Abstract
Objectives
To produce nationally representative population estimates of rates of service use among young adults with autism spectrum disorder (ASD) during their first few years after leaving high school and to examine correlates of use.
Design
Nationally representative telephone survey from 2007-2008.
Setting
United States.
Participants
Parents and guardians of young adults with ASD ages 19-23.
Outcome measures
Use of services in the prior two years or since leaving high school: mental health services, medical evaluation and assessment, speech therapy, and case management.
Results
Rates of service use ranged from a low of 9.1% for speech therapy to a high of 41.9% for case management; 39.1% received no services. The adjusted odds of no services were higher among African Americans and those with low incomes. The adjusted odds of case management were lower among youth with high functional skills and those with low incomes.
Conclusions
Rates of service disengagement are high after exiting high school. Disparities by race and socioeconomic status indicate a need for targeted outreach and services.
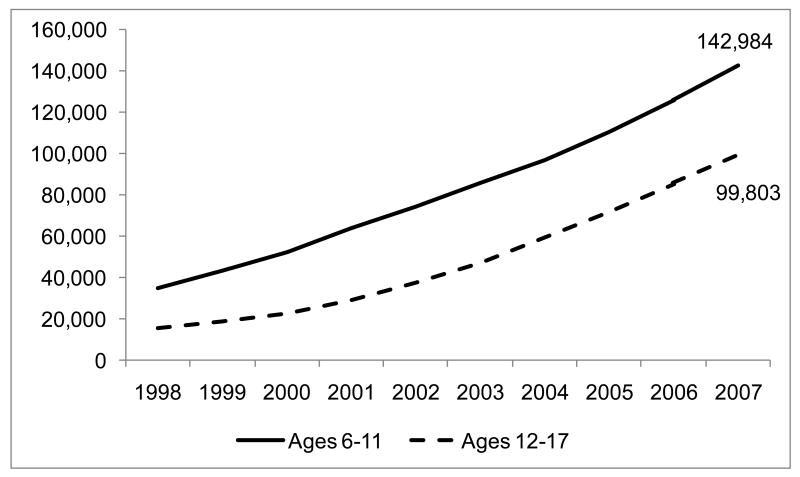
What happens to adolescents with autism spectrum disorder (ASD) once they reach adulthood? The number of young adults labeled with an ASD is increasing rapidly as ever-larger cohorts of children identified as having an ASD age through adolescence. This trend is especially visible in special education enrollment where the number of students ages 12-17 classified in the autism eligibility category increased from 15,480 in 1998 to 99,803 in 2007 (Figure 1).1 It is unclear whether growing enrollment reflects changing identification practices or a true increase in population prevalence.2-4 Regardless of the root cause, the fact remains that treated prevalence is increasing and the implications of this trend for service systems are poorly understood.5
Figure 1.
Number of students enrolled in the special education autism category by age group, 1998 to 2007.1
National, state, and local policy makers have been working hard to meet the needs of the growing numbers of young children identified as having an ASD. Signs of policy activity and resource allocation to improve services for children with ASD include national campaigns to educate clinicians about early warning signs, state efforts to cover the costs of early intervention, and the efforts of state commissions and legislative bodies.5-8 However, there has been no effort of a corresponding magnitude to plan for ensuring continuity of supports and services as these children age into adulthood. Likewise, research on services for adults with ASD is scant relative to the burgeoning literature on children with ASD.9, 10
The majority of an average life span unfolds in adulthood. Life course theory posits the few years immediately following the age that students typically exit from high school is a pivotal time for all youth. A positive transition creates a solid foundation for an adaptive adult life course pathway. A negative transition can set the stage for a pathway fraught with developmental, health, and social difficulties.11-13
Youth with ASD are especially vulnerable during this period because of their challenges with communication and social interaction, greater reliance on others for aid, and high rates of comorbid health and mental health problems. 14-16 Adolescents who receive special education services face an end of this entitlement as they exit high school. According to the National Institute of Mental Health, “The termination of eligibility and availability of school-based services is particularly problematic for those with disorders that require intensive services that are principally delivered through educational settings, such as youth with autism spectrum disorders.”17 Thus, service use in the years immediately following high school occurs at a critical developmental period in the context of a shift in the mechanisms through which care is accessed and delivered.
There is a dearth of nationally representative data on the prevalence and correlates of service use among young adults with ASD. Basic descriptive data on the prevalence and patterns of service use is necessary for planning by policymakers and administrators. Knowledge of the correlates of service use can help identify underserved populations and plan targeted services. If there are significant disparities in rates of service use, despite similar levels of need, then new strategies are needed for improving access. Understanding which factors are most strongly related to service use can suggest policy targets that may have the greatest potential leverage for improving access. Lastly, estimates of service use and correlates will help clinicians, service providers, and family members be more informed and better prepared as they try to help teens with ASD navigate the transition from adolescence to young adulthood.
The aims of this study were to produce nationally representative estimates of rates of service use among young adults with ASD during their first few years after leaving high school and to examine correlates of use. We focused on four services especially salient for youth with ASD: mental health services, medical evaluation and assessment, speech therapy, and case management. Mental and physical health comorbidities are common in ASD, with evidence that the risk for some conditions (e.g. epilepsy) may actually increase during adolescence and young adulthood.18 Thus, the need for mental health and medical services tends to be high and ongoing. Language impairment is a core characteristic of ASD, with many individuals having no ability to speak, and there is a need for continuing support related to communication.14 Speech therapy is the most commonly received form of service among students with ASD in high school.19 By definition, ASD is pervasive in impact and affected individuals typically need help from multiple health and service providers to address various needs. Thus, the need for case management and care coordination is also high in this population. To our knowledge, this will be the first paper to report such national estimates for the United States.
Methods
Study Sample
Data for this report came from the National Longitudinal Transition Study 2 (NLTS2), a 10-year prospective study being conducted by SRI International for the U.S. Department of Education that is following more than 11,000 youth enrolled in special education as they age into young adulthood. The study included 920 youth enrolled in the special education autism category at the start of data collection in 2001. Unweighted sample size numbers were rounded to the nearest ten as required by the data use agreement with the U.S. Department of Education. Analyses for this paper are based on data from wave 4, collected in 2007 and 2008, which included 680 youth with an ASD. The subset of 410 youth who had exited high school by wave 4 was used as the basis for this paper. Use of these data is governed by a data use agreement with the U.S. Department of Education and was approved by the Washington University Institutional Review Board.
The NLTS2 sampling plan was designed to produce a nationally representative sample that would generalize to all special education students who were in 7th through 12th grade or in ungraded programs and who were ages 13 through 16 on December 1, 2000. A two-stage process first sampled school districts and then students within districts.20 Determination of a student's eligibility for special education services in the autism category was made by the school district from whose roster the student was sampled and, thus, the sample is subject to some unknown amount of district-to-district variation in eligibility criteria. Of the 1,100 sample-eligible students with ASD, 920 participated in wave 1 for an initial response rate of 84%. The 680 participating at wave 4 represented a 74% retention rate from wave 1.
Unique weights are included in the data file for each wave of data collection so that estimates generalize to the national population of youth who had been receiving special education services for a given age range and disability type. Weights include adjustment for nonresponse at each wave. Detailed information on the weighting strategy for NLTS2 has been previously published.21
Special education enrollment is tracked categorically by type of disability. For the sake of official enrollment reports, each student is counted only once in a primary classification category. Autism is now one of thirteen primary disability classification categories mandated by the Individuals with Disabilities Education Act (I.D.E.A.) after being added in 1990 as part of Public Law 101-476.
Schools do not necessarily use standardized DSM-IV diagnostic criteria for assigning a label of autism to children in special education. The U.S. Department of Education's definition of autism is consistent with DSM-IV criteria but not as specifically detailed. States and districts are left to operationalize the details of diagnostic criteria. Epidemiological research in the U.S. has found that 99% of children reported in the special education autism category also meet DSM-IV-based criteria for ASD.22, 23 Relative to population-based epidemiological ascertainment, the special education autism designation is very specific and moderately sensitive. It is very unlikely that youth in this enrollment category do not have ASD, but not all youth with ASD will be captured by this administrative classification. An unknown proportion of youth with ASD are enrolled in special education under different primary disability categories such as mental retardation or speech-language impairment. Such youth are not included in the present analyses.
Data collection procedures
The present analyses are based on responses to the wave 4 parent/guardian surveys, collected by computer assisted telephone interviewing. The surveys began with screening to identify the adult most knowledgeable about the youth. Families unavailable by telephone were sent a simplified mail questionnaire and an offer to participate in a drawing for cash and gift incentives. Thirty-five families out of 410 (8.5%) received the simplified mail questionnaire.
Measures and variables
Three dependent variables came from a sequence of questions on service use that began one of two ways “Any time since high school…” (for youth who had been in high school during the prior wave of interviews), or “Any time in the past two years…” (for youth who had already exited high school at the prior wave), “…has [YOUTH] received any of the following services?” A list of services was then read to respondents that included: “Psychological or mental health services or counseling,” “Medical services for diagnosis or evaluation related to [his/her] disability,” and “Speech or language therapy, or communication services”. A separate question asked whether the youth had a case manager to coordinate services. We also created an indicator variable if none of the 4 services were received.
Covariates included measures of demographic factors, need and severity indicators, and measures of socioeconomic resources. Age and residential status were included as demographic controls. We included ethnicity and race in order to be able to identify disparities in service receipt. An indicator for severe language impairment was coded 1 if respondents indicated a youth “has a lot of trouble speaking clearly” or “doesn't speak at all.” We included an indicator for parent-reported diagnosis of attention deficit hyperactivity disorder (ADHD) because it is a common comorbidity among those with ASD.8 Unfortunately, the survey did not directly ask parents about other common comorbidities such as intellectual disability. A functional mental skills scale was constructed by summing 4 questions about how well the youth can do the following tasks without help: tell time, read and understand common signs, count change, look up telephone numbers and use a telephone (each item had 4 response categories: not at all well, not very well, pretty well, very well). We collapsed the scale into quartiles with higher values corresponding to greater skills. Youth in the highest quartile had values of “very well” on all 4 constituent indicators. The respondent's household income was used as a measure of family financial resources even though 22% of youth were not living with respondents at the time of the interviews. Health insurance status was another measure of resources.
Data Analysis
Rates of missing data per variable ranged from 0% to 21%, with 3 variables missing more than 10% (income 21%, functional mental skills 14%, and insurance 14%) and the remaining variables missing less than 5%. Missing data were imputed using sequential regression to create 20 sets of data with no missing values.24, 25 Standard methods for analysis of multiply imputed data were used for combining estimates.26
Univariate proportions with 95% confidence intervals were computed for describing the sample. Multivariate logistic regression models estimated the correlates of outcomes. The speech therapy model would not converge because the prevalence was so low. All reported estimates were weighted and variances adjusted to account for the complex sampling.
Results
Consistent with the higher prevalence of ASD among males, the ratio of males to females was 6:1. The mean age was 21.5 years old. Measures of impairment and co-morbid conditions suggest a range of need for services: 21.2% were nonverbal and 34.5% had ADHD. Most youth lived with their parents (79.0%) and had health insurance (91.5%).
Overall rates of service use were 23.5% for medical services, 35.0% for mental health services, 41.9% for case management, and 9.1% for speech therapy. About two-fifths (39.1%) had not received any of these services.
The adjusted odds of not receiving any services were 3.31 times higher for African American compared to white youth, and 5.96 times higher for those with incomes ≤ $25,000 compared to those with incomes over $75,000. The adjusted odds of no case management were 5.88 times higher among those with incomes ≤ $25,000 compared to those with incomes over $75,000.
Across models, the need indicators of verbal status and attention deficit were unrelated to outcomes. Higher functional mental skills were associated with increased odds of no services and reduced odds of case management or medical services.
Comment
We reported on the prevalence and correlates of service use among a nationally representative sample of post-high school youth with ASD. Rates of service use ranged from a low of 9.1% for speech therapy to a high of 41.9% for case management. These rates are lower when compared to estimates for high school students with ASD from the first wave of the same study, six years earlier, when all youth were still in high school: 46.2% received mental health services, 46.9% had medical services, 74.6% were getting speech therapy, and 63.6% had a case manager.19 The estimates are not perfectly comparable because the post-high school sample does not include all the youth from the first wave, as some had not yet exited school and some were lost to follow up. Nonetheless, the differences clearly support the general conclusion that exiting high school is associated with a steep drop in service receipt.
Notably, 39.1% of all youth received none of these services. Compared to white youth, the odds of no service use was 3.3 times higher among African-American youth despite there being no corresponding disparity when services were examined individually. This heightened risk for total service disengagement among African-American youth suggests a need for targeted prevention and outreach. This finding also highlights the importance of examining broad patterns of service disengagement, in addition to the use of individual services, when devising systems for monitoring service equity, as the latter strategy may miss important disparities.
There was no association between need and service use when we examined verbal ability and attention deficit disorder. Functional mental skill was the only need factor consistently related with outcomes, with more able youth being less likely to receive case management or medical services and more likely to be receiving no services. The particularly strong link between functional mental skills and case management may be due to the fact these services are often provided for adults via state mental retardation and developmental disabilities (MRDD) departments. Qualifying for adult MRDD services in many states requires demonstrable functional impairment in addition to a diagnostic label. In particular, many Medicaid home and community based services waiver programs require a level of care determination that emphasizes functional impairments and self care skills.
Youth from lower income households had higher odds of receiving no services at all and of receiving no case management. Multiple factors beyond merely a reduced ability to privately purchase services may be underlying this association. Services may not be located in neighborhoods where poorer families live and transportation to reach distant services may be expensive or prohibitively time-consuming. Poorer families may also have reduced access to information resources, such as Internet access, where they can learn about available services.
The socioeconomic and racial disparities in service engagement documented in our study clearly indicate a need for further research into access barriers, the development and evaluation of equitable service delivery models, and targeted policies to promote access among underserved populations. The Federal Interagency Autism Coordinating Committee (IACC) is responsible for establishing autism research priorities and updating them annually. The 2010 report had two sections of recommendations for research related to services and adults, however no explicit mention was made of addressing racial or socioeconomic disparities in service use among adults.27 We recommend that future revisions of IACC research priorities include explicit calls for investigating racial and socioeconomic disparities in service access and individual outcomes among adults with ASD.
This study has some limitations. First, the sample is representative of youth who had been enrolled in the special education autism category at baseline and may not be fully representative of all youth with ASD in the general population in so far as some may be served in other special education categories. Second, respondents' knowledge and recollection of service use and related factors may not be perfect. The use of self-report to measure health care utilization may lead to underreporting, the most common problem with this form of data collection.28 If it were feasible, direct examination of health and services records might yield different prevalence estimates. Unfortunately, there was no way of verifying the reports of respondents by checking medical records. Third, the study does not include an indicator for state location precluding the potential analysis of important state-to-state differences in policies that can influence service use and related outcomes.5, 29-31 Finally, these are cross-sectional associations and therefore causal attributions are not possible. Once all the NLTS2 youth have exited high school and the data become available, future research should examine longitudinal trajectories of service use in order to discover risk factors for service discontinuity.
Several strengths of the study counterbalance its limitations. First, the national representativeness of the sampling design makes findings highly generalizable and relevant for policy and practice. Second, in contrast to most prior research in the U.S., the size and diversity of the sample allowed us to examine disparities in service use by demographic factors including ethnicity, race, and socioeconomic status. Third, the data is very recent and presents an up-to-date picture as compared to the handful of extant studies of young adults with ASD, many of which are over a decade old.
The number of youth labeled with ASD and entering young adulthood will continue to rise in the foreseeable future. The National Institutes of Health Strategic Plan for Autism Research has flagged research on services and adulthood as deserving increased attention. This study represents an important step in the process of building a foundation of evidence that can help improve services and foster independence and health among youth with ASD.
Table 1.
Characteristics of youth with ASD no longer in high school from wave 4 (2007-2008) of the National Longitudinal Transition Study – 2.
| Variable | Values | Weighted % | 95% Confidence interval |
|---|---|---|---|
| Demographic Factors | |||
| Male | 85.8 | [79.1, 90.6] | |
| Age | |||
| 19 | 6.8 | [3.5, 12.7] | |
| 20 | 17.3 | [12.9, 22.9] | |
| 21 | 17.9 | [13.4, 23.6] | |
| 22 | 33.8 | [26.0, 42.7] | |
| 23 | 24.2 | [17.2, 32.9] | |
| Ethnicity, Hispanic | 8.5 | [4.9, 14.4] | |
| Race | |||
| White | 74.8 | [66.3, 81.8] | |
| African-American | 16.4 | [10.6, 24.6] | |
| Other, mixed | 8.7 | [5.1, 14.4] | |
| Residential status | |||
| With parent, guardian, relative | 79.0 | [69.8, 85.9] | |
| Independent | 13.1 | [7.2, 22.7] | |
| Group home, supervised setting | 7.9 | [4.7, 13.1] | |
| Need Factors | |||
| Nonverbal | 21.2 | [14.3, 30.3] | |
| Attention deficit hyperactivity disorder | 34.5 | [26.8, 43.2] | |
| Functional mental skills quartiles | |||
| 1 | 22.7 | [15.4, 31.9] | |
| 2 | 21.3 | [14.0, 30.8] | |
| 3 | 33.1 | [24.4, 43.1] | |
| 4 | 22.9 | [16.2, 31.4] | |
| Resource Factors | |||
| Income | |||
| $25,000 or less | 16.7 | [10.5, 25.0] | |
| $25,001- $50,000 | 30.2 | [21.0, 41.2] | |
| $50,001-$75,000 | 35.3 | [27.0, 44.6] | |
| Over $75,000 | 17.8 | [12.1, 25.5] | |
| Insurance status | |||
| Private | 58.6 | [48.5, 68.1] | |
| Public | 30.2 | [21.1, 41.1] | |
| Uninsured | 8.5 | [4.7, 14.5] | |
| Other, multi | 2.7 | [0.8, 7.8] | |
| Dependent Variables | |||
| No services | 39.1 | [30.5, 48.5] | |
| Mental health services | 35.0 | [27.4, 43.4] | |
| Medical services | 23.5 | [16.5, 32.3] | |
| Speech therapy | 9.1 | [5.8, 14.1] | |
| Has a case manager | 41.9 | [34.0, 50.2] |
Table 2.
Logistic regression models predicting post-high school use of services among young adults with ASD, from wave 4 (2007-2008) of the National Longitudinal Transition Study - 2.
| Odds ratios [95% confidence interval] |
|||||
|---|---|---|---|---|---|
| Variable | Values | No services | Case management | Mental health | Medical |
| Demographic Factors | |||||
| Female | 0.47 [0.11, 1.94] |
2.02 [0.65, 6.30] |
1.81 [0.54, 6.03] |
0.95 [0.28, 3.25] |
|
| Age | |||||
| 19 | 1 | 1 | 1 | 1 | |
| 20 | 0.50 [0.13, 1.88] |
1.63 [0.38, 6.96] |
1.22 [0.35, 4.29] |
1.89 [0.37, 9.68] |
|
| 21 | 0.37 [0.09, 1.47] |
1.87 [0.45, 7.78] |
0.78 [0.23, 2.70] |
1.96 [0.35, 10.83] |
|
| 22 | 0.37 [0.09, 1.54] |
2.27 [0.50, 10.31] |
1.12 [0.32, 3.91] |
1.28 [0.26, 6.42] |
|
| 23 | 0.89 [0.19, 4.08] |
1.23 [0.23, 6.55] |
0.60 [0.13, 2.71] |
3.39 [0.58, 19.71] |
|
| Ethnicity, Hispanic | 1.33 [0.41, 4.31] |
0.75 [0.24, 2.29] |
2.39 [0.67, 8.56] |
0.41 [0.10, 1.68] |
|
| Race | |||||
| White | 1 | 1 | 1 | 1 | |
| African American | 3.31 [1.29, 8.48] |
0.73 [0.26, 2.02] |
0.53 [0.23, 1.23] |
0.58 [0.19, 1.79] |
|
| Other, mixed | 1.30 [0.29, 5.81] |
1.01 [0.28, 3.66] |
0.30 [0.06, 1.40] |
0.34 [0.09, 1.24] |
|
| Residential status | |||||
| With parent, guardian, relative | 1 | 1 | 1 | 1 | |
| Independent, roommate, dorm, barracks | 2.85 [0.66, 12.35] |
0.14 [0.03, 0.61] |
0.83 [0.22, 3.11] |
0.22 [0.04, 1.23] |
|
| Group home, supervised setting | 2.76 [0.59, 12.98] |
0.80 [0.20, 3.20] |
1.37 [0.35, 5.39] |
0.44 [0.14, 1.41] |
|
| Need Factors | |||||
| Nonverbal | 1.30 [0.44, 3.88] |
0.86 [0.33, 2.27] |
0.56 [0.20, 1.55] |
1.42 [0.50, 4.09] |
|
| Attention deficit hyperactivity disorder | 1.01 [0.46, 2.24] |
0.99 [0.51, 1.95] |
1.27 [0.66, 2.44] |
1.04 [0.51, 2.12] |
|
| Functional mental skills quartiles | |||||
| 1 (Very low skills) | 1 | 1 | 1 | 1 | |
| 2 | 3.79 [0.77, 18.62] |
0.22 [0.06, 0.77] |
0.43 [0.13, 1.40] |
0.26 [0.08, 0.85] |
|
| 3 | 4.70 [1.00, 22.19] |
0.25 [0.07, 0.83] |
0.66 [0.21, 2.13] |
0.29 [0.09, 0.92] |
|
| 4 (High skills) | 1.86 [0.38, 8.95] |
0.22 [0.07, 0.76] |
1.21 [0.40, 3.68] |
0.41 [0.11, 1.48] |
|
| Resource Factors | |||||
| Respondent income | |||||
| $25,000 or less | 5.96 [1.20, 29.66] |
0.17 [0.04, 0.67] |
0.71 [0.21, 2.40] |
0.75 [0.18, 3.15] |
|
| $25,001 - $50,000 | 2.92 [0.91, 9.39] |
0.42 [0.14, 1.28] |
0.74 [0.26, 2.13] |
0.92 [0.32, 2.68] |
|
| $50,001-$75,000 | 1.86 [0.66, 5.27] |
0.47 [0.18, 1.21] |
1.45 [0.58, 3.65] |
1.13 [0.42, 3.06] |
|
| Over $75,000 | 1 | 1 | 1 | 1 | |
| Insurance | |||||
| Private insurance | 1 | 1 | 1 | 1 | |
| Public insurance | 0.45 [0.11, 1.88] |
1.19 [0.41, 3.47] |
1.81 [0.68, 4.82] |
2.38 [0.79, 7.15] |
|
| Uninsured | 2.49 [0.54, 11.36] |
0.34 [0.06, 2.12] |
0.50 [0.10, 2.47] |
1.01 [0.22, 4.56] |
|
| Multiple coverage | 0.79 [0.03, 19.82] |
3.89 [0.18, 84.13] |
1.80 [0.15, 21.53] |
5.53 [0.34, 90.04] |
|
Acknowledgments
This research was supported with funding from the National Institute of Mental Health (R01 MH086489-01) and the Organization for Autism Research. The first author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Publisher's Disclaimer: This document is the submitted version of the manuscript. Interested readers should visit the journal website in order to obtain the finalized version that appeared in print with further modifications and revisions. There may be discrepancies between this posted version and the final version that appeared in print. http://archpedi.ama-assn.org/
References
- 1.U.S. Department of Education Office of Special Education Programs DAS. Table 1-11. Children and students served under IDEA, Part B, in the U.S. and outlying areas by age group, year, and disability category: Fall 1998 through fall 2007. [Accessed August 17, 2009]; https://www.ideadata.org/TABLES31ST/AR_1-11.htm.
- 2.Shattuck P. The contribution of diagnostic substitution to the growing administrative prevalence of autism in U.S. special education. Pediatrics. 2006;117(4):1028–1037. doi: 10.1542/peds.2005-1516. [DOI] [PubMed] [Google Scholar]
- 3.Rutter M. Incidence of autism spectrum disorders: Changes over time and their meaning. Acta Pediatrica. 2005;94:2–15. doi: 10.1111/j.1651-2227.2005.tb01779.x. [DOI] [PubMed] [Google Scholar]
- 4.Fombonne E. The changing epidemiology of autism. Journal of Applied Research in Intellectual Disabilities. 2005;18:281–294. [Google Scholar]
- 5.Shattuck PT, Grosse SD. Issues related to the diagnosis and treatment of autism spectrum disorders. Mental Retardation and Developmental Disabilities Research Reviews. 2007;13:129–135. doi: 10.1002/mrdd.20143. [DOI] [PubMed] [Google Scholar]
- 6.National Conference of State Legislatures. Autism policy issues overview. [Accessed December 21, 2009]; http://www.ncsl.org/IssuesResearch/Health/AutismPolicyIssuesOverview/tabid/14390/Default.aspx.
- 7.Centers for Disease Control and Prevention. Learn the Signs. Act Early. Early Identification of Children with Autism or other Developmental Disorders Awareness Campaign. [Accessed May 16, 2006]; http://www.cdc.gov/ncbddd/autism/actearly/
- 8.Johnson CP, Myers SM Council on Children with Disabilities. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120(5):1183–1215. doi: 10.1542/peds.2007-2361. [DOI] [PubMed] [Google Scholar]
- 9.Howlin P. Redressing the balance in autism research. Nature Clinical Practice Neurology. 2008;4:407. doi: 10.1038/ncpneuro0860. [DOI] [PubMed] [Google Scholar]
- 10.Interagency Autism Coordinating Committee. The Interagency Autism Coordinating Committee strategic plan for autism spectrum disorder research - January 26, 2009. [Accessed May 1, 2009]; http://iacc.hhs.gov/reports/2009/iacc-strategic-plan-for-autism-spectrum-disorder-research-jan26.shtml.
- 11.Hogan DP, Astone NM. The transition to adulthood. Annual Review of Sociology. 1986;12:109–130. [Google Scholar]
- 12.Gore S, Aseltine RH, Schilling EA. Transition to adulthood, mental health, and inequality. In: Avison WR, McLeod JD, Pescosolido BA, editors. Mental Health, Social Mirror. New York: Springer; 2007. pp. 219–237. [Google Scholar]
- 13.Rutter M. Pathways from childhood to adult life. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1989;30:23–51. doi: 10.1111/j.1469-7610.1989.tb00768.x. [DOI] [PubMed] [Google Scholar]
- 14.Seltzer MM, Shattuck P, Abbeduto L, Greenberg JS. Trajectory of development in adolescents and adults with autism. Mental Retardation and Developmental Disabilities Research Reviews. 2004;10:234–247. doi: 10.1002/mrdd.20038. [DOI] [PubMed] [Google Scholar]
- 15.Schall C, Cortijo-Doval E, Targett PS, Wehman P. Applications for youth with autism spectrum disorders. In: Wehman P, editor. Life beyond the classroom: Transition strategies for young people with disabilities. 4th. Baltimore: Paul H. Brookes; 2006. [Google Scholar]
- 16.Gerhardt PE. Effective transition planning for learners with ASD approaching adulthood. Impact. 2006;19:18–19. [Google Scholar]
- 17.National Institute of Mental Health. Refining and Testing Mental Health Interventions and Services for Youth with Mental Illness who are Transitioning to Adulthood (R34, RFA-MH-07-051) [Accessed August 20, 2008]; http://grants.nih.gov/grants/guide/rfa-files/RFA-MH-07-051.html.
- 18.Myers SM, Johnson CP Disabilities CoCw. Management of children with Autism Spectrum Disorders. Pediatrics. 2007;120(5):1162–1182. doi: 10.1542/peds.2007-2362. [DOI] [PubMed] [Google Scholar]
- 19.Levine P, Marder C, Wagner M. Services and supports for secondary school students with disabilities. Menlo Park, CA: SRI International; 2004. [Google Scholar]
- 20.SRI International. National Longitudinal Transition Study II (NLTS2) Sampling Plan. Menlo Park, CA: Author; Februrary 25, 2000. [Google Scholar]
- 21.Wagner M, Kutash K, Duchnowski AJ, Epstein MH. The Special Education Elementary Longitudinal Study and the National Longitudinal Transition Study: Study designs and implications for children and youth with emotional disturbance. Journal of Emotional & Behavioral Disorders. 2005;13:25–41. [Google Scholar]
- 22.Bertrand J, Boyle C, Yeargin-Allsopp M, Decoufle P, Mars A, Bove F. Prevalence of Autism in a United States Population: The Brick Township, New Jersey, Investigation. Pediatrics. 2001;108(5):1155–1162. doi: 10.1542/peds.108.5.1155. [DOI] [PubMed] [Google Scholar]
- 23.Yeargin-Allsopp M, Rice C, Karapurkar T, Doernberg N, Boyle C, Murphy C. Prevalence of autism in a US metropolitan area. JAMA: Journal of the American Medical Association. 2003;289(1):49–55. doi: 10.1001/jama.289.1.49. [DOI] [PubMed] [Google Scholar]
- 24.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger PW. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001;27(1):85–95. [Google Scholar]
- 25.IVEware: Imputation and variance estimation software [computer program]. Version 1.0. 2002. [Google Scholar]
- 26.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley & Sons; 1987. [Google Scholar]
- 27.Interagency Autism Coordinating Committee. The 2010 Interagency Autism Coordinating Committee Strategic Plan for Autism Spectrum Disorder Research. [Accessed April 21, 2010]; http://iacc.hhs.gov/strategic-plan/2010/index.shtml.
- 28.Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Medical Care Research and Review. 2006;63(2):217–235. doi: 10.1177/1077558705285298. [DOI] [PubMed] [Google Scholar]
- 29.Parish SL, Rose RA, Andrews ME, Shattuck PT. Receipt of professional care coordination among families raising children with special health care needs: A multilevel analysis of state policy needs. Children and Youth Services Review. 2009;31:63–70. [Google Scholar]
- 30.Shattuck PT, Parish SL. Financial burden in families of children with special health care needs: Variability among states. Pediatrics. 2008;122(1):13–18. doi: 10.1542/peds.2006-3308. [DOI] [PubMed] [Google Scholar]
- 31.Parish SL, Shattuck PT, Rose RA. Financial burden of raising CSHCN: Association with state policy choices. Pediatrics. 2009;124:S435–S442. doi: 10.1542/peds.2009-1255P. [DOI] [PubMed] [Google Scholar]