Abstract
Background
To identify sources of race/ethnic differences related to post-traumatic stress disorder (PTSD), we compared trauma exposure, risk for PTSD among those exposed to trauma, and treatment-seeking among Whites, Blacks, Hispanics and Asians in the US general population.
Method
Data from structured diagnostic interviews with 34 653 adult respondents to the 2004–2005 wave of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) were analysed.
Results
The lifetime prevalence of PTSD was highest among Blacks (8.7%), intermediate among Hispanics and Whites (7.0% and 7.4%) and lowest among Asians (4.0%). Differences in risk for trauma varied by type of event. Whites were more likely than the other groups to have any trauma, to learn of a trauma to someone close, and to learn of an unexpected death, but Blacks and Hispanics had higher risk of child maltreatment, chiefly witnessing domestic violence, and Asians, Black men, and Hispanic women had higher risk of war-related events than Whites. Among those exposed to trauma, PTSD risk was slightly higher among Blacks [adjusted odds ratio (aOR) 1.22] and lower among Asians (aOR 0.67) compared with Whites, after adjustment for characteristics of trauma exposure. All minority groups were less likely to seek treatment for PTSD than Whites (aOR range: 0.39–0.61), and fewer than half of minorities with PTSD sought treatment (range: 32.7–42.0%).
Conclusions
When PTSD affects US race/ethnic minorities, it is usually untreated. Large disparities in treatment indicate a need for investment in accessible and culturally sensitive treatment options.
Keywords: Ethnic groups, post-traumatic stress disorder, race, traumatic events, treatment-seeking
Introduction
Post-traumatic stress disorder (PTSD) develops in response to exposure to a traumatic event during which an individual feels extremely fearful, horrified or helpless. The diagnosis is characterized by persistent re-experiencing of the event, persistent avoidance of stimuli associated with the event, emotional numbing and hyper-arousal (APA, 1994). The public health consequences of PTSD are substantial, and include suicide (Kessler, 2000), secondary mental disorders, substance dependence (Breslau, 2002; Breslau et al. 2003), impaired role functioning, health problems (Farley & Patsalides, 2001; Simpson, 2002; Zayfert et al. 2002; Acierno et al. 2007; Kubzansky et al. 2007, 2009; Koenen et al. 2008) and reduced life course opportunities, such as unemployment and marital instability (Kessler, 2000). Identifying race/ethnic differences in PTSD and their origins is necessary to target public health interventions aimed at preventing the development of PTSD and improving its course. This paper examines race/ethnic disparities in PTSD in the general population of the USA.
PTSD is unique among psychiatric disorders, in that exposure to a traumatic event is a diagnostic criterion. Race/ethnic differences in risk for PTSD can therefore arise from two sources: (1) differences in exposure to a qualifying traumatic event and (2) differences in the risk for developing PTSD among those who are exposed to trauma. Epidemiologic studies have shown that trauma exposure varies by demographic characteristics including race (Bromet et al. 1998; Breslau, 2002). Factors that lead to trauma exposure may be different from those that increase vulnerability to the effects of that exposure.
It is unknown whether in the general US population racial and ethnic differences exist in lifetime prevalence of PTSD, exposure to traumatic events, development of PTSD among exposed individuals, or treatment-seeking among people with PTSD. Two national studies of the prevalence of PTSD report conflicting results regarding racial differences. Breslau et al. (2006a) found no statistically significant difference in PTSD between Blacks or Hispanics and Whites, but Himle et al. (2009) found Blacks had higher lifetime prevalence of PTSD than Whites. These studies did not decompose risk of PTSD by exposure to potentially traumatic events or the subsequent development of PTSD once exposed, however.
Studies of race/ethnic differences in exposure to potentially traumatic events are limited by their data collection from a specific geographic area or by their focus on a limited number of event types. Furthermore, reviews of this literature highlight its inconclusive results (Kilpatrick & Acierno, 2003; Hatch & Dohrenwend, 2007). Race/ethnic differences in type of event exposure, particularly elevated rates of exposure to violence, may account for possible differences in PTSD by race/ethnicity, because type of event exposure is an important determinant of PTSD. Furthermore, few studies examine race/ethnic differences in other characteristics of event exposure which increase risk of developing PTSD, such as exposure to multiple events or younger age at exposure (Kessler et al. 1995; Breslau et al. 1998, 1999, 2004a; Bromet et al. 1998).
Existing studies of the conditional risk of developing PTSD once exposed to a traumatic event are limited in their generalizability by their focus on specific geographic regions, specific types of event exposures, and use of clinic-based samples. Moreover, a review of the literature emphasized discrepant findings among studies (Kilpatrick & Acierno, 2003). Two studies of specific localities found no difference in Whites and Blacks in their conditional risk of PTSD (Breslau et al. 1991; Norris, 1992), while studies of hospital and clinic samples have found elevated rates of PTSD following event exposure in minorities (Santos et al. 2008).
Several studies on race/ethnic differences in treatment- seeking following trauma exposure have found that Whites are more likely to seek treatment than minorities, but these studies include treatment-seeking for depression and anxiety as well as PTSD, and each focuses on only one type of trauma exposure (e.g. sexual assault, community violence) (Ullman & Brecklin, 2002; Boscarino et al. 2004; Jaycox et al. 2004; Gavrilovic et al. 2005; Lewis et al. 2005). One study using a national clinic-based sample found that non-Whites were less likely to seek treatment for PTSD than Whites but did not look specifically at different minority groups (Koenen et al. 2003).
This study aims to address these gaps using data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a large national sample which includes information on a comprehensive set of traumatic events, including war-related events, violent victimization, and accidents and illnesses. First, we examined race/ethnic differences in lifetime prevalence of PTSD. Next, we decomposed risk of PTSD into : (1) risk of exposure to potentially traumatic events, and (2) risk of developing PTSD once exposed to an event. To do so, we first examined race/ethnic differences in exposure to 22 potentially traumatic events. We then examined race/ethnic differences in development of PTSD among people exposed to potentially traumatic events (i.e. the ‘conditional risk ’ of PTSD). Finally, we looked at race/ethnic differences in mental health treatment-seeking among individuals with PTSD.
Method
Data
We used data from wave 2 (n=34 653) of the NESARC conducted in 2004–2005. The NESARC, established in 2001, entailed a multi-stage sampling design that yielded a representative sample of the civilian, non-institutionalized population aged 18 years and older residing in the USA (81% response rate) (Grant & Kaplan, 2005; Ruan et al. 2008). The current study uses data from the wave 2 follow-up interview (response rate, 86.7%; cumulative response, 70.2%) (Ruan et al. 2008), conducted approximately 3 years after the original survey, which assessed potentially traumatic events and PTSD.
Measures
Traumatic events, PTSD and treatment-seeking
The National Institute on Alcohol Abuse and Alcoholism Alcohol Use Disorder and Associated Disabilities Interview Schedule DSM-IV version (Grant et al. 2001) was administered to assess lifetime experience of traumatic events and PTSD. In a test–retest study of wave 2 NESARC, reliability for lifetime PTSD was in the fair to good range (k=0.64) (Ruan et al. 2008). The interview queried 27 specific events. Four events were merged with similar events to yield 22 traumatic event types. One event, indirect exposure to a terrorist attack through watching television or listening to the radio, was excluded. These 22 events were then grouped into six major categories based on prior research on PTSD (Breslau et al. 2004b, 2006b) : child maltreatment (three items) ; interpersonal violence (six items) ; war-related traumas (four items) ; other injury or shocking event (five items) ; learning of a trauma to a close friend or relative (three items) ; and learning of an unexpected death (one item).
Respondents who endorsed more than one traumatic event (85% of the sample) were asked to designate one of these as their ‘worst stressful event’. This worst event (for respondents with more than one event) or their only reported event (for respondents with one event) was used to diagnose PTSD. The worst event procedure has been widely used in epidemiologic studies to reduce respondent burden (Breslau et al. 1991, 1998; Kessler et al. 1995, 2005), because it is an efficient way to identify persons with lifetime PTSD and to estimate the conditional risk of PTSD associated with specific events (Breslau et al. 1997, 2004a).
PTSD resulting from this event was diagnosed strictly according to the DSM-IV criteria (APA, 1994). This required respondents with a worst trauma to endorse each of six criteria : (1) having felt extremely frightened, helpless, or horrified during the event; (2) one re-experiencing symptom; (3) three avoidance or numbness symptoms; (4) two hyper-arousal symptoms; (5) duration of more than 1 month; and (6) functional impairment resulting from these symptoms. Functional impairment was defined in this study as an affirmative answer to at least one of five items from the interview. A sixth item judged as vague and insufficient was not included: ‘Were you uncomfortable or upset by any of these reactions ?’.
Prior research has shown that characteristics of trauma exposure influence the conditional risk of PTSD following an exposure, and may explain race/ethnic differences in risk for the disorder (Breslau et al. 1998; Brewin et al. 2000; Acierno et al. 2007; Dohrenwend et al. 2008; Roberts et al. in press). These include: (1) worst trauma type; (2) age at worst trauma, divided into : ≤11 years, 12–17 years, 18–29 years, and ≥30 years; and (3) number of event types prior to worst trauma, measured by number of different event types (e.g. serious accident, natural disaster) experienced before the worst trauma. Total number of prior events (e.g. number of serious accidents) could not be assessed from NESARC data.
Treatment-seeking among people with PTSD was defined as having seen a counselor, doctor, or therapist, or having visited a hospital to get help for PTSD symptoms related to their worst trauma.
Race/ethnicity
Respondents chose among the following race categories : (1) American Indian or Alaskan Native; (2) Asian; (3) Black or African American; (4) Native Hawaiian or other Pacific Islander ; and (5) White. Respondents also indicated whether they were of Hispanic origin. Following a US Census Bureau algorithm, NESARC classified respondents to one race/ethnicity in the following preferential order: Hispanic, non-Hispanic Black, non-Hispanic American Indian/Native Alaskan, non-Hispanic Native Hawaiian/Pacific Islander/Asian, and non-Hispanic White (National Epidemiologic Survey on Alcohol and Related Conditions, 2004). Due to a small sample size (n=578) and availability of larger datasets of American Indians elsewhere (Beals et al. 2005a, b; Libby et al. 2005; Sawchuk et al. 2005), we excluded non-Hispanic American Indian/Alaska Natives from these analyses†.
Covariate
Age at interview was measured continuously.
Missing data
The NESARC dataset includes assigned data for respondents missing race/ethnicity or age at interview (fewer than 1% of respondents) (Grant & Kaplan, 2005). For respondents missing exposure to any specific traumatic event, we assigned ‘no exposure’ (1.4% of the sample). Respondents missing any PTSD symptoms were assigned as not experiencing those symptoms (1.8% of the sample). Results were unchanged in sensitivity analyses excluding respondents with missing data.
Analyses
We first examined whether there were race/ethnic differences in lifetime prevalence of PTSD, using χ2 tests of significance. The second set of analyses addressed race/ethnic differences in exposure to potentially traumatic events. Lifetime prevalence for any event, the six categories of events, and each individual event are reported by race/ethnicity. We used discrete- time survival analysis to estimate race/ethnic differences in the risk of each individual event and the six categories of events, adjusted for gender (Cox, 1972). The dependent variable in these analyses is the age at which each event first occurred; person-time was censored at the age at interview. Because risk for particular traumatic event types varies significantly by age, and the age distribution among respondents is different in the race/ethnic groups, accounting for the underlying risk of traumatic events at each age is important. To see if risk of events differed for race/ethnic groups by gender, we tested gender × race/ethnicity interaction terms for each event. The gender × race/ethnicity interaction term was only significant for risk of war-related events; therefore we analyzed war-related events separately for men and women.
The third set of analyses addressed race/ethnic differences in the conditional risk of PTSD following exposure to a potentially traumatic event by fitting logistic regression models of PTSD among respondents reporting an event. We then added characteristics of event exposure, including worst trauma type, age at worst trauma, and number of event types prior to worst trauma, to see if differences in these characteristics of event exposure accounted for possible race/ethnic differences in the risk of developing PTSD.
The final set of analyses addressed race/ethnic differences in treatment-seeking among individuals with PTSD. We conducted χ2 tests for race/ethnic differences in the percentage of individuals with PTSD receiving treatment, and subsequently fitted logistic regression models of treatment-seeking among all individuals with PTSD, adjusting for gender and age at interview.
All analyses were conducted using SUDAAN software (2008; RTI International, USA), to account for the complex sampling design of the NESARC. We used the wave 2 sampling weights, which weight the data to reflect the US population in terms of age, geographic region, and race/ethnicity.
Results
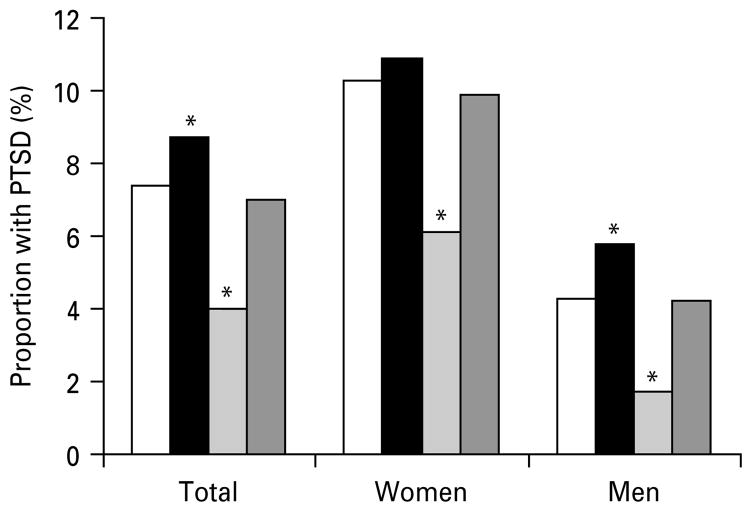
The NESARC wave 2 sample was 58.2% White, 19.0% Black, 2.8% Asian and 18.4% Hispanic. The lifetime prevalence of PTSD in the population was 7.3 [standard error (S.E.)=0.2]%. Blacks had significantly higher prevalence of PTSD than Whites [8.7 (S.E.=0.5)% v. 7.4 (S.E.=0.2)%, p=0.03], Hispanics [7.0 (S.E.=0.5)%, p=0.55] had a similar prevalence as Whites, and Asians had significantly lower prevalence [4.0 (S.E.=0.7)%, p=0.001] (Fig. 1).
Fig. 1.
Lifetime prevalence of post-traumatic stress disorder (PTSD) in non-institutionalized US residents, 2004–2005, by race/ethnicity (n=34 075). □, White, non-Hispanic ; ■, Black, non-Hispanic ;
 , Asian/Hawaiian/Pacific Islander, non-Hispanic ;
, Asian/Hawaiian/Pacific Islander, non-Hispanic ;
 , Hispanic. * Significantly different from White, non-Hispanic (p<0.05).
, Hispanic. * Significantly different from White, non-Hispanic (p<0.05).
Prevalence of exposure to traumatic events
Table 1 presents the lifetime prevalence of exposure to each of the six categories and individual events by race/ethnicity. Whites had significantly higher exposure to any event, other injury or shocking event, learning of trauma to a close friend or relative, and learning of an unexpected death, compared with Blacks, Asians, or Hispanics. However, Hispanics and Blacks had significantly higher exposure to child maltreatment compared with Whites, due primarily to higher rates of witnessing domestic violence. Blacks also had significantly higher exposure to assaultive violence than Whites. Asian men and women had the highest rates for war-related events of the four race/ethnic groups, with 19.1% of men and 10.6% of women reporting an event. Compared with Whites, Asian men reported significantly higher prevalence of having been a refugee (12.3% v. 0.5%) or having been a civilian in a war zone (7.5% v. 2.0%), but lower prevalences of combat exposure (5.4% v. 12.9%). Asian women, like Asian men, had far higher rates than Whites of having been a refugee or having been a civilian in a war zone. For every major event category except war-related events, Asians had the lowest exposure of the four race/ethnic groups.
Table 1.
Lifetime exposure to potentially traumatic events by race/ethnicity: non-institutionalized US residents (n=34 075)
| White, non-Hispanic (n=20 161) | Black, non-Hispanic (n=6587) | Asian/Hawaiian/Pacific Islander, non-Hispanic (n=968) | Hispanic (n=6359) | |
|---|---|---|---|---|
| Any trauma*** | 83.66 (0.44) | 76.37 (1.25) | 66.38 (2.28) | 68.17 (1.17) |
| Any war-related trauma: men (n=14 324)*** | 12.89 (0.42) | 13.66 (0.99) | 19.14 (2.43) | 10.30 (1.85) |
| Combat*** | 10.01 (0.36) | 10.03 (0.89) | 5.35 (1.17) | 4.38 (0.53) |
| Peacekeeper/relief worker* | 2.04 (0.17) | 3.05 (0.39) | 1.90 (0.56) | 1.44 (0.31) |
| Unarmed civilian in war zone** | 2.02 (0.17) | 1.89 (0.37) | 7.46 (1.47) | 3.76 (0.80) |
| Refugee*** | 0.51 (0.10) | 1.43 (0.45) | 12.30 (2.24) | 4.10 (1.77) |
| Any war-related trauma: women (n=19 751)*** | 1.81 (0.15) | 2.09 (0.35) | 10.60 (1.51) | 3.94 (0.95) |
| Combat | 0.19 (0.05) | 0.42 (0.12) | 0.53 (0.34) | 0.26 (0.11) |
| Peacekeeper/relief worker | 0.15 (0.03) | 0.51 (0.25) | 0.79 (0.63) | 0.09 (0.04) |
| Unarmed civilian in war zone** | 1.32 (0.12) | 1.34 (0.27) | 7.20 (1.45) | 1.91 (0.34) |
| Refugee*** | 0.52 (0.09) | 0.53 (0.16) | 6.10 (1.23) | 2.56 (0.98) |
| Any child maltreatment*** | 11.43 (0.28) | 13.98 (0.69) | 7.78 (1.1) | 14.78 (0.86) |
| Physical abuse** | 3.42 (0.14) | 2.66 (0.22) | 2.42 (0.46) | 4.33 (0.36) |
| Neglect* | 2.97 (0.12) | 3.49 (0.28) | 1.83 (0.53) | 3.11 (0.31) |
| Witness to domestic violence*** | 9.26 (0.26) | 11.72 (0.65) | 6.46 (0.94) | 12.53 (0.82) |
| Any assaultive violence*** | 26.13 (0.43) | 29.26 (1.02) | 16.34 (1.34) | 25.56 (0.81) |
| Unwanted sex*** | 9.14 (0.28) | 9.13 (0.51) | 2.99 (0.45) | 6.49 (0.45) |
| Victim domestic violence*** | 5.90 (0.20) | 7.92 (0.46) | 3.01 (0.56) | 5.61 (0.39) |
| Attacked/beaten up*** | 8.01 (0.23) | 6.45 (0.37) | 4.62 (0.69) | 7.61 (0.58) |
| Kidnapped | 0.79 (0.07) | 1.07 (0.16) | 0.50 (0.17) | 0.72 (0.13) |
| Stalked* | 5.24 (0.16) | 6.66 (0.43) | 4.39 (0.90) | 5.05 (0.46) |
| Mugged*** | 11.13 (0.32) | 15.03 (0.82) | 8.25 (1.19) | 12.97 (0.73) |
| Any other injury or shocking event*** | 52.5 (0.58) | 46.44 (1.08) | 38.55 (1.91) | 41.26 (1.15) |
| Serious or life-threatening accident*** | 17.35 (0.36) | 16.11 (0.66) | 12.12 (1.28) | 12.57 (0.66) |
| Serious or life-threatening illness*** | 19.15 (0.33) | 14.01 (0.53) | 7.93 (1.19) | 8.89 (0.78) |
| Natural disaster** | 16.14 (0.66) | 12.97 (0.86) | 13.56 (1.69) | 15.92 (1.13) |
| Experienced terrorist attack | 0.90 (0.09) | 1.14 (0.30) | 2.04 (0.50) | 0.76 (0.17) |
| Saw someone injured/killed/discovered a dead body*** | 25.13 (0.42) | 23.25 (0.84) | 15.75 (1.53) | 19.73 (0.89) |
| Unexpected death*** | 44.65 (0.54) | 39.90 (1.18) | 25.75 (1.82) | 29.63 (1.35) |
| Any learned of trauma to a close friend/relative*** | 56.86 (0.54) | 44.82 (1.1) | 36.14 (2.28) | 36.39 (1.12) |
| Close friend or relative experienced serious or life-threatening accident or injury*** | 51.39 (0.55) | 38.25 (1.28) | 28.79 (2.07) | 30.23 (1.04) |
| Someone close experienced terrorist attack | 5.26 (0.37) | 5.64 (0.60) | 6.58 (1.04) | 4.61 (0.65) |
| Close friend or relative experienced other stressful or traumatic experience*** | 14.87 (0.33) | 12.43 (0.54) | 9.59 (1.12) | 10.30 (0.65) |
Values are given as percentage (standard error).
Significant difference for prevalence of traumatic event between race/ethnic groups, evaluated with a Cochran Mantel–Haenszel Wald F test:
p<0.05,
p<0.01,
p<0.001.
Risk of exposure to traumatic events
Table 2 presents results of the discrete time survival models predicting exposure to traumatic events adjusted for gender and age at interview. Blacks, Asians, and Hispanics had lower risk than Whites for any event, learning of trauma to a close friend or relative, learning of an unexpected death, and other injury or shocking event. Asians and Hispanics also had lower risk of assaultive violence than Whites. However, Hispanics and Blacks had significantly higher risk of child maltreatment than Whites. Risk for war-related events was substantially higher for both Asian men and women than for White men and women. Black men and Hispanic women also had higher risk for war-related events than Whites.
Table 2.
Survival models for risk of potentially traumatic event by race/ethnicity: non-institutionalized US residents, adjusted for gender and age at interview (n=34 075)
| White, non-Hispanic | Black, non-Hispanic | Asian/Hawaiian/Pacific Islander, non-Hispanic | Hispanic | |
|---|---|---|---|---|
| Any trauma*** | 1.00 (Ref.) | 0.86 (0.81–0.91) | 0.68 (0.60–0.77) | 0.76 (0.72–0.81) |
| Any war-related trauma: men*** | 1.00 (Ref.) | 1.30 (1.10–1.55) | 2.01 (1.44–2.80) | 1.20 (0.85–1.70) |
| Combat*** | 1.00 (Ref.) | 1.31 (1.08–1.58) | 0.72 (0.47–1.10) | 0.72 (0.55–0.95) |
| Peacekeeper/relief worker* | 1.00 (Ref.) | 1.70 (1.23–2.34) | 1.08 (0.58–2.01) | 0.90 (0.58–1.39) |
| Unarmed civilian in war zone*** | 1.00 (Ref.) | 1.02 (0.66–1.58) | 4.32 (2.71–6.91) | 2.28 (1.50–3.47) |
| Refugee*** | 1.00 (Ref.) | 2.87 (1.32–6.24) | 26.50 (13.99–50.22) | 8.56 (2.91–25.17) |
| Any war-related trauma: women*** | 1.00 (Ref.) | 1.26 (0.87–1.84) | 6.98 (4.77–10.20) | 2.61 (1.61–4.26) |
| Combat | 1.00 (Ref.) | 2.35 (1.07–5.18) | 2.96 (0.74–11.89) | 1.47 (0.53–4.08) |
| Peacekeeper/relief worker* | 1.00 (Ref.) | 3.31 (1.15–9.55) | 5.18 (0.94–28.48) | 0.57 (0.20–1.62) |
| Unarmed civilian in war zone*** | 1.00 (Ref.) | 1.14 (0.75–1.74) | 6.59 (4.07–10.66) | 1.80 (1.22–2.66) |
| Refugee*** | 1.00 (Ref.) | 1.13 (0.59–2.19) | 13.66 (7.76–24.04) | 5.97 (2.66–13.40) |
| Any child maltreatment*** | 1.00 (Ref.) | 1.17 (1.05–1.30) | 0.64 (0.48–0.86) | 1.23 (1.08–1.40) |
| Physical abuse*** | 1.00 (Ref.) | 0.73 (0.61–0.87) | 0.67 (0.45–1.00) | 1.18 (0.97–1.43) |
| Neglect | 1.00 (Ref.) | 1.12 (0.94–1.33) | 0.58 (0.33–1.04) | 0.98 (0.78–1.22) |
| Witness to domestic violence*** | 1.00 (Ref.) | 1.20 (1.07–1.36) | 0.66 (0.49–0.89) | 1.28 (1.11–1.47) |
| Any assaultive violence*** | 1.00 (Ref.) | 1.06 (0.97–1.15) | 0.54 (0.45–0.96) | 0.87 (0.80–0.94) |
| Unwanted sex*** | 1.00 (Ref.) | 0.86 (0.76–0.96) | 0.28 (0.20–0.39) | 0.62 (0.53–0.72) |
| Victim domestic violence*** | 1.00 (Ref.) | 1.21 (1.07–1.37) | 0.47 (0.32–0.68) | 0.90 (0.76–1.05) |
| Attacked/beaten up*** | 1.00 (Ref.) | 0.78 (0.68–0.88) | 0.52 (0.37–0.71) | 0.81 (0.68–0.95) |
| Kidnapped | 1.00 (Ref.) | 1.28 (0.91–1.78) | 0.60 (0.31–1.16) | 0.84 (0.54–1.30) |
| Stalked* | 1.00 (Ref.) | 1.11 (0.96–1.27) | 0.75 (0.49–1.14) | 0.83 (0.69–1.01) |
| Mugged*** | 1.00 (Ref.) | 1.39 (1.23–1.58) | 0.69 (0.50–0.95) | 1.09 (0.96–1.23) |
| Any other injury or shocking event*** | 1.00 (Ref.) | 0.87 (0.82–0.92) | 0.68 (0.60–0.77) | 0.77 (0.72–0.83) |
| Serious accident*** | 1.00 (Ref.) | 0.95 (0.87–1.05) | 0.67 (0.53–0.86) | 0.71 (0.63–0.80) |
| Serious illness*** | 1.00 (Ref.) | 0.81 (0.75–0.88) | 0.46 (0.34–0.62) | 0.57 (0.48–0.69) |
| Natural disaster* | 1.00 (Ref.) | 0.83 (0.74–0.94) | 0.87 (0.68–1.11) | 1.06 (0.93–1.22) |
| Experienced terrorist attack* | 1.00 (Ref.) | 1.29 (0.83–2.01) | 2.25 (1.31–3.88) | 0.82 (0.51–1.32) |
| Saw someone killed/saw a dead body*** | 1.00 (Ref.) | 0.95 (0.87–1.03) | 0.59 (0.47–0.74) | 0.76 (0.68–0.84) |
| Other trauma to self*** | 1.00 (Ref.) | 0.58 (0.47–0.70) | 0.69 (0.48–1.00) | 0.65 (0.53–0.81) |
| Unexpected death of somebody close*** | 1.00 (Ref.) | 0.82 (0.77–0.88) | 0.50 (0.42–0.58) | 0.59 (0.53–0.65) |
| Any learning of trauma to close friend or relative*** | 1.00 (Ref.) | 0.68 (0.64–0.72) | 0.52 (0.45–0.61) | 0.53 (0.49–0.57) |
| Illness/accident to someone close*** | 1.00 (Ref.) | 0.65 (0.60–0.70) | 0.47 (0.40–0.55) | 0.50 (0.46–0.55) |
| Someone close experienced terrorist attack | 1.00 (Ref.) | 1.02 (0.87–1.19) | 1.18 (0.87–1.61) | 0.79 (0.61–1.03) |
| Other trauma to someone close*** | 1.00 (Ref.) | 0.78 (0.70–0.85) | 0.59 (0.46–0.75) | 0.62 (0.54–0.71) |
Values are given as odds ratio (95% confidence interval).
Significant difference for prevalence of traumatic event between race/ethnic groups, evaluated with a Cochran Mantel–Haenszel Wald F test:
p<0.05,
p<0.01,
p<0.001.
Development of PTSD conditional on exposure to a traumatic event
Table 3 presents the risk of developing PTSD among people exposed to a traumatic event. Among people experiencing an event (n=27 147), 9.1 (S.E.=0.2)% developed PTSD (n=2768). Similar to lifetime prevalences presented in Fig. 1, conditional risk of developing PTSD was significantly higher for Blacks, statistically equivalent for Hispanics, and lower for Asians compared with Whites, in a model adjusting for gender and age at interview. However, the excess PTSD risk for Blacks compared with Whites was small (adjusted odds ratio=1.21 v. 1.00). Race/ethnic groups differed significantly in some characteristics of exposure to potentially traumatic events, including worst event type [Wald F(15)=3.97, p=0.0000], and age at worst event [Wald F(12)=3.16, p=0.001], but not number of prior trauma types. Each of these factors was also significantly related to the probability of developing PTSD in a model adjusting for the other factors, race/ethnicity and gender (Table 3, model 2). However, characteristics of trauma exposure did not account for the relationship between race/ethnicity and conditional risk of PTSD once exposed to an event.
Table 3.
Logistic regression models of development of post-traumatic stress disorder among people exposed to a traumatic event: non-institutionalized US residents (n=27 147)
| Model 1: adjusted for gender and age at interview | Model 2: adjusted for gender, age at interview, and trauma characteristics | |
|---|---|---|
| Race/ethnicity | ||
| White, non-Hispanic (n=14 911) | 1.00 (Ref.) | 1.00 (Ref.) |
| Black, non-Hispanic (n=4370) | 1.21 (1.05–1.40)* | 1.22 (1.05–1.43)* |
| Asian/Hawaiian/Pacific Islander, non-Hispanic (n=519) | 0.62 (0.43–0.89)* | 0.67 (0.45–0.99)* |
| Hispanic (n=3651) | 1.11 (0.93–1.32) | 1.12 (0.93–1.34) |
| Worst trauma type | ||
| War-related | ||
| Combat (n=658) | 3.41 (2.35–4.96)* | |
| Peacekeeper/relief worker (n=28) | 1.27 (0.26–6.28) | |
| Civilian in war zone (n=81) | 2.45 (1.10–5.46)* | |
| Refugee (n=68) | 1.66 (0.46–5.97) | |
| Child maltreatment | ||
| Physical abuse in childhood (n=164) | 8.40 (5.48–12.87)* | |
| Neglect in childhood (n=92) | 6.90 (3.79–12.57)* | |
| Witnessed domestic violence in childhood (n=434) | 3.77 (2.63–5.42)* | |
| Assaultive violence | ||
| Unwanted sex (n=1031) | 7.85 (6.35–9.71)* | |
| Victim domestic violence (n=459) | 6.47 (4.71–8.90)* | |
| Attacked/beaten up (n=149) | 3.49 (1.94–6.28)* | |
| Kidnapped (n=37) | 4.04 (1.43–11.37)* | |
| Stalked (n=174) | 2.75 (1.56–4.83)* | |
| Mugged (n=515) | 1.57 (1.01–2.45)* | |
| Other injury or shocking event | ||
| Serious accident (n=765) | 2.04 (1.51–2.77)* | |
| Serious illness (n=1006) | 1.88 (1.38–2.55)* | |
| Natural disaster (n=575) | 1.13 (0.69–1.86) | |
| Experienced terrorist attack (n=52) | 0.99 (0.35–2.83) | |
| Saw somebody die/saw a dead body (n=1293) | 1.91 (1.49–2.46)* | |
| Other trauma to self (n=722) | 2.95 (2.26–3.85)* | |
| Unexpected death of somebody close (n=7000) | 1.75 (1.49–2.06)* | |
| Learning of trauma to close friend or relative | ||
| Illness/accident to somebody close (n=6600) | 1.00 (Ref.) | |
| Someone close experienced terrorist attack (n=290) | 0.49 (0.24–1.00) | |
| Other trauma to someone close (n=1258) | 0.80 (0.58–1.10) | |
| Age at worst trauma, years | ||
| <12 (n=3081) | 1.76 (1.46–2.12)* | |
| 12–17 (n=3247) | 1.61 (1.31–1.97)* | |
| 18–29 (n=6960) | 1.33 (1.14–1.56)* | |
| ≥30 (n=10 163) | 1.00 (Ref.) | |
| Number of trauma types prior to worst trauma | 1.34 (1.20–1.37)* | |
Values are given as adjusted odds ratio (95% confidence interval).
Statistically significantly different from Ref. group (p<0.05).
Race/ethnic differences in treatment-seeking for PTSD
Among people with PTSD, a significantly lower percentage of all race/ethnic minority groups received treatment for PTSD symptoms in the form of visiting a doctor, counselor, or hospital than Whites, unadjusted for other factors, with 53.3 (S.E.=1.5)% of Whites receiving treatment, but only 35.3 (S.E.=2.6)% of Blacks, 42.0 (S.E.=2.9)% of Hispanics and 32.7 (S.E.=7.1)% of Asians. Table 4 presents logistic regression models for treatment-seeking, adjusted for gender and age at interview. Blacks, Asians and Hispanics were significantly less likely to receive treatment for PTSD symptoms than Whites in adjusted models.
Table 4.
Logistic models for receipt of treatment among people with post-traumatic stress disorder by race/ethnicity
| Odds ratio (95% CI)a | |
|---|---|
| Race/ethnicity | |
| White, non-Hispanic | 1.00 (Ref.) |
| Black, non-Hispanic | 0.46 (0.35–0.60)* |
| Asian/Hawaiian/Pacific Islander, non-Hispanic | 0.39 (0.20–0.77)* |
| Hispanic | 0.61 (0.46–0.80)* |
| Gender | |
| Men | 1.00 (Ref.) |
| Women | 1.34 (1.09–1.65)* |
CI, Confidence interval.
Adjusted for gender and age at interview.
Statistically different from reference group (p<0.05, Wald χ2).
Discussion
In this national survey, we found marked racial/ethnic differences in lifetime risk of PTSD and treatment- seeking for PTSD symptoms. Specifically, we found that Blacks had higher lifetime prevalence of PTSD (8.7%) and Asians (4.0%) considerably lower prevalence than Whites (7.4%). After partitioning risk of PTSD into (1) risk of exposure to potentially traumatic events, and (2) risk of developing PTSD once exposed to an event, we found that Asians had both lower risk of exposure to any traumatic event and lower risk of developing PTSD once exposed, compared with Whites. In contrast, although Blacks had lower rates of exposure to any traumatic event, their risk of developing PTSD once exposed was slightly higher than Whites.
Our finding that Asians were at lower risk for the development of PTSD once exposed to a potentially traumatic event, and that Blacks were at higher risk, has not been found in prior studies of specific events (Vogel & Marshall, 2001; Adams & Boscarino, 2005; Alim et al. 2006) or in non-representative samples from specific geographic areas (Breslau et al. 1991, 2004b). Prior studies with smaller sample sizes may have lacked the power to detect the modest difference we found in conditional risk of developing PTSD for Blacks compared with Whites (Norris, 1992; Vogel & Marshall, 2001). Moreover, many prior studies were restricted by socio-economic status, geography, or other factors ; therefore their findings may not reflect national circumstances (Breslau et al. 1991; Norris, 1992; Vogel & Marshall, 2001). The characteristics of exposure to potentially traumatic events that we examined (e.g. worst event type, age at worst event, and number of prior traumatic events) did not explain race/ethnic differences in conditional risk of PTSD.
Different patterns of adverse experiences outside of the events examined here, or protective factors among race/ethnic groups, may explain the differences that we found in risk of PTSD (Loo et al. 2007; Ellis et al. 2008; Williams et al. 2008). For example, perceived discrimination, race-related verbal assault and racial stigmatization have been linked to PTSD symptoms and may partially account for the higher conditional risk of PTSD among Blacks (Loo, 1994; Loo et al. 2005; Ellis et al. 2008). In contrast, higher socio-economic status has been found to reduce the conditional risk of developing PTSD (Brewin et al. 2000; Koenen et al. 2002; Dohrenwend et al. 2008); thus higher educational attainment and higher income among Asians, and lower educational attainment and income among Blacks, may contribute to those race/ethnicities’ respective risks of developing PTSD (Stoops, 2004; DeNavas-Walt et al. 2008). Finally, pre-existing anxiety and depression have been linked to higher conditional risk of PTSD (Breslau et al. 1991, 1997; Hapke et al. 2006), and epidemiologic research suggests that Asian Americans may have lower prevalence of these illnesses than Whites (Harris et al. 2005). However, Blacks also have lower reported rates of anxiety and depression than Whites, yet we found elevated conditional risk of PTSD among Blacks compared with Whites (Breslau et al. 2006a; Himle et al. 2009). These explanatory factors would best be explored in prospective longitudinal studies, given that prior PTSD is associated with subsequent anxiety, depression and decreased socio-economic attainment (Breslau et al. 1997; Jayakody et al. 1998; Perkonigg et al. 2005; Copeland et al. 2007).
Minorities reported lower exposure to any potentially traumatic event, learning of a trauma to a close friend or relative, learning of an unexpected death, and other traumatic events compared with Whites. Furthermore, they had lower risk of experiencing unwanted sex, an event that was both fairly common and carried an extremely elevated risk of developing PTSD. However, among two of the event groups with the highest risk of development of PTSD, war-related events and child maltreatment, minority groups experienced some higher risks. Blacks and Hispanics had higher risk of witnessing domestic violence as children, Blacks had higher risk of active combat, and Asians had higher risk of having been a civilian in a war zone than Whites.
Our findings that Blacks experienced higher levels of violent victimization and Asians had substantially lower levels compared with Whites are supported by The US Department of Justice’s National Crime Victimization Survey, an annual survey of crime victimization (Rand, 2008; Harrell, 2009). We could find no studies comparing rates of other event exposures in Asians with Whites in a US general population, although a study of pregnant women found significantly lower prevalence of emotional stressors, such as loss of a loved one, in Asians compared with Whites (Lu & Chen, 2004).
Our finding that Blacks in the USA have the same or lower exposure than Whites to unexpected deaths and traumas to friends and relatives is counter-intuitive, given that Blacks experience higher mortality and higher crime victimization rates than Whites (Williams & Jackson, 2005; Harrell, 2007). However, two regional studies found Blacks at lower risk for some events: Breslau found Blacks had lower exposure to learning of a trauma to a close friend or relative (Breslau et al. 2004b), and Norris found that lifetime exposure to any event, physical assault, tragic death, and disaster other than fire were lower for Blacks than for Whites (Norris, 1992). However, several other regional studies have found no difference between Whites and Blacks in exposure to most event types (Norris, 1992; Breslau et al. 1995, 1998, 2004b).
Asians’ lower risk for exposure to all types of potentially traumatic events other than war-related events, compared with other race/ethnic groups, may be related to their relatively higher socio-economic status and lower rates of certain behavioral and substance problems (Stoops, 2004; DeNavas-Walt et al. 2008). High socio-economic status, including high education, high income and high maternal education are linked with lower exposure to assault, witnessing violence, and emotional abuse in childhood, and serious illness, traffic accidents, and any trauma (Hasselberg et al. 2001; Finkelhor et al. 2005, 2007; Breslau et al. 2006b; Todd et al. 2006). However, Whites experienced higher risk for any traumatic event although they have higher average income and educational attainment than both Blacks and Hispanics in the USA (Stoops, 2004; DeNavas-Walt et al. 2008). Conduct disorder, hyperactivity, aggression and antisocial behavior have also been linked prospectively to greater exposure to potentially traumatic events (Koenen et al. 2005, 2007; Breslau et al. 2006b; Storr et al. 2007), mediated in part through alcohol and drug abuse (Koenen et al. 2005). Asians have significantly lower rates of conduct disorder and substance dependence than Whites (Sakai et al. 2005, 2008), possibly further contributing to their lower risk of exposure to potentially traumatic events.
Minorities in this study had substantially lower odds of treatment-seeking for their PTSD-related symptoms than Whites, which agrees with findings from prior studies of mental illnesses (Wang et al. 2005; Huang et al. 2007; Ta et al. 2008). Explanations for why race/ethnic minorities receive treatment less frequently than Whites vary by race/ethnic group, and include: shared group perceptions that mental illness is highly stigmatizing (Yamashiro & Matsuoka, 1997); reluctance to seek help outside the family except in extreme circumstances (Yamashiro & Matsuoka, 1997); mistrust of physicians (Alim et al. 2006); perception of racial or ethnic bias in care providers (Johnson et al. 2004); and reduced access to general- and mental-health facilities due to residence in poverty areas (Chow et al. 2003). Health professionals must continue to work to remove stigma from mental illness, particularly among minority groups, and to reduce minorities’ barriers to mental health care.
Limitations
Current findings should be interpreted in the context of three notable limitations. First, this study relies on retrospective reporting of traumatic event exposure, PTSD symptoms and treatment-seeking for PTSD. Retrospective reporting results in lower prevalence estimates of events and illness than repeated contemporaneous reporting (Brewin et al. 1993; Kruijshaar et al. 2005; Moffitt et al. 2009). However, reduced prevalences due to retrospective reports are unlikely to operate differentially across racial and ethnic groups to produce the differences reported here. Second, cultural differences between race/ethnic groups in willingness to disclose stigmatizing events, such as child maltreatment and sexual assault, may introduce bias (Zhai & Gao, 2009). Such bias could account for, in part, Asians’ lower prevalences of trauma exposure for most events. However, US national data indicate that rates of reporting crimes to police are similar among race/ethnic groups for most types of crime (Harrell, 2009). Third, we used broad categories of race/ethnicity as defined by the US Census. Recent work on other mental disorders has found significant differences within race/ethnic groups based on age, gender, education, immigrant status, country of origin and length of stay in the USA (Dawson, 1998; Ortega et al. 2000; Alegria et al. 2006, 2008; Breslau et al. 2006a ; Breslau & Chang, 2006; Huang et al. 2007; Takeuchi et al. 2007). Future research needs to examine the ways in which the distribution of trauma exposure and PTSD varies within racial groups by ethnic background, nativity status, length of stay in the USA, and ancestry.
Acknowledgments
The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) is funded by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) with supplemental support from the National Institute on Drug Abuse (NIDA). A.L.R. was supported by the Harvard Training Program in Psychiatric Genetics and Translational Research no. T32MH017119. K.C.K. was supported by US National Institutes of Health grant no. K08MH070627 and grant no. 5R01MH078928. J.B. was supported by National Institute of Mental Health grant no. MH082023. S.E.G. was supported by National Institutes of Health grant no. RO3DA20887. N.B. was supported by National Institute of Mental Health grant no. MH71395.
Footnotes
For brevity, we refer to non-Hispanic Whites as ‘ Whites ’, non-Hispanic Blacks as ‘ Blacks ’, and non-Hispanic Native Hawaiian/Pacific Islander/Asians as ‘ Asians ’ in this paper.
Declaration of Interest
None.
References
- Acierno R, Ruggiero KJ, Galea S, Resnick HS, Koenen K, Roitzsch J, de Arellano M, Boyle J, Kilpatrick DG. Psychological sequelae resulting from the 2004 Florida hurricanes : implications for postdisaster intervention. American Journal of Public Health. 2007;97 (Suppl 1):S103–S108. doi: 10.2105/AJPH.2006.087007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA. Differences in mental health outcomes among Whites, African Americans, and Hispanics following a community disaster. Psychiatry. 2005;68:250–265. doi: 10.1521/psyc.2005.68.3.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Canino G, Shrout PE, Woo M, Duan N, Vila D, Torres M, Chen CN, Meng XL. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. American Journal of Psychiatry. 2008;165:359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Canino G, Stinson FS, Grant BF. Nativity and DSM-IV psychiatric disorders among Puerto Ricans, Cuban Americans, and non-Latino Whites in the United States : results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67:56–65. doi: 10.4088/jcp.v67n0109. [DOI] [PubMed] [Google Scholar]
- Alim TN, Charney DS, Mellman TA. An overview of posttraumatic stress disorder in African Americans. Journal of Clinical Psychology. 2006;62:801–813. doi: 10.1002/jclp.20280. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 4. APA; Washington, DC: 1994. [Google Scholar]
- Beals J, Manson SM, Whitesell NR, Spicer P, Novins DK, Mitchell CM. Prevalence of DSM-IV disorders and attendant help-seeking in 2 American Indian reservation populations. Archives of General Psychiatry. 2005a;62:99–108. doi: 10.1001/archpsyc.62.1.99. [DOI] [PubMed] [Google Scholar]
- Beals J, Novins DK, Whitesell NR, Spicer P, Mitchell CM, Manson SM. Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations : mental health disparities in a national context. American Journal of Psychiatry. 2005b;162:1723–1732. doi: 10.1176/appi.ajp.162.9.1723. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Galea S, Adams RE, Ahern J, Resnick H, Vlahov D. Mental health service and medication use in New York City after the September 11, 2001, terrorist attack. Psychiatric Services. 2004;55:274–283. doi: 10.1176/appi.ps.55.3.274. [DOI] [PubMed] [Google Scholar]
- Breslau J, Aguilar-Gaxiola S, Kendler KS, Su M, Williams D, Kessler RC. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychological Medicine. 2006a;36:57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Chang DF. Psychiatric disorders among foreign-born and US-born Asian-Americans in a US national survey. Social Psychiatry and Psychiatric Epidemiology. 2006;41:943–950. doi: 10.1007/s00127-006-0119-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N. Epidemiologic studies of trauma, posttraumatic stress disorder, and other psychiatric disorders. Canadian Journal of Psychiatry. 2002;47:923–929. doi: 10.1177/070674370204701003. [DOI] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. American Journal of Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P. Risk factors for PTSD-related traumatic events : a prospective analysis. American Journal of Psychiatry. 1995;152:529–535. doi: 10.1176/ajp.152.4.529. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Archives of General Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Peterson EL, Schultz L. Psychiatric sequelae of posttraumatic stress disorder in women. Archives of General Psychiatry. 1997;54:81–87. doi: 10.1001/archpsyc.1997.01830130087016. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Archives of General Psychiatry. 2003;60:289–294. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler R, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Breslau N, Lucia VC, Alvarado GF. Intelligence and other predisposing factors in exposure to trauma and posttraumatic stress disorder : a follow-up study at age 17 years. Archives of General Psychiatry. 2006b;63:1238–1245. doi: 10.1001/archpsyc.63.11.1238. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Poisson LM, Schultz LR, Lucia VC. Estimating post-traumatic stress disorder in the community: lifetime perspective and the impact of typical traumatic events. Psychological Medicine. 2004a;34:889–898. doi: 10.1017/s0033291703001612. [DOI] [PubMed] [Google Scholar]
- Breslau N, Wilcox HC, Storr CL, Lucia VC, Anthony JC. Trauma exposure and posttraumatic stress disorder : a study of youths in urban America. Journal of Urban Health. 2004b;81:530–544. doi: 10.1093/jurban/jth138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Gotlib IH. Psychopathology and early experience : a reappraisal of retrospective reports. Psychological Bulletin. 1993;113:82–98. doi: 10.1037/0033-2909.113.1.82. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Bromet E, Sonnega A, Kessler RC. Risk factors for DSM-III-R posttraumatic stress disorder : findings from the National Comorbidity Survey. American Journal of Epidemiology. 1998;147:353–361. doi: 10.1093/oxfordjournals.aje.a009457. [DOI] [PubMed] [Google Scholar]
- Chow JC, Jaffee K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. American Journal of Public Health. 2003;93:792–797. doi: 10.2105/ajph.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64:577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Cox D. Regression models and life-tables. Journal of the Royal Statistical Society, Series B (Methodological) 1972;34:187–220. [Google Scholar]
- Dawson DA. Beyond black, white and Hispanic : race, ethnic origin and drinking patterns in the United States. Journal of Substance Abuse. 1998;10:321–339. doi: 10.1016/s0899-3289(99)00009-7. [DOI] [PubMed] [Google Scholar]
- DeNavas-Walt C, Proctor BD, Smith JC. Current Population Reports : Consumer Income. United States Census Bureau and United States Department of Commerce; Washington, DC: 2008. Income, poverty, and health insurance coverage in the United States : 2007; pp. 1–71. [Google Scholar]
- Dohrenwend BP, Turner JB, Turse NA, Lewis-Fernandez R, Yager TJ. War-related posttraumatic stress disorder in Black, Hispanic, and majority White Vietnam veterans : the roles of exposure and vulnerability. Journal of Traumatic Stress. 2008;21:133–141. doi: 10.1002/jts.20327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis BH, MacDonald HZ, Lincoln AK, Cabral HJ. Mental health of Somali adolescent refugees : the role of trauma, stress, and perceived discrimination. Journal of Consulting and Clinical Psychology. 2008;76:184–193. doi: 10.1037/0022-006X.76.2.184. [DOI] [PubMed] [Google Scholar]
- Farley M, Patsalides BM. Physical symptoms, posttraumatic stress disorder and healthcare utilization of women with and without childhood physical and sexual abuse. Psychological Reports. 2001;89:595–606. doi: 10.2466/pr0.2001.89.3.595. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod R, Turner H, Hamby SL. The victimization of children and youth: a comprehensive, national survey. Child Maltreatment. 2005;10:5–25. doi: 10.1177/1077559504271287. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod RK, Turner HA. Re-victimization patterns in a national longitudinal sample of children and youth. Child Abuse and Neglect. 2007;31:479–502. doi: 10.1016/j.chiabu.2006.03.012. [DOI] [PubMed] [Google Scholar]
- Gavrilovic JJ, Schutzwohl M, Fazel M, Priebe S. Who seeks treatment after a traumatic event and who does not ? A review of findings on mental health service utilization. Journal of Traumatic Stress. 2005;18:595–605. doi: 10.1002/jts.20068. [DOI] [PubMed] [Google Scholar]
- Grant B, Dawson D, Hasin D. The Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM-IV Version. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2001. [Google Scholar]
- Grant B, Kaplan K. Source and Accuracy Statement for the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 2005. [Google Scholar]
- Hapke U, Schumann A, Rumpf HJ, John U, Meyer C. Post-traumatic stress disorder – the role of trauma, pre-existing psychiatric disorders, and gender. European Archives of Psychiatry and Clinical Neuroscience. 2006;256:299–306. doi: 10.1007/s00406-006-0654-6. [DOI] [PubMed] [Google Scholar]
- Harrell E. Bureau of Justice Statistics Special Report. United States Department of Justice, Office of Justice Programs; Washington, DC: 2007. Black victims of violent crime; pp. 1–12. [Google Scholar]
- Harrell E. Bureau of Justice Statistics Special Report. United States Department of Justice, Office of Justice Programs; Washington, DC: 2009. Asian, Native Hawaiian, and Pacific Islander victims of crime; pp. 1–8. [Google Scholar]
- Harris KM, Edlund MJ, Larson S. Racial and ethnic differences in the mental health problems and use of mental health care. Medical Care. 2005;43:775–784. doi: 10.1097/01.mlr.0000170405.66264.23. [DOI] [PubMed] [Google Scholar]
- Hasselberg M, Laflamme L, Weitoft GR. Socioeconomic differences in road traffic injuries during childhood and youth: a closer look at different kinds of road user. Journal of Epidemiology and Community Health. 2001;55:858–862. doi: 10.1136/jech.55.12.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatch SL, Dohrenwend BP. Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: a review of the research. American Journal of Community Psychology. 2007;40:313–332. doi: 10.1007/s10464-007-9134-z. [DOI] [PubMed] [Google Scholar]
- Himle JA, Baser RE, Taylor RJ, Campbell RD, Jackson JS. Anxiety disorders among African Americans, blacks of Caribbean descent, and non-Hispanic whites in the United States. Journal of Anxiety Disorders. 2009;23:578–590. doi: 10.1016/j.janxdis.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang ZJ, Wong FY, Ronzio CR, Yu SM. Depressive symptomatology and mental health help-seeking patterns of U.S.- and foreign-born mothers. Maternal and Child Health Journal. 2007;11:257–267. doi: 10.1007/s10995-006-0168-x. [DOI] [PubMed] [Google Scholar]
- Jayakody R, Danziger S, Kessler RC. Early-onset psychiatric disorders and male socioeconomic status. Social Science Research. 1998;27:371–387. [Google Scholar]
- Jaycox LH, Marshall GN, Schell T. Use of mental health services by men injured through community violence. Psychiatric Services. 2004;55:415–420. doi: 10.1176/appi.ps.55.4.415. [DOI] [PubMed] [Google Scholar]
- Johnson RL, Saha S, Arbelaez JJ, Beach MC, Cooper LA. Racial and ethnic differences in patient perceptions of bias and cultural competence in health care. Journal of General Internal Medicine. 2004;19:101–110. doi: 10.1111/j.1525-1497.2004.30262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC. Posttraumatic stress disorder : the burden to the individual and to society. Journal of Clinical Psychiatry. 2000;61:4–12. [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R. Mental health needs of crime victims : epidemiology and outcomes. Journal of Traumatic Stress. 2003;16:119–132. doi: 10.1023/A:1022891005388. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Fu QJ, Lyons MJ, Toomey R, Goldberg J, Eisen SA, True W, Ming T. Juvenile conduct disorder as a risk factor for trauma exposure and posttraumatic stress disorder. Journal of Traumatic Stress. 2005;18:23–32. doi: 10.1002/jts.20010. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Goodwin R, Struening E, Hellman F, Guardino M. Posttraumatic stress disorder and treatment seeking in a national screening sample. Journal of Traumatic Stress. 2003;16:5–16. doi: 10.1023/A:1022051009330. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Harley R, Lyons MJ, Wolfe J, Simpson JC, Goldberg J, Eisen SA, Tsuang M. A twin registry study of familial and individual risk factors for trauma exposure and posttraumatic stress disorder. Journal of Nervous and Mental Disease. 2002;190:209–218. doi: 10.1097/00005053-200204000-00001. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Moffitt TE, Poulton R, Martin J, Caspi A. Early childhood factors associated with the development of post-traumatic stress disorder : results from a longitudinal birth cohort. Psychological Medicine. 2007;37:181–192. doi: 10.1017/S0033291706009019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenen KC, Stellman SD, Sommer JF, Jr, Stellman JM. Persisting posttraumatic stress disorder symptoms and their relationship to functioning in Vietnam veterans : a 14-year follow-up. Journal of Traumatic Stress. 2008;21:49–57. doi: 10.1002/jts.20304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruijshaar ME, Barendregt J, Vos T, de Graaf R, Spijker J, Andrews G. Lifetime prevalence estimates of major depression : an indirect estimation method and a quantification of recall bias. European Journal of Epidemiology. 2005;20:103–111. doi: 10.1007/s10654-004-1009-0. [DOI] [PubMed] [Google Scholar]
- Kubzansky LD, Koenen KC, Jones C, Eaton WW. A prospective study of posttraumatic stress disorder symptoms and coronary heart disease in women. Health Psychology. 2009;28:125–130. doi: 10.1037/0278-6133.28.1.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubzansky LD, Koenen KC, Spiro A, 3rd, Vokonas PS, Sparrow D. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Archives of General Psychiatry. 2007;64:109–116. doi: 10.1001/archpsyc.64.1.109. [DOI] [PubMed] [Google Scholar]
- Lewis SF, Resnick HS, Ruggiero KJ, Smith DW, Kilpatrick DG, Best CL, Saunders BE. Assault, psychiatric diagnoses, and sociodemographic variables in relation to help-seeking behavior in a national sample of women. Journal of Traumatic Stress. 2005;18:97–105. doi: 10.1002/jts.20012. [DOI] [PubMed] [Google Scholar]
- Libby AM, Orton HD, Novins DK, Beals J, Manson SM. Childhood physical and sexual abuse and subsequent depressive and anxiety disorders for two American Indian tribes. Psychological Medicine. 2005;35:329–340. doi: 10.1017/s0033291704003599. [DOI] [PubMed] [Google Scholar]
- Loo CM. Race-related PTSD: the Asian American Vietnam veteran. Journal of Traumatic Stress. 1994;7:637–656. doi: 10.1007/BF02103012. [DOI] [PubMed] [Google Scholar]
- Loo CM, Fairbank JA, Chemtob CM. Adverse race-related events as a risk factor for posttraumatic stress disorder in Asian American Vietnam veterans. Journal of Nervous and Mental Disease. 2005;193:455–463. doi: 10.1097/01.nmd.0000168239.51714.e6. [DOI] [PubMed] [Google Scholar]
- Loo CM, Ueda SS, Morton RK. Group treatment for race-related stresses among minority Vietnam veterans. Transcultural Psychiatry. 2007;44:115–135. doi: 10.1177/1363461507074980. [DOI] [PubMed] [Google Scholar]
- Lu MC, Chen B. Racial and ethnic disparities in preterm birth : the role of stressful life events. American Journal of Obstetrics and Gynecology. 2004;191:691–699. doi: 10.1016/j.ajog.2004.04.018. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders ? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine. 2009 doi: 10.1017/S0033291709991036. Published online 1 September 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Epidemiologic Survey on Alcohol and Related Conditions. [Accessed 27 February 2008.];Wave 1 NESARC Data Notes. US government, National Institute on Alcohol Abuse and Alcoholism. 2004 http://niaaa.census.gov.
- Norris FH. Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. Journal of Consulting and Clinical Psychology. 1992;60:409–418. doi: 10.1037//0022-006x.60.3.409. [DOI] [PubMed] [Google Scholar]
- Ortega AN, Rosenheck R, Alegria M, Desai RA. Acculturation and the lifetime risk of psychiatric and substance use disorders among Hispanics. Journal of Nervous and Mental Disease. 2000;188:728–735. doi: 10.1097/00005053-200011000-00002. [DOI] [PubMed] [Google Scholar]
- Perkonigg A, Pfister H, Stein MB, Hofler M, Lieb R, Maercker A, Wittchen HU. Longitudinal course of posttraumatic stress disorder and posttraumatic stress disorder symptoms in a community sample of adolescents and young adults. American Journal of Psychiatry. 2005;162:1320–1327. doi: 10.1176/appi.ajp.162.7.1320. [DOI] [PubMed] [Google Scholar]
- Rand MR. Bureau of Justice Statistics Bulletin. United States Department of Justice, Office of Justice Programs; Washington, DC: 2008. National crime victimization survey: criminal victimization, 2007; pp. 1–12. [Google Scholar]
- Roberts AL, Austin SB, Corliss HL, Vandermorris AK, Koenen KC. Pervasive trauma exposure among US sexual orientation minority adults linked to posttraumatic stress disorder risk. American Journal of Public Health. doi: 10.2105/AJPH.2009.168971. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug and Alcohol Dependence. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai JT, Ho PM, Shore JH, Risk NK, Price RK. Asians in the United States : substance dependence and use of substance-dependence treatment. Journal of Substance Abuse Treatment. 2005;29:75–84. doi: 10.1016/j.jsat.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Sakai JT, Risk NK, Tanaka CA, Price RK. Conduct disorder among Asians and Native Hawaiian/Pacific Islanders in the USA. Psychological Medicine. 2008;38:1013–1025. doi: 10.1017/S0033291707001316. [DOI] [PubMed] [Google Scholar]
- Santos MR, Russo J, Aisenberg G, Uehara E, Ghesquiere A, Zatzick DF. Ethnic/racial diversity and posttraumatic distress in the acute care medical setting. Psychiatry. 2008;71:234–245. doi: 10.1521/psyc.2008.71.3.234. [DOI] [PubMed] [Google Scholar]
- Sawchuk CN, Roy-Byrne P, Goldberg J, Manson S, Noonan C, Beals J, Buchwald D. The relationship between post-traumatic stress disorder, depression and cardiovascular disease in an American Indian tribe. Psychological Medicine. 2005;35:1785–1794. doi: 10.1017/S0033291705005751. [DOI] [PubMed] [Google Scholar]
- Simpson TL. Women’s treatment utilization and its relationship to childhood sexual abuse history and lifetime PTSD. Substance Abuse. 2002;23:17–30. doi: 10.1080/08897070209511472. [DOI] [PubMed] [Google Scholar]
- Stoops N. Educational Attainment in The United States : 2003 Population Characteristics. United States Census Bureau and United States Department of Commerce; Washington, DC: 2004. pp. 1–10. [Google Scholar]
- Storr CL, Ialongo NS, Anthony JC, Breslau N. Childhood antecedents of exposure to traumatic events and posttraumatic stress disorder. American Journal of Psychiatry. 2007;164:119–125. doi: 10.1176/ajp.2007.164.1.119. [DOI] [PubMed] [Google Scholar]
- Ta VM, Juon HS, Gielen AC, Steinwachs D, Duggan A. Disparities in use of mental health and substance abuse services by Asian and Native Hawaiian/other Pacific Islander women. Journal of Behavioral Health Services and Research. 2008;35:20–36. doi: 10.1007/s11414-007-9078-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi DT, Zane N, Hong S, Chae DH, Gong F, Gee GC, Walton E, Sue S, Alegria M. Immigration-related factors and mental disorders among Asian Americans. American Journal of Public Health. 2007;97:84–90. doi: 10.2105/AJPH.2006.088401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd J, Armon C, Griggs A, Poole S, Berman S. Increased rates of morbidity, mortality, and charges for hospitalized children with public or no health insurance as compared with children with private insurance in Colorado and the United States. Pediatrics. 2006;118:577–585. doi: 10.1542/peds.2006-0162. [DOI] [PubMed] [Google Scholar]
- Ullman S, Brecklin L. Sexual assault history, PTSD, and mental health service seeking in a national sample of women. Journal of Community Psychology. 2002;30:261–279. [Google Scholar]
- Vogel LC, Marshall LL. PTSD symptoms and partner abuse: low income women at risk. Journal of Traumatic Stress. 2001;14:569–584. doi: 10.1023/A:1011116824613. [DOI] [PubMed] [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States : results from the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Williams DR, Jackson PB. Social sources of racial disparities in health. Health Affairs (Millwood) 2005;24:325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health : findings from community studies. American Journal of Public Health. 2008;98:S29–S37. doi: 10.2105/ajph.98.supplement_1.s29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamashiro G, Matsuoka JK. Help-seeking among Asian and Pacific Americans: a multiperspective analysis. Social Work. 1997;42:176–186. doi: 10.1093/sw/42.2.176. [DOI] [PubMed] [Google Scholar]
- Zayfert C, Dums AR, Ferguson RJ, Hegel MT. Health functioning impairments associated with posttraumatic stress disorder, anxiety disorders, and depression. Journal of Nervous and Mental Disease. 2002;190:233–240. doi: 10.1097/00005053-200204000-00004. [DOI] [PubMed] [Google Scholar]
- Zhai F, Gao Q. Child maltreatment among Asian Americans: characteristics and explanatory framework. Child Maltreatment. 2009;14:207–224. doi: 10.1177/1077559508326286. [DOI] [PubMed] [Google Scholar]