD criteria resulted in significant differences between CFTSI and Comparison groups in PTSD diagnosis. At 3-month F/U, there were significant group differences in Re-experiencing with 85% of comparison and 57% of CFTSI (X2 (1, 83) =8.04, p=.005) and Avoidance with 37% comparison and 17% CFTSI (X2 (1, 83) =4.23, p=.04) meeting criteria, but not Hyperarousal (X2 (1, 83) =2.57, p=.11).
DISCUSSION
Results of this randomized pilot study indicate that the CFTSI has promise as an early intervention designed to prevent the development of chronic PTSD and associated symptoms. Children that received the CFTSI were 65% less likely to meet criteria for PTSD at the 3-month follow up than children that received the comparison condition as measured by the PTSD-RI. In addition, when PTSD and sub-clinical PTSD were combined, the CFTSI continued to demonstrate a statically significant decrease by 73% at F/U. Importantly on the TSCC posttraumatic and anxiety indices, symptoms were significantly lower in the CFTSI group post-treatment and remained lower at follow-up, possibly indicating CFTSI reduces symptoms and promotes recovery more quickly than the comparison condition.
CFTSI participants showed a significant decrease in the Avoidance and Re-experiencing criteria, while the Hyperarousal criteria did not show a significant difference. Since CFTSI’s core therapeutic method is focused on increasing caregiver-child communication, a decrease in avoidance symptomatology was an anticipated outcome. Caregiver attunement to their children’s symptoms is more likely to lead to their raising concerns about the child’s status and the recent PTE. While it is not clear which element of the CFTSI positively impacted the Re-experiencing criteria, it is likely related to the decrease in Avoidance. The lack of significant change in the Hyperarousal criteria needs further exploration. But given that the majority of study participants lived in highly stressed impoverished urban environments, Hyperarousal may be a necessary and unmodifiable adaptation.
Limitations
This was a pilot study with several notable limitations. Attrition from phone screen to study consent was high with 64 of 176 families failing to attend their first appointment. An additional 15 dropped out after the baseline research and clinical meeting and 8 more did not complete the 3 month F/U. Although, we are unable to report on the reasons for the attrition, high attrition rates are common in urban child mental heal treatment. Of the youth who are referred to child public sector clinics, 50 to 75% do not initiate treatment or drop out prematurely (Kazdin, Holland, & Crowley, 1997). With regards to the 64 families who did not attend a first appointment, some youth’s symptoms may have resolved and the others may have succumbed to Avoidance and refused to attend. Fourteen percent dropped out after their baseline interview for unclear reasons, but were included in the analysis as were the 8 who dropped out during the intervention study. It may be that a shorter research interview prior to commencement of intervention may have resulted in fewer dropouts. A larger more rigorous study will require greater outreach efforts and higher reimbursement rate for participation in the research interview.
The current study did not evaluate which elements of the CFTSI acted as the essential therapeutic mechanisms. It remains unclear, whether the hypothesized mechanism, caregiver support of the child, is the central active ingredient of the CFTSI. One may argue that the process of discussing symptoms acted to promote imaginal exposure, which therefore, was the primary reason for improvement. Also the frequency of use or the effectiveness of the Behavioral Skill Modules was not evaluated, nor or was the presumption that attention to recent PTE related case management issues would alleviate external stresses and permit greater focus on psychological concerns. Further studies that disaggregate the various elements of the CFTSI and evaluate their hypothesized effect will be necessary to refine the model and clarify which ingredients should be maintained.
Study participants experienced a wide variety of trauma types. Whether the CFTSI is more effective with specific trauma types is beyond the scope of the current evaluation but should be studied in future trials. In addition, the inclusion criteria set a low threshold of one new distressing symptom since the PTE, yet at baseline screening, most were symptomatic as measured by the PTSD-RI. Baseline severity scores on the PTSD-RI were 23.5 for the CFTSI group and 25 for the Comparison. Since, participants were drawn from an urban community confronted by multiple factors of social adversity associated with poverty; a low threshold for inclusion seems warranted. The finding that the mean number of different previous PTEs in the sample was 6 seems to justify the low threshold for inclusion. However, the number of prior PTEs experienced by the youth in the study leads to the question of whether the CFTSI was preventing or treating established PTSD. A future study with symptomatic children after a single incident with minimal trauma histories would assist in answering this question. One methodological issue in the study is the use of the PTSD-RI as both part of the interventions and an outcome measure. Since the PTSD-RI was administered by RA 3 months after the last session, it is unlikely a practice effect invalidated the outcomes. However, future and methodologically more rigorous studies require the use of a different outcome measure to assess diagnosis
Conclusion
The inability to recover after exposure to a PTE is a multi-factorial interaction among event, individual and post-traumatic factors. Clearly, the prevention of traumatic exposure would have the most robust outcomes in preventing posttraumatic psychopathology. Unfortunately, while universal primary prevention strategies may decrease children’s rates of exposure, it would be impossible to prevent all PTEs and subsequent Full or Partial PTSD. Effective early and brief intervention strategies that prevent the development of PTSD are a necessary and cost effective addition to behavioral health services. In addition to the problem of access to early intervention, there is a need for better identification of children that are in distress following a PTE. Caregivers are notoriously poor at recognizing acute PTSS in their children (Kassam-Adams, Garcia-Espana, Miller, & Winston, 2006; Shemesh, et al., 2005). It is incumbent upon child serving systems such as pediatric emergency departments and child welfare agencies to facilitate the identification of exposed children in need of early intervention. Early interventions grounded in the protective factors that support resilience and recovery should be able to prevent PTSD symptoms and the development of disorders. The current results suggest that CFTSI offers promise effective for just such an evidenced-based early intervention.
Figure 2.
Percent Youth Meeting Re-Experiencing, Avoidance, and Hyperarousal by Condition
Acknowledgements
Drs. Berkowitz and Marans are co-developers of the CFTSI. Dr. Stover coordinated research efforts. Miriam Berkman, J.D., MSW2 contributed to manual development. Hilary Hahn, MPH contributed to this article. Gina Poole, B.A. and Arthur Roy, B.A. were instrumental to the study. Statistical Consultant: Rani Desai3, Ph.D.
This study was funded by SAMHSA (U79 SM54318) and NIDA (K23 DA023334)
Abbreviations
- CFTSI
Child and Family Traumatic Stress Intervention, F/U-3-month follow-up
- PTSD-RI
UCLA PTSD Reaction Index
- TSCC
Trauma Symptom Checklist for Children
Footnotes
Clinical trial registry: URL: www.clinicaltrials.gov; Evaluation of the Child and Family Traumatic Stress Initiative, unique identifier: NCT0103165
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- Allison P. Multiple Imputation for Missing Data: A Cautionary Tale. Sociological Methods and Research. 2000;28:301–309. [Google Scholar]
- Angold A, Costello EJ. Mood and Feelings Questionnaire (MFQ) 1987 [Google Scholar]
- Berkowitz S, Stover CS. Trauma history questionnaire parent and child version. Yale Child Study Center Trauma Section; 2005. Unpublished questionnaire. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour Research and Therapy. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Boney-McCoy S, Finkelhor D. Psychosocial sequelae of violent victimization in a national youth sample. Journal of Consulting and Clinical Psychology. 1995;63(5):726–736. doi: 10.1037//0022-006x.63.5.726. [DOI] [PubMed] [Google Scholar]
- Briere J. Trauma Symptom Checklist for Children (TSCC) Odessa, FL: Psychological Assessment Resources; 1996. [Google Scholar]
- Centers for Disease Control and Prevention. Youth violence: Facts at a glance. 2009 Retrieved November 24, 2009, from http://www.cdc.gov/violenceprevention/pdf/YV_DataSheet_Summer2009-a.pdf.
- Cooley-Quille MR, Boyd RC, Frantz E, Walsh J. Emotional and behavioral impact of exposure to community violence in inner-city adolescents. Journal of Clinical Child and Adolescent Psychology. 2001;30(2):199–206. doi: 10.1207/S15374424JCCP3002_7. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod RK, Turner HA. Lifetime assessment of poly-victimization in a national sample of children and youth. Child Abuse and Neglect. 2009;33(7):403–411. doi: 10.1016/j.chiabu.2008.09.012. [DOI] [PubMed] [Google Scholar]
- Foa EB, Meadows EA. Psychosocial treatments for posttraumatic stress disorder: A critical review. Annual Review of Psychology. 1997;48:449–480. doi: 10.1146/annurev.psych.48.1.449. [DOI] [PubMed] [Google Scholar]
- Ghosh-Ippen C, Ford J, Racusin R, Acker M, Bosquet K, Rogers C, et al. Trauma events screening inventory-parent report revised: The Child Trauma Research Project of the Early Trauma Network and The National Center for PTSD Dartmouth Child Trauma Research Group. 2002 [Google Scholar]
- Hill H, Levermore M, Twaite J, Jones L. Exposure to community violence and social support as predictors of anxiety and social and emotional behavior among African American children. Journal of Child and Family Studies. 1996;5(4):399–414. [Google Scholar]
- Holm S. A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics. 1979;6(2):65–70. [Google Scholar]
- Horowitz K, McKay M, Marshall R. Community violence and urban families: experiences, effects, and directions for intervention. American Journal of Orthopsychiatry. 2005;75(3):356–368. doi: 10.1037/0002-9432.75.3.356. [DOI] [PubMed] [Google Scholar]
- Kahana SY, Feeny NC, Youngstrom EA, Drotar D. Posttraumatic stress in youth experiencing illnesses and injuries: An exploratory meta-analysis. Traumatology. 2006;12(2):148–161. [Google Scholar]
- Kassam-Adams N, Garcia-Espana JF, Miller VA, Winston F. Parent-child agreement regarding children's acute stress: The role of parent acute stress reactions. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(12):1485–1493. doi: 10.1097/01.chi.0000237703.97518.12. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Holland L, Crowley M. Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting & Clinical Psychology. 1997;65(3):453–463. doi: 10.1037//0022-006x.65.3.453. [DOI] [PubMed] [Google Scholar]
- Kenardy J, Thompson K, Le Brocque R, Olsson K. Information-provision intervention for children and their parents following pediatric accidental injury. European Child and Adolescent Psychiatry. 2008;17(5):316–325. doi: 10.1007/s00787-007-0673-5. [DOI] [PubMed] [Google Scholar]
- Kerr M, Stattin H. What parents know, how they know it, and several forms of adolescent adjustment: Further support for a reinterpretation of monitoring. Developmental Psychology. 2000;36(3):366–380. [PubMed] [Google Scholar]
- Kerr M, Stattin H, Trost K. To know you is to trust you: Parents' trust is rooted in child disclosure of information. Journal of Adolescence. 1999;22(6):737–752. doi: 10.1006/jado.1999.0266. [DOI] [PubMed] [Google Scholar]
- Kliewer W, Cunningham JN, Diehl R, Parrish KA, Walker JM, Atiyeh C, et al. Violence exposure and adjustment in inner-city youth: Child and caregiver emotion regulation skill, caregiver-child relationship quality, and neighborhood cohesion as protective factor. Journal of Clinical Child & Adolescent Psychology. 2004;33(3):477–487. doi: 10.1207/s15374424jccp3303_5. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Weis R, O'Hare E, Rubin EC. Development and initial validation of the parent behavior inventory. Psychological Assessment. 1999;11(4):534–545. [Google Scholar]
- Margolin G. Effects of domestic violence on children. In: Trickett PK, Schellenbach CJ, editors. Violence against children in the family and the community. 1998. pp. 57–101. [Google Scholar]
- McCaig LF, Nghi L. National hospital ambulatory medical care survey: 2000 emergency department summary. Advance Data. 2002;(326):1–31. [PubMed] [Google Scholar]
- McDonald R, Jouriles EN, Ramisetty-Mikler S, Caetano R, Green CE. Estimating the number of American children living in partner-violent families. Journal of Family Psychology. 2006;20(1):137–142. doi: 10.1037/0893-3200.20.1.137. [DOI] [PubMed] [Google Scholar]
- Overstreet S, Braun S. Exposure to community violence and post-traumatic stress symptoms: Mediating factors. [Journal; Peer Reviewed Journal] American Journal of Orthopsychiatry. 2000;70(2):263–271. doi: 10.1037/h0087828. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychological Bulletin. 2003;129(1):52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Procidano ME, Heller K. Measures of Perceived Social Support from Friends and from Family - 3 Validation Studies. American Journal of Community Psychology. 1983;11(1):1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- Pynoos R, Rodriguez N, Steinberg A, Stuber M, Frederick C. The UCLA PTSD reaction index for DSM IV (Revision 1) Univerity of California, Los Angeles Trauma Psychiatry Program; 1998. [Google Scholar]
- Pynoos R, Rodriguez N, Steinberg AM, Stuber M, Frederick C. The UCLA PTSD reaction index for DSM IV (Revision 1) Los Angeles: Univerity of California, Los Angeles Trauma Psychiatry Program; 1998. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Reynolds CR, Kamphaus RW. BASC-2: Behavior assessment system for children second edition. Circle Pines, MN: AGS Publishing; 2004. [Google Scholar]
- Rothbaum BO, Davis M. Applying learning principles to the treatment of post-trauma reactions. Annals of the New York Academy of Sciences. 2003;1008:112–121. doi: 10.1196/annals.1301.012. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Sharfstein S. New task force will address early childhood violence. Psychiatric News. 2006;41(3) [Google Scholar]
- Shemesh E, Newcorn JH, Rockmore L, Shneider BL, Emre S, Gelb BD, et al. Comparison of parent and child reports of emotional trauma symptoms in pediatric outpatient settings. Pediatrics. 2005;115(5):582–589. doi: 10.1542/peds.2004-2201. [DOI] [PubMed] [Google Scholar]
- Stallard P, Velleman R, Salter E, Howse I, Yule W, Taylor G. A randomized controlled trial to determine the effectiveness of an early psychological intervention with children involved in road traffic accidents. Journal of Child Psychology and Psychiatry. 2006;47(2):127–134. doi: 10.1111/j.1469-7610.2005.01459.x. [DOI] [PubMed] [Google Scholar]
- Stattin H, Kerr M. Parental monitoring: A reinterpretation. Child Development. 2000;71(4):1072–1085. doi: 10.1111/1467-8624.00210. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index. Current Psychiatry Reports. 2004;6(2):96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Trickett EJ. Ecology and primary prevention: Reflections on a meta-analysis. American Journal of Community Psychology. 1997;25(2):197–205. [Google Scholar]
- Valentino K, Berkowitz S, Stover CS. Parenting behaviors and posttraumatic symptoms in relation to children's symptomatology following a traumatic event. Journal of Traumatic Stress. 2010;23:403–407. doi: 10.1002/jts.20525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Huska JA, Keane TM. PTSD checklist- civilian version. Boston, MA: National Center for PTSD Behavioral Science Division; 1994. [Google Scholar]
- Windle M, Miller-Tutzauer C. Confirmatory Factor Analysis and Concurrent Validity of the Perceived Social Support-Family Measure among Adolescents. Journal of Marriage and Family. 1992;54(4):777–787. [Google Scholar]