Abstract
Over the last years, cholangiocytes, the cells that line the biliary tree, have been considered an important object of study for their biological properties which involves bile formation, proliferation, injury repair, fibrosis and angiogenesis. Cholangiocyte proliferation occurs in all pathologic conditions of liver injury where it is associated with inflammation and regeneration. During these processes, biliary cells start to secrete different cytokines, growth factors, neuropeptides and hormones which represent potential mechanisms for cross talk with other liver cells. Several studies suggest that hormones, and in particular, sex hormones, play a fundamental role in the modulation of the growth of this compartment in the injured liver which functionally conditions the progression of liver disease. Understanding the mechanisms of action and the intracellular pathways of these compounds on cholangiocyte pathophysiology will provide new potential strategies for the management of chronic liver diseases. The purpose of this review is to summarize the recent findings on the role of sex hormones in cholangiocyte proliferation and biology.
Keywords: Biliary epithelium, Sex hormones, Cholestatic diseases
INTRODUCTION
The intrahepatic biliary tree is a complex three-dimensional network of interconnected ducts which starts at the level of canals of Hering, continues into intrahepatic ducts of increasing diameter and ends at the level of the extrahepatic bile ducts[1]. The intrahepatic biliary tree plays a critical role in many liver functions including bile formation, regeneration, injury repair, fibrosis, angiogenesis and regulation of blood flow. Most of these events are regulated by several neuropeptides, hormones, cytokines and growth factors which target cholangiocytes[2], the epithelial cells lining the biliary tree. Cholangiocytes are the preferential target of damage in a group of chronic cholestatic liver diseases called cholangiopathies, with a high social and economic impact due to their high prevalence and morbidity such as primary biliary cirrhosis (PBC), primary sclerosing cholangitis (PSC), polycystic liver disease (PCLD) and cholangiocarcinoma (CCA)[3-7]. In laboratory animals, ‘‘typical’’ cholangiocyte proliferation is achieved by a number of experimental models including bile duct ligation (BDL), partial hepatectomy, acute CCl4 feeding and chronic feeding of a-naphthylisothiocyanate (ANIT) or bile salts[8-11]. In these hyperplastic models, cholangiocyte proliferation is closely associated with increased secretin receptor gene expression and secretin-stimulated cAMP levels[12-18]. A variety of clinical and epidemiological observations have shown the involvement of sex hormones as inducers of growth and differentiation of target cells expressing their receptors[3]. The molecular mechanism of these complicated events, especially sex hormone-dependent growth enhancement, has been studied extensively. In MCF-7 cells, an estrogen-induced autocrine loop has been demonstrated to play an important role for estrogen-dependent growth. Androgen has been also found to promote the growth of SC-3 cell through the induction of several autocrine growth factors[4].
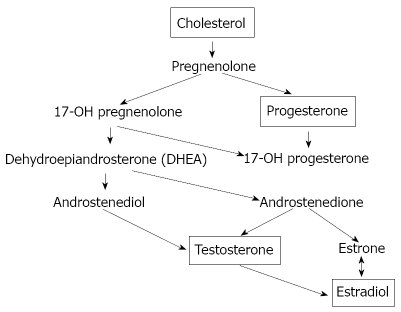
Sex hormones such as estrogens and androgens have been well known to regulate the growth of normal as well as transformed target cells[19-24]. Generally, they have been proposed to promote cell growth whereas so-called anti-hormones inhibit the hormone-dependent growth. For example, anti-androgens such as cyproterone acetate have also been known to accelerate the growth of prostate cancer in some circumstances[5]. Conversely, administration of a large amount of estrogens frequently causes the regression of estrogen-receptor-positive breast cancer[6]. Tamoxifen, the most widely used therapeutic agent of estrogen-dependent breast cancer, exhibits organ- and species-dependent differences in cell growth regulation[7]. Even in the same cells, growth response to tamoxifen has been observed to differ in a dose-dependent manner. One plausible explanation is that two pathways exist for estrogen-dependent growth in target cells, one for the stimulatory and another for the inhibitory signal[4] (Figure 1).
Figure 1.
Two-pathway theory of estrogen-receptor-dependent growth. Many estrogen target cells contain growth-stimulatory and -inhibitory pathways. Both pathways are mediated through ERs. Tamoxifen may possess relatively high affinity for the growth-inhibitory pathway whereas estrogen can mainly activate the growth-stimulatory pathway. However, any ligand for ER can stimulate both pathways.
In particular, estrogens exert a trophic action in several target organs such as liver[8] where they modulate growth and repair, intervening in neonatal liver growth and regeneration after injury in adults[3]. Moreover, chronic administration of estrogens for pharmacological purposes induces an enlargement of liver mass[25,26] and after partial hepatectomy, ERs expression in hepatocytes increases with subsequent transcription of genes involved in proliferation to restore a normal liver mass[25,27]. With this review, we aim to summarize the latest findings about the role of sex hormones on biliary epithelium function, their effects and alterations during cholestasis. The role and mechanism by which sex hormones modulate cholangiocyte functions have been explored only over the last few years at both experimental and clinical levels[28-50].
SEX HORMONES
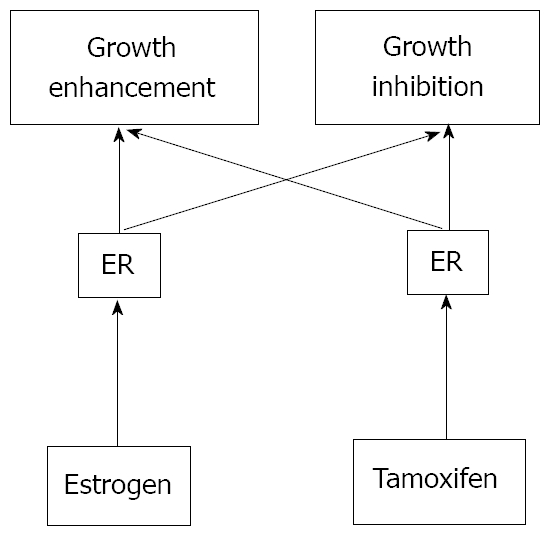
Hormones are the chemical messengers of the body since they are involved in transmission of information from one tissue to another and from cell to cell. Hormones circulate in the bloodstream and interact with target cells that possess receptors that can only be activated by a specific type of hormone. Several kinds of hormones exist for their structure or activity in the cell. Usually they are known as steroids and peptides (Figure 2). In general, steroids are sex hormones, chemical substances made from cholesterol and produced by a sex gland or other organ that has an effect on the sexual features of an organism[9]. Like many other kinds of hormones, they may also be artificially synthesized. On the other hand, peptides are made from long strings of amino acids to regulate other functions and are sometimes referred to as “protein” hormones.
Figure 2.
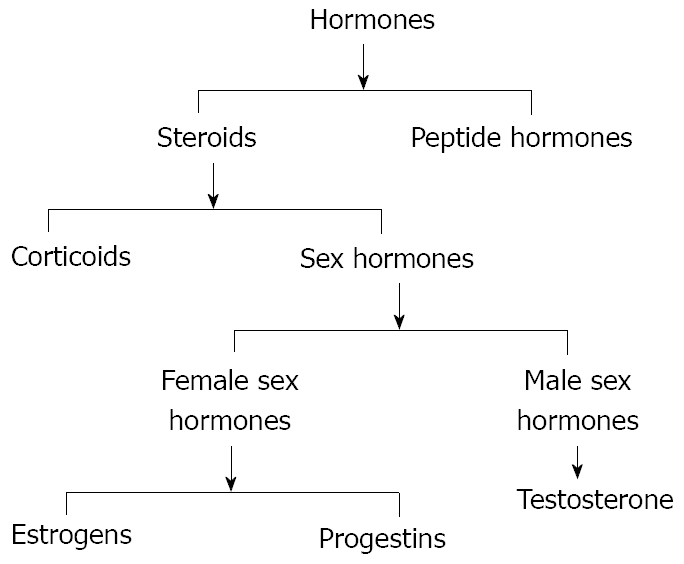
Scheme of the two classes of hormones, steroids and peptide hormones that successively can be divided in corticoids and sex hormones.
Sex hormones are divided into 3 groups: (1) female sex hormones or estrogens; (2) male sex hormones or androgens; and (3) pregnancy hormones or progestins.
Estrogens
Estrogen is a generic term for estrus-producing compounds; the female sex hormones including estradiol, estriol and estrone (Figure 3). In humans, the estrogens are formed in the ovary, adrenal cortex, testis and fetoplacental unit and are responsible for female secondary sex characteristic development and, during the menstrual cycle, act on the female genitalia to produce an environment suitable for fertilization, implantation and nutrition of the early embryo[10]. Uses for estrogens include oral contraceptives, hormone replacement therapy, advanced prostate or postmenopausal breast carcinoma treatment and osteoporosis prophylaxis[51-55]. They also antagonize the effects of the parathyroid hormone minimizing the loss of calcium from bones and thus helping to keep bones strong[11]. Estradiol (E2) is the main female sex hormone. Its actions are mediated by two members of the nuclear receptor superfamily, estrogen receptor ERα and ERβ, and a recently discovered G protein-coupled membrane receptor, GPR30[56,57]. Mechanisms by which ERα and ERβ bind ligand, dimerize, associate with coactivators or corepressors and regulate gene transcription are typically referred to as “genomic” actions[12], which ultimately regulate both cell proliferation and survival[58-61]. Estrogens play biological activities in several organs[13] including the cardiovascular system, nervous system, digestive system and “male” organs such as the prostate. In target tissues, estrogens may exert opposite actions and heterogeneous effects[62-66]. In detail, overexpression of ERα has been associated with cancer development and progression in several organs[14]. The functions of ERβ are linked to a protective effect against uncontrolled or neoplastic cell proliferation[64,67]. In different types of cancer, estrogens synergize the effects of growth factors by acting at both receptor and post-receptor levels favouring the growth and spreading of tumour mass[68-73]. The liver is a hormone-sensitive organ. Both normal liver and hepatocellular carcinoma (HCC) tissues from male and female mammals have been shown to express specific ERs, stimulating both in vivo and in vitro hepatocyte proliferation[15]. Moreover, anti-estrogens like tamoxifen have been shown to reduce levels of ERs and to inhibit hepatocyte proliferation following partial hepatectomy[16]. Long-term use of oral contraceptives (OCs) and anabolic androgenic steroids (AASs) can induce both benign and hepatocellular tumors[17]. Other experimental findings suggest that estrogens have numerous neuroprotective actions. This responsiveness can diminish with age, reducing neuroprotective actions of estrogen[18]. Hormonal treatment plays an established role in several solid tumors, first of all in breast cancer where, for the last decades, the antiestrogen tamoxifen has been the most commonly used treatment for patients with estrogen receptor alpha (ER)-positive breast cancer[19]. Tamoxifen is characterized by a favourable toxicity profile which, together with the easy oral administration, makes this drug an interesting candidate for treatment of other solid tumors potentially responding to hormonal manipulation[74-77]. In addition, there is increasing evidence showing that adipose tissue is a site of steroid metabolism, including the interconversion of estrone (E1) and E2. The presence of both estrogen receptors (ERα and ERβ) in preadipocytes and mature adipocytes strongly suggest a role for active estrogen in these cells. For that reason, adipose tissue can be considered a significant source of estrogenic compounds.
Figure 3.
The biosynthesis of the sex hormones starts with the oxidation of the side chain of cholesterol, which is catalyzed by the enzyme cytochrome P450scc to form pregnenolone. The next steps in the biosynthesis of testosterone can proceed via two different routes. Pregnenolone can be oxidised first by cytochrome P45017a to 17a-hydroxypregnenolone. The enzyme 3β-HSD also can convert pregnenolone first into progesterone. Both pregnenolone and progesterone are accepted as substrate by the enzyme cytochrome P45017a. In this way, after 3β-hydroxy-5-androstene-17-one (DHEA) synthesis, there is the testosterone and successively the estradiol formation.
Androgens
Androgens are a special kind of fat molecule with a four-ringed, carbon atom backbone or core[20]. A series of chemical reactions transform cholesterol first into the steroid pregnenolone and then into testosterone and other androgens (Figure 3). Like all steroid hormones, androgens produce effects by docking with receptors on the cell’s membrane surface or inside the cell in the liquid cytoplasm[20]. The steroid hormone/receptor unit moves into the nucleus activating specific genes. These genes drive the cell changes guiding androgen-controlled growth and development[21]. Scientists have studied androgens since the 18th century. John Hunter initially described androgenic actions in 1771. Almost two century later in 1935, Leopold Ruzicka worked out the chemical structure of the “androgenic principle” from the testes, calling it testosterone[22]. Testosterone and dihydrotestosterone (17-beta-hydroxy-5-alpha-androstan-3-one) are the most potent androgens in humans and four-legged vertebrates[20]. The weaker androgens androstenedione and dehydroepiandrosterone (DHEA) occur in small amounts in all vertebrates[23]. Testosterone is essential for the production of sperm and is manufactured by the interstitial Leydig cells of the testes. Its secretion increases sharply at puberty and is responsible for the development of the so-called secondary sexual characteristics of men during puberty[20]. Synthetic testosterone analogs are used in medicine to promote muscle and tissue growth in patients with muscular atrophy[24]. Testosterone therapy is indicated in adult men for the treatment of hypogonadism[25]. Over the last three decades it has become apparent that testosterone plays a significant role in the maintenance of bone and muscle mass, in erythropoiesis and in mental functions. Androgens are also key players in glucose homeostasis and lipid metabolism and exert an important role in liver. In fact, it has been observed that androgen receptors (ARs) are present in normal liver tissue from both males and females and that their expression is increased in tumor tissue[16]. Moreover, cross-sectional epidemiological studies have reported a direct correlation between plasma testosterone and insulin sensitivity and low testosterone levels are associated with an increased risk of type 2 diabetes mellitus, dramatically illustrated by androgen deprivation in men with prostate carcinoma[42,43]. Prostate cancer is one of the most common cancers among men and androgens are involved in controlling the growth of androgen-sensitive malignant prostatic cells[26]. The model of LNCaP prostate cancer cell line was used to study androgen and estrogen metabolism during the transformation process. It was discovered that substantial changes in androgen and estrogen metabolism occur in the cells during the process[45-47]. Recent evidence indicates androgen actions in protecting the brain against neurodegenerative diseases and their positive effects on age-related testosterone loss in men and increased risk for Alzheimer’s disease (AD)[27]. The successful use of hormone therapies in aging men and women to delay, prevent and/or treat Alzheimer’s disease will require additional research to optimize key parameters of hormone therapy[28].
Progestins
The term progestins is defined as the natural or synthetic progestational substances that mimics some or all of the actions of progesterone, a crude hormone of the corpus luteum from which progesterone can be isolated in pure form[29]. Progesterone is responsible for preparing the uterus for implementation of the fertilized egg. It also has an important role as a birth control agent[30]. It is a steroid hormone produced in the ovary under the control of the pituitary gonadotropins[78-80] (Figure 4). It has also been recently demonstrated that the synthetic progestogen, levonorgestrel, increases progesterone accumulation in cultured, stable porcine granulosa cells, the JC-410[81-93]. Results of those studies have been interpreted to suggest that progestins may affect progesterone synthesis by the regulation of steroidogenic enzymes, the cytochrome P450 side-chain cleavage (P450scc) and 3β-hydroxysteroid dehydrogenase (3β-HSD)[31]. The genomic action of progesterone is mediated by two progesterone receptor (PR) isoforms, A and B[84,85]. PR-B is a strong activator of gene transcription, whereas PR-A can act as a ligand-dependent trans-repressor of PR-B[32]. The large majority of PR target genes have been identified in breast cancer cells[87,88]. Different evidence indicates that this hormone also exerts neuroprotective effects on the central nervous system (CNS). Its neuroprotective actions make it a particularly promising therapeutic agent for neuroinjury and neurodegenerative diseases. Progesterone appears to exert its protective effects by protecting or rebuilding the blood-brain barrier, decreasing the development of cerebral edema, down-regulating the inflammatory cascade and limiting cellular necrosis and apoptosis[33]. The family of anti-progestins, i.e. mifepristone, includes pure agonists such as progesterone itself or progestins and, at the other end of the biological spectrum, pure progesterone receptor antagonists (PA). Selective progesterone receptor modulators (SPRM) have mixed agonist-antagonist properties and occupy an intermediate position of the spectrum. Mifepristone is used to terminate pregnancy[34]. Many PA and SPRM display direct antiproliferative effects in the endometrium although with variable actions which seem product- and dose-dependent. This property justifies their use in the treatment of myomas and endometriosis. Interestingly, clinical data show that treatment with these compounds is not associated with hypo-estrogenism and bone loss. The potential clinical applications of these compounds cover a broad field and are very promising in major public health areas. Further developments might also include hormone replacement therapy in post-menopausal women as well as the treatment of hormone-dependent tumors[35].
Figure 4.
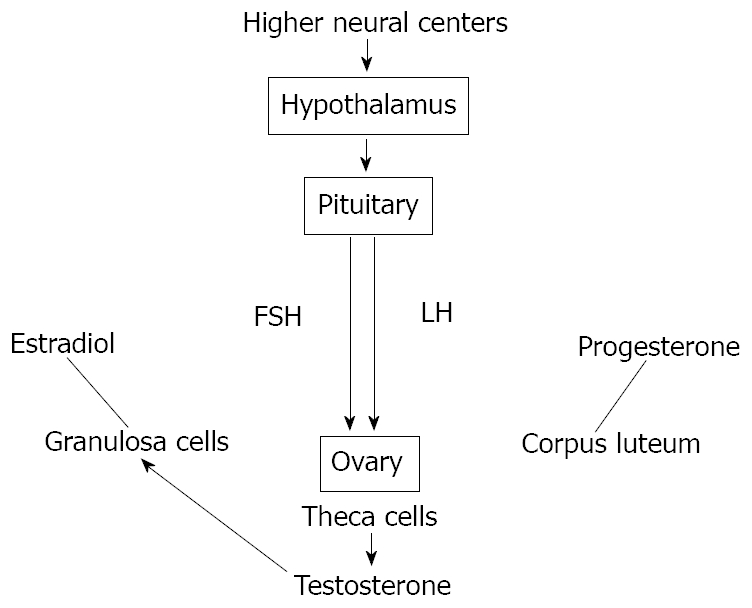
Scheme of hypothalamic-pituitary-gonadal (HPG) axis control exerted by both circulating and in situ locally produced estradiol in men. This axis controls development, reproduction, and aging in animals. The hypothalamus produces gonadotropin-releasing hormone (GnRH). The pituitary gland produces luteinizing hormone (LH) and follicle-stimulating hormone (FSH), and the gonads produce estrogen, progesterone and testosterone from different kinds of cells.
Other sex hormones
Another group of substances secreted by the pituitary gland can be defined sex hormones. They include the follicle-stimulating hormone (FSH), the luteinizing hormone (LH) and the prolactin (Prl). The synthesis and secretion of estrogens is stimulated by FSH which is in turn controlled by the hypothalamic gonadotropin releasing hormone (GnRH) (Figure 4). High levels of estrogens suppress the release of GnRH providing a negative-feedback control of hormone levels[36]. Progesterone production is stimulated by LH which is also stimulated by GnRH[36]. Elevated levels of progesterone control themselves by the same negative feedback loop used by estrogen[37]. The two gonadotropins, FSH and LH, are key regulators of ovarian cell functions and the potential role of gonadotropins in the pathogenesis of ovarian cancer is suggested. The presence of gonadotropins in ovarian tumor fluid and their receptors expression suggests the importance of these factors in the transformation and progression of ovarian cancers as well as being prognostic indicators[94-97]. The recent cDNA microarray analyses and characterization in the molecular mechanisms of gonadotropin signaling have indicated the effects of gonadotropins on the regulation of some ovarian cancer cell growth, survival and metastasis that may involve other growth factors[38]. Prl is another hormone released by the pituitary gland that stimulates breast development and milk production in women[39]. It is secreted by so-called lactotrophs in the anterior pituitary as a prohormone. Although the pleiotropic actions of Prl are recognized, its role in regulating growth and differentiation of mammary tissues is better understood[98,99]. Several lines of evidence have also indicated that Prl acts as an autocrine, paracrine and endocrine progression factor for mammary carcinoma in vitro and in vivo in rodents and humans[100]. These data include recent epidemiologic studies indicating that postmenopausal women with ‘high-normal’ levels of Prl are at increased risk of breast cancer[101-105]. Elevated prolactin (hyperprolactinemia) may be due to a benign tumor in the pituitary gland called a prolactinoma. Abnormally low prolactin (hypoprolactinemia) can cause menstrual disorders and lead to inadequate lactation[31]. It is concluded that the rat is a predictive model for human mammary carcinogenesis and that rat mammary carcinogenesis induced by hyperprolactinaemic drugs may have greater importance in human toxicological risk than previously thought[40].
ESTROGENS AND BILIARY EPITHELIUM
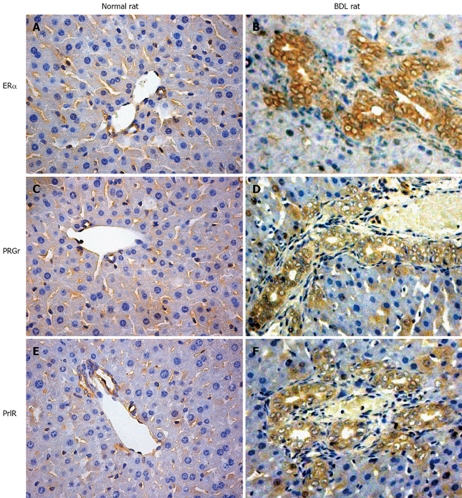
Estrogens and their metabolites have been hypothesized to have a pathogenic role in the diseases which preferentially affect the female sex[106-109]. Furthermore, marked alterations of estrogen hepatic metabolism occurs in cholestasis which is one of the hallmarks of cholangiopathies, including the decreased hepatic levels of P450-dependent microsomal enzymes with a consequent enhanced estradiol serum level[41]. Over the last years, we have discovered that rat cholangiocytes express both ERα and ERβ subtypes while hepatocytes only express ERα[28]. In addition to that, cholangiocyte proliferation after BDL is associated with a marked increase in the expression of ER and especially the ERβ while hepatocytes which do not proliferate after BDL display a decrease of ERα protein expression[42] (Figure 5). This important role of estrogens in modulating cholangiocyte proliferation during BDL is associated with enlarged bile duct mass and enhanced estradiol serum levels[29].
Figure 5.
Some representative immunohistochemistry for Erα, progesterone and prolactin receptors in normal and bile duct ligation (BDL) rats. A, B: Erα receptors; C, D: progesterone receptors; E, F: prolactin receptors. The expression of all these receptors is highly increased after BDL compared with that in the biliary epithelium of the normal animal. Original magnification × 40.
The role of estrogens in modulating cholangiocyte proliferation has been confirmed by experiments showing that when BDL rats were treated with tamoxifen or the pure ER antagonist, ICI 182,780, the intrahepatic bile duct mass was markedly decreased in comparison with the control rats by impaired proliferation and enhanced cholangiocyte apoptosis. In breast cancer and hepatocellular carcinoma, tamoxifen induces cell death by multiple mechanisms including the blocking of the mitogenic effect of estrogens and induction of apoptosis-related genes[43]. In fact, the Fas receptor/Fas ligand pathway plays a crucial role in tamoxifen-induced apoptosis in hepatocellular carcinoma and cholangiocarcinoma cell lines[110-112]. To support the positive modulatory effect of estrogens on cholangiocyte proliferation, in vitro experiments show that proliferation of isolated rat cholangiocytes were significantly increased by 17β-estradiol and that these effects were individually blocked by ER antagonists[28]. Regarding the role of endogenous estrogens on modulating cholangiocyte proliferation during experimental cholestasis, we also evaluated the effects of ovariectomy (OVX) and estrogen replacement treatment in BDL rats[44]. OVX rats were submitted to BDL and the bile duct mass was compared with control BDL rats submitted to sham-OVX and with BDL-OVX rats treated with exogenous administration of 17β estradiol. OVX induced a significant reduction of bile duct mass in BDL rats that was associated with a decreased expression of ERβ. Administration of 17β estradiol induced a normalization of bile duct mass, ER expression and cholangiocyte proliferation in comparison with untreated BDL rats. A probable cross-talk between estrogens and growth factors including IGF1 (insulin like growth factor) has been proposed and later demonstrated that result in a synergistic growth stimulation[4,112]. This signaling cascade, typically activated by growth factors acting through tyrosine kinase receptors, involves the recruitment of the steroid receptor-coactivator (Src) and adapter protein Shc (Src-homology/collagen protein) which act upstream to the mitogen-activated protein (MAP) kinase isoforms ERK1/2 (extracellular signal-regulated kinase)[113,114]. We found that cholangiocyte proliferation induced by BDL involves the activation of the Src/Shc/ERK signalling cascade blocked through administration of ER antagonists[45].
Normally, human cholangiocytes do not express ERs but they stain positive for ERα and β in different pathological conditions such as primary biliary cirrhosis (PBC)[31], polycystic liver disease[115] and cholangiocarcinoma[116-121]. All these conditions are characterized by reactive or neoplastic cholangiocyte proliferation, suggesting that estrogens and their receptors may play a role in modulating the proliferative activities of cholangiocytes and therefore the course of these diseases.
PBC is one of the chronic cholestatic liver diseases which represent the most frequent acquired cholangiopathy. This is an autoimmune liver disease in that the key pathology involves the attack upon the small, microscopic bile ducts by immune system inflammatory cells. The result is a chronic granulomatous inflammatory infiltrate invading and progressively destroying the small bile ducts within the portal tracts of the liver[46]. The disease predominantly affects females with a typical clinical presentation occurring during the peri- and post-menopausal period[47]. Recent findings suggest that estrogens may influence the course of PBC by directly modulating the pathophysiology of cholangiocytes[31]. In fact, in PBC, such as in other chronic cholestatic conditions, estrogen serum levels are increased as a consequence of impaired hepatic metabolism and biliary excretion of estrogens and their metabolites[48]. However, estrogen replacement therapy as osteoporosis treatment has been shown to be safe in PBC patients[49]. These clinical studies allowed summarizing the concept that administration of estrogens in PBC patients exerts deleterious effects on the liver but they can improve liver function. During PBC, the ER expression varies according to different stages and correlates with markers of proliferation and apoptosis. ERα expression increases from 1% of cholangiocytes in PBC stage I to 12% in stage III while ERβ is stably high in all histological stages. Interestingly, in stages I-III, ERα expression co-localizes with PCNA indicating that the expression of this receptor subtype is a typical feature of proliferating cholangiocytes. Furthermore, in stage IV of PBC where there is the maximal degree of ductopenia, cholangiocytes are negative for ERα and express the lowest proliferation/apoptosis ratio[31]. We can speculate that a relative proliferative deficiency of cholangiocytes in the terminal ductopenic stages of PBC is associated with the disappearance of ERα. These findings could have important therapeutic implication by the modulation of ERs. To this latter regard, preliminary clinical observations indicate that tamoxifen improves biochemical parameters of cholestatis in PBC patients. Interestingly, through the ERα, estrogens can positively modulate the GH/ IGF-1 axis[14].
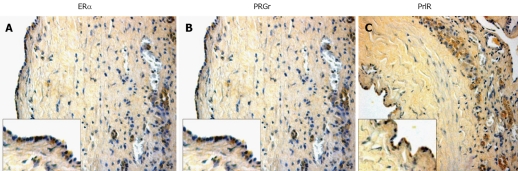
Autosomal dominant polycystic kidney disease (ADPKD) is one of the most prevalent human genetic diseases[50]. Hepatic cysts are the most common extra-renal clinical manifestation of ADPKD[51]. Estrogens have a role in the development and progression of hepatic cysts in ADPKD patients. The probability of developing hepatic cysts is higher in women than in men. Many studies and the clinical observations show a strict estrogen sensitivity of cyst formation and progression in ADPKD patients[122,123]. First of all, the epithelial layer of hepatic cysts presents the expression of ERβ and this occurs in all cysts examined, whereas the staining for ERα was less evident (Figure 6). Estrogens act not only directly but also by promoting the synthesis and release of growth factors from the cyst epithelium[115]. These findings show how the formation and progression of hepatic cysts is highly sensitive to changes in the estrogen status in the body[4,115].
Figure 6.
Immunohistochemistry for ERα, progesterone and prolactin receptors in liver sections from patients affected with polycystic liver disease. A: Erα receptors; B: progesterone recepors; C: prolactin receptors. Also in course of human cholangiopathies, these three considered receptors seem to play an important role in cholangiocyte physiology. Original magnification × 20.
Cholangiocarcinoma is a malignant tumor arising from cholangiocytes and characterized by a poor prognosis and scarce response to current therapies[124-132]. Human intrahepatic cholangiocarcinoma and the human intrahepatic cholangiocarcinoma cell line HuH-28 express ERs. The use of 17β-estradiol stimulates proliferation and inhibits apoptosis of HuH-28 cell lines, findings comparable with the proliferative response of MCF7, a breast cancer cell line. Proliferation of these cells induced by 17β-estradiol is associated with enhanced protein expression of ERα, p-ERK1/2 and pAKT but with decreased protein expression of ERβ[32,116]. This further supports the role of ERα in the estrogen-dependent modulation of neoplastic cell growth. Estrogens appear to act in several critical points of the IGF signal transduction pathway. ERα and IGF-1R have been shown to co-precipitate and their state of activation as well as the related signaling pathways have been shown to be potentiated by their coupling[52]. Finally, this mechanism may converge at different common transduction pathways modulating proliferation including ERK and phosphatidylinositol-3 kinase/Akt pathways[53]. Thus, the role played by estrogens and their receptors in the growth of ER-positive neoplasms represents the basis for the pharmacological treatment and/or prevention of different cancers with ER antagonists.
ANDROGENS AND BILIARY EPITHELIUM
The role of androgens on biliary epithelium has been poorly investigated. In fact, we have only preliminary data on the castration effects in normal and experimental rat model of BDL in which there is a decrease in androgen receptors expression and impairment in cholangiocyte growth especially after bile duct ligation to support the hypothesis that testosterone, as estrogens, may play a key role in biliary epithelium proliferation[54]. In human conditions, several studies exist on the use of anabolic androgenic steroid (AAS). They are frequently utilized at high doses by bodybuilders to achieve a rapid increase in muscle mass although they are associated with a number of side effects. Several liver disorders have been reported to be associated with AAS consumption such as cholestasis, peliosis hepatis and liver tumors[55]. In recent times, this use has also been proved to be involved in the development of hepatic adenomas (HA)[56]. Although more than 750 cases of oral contraceptive-induced HA have been reported, apparently androgen-induced HA are relatively rare. HA are not malignant tumors but surgical intervention may be required if sudden massive bleeding or liver failure occurs; rupture of HA with haemoperitoneum can be a life threatening complication[57]. A non-surgical approach should be considered for androgen-induced HA given that some tumors have regressed after AAS administration was stopped[58]. In any case, after a diagnosis of liver tumors the administration of AAS should cease[133-135].
PROGESTINS AND BILIARY EPITHELIUM
As previously summarized, a number of studies have shown that, not only estrogens and androgens but also progestins strongly regulate cholangiocyte functions. Glaser et al have been found that female and male rat cholangiocytes express nuclear and membrane receptors that bind progesterone (PR, PGRMC1, PGRMC2, and mPRα). Following chronic administration of progesterone to normal female and male rats, there is an increase in biliary growth which can be partly prevented by the simultaneous administration of the nuclear progesterone receptor antagonist RU-486[59] or with administration of a neutralizing anti-progesterone antibody[60]. Finally, this study also demonstrated for the first time that the biliary epithelium possesses the enzymatic pathway for the steroidogenesis of progesterone and secrete progesterone, indicating that, in addition to a paracrine pathway, cholangiocytes regulate their growth in an autocrine mechanism[136-142] (Figure 6). In humans, the concentrations in serum of sulfated metabolites of progesterone are known to be elevated in patients with intrahepatic cholestasis of pregnancy (ICP)[61]. Some studies propose that patients with ICP have a selective defect in this secretion into bile probably for a genetic polymorphism of canalicular transporters for steroid sulphates or their regulation. Interaction with estrogen metabolites may further enhance the process triggering ICP in genetically predisposed individuals[62]. Ursodeoxycholic acid, an important bile acid, stimulates the biliary excretion of these metabolites, particularly those with a 3alpha-hydroxy-5alpha (H) configuration and disulphates. The effect appears to be independent of the stimulation of bile acid secretion. An effect of ursodeoxycholic acid on the reductive metabolism of progesterone cannot be excluded[63].
OTHER SEX HORMONES AND BILIARY EPITHELIUM
Information on the role of FSH in liver pathophysiology is limited[64]. A study has demonstrated that liver cirrhosis is associated with endocrine dysfunction, notably in the gonadal axis[65]. In males it has been recognized that cirrhotic liver disease is associated with hypogonadism and feminization parallel with impairments in the serum level of sex hormones[66]. The derangement of hypothalamic-pituitary function may play a role in the sexual dysfunction and changes in sex hormones in male patients with cirrhosis[64]. For the first time, we have shown that the biliary epithelium expresses FSHR and that FSH is a trophic factor for the biliary epithelium since chronic administration of FSH to normal rats increased cholangiocyte proliferation and intrahepatic ductal mass by cAMP-dependent phosphorylation of ERK1/2 and Elk-1[12-13]. In support of the findings that FSH treatment increases cholangiocyte FSH receptor expression, it has been demonstrated that it induces follicular growth and ovulation together with an increase in FSH binding and mRNA levels in ovaries[143,144]. In addition, another study has demonstrated that treatment of these cells with FSH increases the levels of two FSH receptor mRNA transcripts[67]. Although FSH may modulate cholangiocyte growth by a paracrine mechanism, our studies support the novel concept that FSH is a key player in the autocrine loop regulating the balance between cholangiocyte proliferation and loss. These findings have important pathological implications since modulation of cholangiocyte expression and secretion of the trophic factor FSH may be important in the management of chronic cholestatic liver diseases[145].
Regarding the other gonadotropin, it has been observed that with a reduction in the plasma level of testosterone there is an elevation of the LH level in BDL rats demonstrating a primary defect in testosterone production by testes[146].
If the BDL rats were treated with L-NAME, a NO inhibitor, to reduce its over production during bile duct ligation, there is an interesting effect on the LH levels[68]. Prolonged L-NAME treatment could not decrease the elevated level of LH in BDL rats while it could increase the level of testosterone in those rats. These data suggest that the primary effect of bile duct ligation is at the level of Leydig cells and the increase of LH is secondary to the decrease in circulating testosterone. One interpretation is that L-NAME has only a partial effect on the NO inhibited Leydig cells which can produce normal levels of testosterone after being stimulated by an increased level of LH. The other interpretation is based on the complex effect of NO on gonadotropin secretion. In fact, it has previously been clearly demonstrated that NO stimulates LHRH secretion by activating guanylate cyclase and supports a potential role of NO as a neuroactive agent involved in the control of LHRH secretion and, thereby, reproductive functions[69]. It has also been suggested that the endogenous level of NO may determine the sensitivity of GnRH-stimulated gonadotropin released by the anterior pituitary[146-151].
In addition, Prl participates in the regulation of liver function. Their receptors (PrlR) are expressed by rat hepatocytes in the sinusoidal domain of cellular membranes and in perinuclear areas[70]. They are also expressed by human hepatocytes of patients with obstructive jaundice of different etiology but prolactin receptor expression is lower in hepatocytes compared to human cholangiocytes[71]. The expression pattern and regulation of PrlR isoforms is totally different in cholangiocytes compared to hepatocytes. In fact, mature rat cholangiocytes express low levels of PrlR while it is very high in hepatocytes; only the long isoform is detected in cholangiocytes while the short isoform predominates in hepatocytes; and PrlR levels in cholangiocytes are induced by obstructive cholestasis while it is the opposite in hepatocytes. From these data, the actions of prolactin on liver are anticipated to exhibit strong cell-type specificity in both normal and pathological conditions[72] (Figure 6).
Taffetani et al have demonstrated that Prl regulates the growth of female cholangiocytes, presumably by an autocrine mechanism. In fact, cholangiocytes from normal and BDL female and male rats express prolactin receptors. Furthermore, Prl has a trophic effect on the growth of normal female cholangiocytes by phosphorylation of PKCβ-I and dephosphorylation of PKCα. In addition, cholangiocytes express the protein for and secrete prolactin, suggesting that prolactin participates by an autocrine mechanism in the modulation of cholangiocyte proliferation and that it may be an important therapeutic approach for the management of cholangiopathies[152-159].
CONCLUSION
A large body of evidence supports the therapeutic potential of sex hormones in animal models and human clinical conditions in the modulation of cholangiocyte growth/loss. Mechanisms of action for most of them have been studied and others are in the course of study. Further investigations are needed to elucidate the precise mechanism of androgens, progestins and their receptors in regulating normal liver physiology and pathophysiology of cholestatic diseases. All of this interestingly suggests that sex hormones represent novel and important treatment options that could beneficially affect the pathophysiology of the biliary epithelium. Sex hormones clearly function as more than reproductive compounds by exhibiting a myriad of roles that are also essential to protect liver and biliary functions. In particular, the main concept is that estrogens and probably other hormones act by synergizing the effects of growth factors. This interaction may have more clinical implications for diseases involving the biliary epithelium in which cholangiocyte proliferation is a typical hallmark influencing disease progression and may also be relevant in the course of the neoplastic transformation. In conclusion, sex hormones are regulators of cholangiocyte proliferation in cholestasis and their modulation could represent a future therapeutic strategy for the management of cholangiopathies.
Footnotes
Supported partly by the University Federate Athenaeum Funds from University of Rome “La Sapienza” and PRIN 2007 to Gaudio E, University Funds to Onori P, the Dr. Nicholas C Hightower Centennial Chair of Gastroenterology from Scott and White, the VA Research Scholar Award, a VA Merit Award and the NIH Grants DK58411, and DK76898 to Dr. Alpini, a NIH RO1 Grant Award to Dr. Glaser (DK081442), a NIH K01 Grant Award (DK078532) to Dr. DeMorrow
Peer reviewer: Wei-Biao Cao, MD, Assistant Professor, Department of Medicine and Pathology, Rhode Island Hospital and the Warren Alpert Medical School of Brown University 55 Claverick St, Room 337, Providence, RI 02903, United States
S- Editor Zhang HN L- Editor Roemmele A E- Editor Liu N
References
- 1.Alpini G, McGill JM, Larusso NF. The pathobiology of biliary epithelia. Hepatology. 2002;35:1256–1268. doi: 10.1053/jhep.2002.33541. [DOI] [PubMed] [Google Scholar]
- 2.Marzioni M, Fava G, Alvaro D, Alpini G, Benedetti A. Control of cholangiocyte adaptive responses by visceral hormones and neuropeptides. Clin Rev Allergy Immunol. 2009;36:13–22. doi: 10.1007/s12016-008-8090-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glaser SS, Gaudio E, Miller T, Alvaro D, Alpini G. Cholangiocyte proliferation and liver fibrosis. Expert Rev Mol Med. 2009;11:e7. doi: 10.1017/S1462399409000994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alvaro D, Mancino MG, Onori P, Franchitto A, Alpini G, Francis H, Glaser S, Gaudio E. Estrogens and the pathophysiology of the biliary tree. World J Gastroenterol. 2006;12:3537–3545. doi: 10.3748/wjg.v12.i22.3537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gigliozzi A, Alpini G, Baroni GS, Marucci L, Metalli VD, Glaser SS, Francis H, Mancino MG, Ueno Y, Barbaro B, et al. Nerve growth factor modulates the proliferative capacity of the intrahepatic biliary epithelium in experimental cholestasis. Gastroenterology. 2004;127:1198–1209. doi: 10.1053/j.gastro.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 6.Gaudio E, Carpino G, Cardinale V, Franchitto A, Onori P, Alvaro D. New insights into liver stem cells. Dig Liver Dis. 2009;41:455–462. doi: 10.1016/j.dld.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Gaudio E, Franchitto A, Pannarale L, Carpino G, Alpini G, Francis H, Glaser S, Alvaro D, Onori P. Cholangiocytes and blood supply. World J Gastroenterol. 2006;12:3546–3552. doi: 10.3748/wjg.v12.i22.3546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LeSage G, Glaser S, Alpini G. Regulation of cholangiocyte proliferation. Liver. 2001;21:73–80. doi: 10.1034/j.1600-0676.2001.021002073.x. [DOI] [PubMed] [Google Scholar]
- 9.Ueno Y, Francis H, Glaser S, Demorrow S, Venter J, Benedetti A, Fava G, Marzioni M, Alpini G. Taurocholic acid feeding prevents tumor necrosis factor-alpha-induced damage of cholangiocytes by a PI3K-mediated pathway. Exp Biol Med (Maywood) 2007;232:942–949. [PubMed] [Google Scholar]
- 10.Marucci L, Alpini G, Glaser SS, Alvaro D, Benedetti A, Francis H, Phinizy JL, Marzioni M, Mauldin J, Venter J, et al. Taurocholate feeding prevents CCl4-induced damage of large cholangiocytes through PI3-kinase-dependent mechanism. Am J Physiol Gastrointest Liver Physiol. 2003;284:G290–G301. doi: 10.1152/ajpgi.00245.2002. [DOI] [PubMed] [Google Scholar]
- 11.Lesage G, Glaser S, Ueno Y, Alvaro D, Baiocchi L, Kanno N, Phinizy JL, Francis H, Alpini G. Regression of cholangiocyte proliferation after cessation of ANIT feeding is coupled with increased apoptosis. Am J Physiol Gastrointest Liver Physiol. 2001;281:G182–G190. doi: 10.1152/ajpgi.2001.281.1.G182. [DOI] [PubMed] [Google Scholar]
- 12.Francis H, Franchitto A, Ueno Y, Glaser S, DeMorrow S, Venter J, Gaudio E, Alvaro D, Fava G, Marzioni M, et al. H3 histamine receptor agonist inhibits biliary growth of BDL rats by downregulation of the cAMP-dependent PKA/ERK1/2/ELK-1 pathway. Lab Invest. 2007;87:473–487. doi: 10.1038/labinvest.3700533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Francis H, LeSage G, DeMorrow S, Alvaro D, Ueno Y, Venter J, Glaser S, Mancino MG, Marucci L, Benedetti A, et al. The alpha2-adrenergic receptor agonist UK 14,304 inhibits secretin-stimulated ductal secretion by downregulation of the cAMP system in bile duct-ligated rats. Am J Physiol Cell Physiol. 2007;293:C1252–C1262. doi: 10.1152/ajpcell.00031.2007. [DOI] [PubMed] [Google Scholar]
- 14.Glaser S, Alvaro D, Francis H, Ueno Y, Marucci L, Benedetti A, De Morrow S, Marzioni M, Mancino MG, Phinizy JL, et al. Adrenergic receptor agonists prevent bile duct injury induced by adrenergic denervation by increased cAMP levels and activation of Akt. Am J Physiol Gastrointest Liver Physiol. 2006;290:G813–G826. doi: 10.1152/ajpgi.00306.2005. [DOI] [PubMed] [Google Scholar]
- 15.Svegliati-Baroni G, Ghiselli R, Marzioni M, Alvaro D, Mocchegiani F, Saccomanno S, Sisti V, Ugili L, Orlando F, Alpini G, et al. Estrogens maintain bile duct mass and reduce apoptosis after biliodigestive anastomosis in bile duct ligated rats. J Hepatol. 2006;44:1158–1166. doi: 10.1016/j.jhep.2005.10.032. [DOI] [PubMed] [Google Scholar]
- 16.Gaudio E, Barbaro B, Alvaro D, Glaser S, Francis H, Ueno Y, Meininger CJ, Franchitto A, Onori P, Marzioni M, et al. Vascular endothelial growth factor stimulates rat cholangiocyte proliferation via an autocrine mechanism. Gastroenterology. 2006;130:1270–1282. doi: 10.1053/j.gastro.2005.12.034. [DOI] [PubMed] [Google Scholar]
- 17.Diel P. Tissue-specific estrogenic response and molecular mechanisms. Toxicol Lett. 2002;127:217–224. doi: 10.1016/s0378-4274(01)00503-3. [DOI] [PubMed] [Google Scholar]
- 18.Sato B. Can an autocrine loop explain sex-hormone-dependent tumor growth? A brief overview. Oncology. 1999;57 Suppl 2:3–6. doi: 10.1159/000055269. [DOI] [PubMed] [Google Scholar]
- 19.McPherson SJ, Ellem SJ, Risbridger GP. Estrogen-regulated development and differentiation of the prostate. Differentiation. 2008;76:660–670. doi: 10.1111/j.1432-0436.2008.00291.x. [DOI] [PubMed] [Google Scholar]
- 20.Ray R, Novotny NM, Crisostomo PR, Lahm T, Abarbanell A, Meldrum DR. Sex steroids and stem cell function. Mol Med. 2008;14:493–501. doi: 10.2119/2008-00004.Ray. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scher HI, Kelly WK. Flutamide withdrawal syndrome: its impact on clinical trials in hormone-refractory prostate cancer. J Clin Oncol. 1993;11:1566–1572. doi: 10.1200/JCO.1993.11.8.1566. [DOI] [PubMed] [Google Scholar]
- 22.Dorssers LC, Van der Flier S, Brinkman A, van Agthoven T, Veldscholte J, Berns EM, Klijn JG, Beex LV, Foekens JA. Tamoxifen resistance in breast cancer: elucidating mechanisms. Drugs. 2001;61:1721–1733. doi: 10.2165/00003495-200161120-00004. [DOI] [PubMed] [Google Scholar]
- 23.De Matteis F, White IN, Smith LL. Species differences in the metabolic activation of tamoxifen into genotoxic derivatives: risk assessment in women. Eur J Drug Metab Pharmacokinet. 1998;23:425–428. doi: 10.1007/BF03192304. [DOI] [PubMed] [Google Scholar]
- 24.Eagon PK, Porter LE, Francavilla A, DiLeo A, Van Thiel DH. Estrogen and androgen receptors in liver: their role in liver disease and regeneration. Semin Liver Dis. 1985;5:59–69. doi: 10.1055/s-2008-1041758. [DOI] [PubMed] [Google Scholar]
- 25.Francavilla A, Polimeno L, DiLeo A, Barone M, Ove P, Coetzee M, Eagon P, Makowka L, Ambrosino G, Mazzaferro V. The effect of estrogen and tamoxifen on hepatocyte proliferation in vivo and in vitro. Hepatology. 1989;9:614–620. doi: 10.1002/hep.1840090417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ni N, Yager JD. Comitogenic effects of estrogens on DNA synthesis induced by various growth factors in cultured female rat hepatocytes. Hepatology. 1994;19:183–192. [PubMed] [Google Scholar]
- 27.Wang AG, Lee KY, Kim SY, Choi JY, Lee KH, Kim WH, Wang HJ, Kim JM, Park MG, Yeom YI, et al. The expression of estrogen receptors in hepatocellular carcinoma in Korean patients. Yonsei Med J. 2006;47:811–816. doi: 10.3349/ymj.2006.47.6.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alvaro D, Alpini G, Onori P, Perego L, Svegliata Baroni G, Franchitto A, Baiocchi L, Glaser SS, Le Sage G, Folli F, et al. Estrogens stimulate proliferation of intrahepatic biliary epithelium in rats. Gastroenterology. 2000;119:1681–1691. doi: 10.1053/gast.2000.20184. [DOI] [PubMed] [Google Scholar]
- 29.Alvaro D, Alpini G, Onori P, Franchitto A, Glaser SS, Le Sage G, Folli F, Attili AF, Gaudio E. Alfa and beta estrogen receptors and the biliary tree. Mol Cell Endocrinol. 2002;193:105–108. doi: 10.1016/s0303-7207(02)00103-x. [DOI] [PubMed] [Google Scholar]
- 30.Alvaro D, Alpini G, Onori P, Franchitto A, Glaser S, Le Sage G, Gigliozzi A, Vetuschi A, Morini S, Attili AF, et al. Effect of ovariectomy on the proliferative capacity of intrahepatic rat cholangiocytes. Gastroenterology. 2002;123:336–344. doi: 10.1053/gast.2002.34169. [DOI] [PubMed] [Google Scholar]
- 31.Alvaro D, Invernizzi P, Onori P, Franchitto A, De Santis A, Crosignani A, Sferra R, Ginanni-Corradini S, Mancino MG, Maggioni M, et al. Estrogen receptors in cholangiocytes and the progression of primary biliary cirrhosis. J Hepatol. 2004;41:905–912. doi: 10.1016/j.jhep.2004.08.022. [DOI] [PubMed] [Google Scholar]
- 32.Mancino A, Mancino MG, Glaser SS, Alpini G, Bolognese A, Izzo L, Francis H, Onori P, Franchitto A, Ginanni-Corradini S, et al. Estrogens stimulate the proliferation of human cholangiocarcinoma by inducing the expression and secretion of vascular endothelial growth factor. Dig Liver Dis. 2009;41:156–163. doi: 10.1016/j.dld.2008.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Torrice A, Cardinale V, Gatto M, Semeraro R, Napoli C, Onori P, Alpini G, Gaudio E, Alvaro D. Polycystins play a key role in the modulation of cholangiocyte proliferation. Dig Liver Dis. 2010;42:377–385. doi: 10.1016/j.dld.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 34.Gann PH, Hennekens CH, Ma J, Longcope C, Stampfer MJ. Prospective study of sex hormone levels and risk of prostate cancer. J Natl Cancer Inst. 1996;88:1118–1126. doi: 10.1093/jnci/88.16.1118. [DOI] [PubMed] [Google Scholar]
- 35.Lee HJ, Chang C. Recent advances in androgen receptor action. Cell Mol Life Sci. 2003;60:1613–1622. doi: 10.1007/s00018-003-2309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cato AC, Nestl A, Mink S. Rapid actions of steroid receptors in cellular signaling pathways. Sci STKE. 2002;2002:re9. doi: 10.1126/stke.2002.138.re9. [DOI] [PubMed] [Google Scholar]
- 37.Shampo MA, Kyle RA, Steensma DP. Leopold Ruzicka-1939 Nobel Prize in chemistry. Mayo Clin Proc. 2007;82:1p preceeding table of contents. [PubMed] [Google Scholar]
- 38.Notelovitz M. Androgen effects on bone and muscle. Fertil Steril. 2002;77 Suppl 4:S34–S41. doi: 10.1016/s0015-0282(02)02968-0. [DOI] [PubMed] [Google Scholar]
- 39.Kamel HK, Maas D, Duthie EH, Jr Role of hormones in the pathogenesis and management of sarcopenia. Drugs Aging. 2002;19:865–877. doi: 10.2165/00002512-200219110-00004. [DOI] [PubMed] [Google Scholar]
- 40.Johansen KL. Testosterone metabolism and replacement therapy in patients with end-stage renal disease. Semin Dial. 2004;17:202–208. doi: 10.1111/j.0894-0959.2004.17307.x. [DOI] [PubMed] [Google Scholar]
- 41.Ohnishi S, Murakami T, Moriyama T, Mitamura K, Imawari M. Androgen and estrogen receptors in hepatocellular carcinoma and in the surrounding noncancerous liver tissue. Hepatology. 1986;6:440–443. doi: 10.1002/hep.1840060320. [DOI] [PubMed] [Google Scholar]
- 42.Saad F, Gooren L. The role of testosterone in the metabolic syndrome: a review. J Steroid Biochem Mol Biol. 2009;114:40–43. doi: 10.1016/j.jsbmb.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 43.Corona G, Mannucci E, Forti G, Maggi M. Following the common association between testosterone deficiency and diabetes mellitus, can testosterone be regarded as a new therapy for diabetes? Int J Androl. 2009;32:431–441. doi: 10.1111/j.1365-2605.2009.00965.x. [DOI] [PubMed] [Google Scholar]
- 44.Attard G, Cooper CS, de Bono JS. Steroid hormone receptors in prostate cancer: a hard habit to break? Cancer Cell. 2009;16:458–462. doi: 10.1016/j.ccr.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 45.Harkonen P, Torn S, Kurkela R, Porvari K, Pulkka A, Lindfors A, Isomaa V, Vihko P. Sex hormone metabolism in prostate cancer cells during transition to an androgen-independent state. J Clin Endocrinol Metab. 2003;88:705–712. doi: 10.1210/jc.2002-020236. [DOI] [PubMed] [Google Scholar]
- 46.Vihko P, Herrala A, Härkönen P, Isomaa V, Kaija H, Kurkela R, Pulkka A. Control of cell proliferation by steroids: the role of 17HSDs. Mol Cell Endocrinol. 2006;248:141–148. doi: 10.1016/j.mce.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 47.Soronen P, Laiti M, Törn S, Härkönen P, Patrikainen L, Li Y, Pulkka A, Kurkela R, Herrala A, Kaija H, et al. Sex steroid hormone metabolism and prostate cancer. J Steroid Biochem Mol Biol. 2004;92:281–286. doi: 10.1016/j.jsbmb.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 48.Pike CJ, Nguyen TV, Ramsden M, Yao M, Murphy MP, Rosario ER. Androgen cell signaling pathways involved in neuroprotective actions. Horm Behav. 2008;53:693–705. doi: 10.1016/j.yhbeh.2007.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pike CJ, Carroll JC, Rosario ER, Barron AM. Protective actions of sex steroid hormones in Alzheimer’s disease. Front Neuroendocrinol. 2009;30:239–258. doi: 10.1016/j.yfrne.2009.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pfaff DW, Vasudevan N, Kia HK, Zhu YS, Chan J, Garey J, Morgan M, Ogawa S. Estrogens, brain and behavior: studies in fundamental neurobiology and observations related to women’s health. J Steroid Biochem Mol Biol. 2000;74:365–373. doi: 10.1016/s0960-0760(00)00114-x. [DOI] [PubMed] [Google Scholar]
- 51.Imai Y, Kondoh S, Kouzmenko A, Kato S. Minireview: Osteoprotective Action of Estrogens Is Mediated by Osteoclastic Estrogen Receptor{alpha} Mol Endocrinol. 2009:Epub ahead of print. doi: 10.1210/me.2009-0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Canonico M, Fournier A, Carcaillon L, Olie V, Plu-Bureau G, Oger E, Mesrine S, Boutron-Ruault MC, Clavel-Chapelon F, Scarabin PY. Postmenopausal Hormone Therapy and Risk of Idiopathic Venous Thromboembolism. Results From the E3N Cohort Study. Arterioscler Thromb Vasc Biol. 2009:Epub ahead of print. doi: 10.1161/ATVBAHA.109.196022. [DOI] [PubMed] [Google Scholar]
- 53.Fournier A, Mesrine S, Boutron-Ruault MC, Clavel-Chapelon F. Estrogen-progestagen menopausal hormone therapy and breast cancer: does delay from menopause onset to treatment initiation influence risks? J Clin Oncol. 2009;27:5138–5143. doi: 10.1200/JCO.2008.21.6432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hayes TG. Pharmacologic treatment of male breast cancer. Expert Opin Pharmacother. 2009;10:2499–2510. doi: 10.1517/14656560903200634. [DOI] [PubMed] [Google Scholar]
- 55.Borer KT. Physical activity in the prevention and amelioration of osteoporosis in women : interaction of mechanical, hormonal and dietary factors. Sports Med. 2005;35:779–830. doi: 10.2165/00007256-200535090-00004. [DOI] [PubMed] [Google Scholar]
- 56.Nilsson S, Mäkelä S, Treuter E, Tujague M, Thomsen J, Andersson G, Enmark E, Pettersson K, Warner M, Gustafsson JA. Mechanisms of estrogen action. Physiol Rev. 2001;81:1535–1565. doi: 10.1152/physrev.2001.81.4.1535. [DOI] [PubMed] [Google Scholar]
- 57.Prossnitz ER, Oprea TI, Sklar LA, Arterburn JB. The ins and outs of GPR30: a transmembrane estrogen receptor. J Steroid Biochem Mol Biol. 2008;109:350–353. doi: 10.1016/j.jsbmb.2008.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Parsons SJ, Parsons JT. Src family kinases, key regulators of signal transduction. Oncogene. 2004;23:7906–7909. doi: 10.1038/sj.onc.1208160. [DOI] [PubMed] [Google Scholar]
- 59.Shupnik MA. Crosstalk between steroid receptors and the c-Src-receptor tyrosine kinase pathways: implications for cell proliferation. Oncogene. 2004;23:7979–7989. doi: 10.1038/sj.onc.1208076. [DOI] [PubMed] [Google Scholar]
- 60.Levin ER. Bidirectional signaling between the estrogen receptor and the epidermal growth factor receptor. Mol Endocrinol. 2003;17:309–317. doi: 10.1210/me.2002-0368. [DOI] [PubMed] [Google Scholar]
- 61.Tiidus PM. Influence of estrogen on skeletal muscle damage, inflammation, and repair. Exerc Sport Sci Rev. 2003;31:40–44. doi: 10.1097/00003677-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 62.Koh KK. Effects of estrogen on the vascular wall: vasomotor function and inflammation. Cardiovasc Res. 2002;55:714–726. doi: 10.1016/s0008-6363(02)00487-x. [DOI] [PubMed] [Google Scholar]
- 63.Merchenthaler I, Dellovade TL, Shughrue PJ. Neuroprotection by estrogen in animal models of global and focal ischemia. Ann N Y Acad Sci. 2003;1007:89–100. doi: 10.1196/annals.1286.009. [DOI] [PubMed] [Google Scholar]
- 64.Ikeda K, Inoue S. Estrogen receptors and their downstream targets in cancer. Arch Histol Cytol. 2004;67:435–442. doi: 10.1679/aohc.67.435. [DOI] [PubMed] [Google Scholar]
- 65.Bardin A, Boulle N, Lazennec G, Vignon F, Pujol P. Loss of ERbeta expression as a common step in estrogen-dependent tumor progression. Endocr Relat Cancer. 2004;11:537–551. doi: 10.1677/erc.1.00800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Invernizzi P, Alvaro D, Crosignani A, Gaudio E, Podda M. Tamoxifen in treatment of primary biliary cirrhosis. Hepatology. 2004;39:1175–1176. doi: 10.1002/hep.20164. [DOI] [PubMed] [Google Scholar]
- 67.Reddy A, Prince M, James OF, Jain S, Bassendine MF. Tamoxifen: a novel treatment for primary biliary cirrhosis? Liver Int. 2004;24:194–197. doi: 10.1111/j.1478-3231.2004.00920.x. [DOI] [PubMed] [Google Scholar]
- 68.Migliaccio A, Castoria G, Di Domenico M, de Falco A, Bilancio A, Lombardi M, Bottero D, Varricchio L, Nanayakkara M, Rotondi A, et al. Sex steroid hormones act as growth factors. J Steroid Biochem Mol Biol. 2002;83:31–35. doi: 10.1016/s0960-0760(02)00264-9. [DOI] [PubMed] [Google Scholar]
- 69.Wimalasena J, Meehan D, Dostal R, Foster JS, Cameron M, Smith M. Growth factors interact with estradiol and gonadotropins in the regulation of ovarian cancer cell growth and growth factor receptors. Oncol Res. 1993;5:325–337. [PubMed] [Google Scholar]
- 70.Francavilla A, Polimeno L, Barone M, Azzarone A, Starzl TE. Hepatic regeneration and growth factors. J Surg Oncol Suppl. 1993;3:1–7. doi: 10.1002/jso.2930530503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Giannitrapani L, Soresi M, La Spada E, Cervello M, D’Alessandro N, Montalto G. Sex hormones and risk of liver tumor. Ann N Y Acad Sci. 2006;1089:228–236. doi: 10.1196/annals.1386.044. [DOI] [PubMed] [Google Scholar]
- 72.Suzuki S, Brown CM, Wise PM. Mechanisms of neuroprotection by estrogen. Endocrine. 2006;29:209–215. doi: 10.1385/ENDO:29:2:209. [DOI] [PubMed] [Google Scholar]
- 73.De Maria N, Manno M, Villa E. Sex hormones and liver cancer. Mol Cell Endocrinol. 2002;193:59–63. doi: 10.1016/s0303-7207(02)00096-5. [DOI] [PubMed] [Google Scholar]
- 74.Tamoxifen for early breast cancer: an overview of the randomised trials. Early Breast Cancer Trialists’ Collaborative Group. Lancet. 1998;351:1451–1467. [PubMed] [Google Scholar]
- 75.Di Maio M, De Maio E, Morabito A, D’Aniello R, De Feo G, Gallo C, Perrone F. Hormonal treatment of human hepatocellular carcinoma. Ann N Y Acad Sci. 2006;1089:252–261. doi: 10.1196/annals.1386.007. [DOI] [PubMed] [Google Scholar]
- 76.Fisch B, Margara RA, Winston RM, Hillier SG. Cellular basis of luteal steroidogenesis in the human ovary. J Endocrinol. 1989;122:303–311. doi: 10.1677/joe.0.1220303. [DOI] [PubMed] [Google Scholar]
- 77.Lamont RF, Jayasooriya GS. Progestational agents for the prevention of preterm birth. J Perinat Med. 2009;37:12–14. doi: 10.1515/JPM.2009.029. [DOI] [PubMed] [Google Scholar]
- 78.Graham JD, Clarke CL. Physiological action of progesterone in target tissues. Endocr Rev. 1997;18:502–519. doi: 10.1210/edrv.18.4.0308. [DOI] [PubMed] [Google Scholar]
- 79.Spears N, Murray AA, Allison V, Boland NI, Gosden RG. Role of gonadotrophins and ovarian steroids in the development of mouse follicles in vitro. J Reprod Fertil. 1998;113:19–26. doi: 10.1530/jrf.0.1130019. [DOI] [PubMed] [Google Scholar]
- 80.Bartlewski PM, Beard AP, Rawlings NC. Ultrasonographic study of the effects of the corpus luteum on antral follicular development in unilaterally ovulating western white-faced ewes. Anim Reprod Sci. 2001;65:231–244. doi: 10.1016/s0378-4320(00)00229-3. [DOI] [PubMed] [Google Scholar]
- 81.Rodway MR, Swan CL, Gillio-Meina C, Crellin NK, Flood PF, Chedrese PJ. Regulation of steroidogenesis in jc-410, a stable cell line of porcine granulosa origin. Mol Cell Endocrinol. 1999;148:87–94. doi: 10.1016/s0303-7207(98)00233-0. [DOI] [PubMed] [Google Scholar]
- 82.Rodway MR, Swan CL, Crellin NK, Gillio-Meina C, Chedrese PJ. Steroid regulation of progesterone synthesis in a stable porcine granulosa cell line: a role for progestins. J Steroid Biochem Mol Biol. 1999;68:173–180. doi: 10.1016/s0960-0760(99)00028-x. [DOI] [PubMed] [Google Scholar]
- 83.Swan CL, Agostini MC, Bartlewski PM, Feyles V, Urban RJ, Chedrese PJ. Effects of progestins on progesterone synthesis in a stable porcine granulosa cell line: control of transcriptional activity of the cytochrome p450 side-chain cleavage gene. Biol Reprod. 2002;66:959–965. doi: 10.1095/biolreprod66.4.959. [DOI] [PubMed] [Google Scholar]
- 84.Li X, Lonard DM, O’Malley BW. A contemporary understanding of progesterone receptor function. Mech Ageing Dev. 2004;125:669–678. doi: 10.1016/j.mad.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 85.Leonhardt SA, Boonyaratanakornkit V, Edwards DP. Progesterone receptor transcription and non-transcription signaling mechanisms. Steroids. 2003;68:761–770. doi: 10.1016/s0039-128x(03)00129-6. [DOI] [PubMed] [Google Scholar]
- 86.Edwards DP. Regulation of signal transduction pathways by estrogen and progesterone. Annu Rev Physiol. 2005;67:335–376. doi: 10.1146/annurev.physiol.67.040403.120151. [DOI] [PubMed] [Google Scholar]
- 87.Richer JK, Jacobsen BM, Manning NG, Abel MG, Wolf DM, Horwitz KB. Differential gene regulation by the two progesterone receptor isoforms in human breast cancer cells. J Biol Chem. 2002;277:5209–5218. doi: 10.1074/jbc.M110090200. [DOI] [PubMed] [Google Scholar]
- 88.Wasserman WJ, Pinto LH, O’Connor CM, Smith LD. Progesterone induces a rapid increase in [Ca2+]in of Xenopus laevis oocytes. Proc Natl Acad Sci USA. 1980;77:1534–1536. doi: 10.1073/pnas.77.3.1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hu Z, Li Y, Fang M, Wai MS, Yew DT. Exogenous progesterone: a potential therapeutic candidate in CNS injury and neurodegeneration. Curr Med Chem. 2009;16:1418–1425. doi: 10.2174/092986709787846523. [DOI] [PubMed] [Google Scholar]
- 90.Spitz IM. Progesterone antagonists and progesterone receptor modulators: an overview. Steroids. 2003;68:981–993. doi: 10.1016/j.steroids.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 91.Chabbert-Buffet N, Meduri G, Bouchard P, Spitz IM. Selective progesterone receptor modulators and progesterone antagonists: mechanisms of action and clinical applications. Hum Reprod Update. 2005;11:293–307. doi: 10.1093/humupd/dmi002. [DOI] [PubMed] [Google Scholar]
- 92.Junaidi A, Williamson PE, Martin GB, Stanton PG, Blackberry MA, Cummins JM, Trigg TE. Pituitary and testicular endocrine responses to exogenous gonadotrophin-releasing hormone (GnRH) and luteinising hormone in male dogs treated with GnRH agonist implants. Reprod Fertil Dev. 2007;19:891–898. doi: 10.1071/rd07088. [DOI] [PubMed] [Google Scholar]
- 93.Ciccone NA, Kaiser UB. The biology of gonadotroph regulation. Curr Opin Endocrinol Diabetes Obes. 2009;16:321–327. doi: 10.1097/MED.0b013e32832d88fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chen FC, Oskay-Ozcelik G, Bühling KJ, Köpstein U, Mentze M, Lichtenegger W, Sehouli J. Prognostic value of serum and ascites levels of estradiol, FSH, LH and prolactin in ovarian cancer. Anticancer Res. 2009;29:1575–1578. [PubMed] [Google Scholar]
- 95.Choi JH, Wong AS, Huang HF, Leung PC. Gonadotropins and ovarian cancer. Endocr Rev. 2007;28:440–461. doi: 10.1210/er.2006-0036. [DOI] [PubMed] [Google Scholar]
- 96.Parrott JA, Doraiswamy V, Kim G, Mosher R, Skinner MK. Expression and actions of both the follicle stimulating hormone receptor and the luteinizing hormone receptor in normal ovarian surface epithelium and ovarian cancer. Mol Cell Endocrinol. 2001;172:213–222. doi: 10.1016/s0303-7207(00)00340-3. [DOI] [PubMed] [Google Scholar]
- 97.Voogt JL. Control of hormone release during lactation. Clin Obstet Gynaecol. 1978;5:435–455. [PubMed] [Google Scholar]
- 98.Bachelot A, Binart N. Reproductive role of prolactin. Reproduction. 2007;133:361–369. doi: 10.1530/REP-06-0299. [DOI] [PubMed] [Google Scholar]
- 99.Harris J, Stanford PM, Oakes SR, Ormandy CJ. Prolactin and the prolactin receptor: new targets of an old hormone. Ann Med. 2004;36:414–425. doi: 10.1080/07853890410033892. [DOI] [PubMed] [Google Scholar]
- 100.Graichen R, Sandstedt J, Goh EL, Isaksson OG, Törnell J, Lobie PE. The growth hormone-binding protein is a location-dependent cytokine receptor transcriptional enhancer. J Biol Chem. 2003;278:6346–3654. doi: 10.1074/jbc.M207546200. [DOI] [PubMed] [Google Scholar]
- 101.Clevenger CV, Gadd SL, Zheng J. New mechanisms for PRLr action in breast cancer. Trends Endocrinol Metab. 2009;20:223–229. doi: 10.1016/j.tem.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 102.Hankinson SE, Willett WC, Michaud DS, Manson JE, Colditz GA, Longcope C, Rosner B, Speizer FE. Plasma prolactin levels and subsequent risk of breast cancer in postmenopausal women. J Natl Cancer Inst. 1999;91:629–634. doi: 10.1093/jnci/91.7.629. [DOI] [PubMed] [Google Scholar]
- 103.Harvey PW, Everett DJ. Significance of the detection of esters of p-hydroxybenzoic acid (parabens) in human breast tumours. J Appl Toxicol. 2004;24:1–4. doi: 10.1002/jat.957. [DOI] [PubMed] [Google Scholar]
- 104.Harvey PW. Human relevance of rodent prolactin-induced non-genotoxic mammary carcinogenesis: prolactin involvement in human breast cancer and significance for toxicology risk assessments. J Appl Toxicol. 2005;25:179–183. doi: 10.1002/jat.1063. [DOI] [PubMed] [Google Scholar]
- 105.Harvey PW, Everett DJ, Springall CJ. Adverse effects of prolactin in rodents and humans: breast and prostate cancer. J Psychopharmacol. 2008;22:20–27. doi: 10.1177/0269881107082624. [DOI] [PubMed] [Google Scholar]
- 106.Chapman AB. Cystic disease in women: clinical characteristics and medical management. Adv Ren Replace Ther. 2003;10:24–30. doi: 10.1053/jarr.2003.50005. [DOI] [PubMed] [Google Scholar]
- 107.Myers RP, Shaheen AA, Fong A, Burak KW, Wan A, Swain MG, Hilsden RJ, Sutherland L, Quan H. Epidemiology and natural history of primary biliary cirrhosis in a Canadian health region: a population-based study. Hepatology. 2009;50:1884–1892. doi: 10.1002/hep.23210. [DOI] [PubMed] [Google Scholar]
- 108.Parkin DR, Malejka-Giganti D. Differences in the hepatic P450-dependent metabolism of estrogen and tamoxifen in response to treatment of rats with 3,3'-diindolylmethane and its parent compound indole-3-carbinol. Cancer Detect Prev. 2004;28:72–79. doi: 10.1016/j.cdp.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 109.Jordan VC. Molecular mechanisms of antiestrogen action in breast cancer. Breast Cancer Res Treat. 1994;31:41–52. doi: 10.1007/BF00689675. [DOI] [PubMed] [Google Scholar]
- 110.Pan G, Vickers SM, Pickens A, Phillips JO, Ying W, Thompson JA, Siegal GP, McDonald JM. Apoptosis and tumorigenesis in human cholangiocarcinoma cells. Involvement of Fas/APO-1 (CD95) and calmodulin. Am J Pathol. 1999;155:193–203. doi: 10.1016/S0002-9440(10)65113-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yano H, Fukuda K, Haramaki M, Momosaki S, Ogasawara S, Higaki K, Kojiro M. Expression of Fas and anti-Fas-mediated apoptosis in human hepatocellular carcinoma cell lines. J Hepatol. 1996;25:454–464. doi: 10.1016/s0168-8278(96)80204-2. [DOI] [PubMed] [Google Scholar]
- 112.Alvaro D, Metalli VD, Alpini G, Onori P, Franchitto A, Barbaro B, Glaser SS, Francis H, Cantafora A, Blotta I, et al. The intrahepatic biliary epithelium is a target of the growth hormone/insulin-like growth factor 1 axis. J Hepatol. 2005;43:875–883. doi: 10.1016/j.jhep.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 113.Tremblay A, Giguere V. Contribution of steroid receptor coactivator-1 and CREB binding protein in ligand-independent activity of estrogen receptor beta. J Steroid Biochem Mol Biol. 2001;77:19–27. doi: 10.1016/s0960-0760(01)00031-0. [DOI] [PubMed] [Google Scholar]
- 114.Peyssonnaux C, Eychene A. The Raf/MEK/ERK pathway: new concepts of activation. Biol Cell. 2001;93:53–62. doi: 10.1016/s0248-4900(01)01125-x. [DOI] [PubMed] [Google Scholar]
- 115.Alvaro D, Onori P, Alpini G, Franchitto A, Jefferson DM, Torrice A, Cardinale V, Stefanelli F, Mancino MG, Strazzabosco M, et al. Morphological and functional features of hepatic cyst epithelium in autosomal dominant polycystic kidney disease. Am J Pathol. 2008;172:321–332. doi: 10.2353/ajpath.2008.070293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Alvaro D, Barbaro B, Franchitto A, Onori P, Glaser SS, Alpini G, Francis H, Marucci L, Sterpetti P, Ginanni-Corradini S, et al. Estrogens and insulin-like growth factor 1 modulate neoplastic cell growth in human cholangiocarcinoma. Am J Pathol. 2006;169:877–888. doi: 10.2353/ajpath.2006.050464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kaplan MM, Gershwin ME. Primary biliary cirrhosis. N Engl J Med. 2005;353:1261–1273. doi: 10.1056/NEJMra043898. [DOI] [PubMed] [Google Scholar]
- 118.Floreani A, Paternoster D, Mega A, Farinati F, Plebani M, Baldo V, Grella P. Sex hormone profile and endometrial cancer risk in primary biliary cirrhosis: a case-control study. Eur J Obstet Gynecol Reprod Biol. 2002;103:154–157. doi: 10.1016/s0301-2115(02)00046-5. [DOI] [PubMed] [Google Scholar]
- 119.Chen J, Robertson G, Field J, Liddle C, Farrell GC. Effects of bile duct ligation on hepatic expression of female-specific CYP2C12 in male and female rats. Hepatology. 1998;28:624–630. doi: 10.1002/hep.510280304. [DOI] [PubMed] [Google Scholar]
- 120.Lööf L, Adami HO, Sparén P, Danielsson A, Eriksson LS, Hultcrantz R, Lindgren S, Olsson R, Prytz H, Ryden BO. Cancer risk in primary biliary cirrhosis: a population-based study from Sweden. Hepatology. 1994;20:101–104. [PubMed] [Google Scholar]
- 121.Everson GT. Hepatic cysts in autosomal dominant polycystic kidney disease. Mayo Clin Proc. 1990;65:1020–1025. doi: 10.1016/s0025-6196(12)65165-9. [DOI] [PubMed] [Google Scholar]
- 122.Gabow PA, Johnson AM, Kaehny WD, Manco-Johnson ML, Duley IT, Everson GT. Risk factors for the development of hepatic cysts in autosomal dominant polycystic kidney disease. Hepatology. 1990;11:1033–1037. doi: 10.1002/hep.1840110619. [DOI] [PubMed] [Google Scholar]
- 123.Stellon AJ, Williams R. Increased incidence of menstrual abnormalities and hysterectomy preceding primary biliary cirrhosis. Br Med J (Clin Res Ed) 1986;293:297–298. doi: 10.1136/bmj.293.6542.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Blechacz B, Gores GJ. Cholangiocarcinoma: advances in pathogenesis, diagnosis, and treatment. Hepatology. 2008;48:308–321. doi: 10.1002/hep.22310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Patel T. Cholangiocarcinoma. Nat Clin Pract Gastroenterol Hepatol. 2006;3:33–42. doi: 10.1038/ncpgasthep0389. [DOI] [PubMed] [Google Scholar]
- 126.Kahlert S, Nuedling S, van Eickels M, Vetter H, Meyer R, Grohe C. Estrogen receptor alpha rapidly activates the IGF-1 receptor pathway. J Biol Chem. 2000;275:18447–18453. doi: 10.1074/jbc.M910345199. [DOI] [PubMed] [Google Scholar]
- 127.Cardona-Gomez GP, Mendez P, DonCarlos LL, Azcoitia I, Garcia-Segura LM. Interactions of estrogens and insulin-like growth factor-I in the brain: implications for neuroprotection. Brain Res Brain Res Rev. 2001;37:320–334. doi: 10.1016/s0165-0173(01)00137-0. [DOI] [PubMed] [Google Scholar]
- 128.J Venter SG, C Wise, H Francis, B Vaculin, S Kopriva, J Savage, and G Alpini. Castration reduces cholangiocyte hyperplasia and secretin-stimulated ductal secretion of bile duct ligated (BDL) rats by downregulation of the cAMP-dependent ERK1/2 pathway. Gastroenterology. 2008;134:A777. [Google Scholar]
- 129.Kopera H. Side effects of anabolic steroids and contraindications. Wien Med Wochenschr. 1993;143:399–400. [PubMed] [Google Scholar]
- 130.Nakao A, Sakagami K, Nakata Y, Komazawa K, Amimoto T, Nakashima K, Isozaki H, Takakura N, Tanaka N. Multiple hepatic adenomas caused by long-term administration of androgenic steroids for aplastic anemia in association with familial adenomatous polyposis. J Gastroenterol. 2000;35:557–562. doi: 10.1007/s005350070081. [DOI] [PubMed] [Google Scholar]
- 131.Minami Y, Kudo M, Kawasaki T, Chung H, Matsui S, Kitano M, Suetomi Y, Onda H, Funai S, Kou K, et al. Intrahepatic huge hematoma due to rupture of small hepatocellular adenoma: a case report. Hepatol Res. 2002;23:145–151. doi: 10.1016/s1386-6346(01)00164-4. [DOI] [PubMed] [Google Scholar]
- 132.Stimac D, Milić S, Dintinjana RD, Kovac D, Ristić S. Androgenic/Anabolic steroid-induced toxic hepatitis. J Clin Gastroenterol. 2002;35:350–352. doi: 10.1097/00004836-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 133.Socas L, Zumbado M, Pérez-Luzardo O, Ramos A, Pérez C, Hernández JR, Boada LD. Hepatocellular adenomas associated with anabolic androgenic steroid abuse in bodybuilders: a report of two cases and a review of the literature. Br J Sports Med. 2005;39:e27. doi: 10.1136/bjsm.2004.013599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lee HY, Sherwood OD. The effects of blocking the actions of estrogen and progesterone on the rates of proliferation and apoptosis of cervical epithelial and stromal cells during the second half of pregnancy in rats. Biol Reprod. 2005;73:790–797. doi: 10.1095/biolreprod.105.043984. [DOI] [PubMed] [Google Scholar]
- 135.Greenwald GS, Wang MW. A monoclonal antibody to progesterone interrupts pregnancy in the hamster by curtailing secretion of the luteotropic complex of prolactin and follicle-stimulating hormone. Endocrinology. 1991;129:1735–1743. doi: 10.1210/endo-129-4-1735. [DOI] [PubMed] [Google Scholar]
- 136.Glaser S, DeMorrow S, Francis H, Ueno Y, Gaudio E, Vaculin S, Venter J, Franchitto A, Onori P, Vaculin B, et al. Progesterone stimulates the proliferation of female and male cholangiocytes via autocrine/paracrine mechanisms. Am J Physiol Gastrointest Liver Physiol. 2008;295:G124–G136. doi: 10.1152/ajpgi.00536.2007. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 137.Meng LJ, Reyes H, Axelson M, Palma J, Hernandez I, Ribalta J, Sjövall J. Progesterone metabolites and bile acids in serum of patients with intrahepatic cholestasis of pregnancy: effect of ursodeoxycholic acid therapy. Hepatology. 1997;26:1573–1579. doi: 10.1002/hep.510260627. [DOI] [PubMed] [Google Scholar]
- 138.Reyes H, Sjövall J. Bile acids and progesterone metabolites in intrahepatic cholestasis of pregnancy. Ann Med. 2000;32:94–106. doi: 10.3109/07853890009011758. [DOI] [PubMed] [Google Scholar]
- 139.Meng LJ, Reyes H, Palma J, Hernandez I, Ribalta J, Sjovall J. Effects of ursodeoxycholic acid on conjugated bile acids and progesterone metabolites in serum and urine of patients with intrahepatic cholestasis of pregnancy. J Hepatol. 1997;27:1029–1040. doi: 10.1016/s0168-8278(97)80147-x. [DOI] [PubMed] [Google Scholar]
- 140.Wang YJ, Wu JC, Lee SD, Tsai YT, Lo KJ. Gonadal dysfunction and changes in sex hormones in postnecrotic cirrhotic men: a matched study with alcoholic cirrhotic men. Hepatogastroenterology. 1991;38:531–534. [PubMed] [Google Scholar]
- 141.Gonzales PH, Rhoden CR, Luz C, Corrêa G, Barbosa-Coutinho LM, Oliveira MC. Male gonadal function, prolactin secretion and lactotroph population in an experimental model of cirrhosis. Braz J Med Biol Res. 2007;40:1383–1388. doi: 10.1590/s0100-879x2006005000150. [DOI] [PubMed] [Google Scholar]
- 142.Bell H, Raknerud N, Falch JA, Haug E. Inappropriately low levels of gonadotrophins in amenorrhoeic women with alcoholic and non-alcoholic cirrhosis. Eur J Endocrinol. 1995;132:444–449. doi: 10.1530/eje.0.1320444. [DOI] [PubMed] [Google Scholar]
- 143.LaPolt PS, Tilly JL, Aihara T, Nishimori K, Hsueh AJ. Gonadotropin-induced up- and down-regulation of ovarian follicle-stimulating hormone (FSH) receptor gene expression in immature rats: effects of pregnant mare's serum gonadotropin, human chorionic gonadotropin, and recombinant FSH. Endocrinology. 1992;130:1289–1295. doi: 10.1210/endo.130.3.1537292. [DOI] [PubMed] [Google Scholar]
- 144.Tilly JL, LaPolt PS, Hsueh AJ. Hormonal regulation of follicle-stimulating hormone receptor messenger ribonucleic acid levels in cultured rat granulosa cells. Endocrinology. 1992;130:1296–1302. doi: 10.1210/endo.130.3.1311235. [DOI] [PubMed] [Google Scholar]
- 145.Mancinelli R, Onori P, Gaudio E, DeMorrow S, Franchitto A, Francis H, Glaser S, Carpino G, Venter J, Alvaro D, et al. Follicle-stimulating hormone increases cholangiocyte proliferation by an autocrine mechanism via cAMP-dependent phosphorylation of ERK1/2 and Elk-1. Am J Physiol Gastrointest Liver Physiol. 2009;297:G11–G26. doi: 10.1152/ajpgi.00025.2009. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 146.Kiani S, Valizadeh B, Hormazdi B, Samadi H, Najafi T, Samini M, Dehpour AR. Alteration in male reproductive system in experimental cholestasis: roles for opioids and nitric oxide overproduction. Eur J Pharmacol. 2009;615:246–251. doi: 10.1016/j.ejphar.2009.04.049. [DOI] [PubMed] [Google Scholar]
- 147.Barnes MJ, Lapanowski K, Rafols JA, Lawson DM, Dunbar JC. Chronic nitric oxide deficiency is associated with altered leutinizing hormone and follicle-stimulating hormone release in ovariectomized rats. Exp Biol Med (Maywood) 2002;227:817–822. doi: 10.1177/153537020222700915. [DOI] [PubMed] [Google Scholar]
- 148.Moretto M, López FJ, Negro-Vilar A. Nitric oxide regulates luteinizing hormone-releasing hormone secretion. Endocrinology. 1993;133:2399–2402. doi: 10.1210/endo.133.5.8104781. [DOI] [PubMed] [Google Scholar]
- 149.Ouhtit A, Ronsin B, Kelly PA, Morel G. Ultrastructural expression of prolactin receptor in rat liver. Biol Cell. 1994;82:169–176. doi: 10.1016/s0248-4900(94)80019-7. [DOI] [PubMed] [Google Scholar]
- 150.Zenkova TY, Kulikov AV, Bogorad RL, Rozenkrants AA, Platonova LV, Shono NI, Gal'perin EI, Smirnova OV. Expression of prolactin receptors in human liver during cholestasis of different etiology and secondary liver cancer. Bull Exp Biol Med. 2003;135:566–569. doi: 10.1023/a:1025429318932. [DOI] [PubMed] [Google Scholar]
- 151.Bogorad RL, Ostroukhova TY, Orlova AN, Rubtsov PM, Smirnova OV. Long isoform of prolactin receptor predominates in rat intrahepatic bile ducts and further increases under obstructive cholestasis. J Endocrinol. 2006;188:345–354. doi: 10.1677/joe.1.06468. [DOI] [PubMed] [Google Scholar]
- 152.Taffetani S, Glaser S, Francis H, DeMorrow S, Ueno Y, Alvaro D, Marucci L, Marzioni M, Fava G, Venter J, et al. Prolactin stimulates the proliferation of normal female cholangiocytes by differential regulation of Ca2+-dependent PKC isoforms. BMC Physiol. 2007;7:6. doi: 10.1186/1472-6793-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Bélanger C, Luu-The V, Dupont P, Tchernof A. Adipose tissue intracrinology: potential importance of local androgen/estrogen metabolism in the regulation of adiposity. Horm Metab Res. 2002;34:737–745. doi: 10.1055/s-2002-38265. [DOI] [PubMed] [Google Scholar]
- 154.Bleau G, Roberts KD, Chapdelaine A. The in vitro and in vivo uptake and metabolism of steroids in human adipose tissue. J Clin Endocrinol Metab. 1974;39:236–246. doi: 10.1210/jcem-39-2-236. [DOI] [PubMed] [Google Scholar]
- 155.Dieudonné MN, Leneveu MC, Giudicelli Y, Pecquery R. Evidence for functional estrogen receptors alpha and beta in human adipose cells: regional specificities and regulation by estrogens. Am J Physiol Cell Physiol. 2004;286:C655–C661. doi: 10.1152/ajpcell.00321.2003. [DOI] [PubMed] [Google Scholar]
- 156.Pedersen SB, Bruun JM, Hube F, Kristensen K, Hauner H, Richelsen B. Demonstration of estrogen receptor subtypes alpha and beta in human adipose tissue: influences of adipose cell differentiation and fat depot localization. Mol Cell Endocrinol. 2001;182:27–37. doi: 10.1016/s0303-7207(01)00557-3. [DOI] [PubMed] [Google Scholar]
- 157.Bray GA. The underlying basis for obesity: relationship to cancer. J Nutr. 2002;132:3451S–3455S. doi: 10.1093/jn/132.11.3451S. [DOI] [PubMed] [Google Scholar]
- 158.Maggiolini M, Bonofiglio D, Marsico S, Panno ML, Cenni B, Picard D, Andò S. Estrogen receptor alpha mediates the proliferative but not the cytotoxic dose-dependent effects of two major phytoestrogens on human breast cancer cells. Mol Pharmacol. 2001;60:595–602. [PubMed] [Google Scholar]
- 159.Onori P, Alvaro D, Floreani AR, Mancino MG, Franchitto A, Guido M, Carpino G, De Santis A, Angelico M, Attili AF, et al. Activation of the IGF1 system characterizes cholangiocyte survival during progression of primary biliary cirrhosis. J Histochem Cytochem. 2007;55:327–334. doi: 10.1369/jhc.6R7125.2006. [DOI] [PubMed] [Google Scholar]