Abstract
Objective
Prolonged prehospital delay in persons experiencing acute coronary syndrome (ACS) remains a problem. Understanding which patients respond best to particular interventions designed to decrease delay time would provide mechanistic insights into the process by which interventions work.
Methods
In the PROMOTION trial, 3522 at-risk patients were enrolled from 5 sites in the United States (56.4%), Australia and New Zealand; 490 (N=272 intervention, N=218 control) had an acute event within two years. Focusing on these 490, we (1) identified predictors of a rapid response to symptoms, (2) identified intervention group subjects with a change in these predictors over three months of follow-up, and (3) compared intervention group participants with and without the favorable response pattern. Hypothesized predictors of rapid response were increased perceived control and decreased anxiety. Knowledge, attitudes, and beliefs were hypothesized to differ between responders and nonresponders.
Results
Contrary to hypothesis, responders had low anxiety and low perceived control. Only 73 (26.8%) subjects showed this pattern 3 months following the intervention. No differences in ACS knowledge, attitudes, or beliefs were found.
Conclusion
The results of this study challenge existing beliefs.
Practice Implications
New intervention approaches that focus on a realistic decrease in anxiety and perceived control are needed.
Keywords: acute coronary syndrome, treatment seeking delay, denial, common sense model, responder analysis
1. Introduction
Prolonged prehospital delay in patients experiencing symptoms of acute coronary syndrome (ACS) remains a problem, with most patients delaying at least two hours before seeking health care.(1) Over the past three decades, numerous investigators have described the characteristics of patients who delay in response to ACS symptoms.(2) These studies have helped to identify high-risk groups needing intervention. Yet, after patients are enrolled in a clinical trial and receive an intervention designed to decrease delay time, some seek care quickly and some do not.(3, 4) At this point we remain uncertain about who responds to our interventions. Understanding which patients respond best to particular interventions would provide mechanistic insights into the process by which intervention approaches work in particular patient groups. Therefore, the purpose of this study was to identify patients who responded appropriately to an educational intervention designed to reduce ACS treatment seeking delay and to compare their clinical and sociodemographic characteristics with those of patients who failed to respond to the intervention. This was a secondary analysis of data from the PROMOTION (Patient Response tO Myocardial Infarction fOllowing a Teaching Intervention Offered by Nurses) trial, described further below. After 2 years of follow-up, neither median prehospital delay time nor emergency medical system use differed between the intervention and control groups.(5)
Most educational interventions seek to increase knowledge and change attitudes and beliefs. A concern when educating patients about the risk of ignoring ACS symptoms is the possibility that education could increase anxiety, a response known to be associated independently with poor outcomes.(6, 7) Perceived control, the belief that one has at one’s disposal strategies to reduce the aversiveness of an event, is associated with low levels of anxiety.(6, 8, 9) Based on this rationale, we hypothesized that patients with an increase in perceived control and a decrease in anxiety would be most likely to seek treatment rapidly when ACS symptoms occur.(8, 10–12)
This hypothesis was tested in subjects who sought care for an acute event, regardless of assignment to the experimental or control group. Then we identified intervention group patients who experienced a change reflecting this responder pattern, presumably in response to the intervention. Then we described how these intervention group responders differed from nonresponders. Here we hypothesized that intervention group subjects with the responder pattern would have higher ACS knowledge, attitudes, and beliefs than intervention group subjects without the responder pattern.
The common sense model (CSM) of illness representation was used to guide the educational intervention and our interpretation of the results obtained in this study. Leventhal(13) hypothesized that people form commonsense or lay representations when confronted with illness-related information. These lay representations or mental schema influence the manner in which symptoms are interpreted and how decisions are made. Leventhal et al.(14) viewed this formation of a mental schema as a critical first step prior to the mobilization of coping resources to manage a health threat.
Mental schemas are formed, activated, and modified in response to information about an illness. These schemas have five main components: identity, perceived consequences, timeline, perceived cause, and cure or control.(15) Identity includes the label and the symptoms of an illness, such as chest pain. Consequences are beliefs about the seriousness of the illness and its potential influence on everyday life or normal functioning. Timeline is the length of time the illness is expected to last. Cause is the biological, psychological, or environmental factor believed to cause the illness. Cure or control refers to the person’s perceived ability to cure or control the illness. Additional dimensions recently added to the CSM, which are pertinent to this study are acute or chronic; two subcomponents of control: treatment control and personal control; illness coherence, which reflects the clarity with which the person understands the illness; and emotional representations, which reflect distress and anger in response to illness.(16) In this study we used a three step analytic approach to (1) identify predictors of a rapid response time, (2) identify subjects with a change in the value of these predictors between baseline and three months follow-up, and (3) compare participants with and without the favorable pattern of response three months after the intervention.
2. Methods
The study was reviewed and approved by Institutional Review boards at each local site. We enrolled 3,522 patients previously diagnosed with ischemic heart disease into a randomized controlled trial known as PROMOTION. The study design has been previously described,(4) but in brief, patients were randomized to receive a single, face-to-face education session with a reinforcing telephone call that occurred approximately one month later or to a control group that received care-as-usual. The content of the education session is described below. Data were collected at enrollment, 3- and 12-months follow-up; data collected at 3-months were the focus of this analysis. All participants were followed for two years to ascertain the effect of the intervention on the time taken to seek care for ACS symptoms. Physicians caring for the patients and the research assistants collecting follow-up data were blinded to study assignment.
Patients were recruited from in-hospital and out-patient settings in the United States (n=1985, 56.4%), Australia and New Zealand (n=1537, 43.6%). For this analysis, only those 490 subjects who sought care for an ACS event were included (N=272 intervention group, N=218 control group). Enrollment occurred between 2001 and 2003. Patients were eligible for the study if they had a diagnosis of ischemic heart disease, confirmed by their physicians or hospital medical records, and if they lived independently (i.e., not in an institutional setting). Patients were excluded if they were unable to participate in data collection because of an inability to read or understand English or a major and uncorrected hearing loss. Patients also were excluded if they had a serious complicating comorbid illness such as a psychiatric illness, impaired cognition, or a terminal illness.
The initial contact with patients was a face-to-face interview conducted in a place convenient to the patient (e.g., out-patient clinic, physician’s office, or patient’s home). The study was explained in detail and written informed consent was obtained from all participants. Baseline data were collected following enrollment and prior to randomization. Subsequent data were collected at a convenient location or by telephone after the patients had received a mailed copy of the data collection instruments.
The intervention, described in detail elsewhere,(4) was based on the CSM, with ACS symptoms conceptualized as the stimulus that patients must process both cognitively and emotionally. Patients in the intervention group received structured education in the three areas recommended by National Heart Lung and Blood Institute Working Group on Educational Strategies to Prevent Prehospital Delay in Patients at High Risk for Acute Myocardial Infarction—information about ACS, anticipated emotional issues, and social factors that influence the response (http://www.nhlbi.nih.gov/about/nhaap/nhaap_pd.htm).
Information focused on typical and atypical symptoms and possible variability in symptom presentation. Study participants were advised about when and how to take aspirin and nitroglycerin and to call the Emergency Medical Service (EMS) immediately if their discomfort was not relieved rapidly. The National Heart Attack Alert Program advisory form was provided to all intervention group participants. The emotional component of the intervention led patients through the process of anticipating their emotional responses to ACS symptoms that might lead to delay. Prior experiences accessing the medical system were discussed. Role playing was used to help patients deal with potential scenarios. Social factors were addressed by asking patients to bring their spouse, another family member, or a friend to the intervention session if possible. Spouses and significant others were “deputized” to act as the decision maker if the patient hesitated to call EMS in the event of cardiac symptoms.
The intervention was delivered in a quiet, private setting and required, on average, 40 minutes. One month after the initial intervention session, patients in the intervention group were telephoned and the main points of the intervention session were reviewed. The usual length of the phone call was 15 minutes.
Variables used in this analysis were time to first emergency department (ED) presentation and demographic (age, gender, education, insurance status), clinical (history of angina), treatment related (cardiologist provider, prior participation in cardiac rehabilitation, presence of the family at the intervention), and psychosocial (ACS attitudes, ACS beliefs, ACS knowledge, anxiety, depression, and perceived control) factors.
Data collected from the medical record at baseline included clinical history, type of health care insurance, and the specialty of the treating physician. Standardized questionnaires were used to collect data on the sociodemographic, psychosocial, and prior participation in cardiac rehabilitation. Presence of the family at the intervention and whether reinforcement was provided one month later were noted in the intervention records. All data were entered via the Internet into a database specifically designed for this study that had appropriate privacy safeguards.
Perceived control was measured using the Control Attitudes Scale-Revised (CAS-R), an 8 item scale scored by adding the item scores, reversing 2 items. Total scores range from 8 to 40; higher scores indicate greater perceived control. Scale items measuring perceived control address the perception of being able to manage one’s heart condition by doing “all the right things” and being able to cope with the heart condition. A typical item from the scale is: When I manage my personal life well, my heart condition does not bother me as much. Cronbach alpha coefficient was .72 in this sample. Construct validity has been previously established.(17)
Emotions (i.e., anxiety and depression) were measured using the Multiple Affect Adjective Checklist (MAACL)(18), a list of 132 alphabetically ordered adjectives that are either negative (e.g. fearful) or positive (e.g. calm). Responses to relevant negative adjectives are summed and positive adjectives are subtracted to calculate scores. Internal consistency in this study was .79 for anxiety and .86 for depression. Convergent validity has been established.(19)
Knowledge, attitudes and beliefs about ACS were measured using the ACS Response Index.(20) This self-report instrument has 31 items in three embedded scales. Knowledge about ACS is measured with 21 items (e.g., lower abdominal pain) rated yes or no as symptoms of a heart attack (alpha .82 in this sample). Another 12 Likert-type items assess patients’ attitudes toward ACS (5 items) and beliefs about the appropriate responses to ACS symptoms (7 items) (alpha .76 in this sample). Scale items reflecting higher, more accurate ACS beliefs address getting to the hospital as soon as possible with chest pain, not being embarrassed to go to the hospital if a heart attack is suspected, and taking an ambulance, regardless of cost. Items reflecting more positive attitudes focus on symptom recognition and confidence in the ability to get help for oneself or someone else if a heart attack was suspected. Discriminant validity of the ACS Response Index has been established.(20)
All analyses were restricted to admissions for clinically validated cardiac events. To identify all such events, participants were asked to telephone the research office if they sought medical treatment for possible ACS symptoms. In addition, all participants were called every six months and asked if they had experienced ACS symptoms and sought medical care. During these phone calls subjects were queried about these ACS symptoms, and only 25 symptoms not on the list were mentioned; only 2 of these symptoms were “anxiety”. The most commonly added symptom was “back pain”. Electronic hospital records were screened whenever available. In all cases of admission to the emergency department, medical records were reviewed by registered nurses to determine ED diagnosis, prehospital delay time, and mode of transport to the hospital. Time from symptom onset to hospital presentation was obtained from the hospital medical record or, in those cases with no notation in the medical record, from the EMS prehospital medical reports.
We used a three step analytic procedure to identify and describe the subjects who responded to the intervention. First, using baseline data from the sample experiencing an acute event, we tested anxiety and perceived control as predictors of delay time. Next, using only the intervention group, we examined the change in the value of the significant predictors identified in step one between baseline and three months follow-up. The objective was to identify subjects with the desired pattern of change following receipt of the intervention. Those subjects who demonstrated the desired pattern were classified as responders. Finally, a descriptive analysis was performed to identify any differences in demographic, clinical, or psychosocial characteristics between responders and non-responders. Here we tested the hypothesis that knowledge, attitudes, and beliefs would differ between responders and non-responders.
In step one, delay time was first log transformed to better fit the assumptions of regression modeling. Then, a multiple regression model was used to assess the significance of the hypothesized covariates in explaining response time in the full sample of 490. A decrease in anxiety and perceived control were associated with shorter delay time.
In step two, the intervention group (N=272) was examined to identify those who experienced a decrease in anxiety and perceived control from baseline to 3-months. After computing the difference between the 3-month and baseline values of anxiety and perceived control, a multiple regression model was used to predict the difference while adjusting for the baseline values of both variables. We classified subjects with decreases in both anxiety and perceived control to be responders to the intervention.
In step three, we compared responders to non-responders from the intervention group in terms of demographics, clinical, and psychosocial factors. Pearson’s Chi-Square was used to assess the significance of the bivariable relationship between being a responder and any categorical predictor. A simple comparison of means via Student’s two-sample t-test was used to summarize the relationship for continuous variables with an F-test for equal variances used to determine whether or not homogeneity of variances should be assumed. Together, these three analytic steps answered the question of who was most likely to respond to the educational intervention provided in this study. All analyses were performed using SAS v. 9.2.
3. Results
The total sample of 490 was predominantly Caucasian (90.4%), male (64.1%), 65 years of age or older (61.8%), well-educated (58.5% with at least some college), and under the care of a cardiologist (84.4%). The median prehospital delay time in hours was 2.20 in the experimental group and 2.25 in the control group (p>.05).(5)
In the first step, the multiple regression models identified anxiety and perceived control as significantly explaining the variability in delay time (Table 1). The positive terms for anxiety and perceived control suggest that subjects with lower anxiety and lower perceived control had shorter delay times.
Table 1.
Regression Model for the Log Transformed Delay Time (N=490)
| Parameter Estimates | |||
|---|---|---|---|
| Variable | DF | Estimate | p-value |
| Intercept | 1 | 1.75 | <.0001 |
| Control | 1 | 0.013 | 0.0209 |
| Anxiety | 1 | 0.012 | 0.0336 |
The positive coefficient associated with anxiety and perceived control suggests that as anxiety and perceived control decrease, delay time also decreases.
ACS = acute coronary syndrome
Having identified lower anxiety and perceived control as significant predictors of shorter delay time, in step two, a predicted difference in these variables over three months was computed. A subgroup of 73 subjects (26.8%) of the 272 intervention group participants had a decrease in both anxiety and perceived control within three months after participating in the intervention. As seen in table 2, the regression parameter estimates suggest that subjects with higher baseline anxiety and perceived control were more likely to be responders. At baseline, responders had a mean MAACL score that was approximately twice as high as non-responders. Notably, though, higher values of baseline anxiety and perceived control were associated with smaller differences between 3-months and baseline.
Table 2.
Regression Models for the 3-month differences in Perceived Control and Anxiety (N=272)
| Perceived Control | |||
|---|---|---|---|
| Variable | DF | Estimate | p-value |
| Intercept | 1 | 13.28 | <.0001 |
| Baseline Control | 1 | −0.41 | <.0001 |
| Baseline Anxiety | 1 | −0.15 | 0.0093 |
| Anxiety | |||
|---|---|---|---|
| Variable | DF | Estimate | p-value |
| Intercept | 1 | 5.91 | .0031 |
| Baseline Anxiety | 1 | −0.36 | <.0001 |
| Baseline Control | 1 | −0.11 | 0.0626 |
The negative coefficient associated with baseline perceived control suggests that adjusting for baseline anxiety, a higher baseline value of perceived control is associated with a smaller difference in perceived control observed between 3-months and baseline. A similar interpretation follows for anxiety.
In step three, we compared responders (N=73) and non-responders (N=198) in terms of ACS knowledge, attitudes, beliefs, demographic, clinical, and psychosocial variables. As seen in Table 3, there was no difference in knowledge, attitudes, or beliefs between responders and nonresponders. The only demographic characteristic that differed significantly from homogeneity in the proportion of responders was insurance status with subjects who were uninsured or government-insured, including those served by the Veterans Affairs system, being most likely to be responders in comparison with the other groups. The only psychosocial characteristic, other than anxiety and perceived control, that differed significantly between responders and nonresponders was baseline depression. Responders were significantly more depressed than nonresponders. No differences were identified in clinical characteristics.
Table 3.
Demographic, Clinical, and Psychosocial Characteristics of Intervention Group Participants (N=272) Separated by Those who Responded to the Intervention and Those Who Did Not Respond
| Patient Characteristics | Total | Responders N=73 | Non-Responders N=198 | p-value |
|---|---|---|---|---|
| Age (years) | 0.463 | |||
| < 65 yrs | 111 | 29 | 82 | |
| 65–79 yrs | 121 | 34 | 87 | |
| 80+ yrs | 40 | 10 | 30 | |
| Gender | 0 | 0.358 | ||
| Male | 165 | 41 | 124 | |
| Female | 107 | 32 | 75 | |
| Marital Status | 0 | 0.340 | ||
| Not Currently Married | 93 | 28 | 65 | |
| Married or Cohabit | 178 | 44 | 134 | |
| Education | 0 | 0.787 | ||
| Some High School | 57 | 17 | 40 | |
| Completed High School | 44 | 14 | 30 | |
| Some College | 40 | 9 | 31 | |
| Completed College | 46 | 13 | 33 | |
| Other | 85 | 20 | 65 | |
| Annual Income | 0 | 0.256 | ||
| <$15,000 | 61 | 23 | 38 | |
| $15,000–$30,000 | 59 | 15 | 44 | |
| $30,000–$45,000 | 37 | 7 | 30 | |
| $45,000–$60,000 | 37 | 8 | 29 | |
| >$60,000 | 53 | 11 | 42 | |
| Did Not State | 23 | 7 | 16 | |
| Insurance | 0 | 0.006 | ||
| Uninsured, government, Veterans Affairs | 137 | 47 | 90 | |
| Any private insurance | 134 | 26 | 108 | |
| Insured for Ambulance | 0 | 0.963 | ||
| No | 36 | 10 | 26 | |
| Yes | 208 | 57 | 151 | |
| History of Angina | 0 | 0.124 | ||
| No | 78 | 16 | 62 | |
| Yes | 185 | 55 | 130 | |
| Care by a Cardiologist | 0 | 0.540 | ||
| No | 53 | 16 | 37 | |
| Yes | 219 | 57 | 162 | |
| Presence of Family at Intervention | 0.566 | |||
| No | 169 | 39 | 130 | |
| Yes | 48 | 13 | 35 | |
| Anxiety from MAACL at Baseline | 272 | 10.05 (9.37–10.74) | 4.99 (4.47–5.51) | <.0001 |
| Perceived Control Score at Baseline | 272 | 31.21 (30.61–31.83) | 28.92 (28.25–29.59) | <.0001 |
| Depression | 271 | 17.25 (16.04–18.46) | 11.67 (10.76–12.58) | <.0001 |
| ACS Knowledge Score at Baseline | 272 | 19.09 (18.48–19.71) | 18.58 (18.23–18.96) | 0.162 |
| ACS Attitudes Score at Baseline | 272 | 14.72 (14.09–15.35) | 14.72 (14.35–15.10) | 0.994 |
| ACS Belief Score at Baseline | 272 | 22.72 (21.84–23.60) | 22.78 (22.32–2.324) | 0.908 |
MAACL = Multiple Adjective Affect Check List
ACS=acute coronary syndrome
4. Discussion and Conclusions
4.1 Discussion
The results of this analysis suggest that an intervention that decreases anxiety and perceived control may decrease ACS treatment-seeking delay. The goal of decreasing anxiety was anticipated but the beneficial effect of decreasing perceived control was surprising. We have previously shown that increases rather than decreases in perceived control are associated with lower anxiety and better outcomes.(8, 12)
These results suggest that maintaining a high level of perceived control during an acute illness event may be counterproductive. The beneficial decrease in perceived control may be able to be explained by accounting for the passage of time. That is, it may be the change from an early perception of control to a realization that true control is lacking when it comes to ACS that stimulated these responders to seek care. When an illness is acute, a high level of perceived control coupled with low anxiety can result in self-deception, denial, and failure to seek care (Figure 1).(21) When perceived control is high and anxiety is high, the threat may be perceived appropriately but the anxiety may cause an inability to relinquish control to others. Relinquishing control may be recognized by patients as beneficial in response to acute symptoms. Perhaps when perceptions of control decrease, acute symptoms force patients to deal appropriately with the situation.(22)
Figure 1.
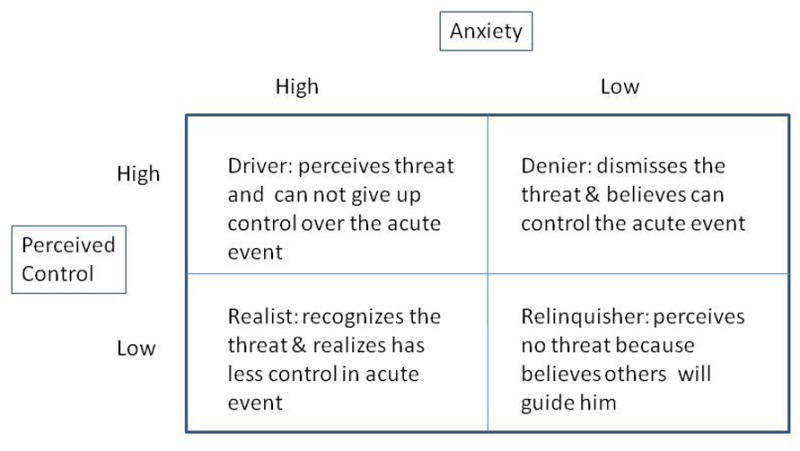
Graphic Depiction of the Manner in which Anxiety and Perceived Control were Hypothesized to Interact to Influence Treatment-Seeking Delay
Most interventions aimed at decreasing delay in response to ACS symptoms, including our own, have focused on increasing knowledge, changing attitudes, and influencing beliefs about the need to seek care. Thus, we hypothesized that responders would have an increase in ACS knowledge, attitudes, and beliefs. It was surprising, therefore, that the responders experienced no change in any of these three key factors within the first three months after the intervention. This finding suggests that tailoring interventions to address the psychosocial responses may be more important than addressing knowledge, attitudes, and beliefs. That said, though, discussions of knowledge, attitudes, and beliefs may be the method by which psychosocial responses are influenced. Other factors such as social support or the availability of help are known to influence prehospital delay time. Although these factors were not significant in this analysis does not indicate that they do not influence help-seeking behavior. Support is a major influence on psychosocial responses. Further research is needed to clarify the interaction between knowledge, attitudes, beliefs, anxiety, and perceived control.
Another interesting finding from this study was that the intervention appears to have been effective in an unlikely group of individuals—those without private health insurance. This is a hopeful finding that suggests that this style of intervention may be useful in decreasing health disparities in low income groups. Others have found that low income groups delay seeking care for acute symptoms.(23) For example, in a sample of predominantly African American women, they delayed an average of 20.4 hours for ACS symptoms (median = 4.5 hours); most (69%) delayed more than one hour. The major factor associated with longer delay in this low-income group was the belief that she could not personally ever have an acute myocardial infarction. It appears that our intervention approach might be useful in this particular group.
Limitations of this study were the use of primarily self-report data, although treatment seeking delay was measured objectively from the medical records. However, the major characteristics of responders were psychosocial, which must be judged by self-report. Thus, self-report is not judged to be a major limitation of this analysis. Our sample was largely Caucasian, so we could not consider race or ethnicity as a factor. Finally, as the original trial produced a null result for the primary outcome of prehospital delay time, these results must be interpreted considering the possibility that the intervention was too weak to effect change not only in the primary outcome but also in the underlying psychosocial mechanisms.
4.2 Conclusion
In conclusion, the results of this study suggest a specific desired pattern of response—a decrease in anxiety and perceived control in response to an intervention of this type. Only 26.8% of those in the intervention group responded appropriately. Further research is needed to understand how perceptions of control change with time and reflection. These data suggest that perhaps the ultimate goal of an intervention designed to improve the response to ACS symptoms is one that decreases anxiety and perceived control.
4.3 Practice Implications
The results of this study challenge our existing beliefs about anxiety and perceived control. Those most likely to respond to this type of educational intervention were most likely to be those experiencing a decrease in both anxiety and perceived control following the intervention. New intervention approaches aimed at decreasing both anxiety and perceived control are needed.
Acknowledgments
Funding was provided by the NIH National Institute of Nursing Research R01-NR07952.
Footnotes
Barbara Riegel had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Barbara Riegel, School of Nursing, University of Pennsylvania, Philadelphia, PA, USA.
Angelo Elmi, Department of Epidemiology and Biostatistics, The George Washington University School of Public Health and Health Services, Washington D.C., USA.
Debra K. Moser, College of Nursing, University of Kentucky, Lexington, KY, USA.
Sharon McKinley, Nursing Midwifery and Health, University of Technology Sydney and Northern Sydney Central Coast Health, Australia.
Hendrika Meischke, Department of Health Services, University of Washington, Seattle, WA, USA.
Lynn V. Doering, School of Nursing, University of California, Los Angeles, USA.
Patricia Davidson, School of Nursing and Midwifery, Curtin University, Sydney, Australia.
Michele Pelter, School of Nursing, University of Nevada, Reno, NV, USA.
Heather Baker, University of Auckland, Auckland, New Zealand.
Kathleen Dracup, School of Nursing, University of California, San Francisco, CA, USA.
References
- 1.Goldberg RJ, Steg PG, Sadiq I, Granger CB, Jackson EA, Budaj A, et al. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry) Am J Cardiol. 2002 Apr 1;89(7):791–6. doi: 10.1016/s0002-9149(02)02186-0. [DOI] [PubMed] [Google Scholar]
- 2.Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation. 2006 Jul 11;114(2):168–82. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- 3.Luepker RV, Raczynski JM, Osganian S, Goldberg RJ, Finnegan JR, Jr, Hedges JR, et al. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: The Rapid Early Action for Coronary Treatment (REACT) Trial. JAMA. 2000 Jul 5;284(1):60–7. doi: 10.1001/jama.284.1.60. [DOI] [PubMed] [Google Scholar]
- 4.Dracup K, McKinley S, Riegel B, Mieschke H, Doering LV, Moser DK. A nursing intervention to reduce prehospital delay in acute coronary syndrome: a randomized clinical trial. J Cardiovasc Nurs. 2006 May–Jun;21(3):186–93. doi: 10.1097/00005082-200605000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Dracup K, McKinley S, Riegel B, Moser DK, Meischke H, Doering LV, et al. A randomized clinical trial to reduce patient prehospital delay to treatment in acute coronary syndrome. Circ Cardiovasc Qual Outcomes. 2009 Nov;2(6):524–32. doi: 10.1161/CIRCOUTCOMES.109.852608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moser DK, Riegel B, McKinley S, Doering LV, An K, Sheahan S. Impact of anxiety and perceived control on in-hospital complications after acute myocardial infarction. Psychosomatic medicine. 2007 Jan–Feb;69(1):10–6. doi: 10.1097/01.psy.0000245868.43447.d8. [DOI] [PubMed] [Google Scholar]
- 7.Shibeshi WA, Young-Zu Y, Blatt CM. Anxiety worsens prognosis in patients with coronary artery disease. J Am Coll Cardiol. 2007;49(20):2021–7. doi: 10.1016/j.jacc.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Dracup K, Westlake C, Erickson VS, Moser DK, Caldwell ML, Hamilton MA. Perceived control reduces emotional stress in patients with heart failure. J Heart Lung Transplant. 2003 Jan;22(1):90–3. doi: 10.1016/s1053-2498(02)00454-0. [DOI] [PubMed] [Google Scholar]
- 9.Evangelista LS, Moser D, Dracup K, Doering L, Kobashigawa J. Functional status and perceived control influence quality of life in female heart transplant recipients. Journal of Heart and Lung Transplantation. 2004 Mar;23(3):360–7. doi: 10.1016/S1053-2498(03)00196-7. [DOI] [PubMed] [Google Scholar]
- 10.Moser DK, Dracup K. Impact of cardiopulmonary resuscitation training on perceived control in spouses of recovering cardiac patients. Res Nurs Health. 2000 Aug;23(4):270–8. doi: 10.1002/1098-240x(200008)23:4<270::aid-nur3>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 11.Moser DK, Dracup K, Doering LV. Effect of cardiopulmonary resuscitation training for parents of high-risk neonates on perceived anxiety, control, and burden. Heart Lung. 1999 Sep–Oct;28(5):326–33. doi: 10.1053/hl.1999.v28.a101053. [DOI] [PubMed] [Google Scholar]
- 12.Moser DK. “The rust of life”: impact of anxiety on cardiac patients. Am J Crit Care. 2007 Jul;16(4):361–9. [PMC free article] [PubMed] [Google Scholar]
- 13.Leventhal H, Cameron L. Behavioral therories and the problem of compliance. Patient Educ Counseling. 1987;10:117–38. [Google Scholar]
- 14.Leventhal H, Meyer D, Nerenz D. The common sense representation of illness danger. In: Rachman S, editor. Medical psychology. New York: Pergamon Press; 1980. pp. 17–30. [Google Scholar]
- 15.Hagger MS, Orbell S. A meta-analytic review of the common-sense model of illness representations. Psychology and Health. 2003;18(2):141–84. [Google Scholar]
- 16.Moss-Morris R, Petrie KJ. Experimental evidence for interpretive but not attention biases towards somatic information in patients with chronic fatigue syndrome. Br J Health Psychol. 2003 May;8(Pt 2):195–208. doi: 10.1348/135910703321649169. [DOI] [PubMed] [Google Scholar]
- 17.Moser DK, Riegel B, McKinley S, Doering LV, Meischke H, Heo S, et al. The Control Attitudes Scale-Revised: psychometric evaluation in three groups of patients with cardiac illness. Nurs Res. 2009 Jan–Feb;58(1):42–51. doi: 10.1097/NNR.0b013e3181900ca0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zuckerman M, Lubin B, Robins S. Validation of the multiple affect adjective check list in clinical situations. J Consult Psychol. 1965 Dec;29(6):594. doi: 10.1037/h0022750. [DOI] [PubMed] [Google Scholar]
- 19.Maloni JA, Park S, Anthony MK, Musil CM. Measurement of antepartum depressive symptoms during high-risk pregnancy. Res Nurs Health. 2005 Feb;28(1):16–26. doi: 10.1002/nur.20051. [DOI] [PubMed] [Google Scholar]
- 20.Riegel B, McKinley S, Moser DK, Meischke H, Doering L, Dracup K. Psychometric evaluation of the Acute Coronary Syndrome (ACS) Response Index. Res Nurs Health. 2007 Dec;30(6):584–94. doi: 10.1002/nur.20213. [DOI] [PubMed] [Google Scholar]
- 21.Goldbeck R. Denial in physical illness. J Psychosom Res. 1997 Dec;43(6):575–93. doi: 10.1016/s0022-3999(97)00168-2. [DOI] [PubMed] [Google Scholar]
- 22.Sirri L, Fabbri S, Fava GA, Sonino N. New strategies in the assessment of psychological factors affecting medical conditions. J Pers Assess. 2007 Dec;89(3):216–28. doi: 10.1080/00223890701629649. [DOI] [PubMed] [Google Scholar]
- 23.Harralson TL. Factors influencing delay in seeking treatment for acute ischemic symptoms among lower income, urban women. Heart Lung. 2007 Mar–Apr;36(2):96–104. doi: 10.1016/j.hrtlng.2006.08.002. [DOI] [PubMed] [Google Scholar]


