Abstract
Although concordance between husbands’ and wives’ mental health problems is often reported, questions remain about the nature of these relations. Extending research in this area, this study examined dynamic-longitudinal pathways among husbands’ and wives’ depressive symptoms and marital satisfaction as a moderator of associations. Participants were 296 heterosexual couples. Husbands and wives reported on their depressive symptoms and marital satisfaction. Results from dynamic bivariate latent difference score analyses indicated unidirectional longitudinal coupling such that higher levels of husbands’ depressive symptoms predicted subsequent elevations in wives’ depressive symptoms over time. This relation was stronger among couples reporting marital distress as compared to couples reporting higher marital satisfaction. The findings underscore the importance of considering one’s spouses’ depressive symptoms in treatment efforts.
Keywords: depression, dyadic or couple data, longitudinal method, marriage and close relationships
Although much attention has justifiably focused on the serious public heath concerns posed by clinical depression, subclinical depressive symptoms also pose a significant public health problem and have been repeatedly linked with impaired functioning across multiple domains (Greenberg et al., 2003; Judd, Paulus, Wells, & Rapaport, 1996; Kessler, Zhao, Blazer, & Swartz, 1997; Wells et al., 1989). For example, Judd et al. (1996) found similar levels of social impairment, including household and financial strain, restricted activity, and poor health status, among subsyndromal and clinically depressed participants. Subclinical problems are an especially common depressive condition in community samples (e.g., Judd, Akiskal, & Paulus, 1997) and are a risk factor for developing depression (e.g., Beach, Martin, Blum, & Roman, 1993; Broadhead, Blazer, George, & Tse, 1990; Horwath, Johnson, Klerman, & Weissman, 1992; Judd et al., 1998; Wells et al., 1989). Depressive symptoms before the onset of depression also characterize its longitudinal course (Fava, Grandi, Zielezny, Canestrari, & Morphy, 1994; Fava & Mangelli, 2001; Judd et al., 1996).
Concordance is often reported between husbands’ and wives’ depressive symptoms, suggesting that the marital relationship may be an important context for understanding the developmental course of depression (Joiner & Katz, 1999; Kiecolt-Glaser & Newton, 2001; Meyler, Stimpson, & Peek, 2007; Rehman, Gollan, & Mortimer, 2008). The positive relation between spouses’ depression has been referred to as depression contagion (Joiner & Katz) and stems from the interactional theory of depression proposed by Coyne (1976). The interactional theory of depression posits that depressed individuals simultaneously seek excessive reassurance and negative feedback from those close to them; that is, people with depressive symptoms seek reassurance yet doubt the sincerity of it. Although those close to people with depressive symptoms may at first respond with support, over time they may become increasingly frustrated and respond in less supportive ways. Further, Coyne posited that this cycle of excessive reassurance and negative feedback elicits negative affect in those close to individuals with depressive symptoms. Thus, in elucidating the processes that may account for the concordance of depressive symptoms among spouses, or depression contagion, Coyne’s theory implies that interactions and communication between people with depressive symptoms and their partners may be a mechanism by which depressive symptoms in one spouse are related to their partners’ symptoms. In a meta-analysis, Joiner and Katz found evidence for depression contagion among different types of close partner relationships, including dating couples and spouses. Notably, evidence was stronger for the contagion of depressive symptoms than general negative affect.
A central tenant of Coyne’s (1976) theory is that the relation between spouses’ symptoms is transactional and occurs over time. Previous studies on the relationship between spouses’ depressive symptoms, however, have typically been based on cross-sectional data, which report positive correlations among husbands’ and wives’ concurrent levels of depressive symptoms (Galbaud du Fort, Kovess, & Boivin, 1994; Hippisley-Cox, Coupland, Pringle, Crown, & Hammersley, 2002; Tower & Kasl, 1995). When longitudinal studies are conducted, typically only two waves of data are used to predict one’s depressive symptoms from his or her partner’s depression at an earlier point in time (e.g., Siegel, Bradley, Gallo, & Kasl, 2004; Tower & Kasl, 1996). Few longitudinal studies with more than two occasions of measurement have been conducted, and most have been with older couples (e.g., Holahan et al., 2007; Townsend, Miller, & Guo, 2001). Holahan et al. (2007) assessed spouses’ depressive symptoms four times over a 10-year period. Controlling for changes in depressive symptoms as a function of time, results from hierarchical linear models indicated that husbands’ and wives’ depressive symptoms were positively related over time. Butterworth and Rodgers (2006) reported similar findings among couples during the first 5 years of marriage.
A limitation of previous research, therefore, is scant longitudinal study of relations among depressive symptoms in spouses and limitations of data analytic techniques to assess whether one’s depressive symptoms predict changes in his or her partner’s symptoms over time, as implied by the phenomena of depression contagion and Coyne’s (1976) theory. Further, longitudinal research is necessary in order to tease apart whether observed concordance between spouses’ symptoms is simply attributable to assortative mating or whether there is in fact a dynamic-transactional relation between spouses’ mental health (Segrin, 2004; see also van Orden & Joiner, 2006).
Another gap in this literature is investigation of which couples are most likely to experience depression contagion (Joiner & Katz, 1999). Although the marital relationship provides a context for understanding the association between spouses’ mental health symptoms, the specific role that marital processes play in this association depends on the particular marital processes being examined. Whereas some theoretical perspectives underscore marital interactions and communication as a possible mechanism linking spouses’ depressive symptoms (i.e., mediator), other marital processes, such as marital satisfaction or the quality of the marital relationship, are supported in the literature as moderators of this relationship (Larson & Almeida, 1999). That is, empirical evidence supports the role of marital quality as a moderator of the relationship between spouses’ symptoms, although the impact of marital quality on the strength and direction of this association has differed across studies.
For example, Tower and Kasl (1996) found that marital closeness was a significant moderator, such that ones’ depressive symptoms were more strongly linked with his or her partner’s depressive symptoms for couples in which both partners felt close to each other (e.g., feeling close and intimate, depending on partner for emotional support). Other studies, however, have suggested that the relation between spouses’ symptoms is stronger for couples with lower levels of marital satisfaction as compared to couples reporting higher marital satisfaction (e.g., Yorgason, Almeida, Neupert, Spiro, & Hoffman, 2006). That is, individuals with lower levels of marital satisfaction and whose partner has high levels of depressive symptoms would experience higher levels of depressive symptoms compared to individuals with higher levels of marital satisfaction. For example, Hammen et al. (1995) found that women experiencing a negative life event were more likely to be depressed when they felt they did not have anyone they could depend on, suggesting that high marital quality may buffer woman from developing depressive symptoms, whereas low marital quality may place woman at greater risk for experiencing depressive symptoms. Indirect support for marital satisfaction as a moderator also comes from studies and theoretical perspectives on the transmission of negative emotions (Larson & Almeida, 1999). Margolin (1981) found that couples with lower marital satisfaction showed greater negative reciprocity during daily interactions compared to couples with higher marital satisfaction. Overall, however, few studies have examined marital processes as moderators of the longitudinal association between spouses’ depressive symptoms, underscoring the need for research in this area (Joiner & Katz, 1999). Thus, given the relative lack of longitudinal study, uncertainty exists about the possible role of marital satisfaction as a moderator of these relations.
The present study advances research on the concordance among spouses’ mental health problems by uniquely examining dynamic-longitudinal relations between husbands’ and wives’ depressive symptoms. Although theoretical perspectives on depression in the context of interpersonal relationships posit a transactional association between partners’ symptoms, there have been no direct tests of how husbands’ and wives’ symptoms are dynamically related over time. Instead, husbands’ and wives’ depressive symptoms are treated as two separate, but correlated, processes. Notably, spouses may represent a coupled dynamic system (Berg & Upchurch, 2007; Schoebi, 2008), such that changes in one’s symptoms are partly a function of his or her partner’s level of symptoms. For example, valuable information about how or why wives’ depressive symptoms change may be provided by how their partner changes over time. Using dynamic factor models, we simultaneously examined (1) linear and proportional change in depressive symptoms among husbands and wives and (2) whether changes in husbands’ and wives’ symptoms over time were predicted by their partners’ previous level of symptoms. It was hypothesized that there would be significant dynamic-longitudinal relations between husbands’ and wives’ symptoms such that higher levels of depressive symptoms would predict subsequent elevations in one’s spouse’s symptoms over time. Examining whether or how spouses’ symptoms are dynamically related over time may have important clinical implications for developing and refining treatment efforts when dealing with depression among married adults.
Taking into the account the marital context of depression, we also tested marital satisfaction as a moderator of the longitudinal association between spouses’ depressive symptoms. We hypothesized that among couples with low marital satisfaction, the positive association between partners’ depressive symptoms over time would be stronger compared to couples with higher levels of marital satisfaction. Understanding marital processes that may strengthen or weaken the longitudinal association between partners’ depressive symptoms has implications for which couples would most benefit from specific treatment and prevention efforts.
Method
Participants
Participants for this study were 296 heterosexual couples living in a small city in the Midwest recruited to participate in a 3-year prospective longitudinal study on family processes and child development. Participants were recruited from the community through flyers, newspapers, television, and radio advertisements, community events, and letters distributed to local schools and neighborhood residents. To be eligible to participate, couples had to be living together for at least 2 years and have a child between the ages of 8 and 16 (M = 11.12, SD = 2.31, 155 boys). The majority of couples were married (97%, M = 12.37 years), and a small percentage (3.4%) included unmarried cohabiting couples. Given the small percentage of cohabiting couples, we use the terms “spouses” and “husbands and wives” in the present study for the sake of parsimony. On average, couples had been living together for 13 years (SD = 6.02). Husbands’ and wives’ mean ages at the beginning of the study were 40.22 (SD = 37.84, range = 25–70) and 37.84 (SD = 5.97, range = 24–70) years, respectively. The sample was predominantly European American (87%; 8.5% African-American, 1% Hispanic, and 3.5% biracial), with a median household income in the $40,000 to $65,000 range, and was representative of the geographic area from which families were recruited (see Cummings, Schermerhorn, Davies, Goeke-Morey, & Cummings, 2006). The attrition rate from the first to third time point was 16%. Couples that dropped from our study did not significantly differ from participating couples with regard to age, income, ethnicity, years living together, Time 1 depressive symptom scores, or reported marital distress (MAT scores <100) at Time 1. Participating couples, however, were more likely to be married at Time 1 compared to couples who dropped from the study, χ2 (df = 1, N = 296) = 8.70, p < .05.
Procedures
Families visited the university laboratory yearly for 3 years to complete measures. Participants provided informed consent, and the study procedures met the approval of the university’s institutional review board. Only the measures pertinent to the present study are discussed. Couples completed self-report measures about their depressive symptoms and marital satisfaction in separate rooms. Families received monetary compensation for their participation: $100 at Time 1, $120 at Time 2, and $140 at Time 3; a subset of families were paid $200 at Time 2 and 3 for completing additional measures and tasks.
Measures
Depressive symptoms
Husbands and wives completed the Symptom Checklist 90-Revised (SCL-90-R; Derogatis, 1994). The Depression Subscale was used in the current study and contains 13 items. Participants rated how much a list of problems (e.g., feeling hopeless about the future, feeling no interest in things) had bothered or distressed them during the past week on a 5-point Likert scale, ranging from 0 (not at all) to 4 (extremely). Items were averaged to create a depressive symptoms score, with higher scores reflecting higher levels of depressive symptoms. As a reference point, scores of .52 for males and .76 for females correspond to a T score of 60, which would indicate borderline-clinical levels of symptoms. Mean levels of depressive symptoms in our sample were comparable to levels reported in other community samples (e.g., Cummings, El-Sheikh, Kouros, & Keller, 2007). The reliability of this scale for husbands’ and wives’ reports was high across all three time points (Cronbach’s αrange = .85–.91).
Marital satisfaction
Husbands and wives provided self-reports of marital satisfaction on the Marital Adjustment Test (MAT; Locke & Wallace, 1959), which contains 15 items that are differentially weighted (e.g., “Do you ever wish you had not married?” rated on a 4-point scale from frequently to never). The MAT is widely used, has good concurrent and predictive validity, and reliably distinguishes between distressed and nondistressed couples (O’Leary & Turkewitz, 1978). Higher scores on this measure reflect a more well-adjusted relationship and greater satisfaction, whereas scores below 100 reflect marital distress. Husbands’ and wives’ average level of reported marital satisfaction at Time 1 was 109.60 (SD = 22.78) and 112.09 (SD = 25.31), respectively. Levels of marital satisfaction in this study were similar to those reported in other studies with community samples (e.g., Lawrence et al., 2008; South, Turkheimer, & Oltmanns, 2008). Reliability of husbands’ and wives’ reports in this sample were acceptable (Cronbach’s α = .70 and .77, respectively).
Results
Preliminary Results
Means, standard deviations, and bivariate correlations between husbands’ and wives’ depressive symptoms scores are presented in Table 1. Examining the mean scores, both husbands’ and wives’ depressive symptom scores decreased over time, and spouses’ depressive symptom scores were positively correlated at each time point. Marital satisfaction was inversely correlated with depressive symptom scores across the study period (mean r = −.29, range = −.18 to −.41, all p < .05). Participants’ age, ethnicity, number of children, and the number of years couples had been living together were not significantly related to depressive symptoms. Couples’ combined yearly income was significantly correlated with wives’ depressive symptoms at Time 1, r = −.16, p < .05, and Time 2, r = −.21, p < .05. Additionally, husbands’ and wives’ education levels were associated with husbands’ Time 1 depressive symptoms and wives’ Times 2 and 3 depressive symptoms, respectively. Although unmarried cohabiting couples comprised only a small percentage of our total sample, cohabiting couples reported higher levels of depressive symptoms and marital dissatisfaction at Time 1 compared to married couples. Therefore, we controlled for marital status, income, and education level in our analyses.
Table 1.
Means, Standard Deviations, and Bivariate Correlations Among Husbands’ and Wives’ Depressive Symptoms
| Depressive Symptom Scores | M | SD | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|---|
| Time 1 | ||||||||
| 1. Husbands | .45 | .48 | — | |||||
| 2. Wives | .64 | .63 | .17** | — | ||||
| Time 2 | ||||||||
| 3. Husbands | .41 | .39 | .62** | .12 | — | |||
| 4. Wives | .60 | .61 | .19** | .75** | .33** | — | ||
| Time 3 | ||||||||
| 5. Husbands | .38 | .42 | .53** | .05 | .59** | .16* | — | |
| 6. Wives | .57 | .55 | .17** | .54** | .10 | .60** | .19** | — |
Note: N = 296 (Time 1) to 248 (Time 3).
p < .05.
p < .01.
Analysis Plan
To address the main study question regarding dynamic-longitudinal relations between spouses’ depressive symptoms, a dynamic bivariate latent difference score (LDS) model was fit (McArdle & Hamagami, 2001), controlling for the relation between husbands’ and wives’ initial levels of marital satisfaction, and their respective starting levels of depressive symptoms. LDS models, an extension of latent growth curve models, incorporate features of cross-lagged regression models and allow one to model longitudinal coupling between two processes. In the context of analyses examining dynamic associations, longitudinal coupling represents that two variables simultaneously predict change in each other over time. An advantage of LDS models is that all available data are utilized, so cases with missing data are not excluded.
As a first step to building our model, observed depressive symptom scores were used to create latent change scores (see Hawley, Ho, Zuroff, & Blatt, 2006, or Sbarra & Allen, 2009, for detailed explanation and example). Second, we predicted latent change in depressive symptoms from (1) a constant slope (i.e., systematic change that occurs as a function of time), (2) one’s level of depressive symptoms at the previous time point (i.e., proportional coefficient/self-feedback), and (3) some proportion of one’s spouse’s depressive symptoms from the previous time point (i.e., longitudinal coupling). Latent changes in husbands’ and wives’ depressive symptoms were simultaneously modeled. Thus,
In the above equations, S represents a linear slope. A significant γ parameter would indicate longitudinal coupling or that husbands’ and wives’ depressive symptoms predict latent change in their partners’ depressive symptoms over time. If one γ parameter is significant, that would represent unidirectional longitudinal coupling, and if neither γ parameter is significant, that would indicate that husbands’ and wives’ depressive symptoms scores are not dynamically related. The H and W subscripts in the equations above denote husband and wife, respectively, and represent that the magnitude and direction of the slope, proportional, and coupling parameters may differ for husbands and wives. Also, the proportional and coupling parameters were modeled as time-invariant parameters (e.g., coupling between husbands’ and wives’ symptoms same across time).
Are Husbands’ and Wives’ Depressive Symptoms Dynamically Related Over Time?
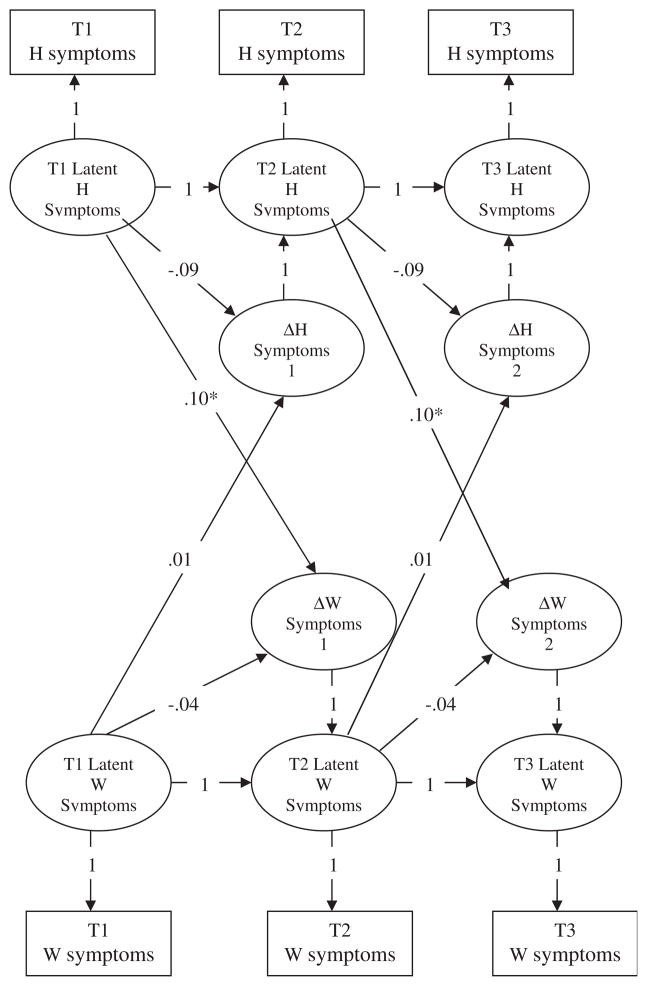
Results from the bivariate LDS model are presented in Table 2, and the parameter estimates of particular interest (proportional and coupling parameters) are depicted in Figure 1. The model provided a good fit to the sample data, χ2(df = 37, N = 296) = 63.82, χ2/df = 1.73, CFI = .97, RMSEA = .05 (90% CI: .03–.07). Evidence for unidirectional longitudinal coupling was found: Wives’ latent change in depressive symptoms over time was predicted by their husbands’ previous level of depressive symptoms, and this effect was positive. That is, higher levels of husbands’ depressive symptoms predicted subsequent elevations in wives’ symptoms over time. Longitudinal coupling was not found with regard to husbands’ latent change in symptoms on the basis of wives’ previous level of depressive symptoms.
Table 2.
Results From Bivariate Latent Difference Score Model Examining Longitudinal Coupling Between Husbands’ and Wives’ Depressive Symptoms
| Parameter Estimates | Depressive Symptoms
|
|
|---|---|---|
| Husbands | Wives | |
| Intercept | ||
| Mean | .47 (.03)** | .64 (.04)** |
| Variance | .16 (.02)** | .32 (.04)** |
| Slope | ||
| Mean | .02 (.04) | −.04 (.05) |
| Variance | .01 (.01)* | .02 (.01)** |
| Proportional coefficient | ||
| β | −.12 (.08) | −.04 (.07) |
| Coupling coefficient | ||
| γ | .00 (.03) | .10 (.05)* |
| Fit indices | ||
| χ2 | 63.82 | |
| df | 37 | |
| χ2/df | 1.73 | |
| CFI | .97 | |
| RMSEA (90% CI) | .05 (.03–.07) | |
Note. Unstandardized parameter estimates are presented with the standard error in parentheses.
p < .05.
p < .01.
Figure 1.
Dynamic Bivariate Latent Difference Score Model Examining Longitudinal Coupling Between Husbands’ and Wives’ Depressive Symptoms.
Note. Unstandardized parameter estimates are presented. Analyses controlled for initial levels of marital satisfaction, marital status, income, and education level (not depicted in the model). H and W denote husband and wife, respectively. ΔSymptoms 1 represents latent change score from Time 1 to Time 2 and ΔSymptoms 2 represents the latent change from Time 2 to Time 3. Given the graphical complexity of this model, the following parameters were estimated but not included in the model: intercept and slope of latent difference scores, error variances and covariances between husbands’ and wives’ error variances within the same time point, covariances between husbands’ and wives’ respective intercepts and slopes, and the covariance between husbands’ and wives’ slopes.
*p < .05.
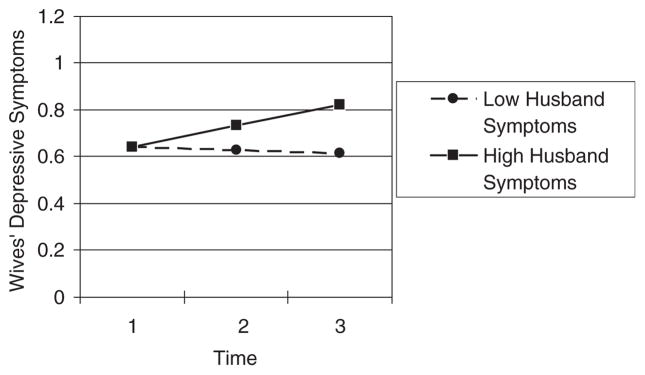
Taken together, these parameter estimates can be substituted into the above LDS equations to determine the expected change in husbands’ and wives’ symptoms over the study period, on the basis of different initial levels of husbands’ and wives’ depressive symptoms (Figure 2). The expected change in depressive symptoms among wives with mean levels of depressive symptoms and whose husbands had high levels of depressive symptoms at the beginning of the study (scores 1 SD above the mean) was .19 points on the SCL-90-R over a 2-year period. In contrast, the expected change among wives whose husbands had lower levels of depressive symptoms at the beginning of the study (scores 1 SD below the mean) was .02 points.
Figure 2.
Expected Change in Depressive Symptoms Among Wives.
Note. The expected change is plotted on the basis of average levels of depressive symptoms at Time 1 among wives. Low Husband Symptoms = expected change for wives whose husbands’ depressive symptom scores were 1 SD below the mean at Time 1. High Husband Symptoms = expected change for wives whose husbands’ depressive symptom scores were 1 SD above the mean at Time 1.
Does Marital Satisfaction Moderate the Dynamic Relation Between Husbands’ and Wives’ Depressive Symptoms?
Next, we examined whether marital satisfaction moderated the dynamic association between husbands’ and wives’ depressive symptoms. Specifically, multigroup bivariate latent difference score models were fit to examine whether the dynamic relation (i.e., coupling parameters) differed for couples reporting marital distress compared to couples who reported themselves as maritally satisfied. Two groups were created: (1) couples were classified in a “maritally distressed” group (n = 118) if either the husband or wife reported being maritally distressed at Time 1 (score <100 on MAT), and (2) couples were classified in a “maritally satisfied” group (n = 178) if neither the husband nor wife reported being maritally distressed (score ≥ 100 on MAT).
Multigroup analyses compare a series of increasingly restricted models to determine whether constraining parameters to be equivalent across groups provides a better fit to the sample data compared to a model in which parameters are allowed to differ between groups (e.g., Hawley, Ho, Zuroff, & Blatt, 2007). The chi-square difference test can be used to compare two nested models. A nonsignificant chi-square difference test would indicate that the constrained parameter(s) is equivalent across groups (i.e., parameter invariance or equivalence), whereas a significant chi-square difference test would indicate that the parameter(s) differs between groups.
We first established measurement invariance by comparing a model in which all parameters were freely estimated to a model in which the measurement residuals for husbands’ and wives’ symptom scores and the covariance between husbands’ and wives’ residuals were constrained to be equal across groups, Δχ2(3) = 7.67, p = .06.
Next, holding these constraints in place, we tested a series of models that increasingly placed constraints on the parameters between groups to test for invariance in the remaining parameters. If the chi-square difference test was not significant, these constraints were held as additional constraints were placed on the model. The final model included parameter equivalence in (1) the proportional coefficient for wives (βW), (2) the coupling parameter representing the association between wives’ depressive symptoms and change in husbands’ symptoms over time (γH), and (3) the average slope for wives (SW). The final model provided an acceptable fit to the sample data, χ2 (df = 66, N = 296) = 106.73, χ2/df = 1.62, CFI = .94, RMSEA = .05. Estimates of the parameters for both groups are presented in Table 3. Of particular interest in the present study, group differences were found in the dynamic association between husbands’ depressive symptoms and change in their wives’ symptoms. That is, husbands’ depressive symptoms were associated with change in wives’ symptoms for maritally distressed couples, γ = .25, SE = .07, p < .01, but not for couples who were maritally satisfied.
Table 3.
Results From Final Multigroup Bivariate Latent Difference Score Model Examining Longitudinal Relations Between Husbands’ and Wives’ Depressive Symptoms as Moderated by Marital Satisfaction
| Parameter Estimates | Maritally Distressed Group (MAT Score <100)
|
Maritally Satisfied Group (MAT Score ≥ 100)
|
||
|---|---|---|---|---|
| Husbands | Wives | Husbands | Wives | |
| Intercept | ||||
| Mean | .37 (.03)** | .46 (.04)** | .61 (.06)** | .90 (.07)** |
| Variance | .09 (.02)** | .14 (.02)** | .27 (.05)** | .47 (.08)** |
| Slope | ||||
| Mean | −.03 (.03) | −.01 (.03)a | .17 (.05)** | −.01 (.03)a |
| Variance | .00 (.004) | .01 (.01) | .04 (.01)** | .03 (.01)* |
| Proportional coefficient | ||||
| β | .02 (.07) | −.12 (.04)**b | −.45 (.07)** | −.12 (.04)**b |
| Coupling coefficient | ||||
| γ | .00 (.03)c | .23 (.06)** | .00 (.03)c | .09 (.05) |
Note. Unstandardized parameter estimates are presented with the standard error in parentheses. Similar subscripts denote parameters that were constrained to be equal between groups. MAT = Marital Adjustment Test.
p < .05.
p < .01.
Considering all parameters together (and substituting the parameter estimates into the LDS equations presented above), the results indicated that, for maritally distressed couples, higher levels of husbands’ symptoms at Time 1 (scores 1 SD above the mean) were related to elevated levels of wives’ depressive symptoms over the study period (.24-point increase on SCL-90-R score), whereas lower levels of husbands’ symptoms at Time 1 (scores 1 SD below the mean) were related to a decrease in symptoms (.08-point decrease in SCL-90-R score over 2 years). For couples who are maritally satisfied, however, wives’ symptoms were expected to decrease by .15 points on the SCL-90-R over 2 years regardless of husbands’ level of symptoms at Time 1. With regard to changes in symptoms for the average husband, the findings indicated that, for couples that are maritally satisfied, husbands’ depressive symptoms decreased (.03 points on SCL-90-R over 2 years), whereas husbands’ symptoms were stable for couples who reported being maritally distressed.
Discussion
Consistent with theoretical perspectives on these relations (e.g., depression contagion, interactional theory of depression), this study found evidence for dynamic-longitudinal relations between husbands’ and wives’ depressive symptoms. We expected that there would be significant longitudinal coupling among husbands’ and wives’ symptoms, and this was partially supported. Higher levels of husbands’ depressive symptoms predicted subsequent elevations in wives’ symptoms over time. This association was stronger for couples that reported being maritally distressed as compared to couples that reported being maritally satisfied. Of importance, given the relatively low levels of depressive symptoms in this sample, the results highlight that symptoms do not have to reach clinical levels before one’s spouse’s mental health is affected.
The findings support the notion that marital satisfaction buffers individuals from depressive symptomatology. One interpretation is that a relationship characterized by low marital quality reflects that one’s spouse is less available as a source of social support for dealing with ones’ own or his or her partner’s symptoms, thereby maintaining or exacerbating the positive relation between spouses’ depressive symptoms over time. Moos and colleagues found that individuals with supportive families engaged in more adaptive coping strategies when faced with stressors that may buffer them from mental and physical illness (Fondacaro & Moos, 1989; Holahan, Moos, & Bonin, 1999). On the other hand, results are not consistent on these relations. For example, Tower and Kasl (1996) found that spouses’ symptoms were more strongly related among couples with higher levels of marital closeness. Notably, many people with a depressed spouse do not develop depressive symptoms; therefore, future studies on the variables that moderate the association between spouses’ symptoms over time in order to determine which couples are most vulnerable to experiencing depressive symptoms in the context of their partners’ symptoms are clearly warranted.
Although husbands’ symptoms were associated with elevations in wives’ symptoms over time, wives’ symptoms were not significantly associated with changes in husbands’ symptoms. Gender differences in the association between changes in spouses’ symptoms over time are consistent with past studies suggesting marital processes are more strongly related to wives’ mental health as compared to husbands (see Kiecolt-Glaser & Newton, 2001). Stimpson, Peek, and Markides (2006), for example, found that whereas husbands’ depression significantly predicted wives’ well-being (e.g., self-esteem, social support, life satisfaction), wives’ depression was not strongly associated with their husbands’ well-being. In addition, in a meta-analysis of marriage and physical health, Kiecolt-Glaser and Newton found that marital processes were more closely linked with wives’ physiological functioning as compared to husbands. Larson and Almeida (1999) also noted that husbands’ negative emotions better predict wives’ negative emotions, whereas the transmission of negative emotions from wives to husbands is less robust.
Several alternative explanations merit consideration. Cross and Madson (1997) have proposed that women are more relationally interdependent such that their representations of themselves develop in the context of close relationships. Thus, women may be more attuned to disruptions in their interpersonal relationships in this regard, as compared to men. Second, women are more likely to express and seek help for depression (e.g., Bertakis et al., 2001; Brommelhoff, Conway, Merikangas, & Levy, 2004) such that woman’s depressive symptoms may be viewed by husbands as a more normative process, whereas men’s depressive symptoms may be viewed as atypical and therefore may promote greater reactions from wives that disrupt the relationship and wives’ mental health. Third, and relatedly, Du Rocher Schudlich, Papp, and Cummings (2004) found that husbands’ depressive symptoms were related to less productive and more angry conflict expressions between partners, even after controlling for marital satisfaction. Thus, depressive symptoms among husbands constitute greater disruptions to the marital dyad than wives’ depressive symptoms, contributing to elevations in wives’ symptoms over time.
Findings regarding gender differences in the relation between marriage and health, however, are inconsistent in the literature on close relationships. In the health psychology literature, marital status has been linked to better health among men as compared to women (see Kiecolt-Glaser & Newton, 2001). Further, several studies report no gender difference between marital functioning and health (see Kiecolt-Glaser & Newton). With respect to depression contagion, Joiner and Katz (1999) found no gender differences in the transmission of depression. They also noted, however, that few studies have explicitly examined gender differences in the context of the association between depressive symptoms among spouses. This underscores the need for future work on gender differences to further our understanding of how the impact of spouses’ symptoms may differ for men as compared to women.
This study advances our knowledge of depression among spouses by further articulating how one’s spouse’s symptoms contribute to one’s mental health trajectory. Although the phenomenon of depression contagion has been supported, recent studies have raised further questions about whether this process is truly evident in close relationships (e.g., Segrin, 2004). The current study adds to the case for this phenomenon in relationships by showing that spouses’ symptoms are transactionally related over time. Moreover, the results suggested that concordance among spouses’ symptoms over time is not simply because of assortative mating, that is, that people with similar levels of depressive symptoms are more likely to date or get married. The current study met multiple criteria for teasing apart whether associations can be accounted for by assortative mating, including employing a longitudinal design, controlling for partner similarity at Time 1, and showing how partners’ symptoms predict changes in each others’ symptoms over and above the changes one would expect in symptoms over time (Segrin; van Orden & Joiner, 2006). Moreover, the current study advanced support for examining mental health trajectories in the context of close interpersonal relationships (Rehman et al., 2008).
With regard to clinical implications, support is indicated for the utility of couples therapy for the treatment of depression, particularly among wives. If husbands’ and wives’ symptoms contribute to changes in, or maintenance of, their partner’s symptoms, treating both partners may be more effective in alleviating their symptoms. For example, couples therapy may be integrated into one’s current treatment program (Whisman & Uebelacker, 1999). Additionally, the moderating role of marital satisfaction suggests that couples with low levels of marital satisfaction may most benefit from couples therapy compared to couples who are maritally satisfied. The results also suggest that programs aimed at preventing depression may be best targeted toward couples with low levels of marital satisfaction.
Several limitations merit consideration. First, although the findings highlight the importance of examining subsyndromal levels of depression, these findings may not generalize to couples with clinical levels of depression or those experiencing other mental health problems (e.g., anxiety). Second, the current study did not employ a random sample of couples, which may limit the generalizability of findings. There are inevitable trade-offs between conducting data-intensive research and obtaining optimal representativeness in sampling. Given the constraints of recruiting families into a data-intensive research design, our recruitment strategy endeavored to obtain a sample that matched as closely as possible the demographic characteristics of the county. Supporting the effectiveness of this effort, the average levels of depressive symptoms and marital satisfaction in this study were comparable to other studies with different community samples (e.g., Cummings et al., 2007; Lawrence et al., 2008; South et al., 2008). Third, and related to the previous point, participating couples were more likely to be married at Time 1 compared to couples who dropped from the study, suggesting a possible limitation of the generalizability of the findings to unmarried cohabiting couples. Fourth, the observed relations between husbands’ depressive symptoms and elevations in wives’ symptoms over time may be attributable to a third variable not assessed in this study. For example, husbands with high levels of depressive symptoms may become aggressive or use maladaptive coping strategies such as alcohol and substance use (Brownhill, Wilhelm, Barclay, & Schmeid, 2005; Murphy, 1998), and these destructive behaviors may be linked with elevations in wives’ symptoms.
Notably, although the current study focused on the association between spouses’ depressive symptoms, conversely, these findings also imply that spouses’ positive health is related over time as well. That is, stating our findings in reverse, the current study also shows that low levels of husbands’ depressive symptoms predicted decreases in wives’ symptoms over time. Greater understanding of how spouses contribute to and promote positive health and well-being in each other is an important direction for future research. Finally, with regard to the terms depression contagion and transmission of depressive symptoms, theoretical perspectives do no assume that depressive symptoms in one person just elicit symptoms in their partner; rather there are mechanisms that account for this association. Although extant theoretical models have posited that the communication and interaction patterns of spouses may underlie this link, few investigations of the processes by which spouses’ health becomes interrelated over time have been undertaken. Thus, further examining how and why spouses’ symptoms place their partners at increased risk for depression remains an important next step for research in this area.
Acknowledgments
This research was funded in part by National Institute of Child Health and Human Development Grant R01HD36261 awarded to E. Mark Cummings and a Ruth L. Kirschstein National Research Service Award from the National Institute of Mental Health (F31MH080529) to Chrystyna D. Kouros. Dr. Kouros was supported by an NIMH training grant (T32-MH18921, Vanderbilt University) during preparation of this article.
References
- Beach SRH, Martin JD, Blum TC, Roman PM. Subclinical depression and role fulfillment in domestic settings: Spurious relationships, imagined problems, or real effects? Journal of Psychopathology and Behavior Assessment. 1993;15:113–128. [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Bertakis KD, Helms LJ, Callahan EJ, Azari EJ, Leigh R, Robbins JA. Patient gender differences in the diagnosis of depression in primary care. Journal of Women’s Health and Gender Based Medicine. 2001;10:689–698. doi: 10.1089/15246090152563579. [DOI] [PubMed] [Google Scholar]
- Broadhead WE, Blazer DG, George LK, Tse LK. Depression, disability days and days lost from work in a prospective epidemiologic survey. Journal of the American Medical Association. 1990;264:2524–2528. [PubMed] [Google Scholar]
- Brommelhoff JA, Conway K, Merikangas K, Levy BR. Higher rates of depression in women: Role of gender bias within the family. Journal of Women’s Health. 2004;13:69–76. doi: 10.1089/154099904322836474. [DOI] [PubMed] [Google Scholar]
- Brownhill S, Wilhelm K, Barclay L, Schmeid V. “Big build”: Hidden depression in men. Australian and New Zealand Journal of Psychiatry. 2005;39:921–931. doi: 10.1080/j.1440-1614.2005.01665.x. [DOI] [PubMed] [Google Scholar]
- Butterworth P, Rodgers B. Concordance in the mental health of spouses: Analysis of a large national household panel survey. Psychological Medicine. 2006;36:685–697. doi: 10.1017/S0033291705006677. [DOI] [PubMed] [Google Scholar]
- Coyne JC. Toward an interactional description of depression. Psychiatry. 1976;39:28–40. doi: 10.1080/00332747.1976.11023874. [DOI] [PubMed] [Google Scholar]
- Cross SE, Madson L. Models of the self: Self-construals and gender. Psychological Bulletin. 1997;122:5–37. doi: 10.1037/0033-2909.122.1.5. [DOI] [PubMed] [Google Scholar]
- Cummings EM, El-Sheikh M, Kouros CD, Keller PS. Children’ skin conductance reactivity as a mechanism of risk in the context of parental depressive symptoms. Journal of Child Psychiatry and Psychology. 2007;48:436–445. doi: 10.1111/j.1469-7610.2006.01713.x. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Schermerhorn AC, Davies PT, Goeke-Morey MC, Cummings JS. Interparental discord and child adjustment: Prospective investigations of emotional security as an explanatory mechanism. Child Development. 2006;77:132–152. doi: 10.1111/j.1467-8624.2006.00861.x. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. SCL-90-R: Administration, scoring and procedures manual. Minneapolis, MN: Author; 1994. [Google Scholar]
- Du Rocher Schudlich TD, Papp LM, Cummings EM. Relations of husbands’ and wives’ dysphoria to marital conflict resolution strategies. Journal of Family Psychology. 2004;18:171–183. doi: 10.1037/0893-3200.18.1.171. [DOI] [PubMed] [Google Scholar]
- Fava GA, Grandi S, Zielezny M, Canestrari R, Morphy MA. Cognitive behavioral treatment of residual symptoms in primary major depressive disorder. American Journal of Psychiatry. 1994;151:1295–1299. doi: 10.1176/ajp.151.9.1295. [DOI] [PubMed] [Google Scholar]
- Fava GA, Mangelli L. Assessment of subclinical symptoms and psychological well-being in depression. European Archives of Psychiatry and Clinical Neuroscience. 2001;251:47–52. doi: 10.1007/BF03035127. [DOI] [PubMed] [Google Scholar]
- Fondacaro M, Moos RH. Life stressors and coping: A longitudinal analysis among depressed and nondepressed adults. Journal of Community Psychology. 1989;17:330–340. doi: 10.1002/1520-6629(198910)17:4<330::AID-JCOP2290170406>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- Galbaud du Fort GG, Kovess V, Boivin JF. Spouse similarity for psychological distress and well-being: A population study. Psychological Medicine. 1994;24:431–447. doi: 10.1017/s0033291700027409. [DOI] [PubMed] [Google Scholar]
- Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, et al. The economic burden of depression in the United States: How did it change between 1990 and 2000? Journal of Clinical Psychiatry. 2003;64:1465–1475. doi: 10.4088/jcp.v64n1211. [DOI] [PubMed] [Google Scholar]
- Hammen CL, Burge D, Daley SE, Davila J, Paley B, Rudolph KD. Interpersonal attachment cognitions and prediction of systematic responses to interpersonal stress. Journal of Abnormal Psychology. 1995;104:436–443. [PubMed] [Google Scholar]
- Hawley LL, Ho RMH, Zuroff DC, Blatt SJ. The relationship between perfectionism, depression, and therapeutic alliance during treatment for depression: Latent different score analyses. Journal of Consulting and Clinical Psychology. 2006;74:930–942. doi: 10.1037/0022-006X.74.5.930. [DOI] [PubMed] [Google Scholar]
- Hawley LL, Ho RMM, Zuroff DC, Blatt SJ. Stress reactivity following brief treatment for depression: Differential effects of psychotherapy and medication. Journal of Consulting and Clinical Psychology. 2007;75:244–256. doi: 10.1037/0022-006X.75.2.244. [DOI] [PubMed] [Google Scholar]
- Hippisley-Cox J, Coupland C, Pringle M, Crown N, Hammersley V. Married couples’ risk of same disease: Cross sectional study. British Medical Journal. 2002;325:636–640. doi: 10.1136/bmj.325.7365.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Bonin LA. Social context and depression: An integrative stress and coping framework. In: Joiner T, Coyne JC, editors. The interactional nature of depression. Washington, DC: American Psychological Association; 1999. pp. 39–66. [Google Scholar]
- Holahan CJ, Moos RH, Moerkbak ML, Cronkite RC, Holahan CK, Kenney BA. Spousal similarity in coping and depressive symptoms over 10 years. Journal of Family Psychology. 2007;21:551–559. doi: 10.1037/0893-3200.21.4.551. [DOI] [PubMed] [Google Scholar]
- Horwath E, Johnson J, Klerman GL, Weissman MM. Depressive symptoms as relative and attributable risk factors for first-onset major depression. Archives of General Psychiatry. 1992;49:817–823. doi: 10.1001/archpsyc.1992.01820100061011. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Katz J. Contagion of depressive symptoms and mood: Meta-analytic review and explanations from cognitive, behavioral, and interpersonal viewpoints. Clinical Psychology: Science and Practice. 1999;6:149–164. [Google Scholar]
- Judd LL, Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, et al. Major depressive disorder: A prospective study of residual subthreshold depressive symptoms as predictors of rapid relapse. Journal of Affective Disorder. 1998;50:97–108. doi: 10.1016/s0165-0327(98)00138-4. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Paulus MP. The role and clinical significance of subsyndromal depressive symptoms (SSD) in unipolar major depressive disorder. Journal of Affective Disorders. 1997;45:5–18. doi: 10.1016/s0165-0327(97)00055-4. [DOI] [PubMed] [Google Scholar]
- Judd LL, Paulus KB, Wells MH, Rapaport MH. Socioeconomic burden of subsyndromal depressive symptoms and major depression in a sample of the general population. American Journal of Psychiatry. 1996;153:1411–1417. doi: 10.1176/ajp.153.11.1411. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Zhao S, Blazer DG, Swartz M. Prevalence, correlates, and course of minor depression and major depression in the National Comorbidity Survey. Journal of Affective Disorders. 1997;45:19–30. doi: 10.1016/s0165-0327(97)00056-6. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychological Bulletin. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Larson R, Almeida DM. Emotional transmission in the daily lives of families: A new paradigm for studying family process. Journal of Marriage and the Family. 1999;61:5–20. [Google Scholar]
- Lawrence E, Pederson A, Bunde M, Barry RA, Brock RL, Fazio E, et al. Objective ratings of relationship skills across multiple domains as predictors of marital satisfaction trajectories. Journal of Social and Personal Relationships. 2008;25:445–466. doi: 10.1177/0265407508090868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke HL, Wallace K. Short marital-adjustment and prediction tests: Their reliability and validity. Marriage and Family Living. 1959;21:251–255. [Google Scholar]
- Margolin G. Behavior exchange in happy and unhappy marriages: A family cycle perspective. Behavior Therapy. 1981;12:329–343. [Google Scholar]
- McArdle JJ, Hamagami F. Latent difference score structural models for linear dynamic analyses with incomplete longitudinal data. In: Collins LM, Sayer AG, editors. New methods for the analysis of change. Washington, DC: American Psychological Association; 2001. pp. 139–175. [Google Scholar]
- Meyler D, Stimpson JP, Peek MK. Health concordance within couples: A systematic review. Social Science and Medicine. 2007;64:2297–2310. doi: 10.1016/j.socscimed.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Murphy GE. Why women are less likely than men to commit suicide. Comprehensive Psychiatry. 1998;39:165–175. doi: 10.1016/s0010-440x(98)90057-8. [DOI] [PubMed] [Google Scholar]
- O’Leary KD, Turkewitz H. Marital therapy from a behavioral perspective. In: Paolino TJ, McCrady BC, editors. Marriage and marital therapy: Psychoanalytic, behavioral, and systems theory perspectives. Oxford, England: Brunner/Mazel; 1978. pp. 240–297. [Google Scholar]
- Rehman US, Gollan J, Mortimer AR. The marital context of depression: Research, limitations, and new directions. Clinical Psychology Review. 2008;28:179–198. doi: 10.1016/j.cpr.2007.04.007. [DOI] [PubMed] [Google Scholar]
- Sbarra DA, Allen JJB. Decomposing depression: On the prospective and reciprocal dynamics of mood and sleep disturbances. Journal of Abnormal Psychology. 2009;118:171–182. doi: 10.1037/a0014375. [DOI] [PubMed] [Google Scholar]
- Schoebi D. The contagion of daily affect in marital relationships. Journal of Family Psychology. 2008;22:595–604. doi: 10.1037/0893-3200.22.3.595. [DOI] [PubMed] [Google Scholar]
- Segrin C. Concordance of negative emotion in close relationships: Transmission of emotion or assortative mating? Journal of Social and Clinical Psychology. 2004;23:836–856. [Google Scholar]
- Siegel MJ, Bradley EH, Gallo WT, Kasl SV. The effect of spouse mental and physical health on husbands’ and wives’ depressive symptoms, among older adults: Longitudinal evidence from the Health and Retirement Survey. Journal of Aging and Health. 2004;16:398–425. doi: 10.1177/0898264304264208. [DOI] [PubMed] [Google Scholar]
- Stimpson JP, Peek MK, Markides KS. Depression and mental health among older Mexican American spouses. Aging and Mental Health. 2006;10:386–393. doi: 10.1080/13607860500410060. [DOI] [PubMed] [Google Scholar]
- South SC, Turkheimer E, Oltmanns TF. Personality disorder symptoms and marital functioning. Journal of Consulting and Clinical Psychology. 2008;76:769–780. doi: 10.1037/a0013346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tower RB, Kasl SV. Depressive symptoms across older spouses and the moderating effect of marital closeness. Psychology and Aging. 1995;10:625–638. doi: 10.1037//0882-7974.10.4.625. [DOI] [PubMed] [Google Scholar]
- Tower RB, Kasl SV. Depressive symptoms across older spouses: Longitudinal influences. Psychology and Aging. 1996;11:683–697. doi: 10.1037//0882-7974.11.4.683. [DOI] [PubMed] [Google Scholar]
- Townsend AL, Miller B, Guo SY. Depressive symptomatology in middle-age and older married couples: A dyadic analysis. Journals of Gerontology: Psychological Sciences and Social Sciences. 2001;56:S352–S364. doi: 10.1093/geronb/56.6.s352. [DOI] [PubMed] [Google Scholar]
- van Orden KA, Joiner TE. A role for the contagion of emotion? A comment on Segrin (2004) Journal of Social and Clinical Psychology. 2006;25:825–832. [Google Scholar]
- Wells KB, Stewart A, Hays RD, Burman MA, Rogers W, Daniels M, et al. The functioning and well-being of depressed patients. Results from the Medical Outcomes Study. Journal of the American Medical Association. 1989;262:914–919. [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA. Integrating couple therapy with individual therapies and antidepressant medications in the treatment of depression. Clinical Psychology: Science and Practice. 1999;6:415–429. [Google Scholar]
- Yorgason JB, Almeida D, Nuepert SD, Spiro A, Hoffman L. A dyadic examination of daily health symptoms and emotional well-being in late-life couples. Family Relations. 2006;55:613–624. [Google Scholar]