Abstract
Background:
Patient identification (ID) errors in point-of-care testing (POCT) can cause test results to be transferred to the wrong patient's chart or prevent results from being transmitted and reported. Despite the implementation of patient barcoding and ongoing operator training at our institution, patient ID errors still occur with glucose POCT. The aim of this study was to develop a solution to reduce identification errors with POCT.
Materials and Methods:
Glucose POCT was performed by approximately 2,400 clinical operators throughout our health system. Patients are identified by scanning in wristband barcodes or by manual data entry using portable glucose meters. Meters are docked to upload data to a database server which then transmits data to any medical record matching the financial number of the test result. With a new model, meters connect to an interface manager where the patient ID (a nine-digit account number) is checked against patient registration data from admission, discharge, and transfer (ADT) feeds and only matched results are transferred to the patient's electronic medical record. With the new process, the patient ID is checked prior to testing, and testing is prevented until ID errors are resolved.
Results:
When averaged over a period of a month, ID errors were reduced to 3 errors/month (0.015%) in comparison with 61.5 errors/month (0.319%) before implementing the new meters.
Conclusion:
Patient ID errors may occur with glucose POCT despite patient barcoding. The verification of patient identification should ideally take place at the bedside before testing occurs so that the errors can be addressed in real time. The introduction of an ADT feed directly to glucose meters reduced patient ID errors in POCT.
Keywords: Barcode, glucose meter, point-of-care testing
INTRODUCTION
Point-of-care testing (POCT) refers to diagnostic testing performed at the point-of-care or patient bedside, a process that is supervised by the central laboratory of an institution. POCT poses unique quality challenges because the testing is performed outside the well-controlled environment of the clinical laboratory. Until recently, POCT quality has not focused on the pre and postanalytical phase of testing. Most POCT errors are due to preanalytic (e.g., patient identification) and/or postanalytical (e.g., result recorded in the incorrect patient's chart) issues.[1,2] POCT errors are particularly problematic as immediate medical action is often taken on the results prior to recording the result in the medical record. Data management is fundamental to quality, and the analysis of POCT data may indicate quality trends.[3] Newer POCT devices have computerized data capture and storage functions that can collect key information at the time the test is performed and later transmit that data to a POCT data manager or hospital information system (HIS) for review.
Barcoding of patients for POCT was implemented at our institution in 2002 to automate and potentially reduce preanalytical errors caused by the manual operator data entry process. Significant error reduction over time was seen after barcode implementation. However, the goal of zero entry errors could not be reached for several reasons.[4] We found that clinical operators continued to employ manual data entry when the barcode scan was unsuccessful or unavailable. Also, some patients were found to have incorrect patient account numbers due to hospital transfer, multiple wristbands on a single patient, and selection of expired account numbers from previous hospitalizations when printing the barcoded wristbands. Other medical institutions have also reported misidentifications caused by errors in the standard barcode technology when barcodes were scanned for POC glucose testing.[5] Errors in the data entry of patient identification (ID) can cause POC results to be transferred to the wrong patient's chart, can prevent results from being transferred when results do not match an active patient account, and pose compliance issues when results cannot be billed. So, despite the implementation of patient barcoding and ongoing operator training at our institution, patient ID errors still occur. The aim of this study was to develop a solution to reduce identification errors with POCT.
MATERIALS AND METHODS
Baystate Health System conducts over 300,000 POC glucose tests annually by approximately 2,400 operators throughout the system. Glucose POCT utilizes portable glucose meters (previous glucose meters: Precision PCx® Point-of-Care System; new glucose meters: Abbott Diagnostics) with data management features. Patient barcode scanning with the Precision PCx® Point-of-Care System involves entering a five-digit operator identification and a nine-digit patient account number for each patient test. After performing the test, the result is electronically uploaded when the glucose meters are placed into a docking station (i.e., access point, download site, or transmitting station) located on the patient care unit. Automated lock-out features help enforce POC quality by preventing untrained operators from using the meters and forcing analysis of two levels of control solutions on each day of testing. The Precision PCx meter further allows operators to be locked out when they repeatedly make identification errors (“three-strike rule”) by hospital policy, requiring operators to be counseled and retrained after their third error before allowing further testing.[3] Once uploaded, results are transferred to a database server (QCM3, Abbott Diagnostics), an interface manager (Telcor PC), and on to the laboratory information system or LIS (Sunquest v6.2, Sunquest Information Systems) via an HL7 message. POCT data in the LIS then gets sent to the electronic medical record. The interface manager also connects with the admission, discharge, and transfer (ADT) data from the HIS and checks patient ID (a nine-digit patient account number) against patient registration data [Figure 1]. Daily review of the Telcor PC identifies patient ID errors, which are tracked and if appropriate, reconciled. Unmatched results are stopped by the interface manager and not transferred to the patient's medical record.
Figure 1.
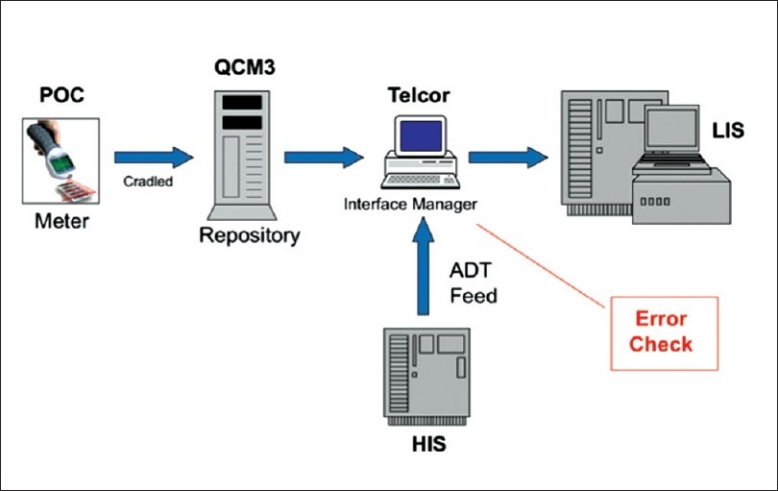
Point-of-care (POC) data transmission scheme. Data acquired and scanned in from the portable glucose meter gets uploaded to the QCM3 database server once the device is cradled. The Telcor interface manager checks the patient ID in the repository against patient registration data transmitted from the ADT feed coming from the hospital information system (HIS). Matched data then gets transmitted to the laboratory information system (LIS)
The clinical laboratory subsequently switched to a new glucose meter (Abbott Xceed Pro) which directly interfaces with the HIS ADT feed [Figure 2]. The barcoding system used by the new glucose meters employs a True ID feature. When the operator scans the patient's wristband, the meter searches the ADT database in its memory, finds a match, and displays the patient's name instead of a nine-digit patient account number. The operator is then required to confirm the ID by entering the year of the patient's birth date before the meter unlocks and allows patient testing to proceed. This is in contrast to the PCx meter that allows testing when a minimum number of any digits is scanned or manually entered for the patient ID. The PCx confirmation of the patient ID occurs when the interface manager attempts to transfer the result to a patient medical record. So, the new Xceed Pro meter checks patient identification before testing occurs and prevents testing if an identification does not match an active patient account number, while the Precision X checked identification after testing was completed.
Figure 2.
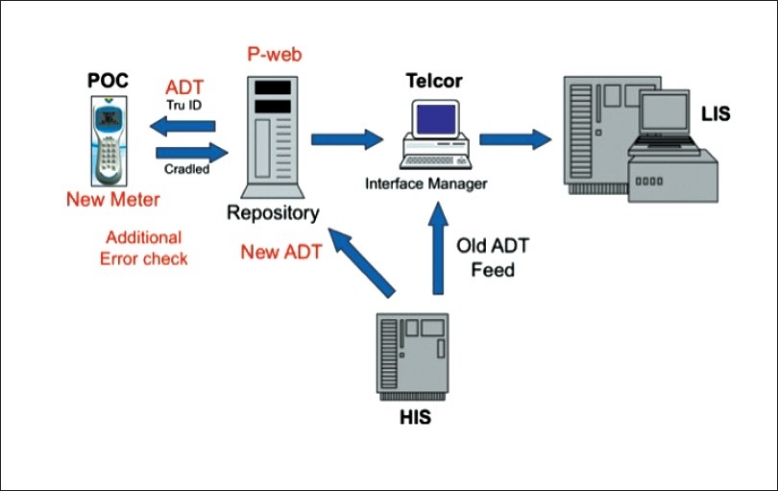
Point-of-care (POC) data transmission scheme with new glucose meters. There was a bidirectional flow of data with portable glucose meters. Glucose measurements and accompanying data are uploaded to the interface manager when devices are docked, and ADT data from the hospital information system (HIS) is directly transmitted via the P-web manager to the POC devices. This permits mismatches to be performed and corrected in real time at the point-of-care or patient bedside. Matched or corrected data then gets transmitted via the interface manager to the laboratory information system (LIS)
A “patient ID error” is defined as a POCT glucose meter result that does not match an active account in the ADT system, preventing the result from being transferred to a medical record, or a result that matches a different patient's account and is transferred to the wrong medical record. The reasons for these errors included incorrect manual entry, barcode scanning failures (illegible barcodes), improper barcode scanning (multiple wrist bands/incorrect/inactive account numbers), and use of transient/arbitrary codes in the emergency settings (e.g., 999-999-999) for unregistered patients. All glucose POCT tests using both PCx meters and Abbott Xceed Pro devices were monitored for a 2-month period. A comparison of the number of errors/month was performed using an unpaired t-test. The error results were separated into patient ID errors occurring in the Emergency Department (ED) setting (where there were more unregistered patients and a higher frequency for using arbitrary emergency identification, e.g., 999-999-999) and all other non-ED settings.
RESULTS
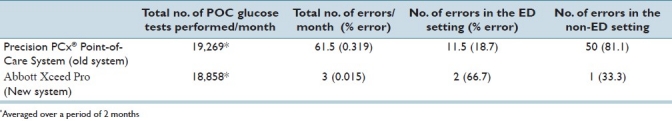
When averaged, 19,269 POCT glucose tests using old (PCx) meters were performed per month. During this period, an average of 61.5 patient ID errors/month were detected, giving an error rate of 0.319%. Most of these errors were noted to occur in the Non-ED setting (81.13%).
In a 2-month period, an average of 18,858 tests/month were performed with the new meters (Abbott Xceed Pro). A statistically significant decline in errors to 3 errors/month (0.015%, P=0.0024) was noticed after the implementation of the Xceed Pro meters [Table 1]. Most of the errors after the implementation of Xceed Pro were due to the transient use of ID numbers/emergency codes (66.7%) for unregistered patients in ED patients. The other error that was noted in this duration was due to the manual entry of patient information for tests performed in the out-patient clinic where patients do not wear barcode wristbands.
Table 1.
Incidence of average error rate/month before and after the implementation of new system (Abbott Xceed Pro)
DISCUSSION
Over the past 6 years, the POCT staff has targeted zero tolerance with regard to errors when utilizing POCT glucose meters. Most of these errors arose from the preanalytic (e.g., patient identification problems) phase of the testing process. Others have also recommended targeting quality initiatives to prevent medical errors in POCT.[6] These include (1) the adoption of operator training and skill validation in POCT programs, (2) implementation of security and validation of performance on existing and new devices, (3) having flexible, user-defined error-prevention system options on instruments, (4) integration of connectivity standards for bidirectional information exchange, (5) ensuring fast turnaround time of POCT test results, and (6) monitoring programs for invalid use, operator competence, quality compliance, and other performance improvement indices to reduce errors.
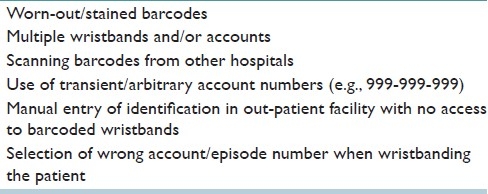
The automation of data entry through the use of barcode scanners on POCT glucose meters was very effective at reducing entry errors over our previous manual process. However, barcoding still failed to reach our goal of zero entry errors for a number of reasons [Table 2]. Most of these errors were detected at the interface manager, after the test was completed when the interface manager noted a result not matching with an active account. By directly interfacing POCT devices with an ADT feed from the HIS, error checks for patient misidentification could be performed and corrected by the clinical operator before the testing occured.
Table 2.
Common causes of data entry errors
The use of two patient identifiers for any patient procedure (including phlebotomy or laboratory tests) is now a patient safety goal of the Joint Commission. The Xceed Pro meters require the operator to verify two patient identifiers, the patient's name and birth date, before the meter unlocks and allows patient testing. The process of stopping the testing process makes the operator pause and check if the ID is correct and is similar to "time-out" required by Joint Commission before any invasive surgical procedure. The change of display from a nine-digit account number in Precision PCx to patient's name in Xceed Pro facilitated the verification.
LIMITATIONS OF THE STUDY
Nursing is responsible for addressing ID errors through follow-up with the operators and corrective action. The POC team in the Pathology department coordinates with the nursing by monitoring and sending reports back to the nursing units. The reduction in the error rates after the implementation of new meters may be attributed to increased awareness and the recent education conducted by the POC staff. This education focused not only on the operation of new meters but also reinforced ongoing docking issues, legibility of the barcode, verifying that the scanned information is correct, and increased operator accountability. The Emergency Department is also working on the rapid registration of new patients with barcoded wristbands as soon as possible after admission to reduce the use of arbitrary emergency identification with POCT.
Potential of errors with new meters
We have not been able to completely eliminate the patient identification errors on the new meters for several reasons. Errors still result from the use of arbitrary identification numbers for unregistered patients in the emergency department (ED). These patients need to be tested by the POC meters for an immediate triage, sometimes resulting in tests being conducted even before the patients have been issued wristbands and hence the use of arbitrary account numbers (e.g., 999-999-999). Also, the POC meters are docked intermittently and the ADT feed only updates when meters are docked, so recently admitted patients may not appear in the meter ADT database until the meter is docked resulting in the use of arbitrary identification numbers for POCT. In most cases, the POC staff are notified of the updated patient information (within 24 h), so that the instance is not counted as a patient identification error.
A small percentage of errors still result from other reasons such as (1) manual entry of the patient information for tests performed in out-patient clinics where patients do not wear barcoded wristbands, (2) scanning barcodes issued to the patients from other hospitals, and (3) the use of an incorrect account/episode number, selecting an out-patient recurring episode for an in-patient admission.
Experience with the new identification system
The Implementation of new glucose meters with an ADT interface and enhanced patient ID has helped to decrease ID errors dramatically. Entering patient's birth date is akin to Joint Commission's mandated “time-out” before any invasive procedure and forces the operator to stop and check the entered patient ID in the meter prior to conducting testing. Direct interfacing of the ADT feed with the POC devices enables the meters to store patient identifiers and display alphanumeric names, and provides the opportunity to catch patient ID errors at the bedside.
The ID errors that continue to occur with this new process are primarily seen in emergency room settings where unregistered patients without a hospital account number may need to be tested or where frequent docking of meters may not be practical to update the meter's ADT database. Wireless meters that can continuously update may help reduce the delays in database updates from intermittent POCT device docking, but most models of current glucose meters do not yet offer continuous wireless connectivity.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2011/2/1/22/80718
REFERENCES
- 1.Plebani M, Carraro P. Mistakes in a stat laboratory: Types and frequency. Clin Chem. 1997;43:1348–51. [PubMed] [Google Scholar]
- 2.Plebani M. Does POCT reduce the risk of error in laboratory testing? Clin Chim Acta. 2009;404:59–64. doi: 10.1016/j.cca.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 3.Nichols JH. Quality in point-of-care testing. Expert Rev Mol Diagn. 2003;3:563–72. doi: 10.1586/14737159.3.5.563. [DOI] [PubMed] [Google Scholar]
- 4.Nichols JH, Bartholomew C, Brunton M, Cintron C, Elliott S, McGirr J, et al. Reducing medical errors through barcoding at the point of care. Clin Leadersh Manag Rev. 2004;18:328–34. [PubMed] [Google Scholar]
- 5.Snyder ML, Carter A, Jenkins K, Fantz CR. Patient misidentifications caused by errors in standard bar code technology. Clin Chem. 2010;56:1554–60. doi: 10.1373/clinchem.2010.150094. [DOI] [PubMed] [Google Scholar]
- 6.Kost GJ. Preventing medical errors in point-of-care testing: Security, validation, safeguards, and connectivity. Arch Pathol Lab Med. 2001;125:1307–15. doi: 10.5858/2001-125-1307-PMEIPO. [DOI] [PubMed] [Google Scholar]


