Abstract
This multigenerational study empirically demonstrates the extent to which offspring whose parents experienced childhood abuse are at increased risk of being abused or neglected. Females with substantiated childhood sexual abuse and nonabused comparison females were assessed at six points spanning 18 years in a prospective, longitudinal study. Nonabusing parents or caregivers and offspring were also assessed. Descriptive results indicate that offspring born to mothers with histories of sexual abuse were more likely to be born preterm, have a teenage mother, and be involved in protective services. Abused mothers were more likely to be high-school dropouts, be obese, and have experienced psychiatric problems, substance dependence, and domestic violence. Results provide evidence for the advantages of intervention and prevention programs for victims of childhood maltreatment and their families. Primary prevention/intervention efforts extending throughout development and focusing on the cumulative risk to offspring will likely improve victim outcomes and curtail intergenerational transmission of adversity.
Keywords: child abuse, child welfare, health consequences, intergenerational transmission
Wilma is a 20-year-old single mother whose 2½-year-old son was removed from her custody by local child protective services because of allegations that he was being neglected. These allegations were brought by EMS personnel who responded to Wilma's frantic 911 call referencing the drowning of her younger 10-month-old son in the bathtub. When EMS arrived they found a heroin-intoxicated mother and her son attempting to revive the deceased infant. Months later in an inpatient drug rehabilitation unit, a clinically depressed, suicidal Wilma recounted the incident, admitting the use of illegal drugs and alcohol as a means to cope with severe depression and the painful reminders of her traumatic childhood—Wilma was continually raped by her father from the time she was a young girl of 6 or 7 until the abuse was disclosed to a social worker when she was 12. With the help of her court testimony, Wilma's father was permanently removed from the home and was incarcerated within the proceeding year. Although the prosecution resulted in some relief that she would finally be safe from further abuse, Wilma reflects on how the harmful effects of her abuse experience were only just beginning.
Although admittedly dramatic, Wilma's case history is a true story (with names and details changed to protect confidentiality)—a story that provides a descriptive example of the compounded struggles facing many child abuse survivors and illustrates the potential for intergenerational transmission of effects of childhood abuse and their dangerous consequences for offspring. It has been estimated that as many as 30% of child abuse victims go on to abuse their own children (Kaufman & Zigler, 1987), but Wilma's story illustrates how the potential for harm to such offspring may extend beyond their risk for being abused and neglected. For example, some of the more common long-term consequences of childhood abuse—such as chronic depression, psychiatric disorders, or substance dependence—may not directly result in the perpetration of child maltreatment, but can have devastating effects on the emotional, psychological, cognitive, and even physical well-being of offspring. Hence, Wilma's case underscores the complex network of risk factors that may be operating in the lives of children born to childhood abuse victims, as many of these children are at risk for (a) being abused or neglected either at the hands of their own care-givers or by other violent or exploitive individuals who are allowed access to vulnerable children, and (b) various deleterious consequences of having a caregiver who suffers from the emotional and psychiatric sequelae of his or her own childhood abuse. The purpose of this article is twofold; first to briefly review theoretical and empirical knowledge regarding various risk factors that constitute threats to the safety and well-being of offspring born to caregivers with histories of childhood abuse, and second to present descriptive data from a multigenerational longitudinal study comparing two groups of children—offspring born to mothers who were sexually abused in childhood and offspring born to nonabused comparison mothers—to provide a snapshot of the compounded impact of these various risk factors and outcomes.
Intergenerational Transmission
In the early 1960s a premier developmental hypothesis in the field of child abuse and neglect was the notion that abusing parents were themselves abused and that abused and neglected children would become tomorrow's perpetrators of family violence (Curtis, 1963). This alleged causal relationship was critically evaluated as subsequent theory and reviews stressed the key roles of social determinants and ecological factors (Brofenbrenner, 1977; Garbarino, 1976). Although the roles of poverty and social discrimination were upheld as indisputable contributors to family failure and abuse, it was also articulated that abusive parents do not fit a single economic, social, or psychological pattern and that no single intrinsic characteristic alone causes abuse—including notions that abused children will inexorably wind up abusing their own children (Cicchetti & Aber, 1980; Kempe & Kempe, 1978).
A subsequent empirical appraisal of the rate of intergenerational transmission of child abuse offered cumulative evidence for a rate of approximately 30%, roughly six times the national average (Kaufman & Zigler, 1987). Several more recent studies have confirmed that a substantial number of childhood abuse victims go on to abuse or neglect their own children (DiLillo, Termblay, & Peterson, 2000; Dixon, Hamilton-Giachritsis, & Browne, 2005; Egeland, Jacobvitz, & Sroufe, 1988; Zuravin, McMillen, DePanfilis, & Risley-Curtiss, 1996). These investigations also highlighted additional risk factors that go beyond abuse and neglect to include various characteristics of caregivers that may impinge on offspring well-being.
Empirical Links
It has been recognized that pathways to intergenerational transmission of the effects of childhood abuse are likely the result of a complex interaction between risk, protective, and mediating factors (Egeland et al., 1988). Our discussion of empirical links focuses on broad categories of empirically derived variables that are thought to characterize risk to children in at least one of two ways: (a) placing offspring directly at risk for being abused or maltreated by caregivers (or others outside the family) or in other ways characterize high-risk environments in which childhood maltreatment is likely to occur, and (b) through characteristics of a caregiver who was abused in childhood, which place the next generation at risk for a host of deleterious outcomes including social, emotional, and physical maldevelopment. The potential for such a set to be unwieldy is high and could easily contain both variables outside the scope of relevant theoretical models, or overly exogenous constructs that exceed conventional measurement capabilities. Therefore, we adhered to the following operational definition when selecting relevant risk factors for inclusion in our review (and subsequent analyses): risk factors must be empirically supported as operating on two distinct levels of analysis. Variables must (a) be sequelae of childhood abuse or directly attributable to the experience of childhood abuse by having been shown to describe the maldevelopment of abuse survivors, and (b) constitute substantial risk to the well-being of offspring—including, but not limited to, risk for maltreatment. Four broad areas are reviewed including caregiver distress (psychiatric problems, posttraumatic stress disorder [PTSD], and alcohol and substance usage), interpersonal and family violence, teen pregnancy, and health consequences. It should be noted that research in this area is complicated by the substantial co-occurrences of childhood abuse victimization with a host of alternative risk factors associated with childhood adversity. Thus, it is difficult to determine whether childhood abuse itself is an independent causal agent in intergenerational transmission, and teasing out the relative importance of any one risk-factor remains a significant challenge as they are largely intercorrelated, often occur comorbidly, and are rarely assessed in the same study.
Caregiver distress
Potential negative long-term consequences of childhood maltreatment often consist of psychiatric problems including depression, anxiety and personality disorders, antisocial behaviors, and suicidality (e.g., Briere & Elliott, 2003; Neumann, Houskamp, Pollock, & Briere, 1996; Trickett, Noll, Reiffman, & Putnam, 2001) as well as PTSD (Boney-McCoy & Finkelhor, 1995; Noll, Horowitz, Bonanno, Trickett, & Putnam, 2003) and its associated symptoms including dissociative experiences (Putnam, 1996). These psychiatric symptoms may interfere with accurate appraisals of threat and consequences, impair judgment, and preclude recognition of potential danger and appropriate escape or action (Bugental, 1993; DePrince & Freyd, 2004; Jones & Barlow, 1990). These conditions have also been shown to be key contributors to the well-being of offspring (Downey & Coyne, 1990; Lovejoy, Graczyk, O'Hare, & Neuman, 2000) including poor physical health (Billings & Moos, 1983; Weissman et al., 1986), impaired cognitive ability (Brennan et al., 2000), disrupted infant/mother attachment (Teti, Gelfand, Messinger, & Isabella, 1995), and risk for maltreatment (DeBellis et al., 2001). Alcohol and substance abuse is quite often comorbid with psychiatric distress and PTSD (Karlovic, Solter, Krizo, & Potkonjak, 2004), and there is considerable evidence for a strong association between adult alcohol and substance abuse and early child maltreatment experiences (Kilpatrick et al., 2000) even when co-occurring forms of childhood adversity were controlled (Anda et al., 2002). The deleterious consequences for children of alcohol and substance dependent parents are numerous (e.g., Bennett, Wolin, & Reiss, 1988) and include increased risk for maltreatment (e.g., McCloskey & Bailey, 2000). Thus, parental psychiatric problems place children at risk for a host of deleterious consequences that are likely amplified in the presence of alcohol and substance misuse.
Interpersonal and family violence
Family-of-origin violence has been shown to be predictive of high rates of subsequent sexual and physical victimizations (Capaldi & Clark, 1998; Noll, Horowitz, et al., 2003). Domestic and interpersonal violence is a primary family stressor, a source of significant family dysfunction, and a key indicator of a lack of familial psychological, emotional, and social resources (Ehrensaft et al., 2003). The use of physical force during conflict characterizes the family system such that aggressive conflicts between adults may spill over to facilitate conflictual responses by children and vice versa. Exposure to physical abuse in childhood coupled with exposure to interpersonal violence as an adult has been shown to be the most powerful predictor of whether a mother was physically abusive to her child (Coohey & Braun, 1997). A large percentage of interpersonal victimization and domestic violence involves the consumption of alcohol and other substances (Fals-Stewart, Leonard, & Birchler, 2005). Thus, it is increasingly clear that it may be vital to incorporate the cumulative nature and interactions among multiple risk factors in our models of intergenerational transmission.
Teen pregnancy
Inordinately high rates of teen pregnancy have been documented for victims of childhood maltreatment (Anda et al., 2002; Boyer & Fine, 1992; Noll, Trickett, & Putnam, 2003; Roosa, 1997). Teenage mothers have been characterized as having low self-esteem and self-concept (Pete-McGadney, 1995), less likely to have completed high school and be gainfully employed (Rosenheim, 1992), more dependent on public assistance and living in persistent poverty (Maynard, 1997; Moore et al., 1993; Zabin, Wong, Weinick, & Emerson, 1992) than their nonpregnant peers. Research has demonstrated a significant correlation between low maternal age and the occurrence of child abuse and neglect (Dixon, Browne, & Hamilton-Giachritsis, 2005) and how this risk is compounded when the pregnancy is unintended and the child is born into poverty (Coley & Chase-Lansdale, 1998). Children born to teenage mothers have been shown to possess poorer cognitive ability and academic performance (Coley & Chase-Lansdale, 1998; Levin, Pollack, & Comfort, 2001) more behavioral difficulties, delinquency, earlier onset of sexual activity, and teenage parenthood themselves (Furstenberg, Brooks-Gunn, & Morgan, 1987; Jaffee, Caspi, Moffitt, Belsky, & Silva, 2001; Spieker, Larson, Lewis, Keller, & Gilchrist, 1999) than do children of older mothers. Although these effects have been upheld even when several demographic confounds were controlled (Hardy et al., 2006), it remains difficult to disentangle effects on offspring associated with low education, poverty, and lack of social support from those associated with early motherhood.
Infant prematurity
Several retrospective studies have reported that mothers with a history of childhood abuse were more likely to give birth to preterm infants than controls even after controlling for potential confounds such as poor prenatal care and poverty (Stevens-Simon, Kaplan, & McAnarney, 1993; Van Der Leder & Raskin, 1993). The gynecological immaturity and decreased placental size of adolescent mothers (Menacker, Martin, MacDorman, & Ventura, 2004; Wallace, Aitken, Milne, & Hay, 2004) is one plausible explanation for this link. Moreover, increased maternal cortisol secretion (i.e., that may accompany persistent PTSD in trauma survivors) may signal premature parturition (Majzoub et al., 1999; Wadhwa, Sandman, Porto, Dunkel-Schetter, & Garite, 1993). Although the majority of premature newborns survive, they have unique developmental needs, are often demanding and inconsolable, and require inordinate patience on the part of parents. When this patience runs thin premature babies are at greater risk for maltreatment. Outcomes for children born prematurely also include sensory and intellectual impairments, respiratory, gastrointestinal and renal problems, and other neurological disorders (Slattery & Morrison, 2002).
Obesity
There is increasing evidence for an association between childhood abuse and the subsequent development of obesity (Felitti, 1991; Grilo et al., 2005). Several psychosocial conditions are comorbid with both childhood abuse and obesity such as depression, behavioral impulsivity, drug and alcohol use, difficulties with peers, and poor self-esteem (Beitchman et al., 1992; Trickett et al., 2001) which may help explain this association. Having a parent who is obese is a highly salient risk-factor for the development of obesity and diabetes in children (Agras, Hammer, McNicholas, & Kraemer, 2004; Francis & Birch, 2005). Obese children are also at risk for a host of emotional and social difficulties (Zeller & Modi, 2006).
Methodological Challenges
Although there are notable exceptions (e.g., Egeland, Jacobvitz, & Papatola, 1987), much of what we know about the intergenerational transmission of the effects of childhood maltreatment comes from uncontrolled cross-sectional, retrospective studies of at-risk samples. Prospective studies are rare, follow-up periods are relatively short, and assessment batteries are often limited. Intergenerational studies can be methodological and statistical nightmares. For example, members of longitudinal cohorts reproduce at differing rates and schedules presenting unique challenges for multigenerational analyses. Offspring at different developmental stages (e.g., infants versus adolescents) can result in substantial measurement and assessment challenges. Furthermore, evolving theory, paradigm shifts, and ever-changing technology can result in assessments used early on being deemed invalid or outdated requiring the adoption of new procedures or instruments midway through a study. The inclusion of siblings is often preferred because many longitudinal cohort studies begin with relatively low sample sizes that are somewhat attritted and because sibling selection is somewhat arbitrary. Including siblings can inflate intraclass correlations resulting in substantial interindividual dependence and biased estimates. Complications are also introduced when offspring die young precluding assessment of those who may have been at highest risk for maldevelopment. Finally, although being among the most important models to test, attempts to perform analyses in a multivariate system—that is, where correlated risk-factors can be evaluated for their relative importance in predicting deleterious outcome—are exceptionally challenging because of issues related to nonrandom missing data. These are just a few of the methodological issues that complicate the quantification of multigenerational life trajectories.
The Present Study
The present study is a multigenerational attempt to describe the ways in which maternal histories of childhood abuse place offspring at risk for various forms of adversity. We have compiled data gathered during the course of a prospective, longitudinal study of the long-term effects of childhood sexual abuse on female development. The data for the present analysis concern risk factors operating in the lives of the offspring born to the original sample and include maternal characteristics such as high-risk behaviors, psychopathology, and health consequences that have been empirically upheld as (a) sequelae of childhood abuse, and (b) constituting significant potential harm to offspring. The data also include characteristics of offspring regarding their general well-being (including involvement in protective services and cognitive functioning) and characterize their risk for subsequent maldevelopment and hardship (including being born to a teen mother and being born premature). In compiling these data for offspring born to mothers who were abused in childhood, and providing a direct comparison of the prevalence and incidences of these constructs to a demographically similar sample of children born to mothers who did not experience this same type of childhood adversity, we attempt a descriptive analysis of the intergenerational transmission of the effects of childhood abuse.
Method
Participants
Study participants span three generations, sexually abused and comparison females comprising the original sample recruited for participation in the longitudinal study, the caregivers (usually the mother) of these females, and the offspring of these females. Henceforth the caregivers of the original sample will be referred to as the first generation (G1), the original sexually abused and comparison female participants of the longitudinal study will be referred to as the second generation (G2), and the offspring of these original participants will be referred to as the third generation (G3).
Original sample (G2)
Sexually abused females (N = 84) were referred by child protective service (CPS) agencies in the greater Washington, D.C., metropolitan area. Eligibility criteria included: (a) age 6 to 16; (b) participation within 6 months of disclosure; (c) substantiated contact sexual abuse including genital contact and/or penetration; (d) perpetration by a family member (parent, grandparent, older sibling, uncle); and (e) participation of a nonabusing caregiver who was usually the biological mother (i.e., constituting the G1 sample) to inform on participants' functioning, family environment, demographics, and provide some limited information regarding her own developmental history. CPS records indicated that the median age at onset of abuse was 7.8 years, the median duration was 24 months; 70% experienced vaginal and/or anal penetration, and 60% of perpetrators were the primary father figure (biological fathers, stepfathers, or mothers' live-in boyfriends). The information on the perpetrators, the average age of onset, and the average duration is similar to comparable information reported in national surveys of protective services caseloads in years proximal to obtaining the sample via data reported in the National Incidence Study conducted by the National Center on Child Abuse and Neglect (1988).
The comparison sample (N = 82) was recruited via advertisements in community newspapers and posters in welfare, daycare, and community facilities in the same neighborhoods in which the abused participants lived. Comparison families contacted study personnel and were screened for eligibility, which included having no prior contact with protective service agencies and being demographically similar to a same-aged abused participant. Of the comparison families, 70% resided in the same zip code district, 20% in adjacent districts, and 10% in comparable, nearby districts. Comparison females were similar to the abused females in terms of racial/ethnic group, age, predisclosure socioeconomic status, family constellation (one or two parent families), and other nonsexual traumas.
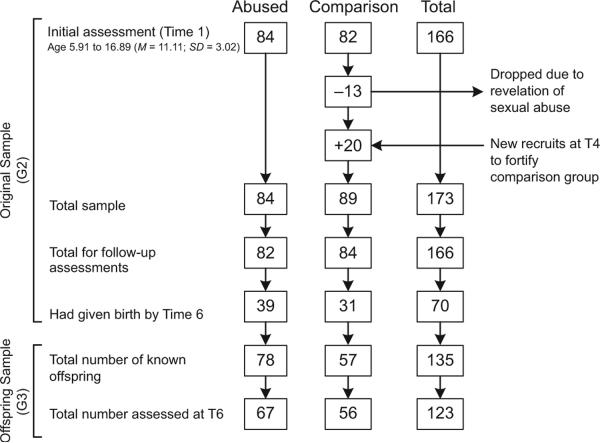
Of the sample, 49% were Caucasian, 46% African American, 4% Hispanic, and 1% Asian American. The study design flow is depicted in Figure 1. At the initial assessment (Time 1; T1), females ranged in age from 5.91 to 16.89 (M = 11.11, SD = 3.02) and reported low to middle socioeconomic status (Hollingshead, 1975). Five follow-up assessments were conducted (Times 2 through 6; T2–T6). Ages at follow-up assessments were as follows: T2 6.92 to 18.20 (M = 12.22, SD = 2.96); T3 7.78 to 20.22 (M = 13.42, SD = 3.00); T4 10.63 to 25.91 (M = 18.05, SD = 3.42); T5 13.25 to 26.67 (M = 19.85, SD = 3.24); T6 18.12 to 32.14 (M = 24.89, SD = 3.51).
Figure 1. Multigeneration Study Flow of the Original Sample (G2) and Their Offspring (G3).
At some point after entry into the study, 13 comparison females revealed that they had experienced some form of childhood sexual abuse and were dropped from the study (see Figure 1). At T4, 20 new comparison females were recruited (utilizing the original recruitment methods) to fortify the sample for longitudinal follow-up. More than 96% of the total sample were retained and reassessed at T5 and T6 follow-up assessments. By the conclusion of T6, 70 females reported having had at least one child.
Offspring sample (G3)
At the conclusion of the T6 assessment there were 135 known offspring; 78 offspring of abused mothers (OA), and 57 offspring of comparison mothers (OC). These offspring ranged in age from 5 months to 11 years 10 months with the mean age being similar across groups (OA M = 4.60, SD = 3.35, OC M = 3.56, SD = 2.57; p = n.s.) and were 53.66% minority (mostly African American with 3% Hispanic and 1% Asian). There were significantly more minority offspring in the OC sample (66.12%) than the OA sample (43.23%) F(1, 133) = 5.61, p < .05. Neither the average number of children per family nor gender differed significantly across the OA and OC groups (see Table 1). The G3 sample included 76 only-children, 18 sibling pairs, 5 sibling trios, 2 families with four siblings, and 0 multiples. Of the 135 known offspring, 123 (91%) were assessed as part of the T6 protocol. Hence, G3 outcome information was not available for 12 offspring—6 were unable to be scheduled (3 OA, 3 OC), 3 had fathers who expressed their wishes that their children not participate (all 3 OA), and 3 were deceased (all 3 OA). Of the deceased, 2 died from complications of prematurity and one drowned in a bathtub as a result of maternal neglect.
Table 1.
Percentage of Occurrence (± SE) for Variables Assessed Across the Three Generations Arrayed By the Original (G2) Abused and Comparison Groupings
| Variable | Abused Group | Comparison Group | F(df), p |
|---|---|---|---|
| G1 (caregivers): | N = 60 | N = 68 | |
| History of childhood sexual abuse | 49.23 ± 13.15 | 16.01 ± 4.91 | 15.41(1, 124), p < .01 |
| G2 (original sample): | N = 82 | N = 84 | |
| At least one sexual victimization | 29.55 ± 8.78 | 15.54 ± 5.13 | n.s. |
| At least one physical victimization | 56.85 ± 14.99 | 30.33 ± 10.45 | 9.67(1, 162), p < .01 |
| Childhood depression via CDI | 15.11 ± 5.45 | 7.08 ± 3.13 | n.s. |
| Adulthood depression via BDI | 18.19 ± 6.56 | 5.87 ± 2.10 | 6.45(1, 162), p < .01 |
| PTSD | 13.14 ± 4.14 | 6.16 ± 2.23 | n.s. |
| At least one psychiatric diagnosis | 30.06 ± 10.02 | 13.96 ± 4.19 | 5.37(1, 162), p < .05 |
| Substance dependence | 19.44 ± 6.88 | 5.46 ± 2.42 | 6.28(1, 162), p < .05 |
| Alcohol dependence | 13.35 ± 3.19 | 2.56 ± 0.98 | 5.01(1, 162), p < .05 |
| Regular smoker | 39.68 ± 10.14 | 29.78 ± 9.05 | n.s. |
| Dissociation via DES | 12.23 ± 4.11 | 8.88 ± 3,89 | n.s. |
| High school dropout | 15.23 ± 5.34 | 6.09 ± 2.13 | 6.07(1, 162), p < .05 |
| Domestic violence | 53.23 ± 14.23 | 24.01 ± 10.76 | 9.45(1, 162), p < .01 |
| Obese | 42.33 ± 10.23 | 28.01 ± 9.45 | 5.67(1, 162), p < .05 |
| G3 (offspring): | OA N = 78 | OC N = 57 | |
| Racial minority | 43.56 ± 10.11 | 66.07 ± 9.22 | 5.67(1, 132), p < .05 |
| Female | 56.06 ± 8.00 | 49.12 ± 7.54 | n.s. |
| Children per family (average #) | 1.74 ± 0.22 | 1.70 ± 0.23 | n.s. |
| Deceased (#) | 3 | 0 | NAc |
| Unintendeda | 22.56 ± 8.12 | 23.51 ± 9.34 | n.s. |
| Born to a teenage mother | 37.25 ± 9.11 | 20.26 ± 8.34 | 4.99(1, 130), p < .05 |
| Born preterma | 19.11 ± 7.12 | 10.06 ± 6.12 | 4.97(1, 118), p < .05 |
| Child protective services involvedb | 17.91 ± 3.34 | 1.78 ± 0.01 | 12.23(1, 118), p < .01 |
| Cognitive deficitb | 32.02 ± 9.98 | 22.11 ± 7.61 | n.s. |
Note: Mean comparisons based on individual F tests via ANCOVA models with minority status and age covaried (Bonferroni corrections imposed). Number of siblings (0–3) and gender were additional covariates in G3 models. CDI = Childhood Depression Inventory; BDI = Beck Depression Inventory; DES = Dissociative Experiences Scale; PTSD = posttraumatic stress disorder; OA = offspring born to abused mothers; OC = offspring born to comparison mothers.
data available only for T6 assessments (N = 123);
data available only for a restricted developmental range (N = 86);
test not applicable because of zero variance in the OC sample.
Procedures
Assessments were completed in two 3-hr sessions by female-trained female clinical interviewers. In general, the bulk of assessments were focused on the original G2 sample of abused and comparison females. These assessments were comprehensive and spanned biological, psychological, and social domains. For purposes of the present investigation, we focus on a subset of constructs assessed during the final three assessments of this longitudinal study (T4–T6), reporting only on those constructs hypothesized to constitute significant risk factors associated with deleterious outcome for offspring. Caregivers of these original participants (G1) functioned mainly as informants of their daughters' functioning, but also provided limited self-reports of their own functioning and retrospective reports of their past histories. Offspring of the original sample (G3) were assessed as part of the T6 protocol and varied considerably with respect to age and developmental stage thus resulting in variable assessment tools and variable Ns for offspring outcomes.
G1 caregivers provided consent for G2 participants who were younger than the age of 18; those 18 and older signed for themselves, and those younger than 18 also provided assent. G2 mothers provided consent for G3 participants. All participants were awarded monetary compensation at a rate put forth by the National Institutes of Health Normal Volunteer Office. The study received approval from the University Institutional Review Board and obtained a Federal Certificate of Confidentiality.
Maintaining and engaging the G2 sample over the course of this longitudinal study was a significant challenge. Several strategies were employed including (a) frequent mailings (birthday and holiday cards, quarterly newsletters) and certified letters to maintain current addresses, (b) home visits to those whose telephone service was interrupted or unlisted, (c) address tracking software, and (d) obtaining information for two additional contact persons (family members, friends) who would likely have knowledge of participants' whereabouts. In addition, by communicating the importance of scientific knowledge gained from this type of longitudinal research, the research staff was able to foster considerable participant fulfillment as many participants viewed the study as a chance to contribute to something bigger than themselves and took tremendous pride in doing so. Finally, the research staff was inordinately cohesive, dedicated, consistent, and diligent.
Measures
Because of space constraints, measurement instruments are not discussed in detail as they are either widely used assessment tools or have been detailed in the referenced manuscripts.
Original sample (G2) assessments
Traumatic victimization histories were assessed via the Comprehensive Trauma Interview (Noll, Horowitz, et al., 2003). Analyses included up to four of the most recent victimizations that occurred subsequent to study entry and were subjectively rated by participants as being “very” or “extremely” upsetting as anchored to their identified “most upsetting” traumatic experience. Sexual victimizations were sexual assaults or rapes involving bodily contact (e.g. genital fondling) by peers defined as individuals within 4 years of age of victims younger than 18, or any incident for victims older than 18. Nonpeer (i.e., individuals 4 or more years older than victims younger than 18) sexual victimizations occurring subsequent to their referring abuse were included for sexually abused participants. Physical victimizations were contact (e.g., leaving marks or requiring medical attention) peer or nonpeer assaults. To increase reliability of responding, only victimizations reported at least twice during consecutive interviews, or those occurring during the time period preceding T6, were included.
Domestic Violence was assessed via the Domestic Conflict Inventory (Margolin, 1981), which assesses a host of violent acts (e.g., physically threatened, hit, or beaten) perpetrated by an intimate partner. Domestic violence was defined as the most recent occurrence of having experienced three or more of these acts at the hands of an intimate partner. Dropout was defined via self-reports of having not completed high school and not being currently enrolled in high school or GED classes by the conclusion of the T6 assessment.
For the remaining constructs, Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV) diagnostic threshold or clinical cutoff scores (according to published norms) were used to define each occurrence. If multiple occurrences were observed, the most recent occurrence was included in present analyses. Posttraumatic Stress Disorder (PTSD) was assessed via the Diagnostic and Statistical Manual of Mental Disorders (3rd ed.; DSM-IV) PTSD criteria inventory (Davidson, Kudler, & Smith, 1989) which was modified to be DSM-IV compliant and concerned the traumatic event identified by the participant as the “worst” or “most upsetting.” Depression was assessed via the Childhood Depression Inventory (Kovacs, 1981) until age 18 and the Beck Depression Inventory (Beck, Steer, & Brown, 1986) for adults aged 19 and older. Dissociation was assessed via the Dissociative Experience Scale (Berstein & Putnam, 1986). Current and lifetime reports of psychiatric diagnoses were assessed via the Scheduled Clinical Interview for DSM Diagnoses (SCID; First, Spitzer, & Williams, 1995). For the present analyses, Psychiatric Diagnosis was defined as having reached DSM-IV criteria for at least one of the following disorders: anorexia nervosa/bulimia, attention deficit/hyperactivity disorder, oppositional defiant disorder, bipolar disorder, major depression, obsessive compulsive disorder, generalized anxiety disorder, panic disorder, or social phobia. The SCID was also used to assess Alcohol Dependence and Substance Dependence, each of which quantified separately for analyses. Being a Regular Smoker was assessed via direct queries regarding smoking behaviors and was defined as daily consumption of cigarettes. If mothers reported multiple periods of regular smoking, the most recent occurrence was included in present analyses. Obesity was assessed in adulthood via standardized height and weight assessments and was defined per Centers for Disease Control (CDC) guidelines as body mass index (BMI) ≥ 30.
Offspring sample (G3) assessments
Born to a teenage mother was assessed for all 135 known offspring, was calculated as the G3 date of birth minus the respective G2 date of birth, and was defined as being born to a mother who was 18 years 11 months old or younger. This variable was calculated for all 135 known offspring. The remaining G3 outcome variables were assessed at the T6 assessment session and, unless otherwise noted, were available for 123 offspring. G2 mothers reported on the intendedness of each pregnancy with Unintended being defined by combining five items from an intensive labor and birth semistructured interview and questionnaire (α = .78). Two items concerned being unmarried or not cohabitating with the index G3 biological father at either conception and at the time of the birth. Three additional questions concerned the extent to which mothers were reluctant to get pregnant and assessed ambivalent feelings with regard to becoming pregnant and giving birth to the index G3 child. For purposes of the present analyses, a G3 participant was considered unintended if scores on this scale were 2 standard deviations above the sample mean. Born preterm was gleaned from hospital labor and delivery records obtained via a release signed by each G2 and was defined as gestational age of fewer than 37 weeks. Involved in Child Protective Services (CPS) was defined as G2 reports of her children having been neglected, physically abused, or sexually abused, and having been assigned a caseworker in participants'local jurisdiction as a result. Cognitive deficit (N = 86) was defined as scoring 1.5 standard deviations below the population mean according to norms on one of two cognitive assessments: (a) the Bayley Scales of Infant Development 2nd edition (mental scales only; Bayley, 1993) for ages 11 to 42 months, or (b) the Peabody Picture Vocabulary Tests–Revised (PPVT-R; Dunn & Dunn, 1981) scores for ages 43 months and older. The reduced N reflects those who were available for assessment and within the restricted developmental range as per Bayley and PPVT-R protocol instructions.
Caregiver sample (G1) assessments
Data were available for 128 caregivers. As noted earlier, these assessments were limited. For purposes of the present analyses, only caregiver self-reports of sexual abuse were included. G1 history of childhood sexual abuse was gleaned from a maternal developmental history questionnaire assessed at T1 using an intensive interview format and probing sensitive details of child abuse histories. Given that these were retrospective in nature, reports of G1 childhood sexual abuse were not cross-verified with CPS reports.
Analyses and Results
Mean comparisons
Percentages associated with the occurrence of each variable assessed are included in Table 1. Group mean comparisons were conducted via ANCOVA models with age and minority status covaried and Bonferroni alpha corrections imposed using SPSS (v. 13.0). Results indicated that significantly more caregivers (G1) of abused females retrospectively reported being sexually abused in childhood. Abused G2 females were more likely than comparison G2 females to have experienced at least one physical victimization, reached clinical cutoff for adult depression, be diagnosed with at least one psychiatric disorder, report a substance dependence, report an alcohol dependence, be a high-school dropout, be the victim of domestic violence, and be obese. G3 offspring born to abused mothers (OA) were more likely than offspring born to comparison mothers (OC) to have been born to a teen mother, have been born premature, and have been involved in child protective services. Intraclass correlations for G3 variables ranged from .02 to .13 with none reaching significance thus indicating negligible effects of sibling inclusion. However, a variable quantifying sibling number (0, 1, 2, or 3) was included in all models as an additional covariate to provide further assurance that the inclusion of siblings did not inflate results.
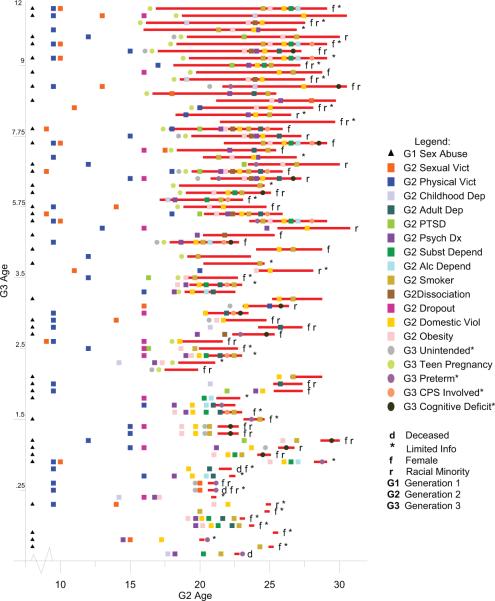
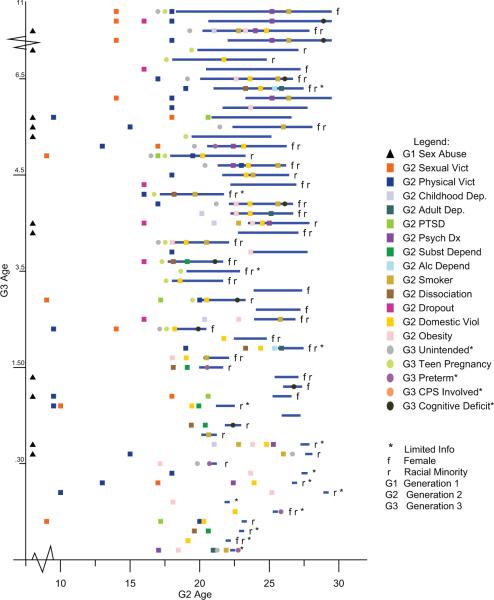
Lifeline plots
Because of fluctuations in sample size and multiple forms and patterns of missing data, neither multivariate comparisons among variables nor multivariate predictions of offspring outcomes were performed on these data. Instead, we opted to present a descriptive account of the number of risk factors operating in the lives of each offspring individually and to place these risk factors in developmental context for both the G2 and G3 participants. The resulting “lifeline” plots depicted in Figures 2 and 3 (OA and OC, respectively) represent the lifeline of each G3 participant superimposed in the life span of his or her G2 mother. In these plots, the age of the G2 mother is arrayed horizontally on the x-axis and the age of G3 offspring is arrayed vertically on y-axis. By way of example, the oldest child in the OA sample (see the topmost lifeline in Figure 2) is an 11-year, 10-month-old non-minority girl who was born when her mother was approximately 17 years old and was last assessed when her mother was approximately 28 years old. The lifeline of this G3 offspring is superimposed on the life span of her G2 mother, and symbols representing the various risk factors are plotted with respect to age of the G2 mother at the occurrence of each. The resulting lifeline plots represent the cumulative risks to G3 offspring associated with (a) the experiences of the two previous generations and (b) the deleterious outcomes observed for these offspring. Thus, risk factors for the G3 sample can fall both directly on their lifelines as well as in the lives of their mother or grandmother prior to their birth. Figures 2 and 3 contain the lifeline plots for the two groups of offspring, offspring born to abused mothers (OA) and offspring born to comparison mothers (OC). Plots were produced for all 135 known offspring; however, as noted above, G3 outcome assessments were not obtained for 12 offspring, and several assessments were conducted only for offspring within a restricted range of development (e.g., cognitive assessments). Those not assessed or assessed with only limited information are identified with (*) symbols in the plots. Results indicated that, on average, the OA sample experienced more risk-factors than the OC sample with age, minority status, gender, and sibling number covaried (OA M = 6.23, SD = 3.14; OC M = 3.88, SD = 2.11; F(1, 129) = 5.89; p < .05).
Figure 2. Third-generation lifelines with transgenerational risk-factors plotted for G3 offspring born to G2 mothers who were sexually abused in childhood (OA).
Note: The average number of risks and the weighted average were both significantly different across the two groups of offspring; those born to abused mothers (OA), and those born to comparison mothers (OC), F(1, 129) = 5.89; p < .05 and F(1, 129) = 8.67; p < .01, respectively. Age, minority status, gender, and sibling number (0–3) were covaried in each analysis. Dep = depression; Vict = victimization; Viol = violence; PTSD = posttraumatic stress disorder; CPS = child protective services. N = 78; average risks = 6.23 (SD = 3.14); weighted average = 9.21 (SD = 4.17).
Figure 3. Third-generation lifelines with transgenerational risk-factors plotted for the comparison group of G3 offspring (OC).
Note: The average number of risks and the weighted average were both significantly different across the two groups of offspring; those born to abused mothers (OA), and those born to comparison mothers (OC) F(1, 129) = 5.89; p < .05 and F(1, 129) = 8.67; p < .01, respectively. Age, minority status, gender, and sibling number (0–3) were covaried in each analysis. Dep = depression; Vict = victimization; Viol = violence; CPS = child protective services; PTSD = posttraumatic stress disorder. N = 57; average risks = 3.88 (SD = 2.11); weighted average = 5.77 (SD = 3.41).
The final analysis was an attempt to place risk factors in developmental context for G3 offspring. For example, it would be logical to assert that domestic violence occurring in the life of a child would be more damaging to a child and have a more lasting impact on that child's future development than domestic violence occurring earlier in the life of the mother before the child was born. To this end, we conducted a weighted analyses where risks that occurred in the lifetime of the G3 offspring, falling on the child's lifeline, were weighted twice (2×) those falling prior to the birth of offspring. Because of substantial crowding of risk factors occurring on or about the time of the birth of G3 offspring, three variables were considered to have fallen on the G3 lifeline although they are depicted just prior each birth and include (a) being born to a teen mother (teen pregnancy), (b) prematurity, and (c) unintendedness. These three variables were assumed to constitute substantial risk to children and were thus weighted 2×. Although selecting a 2× magnitude for all risk factors lying on G3 lifelines is slightly arbitrary, and differential weighting may have been more appropriate for some risks (e.g., the impact of child protective service involvement is likely more deleterious than other risks), we sought to take a parsimonious approach to weighting in the absence of definitive empirical support for a differential weighting scheme. With age, minority status, gender, and sibling number covaried, results of the weighted analysis indicated a significantly higher weighted average for the OA sample (M = 9.21, SD = 4.17) as compared with the OC sample (M = 5.77, SD = 3.41; F(1, 129) = 8.67; p < .01).
Discussion
The likelihood that childhood abuse is transmitted across generations has been a topic of inquiry for decades, but the deleterious effects on offspring because of the various psychological, interpersonal, and physiological sequelae of parents' childhood abuse has been largely overlooked in assessments of the overall impact of child maltreatment. The prospective results presented here demonstrate the inordinate prevalence of various forms of adversity and risk for maldevelopment operating in the lives of offspring born to mothers who experienced childhood sexual abuse. They also provide a snapshot of the cumulative risk to these offspring, the potential for continued victimization and adversity, and a powerful illustration of the amount of burden that children born into adversity are required to bear. By comparing the magnitude of such burden across demographically similar groups of individuals who differ with respect to an objectively determined variable (in this case substantiated maternal childhood sexual abuse), inferences can be made about the extent to which offspring burden is attributable, at least in part, to maternal childhood abuse. This type of descriptive analysis has been utilized in important research regarding how the risk for various maladaptive conditions in adulthood increases in direct proportion to the number of reported adverse childhood experiences (e.g., Anda et al., 2002).
Implications for Public Health
By evaluating the economic and health-related impact of disease, we can begin to discern those opportunities for prevention and intervention with the greatest fiscal benefit to society. A U.S. Department of Justice (1996) report concluded that, aside from murder, child abuse is the most serious crime in terms of monetary and injury consequences with estimated annual costs at approximately $56 billion based on short-term costs associated with property damages and loss, medical care, mental health care, police and fire services, victim services, productivity, and lost wages. These estimates did not include additional expenses incurred when victims begin to consume and utilize services for longer-term physical and psychological sequelae (e.g., Arata & Langhinrichsen-Rohling, 2005). Moreover, these estimates did not include expenses incurred for risk factors directly affecting offspring. For example, estimated annual costs are $3.3 billion for teenage births (Constantine & Nevarez, 2003), $4.3 billion for infant prematurity (St. John, Nelson, Cliver, Bishnoi, & Goldenberg, 2000), and $5.8 billion for domestic violence (CDC, 2003). The cumulative evaluation of these expenditures provides compelling fiscal evidence for the advantages of intervention and prevention programs for victims of childhood maltreatment and their families.
Study Limitations
Several caveats deserve mention. First, this sample of offspring born to women participating in a longitudinal study is a convenience sample and was not randomly obtained from a larger population potentially limiting generaliz-ability. Second, recognizing the difficulty in assessing socioeconomics in young, volatile families and teenage parents, we relied on maternal family-of-origin socioeconomic status as a demographic control and do not purport to have accomplished perfect demographic matching in the G3 sample. Thus, parsing out the impact of childhood abuse as a causal agent in the cumulative risk for offspring is difficult. Furthermore, as these results are not intended to be evaluative of a multivariate system, illuminating the relative importance of any one of these risk factors in determining the well-being of offspring is difficult because many co-occur and/or are comorbid conditions. Several of the null findings presented are somewhat contrary to those reported in other studies. For example, we do not report abused versus comparison differences in childhood depression and adult PTSD in the G2 sample. This contrariness could be a result of the clinical cutoff scores on assessment devices (which were not necessarily diagnostic) not being sensitive enough to capture these differences. Moreover, there may be state-like depression and PTSD symptomatology that were not captured by our assessment schedule because of the slightly arbitrary nature of when the interviews took place. The reality of conducting longitudinal research over a long period necessitates dependence on funding that does not always coincide with optimal timing of follow-up time points. Had assessments been more strategically planned to occur more proximal to significant life events, subsequent traumas, or developmental shifts these results might have been more consistent with the literature.
Finally, although intraclass correlations were taken into account in mean comparisons, siblings are represented in lifeline plots resulting in the replication of G1 and G2 variables across siblings. Concerns about such replication should be somewhat alleviated because the number of siblings did not differ significantly across OA and OC groups and was controlled in mean comparisons. A more pristine analysis might include only one sibling per family, but choosing the most representative sibling may be difficult and somewhat arbitrary. We assert that intergenerational transmission research should include siblings for several reasons: (a) Time varying, dynamic developmental effects would affect some children and not others. (b) The public health impact will ultimately include all offspring of parents who have the tendency to place their children at risk for maldevelopment. (c) Examining the differential impact of risk factors across siblings will inform models of resilience.
Conclusion
Results from this multigenerational study constitute convincing evidence that childhood abuse is a distal risk-factor for later physical, emotional, and psychological problems, and that the sequelae of childhood abuse can become the risks for subsequent violence against women and children. The evidence for the various avenues of intergenerational transmission of the effects of childhood abuse begs the question of whether the majority of resources should be expended on the immediate disease process while ignoring the sequelae of the disease, and whether prevention efforts should extend into (or through) subsequent developmental stages for victims. In general, intervention programs are either primary (targeting general risk-factors to prevent the occurrence of a condition) or secondary (targeting a high-risk or subclinical group to prevent the development of a condition) efforts. There are differential funding priorities and initiatives for each with the majority of large investments having been devoted to primary prevention programs as these are generally thought to affect a greater number of individuals and be more efficacious than secondary efforts in preventing disease. Given the results presented, we assert that intervention programs for child abuse survivors should be characterized as “selective primary prevention efforts” that would likely curtail the large public health burden of the various sequelae of childhood abuse as well as the impact on the next generation who are placed at-risk because of these various sequelae. Such efforts would likely show increased efficacy over primary prevention programs designed for nonabused individuals at lower risk for maldevelopment. Moreover, treatment of childhood abuse should either continue across development or, at the very least, be revisited at various points in development as the salient tasks of particular developmental stages become reminiscent of the original trauma (e.g., becoming sexually active, becoming a parent, protecting children from abusers). Standard pediatrician care-as-usual may need to include inquiries regarding the histories of childhood trauma that may be associated with physical health complaints. With adequate child advocacy support, such inquiries may help improve outcomes for victims and their families.
Acknowledgments
This research was supported by the following federal grants: K01HD41402 (Noll), RO1MH04833 (Trickett/Putnam), ACYF 90CA1686 (Trickett/Noll), and R03HD045346 (Noll). It was also supported in part by generous grants from the W. T. Grant Foundation, the Smith Richardson Foundation, the John Templeton Foundation, and the OhioCanDo4Kids.
References
- Agras WS, Hammer LD, McNicholas F, Kraemer HC. Risk factors for childhood overweight: A prospective study from birth to 9.5 years. Pediatrics. 2004;145:20–25. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- Anda RF, Whitfield CL, Felitti VJ, Chapman D, Edwards VJ, Dube SR, et al. Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatric Services. 2002;53:1001–1009. doi: 10.1176/appi.ps.53.8.1001. [DOI] [PubMed] [Google Scholar]
- Arata C, Langhinrichsen-Rohling J. Single vs. multitype maltreatment: An examination of the long-term effect of child abuse. Journal of Aggression, Maltreatment & Trauma. 2005;11:29–52. [Google Scholar]
- Bayley N. Bayley scales of infant development. 2nd ed. The Psychological Corporation; San Antonio, TX: 1993. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck depression inventory-second edition manual. Harcourt Brace; Psychological Corporation. San Antonio, TX: 1986. [Google Scholar]
- Beitchman JH, Zucker KJ, Hood JE, Dacosta GA, Akman D, Cassavia E. A review of the long-term effects of child sexual abuse. Child Abuse & Neglect. 1992;16:101–118. doi: 10.1016/0145-2134(92)90011-f. [DOI] [PubMed] [Google Scholar]
- Bennett LA, Wolin SJ, Reiss D. Cognitive, behavioral, and emotional problems among school-age children of alcoholic parents. American Journal of Psychiatry. 1988;145:185–190. doi: 10.1176/ajp.145.2.185. [DOI] [PubMed] [Google Scholar]
- Berstein E, Putnam FW. Development, reliability, and validity of a dissociation scale. Journal of Nervous and Mental Disease. 1986;174:727–735. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- Billings AG, Moos RH. Comparisons of children of depressed and nondepressed parents: A social-environmental perspective. Journal of Abnormal Child Psychology. 1983;11(4):463–485. doi: 10.1007/BF00917076. [DOI] [PubMed] [Google Scholar]
- Boney-McCoy S, Finkelhor D. Psychosocial sequelae of violent victimization in a national youth sample. Journal of Consulting and Clinical Psychology. 1995;63(5):726–736. doi: 10.1037//0022-006x.63.5.726. [DOI] [PubMed] [Google Scholar]
- Boyer D, Fine D. Sexual abuse as a factor in adolescent pregnancy and child mal-treatment. Family Planning Perspectives. 1992;24(1):4–11. 19. [PubMed] [Google Scholar]
- Brennan PA, Hammen C, Andersen MJ, Bor W, Najman JM, Williams GM. Chronicity, severity, and timing of maternal depressive symptoms: Relationships with child outcomes at age 5. Developmental Psychology. 2000;36(6):759–766. doi: 10.1037//0012-1649.36.6.759. [DOI] [PubMed] [Google Scholar]
- Briere J, Elliott DM. Prevalence and psychological sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse & Neglect. 2003;27(10):1205–1222. doi: 10.1016/j.chiabu.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Brofenbrenner U. Toward an experimental ecology of human development. American Psychologist. 1977;32:513–531. [Google Scholar]
- Bugental DB. Communication in abusive relationships: Cognitive constructions of interpersonal power. American Behavioral Scientist. 1993;36:288–308. [Google Scholar]
- Capaldi DM, Clark S. Prospecitve family predictors of aggression toward female partners for at risk young men. Developmental Psychology. 1998;34:1175–1188. doi: 10.1037//0012-1649.34.6.1175. [DOI] [PubMed] [Google Scholar]
- CDC . Costs of intimate partner violence in the United States. National Center for Injury Prevention and Control; Atlanta, GA: 2003. [Google Scholar]
- Cicchetti D, Aber LA. Abused children–abusive parents: An overstated case? Harvard Educational Review. 1980;50:244–255. [Google Scholar]
- Coley RL, Chase-Lansdale PL. Adolescent pregnancy and parenthood: Recent evidence and future directions. American Psychologist. 1998;53(2):152–166. doi: 10.1037//0003-066x.53.2.152. [DOI] [PubMed] [Google Scholar]
- Constantine N, Nevarez C. No time for complacency: Teen births in California. Public Health Institute; Sacramento, CA: 2003. [Google Scholar]
- Coohey C, Braun N. Toward an integrated framework for understanding child physical abuse. Child Abuse & Neglect. 1997;21(11):1081–1094. doi: 10.1016/s0145-2134(97)00067-7. [DOI] [PubMed] [Google Scholar]
- Curtis GC. Violence breeds violence–perhaps? American Journal of Psychiatry. 1963;120:386–387. doi: 10.1176/ajp.120.4.386. [DOI] [PubMed] [Google Scholar]
- Davidson JRT, Kudler HS, Smith R. Validity and reliability of the DSM-III criteria for posttraumatic stress disorder. Journal of Nervous and Mental Disorders. 1989;177:336–341. doi: 10.1097/00005053-198906000-00003. [DOI] [PubMed] [Google Scholar]
- DeBellis MD, Broussard ER, Herring DJ, Wexler S, Moritz G, Benitez JG. Psychiatric co-morbidity in caregivers and children involved in maltreatment: A pilot research study with policy implications. Child Abuse & Neglect. 2001;25:923–944. doi: 10.1016/s0145-2134(01)00247-2. [DOI] [PubMed] [Google Scholar]
- Department of Justice . Victim costs and consequences: A new look. National Institute of Justice Research Project: Final summary report, DHHS; Washington, DC: 1996. [Google Scholar]
- DePrince AP, Freyd JJ. Forgetting trauma stimuli. Psychological Science. 2004;15(7):488–492. doi: 10.1111/j.0956-7976.2004.00706.x. [DOI] [PubMed] [Google Scholar]
- DiLillo D, Termblay GC, Peterson L. Linking childhood sexual abuse and abusive parenting: The mediating role of maternal anger. Child Abuse & Neglect. 2000;24:767–779. doi: 10.1016/s0145-2134(00)00138-1. [DOI] [PubMed] [Google Scholar]
- Dixon L, Browne K, Hamilton-Giachritsis C. Risk factors of parents abused as children: A mediational analysis of the intergenerational continuity of child maltreatment. Journal of Child Psychology & Psychiatry. 2005;46(1):47–57. doi: 10.1111/j.1469-7610.2004.00339.x. [DOI] [PubMed] [Google Scholar]
- Dixon L, Hamilton-Giachritsis C, Browne K. Attributions and behaviors of parents abused as children: a mediational analysis of the intergenerational continuity of child maltreatment (Part II) Journal of Child Psychology and Psychiatry. 2005;46(1):58–68. doi: 10.1111/j.1469-7610.2004.00340.x. [DOI] [PubMed] [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108(1):50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Dunn LM, Dunn LM. Peabody picture vocabulary test–revised. American Guidance Service; Circle Pines, MN: 1981. [Google Scholar]
- Egeland B, Jacobvitz D, Papatola K. Intergenerational continuity of child abuse, in child abuse and neglect. In: Lancaster J, Gelles R, editors. Biosocial dimensions. Aldine De Gruyter; New York: 1987. [Google Scholar]
- Egeland B, Jacobvitz DB, Sroufe A. Breaking the cycle of abuse. Child Development. 1988;59:1080–1088. doi: 10.1111/j.1467-8624.1988.tb03260.x. [DOI] [PubMed] [Google Scholar]
- Ehrensaft MK, Cohen P, Brown J, Smailes E, Chen H, Johnson JG. Intergenerational transmission of partner violence: A 20 year prospective study. Journal of Consulting and Clinical Psychology. 2003;71:741–753. doi: 10.1037/0022-006x.71.4.741. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Leonard KE, Birchler GR. The occurrence of male-to-female intimate partner violence on days of men's drinking: The moderating effects of antisocial personality disorder. Journal of Consulting and Clinical Psychology. 2005;73(2):239–248. doi: 10.1037/0022-006X.73.2.239. [DOI] [PubMed] [Google Scholar]
- Felitti VJ. Long-term medical consequences of incest, rape, and molestation. Southern Medical Journal. 1991;84(3):328–331. doi: 10.1097/00007611-199103000-00008. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Williams JBW. Structured clinical interview for DSM-IV (SCID-I) (user's guide and interview) research version. New York Psychiatric Institute; Biometrics Research Department. New York: 1995. [Google Scholar]
- Francis LA, Birch LL. Maternal influences on daughters' restrained eating behavior. Health Psychology. 2005;24:548–554. doi: 10.1037/0278-6133.24.6.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furstenberg FF, Jr., Brooks-Gunn J, Morgan SP. Adolescent mothers and their children in later life. Cambridge University Press; New York: 1987. [PubMed] [Google Scholar]
- Garbarino J. A preliminary study of some ecological correlates of child abuse: The impact of socioeconomic stress on mothers. Child Development. 1976;47:178–185. [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Brody M, Toth C, Burke-Martindale CH, Rothschild BS. Childhood maltreatment in extremely obese male and female bariatric surgery candidates. Obesity Research. 2005;13(1):123–130. doi: 10.1038/oby.2005.16. [DOI] [PubMed] [Google Scholar]
- Hardy JB, Sharpiro S, Astone NM, Miller TL, Brooks-Gunn J, Hilton SC. Adolescent childbearing revisited: The age of inner-city mothers at delivery is a determinant of their children's self-sufficiency at age 27 to 33. Pediatrics. 2006;100:802–809. doi: 10.1542/peds.100.5.802. [DOI] [PubMed] [Google Scholar]
- Hollingshead AF. Four factor index of social status. Department of Sociology, Yale University; New Haven, CT: 1975. [Google Scholar]
- Jaffee S, Caspi A, Moffitt TE, Belsky J, Silva P. Why are children born to teen mothers at risk for adverse outcomes in young adulthood? Results from a 20-year longitudinal study. Development and Psychopathology. 2001;13(2):377–397. doi: 10.1017/s0954579401002103. [DOI] [PubMed] [Google Scholar]
- Jones JC, Barlow DH. The etiology of post-traumatic stress disorder. Clinical Psychology Review. 1990;10:299–328. [Google Scholar]
- Karlovic D, Solter V, Krizo K, Potkonjak J. Alcohol dependence in soldiers with posttraumatic stress disorder or posttraumatic stress disorder comorbid with major depressive disorder. Alcoholism: Journal on Alcoholism and Related Addictions. 2004;40:3–15. [Google Scholar]
- Kaufman J, Zigler E. Do abused children become abusive parents? American Journal of Orthopsychiatry. 1987;57(2):186–192. doi: 10.1111/j.1939-0025.1987.tb03528.x. [DOI] [PubMed] [Google Scholar]
- Kempe R, Kempe C. Child abuse. Harvard University Press; Cambridge, MA: 1978. [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68(1):19–30. doi: 10.1037//0022-006x.68.1.19. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Rating scales to assess depression in school-aged children. Acta Paedopsychiatrica. 1981;46:305–315. [PubMed] [Google Scholar]
- Levin JA, Pollack H, Comfort ME. Academic and behavioral outcomes among the children of young mothers. Journal of Marriage and Family. 2001;63(2):355–369. [Google Scholar]
- Lovejoy MC, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20(5):561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Majzoub JA, McGregor JA, Lockwood CJ, Smith R, Taggart MS, Schulkin J. A central theory of preterm and term labor: Putative role for corticotropin-releasing hormone. American Journal of Obstetrics and Gynecology. 1999;180(1):S232–241. doi: 10.1016/s0002-9378(99)70707-6. [DOI] [PubMed] [Google Scholar]
- Margolin G. The reciprocal relationship between marital and child problems. In: Vincent JP, editor. Advances in family intervention, assessment and theory: An annual compilation of research. Vol. 2. Greenwich, CT: 1981. pp. 131–182. [Google Scholar]
- Maynard RA. The study, the context, and the findings in brief. In: Maynard R, editor. Kids having kids: Economic costs and social consequences of teen pregnancy. Urban Institute Press; Washington, DC: 1997. pp. 1–21. [Google Scholar]
- McCloskey LA, Bailey JA. The intergenerational transmission of risk for child sexual abuse. Journal of Interpersonal Violence. 2000;15:1019–1035. [Google Scholar]
- Menacker F, Martin JA, MacDorman MF, Ventura SJ. Births to 10–14 year-old mothers, 1990–2002: Trends and health outcomes. National vital statistics reports: From the Centers for Disease Control and Prevention. National Center for Health Statistics, National Vital Statistics System. 2004;53(7):1–18. [PubMed] [Google Scholar]
- Moore KA, Myers DE, Morrison DR, Nord CW, Brown B, Edmonston B. Age at first childbirth and later poverty. Journal of Research on Adolescence. 1993;3:393–422. doi: 10.1207/s15327795jra0304_5. [DOI] [PubMed] [Google Scholar]
- National Center on Child Abuse and Neglect . NIS-2: Second study of national incidence and prevalence of child abuse and neglect. National Center of Child Abuse and Neglect; U.S. DHHS; Washington, DC: 1988. [Google Scholar]
- Neumann DA, Houskamp BM, Pollock VE, Briere J. The long-term sequalae of chilhood sexual abuse in women: A meta-analytic review. Child Maltreatment: Journal of the American Professional Society on the Abuse of Children. 1996;1:6–16. [Google Scholar]
- Noll JG, Horowitz LA, Bonanno GA, Trickett PK, Putnam FW. Revictimization and self-harm in females who experienced childhood sexual abuse: Results from a prospective study. Journal of Interpersonal Violence. 2003;18(12):1452–1471. doi: 10.1177/0886260503258035. [DOI] [PubMed] [Google Scholar]
- Noll JG, Trickett PK, Putnam FW. A prospective investigation of the impact of childhood sexual abuse on the development of sexuality. Journal of Consulting and Clinical Psychology. 2003;71(3):575–586. doi: 10.1037/0022-006x.71.3.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pete-McGadney J. Differences in adolescent self-concept as a function of race, geographic location, and pregnancy. Adolescence. 1995;30(117):95–105. [PubMed] [Google Scholar]
- Putnam FW. Traumatic stress and pathological dissociation. Annals of the New York Academy of Sciences, Vol. 771, Stress: Basic mechanisms and clinical implications. 1996:708–716. doi: 10.1111/j.1749-6632.1995.tb44722.x. [DOI] [PubMed] [Google Scholar]
- Roosa MW. The relationship of childhood sexual abuse to teenage pregnancy. Journal of Marriage and Family. 1997;59(1):119–130. [Google Scholar]
- Rosenheim MK. Early parenthood and coming of age in the 1990s. Rutgers University Press; New Brunswick, NJ: 1992. [Google Scholar]
- Slattery MM, Morrison JJ. Preterm delivery. Lancet. 2002;360(9344):1489–1497. doi: 10.1016/S0140-6736(02)11476-0. [DOI] [PubMed] [Google Scholar]
- Spieker SJ, Larson NC, Lewis SM, Keller TE, Gilchrist L. Developmental trajectories of disruptive behavior problems in preschool children of adolescent mothers. Child Development. 1999;70:443–458. doi: 10.1111/1467-8624.00032. [DOI] [PubMed] [Google Scholar]
- St. John EB, Nelson KG, Cliver SP, Bishnoi RR, Goldenberg RL. Costs of neonatal care according to gestational age at birth and survival status. American Journal of Obstetrics and Gynecology. 2000;182(1):170–175. doi: 10.1016/s0002-9378(00)70509-6. [DOI] [PubMed] [Google Scholar]
- Stevens-Simon C, Kaplan DW, McAnarney ER. Factors associated with preterm delivery among pregnant adolescents. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 1993;14(4):340–342. doi: 10.1016/1054-139x(93)90185-r. [DOI] [PubMed] [Google Scholar]
- Teti DM, Gelfand DM, Messinger DS, Isabella R. Maternal depression and the quality of early attachment: An examination of infants, preschoolers, and their mothers. Developmental Psychology. 1995;31:364–376. [Google Scholar]
- Trickett PK, Noll JG, Reiffman A, Putnam FW. Variants of intrafamilial sexual abuse experience: Implications for short- and long-term development. Development & Psychopathology. 2001;13(4):1001–1019. [PubMed] [Google Scholar]
- Van Der Leder ME, Raskin VD. Psychological sequelae of childhood sexual abuse: Relevant in subsequent pregnancy. American Journal of Obstetrics and Gynecology. 1993;168(4):1336–1337. doi: 10.1016/0002-9378(93)90401-4. [DOI] [PubMed] [Google Scholar]
- Wadhwa PD, Sandman CA, Porto M, Dunkel-Schetter C, Garite TJ. The association between prenatal stress and infant birth weight and gestational age at birth: A prospective investigation. American Journal of Obstetrics and Gynocology. 1993;169:858–865. doi: 10.1016/0002-9378(93)90016-c. [DOI] [PubMed] [Google Scholar]
- Wallace JM, Aitken RP, Milne JS, Hay WW., Jr. Nutritionally mediated placental growth restriction in the growing adolescent: Consequences for the fetus. Biology of Reproduction. 2004;71(4):1055–1062. doi: 10.1095/biolreprod.104.030965. [DOI] [PubMed] [Google Scholar]
- Weissman MM, John K, Merikangas KR, Prusoff BA, Wickramaratne P, Gammon GD, et al. Depressed parents and their children. American Journal of Diseases of Childhood. 1986;140(8):801–805. doi: 10.1001/archpedi.1986.02140220083038. [DOI] [PubMed] [Google Scholar]
- Zabin LS, Wong R, Weinick RM, Emerson MR. Dependency in urban black families following the birth of an adolescent's child. Journal of Marriage and Family. 1992;54(3):496–507. [Google Scholar]
- Zeller MH, Modi AC. Predictors of health-related quality of life in obese youth. Obesity Research. 2006;14:122–130. doi: 10.1038/oby.2006.15. [DOI] [PubMed] [Google Scholar]
- Zuravin S, McMillen C, DePanfilis D, Risley-Curtiss C. The intergenerational cycle of child maltreatment: Continuity versus discontinuity. Journal of Interpersonal Violence. 1996;11(3):315–334. [Google Scholar]