Abstract
The Attention Deficit Hyperactivity Disorder (ADHD) symptom presentation of young adolescents with ADHD was examined in association with the transition to middle school. The current study used data collected in the Multimodal Treatment Study of ADHD which included children between 7–9 years of age with a diagnosis of ADHD (n=258) and grade and sex matched controls (n=112). The trajectory of ADHD symptoms before, during and after the transition to middle school was modeled using hierarchical linear modeling. A clear developmental reduction in ADHD symptomatology was observed for all three ADHD symptom domains. For young adolescents with ADHD, the transition to middle school was associated with a disruption in the developmental decline of inattention, hyperactivity and impulsivity symptoms as measured by parent ratings. This effect was also observed for teacher ratings of inattention and hyperactivity. These results support the assertion that the environmental changes associated with transitioning to middle school coincide with a transient reversal in ADHD symptom decline among children with ADHD.
Keywords: ADHD, Middle School, Transition, Adolescents, MTA
Attention Deficit Hyperactivity Disorder (ADHD) is now understood as a chronic disorder that persists throughout childhood and into adolescence and adulthood. Prevalence rates among grade-schoolers are approximately 3%–7% (American Psychiatric Association, 2000) with about 65 to 80% of those children continuing to meet diagnostic criteria into adolescence (Barkley, Fischer, Edelbrock, & Smallish, 1990; Biederman et al., 1996; Hart, Lahey, Loeber, Applegate, & Frick, 1995). As children enter adolescence, the presentation of ADHD symptoms appears to change. Most studies suggest that hyperactive/impulsive symptoms decline during adolescence, whereas symptoms of inattention remain relatively constant (Fischer, Barkley, Fletcher, & Smallish, 1993; Hart et al. 1995). Others have documented decreases in both hyperactive/impulsive symptoms and inattentive symptoms with increased chronological age (Biederman, Mick & Faraone, 2000). It is worth noting that despite the consistent finding that hyperactive/impulsive symptoms decline with age, these symptoms do not normalize (Barkley et al., 1990; Biederman et al., 1998).
This downward trend in ADHD symptom expression is generally attributed to biological changes related to maturation, such as brain development (Willoughby, 2003). However, the child’s environment can significantly affect these biologically-based developmental trends. For example, changing the structure or demands of the environment can alter the way a child with ADHD behaves in that environment (DuPaul & Stoner, 2003). Indeed, much of the behavior modification literature is based on the assertion that the symptoms and behaviors associated with ADHD can be treated by altering the child’s environment (Pelham, Wheeler & Chronis, 1998). For example, manipulating the antecedents and consequences of a behavior in a classroom setting can result in an associated increase or decrease in symptoms (DuPaul & Eckert, 1997).
Just as structuring and simplifying the environment produces behavioral improvement, changing the environment to a less structured or more complex form may produce exacerbations in ADHD symptomatology. A naturally occurring and clinically relevant alteration of a child’s environment is the transition from elementary to middle school. The transition to middle school is associated with numerous environmental changes (Evans, Langberg, Raggi, Allen & Buvinger, 2005; Evans, Serpell & White, 2005) including the move to multiple classes and teachers, increased academic demands during the school day and after school, and the amplified importance of peer relationships (Evans, Allen, Moore, & Strauss, 2005). In middle school, cognitive demands are increased and students are required to function with more independence at school and at home (DuPaul & Stoner, 2003).
Given the increased environmental and contextual demands in middle school, this transition can be a particularly difficult period of time for some students. Significant decreases in Grade Point Average (GPA) and confidence in academic abilities have been documented with the transition to middle school in children without ADHD (Alspaugh & Harting, 1995; Gutman & Midgley, 2000; Midgley & Urdan, 1992). With the increased demand for independent functioning, higher levels of organization, and management of deadlines, behaviors such as procrastination can become particularly problematic (DuPaul & Stoner, 2003). This transition period has the potential to alter the developmental course of ADHD symptoms.
Although clinical lore and several researchers have conceptualized the transition to middle school as exacerbating the symptom presentation of ADHD (Thompson, Morgan & Urquhart, 2003; Robin, 1998), no empirical evidence is available to support this assertion. The purpose of the present study is to examine the manifestation of symptoms of ADHD, as rated by parents and teachers, before, during, and after the transition to middle school. We predicted that the negative downward trend in ADHD symptomatology would be disrupted during the transition year.
Method
Participants
Participants were from the multisite Multimodal Treatment Study of Children with ADHD (MTA). Children (n = 579) were between 7–9 years of age (grades 1–4) and had a diagnosis of ADHD, Combined Type at MTA study entry. Diagnosis was determined using the Diagnostic Interview Schedule for Children, Parent Report (DISC-P 4.0; Shaffer et. al., 2000), supplemented with up to two symptoms from the teacher SNAP-IV (Swanson, 1992) for cases falling just below the DISC diagnostic threshold. Once a diagnosis was confirmed, children were randomly assigned to one of four treatment groups: Medication Only (MedMgt), Psychosocial Treatment Only (Beh), Combined Treatment (Comb), or Community Comparison (CC).
Children in the MTA study were assessed at baseline and 14-, 24-, 36-months, and 6 years post-baseline using a comprehensive assessment battery. The 258 MTA participants who transitioned to middle school at or before the 36-month timepoint are examined in this paper. Children who transitioned after the 36-month timepoint were not included in these analyses because of the extended 3-year gap between the 36-month and 6-year assessment timepoints. The 258 participants who transitioned to middle school at or before the 36-month assessment timepoint had a mean age of 8.83, SD = .83 at baseline. These participants were re-assessed at completion of the 14-month treatment phase, Mage 9.96 (SD = .81) years, at 24-months post-randomization, Mage 10.84 (SD = .83) years, at 36-months post-randomization Mage 12.24 (SD = .80) years, and at 6 years post-randomization Mage 15.36 (SD = .87) years. Participant retention rate was 97% at 14-months; 93% at 24-months; 84% at 36-months; and 75% at 6 years. Co-occurring oppositional defiant disorder (42%), conduct disorder (14%), anxiety disorders (46%), and affective disorders (5%) were diagnosed in this sample at baseline with the DISC-P. Sixty-two percent of the sample was Caucasian, 23% was African-American, 6% was Hispanic and 9% was mixed decent or other ethnicity. Seventy-seven percent were male and 23% were female.
A nonclinical comparison group for the present study was derived from the Local Normative Comparison Group (LNCG) recruited at the time of the 24-month MTA assessment. LNCG children were living in the same communities and attending the same schools as the MTA children. These children (n = 289 across the MTA sites) were identified from school registries to match the MTA sample in terms of grade and sex and then randomly chosen from among those parents who volunteered to participate. LNCG children were assessed at 24-months, 36-months, and 6-years (retention rate at 6 years = 97%) using a similar battery of measures as those used with the ADHD sample. Thirty-one of the LNCG subjects met ADHD diagnostic criteria at baseline using the same DISC-P and SNAP-IV criteria as specified for the MTA study participants. These 31 children were excluded from this study’s sample to avoid confounding the LNCG group with the MTA group (final LNCG n = 258). In order to capture the transition to middle school and ensure comparability with the reduced MTA sample described above, only LNCG participants who transitioned at or prior to the 36-month assessment point were utilized in our analyses (n = 112). The LNCG group at baseline was 83% male and the racial/ethnic composition of the LNCG sample was 69% Caucasian, 9% African-American, 15% Hispanic, and 7% Other. The proportions of males and non-Caucasian participants across the ADHD and LNCG groups were not statistically different (all ps >.05).
Children and their parents provided informed assent and consent respectively during their first clinic visit. This included consent for the collection of rating scales reported in this study. The MTA study was approved by Institutional Review Boards at each of the participating institutions. A more complete description of the assessment battery, interventions, and follow-up procedures and assessment battery are described elsewhere (Hinshaw et al, 1997; MTA Cooperative Group, 1999; Jensen et al., 2007).
Measures
SNAP-IV (Swanson, 1992)
The SNAP-IV has 39 items, which are derived from DSM criteria for ADHD and Oppositional Defiant Disorder (ODD). The items on this scale are reproduced directly from DSM-IV and DSM-III symptoms for ADHD and ODD, and include 18 ADHD items from DSM-IV (9 DSM inattention and 9 DSM hyperactive/impulsive symptoms). Parents and teachers respond on a 4-point Likert scale rating the severity of symptoms in the past four weeks (i.e., 0 = not at all, 1 = just a little, 2 = pretty much, and 3 = very much). The scale yields ADHD-related factor scores on Inattention, Hyperactivity, and Impulsivity. Each factor score is derived by summing the items for each symptom domain and dividing by the number of items on each factor (Inattention = 9 items; Hyperactivity = 6 items; Impulsivity = 3 items). Normative data for the SNAP are provided by Gaub and Carlson (1997) and Swanson (1992). Although psychometric properties have not been investigated for the SNAP-IV, adequate reliability and validity has been established for similar DSM-IV checklists. On other DSM-IV checklists, excellent internal consistency, Cronbach’s alpha >.90, and high correlations with other instruments of established validity and reliability, r = .79 (Wolraich et al., 2003) have been documented. To remain consistent with literature examining the trajectory of ADHD symptoms with increased age (e.g., Biederman, Mick & Faraone, 2000), symptoms of hyperactivity and impulsivity were examined separately even though they are often grouped together diagnostically.
The SNAP-IV was completed by parents and teachers at each of the assessment points. MTA assessments occurred over the course of the academic year due to the logistical need to space each site’s numerous assessments over the course of a 9-month assessment period. Efforts were made to collect parent and teacher ratings concordantly. Seventy-one percent of teacher ratings and 67% of parent ratings were completed during the first academic semester (September – December) and 29% of teacher and 33% of parent ratings during the second academic semester (January – June). T-tests comparing ratings collected in the first academic semester to those collected in the second academic semester revealed no differences related to the timing of assessments; all ps >.05.
For children in elementary school, only one set of teacher ratings was collected, primarily from homeroom teachers. Children in middle school had up to three sets of teacher ratings. In order to equate ratings during middle school with ratings conducted in elementary school, a composite teacher rating was calculated by averaging each participant’s teacher ratings.
Services Use in Children and Adolescents-Parent Interview (SCA-PI); Service Barriers and Attitudes (Jensen et al., 2004)
This structured interview administered to parents captured child and adolescent services use across mental health, primary care, school, and community settings. It was obtained every 6 months, either by phone or during the face-to-face assessments. Medication use was queried at each time point. For this study, the percent of days in the interval between the last assessment and the current assessment that any stimulant medication was taken was used as an indicator of ADHD medication usage. Test-retest reliability using an 18 day between test interval for reporting medication use on the SCAPI is excellent, kappa = .97 (Hoagwood et al., 2004).
Determination of transition year
While the MTA study included comprehensive assessments of children’s symptomatology through a critical developmental period, assessments were not planned to reflect functioning in association with the middle school transition. Neither the assessment schedule, nor the data collection forms were focused on assessing difficulty with transition to middle school. Hence the year of transition to middle school was not recorded. Determination of the transition year was made according to the following decision algorithm. First, all children in grades 1–4 at the time of assessment were assumed to be in elementary school. Similarly, children in the 7th grade were assumed to be in middle school. For children whose data were collected in the fifth or sixth grades, the name of the school and the number of teachers completing rating scales were used to determine if the child was still in elementary school or had transitioned to middle school. For most cases, the name of the school listed by the teacher on top of the rating scale clearly labeled the school as an elementary or middle school (e.g., Johnson Middle School). For cases where this was not clear, we examined the number of teachers who rated the child. In the MTA study, rating scales were collected from one teacher when students were in elementary school and multiple teachers (i.e., Language Arts, Math, and Social Studies teachers) following the transition to middle school. Therefore, children in the fifth or sixth grade who had more than one set of teacher ratings were classified as having made the transition to middle school.
Statistical Analyses
Hierarchical linear modeling (HLM) was used to analyze the data. HLM models were derived separately according to rater (i.e., parent or teacher) and according to each of the three core ADHD symptom domains (i.e., Inattention, Hyperactivity, and Impulsivity). In all, six HLM analyses (2 raters by 3 domains) were conducted (e.g., parent ratings of inattention symptomatology).
Developing the Basic Model
The first step was to develop a basic model for each rater/symptom combination. The initial model was a simple unconditional mean model (i.e., intercept term only). A linear age term was then added to model developmental trajectory of ADHD symptomatology. The age term was entered first as a fixed effect. The new model was evaluated by testing the difference in fit between the new (intercept + linear fixed age) and previous model (intercept only) using −2 log likelihood (−2LL) ratios. Each model was fitted using a full maximum likelihood function. After entering linear age as a fixed effect in the basic model, a linear age random effect term was tested by adding this new variable to the model in a sequential manner, followed by a fixed quadratic age term, and finally a random quadratic age term. Variables were retained if the −2LL ratio was significant (p>.05) and dropped if non-significant. To better illustrate this process, an example of basic model selection is illustrated in Table 1.
Table 1.
Example of the Basic Model Building and Selection using Parent Ratings of Inattention (Variance Component Model)
| Level 1 models | Level 2 models | (−2LL) | Diff | Change | df | p-value | |||
|---|---|---|---|---|---|---|---|---|---|
| (1): |
|
|
7402.8 | ||||||
| (2): |
|
|
7359.0 | (1–2) | 43.8 | 1 | 0.0000 | ||
| (3): |
|
|
7358.3 | (2–3) | 0.7 | 1 | 0.4028 | ||
| (4): |
|
|
7317.8 | (4–2) | 41.2 | 1 | 0.0000 | ||
| (5): |
|
|
7315.6 | (5–4) | 2.2 | 1 | 0.1380 | ||
Note. (1) = Unconditional mean model; (2) = (1) + fixed age; (3) = (2) + random effect for age; (4) = (2) + fixed age2; (5) = (4) + random effect for age2, A = age.
Expanding the Model
Once the basic model for each variable was derived using the procedure outlined above, selected covariates which could potentially affect ADHD symptom trajectories were systematically added to the model. Namely, treatment group, stimulant usage, and their interactions with other terms in the model were added. Stimulant usage was added as a first level, time-varying covariate while treatment group was added as a second level, time-invariant covariate. Treatment group was entered simultaneously as three dummy variables contrasting the CC group to each of the three active MTA treatment conditions (Comb, Med, Beh). Note that the effects of MTA treatment on ADHD symptom reduction over time are unlikely to map onto the MTA results reported in the literature (Jensen et al., 2007) since patients’ age instead of MTA assessment timepoint (baseline, 14-, 24-, 36-month, and 6-year) were used to indicate time.
In building this expanded model, a similar approach as the basic model selection process was used. Each variable was entered first as a fixed effect first then as a random effect. Also, variables were entered in a sequential manner and retained in the model only if the −2LL was significant (p<.05). Note that variables added later in the entry sequence could potentially cause a variable entered prior to become statistically non-significant. In these cases, we compared the relative contribution of the two terms by looking at the −2LL values generated with and without the inclusion of these variables respectively. We then selected the variable that produced the highest change in −2LL values and retained that variable in the final model (e.g., see age2 term in Appendix). Note that some variables were not significant in the final models but were retained in the model because of interaction effects with other variables.
The appropriate variance covariance structures were also examined during model testing by implementing three different variance structures (i.e., auto-regressive, variance component, and unstructured) and examining the Bayesian Informational Criterion (BIC) values. The variance structure that produced the smallest BIC value for the model was selected. In some circumstances the inclusion of a random effect term produced a boundary problem (i.e., a negative variance) regardless of the variance structure used. In these circumstances, as suggested by Singer and Willet (2003), we dropped the random part and treated the variable as fixed. Note that this model selection process allowed final models across dependent measures and raters to vary in the number of variables, random or fixed nature of the variables, and variance structures. An example of the complete modeling process is provided as an Appendix.
The last variables inserted into the expanded model were variables indicating the transition to middle-school year and another indicating the post-transition slope. The transition year variable was created by recoding the grade variable to equal 0 for assessments that occurred during elementary school and 1 for middle school assessments. A significant transition to middle school term would indicate that the trajectory of ADHD symptomatology over time is affected by the transition to middle school.
To indicate the slope after transitioning to middle school, a variable was created by coding this variable as 0 for all the elementary school years including the transition year. Post-transition years were coded as the difference in age at the two subsequent time points. This formulation ensures that the slope variable and age move in lockstep. For example, using this approach a one unit change in the primary linear predictor age will parallel a one unit change in the post transition slope. A significant effect for this slope variable would indicate that the symptom trajectory slope after the transition to middle school year differs from the symptom trajectory slope prior to the transition to middle school.
A similar modeling process was used to develop statistical models for the LNCG group. The primary difference was that treatment group and stimulant usage were not included in these models because they were not applicable to the LNCG participants. Because the LNCG models differed from the MTA models in the exclusion of these variables and also because the two sets of participants had different numbers of observations (i.e., the LNCG participants lacked baseline and 14-month data), the LNCG and MTA models were not contrasted statistically.
Results
The final statistical models for the three ADHD symptom domains are presented in Table 2 (parent ratings) and Table 3 (teacher ratings). The primary purpose of this paper is to examine the impact of the transition to middle school on the developmental trajectory of ADHD symptoms. Accordingly, the variables of interest are time (age or age2), the transition year, and the post-transition slope.
Table 2.
Results from Hierarchical Linear Models Predicting Parent Ratings of Inattention, Hyperactivity and Impulsivity Symptoms over Time and Through the Transition to Middle School
| Variables | Inattention Estimate (se) | Hyperactivity Estimate (se) | Impulsivity Estimate (se) |
|---|---|---|---|
| Intercept | 22.30 (1.03)*** | 15.27 (0.69)*** | 8.12 (0.38)*** |
| Age | −1.68 (0.21)*** | −1.75 (0.14)*** | −1.05 (0.14)*** |
| Age2 | ------------ | ------------ | 0.03 (0.01)* |
| Stimulant usage | −2.50 (0.86)** | −0.70 (0.56)** | −0.76 (0.17)*** |
| Treatment group | |||
| Comb | −0.83 (1.02) | −0.21 (0.70) | ------------ |
| MedMgt | −0.51 (1.02) | −0.75 (0.70) | ------------ |
| Beh | −1.90 (1.00) | −1.11 (0.68) | ------------ |
| CC | 0 | 0 | ------------ |
| Stimulant × treatment | * | ** | |
| Med × Comb | −1.45 (1.13) | −1.73 (0.74)* | ------------ |
| Med × MedMgt | −1.51 (1.12) | −1.48 (0.73)* | ------------ |
| Med × Beh | 1.84 (1.66) | 0.72 (0.90) | ------------ |
| Med × CC | 0 | 0 | ------------ |
| Transition year × treatment | * | ||
| Transition × Comb | ------------ | 1.26 (0.53)* | ------------ |
| Transition × MedMgt | ------------ | 0.80 (0.53) | ------------ |
| Transition × Beh | ------------ | −0.07 (0.57) | ------------ |
| Transition × CC | ------------ | 0 | ------------ |
| Transition year | 3.35 (0.57)*** | 1.75 (0.50)*** | 1.26 (0.21)*** |
| Post transition slope | 1.59 (0.28)*** | 1.50 (0.18)*** | 0.45 (0.14)** |
Note.
p<.05;
p<.01;
p<.001;
Comb = Combined Treatment, MedMgt = Medication Management Only, Beh = Behavioral Only, CC = Community Comparison, Random effects are italicized.
Table 3.
Results from Hierarchical Linear Models Predicting Teacher Ratings of Inattention, Hyperactivity and Impulsivity Symptoms over Time and Through the Transition to Middle School
| Variables | Inattention Estimate (se) | Hyperactivity Estimate (se) | Impulsivity Estimate (se) |
|---|---|---|---|
| Intercept | 21.29 (1.16)*** | 13.53 (1.61)*** | 7.12 (0.90)*** |
| Age | −1.09 (0.21)*** | −1.14 (0.58) | −0.52 (0.33) |
| Age2 | ------------ | 0.01 (0.04) | −0.01 (0.02) |
| Stimulant Usage | −3.94 (1.05)*** | −3.10 (0.72)*** | −1.36 (0.41)*** |
| Treatment group | * | * | |
| Comb | −2.54 (1.58) | −0.79 (2.18) | −0.47 (1.22) |
| MedMgt | −0.29 (1.60) | 2.38 (2.26) | 0.49 (1.27) |
| Beh | −0.08 (1.62) | 5.69 (2.25)* | 2.90 (1.26)* |
| CC | 0 | 0 | 0 |
| Stimulant × treatment | ** | *** | ** |
| Med × Comb | −1.61 (1.48) | −1.59 (1.02) | −0.62 (0.57) |
| Med × MedMgt | −2.79 (1.47)* | −2.06 (1.04)* | −0.87 (0.58) |
| Med × Beh | 4.17 (1.86)* | 3.53 (1.24)** | 1.56 (0.70)* |
| Med × CC | 0 | 0 | 0 |
| Age × treatment | * | ** | * |
| Age × Comb | 0.59 (0.25)* | −0.00 (0.81) | −0.10 (0.45) |
| Age × MedMgt | 0.42 (0.25) | −0.65 (0.83) | −0.20 (0.46) |
| Age × Beh | −0.07 (0.27) | −2.44 (0.82)** | −1.32 (0.45)** |
| Age × CC | 0 | 0 | 0 |
| Age2 × treatment | * | * | |
| Age2 × Comb | ------------ | 0.04 (0.06) | 0.03 (0.04) |
| Age2 × Med Mgt | ------------ | 0.07 (0.06) | 0.03 (0.04) |
| Age2 × Beh | ------------ | 0.19 (0.06)** | 0.11 (0.04)** |
| Age2 × CC | ------------ | 0 | 0 |
| Transition year | 1.38 (0.68)* | 0.88 (0.45)* | 0.20 (0.25) |
| Post transition slope | ------------ | ------------ | ------------ |
Note.
p<.05;
p<.01;
p<.001;
Comb = Combined Treatment, MedMgt = Medication Management Only, Beh = Behavioral Only, CC = Community Comparison, Random effects are italicized.
Time (age)
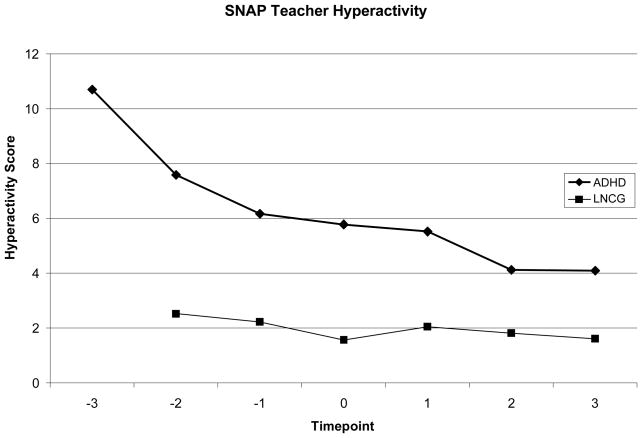
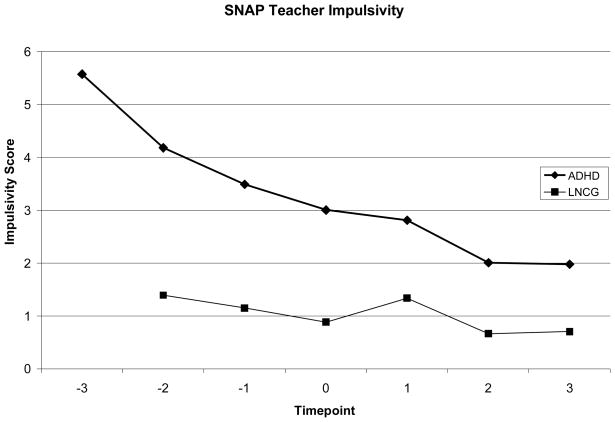
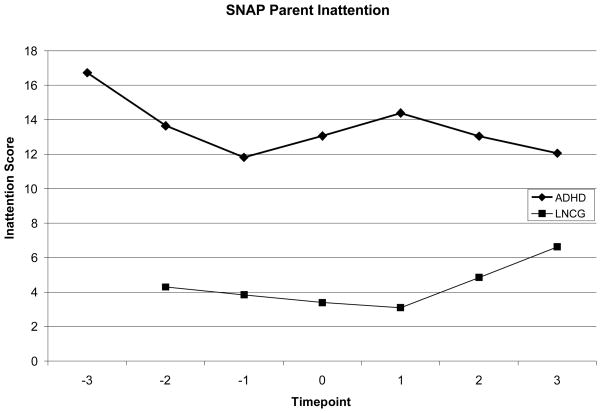
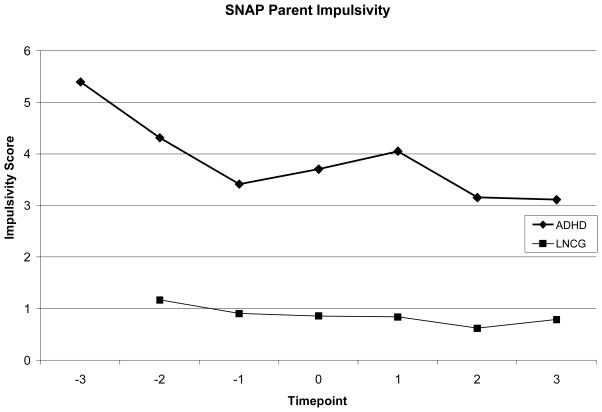
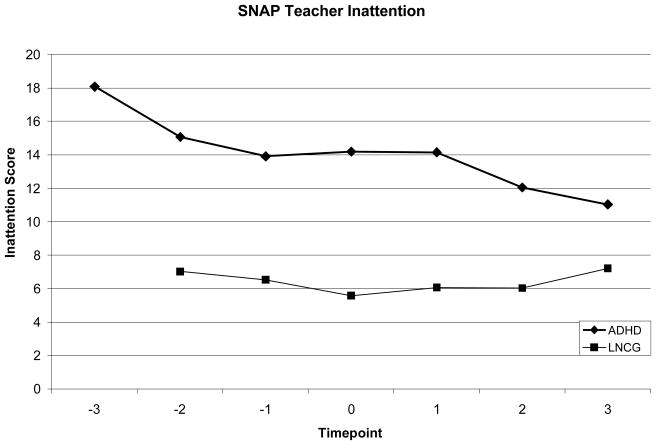
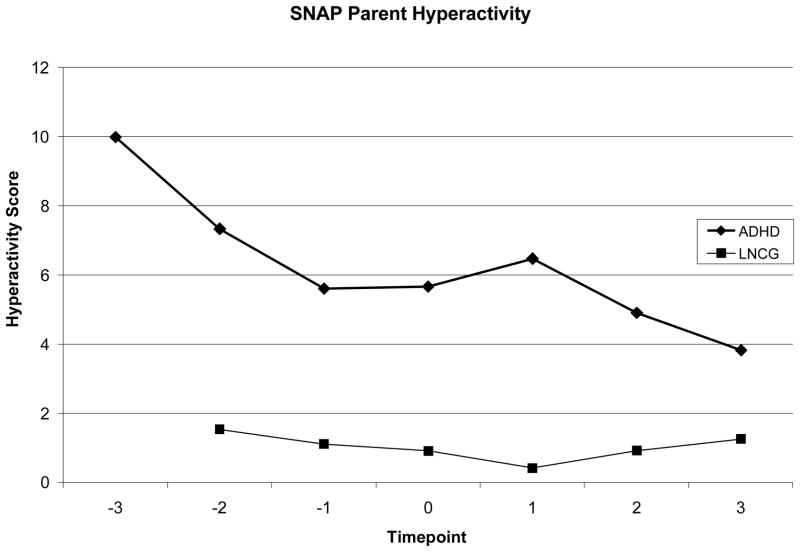
The age variable was significant and retained in all parent models (p<.001) and in the model of teacher rated inattention (p<.001). In all cases the coefficient was negative indicating that ADHD symptoms declined with increased chronological age. Although the age variable alone was not significant in the final models for teacher rated symptoms of hyperactivity and impulsivity, the coefficients in these models were negative (see Figures 5 & 6). The quadratic age term alone (age2) was only significant for parent-rated symptoms of impulsivity (p<.05) suggesting that there is an exponential attenuation in impulsivity symptoms at younger ages that plateaus with development.
Figure 5.
Teacher rated symptoms of hyperactivity on the SNAP Rating Scale. In order to equate the transition year across participants, the x-axis represents grade with the transition year coded as time 0 and consecutive negative integers for the preceding elementary school years (e.g., −2, −1) and positive integers for the post-ceding middle school years (e.g., 1, 2). The LNCG does not have a timepoint −3 because participants were not recruited until the 24 month MTA timepoint.
Figure 6.
Teacher rated symptoms of impulsivity on the SNAP Rating Scale where time-point 0 represents the transition to middle school. In order to equate the transition year across participants, the x-axis represents grade with the transition year coded as time 0 and consecutive negative integers for the preceding elementary school years (e.g., −2, −1) and positive integers for the post-ceding middle school years (e.g., 1, 2). The LNCG does not have a timepoint −3 because participants were not recruited until the 24 month MTA timepoint.
Transition Year
After accounting for age, stimulant usage, treatment group, and their interactions, the transition to middle school produced a statistically significant effect and was retained in all models except for teacher ratings of impulsivity. According to parent ratings, the transition to middle school was associated with an elevation in symptoms or disruption in their decline that would not have been predicted based on the rest of the variables in the model (see Figures 1–3). For teacher ratings, the declining developmental trajectory of inattention and hyperactivity flattened during the transition year (see Figures 4 & 5). Specifically, these symptoms did not continue to decline at the rate predicted by the other variables in the model.
Figure 1.
Parent rated symptoms of inattention on the SNAP Rating Scale where timepoint 0 represents the transition to middle school. In order to equate the transition year across participants, the x-axis represents grade with the transition year coded as time 0 and consecutive negative integers for the preceding elementary school years (e.g., −2, −1) and positive integers for the post-ceding middle school years (e.g., 1, 2). The LNCG does not have a timepoint −3 because participants were not recruited until the 24 month MTA timepoint.
Figure 3.
Parent rated symptoms of impulsivity on the SNAP Rating Scale where time-point 0 represents the transition to middle school. In order to equate the transition year across participants, the x-axis represents grade with the transition year coded as time 0 and consecutive negative integers for the preceding elementary school years (e.g., −2, −1) and positive integers for the post-ceding middle school years (e.g., 1, 2). The LNCG does not have a timepoint −3 because participants were not recruited until the 24 month MTA timepoint.
Figure 4.
Teacher rated symptoms of inattention on the SNAP Rating Scale where timepoint 0 represents the transition to middle school. In order to equate the transition year across participants, the x-axis represents grade with the transition year coded as time 0 and consecutive negative integers for the preceding elementary school years (e.g., −2, −1) and positive integers for the post-ceding middle school years (e.g., 1, 2). The LNCG does not have a timepoint −3 because participants were not recruited until the 24 month MTA timepoint.
Post-Transition Slope
The post-transition slope coefficient measures change in the rate of symptom decline after the middle school transition year. This variable was significant for parent ratings of inattention (p<.001), hyperactivity (p<.001) and impulsivity (p<.01). For example, for parent ratings of inattention, before the transition to middle school, the slope was −1.68. After transition to middle school the trajectory has a slope that is the sum of both the linear age and the post transition slope coefficient (−1.68 + 1.59 = −0.09) indicating that the rapid rate of decrease in inattention symptoms seen prior to the middle transition was attenuated following the transition (see Figure 1). The post-transition slope variable was not significant for any of the teacher rated symptom domains. This finding suggests that while teacher rated symptoms of inattention and hyperactivity were disrupted by the transition year, they resumed the predicted rate of decline post transition.
Magnitude of Transition Effects
To examine the magnitude of the transition effect on ADHD symptom trajectories, Cohen’s d effect sizes were calculated (Cohen, 1992). The predicted post-transition mean score was calculated based upon the data modeled with and without the transition variable. The predicted mean with the transition variable was subtracted from the predicted mean without the transition variable. This mean difference was divided by the pooled SD of predicted scores (see Table 5). For parent ratings, the transition to middle school had a small effect on symptoms of Inattention (d = .22), Hyperactivity (d = .24), and Impulsivity (d = .25). For teacher ratings, the transition had a small effect on Inattention (d = .20) Hyperactivity (d = .14) and a negligible effect on Impulsivity (d = .06).
Table 5.
Effect Size Calculations for SNAP Parent and Teacher Ratings of Inattention, Hyperactivity, and Impulsivity Symptoms (Total Scores) at the Transition to Middle School for ADHD Sample
| Symptom | Predicted Mean Transition | Predicted Mean No Transition | Predicted SD Transition | Predicted SD No Transition | ES |
|---|---|---|---|---|---|
| Parent Ratings | |||||
| Inattention | 13.07 | 12.20 | 4.16 | 3.87 | .22 |
| Hyperactivity | 5.67 | 5.08 | 2.67 | 2.53 | .24 |
| Impulsivity | 3.71 | 3.32 | 1.60 | 1.55 | .25 |
|
| |||||
| Teacher Ratings | |||||
| Inattention | 14.20 | 13.58 | 3.18 | 3.13 | .20 |
| Hyperactivity | 5.79 | 5.46 | 2.38 | 2.35 | .14 |
| Impulsivity | 3.01 | 2.93 | 1.35 | 1.34 | .06 |
Note. ES = Effect Size, SD = Standard Deviation, Pooled SD used to calculate ES; Pooled SD = average of SD Transition and SD No Transition.
Nonclinical Comparison sample
For the LNCG models, age was negatively correlated with ADHD symptomatology in all analyses (p<.05) except for the analysis examining teacher-rated inattentive symptoms (p = .10). The transition to middle school variable was not related to the developmental progression of ADHD symptomatology for any ADHD symptom domain or rater (all ps >.05). Likewise, the post transition slope variable was not significant for any ADHD symptom domain or rater (all ps >.05). The developmental progression of ADHD symptomatology among the comparison group is demonstrated on Figures 1–6.
Discussion
The results of this study support previous research asserting that for children diagnosed with ADHD, symptoms of inattention, hyperactivity and impulsivity decrease with chronological age (Biederman et al., 2000; Fischer, Barkley, Fletcher, & Smallish, 1993; Hart, Lahey, Loeber, Applegate & Frick, 1995). Moreover, this study demonstrates that the transition to middle school is associated with an interruption of this decline in ADHD symptomatology. Regardless of the set of predictors included in our statistical models, a variable indicating the transition to middle school was statistically significant and suggested a disruption in the negative decline in ADHD symptomatology for all domain and rater combinations except for teacher ratings of impulsivity. This finding was unique to children with ADHD as a nonclinical comparison group did not display these trends.
Our analyses provide empirical evidence to support the assertion that the environmental changes associated with transitioning to middle school influences the manifestation of ADHD symptoms among children with ADHD. Interestingly, while the present study supports the hypothesis that the transition is a difficult event for children with ADHD, we found that children without ADHD did not experience significant difficulty with the transition. Thus, the transition appears to disrupt the decline in symptoms of inattention, hyperactivity and impulsivity only for children who exhibited significant levels of ADHD symptoms before the transition.
Both the developmental decline in symptoms of ADHD and the interruption in that decline associated with the transition to middle school were evident even after accounting for MTA treatment and stimulant medication usage. As expected, the use of stimulant medications was associated with decreased ADHD symptomatology across all domains. Based on our findings reported in the 36-month follow-up papers for the MTA (Jensen et al., 2007; Swanson et al., 2007), this association is most likely reflecting the strong effect of medication treatment during the active 14-month treatment phase of the study. We did not find that medication use, either study-managed or subsequently self-selected, prevented the interruption in ADHD symptom decline witnessed during the transition year. While medication improves ADHD symptomatology (MTA Cooperative Group, 1999), medications are unlikely to improve study skills, organizational skills, and time management abilities that are critical to success in middle school. Without these skills, it appears that the developmental decline in ADHD symptoms is disrupted irrespective of whether the child is being treated pharmacologically.
It is noteworthy that the disruption in ADHD symptom decline associated with the transition year and the long-term impact of this disruption (i.e., post transition slope) were more marked as measured by parent ratings (see Figures 1 – 6). According to parent ratings, symptoms of ADHD declined at a statistically slower rate following the transition as compared to the pre-transition decline. This trend was not found for teacher ratings of ADHD symptomatology. It is possible that the impact of the transition to middle school is more evident in the home environment. Specifically, the larger disruption in parent rated symptoms may be a function of increased conflict with parents as children move into middle school, including arguments about homework and autonomy. It is also possible that lower reliability of the teacher ratings may have contributed to these differences. That is, all participants were rated by a different teacher at each time point, whereas the same parent completed ratings at each time point. Having different teachers rate the child each year likely increased the within-child variability of the teacher ratings relative to parent ratings because non-specific factors such as response bias, personal perceptions, class composition, etc. varied each year for teacher ratings but likely remained much more stable for parent ratings. Moreover, individual teachers are likely to have much less knowledge of specific children after the transition, given the increased number of classes accompanying the middle school years. In addition, the stability of parent ratings likely benefit from the fact that they have knowledge about past functioning whereas teachers do not. Indeed, variances for teacher ratings at each assessment point were higher for teachers than for parents.
The scope of this paper was limited to the impact of the transition on symptoms of ADHD because other measures of functioning were not examined. Although it is well documented that a wide variety of functional impairments are associated with ADHD in adolescence (Barkley et al., 1990), it is not clear what triggers these impairments. Determining if the transition to middle school leads to increased functional impairment is important, given the severe nature of impairment difficulties in adolescence (i.e., teen pregnancy, substance abuse, car accidents, and school dropout). Research that includes functional outcomes is particularly relevant because decreased academic confidence and Grade Point Average (GPA) have previously been documented with the transition to middle school in children without ADHD (Alspaugh & Harting, 1995; Gutman & Midgley, 2000; Midgley & Urdan, 1992). Moreover, we recently reported higher rates of delinquency and substance experimentation among the MTA children compared to the LNCG at the 36-month follow-up (Molina et al., 2007). Thus, there are signs of the expected emergence of these more serious behaviors that should, theoretically, be affected by unsuccessful transitions to secondary education.
Another limitation is that ratings were completed throughout the school year. Specifically, approximately half of the sample was assessed during the first academic semester of school, while the other half was rated during the second academic semester. These assessment timepoints varied within patients across assessments. Differences in rating scale collection have the potential to influence the results as behavior has been shown to vary from month to month over the course of a school year, irrespective of treatment (Evans, Langberg et al., 2005). Limited research has been conducted on the month to month natural changes in ADHD symptomatology during the course of a year. One report on a small sample showed that teacher ratings of hyperactivity/impulsivity displayed a significant seasonal effect on a placebo condition such that fall ratings of hyperactivity/impulsivity started higher and showed more decline compared to spring ratings (Yao et al., 2005).
Implications for Research, Policy, and Practice
These findings may have implications for longitudinal research. The seminal longitudinal studies of children with ADHD completed follow-up assessments years after the initial baseline assessment (e.g., 8 years; Barkley et al., 1990). With these large gaps between assessments it is likely that clinically relevant changes in symptoms and/or functioning are missed. This point is highlighted by the fact that even using the MTA sample where assessments were completed yearly for the first three years, a disruption such as the transition to middle school was not readily apparent. For example, if we examined the MTA data at baseline, 36-months and 6-years post-baseline, we would likely conclude that symptoms of ADHD decline in a linear fashion with increased age. It is possible that other significant events (e.g., transitioning to college, parents divorcing, and changing schools) are also associated with disruptions in ADHD symptomatology. Future research evaluating how the course of ADHD symptomatology is influenced by significant developmental events may serve to guide targeted intervention research.
These findings also highlight the need for interventions implemented prior to and during the transition to middle school. Investigators have suggested that changes in class size, number of teachers, increased demands for independence and greater workloads make the transition to middle school a difficult event for children with ADHD (Evans, Serpell & White, 2005; Thompson, Morgan & Urquhart, 2003; Robin, 1998). There are numerous academic changes in middle school, including increased expectations related to organization of materials, independent completion of classwork and homework, and the development of study and note taking skills (Evans, Serpell & White, 2005). An intervention that prepares children with ADHD and their parents for these environmental changes and provides them with the tools necessary to effectively navigate the middle school environment could be particularly beneficial. For example, prior to transitioning, families could receive training in developing and managing an organizational system for academic materials. This could include establishing a specific plan for recording homework and tests in an assignment notebook and for planning out long-term assignments. It is likely that by preparing families, the negative effects of the transition can be minimized, placing children with ADHD on a better developmental trajectory. School-based interventions that specifically target middle school students at-risk for failure and with ADHD have been tested and appear promising (Evans, Langberg et al., 2005; Langberg et al., 2006; Molina et al., in press). However, to our knowledge there is no published research testing the effectiveness of interventions implemented between elementary and middle school.
Figure 2.
Parent rated symptoms of hyperactivity on the SNAP Rating Scale. In order to equate the transition year across participants, the x-axis represents grade with the transition year coded as time 0 and consecutive negative integers for the preceding elementary school years (e.g., −2, −1) and positive integers for the post-ceding middle school years (e.g., 1, 2). The LNCG does not have a timepoint −3 because participants were not recruited until the 24 month MTA timepoint.
Table 4.
ADHD Raw Score Means and SD for SNAP Parent and Teacher Ratings of Inattention, Hyperactivity, and Impulsivity Symptoms (Total Scores) over Time
| Time Point | N | Inattention Mean | Inattention SD | Hyper Mean | Hyper SD | Impulsivity Mean | Impulsivity SD |
|---|---|---|---|---|---|---|---|
| Parent Ratings | |||||||
| −3 | 202 | 18.12 | 5.98 | 10.97 | 3.92 | 5.94 | 2.25 |
| −2 | 245 | 12.42 | 6.80 | 6.40 | 4.44 | 3.89 | 2.43 |
| −1 | 245 | 11.91 | 6.14 | 5.72 | 4.25 | 3.42 | 2.43 |
| 0 | 245 | 13.27 | 6.64 | 5.77 | 4.36 | 3.76 | 2.38 |
| 1 | 43 | 12.83 | 5.76 | 5.26 | 4.11 | 3.60 | 2.57 |
| 2 | 185 | 13.22 | 6.52 | 5.07 | 3.92 | 3.18 | 2.22 |
| 3 | 40 | 12.52 | 6.54 | 3.89 | 3.49 | 3.22 | 2.61 |
|
| |||||||
| Teacher Ratings | |||||||
| −3 | 202 | 19.70 | 5.61 | 11.9 | 4.31 | 6.25 | 2.53 |
| −2 | 245 | 13.40 | 8.13 | 6.53 | 5.16 | 3.63 | 2.86 |
| −1 | 245 | 14.50 | 7.95 | 6.29 | 4.69 | 3.52 | 2.68 |
| 0 | 245 | 14.40 | 6.94 | 5.89 | 4.44 | 3.06 | 2.49 |
| 1 | 43 | 12.90 | 6.70 | 4.39 | 4.17 | 2.18 | 2.16 |
| 2 | 185 | 12.20 | 5.98 | 4.18 | 4.21 | 2.06 | 2.28 |
| 3 | 40 | 11.80 | 6.79 | 4.90 | 4.52 | 2.29 | 2.40 |
Note. Time point 0 designates the transition to middle school, Negative numbers are the elementary school years leading to middle school, Positive numbers are the years following the transition year; Hyper = Hyperactivity.
Appendix
Table 1.
Example of Model Building and Selection: Inattention Symptoms Rated by Parents (Variance Component Model)
| Level 1 Models | Level 2 Models | (−2LL) | Diff | Change | df | p-value | |||
|---|---|---|---|---|---|---|---|---|---|
| (1): |
|
|
7402.8 | ||||||
| (2): |
|
|
7359.0 | (1–2) | 43.8 | 1 | 0.0000 | ||
| (3): |
|
|
7358.3 | (2–3) | 0.7 | 1 | 0.4028 | ||
| (4): |
|
|
7317.8 | (4–2) | 41.2 | 1 | 0.0000 | ||
| (5): |
|
|
7315.6 | (5–4) | 2.2 | 1 | 0.1380 | ||
|
| |||||||||
| (6): |
|
|
7256.5 | (4–6) | 61.3 | 1 | 0.0000 | ||
| (7): |
|
|
7255.3 | (6–7) | 1.2 | 1 | 0.2733 | ||
|
| |||||||||
| (8): |
|
|
7236.3 | (6–8) | 20.2 | 12 | 0.0634 | ||
| (9): |
|
|
7212.9 | (8–9) | 23.4 | 4 | 0.0000 | ||
| (10): |
|
|
7206.6 | (9–10) | 6.3 | 1 | 0.012 | ||
| (11): |
|
|
7170.7 | (10–11) | 35.9 | 4 | 0.000 | ||
| (12): |
|
|
7163.5 | (11–12) | 7.2 | 1 | 0.007 | ||
| (13): |
|
|
7183.1 | (14–15) | 19.6 | 13 | 0.1056 | ||
Note. (1) = Unconditional mean; (2) = Linear age (fixed); (3) = Linear age (random); (4) = Quadratic age (Fixed); (5) = Quadratic age (random); (6) = (4) + med use (Fixed); (7) = (6)+ med use (random); (8) = (6)+ treatment group; (9) = (8)+ transition (fixed); (10) = (9) + transition (random); (11) = 10 + post transition (fixed); (12) = 11 + post transition (random); (13) = final model after dropping quadratic age and non significant interaction terms. A = Age, M = Medication Use, TG = Treatment Group, T = Transition Year, PT = Post Transition Slope.
Footnotes
The Multimodal Treatment Study of Children with ADHD (MTA) was a National Institute of Mental health (NIMH) cooperative agreement randomized clinical trial, and then continued under an NIMH contract as a follow-up study. Collaborators from the National Institute of Mental Health: Benedetto Vitiello, M.D. (Child & Adolescent Treatment and Preventive Interventions Research Branch), Joanne B. Severe, M.S. (Clinical Trials Operations and Biostatistics Unit, Division of Services and Intervention Research), Peter S. Jensen, M.D. (currently at Columbia University), L. Eugene Arnold, M.D., M.Ed. (currently at Ohio State University), Kimberly Hoagwood, Ph.D. (currently at Columbia); previous contributors from NIMH to the early phases: John Richters, Ph.D. (currently at National Institute of Nursing Research); Donald Vereen, M.D. (currently at National Institute on Drug Abuse). Principal investigators and co-investigators from the sites are: University of California, Berkeley/San Francisco: Stephen P. Hinshaw, Ph.D. (Berkeley), Glen R. Elliott, M.D., Ph.D. (San Francisco); Duke University: Karen C. Wells, Ph.D., Jeffery Epstein, Ph.D.; previous Duke contributors to early phases: C. Keith Conners, Ph.D. (former PI); John March, M.D., M.P.H.; University of California, Irvine: James Swanson, Ph.D., Timothy Wigal, Ph.D.; previous contributor from UCLA to the early phases: Dennis P. Cantwell, M.D. (deceased); Long Island Jewish Medical Center/New York University: Howard B. Abikoff, Ph.D.; Montreal Children’s Hospital/McGill University: Lily Hechtman, M.D.; New York State Psychiatric Institute/Columbia University/Mount Sinai Medical Center: Laurence L. Greenhill, M.D. (Columbia), Jeffrey H. Newcorn, M.D. (Mount Sinai School of Medicine). University of Pittsburgh: Brooke Molina, Ph.D., Betsy Hoza, Ph.D. (currently at Purdue University), William E. Pelham, Ph.D. (PI for early phases, currently at State University of New York, Buffalo). Follow-up phase statistical collaborators: Robert D. Gibbons, Ph.D. (University of Illinois, Chicago); Sue Marcus, Ph.D (Mt. Sinai College of Medicine) Kwan Hur, Ph.D. (University of Illinois, Chicago). Original study statistical and design consultant: Helena C. Kraemer, Ph.D. (Stanford University). Collaborator from the Office of Special Education Programs/US Department of Education: Thomas Hanley, Ed.D. Collaborator from Office of Juvenile Justice and Delinquency Prevention/Department of Justice: Karen Stern, Ph.D.
Contributor Information
Joshua M. Langberg, Department of Pediatrics University of Cincinnati College of Medicine, Cincinnati Children’s Hospital Medical Center
Jeffery N. Epstein, Department of Pediatrics University of Cincinnati College of Medicine, Cincinnati Children’s Hospital Medical Center
Mekibib Altaye, Department of Pediatrics University of Cincinnati College of Medicine, Cincinnati Children’s Hospital Medical Center.
Brooke S.G. Molina, Departments of Psychology and Psychiatry, University of Pittsburgh
L. Eugene Arnold, Department of Psychiatry, Ohio State University.
Benedetto Vitiello, National Institute of Mental Health.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. (DSM-IV) [Google Scholar]
- Alspaugh JW, Harting RD. Transition effects of school grade-level organization on student achievement. Journal of Research and Development in Education. 1995;28(3):145–149. [Google Scholar]
- Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29:546–557. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Milberger S, Curtis S, Chen L, Marrs A, Ouellette C, Moore P, Spencer T. Predictors of persistence and remission of ADHD: Results from a four-year prospective follow-up study of ADHD children. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:343–351. doi: 10.1097/00004583-199603000-00016. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Taylor A, Sienna M, Williamson S, Fine C. Diagnostic continuity between child and adolescent ADHD: Findings from a longitudinal clinical sample. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37(3):305–313. doi: 10.1097/00004583-199803000-00016. [DOI] [PubMed] [Google Scholar]
- Biederman J, Mick E, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: impact of remission definition and symptom type. American Journal of Psychiatry. 2000;157:816–818. doi: 10.1176/appi.ajp.157.5.816. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- DuPaul GJ, Eckert TL. The effects of school-based interventions for Attention Deficit Hyperactivity Disorder: A meta-analysis. School Psychology Review. 1997;26(1):5–27. [Google Scholar]
- DuPaul GJ, Stoner G. ADHD in the schools: Assessment and intervention strategies. 2. New York, NY: Guildford Press; 2003. [Google Scholar]
- Evans SW, Allen J, Moore S, Strauss V. Measuring symptoms and functioning of youth with ADHD in middle schools. Journal of Abnormal Child Psychology. 2005;33(6):695–706. doi: 10.1007/s10802-005-7648-0. [DOI] [PubMed] [Google Scholar]
- Evans SW, Langberg JM, Raggi V, Allen J, Buvinger E. Evaluation of a school-based treatment program for middle school youth with ADHD. Journal of Attention Disorders. 2005;9:343–353. doi: 10.1177/1087054705279305. [DOI] [PubMed] [Google Scholar]
- Evans SW, Serpell Z, White C. The transition to middle school: Preparing for challenge and success. Attention! (CHADD) 2005 June;:29–31. [Google Scholar]
- Fischer M, Barkley RA, Fletcher KE, Smallish L. The stability of dimensions of behavior in adhd and normal children over an 8-year follow-up. Journal of Abnormal Child Psychology. 1993;21(3):315–337. doi: 10.1007/BF00917537. [DOI] [PubMed] [Google Scholar]
- Gaub M, Carlson C. Behavioral characteristics of DSM-IV ADHD subtypes in a school-based population. Journal of Abnormal Child Psychology. 1997;25:103–111. doi: 10.1023/a:1025775311259. [DOI] [PubMed] [Google Scholar]
- Gutman LM, Midgley C. The role of protective factors in supporting the academic achievement of poor African American students during the middle school transition. Journal of Youth and Adolescence. 2000;29(2):223–248. [Google Scholar]
- Hart E, Lahey B, Loeber R, Applegate B, Frick P. Developmental change in attention-deficit hyperactivity disorder in boys: a four-year longitudinal study. Journal of Abnormal Child Psychology. 1995;23:729–749. doi: 10.1007/BF01447474. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, March JS, Abikoff H, Arnold LE, Cantwell DP, Conners CK, et al. Comprehensive assessment of childhood attention-deficit hyperactivity disorder in the context of a multisite, multimodal clinical trial. Journal of Attention Disorders. 1997;1(4):217–234. [Google Scholar]
- Hoagwood KE, Jensen PS, Arnold LE, Roper M, Severe J, Odbert C, Molina BS MTA Cooperative Group. Reliability of the services for children and adolescents-parent interview. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(11):1345–54. doi: 10.1097/01.chi.0000139558.54948.1f. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Hoagwood KE, Roper M, Arnold LE, Odbert C, Crowe M, Molina BS, Hechtman L, Hinshaw SP, Hoze B, Newcorn J, Swanson J, Wells K. The services for children and adolescents-parent interview: Development and performance characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(11):1334–1344. doi: 10.1097/01.chi.0000139557.16830.4e. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Swanson J, Arnold LE, Vitiello B, Abikoff HB, et al. MTA Findings at 36 Months Paper 1: Three-Year Follow-up of the NIMH MTA Study. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(8):989–1002. doi: 10.1097/CHI.0b013e3180686d48. [DOI] [PubMed] [Google Scholar]
- Langberg JM, Smith BH, Bogle KE, Schmidt JD, Cole W, Pender C. A pilot evaluation of small group challenging horizons program (CHP): A randomized trial. Journal of Applied School Psychology. 2006;23(1):31–58. [Google Scholar]
- Midgley C, Urdan T. The transition to middle level schools: Making it a good experience for all students. Middle School Journal. 1992;24:5–14. [Google Scholar]
- Molina BSG, Flory K, Bukstein OG, Greiner AR, Baker JL, Krug VM, Evans SW. Feasibility and preliminary efficacy of an after school program for middle schoolers with ADHD: A randomized trial in a large public middle school. Journal of Attention Disorders. doi: 10.1177/1087054707311666. (in press) [DOI] [PubMed] [Google Scholar]
- Molina BSG, Flory K, Hinshaw SP, Greiner AR, Arnold E, Swanson J, Hechtman L, Jensen PS, Vitiello B, Hoza B, Pelham WE, Elliott GR, Wells KC, Abikoff HB, Gibbons RD, Marcus S, Epstein J, Greenhill LL, Newcorn JH, Severe JB, Wigal T. Delinquent behavior and emerging substance use in the MTA at 36-months: Prevalence, course, and treatment effects. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(8):1028–1040. doi: 10.1097/chi.0b013e3180686d96. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Smith BH, Pelham WE. Factor structure and criterion validity of secondary school teacher ratings of ADHD and ODD. Journal of Abnormal Child Psychology. 2001;29:71–82. doi: 10.1023/a:1005203629968. [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group. A 14-month randomized clinical trial of treatment of attention deficit hyperactivity disorder (ADHD) Archives of General Psychiatry. 1999;56:1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Wheeler T, Chronis A. Empirically supported psychosocial treatments for attention deficit hyperactivity disorder. Journal of Clinical Child Psychology. 1998;27(2):190–205. doi: 10.1207/s15374424jccp2702_6. [DOI] [PubMed] [Google Scholar]
- Robin AL. ADHD in Adolescents. New York: The Guilford Press; 1998. [Google Scholar]
- Shaffer D, Fischer P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Swanson JM. School Based Assessments and Interventions for ADD Students. Irvine, CA: K.C.; 1992. [Google Scholar]
- Swanson JM, Hinshaw SP, Arnold LE, Gibbons R, Marcus S, Hur K, Jensen PS, Vitiello B, Abikoff H, Greenhill LL, Hechtman L, Pelham W, Wells K, Conners CK, Elliott G, Epstein JN, Hoagwood K, Hoza B, Molina B, Newcorn JH, Severe J, Odbert C, Wigal T the MTA Cooperative Group . Secondary evaluations of MTA 36-month outcomes: Propensity score and growth mixture model analyses. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(8):1003–1014. doi: 10.1097/CHI.0b013e3180686d63. [DOI] [PubMed] [Google Scholar]
- Thompson AE, Morgan C, Urquhart I. Children with ADHD transferring to secondary schools: Potential difficulties and solutions. Clinical Child Psychology and Psychiatry. 2003;8(1):91–103. [Google Scholar]
- Willoughby M. Developmental course of ADHD symptomatology during the transition from childhood to adolescence: A review with recommendations. Journal of Child Psychology and Psychiatry. 2003;44(1):88–106. doi: 10.1111/1469-7610.t01-1-00104. [DOI] [PubMed] [Google Scholar]
- Wolraich ML, Feurer ID, Hannah JN, Baumgaertel A, Pinnock TY. Obtaining systematic teacher reports of disruptive behavior disorders utilizing DSM-IV. Journal of Abnormal Child Psychology. 1998;26:141–152. doi: 10.1023/a:1022673906401. [DOI] [PubMed] [Google Scholar]
- Wolraich ML, Lambert W, Doffing MA, Bickman L, Simmons T, Worley K. Psychometric properties of the Vanderbilt ADHD Diagnostic Parent Rating Scale in a referred population. Journal of Pediatric Psychology. 2003;28(8):559–568. doi: 10.1093/jpepsy/jsg046. [DOI] [PubMed] [Google Scholar]
- Yao MJ, Arnold LE, Witwer A, Hollway J, Hall K. Placebo Effect in ADHD Parent and Teacher Ratings. Poster at 52nd Annual Meeting American Academy of Child and Adolescent Psychiatry; October 18–23, 2005; Toronto. [Google Scholar]