Abstract
This paper uses data from the National Longitudinal Study of Adolescent Health to examine the mental health of non-Hispanic black and white young adults in the US. We use latent growth curve modeling to characterize the typical stress trajectories experienced by black and white young adults spanning the bulk of their lives. We identify the following four stress trajectories: 1) relatively stress free; 2) stress peak at age 15 and a subsequent decline; 3) stress peak at age 17 and a subsequent decline; and 4) a moderately high chronic stress. Results indicate that black adolescents have significantly higher risk of being in all three of the stressful classes compared to white adolescents. Stress exposure is strongly associated with depression and the race differences in stress profiles account for a modest amount of the observed race differences in mental health. We do not observe any race differences in behavioral responses to stressors; black youth are no more likely than white youth to engage in poor health behaviors (e.g., smoking, drinking, or obesity) in response to stress. We provide tentative support for the notion that poor health behaviors partially reduce the association between stress and depression for blacks but not whites. These findings contribute to unresolved issues regarding mental and physical health disparities among blacks and whites.
Keywords: Health disparities, stress, depression, health behaviors, USA, ethnicity and mental health
Introduction
Persons exposed to a relatively large number of stressors tend to report worse mental health compared to those who have experienced very few of these events in their lives (Kessler, 1997). This is particularly important for health disparities research because racial and ethnic minorities report a greater number of chronic and acute stressors compared to non-Hispanic whites in the US (Williams and Collins, 1995; Schulz et al., 2000; Boardman 2004). However, despite race differences in stress exposure, black adults typically report comparable or better mental health compared to white adults (Breslau et al. 2006; Riolo et al. 2005; Kessler et al. 1994). Although some recent evidence has shown that black adults face an increased risk of depression (8.0%) compared to non-Hispanic white adults (4.8%) [Pratt and Brody, 2008] this finding stands out among research that reports more salutary mental health among black respondents (Kessler et al., 1999; Haralson et al., 2002).
Some have argued that the somewhat contradictory relationship between stress and depression among black and white adults can be resolved by accounting for group differences in poor health behaviors (PHB) including drinking, smoking, and over-eating (Jackson et al., 2010). Specifically, moderate use of alcohol or nicotine denote relatively cheap and effective mechanisms to mitigate the adverse physiological effects of stress (Lipton 1994; Benowitz, 1996; Peele and Brodsky, 2000) and the same has been shown for the consumption of fatty and high caloric foods (Dallman et al., 2003b). The use of substances in light of stress exposure is regularly shown among adults (Boardman et al., 2001) and a growing body of work has linked substance use among adolescents with a myriad of stressful events including abuse, work intensity, academic pressure (high school and/or college), relationship and sexuality issues, exposure to violence, and delinquent behavior (Paschall et al., 2004; Hyucksun et al., 2009; Dauber et al., 2009).
The strongest evidence to date for the moderating influence of PHB on the stress-mental health relationship is the recent study by Jackson et al (2010). The research team used data from the Americans’ Changing Lives Survey to predict a DSM-III measure of depression as a function of nine stressful events within the past three years. They show that increasing numbers of stressful life events increases the risk of depression among both black and white adults. However, they also show that this association is conditional upon the number of PHB in which individuals are engaged. For whites, the association between stressors and mental health is worse (albeit only moderately significant) for those with the highest levels of PHB. Importantly, for blacks, the association between stress and depression is strongest for those who do not engage in any PHB and stressors have virtually no influence on mental health for blacks who engage in several PHB. Importantly, Mezuk et al. (2010) replicate these findings using an independent sample of adults from the Baltimore Epidemiologic Catchment Area Study. Their study uses data from a longer period of time and they focus specifically on depression syndrome rather than general psychological distress. Despite these differences, the convergence of these findings provides fairly strong support for the coping behavior explanation for the seeming paradox between stress exposure and mental health of black adults.
The purposes of this paper are twofold. First, very few studies have made efforts to characterize the role of race as structuring stress exposure, social norms about health-related behaviors, and subsequent mental health sequelae, and none have specifically looked at younger populations. Emphasizing younger populations is important for diagnostic purposes (Eaton and Kessler 1981; Perreira et al. 2005; George and Lynch, 2003) but also because minorities experience higher levels of depressive symptoms in early life (Adkins et al., 2009). If the social mechanisms behind stress-coping responses begin early in life then this denotes an important opportunity to elaborate upon this topic and a potentially important intervention mechanism for effective health policy.
Second, to date, no study has examined race differences in behavioral responses to stress. Jackson et al. (2010) and Mezuk et al. (2010) argue that African-Americans exhibit comparable mental health levels as non-Hispanic whites despite greater levels of chronic stress because of socially acceptable coping strategies involving PHB but neither study presents evidence that blacks are more likely than whites to turn to PHB in response to stress. If the explanation for the stress-mental health paradox is the increased prevalence of PHB among blacks, then the effect of stress on smoking, drinking, and obesity should be higher for blacks compared to whites. If we do not find evidence for this, then it suggests a different mechanism for this fairly complex association. As such, our paper contributes to this important line of research by providing a test of the specific mechanisms of the stress-coping model developed by Jackson et al. (2010) among a younger cohort of black and white adults.
METHODS
Data
All data in these analyses are drawn from the National Longitudinal Study of Adolescent Health (Add Health), a study that examines health and health-related behaviors among a nationally representative sample of adolescents in seventh through twelfth grades (Harris et al. 2003). In 1994, roughly 90,000 adolescents from 134 schools completed questionnaires about their daily activities, health-related behaviors, and basic social and demographic characteristics. Respondents were then followed up with three in-home interviews (Wave I [1995], Wave II [1996], and Wave III [2001]) with more detailed questions across a number of important domains. Our study includes only non-Hispanic White and non-Hispanic Black respondents and we use data obtained from all three waves of data collection to characterize the stress trajectories of the respondents. The measures and their corresponding wave of collection are all described below. All data are weighted to reflect the complex sampling design of the Add Health study (Chantala and Tabor, 1999).
Measures
Social demographic control variables used in this study included sex (1 if male, 0 if female), age, and region (1 if living in south, 0 otherwise) at Wave III. Because behaviors such as smoking and drinking are associated with college attendance, we also include a control which indicates whether the respondent is in college during Wave III. We also include a control for the respondent’s socioeconomic status at wave I which we believe to be a better measure of socioeconomic background compared to the respondents current SES. This measure is a composite of three census tract variables (proportion of tract age 25+ without high school diploma or equivalent; proportion of tract age 15+ with at least a college degree; and median household income), household income, and highest education level of a parent (α=.81).
The key measures in our study include depression, stressful life events, and poor health behaviors. Depression: Our study makes use of the nine item version of the Center for Epidemiologic Studies depression scale (CES-D). Respondents were asked how often during the last seven days (0=never or rarely to 3=most of the time or all of the time) they felt the following: you were bothered by things that usually don’t bother you; you could not shake off the blues, even with help from your family and your friends; you felt that you were just as good as other people (reverse); you had trouble keeping your mind on what you were doing; you were depressed; you were too tired to do things; you enjoyed life (reverse); you were sad; you felt that people disliked you (α = .80). All statistical analyses use Wave III depression as the dependent variable. To estimate the influence of health behaviors and stress on the risk of depression we also control for Wave I depression in the multivariate models. As such, the dependent variable denotes change in depression from Wave I to Wave III. Based on previous research (Schulz et al., 2000) we use a conservative threshold and identified those with score of 10 or higher as having depression.
Poor health behaviors
We followed the approach of Jackson et al. (2010) and identified three PHB for this study obtained from Wave III of the study. Regular drinking is characterized by the consumption alcohol at least 1-2 times per week over the past year. While this amount of alcohol consumption is not necessarily unhealthy, it is included in our scale because of the regularity with which it occurs. Together with smoking and obesity, we believe that this measure captures a less healthy lifestyle compared to those who do not regularly consume alcohol. Similarly, regular smoking is characterized as smoking at least one cigarette per day for 30 consecutive days. Finally, obesity is measured as a function of respondent’s measured height and weight from the Wave III study. Those with a body mass index of 30 or higher are characterized as obese. As with Jackson et al. (2010), PHB is the sum of these three behaviors (ranging from 0 to 3).
Stressful life events
We analyzed all three waves of Add Health and identified for each respondent the age at which various stressful life events (SLE) occurred. As a guideline we used the stressful life events list found in Adkins et al. (2009) and identified the following occurrences of stress: ran away from home, was expelled from school, unwanted pregnancy, abortion, gave baby up for adoption, cohabitation ended romantic relationship ended, marriage ended, non-romantic sexual relationship ended, diagnosed with STD, attempted suicide, threatened someone, shot or stabbed someone, injured someone in a fight, discharged from the military, entered the military, evicted from home, utility service cut off, receiving welfare, involuntarily cut from welfare, juvenile conviction or detention, adult conviction, adult jail time, miscarriage, death of biological father, death of biological mother, death of parental figure, death of a romantic relationship, death of a spouse, death of a baby, suicide of friend or family member, baby had medical problems, relationship abuse (threatening, insulting, swearing, throwing things, pushing), was jumped, saw violence, was shot or stabbed, had sex for money, was threatened, mother or father on public assistance, was raped, was injured in a fight, skipped needed health care.
We used information about the age at which each of the events occurred to calculate the number of SLEs experienced by each individual at each age between 11 and 21. We then conducted latent class trajectory analysis using the mmlcr package (Buyske 2006) in R 2.9.0 (R Development Core Team 2009) for the sum number of stressors for each age across the range of ages. This procedure uses mixed-mode latent class regression to describe intra-individual change over time as a function of group membership (Ci) where group membership in the Kth class is a post-hoc determination based on similarity in initial levels of stress (intercept) and change in stress over time (slope). The general model is specified below.
In this model, the dependent variable is the observed number of stressors reported at each age during the study. The Akaike and Bayseian information criteria (AIC and BIC) are used to estimate the total number of discrete stress trajectories that are evident in the population. That is, a baseline growth model is estimated that simply describes the average growth in which there is only one group. A second model is then estimated for two groups. By comparing the AIC and BIC from this model with the AIC and the BIC from the baseline model, we are able to see if the additional group improves the fit of the model. This procedure is repeated until the next group does not add any additional information to the overall model fit. The main parameter estimate of this model is pk which is the probability of belonging to class k which can also vary as a function of the parameters λk which change differentially over time. Because of the count nature of the dependent variable, we use a Poisson link in this general trajectory model to predict the average number of stressors that individuals in class k are expected to have at each age. We allow for cubic age terms in our estimation of growth trajectories.
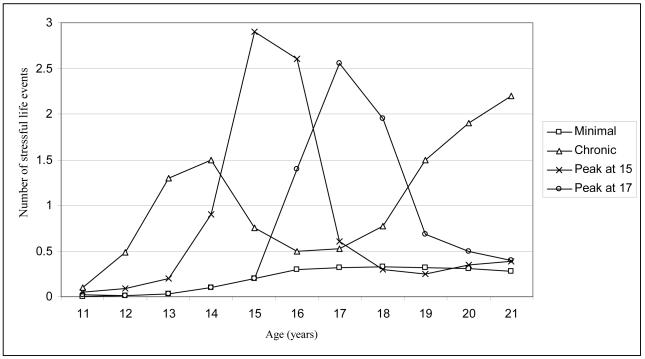
Using these methods, we identify four stress trajectories which are presented in Figure 1. In total 53.9% were minimally exposed to stress. This group showed a slight increase in average stress exposure but at no point did the predicted average number of stressors/year exceed one-half. Two of the remaining three trajectories were similar in that they contained a sharp increase in the number of SLEs but this increase quickly subsided over the following two years. These two trajectories differ by the estimated peak which was early (age 15) for the first group and somewhat later for the second group (age 17). The “peak at 17” group was more common (18.7%) than the “peak at 15” group” (11.4%). Finally, we describe the fourth group as “chronic” because important SLEs occurred as young as 12 and this group demonstrates a fairly chronic stress profile throughout the study. This group comprised the remaining 15.9% of the sample. Although there is an observable dip during mid to late adolescence, there is a return to a fairly regular exposure to SLEs in young adulthood.
Figure 1.
Early life stress exposure among US adolescents: latent growth classes for stressful life events.
Note: all data come from Waves I, II, and III of the National Longitudinal Study of Adolescent Health (Add Health). Values obtained from latent class trajectory modeling using the MMLCR package in R.
Analytic Strategy
To examine the research questions described above we employ the following strategy:
Estimate and classify stress trajectories for all respondents [Table 1 and Figure 1].
Describe the prevalence of depression (Wave III) as a function of stress trajectories [Table 2].
Estimate the effect of stress trajectory on depression (Wave III) controlling for Wave I depression, sociodemographic background, and PHB [Table 3, Models 1-3].
Estimate the interaction between race and PHB on the risk of depression (Wave III). We anticipate that the effect of race (black = 1) should be significantly lower for those who engage in the most PHB [Table 3, Model 4].
Test the hypothesis that blacks are more likely than whites to turn to PHB in light of stress exposure [Table 4]. This is the mechanism proposed by Jackson et al. (2010).
Test the Jackson et al. (2010) model for the association between stress, PHB, and depression as a function of race [Table 5].
Table 1.
Descriptive statistics by self-reported race
| NH White | NH Black | Pr (W=B) | |
|---|---|---|---|
| Stress Trajectories [Waves I-III] | |||
| Minimal | .559 | .454 | <.006 |
| Peak 15 | .109 | .137 | |
| Peak 17 | .180 | .217 | |
| Chronic | .152 | .192 | |
| Poor Health Behaviors [Wave III] | |||
| Regular smoker | .491 | .244 | <.000 |
| Regular drinker | .115 | .065 | <.000 |
| Obese | .256 | .351 | <.000 |
| Sum of behaviors (PHB) | .861 | .660 | <.000 |
| Depression [Wave III] | .101 | .146 | <.000 |
| Sociodemographic Controls | |||
| Sex (Male = 1) | .470 | .441 | <.766 |
| Age (years) [Wave III] | 21.841 | 21.858 | <.677 |
| Region (South = 1) [Wave I] | .345 | .649 | <.000 |
| SES [Wave1] | 0.142 | −.268 | <.000 |
| In College [Wave III] | .364 | .286 | <.006 |
Note: all data come from Waves I, II, and III of the National Longitudinal Study of Adolescent Health (Add Health). All data are weighted to reflect the complex sampling design of the Add Health study (Chantala & Tabor 1999) and all estimates are obtained using the SVY commands in STATA 10.0.
Table 2.
Prevalence of depression by stress trajectory for black and white adolescents and young adults
| Proportion of respondents meeting criteria for depression | |||
|---|---|---|---|
| Stress Trajectory | White | Black | Total |
| Minimal | 0.074 | 0.091 | .076 |
| Peak 15 | 0.141 | 0.214 | .158 |
| Peak 17 | 0.110 | 0.161 | .121 |
| Chronic | 0.158 | 0.214 | .171 |
| Design based F | 17.29 | 10.06 | 27.12 |
| d.f. | 2.89, 352.16 | 2.88, 276.23 | 2.96, 379.46 |
| Pr. < | 0.000 | 0.000 | .000 |
Note: all data come from Waves I, II, and III of the National Longitudinal Study of Adolescent Health (Add Health). All estimates are adjusted for the complex sampling design of the Add Health study using the SVY commands in STATA 10.0 (Chantala & Tabor 1999).
Table 3.
The role of stress, poor health behaviors, and race on depression (Wave 3): logistic regression estimates (odds ratios)
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Depression (W1) | 3.483 (3.007, 4.034) | 3.155 (2.724, 3.654) | 3.127 (2.697, 3.625) | 3.127 (2.697, 3.626) |
| Sex [Female] | ||||
| Male | 0.643 (0.548, 0.755) | 0.622 (0.529, 0.731) | 0.615 (0.522, 0.724) | 0.617 (0.524, 0.726) |
| Age (years) | 0.916 (0.877, 0.957) | 0.972 (0.921, 1.024) | 0.969 (0.919, 1.022) | 0.969 (0.919, 1.022) |
| Region [All others] | ||||
| South | 0.795 (0.670, 0.943) | 0.817 (0.689, 0.969) | 0.811 (0.684, 0.962) | 0.809 (0.682, 0.960) |
| Enrolled in college [No] | ||||
| Yes | 0.691 (0.570, 0.838) | 0.745 (0.617, 0.899) | 0.778 (0.647, 0.936) | 0.780 (0.649, 0.938) |
| Race [NH White] | ||||
| NH Black | 1.411 (1.155, 1.725) | 1.332 (1.091, 1.628) | 1.417 (1.153, 1.742) | 1.678 (1.278, 2.205) |
| Socioeconomic status | 0.857 (0.754, 0.974) | 0.871 (0.764, 0.993) | 0.872 (0.765, 0.994) | 0.873 (0.765, 0.995) |
| Stress Trajectory [Minimal] | ||||
| Peak at 15 | 1.736 (1.318, 2.287) | 1.654 (1.254, 2.180) | 1.649 (1.251, 2.174) | |
| Peak at 17 | 1.273 (0.995, 1.628) | 1.217 (0.948, 1.562) | 1.215 (0.947, 1.560) | |
| Chronic | 2.050 (1.577, 2.664) | 1.938 (1.482, 2.534) | 1.932 (1.478, 2.525) | |
| PHB (0-3) | 1.232 (1.086, 1.397) | 1.295 (1.115, 1.504) | ||
| Black*PHB | 0.809 (0.641, 1.019) | |||
|
| ||||
| Log Likelihood | −3853.793 | −3821.579 | −3813.447 | −3812.150 |
| −2LL | 7707.587 | 7643.158 | 7626.895 | 7624.300 |
| Likelihood Ratio | 493.730 | 64.429 | 16.262 | 2.595 |
| DF | 7 | 3 | 1 | 1 |
| Pr. | 0.000 | 0.000 | 0.000 | 0.107 |
| Pseudo r2 | 0.060 | 0.068 | 0.070 | 0.070 |
Note: all data come from Waves I, II, and III of the National Longitudinal Study of Adolescent Health (Add Health). All estimates are adjusted for the complex sampling design of the Add Health study using the SVY commands in STATA 10.0 (Chantala & Tabor 1999).
Table 4.
The effect of stress on poor health behaviors (Wave 3) by race: ordered logistic regression estimates (odds ratios)
| White | Black | |
|---|---|---|
| PHB W1 (0-3) | 3.899 (3.449, 4.407) | 3.16 (2.478, 4.030) |
| Sex [Female] | ||
| Male | 1.243 (1.107, 1.397) | 1.354 (1.105, 1.661) |
| Age (years) | 0.939 (0.903, 0.976) | 1.021 (0.943, 1.105) |
| Region [All others] | ||
| South | 1.009 (0.863, 1.180) | 1.190 (0.840, 1.685) |
| Enrolled in college [No] | ||
| Yes | 0.659 (0.570, 0.761) | 0.632 (0.502, 0.794) |
| Socioeconomic status | 0.934 (0.841, 1.037) | 1.008 (0.845, 1.203) |
| Stress Trajectory [Minimal] | ||
| Peak at 15 | 1.582 (1.308, 1.913) | 1.567 (1.086, 2.261) |
| Peak at 17 | 1.555 (1.324, 1.827) | 1.542 (1.177, 2.021) |
| Chronic | 2.004 (1.699, 2.364) | 1.820 (1.418, 2.337) |
| Log-Likelihood base model | −7650.242 | −2732.270 |
| Log-Likelihood with stress controls | −7576.108 | −2715.222 |
| Likelihood ratio | 148.268 | 34.0962 |
| d.f. | 3 | 3 |
| Pr. < | .000 | .000 |
| Pseudo r2 | 0.099 | 0.085 |
Note: all data come from Waves I, II, and III of the National Longitudinal Study of Adolescent Health (Add Health). All estimates are adjusted for the complex sampling design of the Add Health study using the SVY commands in STATA 10.0 (Chantala & Tabor 1999).
Table 5.
The interactive role of stress and poor health behaviors as determinants of depression (Wave 3) among black and white adolescents and young adults: logistic regression estimates (odds-ratios)
| White | Black | |
|---|---|---|
| Depression (W1) | 3.507 (2.921, 4.21) | 2.740 (1.992, 3.768) |
| Sex [Female = 0] | ||
| Male | 0.640 (0.525, 0.779) | 0.576 (0.415, 0.800) |
| Age (years) | 0.955 (0.899, 1.014) | 0.999 (0.911, 1.097) |
| Region [All others] | ||
| South | 0.748 (0.607, 0.921) | 0.926 (0.668, 1.283) |
| College attendance [No] | ||
| Yes | 0.810 (0.653, 1.006) | 0.619 (0.438, 0.874) |
| Socioeconomic status | 0.824 (0.707, 0.96) | 0.995 (0.765, 1.295) |
| Stressful profile [All others] | ||
| Chronic | 1.872 (1.204, 2.912) | 2.171 (1.176, 4.006) |
| PHB (0-3) | 1.363 (1.147, 1.621) | 1.143 (0.924, 1.414) |
| Chronic stress* PHB | 0.893 (0.652, 1.223) | 0.733 (0.499, 1.077) |
| Log likelihood without interaction | −2508.702 | −1315.34 |
| Log likelihood with interaction | −2508.434 | −1315.29 |
| d.f. | 1 | 1 |
| Likelihood ratio | 0.5354 | 0.1 |
| Pr. | 0.464 | 0.752 |
| Pseudo R2 | 0.062 | 0.058 |
Note: all data come from Waves I, II, and III of the National Longitudinal Study of Adolescent Health (Add Health). All estimates are adjusted for the complex sampling design of the Add Health study using the SVY commands in STATA 10.0 (Chantala & Tabor 1999).
RESULTS
Table 1 shows the stress profiles, control measures, depression, PHB by race. Three important findings emerge from this table. First, Non-Hispanic blacks are significantly more likely than whites to have an elevated stress profile throughout their teens and into their twenties. Whereas 56% of whites were considered to have minimal stress profiles, only 45% of blacks experienced this relatively low stress exposure throughout adolescence and into early adulthood. Similarly, blacks are more likely to have the two peaked stress profiles as well as the chronically stressed adolescence. The design based estimate suggests that the observed differences in the distribution of stress trajectories is significant (p<.006) for blacks and whites. Relative risk ratios (RRR) were calculated from multinomial logistic regression models and indicate that the observed differences are statistically significant for each elevated stress level compared to the minimal trajectory. Specifically, the RRR estimates (and 95% confidence intervals) for blacks compared to whites are 1.54(1.22, 1.94), 1.48(1.14, 1.91), and 1.56(1.11, 2.18) for the peak 15, peak 17, and chronic stress trajectories, respectively.
Second, the prevalence of depression is significantly higher for blacks (pd = .146) compared to whites (pd = .101). As with the results of other studies (Adkins, 2009), this information is important because it contributes to a fairly large body of work that has, to date, provided fairly inconclusive results regarding depression as a health disparity. Finally, the prevalence of smoking and drinking are significantly higher for whites compared to blacks but blacks are more likely than whites to have an increased risk of obesity. Overall, whites have a significantly worse PHB profile () compared to blacks () and this difference is statistically significant (p<.000). These results are comparable to Jackson et al. (2010) who also showed that blacks had lower rates of PHB compared to whites.
Table 2 presents the prevalence of depression by stress trajectory for by race. These results provide strong evidence that SLEs are associated with depression for young adults regardless of the stress trajectory. However, they also indicate that the prevalence of depression is significantly higher for those who have been exposed to stressors for the longest period of time. The chronic stress group displays the highest risk of depression for both groups and nearly one in five blacks in this category have symptom counts of depression that exceed the criteria for depressive diagnosis. Equally important, blacks display an elevated risk of depression at each stress trajectory. In ancillary analyses (results not shown) we estimated a logistic regression model predicting depression as a function of stress trajectory, race, and race*trajectory interaction terms and none of these interaction terms were statistically significant suggesting that the effects of stress on depression are comparable for whites and blacks.
The results from Tables 1 and 2 support findings from previous research showing an increased risk of depression among blacks compared to whites. We also show that blacks face an increased risk of SLEs across their adolescence and that stress is strongly associated with an increased risk of depression with chronic stress as the most risky stress trajectory. These results pose an important question that is addressed in Table 3. Specifically, to what extent is the increased prevalence of depression among blacks compared to whites due to greater exposure to stress among blacks? Model 1 in Table 3 provides an adjusted baseline risk for blacks compared to whites (OR = 1.411) that is slightly attenuated (OR = 1.332) with the controls for stress (Model 2). This suggests that roughly 17% of the increased risk of depression among blacks is due to the increased average stress levels among blacks compared to whites. Importantly, the strong associations between the two early onset stress categories (e.g., Chronic and Peak 15) remain statistically significant despite controlling for social and demographic background characteristics. Those in the chronic stress trajectory are more than 2 times as likely as those in the minimal stress trajectory to be characterized as depressed in Wave III.
The third model in Table 3 provides an initial look at the complex association between PHB, stress, depression, and race. These results indicate that PHB are positively and significantly associated with a risk of depression; compared to those who do not engage in any PHB, each successive PHB is associated with a 23% increase in the risk of depression. Importantly, these controls act as a moderate suppressor for the race coefficient which increases back to its level prior to the controls for stressors. This provides some (albeit weak) support for the notion that PHB may actually buffer the deleterious effects of stress on depression for blacks. Further support for this idea can be seen from the final model in Table 3 which introduces an interaction term between PHB and race. The interaction is only moderately significant (p<.072, two-tailed) but the direction of the term suggests that the effect of PHB on depression is weaker for blacks compared to whites. Importantly, it also suggests that if one considers the effects of race with PHB removed (e.g., PHB = 0) that blacks actually face an even stronger risk of depression compared to whites (OR = 1.68).
To examine this possibility, Table 4 presents estimates from two ordered logistic regression models in which the sum of poor health behaviors (0-3) is regressed on stress and the full set of controls for blacks and whites separately. The first finding to emerge is that stress leads to an increased risk of PHB. For both groups, there are strong and positive links between each stress trajectory and an increased likelihood of engaging in PHB. However, if, as Jackson et al. (2010) hypothesize, blacks are more likely than whites to turn to PHB in the face of stress, then we should expect a larger regression coefficient for blacks for each of the stress profiles. The results provide strong evidence that this is not the case. The parameter estimates for the two regression models are virtually identical and in the case of chronic stressors, whites are slightly more likely to engage in PHB compared to whites.
As described above, it is still possible that the combined effects of chronic strain and PHB on the risk of depression are still different for blacks and whites. To examine models comparable to the Jackson et al. (2010) paper, we estimate the main and interactive effects of chronic stress and PHB for blacks and whites separately. Because we have four stress categories and three health behaviors, we limited our analysis of stress to chronic stress at this stage of the analysis in order to reduce the number of interactions and to simplify the focus. We chose chronic stress because of the evidence linking this measure of stress to depression and its strong association with PHB. Table 5 presents results from a logistic regression model in which depression at Wave III is regressed on the full set of controls but now we include an interaction term between stress and PHB. In the Jackson et al. (2010) study, the interaction was positive (but not statistically significant) for whites and negative (and statistically significant) for blacks. Thus suggesting that an increasing number of PHB buffers the negative effects of strain on depression for blacks and slightly exacerbates these effects for whites. As shown in Table 5, we show relatively weak evidence for buffering effects among blacks and no moderating effects for whites. The effect for blacks (OR=.733) is only moderately significant at the one-tail level but it remains in the direction suggested by Jackson et al. (2010).
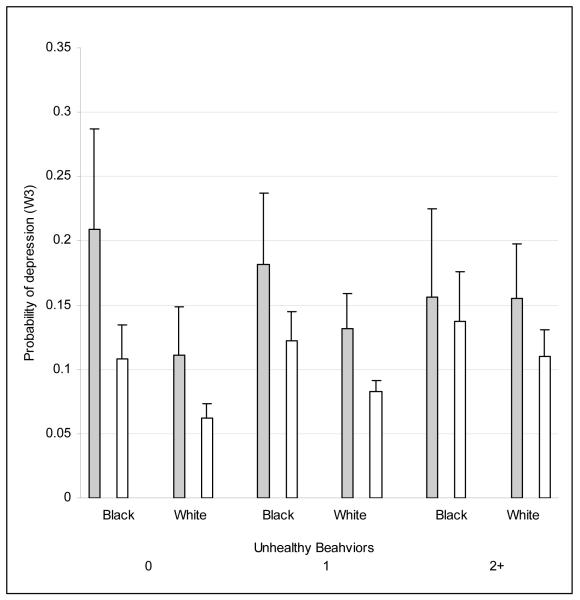
To better illustrate these associations, predicted probabilities for depression are plotted in Figure 2 by race, PHB, and chronic stress status. The shaded bars denote those who are chronically stressed and the non-shaded bars are others. As with Jackson et al. (2010), we show that the greatest mental health disparity occurs for those who are exposed to chronic stress and who do not engage in any PHB; blacks exposed to chronic stress who lead the most healthy lives have the highest estimated probability of depression. There is virtually no disparity among stress exposed blacks and whites who are engaged in at least two PHB. We believe this highlights the importance of characterizing the long-term stress profiles to clarify the role of race and PHB related to mental health. In sum, we find support for the stress-coping model but not for the hypothesized behavioral mechanism.
Figure 2.
The estimated effect of chronic stress on depression for black and white adolescents.
Note: all data come from Waves I and III of the National Longitudinal Study of Adolescent Health (Add Health). Values and error estimates derived from the parameter estimates in Table 4 using the prvalue command following the design based logistic regression routine in STATA 10.0
DISCUSSION AND CONCLUSION
Exposure to chronic stressors is regularly shown to both increase depressive symptoms and to increase the risk of PHB including alcohol use, smoking, and obesity (Adkins et al., 2009; Mason et al., 2008; Meadows et al., 2004; Dallman et al., 2003a; Dallman et al., 2003b; Ge et al., 1994). While some studies have simultaneously investigated the complex relationships between these three factors (stress, PHB, and depression) only a limited number have focused explicitly on adolescents (Chaiton et al., 2009; Lipton, 1994) and few studies examined the ways in which race structures the complex interactions between social stressors, health compromising coping behaviors, and depressive symptoms (Jackson et al. 2010; Mezuk et al. 2010). There is agreement that stress is composed of both operant and cumulative stress (Turner et al. 1995) but measurement strategies typically involve summing the total number of stressors across longer periods of time. A distinguishing feature of our study was the use of stress trajectories rather than simple counts of stressful life events. This allowed us to differentiate not only between low and high stress but between those who faced relatively high stress at younger ages and those who had more typical peaks or minimal stress through adolescence. Others have made a strong case for stress-related trajectories (George and Lynch, 2003), but little work has attempted to characterize the typical stress trajectories that exist in a population of young adults. Our analyses confirmed that non-Hispanic blacks were more likely than non-Hispanic whites to be exposed to early stress and to begin to see increasing stressful life events entering young adulthood. Given that stress and depressive symptoms are typically associated, it was not surprising to find that the rate of depressive symptoms was also higher for non-Hispanic blacks.
We also recognize that there are limitations with our current study that should be considered when interpreting the results. While the trajectory based stress assessment provides new and useful information for stress-related research and health-disparities research in general, we limited our items to comparable measures used in other research (Adkins et al. 2009). To be sure, there are other known sources of stress and strain that could be obtained from the Add Health data that are not included in our analyses. For example, we make no efforts to include ambient stressors related to the physical or built environment. These factors have been linked to psychological well-being (Cohen and Weinstein 1981) and are believed to be an important contributor to mental health disparities (Downey and Van Willigen 2005). Moreover, our stress measure did not differentiate between the different sources of stress. In other words, these stressors may be linked to social, health, residential, work-related, or familial issues which may have very different consequences with respect to mental health and unhealthy coping behaviors.
Second, although our stress measures contain a strong longitudinal component, we are limited in our assessments of both depression and health behaviors, most importantly obesity. That is, we are not able to identify the temporal sequence of the obesity-depression association which may operate in the opposite direction from the one that we have hypothesized (Luppino 2010). While controls for PHB at the different waves did not alter our results in any meaningful way, readers should consider that we do not adjust for childhood obesity which may confound the results presented above.
Third, there is some evidence that the CESD measure of depressive symptoms used in this study is not a valid indicator of depression across racial and ethnic groups. Using Add Health, Perreira et al. (2005) show some inconsistency regarding the validity of CESD as a function of race and suggest that researchers limit their analysis to five questions of the CESD measure which are shown to be valid for all groups. Specifically, they suggest that the past week indication of feeling 1) depressed, 2) sad, 3) you couldn’t shake off the blues, 4) like you enjoyed life, and 5) happy denote reliable and valid components of depressive symptoms. To examine this possibility that measurement differences across groups are responsible for our findings, we re-examined our results using this limited number of items. The “happy” item was not available in the Wave III interview so we used a summary score of the four remaining items and identified a threshold of 5 for the new indication risk of depression. We found virtually identical results using this reduced CESD measurement (results available upon request). Therefore, it is important to consider the influence of measurement issues with the CESD depression scale, however, these limitations should not compromise the results presented above.
Despite these limitations, we believe that this paper makes important contributions to ongoing discussions regarding the complex relationships between stress, coping behaviors, and mental health among members of different racial and ethnic groups. The most intriguing finding to emerge from our analysis was the replication of the findings presented by Jackson et al. (2010) and Mezuk et al. (2010) but our failure to demonstrate support for the purported mechanism through which these disparities may be operating. Importantly, neither Jackson et al. (2010) nor Mezuk et al. (2010) actually test this specific model in their respective papers. We show that PHB moderate the association between stress and depression for blacks but we do not find any evidence that blacks are more likely than whites to use PHB to cope with stress. This may simply be due to the age differences in the two studies; our study examines youth while the Jackson et al. study examines older adults and Mezuk et al. (2010) studies adults (mean age = 46.9, sd = 11.8). Specifically, cigarettes are very expensive and the limited resources of most youth may preclude them from smoking when they may otherwise choose to do so. We used a composite indicator of PHB in order to follow the approach of Jackson et al. (2010), however, it is possible that much of the association is being driven by obesity because the real costs associated with consuming fatty foods may so much cheaper than cigarettes or alcohol; people have to eat and cheap food that is readily available may be ‘costless’ compared to additional fees paid for alcohol. To explore this possibility we examined the association between chronic stress and depression for obese and non-obese respondents (full results are not presented). For both blacks and whites, the effects of chronic stress on the risk of depression were significantly higher for non-obese persons (ORblack = 1.81, p<.023; ORwhite = 2.10, p <.000) compared to obese persons (ORblack = 1.44, n.s.; ORwhite = 1.19, n.s.). Although we show a moderating effect of obesity, again, this effect is not in the direction specified by the stress-coping model.
Another possibility that social responses (e.g., norms) to social stressors do not differ for black and white young adults may have to do with composition of stressors; the stressors presented to persons who are not engaged in any PHB may be very different from the types of stressors faced by persons who smoke, drink, and/or are obese. Persons who are more likely to engage in PHB may also select in to particular types of stressful environments. Therefore, the number of total stressors at any particular time might not be as informative as the types of stressor to which individuals are exposed. This is particularly relevant because this same concern may be further confounded by race such that the specific components of the typical stress profile of a black woman who neither smokes, nor drinks, nor is obese may be very different from a comparable woman with a similar stress profile who is white. For example, others have shown that family stress is one of the strongest predictors of depression, especially among women (Hammen, 2005). It may be that black women with the healthiest lifestyles may have a stress profile that is lower on ambient, external, acute, or other chronic indicators but tend to face much more family-related stressors compared to comparable white women. If this is the case, then it is possible to observe a different interactive association between health behaviors and stress on depression for blacks and whites that has to do with stress composition rather than stress response.
We encourage future researchers to replicate the stress-coping model described by Jackson et al. (2010) and shown here, but we also encourage future research to provide evidence for the mechanism through which these subtle social forces may (or may not) be operating. This research speaks directly to the health disparities, social stress, and life course perspective research. We also encourage others to use a trajectory based stress exposure model that is used here and to make efforts to distill the specific domains and items that are meaningful for different groups at different periods of their lives.
Acknowledgments
This research uses data from Add Health, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by a grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Persons interested in obtaining data files from Add Health should contact Add Health, Carolina Population Center, 123 W. Franklin Street, Chapel Hill, NC 27516-2524 (addhealth@unc.edu). No direct support was received from grant P01-HD31921 for this analysis. This paper is part of a larger study funded by the National Institute of Child Health and Human Development (K01 HD 50336). Research funds were also provided by the NIH/NICHD funded CU Population Center (R21 HD 051146-01).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Adkins D, Wang V, Dupre M, van den Ord E, Elder G. Structure and stress: trajectories of depressive symptoms across adolescence and young adulthood. Social Forces. 2009;88:31–60. doi: 10.1353/sof.0.0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz N. Pharmacology of nicotine: addition and therapeutics. Annual Review of Pharmacological Toxicology. 1996;36:597–613. doi: 10.1146/annurev.pa.36.040196.003121. [DOI] [PubMed] [Google Scholar]
- Boardman J, Finch B, Ellison C, Williams D, Jackson J. Neighborhood disadvantage, stress, and drug use among adults. Journal of Health and Social Behavior. 2001;42:151–165. [PubMed] [Google Scholar]
- Boardman J. Health pessimism among black and white adults: the role of interpersonal and institutional maltreatment. Social Science & Medicine. 2004;59:2523–2533. doi: 10.1016/j.socscimed.2004.04.014. [DOI] [PubMed] [Google Scholar]
- Breslau J, Aguilar S, Kendler K, Su M, Williams D, Kessler RC. Specific race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychological Medicine. 2006;36(1):57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buyske Steve. mmlcr: Mixed-Mode Latent Class Regression. R package version 1.3.5. 2006 http://www.stat.rutgers.edu/~buyske/software.html.
- Chaiton M, Cohen J, O’Loughlin J, Rehm J. A systematic review of longitudinal studies on the association between depression and smoking in adolescents. BMC Public Health. 2009;9:356. doi: 10.1186/1471-2458-9-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chantala K, Tabor J. Strategies to perform a design-based analysis using the Add Health data. Carolina Population Center, University of North Carolina at Chapel Hill; Chapel Hill, NC: [accessed July 31, 2007]. 1999. Available online at: http://www.cpc.unc.edu/projects/addhealth/files/weight1.pdf. [Google Scholar]
- Cohen S, Weinstein N. Nonauditory effects of noise on behavior and health. Journal of Social Issues. 1981;37:36–70. [Google Scholar]
- Dallman M, Akana S, Laugero K, et al. A spoonful of sugar: feedback signals of energy stores and corticosterone regulate responses to chronic stress. Physiology & Behavior. 2003a;79:3–12. doi: 10.1016/s0031-9384(03)00100-8. [DOI] [PubMed] [Google Scholar]
- Dallman M, Pecoraro N, Akana S, et al. Chronic stress and obesity: a new view of “comfort food.”. Procedures from the National Academy of Science USA. 2003a;100:11696–11701. doi: 10.1073/pnas.1934666100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dauber S, Hogue A, Paulson J, Leiferman J. Typologies of alcohol use in White and African American adolescent girls. Substance Use and Misuse. 2009:1121–1141. doi: 10.1080/10826080802494727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downey L, Van Willigen M. Environmental stressors: The mental health impacts of living near industrial activity. Journal of Health and Social Behavior. 2005;46:289–305. doi: 10.1177/002214650504600306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton WW, Kessler LG. Rates of symptoms of depression in a national sample. Am J Epidemiol. 1981;114:528–38. doi: 10.1093/oxfordjournals.aje.a113218. [DOI] [PubMed] [Google Scholar]
- Ge X, Lorenz F, Conger R, Elder G, Simons R. Trajectories of stressful life events and depression during adolescence. Developmental Psychology. 1994;30(4):467–483. [Google Scholar]
- George L, Lynch S. Race differences in depressive symptoms: A dynamic perspective on stress exposure and vulnerability. Journal of Health and Social Behavior. 2003;44(3):353–369. [PubMed] [Google Scholar]
- Hammen C. Stress and Depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Harris K. The national longitudinal study of adolescent health (Add Health), Waves I & II, 1994–1996; Wave III, 2001–2002. Carolina Population Center, University of North Carolina at Chapel Hill; Chapel Hill, NC: 2003. machine-readable data file and documentation. [Google Scholar]
- Haralson T, White T, Regenberg A, Kallan M, Have T, Parmelee P, Johnson J. Similarities and differences in depression among black and white nursing home residents. American Journal of Geriatric Psychiatry. 2002;10:175–84. [PubMed] [Google Scholar]
- Hyucksun S, Edwards E, Heeran T, Amodeo M. The relationship between multiple forms of maltreatment by a parent or guardian and adolescent alcohol use. American Journal on Addictions. 2009;18:226–234. doi: 10.1080/10550490902786959. [DOI] [PubMed] [Google Scholar]
- Jackson J, Knight K, Rafferty J. Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health. 2010;100(5):933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Mickelson K, Williams D. The Prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999;40:208–30. [PubMed] [Google Scholar]
- Kessler R. The effects of stressful life events on depression. Annual Review of Psychology. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- Kessler R, McGonagle K, Zhao S, et al. Lifetime and 12-month prevalence of DSM-II-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(8):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Lipton R. The effect of moderate alcohol use on the relationship between stress and depression. American Journal of Public Health. 1994;84(12):1913–1917. doi: 10.2105/ajph.84.12.1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–9. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- Mason W, Kosterman R, Haggerty K, Hawkins J, Redmond C, Spoth R, Shin C. Dimensions of adolescent alcohol involvement as predictors of young adult major depression. Journal of Studies on Alcohol and Drugs. 2008;69(2):275–285. doi: 10.15288/jsad.2008.69.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meadows S, Brown J, Elder G. Depressive symptoms, stress, and support: Gendered trajectories from adolescence to young adulthood. Journal of Youth and Adolescence. 2006;35(1):93–103. [Google Scholar]
- Mezuk B, Rafferty JA, Kershaw KN, Hudson D, Abdou CM, Lee H, Eaton WE, Jackson JS. Reconsidering the role of social disadvantage in physical and mental health: Stressful life events, health behaviors, race and depression. American Journal of Epidemiology. 2010;172:238–249. doi: 10.1093/aje/kwq283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paschall M, Flewelling R, Russell T. Why is work intensity associated with heavy alcohol use among adolescents? Journal of Adolescent Health. 2004;34:79–87. doi: 10.1016/s1054-139x(03)00206-4. [DOI] [PubMed] [Google Scholar]
- Peele S, Brodsky A. Exploring psychological benefits associated with moderate alcohol use; a necessary corrective assessment of drinking outcomes. Drug and Alcohol Dependency. 2000;60:221–247. doi: 10.1016/s0376-8716(00)00112-5. [DOI] [PubMed] [Google Scholar]
- Perreira KM, Deeb-Sossa N, Harris KM, Bollen K. What are we measuring? An evaluation of the CES-D across race/ethnicity and immigrant generation. Social Forces. 2005;83:1567–1602. [Google Scholar]
- Pratt L, Brody D. [Accessed July 31, 2010];Depression in the United States Household Population, 2005-2006. NCHS Data Brief, 7. 2008 http://www.cdc.gov/nchs/data/databriefs/db07.pdf. [PubMed]
- R Development Core Team . R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2009. [Google Scholar]
- Riolo SA, Nguyen TA, Greden JF, King CA. Prevalence of Depression by Race/Ethnicity: Findings from the National Health and Nutrition Examination Survey III. Am J Public Health. 2005;95(6):998–1000. doi: 10.2105/AJPH.2004.047225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz A, Israel B, Williams D, Perker E, Becker A, James S. Social inequalities, stressors, and self-reported health status among African American and white women in the Detroit metropolitan area. Social Science & Medicine. 2000;51:1639–1653. doi: 10.1016/s0277-9536(00)00084-8. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Lloyd D. The stress process and the social distribution of depression. Journal of Health and Social Behavior. 1999;40:374–404. [PubMed] [Google Scholar]
- Turner RJ. The pursuit of socially modifiable contingencies in mental health. Journal of Health and Social Behavior. 2003;44:1–17. [PubMed] [Google Scholar]
- Turner RJ, Wheaton B, Lloyd D. The Epidemiology of Social Stress. American Sociological Review. 1995;60:104–25. [Google Scholar]
- Williams D, Collins C. U.S. Socioeconomic and racial differences in health: patterns and explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]