Abstract
Objective
The direct measurement of the ability to perform physical tasks yields information about factors contributing to poor function and insights into strategies for preventing disability. Our goal was to evaluate the relationship of walking speed and balance tests with specific radiographic features of knee and ankle osteoarthritis (OA).
Methods
A timed eight foot walk and a standing balance test were performed by 138 participants of a longitudinal observational study of knee OA progression. Radiographic features of OA severity, joint space narrowing (JSN, a surrogate for cartilage loss) and osteophyte formation (OST), were assessed for the knee and ankle. The association of these performance measures with radiographic OA was evaluated using correlation analysis, adjusted for age, gender, BMI, and number of comorbidities.
Results
Knee and ankle JSN, but not OST, was negatively associated with specific performance tests: walking speed was associated with knee JSN (Spearman rho= −0.20, p=0.02) and balance was associated with ankle (subtalar joint) JSN (Spearman rho= −0.22, p=0.01). These relationships remained significant upon further control for knee and ankle pain.
Conclusions
Structural joint damage due to OA (JSN in contrast to OST) negatively impacted specific domains of physical performance. These results indicate that targeting specific joints for specific functional outcomes may be indicated, and suggest that prevention of cartilage damage in these joints is a sensible target for OA disease modification to prevent disability.
Keywords: osteoarthritis, physical performance, knee, ankle
INTRODUCTION
Osteoarthritis (OA) is the most common cause of disability in the Western World. It is estimated that symptomatic OA affects 12% of those over the age of 60 in the United States [1]. The impact of severe OA on personal well being has been reported to rival that of congestive heart failure and end stage renal disease [2, 3]. Additionally, OA exacts a staggering toll on the US economy and is estimated to raise medical care expenditures by $185.5 billion annually [4]. A clear understanding of the impact of OA on physical function is critical for the development and targeting of effective interventions to the appropriate joint sites and impairments, and forms the basis of the rationale for this study whose objective was to assess the association between radiographic OA of the knee and ankle and standardized physical performance tests of gait and balance that have been linked previously to disability and mortality outcomes [1, 2].
Although previous studies have found the ankle to be an important modifier of physical function [3–7], they have failed to assess the severity of ankle OA, quantified radiographically, and its association with physical performance tests. Although the Framingham study suggested that radiographic knee OA is an independent marker of disability [8, 9], physical function was assessed by self-report rather than by physical performance tests that can provide information not available from self-report items, particularly for higher functioning elderly adults with no self-reported disability [2]. Moreover, to our knowledge, studies evaluating the association of knee OA and physical function have utilized the global Kellgren–Lawrence (KL) grading of radiographic OA but not individual radiographic features of OA of joint space narrowing (JSN) and osteophyte (OST) that likely represent different pathologic processes in OA [10]. In this substudy of the Prediction of OA Progression (POP) cohort we evaluated the association of lower extremity disability, measured by walking 8-ft (2.4 meters) at a normal pace, and standing balance ability, with radiographic knee and ankle OA based on KL grade, JSN and OST severity.
SUBJECTS AND METHODS
Subjects
All data for this cross-sectional analysis were derived from the three-year follow-up assessment of the 138 participants (101 females, 37 males) who returned (of the original 159 participants) for re-evaluation in the NIH-funded Prediction of Osteoarthritis (POP) study (further described in [11, 12]). At entry, participants had radiographic OA (Kellgren Lawrence grade >1) [13] and met the American College of Rheumatology criteria for symptomatic knee OA. By the time of follow-up, a total of 26 individuals had undergone total knee arthroplasty (4 individuals bilateral), 7 individuals had total hip arthroplasty, 1 had bilateral ankle arthrodesis and 1 unilateral subtalar/talonavicular arthrodesis; there were no individuals with ankle arthroplasty.
Participants were excluded on the basis of inflammatory joint diseases, endocrinopathies, Paget's disease, neuropathic disorders, avascular necrosis, use of corticosteroids within the prior 3 months, and knee arthroscopy within the prior six months. Comorbidities were reported by participant selection of physician diagnosed diseases from a list that included the following: asthma, cancer, elevated lipids/cholesterol, dementia, depression, diabetes, heart disease, hypertension, kidney disease, liver, osteoporosis, Parkinson’s disease, stroke, thyroid disease, and depression. Knee symptoms were ascertained by the National Health and Nutrition Examination Survey I criterion [14] of pain, aching or stiffness on most days of any one month in the past year; for subjects answering yes, symptoms were quantified as mild, moderate, or severe yielding a total score of 0–3 for each joint. Ankle symptoms were ascertained by summing pain scores graded from a homunculus of the ankles that included grading of the following ankle joint sites: medial and lateral tibia and medial and lateral talus (each graded 0–3. All study procedures were approved by the Duke Institutional Review Board.
Radiographic Imaging
Knee radiographs
Posteroanterior fixed-flexion weight-bearing knee radiographs were obtained with the SynaFlexer™ lower limb positioning frame (Synarc, San Francisco) and a ten degree caudal x-ray beam angle [16]. Each knee radiograph was scored by 2 graders (VBK and GM), for Kellgren Lawrence grade (0–4), and individual radiographic features of OA of JSN (0–3) and OST (0–3) scored for the medial and lateral compartments using the OARSI standardized atlas [15]. JSN scores of 0–6 were possible for each knee and OST scores of 0–12 were possible as all four margins on the knee joint were scored. For analyses of the association of radiographic knee OA with walking and balance measures, the right and left knee radiographic scores for each feature were summed. A total of 29% of knee radiographs were reread, blinded to the original grading, and intraclass correlation coefficients (ICCs) were determined. JSN ICCs were highest (0.86) followed by OST (0.84). Knee radiograph ICCs were lowest for KL grade (0.69).
Ankle radiographs
Individual weight-bearing ankle radiographs were performed with equal distribution of weight on both legs without footwear and 10° internal rotation of the foot/ankle (Mortise view). Lateral weight-bearing ankle radiographs were obtained individually with the beam centered on the medial aspect of the joint with the foot/ankle in 15° external rotation. Ankle radiographs were scored by a musculoskeletal radiologist (JBR) for KL grade (0–4), JSN (0–3) and OST (0–3) using the OARSI standardized atlas for knee OA as a surrogate [15]. The mortise radiograph permitted grading of OA features of the medial and lateral aspects of the tibiotalar joint (TTJ) and the lateral radiograph permitted grading of OA features of the anterior and posterior aspects of the TTJ joint. Therefore, for the TTJ, joint space narrowing scores were derived from the mortise view and osteophyte scores were derived by summing the scores from both the mortise and lateral views. OA features of the ankle subtalar joint (STJ) were viewed exclusively on lateral ankle radiographs (See Figure 1). For each ankle, possible scores were as follows: for the TTJ 0–6 for JSN, and 0–24 for OST; for STJ 0–6 for both JSN and OST. For analyses of the association of radiographic ankle OA, gait speed and balance, the right and left ankle radiographic scores were summed for each feature and for each joint site (TTJ and STJ). A total of 22% of ankle radiographs were reread, blinded to the original grading, and intraclass correlation coefficients (ICCs) were determined. JSN ICCs were highest (0.97) followed by KL (0.93). Ankle radiograph ICCs were lowest for OST (0.90).
Figure 1.
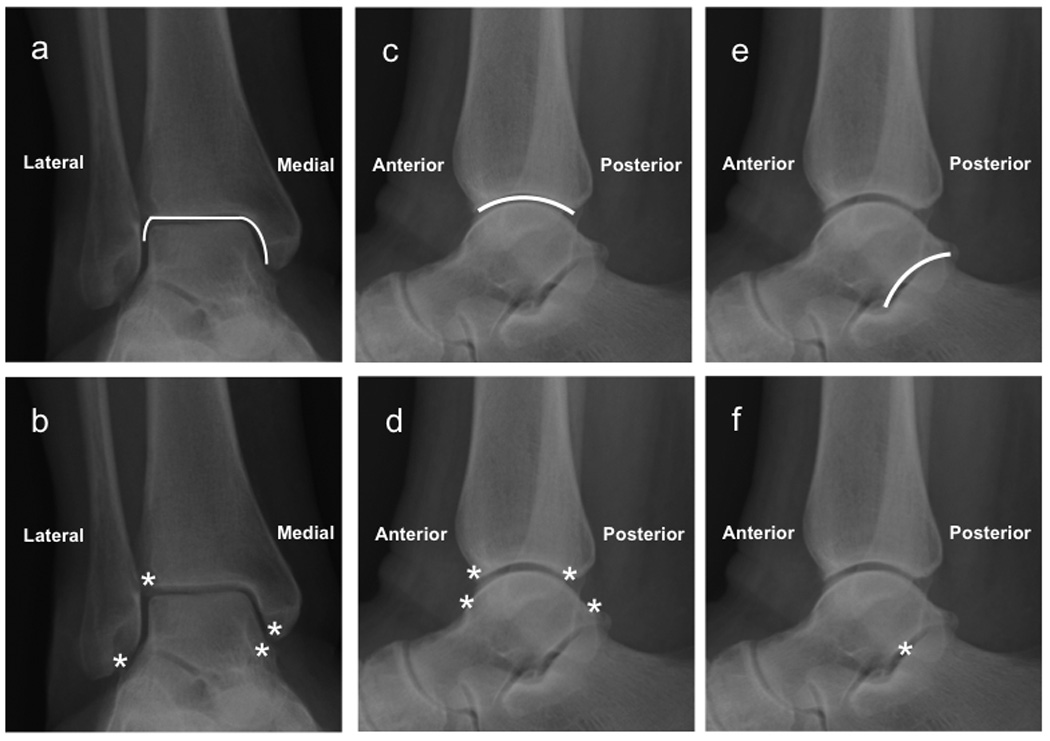
Representative radiographs demonstrating the views used to score OA features of the ankle for joint space narrowing (JSN - solid lines in top panel), and osteophyte (OST - asterisks in bottom panel). Images a – d: ankle tibiotalar joint - TTJ; e – f: ankle subtalar joint - STJ.
Assessment of physical function
Lower-extremity physical function was measured by the following two tests that have demonstrated associations with disability and mortality outcomes [1, 2]: walking 8-ft (2.4 meters) at a normal pace, and standing balance. The test-retest reliability of these measures is high [1] as demonstrated by correlations between observers of more than 0.93 for walking speed [16], and test–retest correlations of more than 0.89 for walking speed [16] and 0.97 for balance [17]. For the timed walk, participants in normal footwear were positioned at the beginning of an 8-ft (2.4-m) course and asked to walk at their normal pace until told to stop. The time taken to travel the 8-ft course was measured with a stopwatch. The process was repeated and the fastest of the two times was used in the analyses. In our study, for evaluation of association with features of radiographic OA, results of the 8-ft walk were converted to a gait velocity in meters per second (m/s). Standing balance was measured with the feet side by side, then in semi-tandem stance (heel of one foot in front and beside the big toe of the other foot), and then in tandem stance (heel of one foot directly in front of the other foot); each stance was held for up to 10 seconds. These test results were converted to scores (range 0 to 4). Higher scores represent better function and a score of 0 represents the inability to complete the test. Subjects were given a score of 1 if they could hold a side-by-side standing position for 10 seconds but were unable to hold a semi-tandem position for 10 seconds, a score of 2 if they could hold a semi-tandem position for 10 seconds but were unable to hold a full tandem position for more than 2 seconds, a score of 3 if they could stand in the full tandem position for 3 to 9 seconds, and a score of 4 if they could stand in the full tandem position for 10 seconds.
Statistical Analyses
Non-parametric Spearman correlation analysis was used to assess the strength of association between radiographic features of knee and ankle OA (JSN and OST) with the two types of physical performance tests. The correlations were conducted in a sequential manner to explore the effect of possible modifier and mediator variables. As a first step, crude (unadjusted) correlations were conducted between the radiographic measures and each of the performance tests. Next, partial correlations were generated by adjusting for age, BMI, numbers of comorbidities (aside from arthritis), and gender. Finally, the additional effects of knee and ankle self-reported pain were added to the above set of adjusted variables. In this way, we were able to explore how key potential confounders were affecting the relationship between radiographic features of OA and function. P values < 0.05 were considered significant. All analyses were performed using SAS software v9.1 (Cary, NC).
RESULTS
A total of 138 participants were evaluated representing 246 non-replaced knees and 276 ankles. The cohort consisted of 73% women, 27% men; mean age was 66 (SD 11.6) years (range 37 – 86) and BMI 31.3 (SD 6.9). The cohort was characterized by a mean of two comorbidities and six painful joint sites at the time of evaluation.
Knee and ankle radiographic OA status
By design, all participants had radiographic knee OA Kellgren Lawrence grade >1 of at least one knee with knee Kellgren Lawrence sum scores ranging from 1 to 8. To assess the impact of joint OA on physical performance, we graded radiographic features of JSN and OST respectively of the knee and ankle. As expected, the prevalence of any knee radiographic features (JSN or OST) in participants was high (86% and 92% respectively). Interestingly, radiographic ankle OA was prevalent in this knee OA cohort, demonstrated by the frequency of ankles (58%) with minimal OA (Kellgren Lawrence grade ≥ 1 scores) observed in 92% of participants; and definite OA (KL grade ≥ 2) in 15% of ankles corresponding to 22% of participants. The highest prevalence of radiographic OA of the ankle in participants was observed for the ankle TTJ (86% with any OST). A full description of the OA radiographic scores and prevalence for the knee and ankle in this cohort is provided in Table 1.
Table 1.
Knee and ankle radiographic scores in the Prediction of Osteoarthritis Progression (POP) cohort.
| Joint Site | OA Feature |
Range (Possible Score) |
Range (Actual Sum Score) |
Median | Grade > 1 n (%) |
|
|---|---|---|---|---|---|---|
| JSN | 0 –12 | 0 – 9 | 3.0 | 127 (92%) | ||
| Knee | OST | 0 – 24 | 0 – 22 | 6.0 | 119 (86%) | |
| KL | 0 – 8 | 0 – 8 | 4.0 | 133 (96%) | ||
| Ankle | TTJ | JSN | 0 – 12 | 0 – 7 | 0 | 20 (15%) |
| Ankle | STJ | JSN | 0 – 6 | 0 – 6 | 0 | 15 (11%) |
| Ankle | TTJ | OST | 0 – 48 | 0 – 27 | 3.0 | 119 (86%) |
| Ankle | STJ | OST | 0 – 6 | 0 – 5 | 0 | 58 (42%) |
| Ankle | TTJ | KL | 0 – 8 | 0 – 8 | 2.0 | 126 (91%) |
TTJ=Tibiotalar joint (ankle); STJ=Subtalar joint (ankle); JSN=joint space narrowing severity; OST=osteophyte severity; KL=Kellgren Lawrence grade. Higher scores represent increasingly severe radiographic OA
Physical performance associations with radiographic OA
The mean (SD) gait velocity was 0.99 m/sec (0.25). The mean balance score was 3.14 (1.29). Gait velocity was significantly reduced with increasing number of comorbidities, gender, and knee and ankle pain (Table 2), and borderline negatively associated with age (p=0.05). Balance was strongly negatively associated with age (p <0.0001) and BMI was negatively associated with gait velocity, but this latter association was not significant. Based on these findings, age, gender, BMI and numbers of comorbidities were used as control variables in analyses evaluating the association of radiographic OA and function. Subsequent models additionally controlled for knee and ankle pain in an effort to understand the role of structural impairment versus symptoms on physical function.
Table 2.
Associations of demographics and joint pain with physical performance measures.
| Gait Velocity (m/sec) (higher better) |
Standing Balance (higher better) |
|
|---|---|---|
| Spearman Correlation Coefficients r, p values | ||
| Age | −0.17, 0.05 | −0.47, <0.0001 |
| BMI | −0.14, 0.10 | 0.01, 0.86 |
| Number of Comorbidities | −0.20, 0.02 | −0.05, 0.53 |
| Gender | −0.23, 0.006 | −0.06, 0.47 |
| Knee Pain | −0.30, 0.0004 | −0.09, 0.31 |
| Ankle Pain | −0.25, 0.0027 | −0.09, 0.31 |
BMI=body mass index
Knee and ankle radiographic OA were both associated with impaired physical function, but these different joint sites differentially impacted specific domains of function (Table 3). In models controlling for age, gender, BMI and numbers of comorbidities, gait velocity was significantly negatively associated with severity of OA based on knee JSN, and showed a similar but non-significant trend with knee OST. These relationships did not change with additional control for knee and ankle pain (r = −0.19, p = 0.03; r = −0.16, p = 0.07 respectively) suggesting that structural impairment of the knee decreases gait speed. In models controlling for age, gender, BMI and numbers of comorbidities, balance was negatively associated with severity of ankle OA based on JSN of the subtalar joints, but not OST. This association was still significant after additional control for knee and ankle pain (r = −0.19, p = 0.03), suggesting that structural impairment of the ankle negatively impacts balance.
Table 3.
Associations of knee and ankle osteoarthritis with physical performance measures (unadjusted and adjusted for age, gender, BMI, number of comorbidities).
| Joint Site | OA Feature |
Gait Velocity (higher better) |
Standing Balance (higher better) |
|
|---|---|---|---|---|
| r*, p unadjusted; (r, p adjusted for age, BMI, comorbidities, and gender); [r, p adjusted for age, BMI, comorbidities, gender, knee and ankle pain] |
||||
| Knee | JSN |
−0.19,0.02 (−0.20,0.02) [−0.19,0.03] |
−0.04,0.62 (−0.03, 0.72) [−0.02,0.81] |
|
| OST | −0.16,0.07 (−0.16,0.06) [−0.16,0.07] |
−0.01,0.91 (−0.01,0.88) [−0.01,0.92] |
||
| KL | −0.12,0.16 (−0.12,0.16) [−0.12,0.16] |
−0.02,0.80 (−0.01,0.88) [−0.02,0.86] |
||
| Ankle | TTJ | JSN | −0.06,0.45 (0.02,0.79) [0.08,0.37] |
−0.15,0.08 (−0.05,0.56) [−0.02,0.83} |
| Ankle | STJ | JSN | −0.13,0.12 (−0.09,0.28) [−0.05,0.56] |
−0.29,0.0006 (−0.22, 0.01) [−0.19,0.03] |
| Ankle | TTJ | OST | 0.03,0.69 (0.06,0.50) [0.05,0.58] |
−0.03,0.72 (0.01,0.96) [−0.002,0.98] |
| Ankle | STJ | OST | −0.03,0.74 (−0.16,0.06) [0.02,0.80] |
−0.10,0.23 (−0.01,0.88) [−0.01,0.87] |
| Ankle | TTJ | KL | −0.10,0.27 (−0.04,0.68) [−0.01,0.96] |
−0.19,0.02 (−0.12,0.16) [−0.10,0.24] |
| *r=Spearman Correlation Coefficients | ||||
TTJ=Tibiotalar joint (ankle); STJ=Subtalar joint (ankle); JSN=joint space narrowing severity; OST=osteophyte severity; KL=Kellgren Lawrence grade.
DISCUSSION
To our knowledge this is the first study describing a relationship between individual physical performance tests (gait velocity and standing balance) and a specific radiographic feature (JSN) of knee and ankle OA. In the large EPESE study, both self-reported function and performance tests of gait and balance were independent predictors of short-term mortality and nursing home admission [2]. However the performance tests provided information not available from self-report items, namely, for the higher functioning elderly adults with no self-reported disability at baseline, the base-line performance tests were associated with a statistically significant, graduated increase in the frequency of disability in the activities of daily living and mobility-related disability at four-year follow-up [1, 2] (relative risk 4.8, 95% CIs 2.4 – 9.6, for subjects with the poorest scores on the baseline tests of walking and balance as compared with relative risk 1.9, 95% CIs 1.2 – 2.9, for those with the best scores) [1]. Gait velocity and standing balance tests can be readily incorporated into large research studies. They require little time, expense, personnel, or equipment, and can be performed by elders with moderate to severe disability. The data from our study, linking JSN to performance tests and thereby to clinically meaningful disability-related outcomes, suggest that prevention of cartilage damage in these joints is a sensible target for OA disease modification to prevent disability.
Previous studies evaluating knee OA and physical performance have utilized the Kellgren Lawrence grading scale, a metric that does not distinguish between the individual radiographic features of JSN and OST that reflect different pathological processes. Past studies of balance have also failed to account for the co-occurrence of knee and ankle radiographic OA. The availability of knee and ankle radiographs in the POP cohort permitted both to be evaluated with respect to physical function. We discovered that ankle OA negatively impacted balance and that knee OA slowed gait. Our study also demonstrated that radiographic JSN of the knee and ankle rather than osteophytes, was associated with functional impairment. In addition, KL grades of the knee and ankle failed to show significant association with gait speed or balance tests in models controlling for age, gender, BMI and numbers of comorbidities, and pain. Others have noted that the Kellgren-Lawrence (KL) grading system is driven primarily by osteophyte size [18] and this may explain the inferior performance of KL relative to specific assessment of JSN in our analyses. Debate regarding limitations and strengths of the KL grading system is not new and will likely continue [19]. Our results demonstrate the utility of assessment of specific radiographic features of OA (JSN and OST), as they provided disease related insights with respect to function over those provided by sole use of the traditional global KL grade.
Balance is a multifactorial task requiring the processing of sensory information (vision, proprioception, and vestibular function) and the subsequent coordinated neuromuscular response expressed as ankle and knee strength. We found that the scores for the balance tests were associated with ankle subtalar (STJ) JSN on radiograph. Previous investigators have reported an association between balance and ankle strength [3, 5–7], however, radiographic ankle OA was not assessed in these studies, perhaps based upon the perception that non-traumatic ankle OA is a rare entity [20]. A number of studies have demonstrated a negative association between balance and radiographic knee OA [21–23]. Jaedelis et al. reported that in the presence of knee pain, the best measure of dynamic balance during forward and backward lean was a combination of strong knees and strong ankles, each independently accounting for 18%, and collectively 22% of the variability in dynamic balance. This model also predicted that knee OA patients with weak knee strength could still maintain high levels of dynamic balance by having strong ankle strength [3]. In our study, balance was not associated with radiographic features of knee OA or knee Kellgren Lawrence grade. Of note, the associations of balance and ankle OA in our cohort were independent of joint pain and BMI, two factors shown in the past to be associated with balance. Associations of reduced gait velocity with degenerative changes in the knee have previously been reported. Astephen et al. stratified a cohort according to knee symptoms, expectant arthroplasty, and the presence and absence of OA, and found that gait speed decreased incrementally with increased severity of knee OA [4].
The cycle of frailty is an emerging hypothesis describing a series of interrelated pathways leading to functional decline in the elderly [24, 25]. Importantly, balance and walking disabilities lie within these pathways and represent opportunities for early intervention. Numerous creative interventions are currently available for lower extremity disability and include progressive resistance training, yoga, Tai Chi, knee bracing, subtalar and talonavicular joint strapping, aqua training, proper footwear, and orthotics. Efforts are ongoing to determine the most efficacious combination of these modalities.
Limitations of this study include the modest overall size of our cohort and the higher prevalence of mild, relative to moderate or severe ankle OA, and the modest, albeit statistically significant correlations of knee and ankle JSN with physical performance. In summary, this pilot substudy has demonstrated that structural joint damage due to OA (JSN in contrast to OST) negatively impacted specific domains of physical performance. These results indicate that targeting specific joints for specific functional outcomes may be indicated. We recommend further study of radiographic OA in these several lower extremity joints for their utility in research protocols and as potential targets for early intervention to prevent disability.
ACKNOWLEDGEMENTS
We wish to thank Dr. Carl Pieper, Duke University Medical Center Department of Biostatistics and Bioinformatics, for his assistance in the analysis and interpretation of data.
This study was supported by the National Institute on Aging at the National Institutes of Health (Claude D. Pepper Older Americans Independence Centers 5P30 AG028716): National Institute of Arthritis and Musculoskeletal and Skin Diseases at the National Institutes of Health (RO1 AR48769): and the National Center for Research Resources at the National Institutes of Health (MO1-RR-30), supporting the Duke General Clinical Research Unit where this study was conducted.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
AUTHORS' CONTRIBUTIONS
"I declare that I participated in this study and that my specific contribution is listed by my name, and I have seen and approved the final version."
Virginia B Kraus: Principal Investigator supervising all aspects of the study and manuscript preparation; I have had full access to all the data in the study and final responsibility for the decision to submit it for publication.
Gary McDaniel: Involved in data acquisition, data analysis and manuscript preparation.
Jordan B. Renner: Involved in scoring of ankle radiographs for osteoarthritis severity, and manuscript preparation.
Richard Sloane: Involved in statistical analyses and manuscript preparation.
CONFLICT OF INTEREST STATEMENTS
Virginia B Kraus: no conflicts
Gary McDaniel: no conflicts
Jordan B. Renner: no conflicts
Richard Sloane: no conflicts
REFERENCES
- 1.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 3.Jadelis K, Miller ME, Ettinger WH, Jr, Messier SP. Strength, balance, and the modifying effects of obesity and knee pain: results from the Observational Arthritis Study in Seniors (oasis) J Am Geriatr Soc. 2001;49:884–891. doi: 10.1046/j.1532-5415.2001.49178.x. [DOI] [PubMed] [Google Scholar]
- 4.Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ. Biomechanical changes at the hip, knee, and ankle joints during gait are associated with knee osteoarthritis severity. J Orthop Res. 2008;26:332–341. doi: 10.1002/jor.20496. [DOI] [PubMed] [Google Scholar]
- 5.Messier SP, Glasser JL, Ettinger WH, Jr, Craven TE, Miller ME. Declines in strength and balance in older adults with chronic knee pain: a 30-month longitudinal, observational study. Arthritis Rheum. 2002;47:141–148. doi: 10.1002/art.10339. [DOI] [PubMed] [Google Scholar]
- 6.Studenski S, Duncan PW, Chandler J. Postural responses and effector factors in persons with unexplained falls: results and methodologic issues. J Am Geriatr Soc. 1991;39:229–234. doi: 10.1111/j.1532-5415.1991.tb01642.x. [DOI] [PubMed] [Google Scholar]
- 7.Whipple RH, Wolfson LI, Amerman PM. The relationship of knee and ankle weakness to falls in nursing home residents: an isokinetic study. J Am Geriatr Soc. 1987;35:13–20. doi: 10.1111/j.1532-5415.1987.tb01313.x. [DOI] [PubMed] [Google Scholar]
- 8.Guccione AA, Felson DT, Anderson JJ. Defining arthritis and measuring functional status in elders: methodological issues in the study of disease and physical disability. Am J Public Health. 1990;80:945–949. doi: 10.2105/ajph.80.8.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48:3359–3370. doi: 10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- 10.Kraus VB, Kepler TB, Stabler T, Renner J, Jordan J. First qualification study of serum biomarkers as indicators of total body burden of osteoarthritis. PLoS One. 2010;5:e9739. doi: 10.1371/journal.pone.0009739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Addison S, Coleman RE, Feng S, McDaniel G, Kraus VB. Whole-body bone scintigraphy provides a measure of the total-body burden of osteoarthritis for the purpose of systemic biomarker validation. Arthritis Rheum. 2009;60:3366–3373. doi: 10.1002/art.24856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kraus VB, McDaniel G, Worrell TW, Feng S, Vail TP, Varju G, et al. Association of bone scintigraphic abnormalities with knee malalignment and pain. Ann Rheum Dis. 2009;60:3366–3373. doi: 10.1136/ard.2008.094722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis MA, Ettinger WH, Neuhaus JM. Obesity and osteoarthritis of the knee: evidence from the National Health and Nutrition Examination Survey (NHANES I) Semin Arthritis Rheum. 1990;20:34–41. doi: 10.1016/0049-0172(90)90045-h. [DOI] [PubMed] [Google Scholar]
- 15.Altman RD, Hochberg M, Murphy WA, Jr, Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage. 1995;3 Suppl A:3–70. [PubMed] [Google Scholar]
- 16.Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. Jama. 1989;261:2663–2668. [PubMed] [Google Scholar]
- 17.Winograd CH, Lemsky CM, Nevitt MC, Nordstrom TM, Stewart AL, Miller CJ, et al. Development of a physical performance and mobility examination. J Am Geriatr Soc. 1994;42:743–749. doi: 10.1111/j.1532-5415.1994.tb06535.x. [DOI] [PubMed] [Google Scholar]
- 18.Hayes CW, Jamadar DA, Welch GW, Jannausch ML, Lachance LL, Capul DC, et al. Osteoarthritis of the knee: comparison of MR imaging findings with radiographic severity measurements and pain in middle-aged women. Radiology. 2005;237:998–1007. doi: 10.1148/radiol.2373041989. [DOI] [PubMed] [Google Scholar]
- 19.Guermazi A, Hunter DJ, Roemer FW. Plain radiography and magnetic resonance imaging diagnostics in osteoarthritis: validated staging and scoring. J Bone Joint Surg Am. 2009;91 Suppl 1:54–62. doi: 10.2106/JBJS.H.01385. [DOI] [PubMed] [Google Scholar]
- 20.Peyron J. The epidemiology of osteoarthritis. Philadelphia: Saunders; 1984. [Google Scholar]
- 21.Hinman RS, Bennell KL, Metcalf BR, Crossley KM. Balance impairments in individuals with symptomatic knee osteoarthritis: a comparison with matched controls using clinical tests. Rheumatology (Oxford) 2002;41:1388–1394. doi: 10.1093/rheumatology/41.12.1388. [DOI] [PubMed] [Google Scholar]
- 22.Wegener L, Kisner C, Nichols D. Static and dynamic balance responses in persons with bilateral knee osteoarthritis. J Orthop Sports Phys Ther. 1997;25:13–18. doi: 10.2519/jospt.1997.25.1.13. [DOI] [PubMed] [Google Scholar]
- 23.Hassan BS, Mockett S, Doherty M. Static postural sway, proprioception, and maximal voluntary quadriceps contraction in patients with knee osteoarthritis and normal control subjects. Ann Rheum Dis. 2001;60:612–618. doi: 10.1136/ard.60.6.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahmed N, Mandel R, Fain MJ. Frailty: an emerging geriatric syndrome. Am J Med. 2007;120:748–753. doi: 10.1016/j.amjmed.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 25.Fried LP, Hadley EC, Walston JD, Newman AB, Guralnik JM, Studenski S, et al. From bedside to bench: research agenda for frailty. Sci Aging Knowledge Environ. 2005;2005:pe24. doi: 10.1126/sageke.2005.31.pe24. [DOI] [PubMed] [Google Scholar]


