Abstract
Background and Objectives
Patients with renal dysfunction (RD) experience worse prognosis after myocardial infarction (MI). The aim of the present study was to investigate the impact of admission estimated glomerular filtration rate (eGFR) on clinical outcomes of patients undergoing primary percutaneous coronary intervention (PCI) for ST-segment elevation MI (STEMI).
Subjects and Methods
We retrospectively evaluated 4,542 eligible patients from the Korea Acute Myocardial Infarction Registry (KAMIR). Patients were divided into three groups according to eGFR (mL/min/1.73 m2): normal renal function (RF) group (eGFR ≥60, n=3,515), moderate RD group (eGFR between 30 to 59, n=894) and severe RD group (eGFR <30, n=133). Baseline characteristics, angiographic and procedural results, and in-hospital outcomes between the three groups were compared.
Results
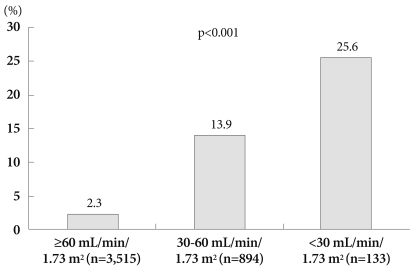
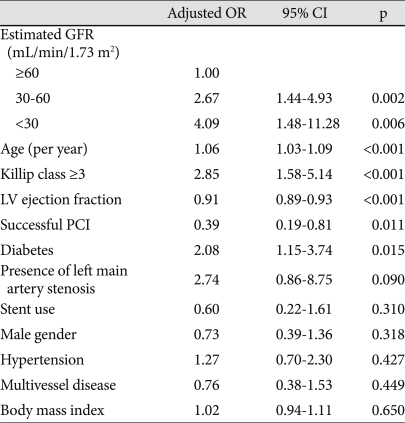
Age, gender, Killip class ≥3, hypertension, diabetes, congestive heart failure, peak creatine kinase-MB, high sensitivity C-reactive protein, B-type natriuretic peptide, left ventricle ejection fraction, multivessel disease, infarct-related artery and rate of successful PCI were significantly different between the 3 groups (p<0.05). With decline in RF, in-hospital complications developed with an increasing frequency (14.1% vs. 31.8% vs. 45.5%, p<0.0001). In-hospital mortality rate was significantly higher in the moderate and severe RD groups as compared to the normal RF group (2.3% vs. 13.9% vs. 25.6%, p<0.0001). Using multivariate logistic regression analysis, adjusted odds ratio for in-hospital mortality was 2.67 {95% confidence interval (CI) 1.44-4.93, p=0.002} in the moderate RD group, and 4.09 (95% CI 1.48-11.28, p=0.006) in the severe RD group as compared to the normal RF group.
Conclusion
Decreased admission eGFR was associated with worse clinical courses and it was an independent predictor of in-hospital mortality in STEMI patients undergoing primary PCI.
Keywords: Glomerular filtration rate, Acute myocardial infarction, Mortality, Percutaneous coronary intervention
Introduction
Renal dysfunction is a strong risk factor for cardiovascular disease in the general population,1) and it is associated with an increased risk of death and cardiovascular events in patients with a broad range of cardiovascular diseases, including heart failure,2) stable coronary artery disease undergoing percutaneous coronary intervention (PCI)3),4) and acute coronary syndromes.5),6)
In the setting of acute myocardial infarction (AMI), mortality risk is increased in patients with renal dysfunction (RD) of any degree of severity.7-9) Primary PCI is the best reperfusion strategy for AMI patients and its mortality benefit has been shown in randomized trials.10-12) However, most of these trials frequently excluded patients with RD, and few studies examining the outcomes of AMI patients with RD undergoing primary PCI have been reported.
To date, several studies evaluating the in-hospital prognostic significance of RD in patients undergoing primary PCI for AMI have reported that RD is an independent predictor of in-hospital mortality,13-15) even in the case of a successful PCI.13),14) However, one of these studies13) used serum creatinine level to determine RD despite the fact that serum creatinine level can be unreliable as an estimate of renal function (RF), while the other studies14),15) included a small number of patients and divided patients according to their RF into merely 2 groups which is insufficient for RD risk stratification. The aim of the present study was to investigate the impact of admission estimated glomerular filtration rate (GFR) on in-hospital outcomes in patients with ST-segment elevation myocardial infarction (STEMI) undergoing primary PCI using data from the Korea Acute Myocardial Infarction Registry (KAMIR).
Subjects and Methods
Korea Acute Myocardial Infarction Registry
KAMIR is a Korean prospective multicenter online registry designed to reflect "real-world" practice trends for patients presenting with AMI in the recent reperfusion era; the registry has been supported by the Korean Circulation Society since November 2005. Online registry of AMI cases (www.kamir.or.kr) has been performed at 41 universities or community hospitals that are high-volume centers with facilities for primary PCI and onsite cardiac surgery. Data were collected at each site by a trained study coordinator using a standardized case report form, and registered and submitted from individual institutions via password-protected internet-based electronic case report forms. The study protocol was approved by the ethics committee at each participating institution.
Study population
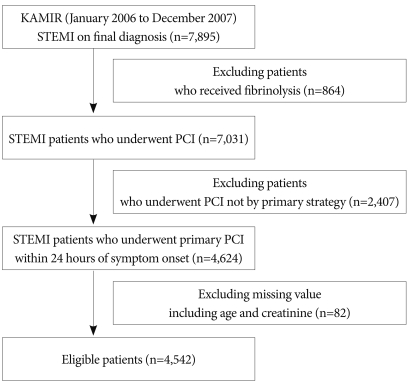
From January 2006 to December 2007, a total of 7,895 STEMI patients were registered in KAMIR. Of these, 864 patients were excluded from this study because they had received fibrinolytic therapy and 2,407 patients were excluded because they did not undergo PCI as the primary treatment strategy; an additional 82 patients were excluded due to missing data needed to calculate estimated GFR. The remaining 4,542 patients were eligible for the present study (Fig. 1). Data on clinical, angiographic and in-hospital outcomes were collected.
Fig. 1.
Study flow chart. STEMI: ST-segment elevation myocardial infarction, KAMIR: Korea Acute Myocardial Infarction Registry, PCI: percutaneous coronary intervention.
The mean age of the study patients was 62.2±12.8 years, and 3,355 (73.8%) patients were males. The mean estimated GFR was 78.3 mL/min/1.73 m2. The angiographic success rate was 91.8%, and the overall in-hospital mortality rate was 5.3%.
Definitions
STEMI was defined by the presence of new ST-segment elevation of at least 1 mm (0.1 mV) in 2 contiguous leads or new left bundle-branch block on the index or subsequent electrocardiogram with at least 1 positive cardiac biochemical marker of necrosis. Presence of left main coronary artery stenosis was defined as a luminal stenosis ≥50%. Primary PCI was defined as percutaneous coronary revascularization within 24 hours of symptom onset without antecedent treatment with a fibrinolytic agent as the initial therapy. Successful PCI was defined as thrombolysis in myocardial infarction 3 flow with residual stenosis ≤50% in the infarct-related artery. Major bleeding was defined as intracranial bleeding, bleeding associated with the need for blood transfusion, or any other clinically relevant bleeding as judged by the investigator.
Assessment of renal function
RF was defined by estimated GFR, which was calculated by the Modification of Diet in Renal Disease equation (MDRD)16) from the serum creatinine level measured on admission. The patients were classified into 3 groups according to the estimated GFR. Normal RF, moderate and severe RD were defined as estimated GFR ≥60 mL/min/1.73 m2, between 30 to 59 mL/min/1.73 m2 and <30 mL/min/1.73 m2, respectively.
Statistical analysis
All analyses were performed using Statistical Package for the Social Sciences (SPSS) software version 17.0 (SPSS Inc, Chicago, IL, USA). Data are presented as mean±standard deviation or median with interquartiles for continuous variables, and as frequency for categorical variables. Comparisons between continuous variables were done using one-way analysis of variance or the Kruskal-Wallis test, while the Pearson's chi-square test was used for categorical variables. Logistic regression analyses were performed to determine predictors of in-hospital mortality. A probability value of p<0.05 was considered significant.
Results
Baseline clinical characteristics
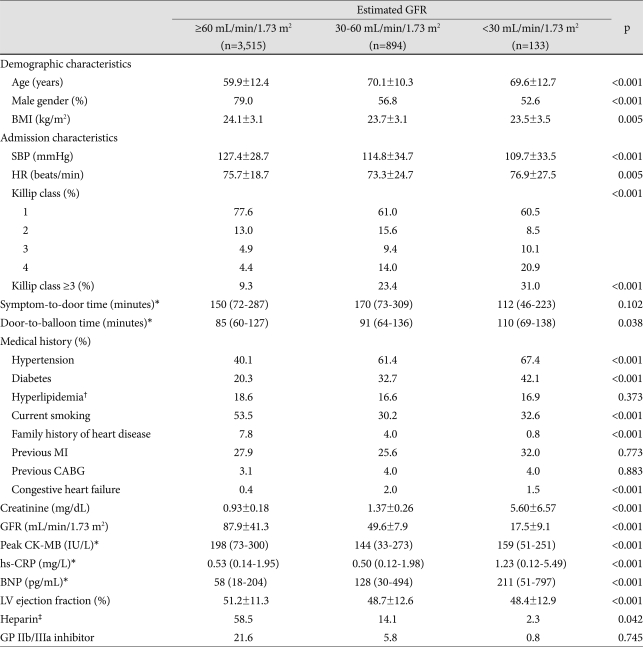
A total 1,027 (22.6%) patients had at least moderate RD. Patients with RD were older, were more often females and had lower BMI values. Also, they were more likely to have lower systolic blood pressure, increased heart rate and higher Killip class at presentation. Pre-hospital delay time was similar in the RD group and the normal RF group, but door-to-balloon time was longer in the RD group as compared to the normal RF group. On medical history, they were more likely to have hypertension, diabetes and congestive heart failure. With respect to laboratory findings, high sensitivity C-reactive protein and B-type natriuretic peptide levels were higher in the RD group, but peak creatine kinase-MB level and left ventricular ejection fraction were lower in the RD group as compared to the normal RF group. Use of both heparin and GP IIb/IIIa inhibitor was lower in the RD group as compared to the normal RF group (Table 1).
Table 1.
Baseline clinical characteristics
*Data are presented as the median with 25-75 percentiles, †Hyperlipidemia was defined as total cholesterol ≥220 mg/dL, ‡Heparin means low-molecular weight heparin or unfractionated heparin. GFR: glomerular filtration rate, BMI: body mass index, SBP: systolic blood pressure, HR: heart rate, PCI: percutaneous coronary intervention, MI: myocardial infarction, CABG: coronary artery bypass graft surgery, CK-MB: creatine kinase MB fraction, BNP: B-type natriuretic peptide, hs-CRP: high sensitivity C-reactive protein, GP: glycoprotein
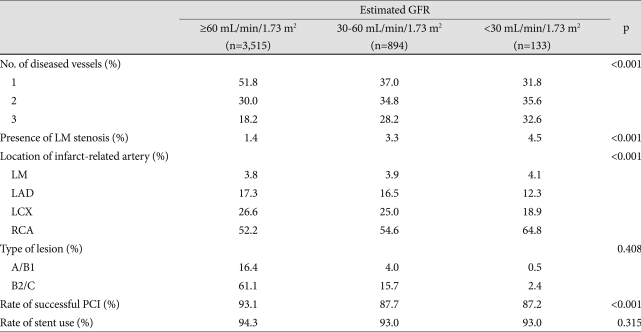
Angiographic and procedural characteristics
Patients with RD were more likely to have multivessel disease and left main coronary artery stenosis. The location of infarct-related artery was significantly different in the three groups, according to their RF. While involvement of the left anterior descending coronary artery was less frequent, involvement of the right coronary artery was more frequent in the severe RD group. Also, rate of successful PCI decreased significantly as RF declined; however, rate of stent insertion remained similar in all the three groups (Table 2).
Table 2.
Angiographic and procedural characteristics
LM: left main, LAD: left anterior descending, LCX: left circumflex, RCA: right coronary artery
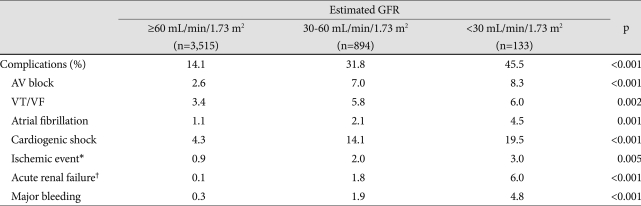
Clinical outcomes
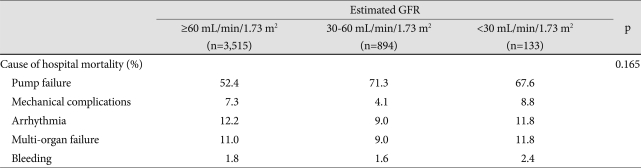
In-hospital complications, including arrhythmia, cardiogenic shock, ischemic events, acute renal failure and major bleeding, developed more frequently in patients with RD (Table 3). In-hospital mortality rates increased significantly as estimated GFR decreased (p<0.001), and approximately one-fourth of the patients (25.6%) in the severe RD group died (Fig. 2). Although the main cause of in-hospital mortality was pump failure (p<0.001), frequencies of the causes of mortality were not significantly different between the three groups (p=0.165) (Table 4). On multivariate logistic regression analysis, age, diabetes, Killip class ≥3, successful PCI and left ventricular ejection fraction were identified as independent predictors of in-hospital mortality. In addition, decreased estimated GFR was also identified as a powerful independent predictor of in-hospital mortality. When compared with the normal RF group, adjusted OR was 2.67 {95% confidence interval (CI): 1.44 to 4.93; p=0.002} in the moderate RD group and 4.09 (95% CI: 1.48 to 11.28; p=0.006) in the severe RD group (Table 5).
Table 3.
Incidence of in-hospital complications
*Ischemic event includes recurrent ischemia, re-infarction and cerebrovascular event, †Acute renal failure requiring renal replacement therapy. AV block: atrioventricular block, VT: ventricular tachycardia, VF: ventricular fibrillation
Fig. 2.
Incidence of in-hospital mortality according to the levels of estimated glomerular filtration rate.
Table 4.
Causes of in-hospital mortality
GFR: glomerular filtration rate
Table 5.
Multivariate logistic regression analysis of predictors of in-hospital mortality
OR: odds ratio, CI: confidence interval, GFR: glomerular filtration rate, LV: left ventricle, PCI: percutaneous coronary intervention
Discussion
The main finding of the present study is that RD defined by estimated GFR at admission is an independent predictor of in-hospital mortality in patients with STEMI undergoing primary PCI; this increased mortality risk was observed not only in the patients with severe RD but also in the patients with moderate RD.
In the present study, RD was defined by estimated GFR calculated using the MDRD equation, which is currently recommended in clinical practice,17) and patients were divided into three groups. Although RD, as defined by either serum creatinine level or estimated GFR, has been associated with increased mortality in patients with AMI,13-15),18),19),21) serum creatinine level is insensitive for an early detection of RD and could underestimate the incidence of moderate or severe RD concealed behind the near-normal creatinine levels,9),22),23) thereby underscoring the risk of RD in AMI patients. Furthermore, a graded risk of RD clearly exists, RF should be classified into at least 3 groups using estimated GFR for appropriate RD risk stratification in clinical practice. Our study on the basis of estimated GFR, showed that patients with moderate RD had a six-fold higher in-hospital mortality rate, while patients with severe RD had a eleven-fold higher in-hospital mortality rate as compared to the patients with normal RF. In our study, patients with RD were older, and were more often women. Although RF decreases with age and women tend to be older than men at the time of AMI presentation,24) it may also be an inherent influence of the variables used in the MDRD equation. In addition to older age and female gender, RD was more frequently associated with hypertension, diabetes, higher Killip class, multivessel disease and low left ventricular ejection fraction. These findings which have been described by other authors13),19),21) predispose to worse clinical outcomes after AMI. However, after adjustment for baseline differences, increased in-hospital mortality persisted in the patients with RD, suggesting that an increased mortality in patients with RD was not fully explained by these associated conditions, and that RD is a strong independent predictor of in-hospital mortality.
The rate of in-hospital complications was higher in the patients with RD as compared to the patients with normal RF. Cardiogenic shock, the most common cause of death in this study regardless of RF, developed with a three-fold higher frequency. It may be possible that the high incidence of unsuccessful PCI, recurrent ischemia or re-infarction and bleeding may potentiate the already existing weakened ischemic resistance reflected by high prevalence of diabetes and multivessel disease in the RD group. Also, acute renal failure developed more frequently in the RD group. After AMI, acute renal failure more commonly developed among those patients with low left ventricular ejection fraction, higher Killip class, anterior wall infarction, a hematocrit <30%, congestive heart failure, cardiogenic shock or stroke during admission.25) The RD group in our study shared many of these features, and although this study did not assess contrast-induced nephropathy (CIN) it may also contribute to it. Usually, the clinical benefit of primary PCI is accompanied by an increased risk of bleeding in AMI patients with RD, and a previous study has reported that RD is independently associated with bleeding after primary PCI.19) As expected, despite the less frequent use of heparin and glycoprotein IIb/IIIa inhibitors in the RD group as compared to the normal RF group, which have a proven efficacy in the setting of AMI, major bleeding increased significantly in the RD group as compared to the normal RF group.
Despite the fact that primary PCI is the most effective AMI treatment in terms of improvement in survival, this mortality benefit is attenuated in some patient subgroups, including the elderly, women, patients with renal insufficiency, heart failure, diabetes, anaemia, acute hyperglycemia, cardiogenic shock, and those developing CIN.15) Because the patients with RD frequently have more than one of these conditions, they might be at a very high risk of mortality after AMI. Therefore, management of AMI in patients with RD is particularly problematic. A recent study by Medi et al.26) which investigated the benefit of reperfusion strategies in STEMI patients in the presence of RD, reported that mortality rates remain high; they also found that primary PCI was associated with a lower adjusted in-hospital mortality than fibrinolytic therapy in the patients with normal RF and moderate RD. However, in the patients with severe RD, primary PCI was not associated with reduced mortality. In conclusion, we have limited knowledge on the optimal reperfusion strategy for the severe RD group.
To improve the survival in AMI patients with RD undergoing primary PCI, more aggressive treatment and meticulous care are needed. Firstly, the success of primary PCI has special importance because a successful PCI is an independent predictor of in-hospital mortality as shown in our study and RD was shown to be associated with the risk of unsuccessful PCI results. Secondly, medications such as aspirin, beta-blockers, and ACE inhibitors should be administered early after AMI, so that the patients with RD could gain a similar mortality benefit as their normal RF counterparts.27),28) Thirdly, reducing bleeding complications29) by using the radial artery approach and direct thrombin inhibitor during PCI is needed.30) Fourthly, an effort should be made to prevent CIN, including adequate hydration, reducing contrast use, use of low-osmolarity contrast and administration of N-acetylcysteine.19),20)
Because KAMIR is a large multicenter population-based prospectively-designed study including unselected patients with AMI, it provides comprehensive information on treatments and outcomes among patients with AMI and RD in the contemporary PCI era. Because this study included STEMI patients only, the median pre-hospital delay time in the RD group was relatively short as compared to that in the previous studies13),19); this feature could minimize the hemodynamic compromising effect of AMI on baseline serum creatinine level.
Limitations
The present study had several limitations. Firstly, we included only those individuals who underwent primary PCI. Similar to a previous study, because the patients with RD underwent PCI less often as compared to those with normal RF, there might be a selection bias and unidentified confounders, which might limit the generalizability of the data. Secondly, we did not collect information on medications relevant for prognostication, and therefore analyses in this study was not controlled for the impact of these drugs. Thirdly, there are inherent limitations of the estimated GFR calculation.17)
Conclusions
Decreased estimated GFR on admission is a strong risk factor for increased in-hospital complications and mortality in STEMI patients undergoing primary PCI. These risks increased in a stepwise fashion according to the degree of decreased estimated GFR. Clinicians should be alert to the increased mortality in patients with RD and make all the attempts to reduce complications of primary PCI and stress intensive medical management of these high-risk patients.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 2.Schiffrin EL, Lipman ML, Mann JF. Chronic kidney disease: effects on the cardiovascular system. Circulation. 2007;116:85–97. doi: 10.1161/CIRCULATIONAHA.106.678342. [DOI] [PubMed] [Google Scholar]
- 3.Best PJ, Lennon R, Ting HH, et al. The impact of renal insufficiency on clinical outcomes in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol. 2002;39:1113–1119. doi: 10.1016/s0735-1097(02)01745-x. [DOI] [PubMed] [Google Scholar]
- 4.Pinkau T, Mann JF, Ndrepepa G, et al. Coronary revascularization in patients with renal insufficiency: restenosis rate and cardiovascular outcomes. Am J Kidney Dis. 2004;44:627–635. [PubMed] [Google Scholar]
- 5.Al Suwaidi J, Reddan DN, Williams K, et al. Prognostic implications of abnormalities in renal function in patients with acute coronary syndromes. Circulation. 2002;106:974–980. doi: 10.1161/01.cir.0000027560.41358.b3. [DOI] [PubMed] [Google Scholar]
- 6.Mielniczuk LM, Pfeffer MA, Lewis EF, et al. Estimated glomerular filtration rate, inflammation, and cardiovascular events after an acute coronary syndrome. Am Heart J. 2008;155:725–731. doi: 10.1016/j.ahj.2007.11.031. [DOI] [PubMed] [Google Scholar]
- 7.Beattie JN, Soman SS, Sandber KR, et al. Determinants of mortality after myocardial infarction in patients with advanced renal dysfunction. Am J Kidney Dis. 2001;37:1191–1200. doi: 10.1053/ajkd.2001.24522. [DOI] [PubMed] [Google Scholar]
- 8.Wright RS, Reeder GS, Herzog CA, et al. Acute myocardial infarction and renal dysfunction: a high-risk combination. Ann Intern Med. 2002;137:563–570. doi: 10.7326/0003-4819-137-7-200210010-00007. [DOI] [PubMed] [Google Scholar]
- 9.Shlipak MG, Heidenreich PA, Noguchi H, Chertow GM, Browner WS, McMClellan MB. Association of renal insufficiency with treatment and outcomes after myocardial infarction in elderly patients. Ann Intern Med. 2002;137:555–562. doi: 10.7326/0003-4819-137-7-200210010-00006. [DOI] [PubMed] [Google Scholar]
- 10.Weaver WD, Simes RJ, Betriu A, et al. Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review. JAMA. 1997;278:2093–2098. [PubMed] [Google Scholar]
- 11.Zijlstra F, Hoorntje JC, de Boer MJ, et al. Long-term benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial infarction. N Engl J Med. 1999;341:1413–1419. doi: 10.1056/NEJM199911043411901. [DOI] [PubMed] [Google Scholar]
- 12.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 13.Yamaguchi J, Kasanuki H, Ishii Y, et al. Prognostic significance of serum creatinine concentration for in-hospital mortality in patients with acute myocardial infarction who underwent successful primary percutaneous coronary intervention (from the Heart Institute of Japan Acute Myocardial Infarction [HIJAMI] Registry) Am J Cardiol. 2004;93:1526–1528. doi: 10.1016/j.amjcard.2004.02.065. [DOI] [PubMed] [Google Scholar]
- 14.Ferrer-Hita JJ, Dominguez-Rodriguez A, Garcia-Gonzalez MJ, Abreu-Gonzalez P. Renal dysfunction is an independent predictor of in-hospital mortality in patients with ST-segment elevation myocardial infarction treated with primary angioplasty. Int J Cardiol. 2007;118:243–245. doi: 10.1016/j.ijcard.2006.06.044. [DOI] [PubMed] [Google Scholar]
- 15.Marenzi G, Moltrasio M, Assanelli E, et al. Impact of cardiac and renal dysfunction on inhospital morbidity and mortality of patients with acute myocardial infarction undergoing primary angioplasty. Am Heart J. 2007;153:755–762. doi: 10.1016/j.ahj.2007.02.018. [DOI] [PubMed] [Google Scholar]
- 16.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1–S266. [PubMed] [Google Scholar]
- 17.Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function: measured and estimated glomerular filtration rate. N Engl J Med. 2006;354:2473–2483. doi: 10.1056/NEJMra054415. [DOI] [PubMed] [Google Scholar]
- 18.Sorensen CR, Brendorp B, Rask-Madsen C, Kober L, Kjoller E, Torp-Pedersen C. The prognostic importance of creatinine clearance after acute myocardial infarction. Eur Heart J. 2002;23:948–952. doi: 10.1053/euhj.2001.2989. [DOI] [PubMed] [Google Scholar]
- 19.Sadeghi HM, Stone GW, Grines CL, et al. Impact of renal insufficiency in patients undergoing primary angioplasty for acute myocardial infarction. Circulation. 2003;108:2769–2775. doi: 10.1161/01.CIR.0000103623.63687.21. [DOI] [PubMed] [Google Scholar]
- 20.Namgung J, Doh JH, Lee SY, Huh WS, Park SW, Lee WR. Effect of N-acetylcysteine in prevention of contrast-induced nephropathy after coronary angiography. Korean Circ J. 2005;35:696–701. [Google Scholar]
- 21.Hirakawa Y, Masuda Y, Kuzuya M, Iguchi A, Kimata T, Uemura K. Association of renal insufficiency with in-hospital mortality in Japanese patients with acute myocardial infarction undergoing percutaneous coronary interventions. Int Heart J. 2006;47:745–752. doi: 10.1536/ihj.47.745. [DOI] [PubMed] [Google Scholar]
- 22.Gibson CM, Pinto DS, Murphy SA, et al. Association of creatinine and creatinine clearance on presentation in acute myocardial infarction with subsequent mortality. J Am Coll Cardiol. 2003;42:1535–1543. doi: 10.1016/j.jacc.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 23.Anavekar NS, McMurray JJ, Velazquez EJ, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285–1295. doi: 10.1056/NEJMoa041365. [DOI] [PubMed] [Google Scholar]
- 24.Lee KH, Jeong MH, Ahn YK, et al. Sex differences of the clinical characteristics and early management in the Korea acute myocardial infarction registry. Korean Circ J. 2007;37:64–71. [Google Scholar]
- 25.Parikh CR, Coca SG, Wang Y, Masoudi FA, Krumholz HM. Long-term prognosis of acute kidney injury after acute myocardial infarction. Arch Intern Med. 2008;168:987–995. doi: 10.1001/archinte.168.9.987. [DOI] [PubMed] [Google Scholar]
- 26.Medi C, Montalescot G, Budaj A, et al. Reperfusion in patients with renal dysfunction after presentation with ST-segment elevation or left bundle branch block: GRACE (Global Registry of Acute Coronary Events) JACC Cardiovasc Interv. 2009;2:26–33. doi: 10.1016/j.jcin.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 27.McCullough PA, Sandberg KR, Borzak S, Hudson MP, Garg M, Manley HJ. Benefits of aspirin and beta-blockade after myocardial infarction in patients with chronic kidney disease. Am Heart J. 2002;144:226–232. doi: 10.1067/mhj.2002.125513. [DOI] [PubMed] [Google Scholar]
- 28.Berger AK, Duval S, Krumholz HM. Aspirin, beta-blocker, and angiotensin-converting enzyme inhibitor therapy in patients with end-stage renal disease and an acute myocardial infarction. J Am Coll Cardiol. 2003;42:201–208. doi: 10.1016/s0735-1097(03)00572-2. [DOI] [PubMed] [Google Scholar]
- 29.Lee KH, Lee SR, Kang KP, et al. Periprocedural hemoglobin drop and contrast-induced nephropathy in percutaneous coronary intervention patients. Korean Circ J. 2010;40:68–73. doi: 10.4070/kcj.2010.40.2.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Manoukian SV, Feit F, Mehran R, et al. Impact of major bleeding on 30-day mortality and clinical outcomes in patients with acute coronary syndromes: an analysis from the ACUITY Trial. J Am Coll Cardiol. 2007;49:1362–1368. doi: 10.1016/j.jacc.2007.02.027. [DOI] [PubMed] [Google Scholar]