Abstract
Background:
Telemedicine has emerged as an efficient means of distributing professional medical expertise over a broad geographic area with few limitations to the various services that can be provided around the globe. Telepathology is particularly well suited to distributing subspecialty expertise in certain environments in an economical fashion, while preserving centers of excellence.
Materials and Methods:
After a decade of intrainstitutional teleneuropathology for intraoperative consultation, we expanded our practice to cross state lines and communicate between geographically and financially separate medical centers.
Results:
The result was an effective means of distributing neuropathological expertise while at the same time preserving a professional center of excellence. While technical and legal (i.e., physician licensing) barriers were surmounted, expected and unexpected issues related to communication required commitment on the part of multiple individuals with diverse expertise and responsibilities.
Conclusion:
Lessons learned from this successful venture can be used to facilitate future efforts in this ever-growing practical vehicle for distributing pathology subspecialty expertise.
Keywords: Neuropathology, pathology practice, professional licensing, telepathology
BACKGROUND
Telepathology has been defined as “the interpretation of transmitted digital histologic images while physically separated from the derivative glass slides.”[1] In many cases this involves viewing glass slides using a computer remotely connected to a robotic microscope. The capacity to perform telepathology has been available for decades (for review, see [2–7]), but with exponential improvements in data transmission, many of the technical barriers have melted away and the reality of providing such service is readily available on a variety of platforms. The University of Pittsburgh Medical Center (UPMC) and University of Pittsburgh Physicians (UPP) have been engaged in telepathology efforts for over a decade.[7,8] Our interest is founded in our health care delivery model based on centers of excellence. A single widely distributed health system faces substantial challenges in delivering the highest quality health care over a geographically diverse region.
Perhaps this challenge is best illustrated in the subspecialty of neuropathology where we have published our experience with intrainstitutional intraoperative consultation.[8] After a decade of experience in this area, we recently examined the feasibility of providing intraoperative consultation to an institution in a different state. Having run such a trial for over a year, we are providing the following description of our experience, lessons learned, and discussion of what the future may hold for developments in this ever-changing health care environment.
In the spring of 2008, Ameripath and the St. Vincent Neuroscience Institute of St. Vincent Indianapolis Hospital approached the Division of Neuropathology at UPMC regarding the feasibility of providing intraoperative consultations for specialty neurosurgery. As this was an area that UPMC had almost a decade of experience in within our own hospital system, we elected to pursue this as a step toward a more generalized distribution of subspecialty surgical pathology expertise.
St. Vincent Hospital is staffed by four or five Ameripath pathologists on a daily basis, providing frozen section coverage (10–30 frozen sections per day) and medical directorship of laboratory services. The surgical pathology volume at the St. Vincent Indianapolis campus is approximately 18,000 cases per year. Surgical pathology at the Indianapolis campus serves St. Vincent Indianapolis Hospital, Peyton Manning Children's Hospital, and St. Vincent Women's Hospital. Combined, those facilities comprise an 800-bed tertiary care hospital.
The St. Vincent Neuroscience Institute is a collaborative endeavor between St. Vincent Indianapolis Hospital and four private neuroscience physician practices: Goodman Campbell Brain and Spine, Indiana Neurology Associates, Josephson Wallack Munshower Neurology, and Northwest Radiology. St. Vincent Indianapolis Hospital is part of the 20-ministry St. Vincent Health System serving 46 counties in central Indiana. St. Vincent Health is a member of Ascension Health, the nation's largest not-for-profit Catholic Healthcare System.
Goodman Campbell Brain and Spine is an independent group of 30 neurosurgeons who have a base at St. Vincent Indianapolis Hospital. Six neurosurgeons are primarily focused at St. Vincent but many others are present on a part-time basis. As of spring 2008, anatomical and clinical pathology services are provided by Ameripath.
UPMC is an integrated global health enterprise with almost 50,000 employees headquartered in Pittsburgh, Pennsylvania. UPMC is closely affiliated with the University of Pittsburgh of the Commonwealth System of Higher Education (University of Pittsburgh). UPMC operates 20 academic, community, and specialty hospitals and 400 outpatient sites both domestically and internationally and employs more than 2,700 physicians in more than 20 specialties. Telepathology is used broadly throughout the system in several subspecialties. Beyond telepathology, UPMC and its physicians provide telemedicine services in a variety of subspecialties including stroke, radiology, dermatology, trauma, psychiatry, wound, critical care medicine, and maternal fetal medicine.
NEED FOR INTRAOPERATIVE NEUROPATHOLOGY CONSULTATION
Each group involved in the decision process to provide teleneuropathology approaches the issues with a different perspective.
Neurosurgery/St. Vincent perspective
Due to the large volume of neurosurgical cases performed at St. Vincent Hospital, it is considered vital to have reliable neuropathology services available. Over previous years, it was not possible with a single neuropathologist (NP) to cover every day of service. While it was relatively straightforward to seek a second opinion from another site on a permanent specimen, an intraoperative consultation does not afford the same opportunity. Because accurate intraoperative frozen sections influence the surgical plan Goodman Campbell worked with St. Vincent and Ameripath to seek solutions for neuropathology coverage. Board-certified NPs are rare and the neurosurgical volume at St. Vincent would not support the recruitment of a full-time individual. The decision to use teleneuropathology was driven by a commitment to provide the best possible care to all patients.
Ameripath perspective
All of the parties involved (local pathology leadership, neurosurgery leadership, and hospital administration) recognized the challenge of providing satisfactory neuropathology services without an on-site board-certified NP. This challenge was the most acute at the time of intraoperative frozen section, when the level of diagnostic confidence was widely felt to be insufficient by the neurosurgery staff. Consideration was given to cost sharing between Ameripath and St. Vincent Hospital in hiring an on-site NP, but the timeline for recruiting was felt to be unacceptably long. Additionally, the pool of available board-certified NP willing to practice in a community hospital setting (where the majority of the daily practice activities are not focused on neuropathology) is small. For these reasons, a telepathology solution was suggested in early discussions between Ameripath, the Neurosurgery Department, and St. Vincent Hospital.
UPMC neuropathology division perspective
A substantial component of an academic center mission is providing a training environment for subspecialty pathology fellows as well as medical residents. While intraoperative neurosurgical consultations are abundant within our own hospital system (>500 consultations per year), the expansion of case volume would provide more abundant and potentially varied case material for trainees and the four attending surgical NPs. It is a general axiom in pathology that more experience translates in tangible and intangible means to greater expertise. Therefore, we also looked upon this venture as a means of sharpening our diagnostic acumen while at the same time expanding our teaching case volume.
Having learned of UPMC's experience in telepathology through a review of the medical literature in this area, Ameripath approached the Division of Neuropathology at UPMC to discuss what sort of assistance could be provided. Initial discussions centered on the scope of desired consultation, compatibility of information systems, and legal issues related to such a service. While there are a variety of existing telemedicine business models, none of the parties involved in the proposed anatomical neurotelepathology arrangement was very familiar with these systems in other branches of medicine and it was not clear how analogous these other systems were to the proposed venture. Consequently, discussions languished over the subsequent 6 months with very little progress. Basically, all parties involved could conceive of dozens of hurdles that would potentially have to be cleared, and in sum these hurdles loomed insurmountable.
Despite the frustratingly nebulous nature of many of the problems, the proposal was clearly in everyone's best interest (e.g., fulfilling an academic department's clinical teaching mission and fulfilling a private practice's need to have highest level of expertise), so it was decided mutually to put pen to paper and draft a potential contract that could be circulated between all involved parties. Naturally, conversations began and were initially restricted to pathologists, but the list of individuals rapidly expanded and precipitated a large number of conference calls before everyone could agree on the scope of the project and who would need to talk to whom to get the project off the ground.
Legal
The health care attorney's perspective regarding telemedicine is one of challenge and diligence. The medical, scientific, and technological advances related to physicians being able to provide safe and efficient telemedicine services to patients throughout the world remain very far ahead of the legal precedents and standards (e.g., provider licensing, credentialing, privacy issues) that are only now in 2011 beginning to catch up to this ever-evolving complex method of delivering safe and effective health care. In the litigious and highly regulated era we live in, no sane physician would consider moving forward in such a complex venture without appropriate counsel. Several daunting hurdles loomed on that horizon. Those hurdles included physician licensing and credentialing issues (did the UPMC physicians need licenses in the state of Indiana and clinical staff privileges for St. Vincent Hospital?), insurance issues (Indiana versus Pennsylvania law), indemnification issues (what happens if one or more of the parties is subject to a lawsuit?), and other legal and contractual issues.
Medical–legal issues related to telepathology have recently been reviewed. [1] Historically, patient safety-related issues have been the purview of state rather than federal law. Thus providing consultation across state boarders can potentially involve the jurisdiction of two different states′ statutes. For intraoperative consultation, a conservative approach to this potential complexity would be for the telepathologist to obtain professional licensing in the state where the patient is being treated in addition to licensure in the pathologist's home state. Based on a review of the applicable medical license laws we elected to license in Indiana all NPs involved in the telepathology agreement.
Another key issue in intraoperative telepathology is whether the remote pathologist is providing a diagnosis independent of a local pathologist, or functioning as a consultant with the intrastate pathologist. In the former case, it is possible that one might take the position that a physician–patient relationship existed between the patient in one state and the telepathologist in a different state. Here too, to avoid this potential construal, we elected to have the telepathologist function purely as a consultant to the local pathologist who would have final jurisdiction over all patient care.
By its very nature, telepathology moves away from a single pathologist's judgment to two (or more!). This begs the question of responsibility. While the local reviewing pathologist has to determine the adequacy of the specimen for diagnosis, the remote pathologist would be liable for determining the adequacy of the resolution of the transmitted and received images.
Finally, and perversely, the mere existence of telepathology raises new concerns. If telepathology technology is readily available and the local pathologist does not use it, does this open the door to a potential malpractice claim if injury results in the absence of subspecialty expertise? While many of these legal and regulatory issues are evolving, the medical expertise and technology advances continue to far outpace the legal and regulatory precedents in this area of health care law.. In the final analysis of our agreement, the legal issues were resolved by the parties through thoughtful and prudent research, negotiations, and careful drafting of an appropriate contractual language.
Of course the very mundane had to be hammered out – what were expected work hours, what was the price, turn-around time, etc. But these issues all proved to be uncomplicated. When a pathologist talked to another pathologist, it was very easy to communicate what was desired and then it was a matter of earnestly defining at the finest level what would be done, by who and when. For motivated professionals in the same field, to communicate in this manner is very straightforward and in truth quite an enjoyable interaction.
What proved to be key to create this collaboration was knowing in detail what we wanted to do (based upon our intrainstitutional use of telepathology) and then getting the experts at two different institutions talking to each other. We are all components of very complex systems and thus, by necessity, we rely heavily upon our colleagues outside of our field to work with us to make complex systems work. Since every institution is organized uniquely there is no pat formula for who to bring to the table. For example, at Indianapolis, the hospital administration was independent of the pathology group while in Pittsburgh it was part of the same department. Cost centers also had different boundaries at the different institutions, thus requiring negotiation of individual responsibilities for equipment purchases and professional contracts.
MATERIALS AND METHODS
Once the administrative issues were resolved, the technological implementation proved to be straightforward. The system included a network-connected, fully robotic microscope with a four-slide loader (Zeiss AxioImager M1 with 3 chip camera and workstation, Thornwood, NY, USA) maintained at St. Vincent with monthly color calibration. The software used is a network accessible remote graphic user interface, MedMicroscopy (Trestle Corp., Newport Beach, CA, USA), which created a "thumbnail" overview of all slides in the storage box. This dynamic system does not require the transfer of large whole slide images across interstate networks, so the necessary bandwidth is low, permitting real time viewing and therefore amenable to intraoperative consultations. The robotic microscope system supports remote operations by allowing full remote access to the functions of a microscope, including high-resolution digital imagery from the connected network computers via web-based communication. The system also has features such as rapid whole slide overview scanning for navigation, and label imagery for verification and annotation. Automatic slide changing is also supported, which allows true remote reading of cases with multiple smears from a single slide up to four slides. This version of the robotic microscope is no longer supported by the vendor; however, because the technology is constantly evolving, several companies have created comparable systems. Several simultaneous users can be connected to a single robotic microscope, allowing a virtual multiheaded consultation. Since all multiple users have control of the scope, we developed the convention that the NP would drive the viewing and other viewers could request control through the conference call.
Once the slide of interest was loaded on the robotic microscope in the St. Vincent's frozen section room, it was viewed via a remote desktop session using a virtual private network (VPN) at the UPMC NP workstation and at the viewing site (frozen section room at St. Vincent Hospital) and St. Vincent operating room (OR). Using the same VPN session, the NP is able to access the pertinent radiology images from the radiology picture archiving and communication systems (PACS), by launching the radiology image viewer from the same workstation in the frozen section room. The NP is provided with a live view of frozen section slides and smears using a 25 in., 1024 × 768, 24 bit color monitor with 52 dpi through the MedMicroscopy application. No color correction except for white balance at the viewing site is performed. Through the internet accessible control system, the NPs are able to remotely control slide loading and microscope operations such as navigating the slide (X, Y axes), changing objective lenses, and adjusting lighting, contrast, and focus (Z axis). Workflow enhancing functions such as autofocus are also present in the system. In addition, the system also permits digital photography of the case by the NP, if needed; however, we did not use this feature.
So what happened?
Our specific contractual and legal details are confidential; however they included the definition of parties and legal relationships and of needed service and market value, exclusivity of service, responsibility for equipment and medical record maintenance, hours and nature of service, term of agreement, termination with or without cause, licensure and privileging, compensation, professional liability, covenant not to disclose confidential information, compliance with applicable law, mediation/arbitration, and business associate agreement. The parties were able to finalize and execute a consultative telehealth services agreement in April, 2009. The agreement memorializes the parties′ duties, obligations, and rights. Just as important, it covers the unique legal issues often associated with telemedicine including but not limited to provider licensing, credentialing, information technology requirements, and patient privacy issues. In the end, the contractual documents captured the specific details of how UPMC could provide telepathology services to patients several hundred miles away and serves as an example of a leap forward in how parties can collaborate on a highly complex means of delivering critical health care services and simultaneously solve the numerous medical, legal, and technological issues that pertain to any telemedicine project.
Standard operating procedure
To carry out the interinstitutional consult service, we adapted our intrainstitutional standard operating procedure (SOP). By noon the day before surgery, a list of planned neurosurgical cases is transmitted by St. Vincent Neuroscience Institute to the UPMC neuropathology administration through a secured and encrypted email. This is distributed to the on-call NP who then uses a VPN connection from the UPMC workstation and remote access to the St. Vincent's frozen section room computer to access the PACS system and look up pertinent radiology reports and images. Findings from these studies are transferred to an intraoperative tracking/data acquisition form [Figure 1]. In the morning, updated neurosurgical schedules are emailed to the NP and any add-on cases are similarly evaluated. When the Indianapolis surgical pathologist (SP) is notified of the biopsy specimen, he or she text pages the UPMC NP, who then calls the SP to confer on proper processing of the case. While the SP prepares the intraoperative specimen, the NP calls the OR to confer with the neurosurgeon. The NP then remotely connects to the robotic microscope system and calls the SP to discuss the findings. While the SP and NP view the specimen, it is possible for the neurosurgeon to view on monitors in the OR in real time the microscopic findings. When the NP and SP conclude the diagnosis, the NP calls back the OR to convey the interpretation to the neurosurgeon and decide what further needs to be done Figure 2. The tracking form is completed and any problems that occurred during the procedure are recorded. In the rare instance where the system did not function, the APs handle the biopsy as they had prior to the contract. Based upon the exact reason for a system failure, the different parties could have terminated the contract.
Figure 1.
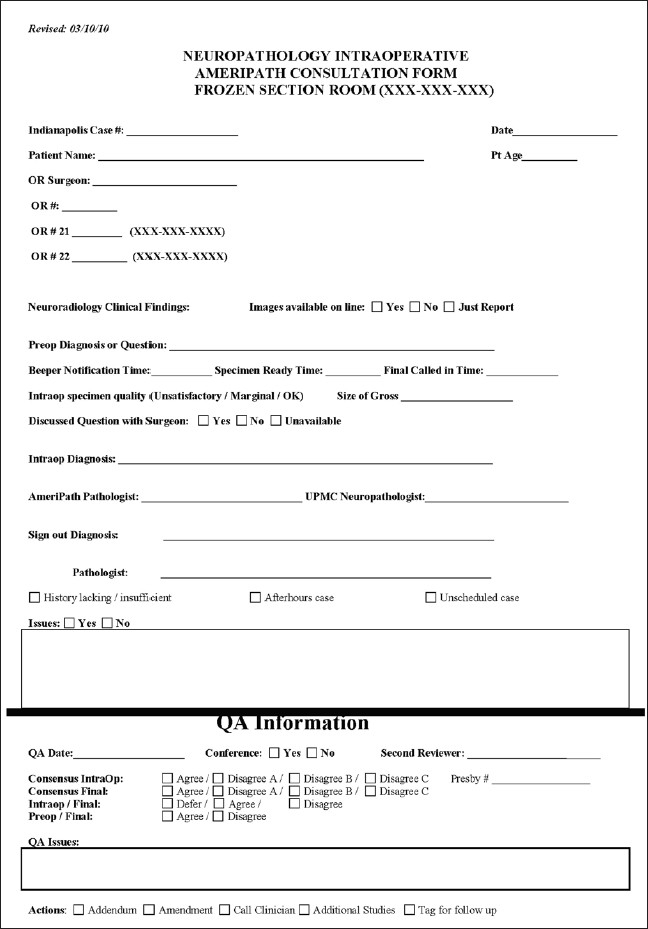
Consultation form completed prior to, during, and after intraoperative consultation. All of these fields are transferred to a database for quality improvement assessment
Figure 2.

Connections between Pittsburgh and Indianapolis sites. Robotic microscope in a frozen section suite at St. Vincent while workstations are available in the St. Vincent's frozen section suite and ORs as well as UPMC NP offices. St. Vincent's SP prepares the intraoperative specimen. The NP calls the operating room to confer with the neurosurgeon. The NP then remotely controls the robotic microscope while the image is transmitted to the SP and surgeon at St. Vincent. After discussing the findings with the SP, the NP calls the neurosurgeon
RESULTS
In the first 15 months of the interinstitutional service, we consulted on 147 neurosurgical cases. A total of four NPs participated in the review. As our tracking process evolved quickly, we developed comprehensive data on 126 of these cases (see the current tracking/data acquisition form; Figure 1). Clinical radiology was available for a preview on 55 of 102 patients (data not recorded for 24). The average age of the patient was 50 (age range 4–84 years; age not recorded for 8 patients). In 83 of the cases, all notification times were recorded. The average time from the initial notification of the NP to specimen being ready for viewing was 10 min (range 1–45 min). The average time from specimen being ready to rendering of diagnosis was 11 min (range 3–40 min), with the average time from the initial notification to diagnosis being 21 min (range 7–60 min). The College of American Pathologists (CAP) guideline for the turn-around time of frozen sections is 20 min. Neuropathology intraoperative consultations can take longer than this, irrespective of whether performed by telepathology, so when a consultation was going to take longer, this was immediately communicated to the neurosurgeons, so that they understood the reason for the delay. Since neurosurgeons had the ability to view the frozen section on monitors in the OR in real time, they could appreciate the nature of any delay. The quality of the intraoperative specimen varied but was subjectively evaluated by the NP as “OK” in 75 cases, “marginal” in 20 cases, and “unsatisfactory” in 1 case. In 30 of the cases, specimen quality was not recorded. An intraoperative diagnosis was rendered in all cases except two deferrals.
The breadth of specimen types biopsied covered a broad range of neurosurgical cases [Table 1] with approximately a third of the cases being gliomas and a quarter being metastases. In our contract, we left the decision to submit the permanent diagnosis to NP review up to the SP. Only a small fraction of the cases were submitted for permanent review where a total of eight discrepancies were noted [Table 2.] As telepathology is only a small component of Ameripath's intraoperative consultations, the CAP mandated correlations of intraoperative and permanent sections for St. Vincent as a whole to be handled independently.
Table 1.
Diagnostic class of 126 intraoperative specimens
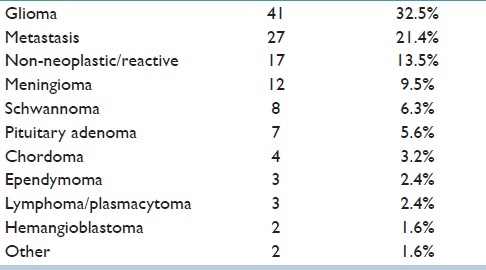
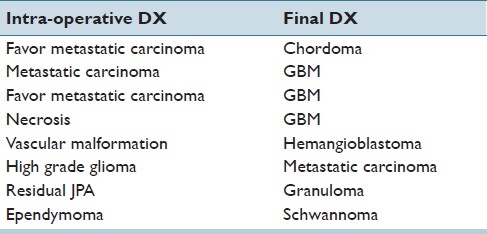
Table 2.
Intraoperative and final diagnoses on discrepant cases
CONCLUSIONS
What at times appeared to be the proverbial Gordian knot, trying to have two institutions in separate states collaborate on immediate medical procedures, eventually gave way to perseverance. Distributing medical subspecialty expertise is a challenge but as with any new enterprise, it is difficult to predict what the challenges were to be. When we began this project almost 3 years ago, certainly technology loomed as the major challenge but technology proved to be one of our lowest hurdles. Secure high-speed Internet access is now readily available throughout most of the United States and much of the world. Robotic microscopy is continually evolving but certainly at its current state offers a relatively economical (beginning around $25,000 but going as high as $250,000) means of remotely viewing specimens in real time.
From a neurosurgical perspective, this telepathology system has worked well. There have been some delays in getting the frozen section results for reasons previously stated but this is not substantially different than prior to using this technology. Two factors have made it most effective for the surgeons: (1) the ability of the pathologist to project and manipulate the images of the specimen onto the large screen monitors mounted in each of the neurosurgical ORs and (2) the direct verbal communication of the surgeon with the NP by phone directly into the OR [Figure 2]. This combination has led to the superb results described in the paper. While doctors tend to resist the new technology, this advance clearly has provided superior service to our patients with virtually no interference to the surgeon.
The practice of medicine, however, is a much more nuanced art that requires communication on many levels among many people with different perspectives. Beyond the initial face-to-face interactions with neurosurgeons at the time of designing the contract, intraoperative phone calls from the NP to the neurosurgeon and frequent follow-up calls in complicated cases were essential in maintaining professional rapport. Much of the learning curve in our implementing this system was bringing together all involved parties to be sure we understood each other. This occurred across medical disciplines and across administrative and state boundaries. What tipped the balance in favor of a working collaboration was trust between all individuals that they wanted the improved system to work and all had clear incentives to make it do so. Linking comparable departments and personnel at the two institutions was essential to be sure communication was carried out in the appropriate dialect.
The mix of cases was similar to what we have observed in our intrainstitutional studies at UPMC.[7,8] Because only a small fraction of the interinstitutional cases were subjected to neuropathological review of the permanent material, it is not possible to compare concordance rates. While there was no contractual policy defining in which cases′ permanent material would be sent for consultation, it is likely that all discordant cases were sent for review, in which case comparison of causes of discrepancies between inter- and intrainstitutional studies is of interest. Of the eight discrepant interinstitutional, intraoperative, and final diagnoses, three related to high-grade glioma versus metastatic carcinoma and two were tumor misclassifications (favor metastatic carcinoma versus chordoma and ependymoma versus schwannoma). This proportion is similar to what we reported for conventional (18 of 41) and telepathology (6 of 13) discrepancies noted in our intrainstitutional studies. Two of the discrepant cases (necrosis/GBM and vascular malformation/heamngioblastoma) probably reflected sampling issues that frequently plague small neurosurgical biopsies. Viewing the actual glass slide from the intraoperative preparation of discordant cases confirmed the difficulty of resolving the differential, but did not suggest that technical issues of image projection accounted for diagnostic difficulties. More frequently, the quality of the intraoperative specimen itself was deemed a potential contributor to the interpretive problem.
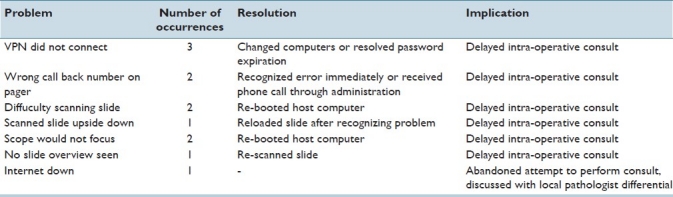
Our tracking form allowed us to record technical problems at the time of each procedure. We reviewed these issues throughout the study and revised the SOP at any point where specimen handling could be optimized. Technical problems relating to the Internet connection and the robotic microscope occurred in up to 10% of cases Table 3. Some of these related to inability to secure a VPN connection from the NP's desktop workstation, and others related to the robotic microscope's software requiring resetting. In all but one instance, these problems caused only time delays in generating the intraoperative diagnosis. In one instance, the problem could not be successfully troubleshot and the intraoperative diagnosis was rendered by the SP, as was the norm, before the telepathology consultation service was begun. During our quality improvement activities, we discovered that some of the connection problems related to unanticipated expired passwords. To avoid these and related issues, we adopted the SOP of checking the VPN connection each Monday morning to be sure it was viable.
Table 3.
Technical problems that occurred during intra-operative consultations
The next most common problem is related to specimen quality. Every pathologist has his or her own technique for preparing intraoperative specimens and so prefers reading slides using his or her own method. NPs may be one of the more finicky groups, possibly related to the types of specimens they assess. Before the contract was initiated, two of the UPMC NPs met with some of the Indianapolis SPs to review how they preferred specimens to be prepared. While this was very helpful, a more complete introduction might have improved the specimen quality. We have subsequently created a PowerPoint with a video web site that demonstrates the production of intraoperative preparations (http://neuro.pathology.pitt.edu/webstuff/Procedure%20Manual/NPIntraopPrepEmbeddedvideo.pps). More time was required to evaluate marginal quality specimens increasing the turn-around time.
Most of the other problems can be classified under the rubric of “communication” errors. These extended from communication problems common to surgical pathology (e.g., late clinical history that impacted differential diagnosis such as previous unreported history of carcinoma) to surgical cases not on the OR schedule that were added during the day. But it is in the nature of telepathology that additional communication issues were interjected. These included errors in paging to the wrong phone number or incorrect phone numbers for surgeons or operating rooms. None of these significantly degraded the service but all of them required vigilance to redouble efforts in communication with back-up information systems as simple as including common OR phone numbers on the tracking form.
But the most important communication problem we headed off before it could surface and that was the absolutely essential face-to-face meeting between the consultant NP, the SP, and the neurosurgical teams. As the digital age continues to develop, there is greater and greater pressure to cost and time saving by eliminating “inefficiencies” related to human interactions. Many of these “savings” are quite naive with respect to the significance of the importance of professional relationships. This is not a topic that gets addressed frequently at formal meetings, nor is it one that is subject to ready quantification, but it may be more important than most of the items we can quantify.
It is also true of medicine in general and subspecialty pathology practice in particular that while much of what transpires at any one moment occurs between a pathologist and a clinician, pathologists frequently consult with each other to share their diverse experiences. Telepathology offers the capacity to quickly involve more than one subspecialty pathologist with specimens under evaluation. Additionally, as part of our intrainstitutional continuous quality improvement activities, we discuss problematic cases retrospectively on a weekly basis. In addition to identifying system errors, we frequently discuss communication errors. Sharing those experiences on a weekly basis are the key to helping us anticipate and avoid future errors by refining our knowledge of how we communicate.
Finally, it is important to reflect on why subspecialty telepathology is being assessed. It is not enough to justify the endeavor simply because technologically it can be done. What gap does telepathology fill that could not be filled by simply hiring an on-site NP? While there may be a dearth of board-certified NPs for all the possible locations where their expertise could be used, even if enough highly trained individuals were available, the solution of dispersing them throughout the world would be only a temporary solution at best. Without an abundance of sub-specialty-related specimens and continual quality feedback in the form of colleagues reviewing diagnoses within a short period of time, the edge of subspecialty training would be dulled and added value diminished. Allowing subspecialists to work together in a critical mass is essential for them to preserve their diagnostic and scientific acumen. Leveraging technology to facilitate this communication is the true added value of the advance.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2011/2/1/21/80717
REFERENCES
- 1.Leung ST, Kaplan KJ. Medicolegal aspects of telepathology. Hum Pathol. 2009;40:1137–42. doi: 10.1016/j.humpath.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Dunn BE, Choi H, Almagro UA, Recla DL, Krupinski EA, Weinstein RS. Routine surgical telepathology in the Department of Veterans Affairs: Experience-related improvements in pathologist performance in 2200 cases. Telemed J. 1999;5:323–37. doi: 10.1089/107830299311899. [DOI] [PubMed] [Google Scholar]
- 3.Chorneyko K, Giesler R, Sabatino D, Ross C, Lobo F, Shuhaibar H, et al. Telepathology for routine light microscopic and frozen section diagnosis. Am J Clin Pathol. 2002;117:783–90. doi: 10.1309/W00T-2CA8-MH68-RVDV. [DOI] [PubMed] [Google Scholar]
- 4.Kaplan KJ, Burgess JR, Sandberg GD, Myers CP, Bigott TR, Greenspan RB. Use of robotic telepathology for frozen-section diagnosis: A retrospective trial of a telepathology system for intraoperative consultation. Mod Pathol. 2002;15:1197–204. doi: 10.1097/01.MP.0000033928.11585.42. [DOI] [PubMed] [Google Scholar]
- 5.Walter GF, Matthies HK, Brandis A, von Jan U. Telemedicine of the future: Teleneuropathology. Technol Health Care. 2000;8:25–34. [PubMed] [Google Scholar]
- 6.Liang WY, Hsu CY, Lai CR, Ho DM, Chiang IJ. Low-cost telepathology system for intraoperative frozen-section consultation: Our experience and review of the literature. Hum Pathol. 2008;39:56–62. doi: 10.1016/j.humpath.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 7.Horbinski C, Wiley CA. Comparison of telepathology systems in neuropathological intraoperative consultations. Neuropathology. 2009;29:655–63. doi: 10.1111/j.1440-1789.2009.01022.x. [DOI] [PubMed] [Google Scholar]
- 8.Horbinski C, Fine JL, Medina-Flores R, Yagi Y, Wiley CA. Telepathology for intraoperative neuropathologic consultations at an academic medical center: A 5-year report. J Neuropathol Exp Neurol. 2007;66:750–9. doi: 10.1097/nen.0b013e318126c179. [DOI] [PubMed] [Google Scholar]


