Abstract
This study examines how mothers with and without a history of childhood-onset depression respond to their 3–9 year-old children’s emotions. Mother-child dyads included 55 offspring of mothers with a history of childhood-onset depressive disorders and 57 offspring of never-depressed mothers. Mothers with a history of childhood depression were less likely than were control mothers to respond in supportive ways to their children’s negative emotions and were more likely to magnify, punish, or neglect their children’s negative emotions. Magnification, neglect, and punishment of children’s negative emotions were concurrently associated with children’s internalizing symptoms, and neglect and punishment were associated with internalizing over a one year follow-up. Maternal neglect of children’s negative emotion was positively associated with later internalizing symptoms for children who already had higher internalizing symptoms at the initial assessment. Findings suggest that atypical socialization of emotion may be one mechanism in the development of internalizing disorders.
Keywords: maternal depression, socialization, emotion regulation, internalizing symptoms
It is well-documented that maternal depression significantly heightens children’s risk for depression and other psychiatric problems (Downey & Coyne, 1990; Wachs, Black, & Engle, 2009). Children of depressed parents are at a 3- to 4-fold risk for developing depression during childhood and adolescence (Beardslee, Versage, & Gladstone, 1998; Weissman, Warner, Wickramaratne, Moreau, & Olfson, 1997). As many as 45% of children with a depressed parent will experience an episode of major depression by late adolescence, with this number as high as 60% by the age of 25 (Beardslee et al., 1998; Hammen, 2000). Depressive disorders are often markedly severe in this population, including an earlier age of onset, longer duration of episodes, higher social impairment, and higher rates of suicide relative to other depressed children and adolescents (Beardslee, Keller, Lavori, & Staley, 1993; Weissman, Fendrich, Warner, & Wickramaratne, 1992; Weissman et al., 1997). Children with depressed parents are also at high risk for developing anxiety disorders (Beidel & Turner, 1997; Weissman et al., 2005; Wickramaratne & Weissman, 1998). The present study focuses on offspring of mothers whose own depression began prior to the age of 14. This group is at particularly high risk for internalizing problems. Children of parents for whom depression began in childhood have a 14-fold greater risk of having depression before age 13 compared to children of parents with older-onset cases (Weissman, Wickramaratne et al., 1984).
In order to improve prevention, early detection, and early intervention of depression and anxiety among children of depressed parents, we need a better understanding of the mechanisms through which risk is transmitted across generations. Despite overwhelming evidence of risk for internalizing symptoms and associated disorders in offspring of depressed parents, the underlying mechanisms of this risk are still unclear (Goodman, 2007; Goodman & Gotlib, 1999). The intergenerational transmission of internalizing problems is likely to result from complex transactional processes between the parent and child. As many researchers have shown (Anderson, Lytton, & Romney, 1986; Patterson, DeBaryshe, & Ramsey, 1989; Sameroff, 1975), child outcomes are the result of reciprocal influences among parental and child behaviors. Child factors shown to be important in the development of internalizing symptoms and disorders include negative emotionality (Eisenberg et al., 2009; Gilliom & Shaw, 2004; Morris et al., 2002; Shaw, Keenan, Vondra, Delliquadri, & Giovannelli, 1997), behavioral inhibition (Kagan, Snidman, Zentner, & Peterson, 1999), low levels of effortful and attentional control, and low levels of positivity and reward processing (Forbes, Shaw, & Dahl, 2007; Silk, Shaw, Forbes, Lane, & Kovacs, 2006). Several characteristics of the family environment can exacerbate these child characteristics in contributing to the development of internalizing problems. These include interparental conflict (Grych, Raynor, & Fosco, 2004; Shaw et al., 1997), parental criticism (Frye & Garber, 2005; Silk et al., 2009), and controlling parenting (Gilliom & Shaw, 2004; Morris et al., 2002). Previous research on the family context of depressed parents has focused primarily on the quality of mother-child interaction. This work has revealed lower levels of positivity and higher levels of negativity in dyads with a depressed mother (i.e. Cohn, Campbell, Matias, & Hopkins, 1990; Cummings, Keller, & Davies, 2005; Field, Healy, Goldstein, & Guthertz, 1990; Foster, Garber, & Durlak, 2008; Tarullo, DeMulder, Martinez, & Radke Yarrow, 1994).
This body of research has pointed to general problems in the parent-child relationship in high-risk families; however, greater specificity is needed in pinpointing the specific parenting practices that promote the development of internalizing symptoms. The present study focuses on emotion-related parenting practices that could contribute to the development of internalizing symptoms in offspring and could be addressed in behavioral and parenting interventions. Emotion-related parenting practices are parenting practices that deal with emotion and emotion management, such as how parents discuss and respond to children’s emotions. These practices are important because they are believed to play a key role in the socialization of emotion and emotion regulation in children (Eisenberg, Cumberland, & Spinrad, 1998; Morris, Silk, Steinberg, Myers, & Robinson, 2007).
Parents’ emotion-related parenting practices appear to be influenced by what Gottman and colleagues refer to as a “meta-emotion philosophy”, defined as a parent’s beliefs about his or her own and his or her children’s emotions that guides responses to these emotions (Gottman, Katz, & Hooven, 1996). Emotion-coaching parents are aware of the child’s emotion, help the child to verbally label emotions, empathize with or validate the child’s emotion, see the child’s emotion as an opportunity for intimacy or teaching, and/or help the child to problem solve (Gottman et al., 1997). Emotion-dismissing parents, on the other hand, believe that negative emotions are potentially harmful to children, and that parents should work to help children minimize negative emotions as quickly as possible (Gottman et al. 1996). In a longitudinal study of 5-year-old children, Gottman et al. (1996) found that emotion-coaching parents, assessed via a meta-emotion interview, were more likely to have children with vagal tone levels conducive to better regulation of emotion. These children also had higher teacher-rated social skills three years after parents’ meta-emotion philosophy was assessed. More recent studies with school-aged youth have supported associations between parents’ meta-emotion philosophy, children’s emotion regulation, and children’s psychosocial adjustment (Cunningham, Kliewer, & Garner, 2009; Lunkenheimer, Shields, & Cortina, 2007).
Research examining parents’ specific responses to children’s emotions suggests that parental reactions to child emotions play a role in conveying implicit and explicit messages to children about how to manage emotions (Eisenberg, Fabes, & Murphy, 1996). Positive responses to emotions can support emotion regulation by encouraging or providing models of potentially adaptive emotion regulation strategies. These supportive responses help children refine and rehearse strategies for managing emotion. Parents may also respond to children’s negative emotions in non-supportive ways. Parents who view negative emotions as aversive, or who lack a sense of efficacy in their own ability to manage emotions, may be particularly likely to have negative responses to their children’s emotional displays (Gottman, Katz, & Hooven, 1997). Critical or other overtly negative reactions, such as mocking or threatening to punish the child for his or her display of emotion, may encourage the suppression of emotion or the use of avoidant or aggressive emotion regulation strategies (Buck, 1984; Eisenberg et al., 1996; Roberts & Strayer, 1987). Buck (1984) theorized that if children’s expression of negative emotions is consistently punished, they may begin to associate the experience of anger or sadness with negative consequences. When these children are faced with situations that provoke negative emotions, they may learn to suppress emotional expression while still experiencing heightened physiological arousal (Gross & Levenson, 1997).
Eisenberg and colleagues have found that parent report of supportive responses to children’s emotions is associated with better effortful control among toddlers (Spinrad et al., 2007) and use of more constructive emotion regulation strategies in peer provocations among school-aged children (Eisenberg et al., 1996). In contrast, parent reports of punitive and minimizing responses are associated with school-age children’s use of avoidant strategies in peer interactions and with parent-report of problem behavior and poor social functioning (Eisenberg, 1994; Eisenberg, Fabes, Carlo, & Karbon, 1992; Eisenberg et al., 1996; Eisenberg et al., 1999). Other research has supported Eisenberg and colleagues’ results. Roberts (1999) found that parents’ non-punitive responses to preschool-age children’s distress were concurrently associated with children’s prosocial behavior. Ramsden and Hubbard (2002) found maternal acceptance of fourth-grade children’s negative emotions to have a concurrent and indirect relationship with lower child aggressiveness through child emotion regulation.
In related work based on Tomkins’ Affect Theory (Tomkins, 1963), Malatesta-Magai (1991) proposed a model of five strategies that parents typically use to socialize children’s emotions: Reward, Punish, Override, Neglect, and Magnify. A rewarding response is a response to the child’s emotion that provides comfort, empathy, and/or helps the child to solve problems. A rewarding response does not actually involve providing a reward to the child for displaying a negative emotion; therefore, to be more consistent with terminology used in existing literature on emotion socialization, we subsequently refer to this type of response as supportive. Override responses are dismissive parental behaviors that attempt to dismiss the emotion, such as telling a child “things aren’t so bad” or distracting the child. Both supportive and override responses are believed to typically decrease children’s negative emotions, although override responses may be experienced as less validating of children’s emotional experience. A punitive response involves discouraging the child’s emotional expression by showing disapproval, mocking, or punishing emotional expression. Magnify occurs when a parent responds to the child’s emotion by matching the emotion with equal or stronger intensity. A neglect response occurs when the parent ignores the child’s emotional expression. Punitive, magnify, and neglect responses are generally considered negative responses likely to increase children’s negative emotions (Klimes-Dougan, Brand, & Garside, 2001).
These five responses can be assessed via parent or adolescent report using the Emotions as a Child Scale (EAC; Magai, 1996). Research using the retrospective reports of young adults on the EAC found that parental use of punish and neglect strategies during childhood were associated with higher levels of psychological distress in young adulthood (Garside & Klimes-Dougan, 2002). Work by O’Neal and Magai (2005) examined the relationship between adolescent-reported parental responses to children’s emotions on the EAC and child problem behavior in a group of inner-city early adolescents. They found neglect, magnify, and punish to be concurrently related to elevated adolescent report of internalizing symptoms and externalizing behavior. Another more recent study using the EAC reported that adolescents with higher levels of internalizing symptoms and/or externalizing symptoms (based on parent and adolescent report) described their parents as less likely to use supportive strategies in response to their emotions. These adolescents also described their parents as more likely to punish, magnify, or neglect their anger, and more likely to neglect sadness when compared to parents of adolescents with low levels of problem behavior (Klimes-Dougan et al., 2007).
The work of Eisenberg and colleagues (Eisenberg, 1994; Eisenberg et al., 1996; Eisenberg et al., 1999; Spinrad et al., 2007) and Gottman and colleagues (Gottman et al., 1996; Gottman et al., 1997) has generally focused on the socialization of global negative emotions (e.g., general negative affect and distress), while most research using the EAC has focused on the socialization of discrete emotions, such as anger, sadness, and fear. O’Neal and Magai (2005) examined whether emotion-specific or global socialization strategies were more strongly associated with symptoms of psychopathology in a study of inner-city adolescents. They found that adolescent reported global responses of punish, neglect, magnify, and override were concurrently associated with their reports of internalizing symptoms. In general, they found that adolescents’ reports of global rather than emotion specific responses were more strongly related to problem behavior, including internalizing symptoms (O’Neal & Magai, 2005).
Research on parental responses to emotion has rarely been extended to clinical populations of parents, and with the exception of one earlier report using a subset of the current sample (author citation), this research has not been extended to the families of parents with a history of depression. Related findings, however, suggest that mechanisms for socializing emotion may be disrupted in families with depressed parents. As discussed above, a vast literature on interactions between depressed and nondepressed mothers and their children reveals increased negativity and disengagement and decreased positivity in the interactions of depressed mothers and their offspring compared to those of non-depressed mothers (see Downey & Coyne, 1990; Goodman, 2007; Goodman & Gotlib, 1999). Second, depressed adult women experience their own deficits in emotional reactivity and regulation (Bradley, 2000; Gilboa & Gotlib, 1997; Gross & Munoz, 1995), further contributing to potential difficulties in emotion-related parenting.
Mothers with a history of childhood-onset depression may be particularly challenged in emotion-related parenting because of early disruptions in their own socialization during childhood (Kovacs & Goldston, 1991; Puig-Antich et al., 1985). The duration and chronicity of emotional impairment in women who have experienced depressive episodes since childhood may have a more pervasive impact on parenting compared to mothers with a less chronic course or more recent onset of depression. These mothers may have a particularly difficult time remaining calm and supportive during children’s emotional displays and may have less of a repertoire of their own adaptive emotion regulation strategies (typically honed during childhood and adolescence) to model and teach in their interactions with their children. Researchers have indeed found that the chronicity and duration of depressive illness is related to the degree of impairment in affective interactions with children (Campbell, Cohn, & Meyers, 1995; Dickstein et al., 1998; Seifer, Dickstein, Sameroff, Magee, & Hayden, 2001). Relatedly, there is some evidence that offspring of mothers with a longer or more recurrent course of depression show greater problems in emotion regulation (Nolen Hoeksema, Wolfson, Mumme, & Guskin, 1995; Silk, Shaw, Skuban, Oland, & Kovacs, 2006). Severity of illness also appears to be important in predicting the emotional quality of parent-child interactions in offspring of depressed parents (Dickstein et al., 1998; Seifer, 1995). For this reason, we examine severity as well as history of depression.
According to an initial report based on a subset of the present sample (author citation), mothers with childhood-onset depression histories reported that they used less supportive strategies in response to fear and sadness and were more likely to neglect fear and sadness than control mothers. There were no differences in magnification of discrete emotions, and punitive and over-ride responses were not examined. The current study extends this initial report by including all five maternal responses to negative emotion. Based on O’Neal and Magai’s (2005) findings that responses to global emotions are more related to internalizing symptoms than responses to discrete emotions, we focused on responses to global negative emotion and also extend this initial work by examining concurrent and longitudinal associations with children’s internalizing symptoms.
Our first question was whether maternal depression was related to the ways that the mothers responded to their children’s negative emotions. We hypothesized that mothers with a history of depression would respond to children’s negative emotions with less supportive responses and more negative responses, such as punishing, neglecting, or magnifying children’s negative emotions. We also hypothesized that mothers higher in current depressive symptoms would show lower levels of supportive responses to children’s negative emotions and higher levels of negative responses to children’s negative emotions. Our second question was whether maternal responses to negative emotions were associated with children’s internalizing symptoms, both concurrently and over one year. We hypothesized that lower supportive responses and higher negative responses would be associated with internalizing symptoms concurrently and at follow-up, especially for offspring of depressed mothers.
Method
Participants
One hundred and twelve children (51 male, 61 female) participated in this study with their mothers (N = 87). Fifty-five were offspring of mothers with a history of childhood-onset depression (COD) and 57 children were offspring of never-depressed mothers (NCOD). Mothers and children were participants in a larger Program Project on risk factors for childhood-onset mood disorder. For inclusion in the larger study, all COD adult probands were required to meet DSM criteria (American Psychiatric Association, 1980; American Psychiatric Association, 1994; Kaufman, Birmaher, Brent, & Rao, 1997) for major depressive disorder (N=31), dysthymic disorder (N=3) or both (N=21) by age 14. All NCOD mothers reported a lifetime history free of major psychiatric disorders. Mothers in the COD group reported a mean current BDI score of 14.21 (SD = 9.57) and NCOD mothers reported a mean current BDI score of 3.55 (SD = 3.74, t = 7.74, p < .001). All participants were free of pre-existing major systemic medical disorders and were without evidence of mental retardation. For inclusion in the current sample, mothers with children between the ages of 3 and 9 had to have a follow-up within 2 years at the Parent-Child Interaction component of the Study.
Children ranged in age from 3 to 9 (M = 4.46, SD = 1.63) and mothers ranged in age from 21 to 41 (M = 29.09, SD = 4.46). Children were 63% Caucasian, 23% African American, and 13% Biracial. Forty-two percent of the mothers were married and 55% were single (2 mothers did not report marital status). Seventeen sets of siblings from the COD group and 4 sets of siblings from the NCOD group participated in the study. The difference in participation of siblings across the two parental groups reflects a decision made by the investigators rather than inherent group differences. Specifically, since we were interested in children at-risk for mood disorder, we actively recruited all the offspring of proband parents who met the age requirements for the various study protocols. Shared variance due to sibling participation was modeled using random effects models as described in the results section.
We did not directly match COD and NCOD mothers, however, we tried to balance the groups with respect to ethnic and other sociodemographic factors by advertising in similar communities for COD and NCOD participants. COD and NCOD groups did not differ in race, marital status, child age, or child gender (all p’s > .05). Despite our attempts to balance the two groups, some differences in sociodemographic factors emerged. COD mothers were younger on average (M = 28.14, SD = 3.52) than NCOD mothers (M = 30.01, SD = 5.07; t = 2.26, p <.05). Maternal education was used as an indicator of SES based on research showing that of the four factors that compose the Hollingshead index (Hollingshead, 1975), maternal education is the most uniquely and strongly related to maternal and child behavior (Bornstein, Hahn, Suwalsky, & Haynes, 2003). In our sample, NCOD mothers had obtained a higher degree of education (5% no high school degree, 39% high school grad/GED, 52% some college, 4% postgraduate degree) than COD mothers (17% no high school degree, 51% high school grad/GED, 19% some college, 13% postgraduate degree; χ2 = 15.05, p < .01). Mother’s age and education level were included as covariates in subsequent analyses. Child’s age was also included as a covariate given the wide age range of the sample.
Recruitment and diagnostic determination
COD mothers were recruited into a larger program project through prior research studies or community advertisements. For adults with a history of COD, the presence of a verifiable early-onset depressive disorder was required. Eight participants (15%) had been enrolled in a longitudinal naturalistic follow-up of COD (Kovacs, Obrosky, Gatsonis, & Richards, 1997). These participants had multiple psychiatric assessments over the course of up to 20 years, using the semistructured Interview Schedule for Children and Adolescents or its version for young adults (Sherrill & Kovacs, 2000). The remaining participants were referred from other studies of pediatric depression or recruited through advertising in the general community. NCOD participants were recruited by using the Cole Directory, which provides phone numbers for families meeting specific sociodemographic criteria; advertising for volunteers in the general community or a local Women, Infants, and Children center (which provides nutritional services for income-eligible families); and by accessing individuals who participated as controls in research when they were children. All NCOD and COD participants for this study were recruited during the same 5 year interval from 1997 to 2002.
Diagnostic status of each mother was confirmed at Time 1 (T1) of the present study based on the results of standardized, semistructured psychiatric interviews, administered by professional-level clinical evaluators. For participants from the Kovacs et al. (1997) study of childhood-onset depression, original diagnoses were made during childhood using DSM-III, and were confirmed at T1 via follow-up interviews using DSM-IV via the Structured Clinical Interview for DSM-IV (SCID). For participants recruited as adults from the community, diagnoses were made based on detailed information about childhood functioning. SCID interviews were conducted with the mother and, separately, with a second informant knowledgeable about the mother’s childhood (e.g. the mother’s parent or sibling). In addition, childhood records were required to establish documented evidence of the mood disorder during childhood (e.g. notes in medical records or childhood psychiatric evaluations). Records were available for approximately 95% of cases. Interviewing clinicians derived initial lifetime diagnoses which were then verified by having 2 experienced psychiatrists, trained in research diagnostic procedures, independently derive the diagnoses. Disagreements were resolved via consensus to arrive at a final DSM-based consensus diagnoses (Leckman, Sholomskas, Thompson, Belanger, & Weissman, 1982; Maziade et al., 1992). There was no difference in age of first depression onset for participants recruited as adults (M = 10.00, SD = 2.03) compared to participants recruited from the original Kovacs et al. 1997 sample (M = 10.00, SD = 2.03; t = .39, p = .70).
Structured Clinical Interview for DSM-IV Patient Version (SCID)
The Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (First, Spitzer, Gibbon, & Williams) was used to assess lifetime psychiatric disorders among prospectively recruited COD probands and NCOD probands, and to confirm original diagnoses among COD probands from the Kovacs et al. (1997) study. The SCID is a semi-structured, clinician-administered diagnostic interview that includes modules corresponding to major DSM psychiatric classes. The SCID was expanded to include criteria for selected childhood diagnoses and DSM-III (APA, 1980) current and lifetime criteria for affective disorders. Based on a subset of 50 randomly selected cases, internal consistencies (i.e., kappas) for DSM–IV diagnosis of major depression and dysthymia were .92 and .63, respectively.
Procedures and Measures
Participants were part of a larger study that included a 2 to 2.5 hour laboratory visit during which behavioral data and questionnaires were collected. The present investigation focuses on self-report data from questionnaires only. All visits began with the child playing with toys on his/her own while the mother completed questionnaires regarding the child and family. Questionnaires were re-administered to all participants at a follow-up assessment (T2). The average time between assessments was 12.03 months (range 6 months to 24 months).
Beck Depression Inventory (BDI)
Data were also collected on current depressive symptoms using the Beck Depression Inventory (Beck, Steer, & Garbin, 1988). The BDI is a well-established 21-item measure designed to assess current depressive symptoms among clinically referred or community samples of adults. The BDI possesses stable internal consistency, adequate test–retest reliability, and good construct validity (Carlson, 1998). Cronbach’s alpha in the present sample was .92. T1 data were used for the BDI.
Emotions as a Child Scales (EAC; Klimes-Dougan et al., 2001; Magai & O’Neal, 1997)
This parent-report instrument was adapted from Magai’s (1996) original child-report version of the Emotion Socialization Scales of the EAC Inventory. These scales were developed to assess maternal responses to children’s expression of sadness, anger, and fear. Evidence of reliability and validity has been documented (Klimes-Dougan et al., 2007). Respondents are asked to rate how typical their responses to children’s expression of emotion are on a 5-point Likert scale. The scales includes 3 items specific to each emotion grouped according to 5 strategies (total of 9 items per response type for 45 items total): Support (e.g., “Helped my child deal with the issue,” “Comforted my child”); Override (e.g.. “Told him/her not to worry,” “Distract him/her”); Magnify (e.g., “Got tearful and cried,” “Got angry with my child”); Neglect (e.g., “Usually didn’t notice,” “Ignored him/her”); and Punish (e.g., “Punished him/her,” “Gave him/her a disgusted look”). Support refers to responses that comfort or assist the child in managing emotion and Override refers to attempts to minimize the emotion or distract the child from the emotion. Magnify refers to responses that amplify the child’s initial expression of emotion, Punitive refers to punishing or critical responses, and Neglect involves parental unresponsiveness to these expressions of emotion. To create indices of global socialization of emotion, items for each type of response were averaged across anger, sadness, and fear. Cronbach’s alphas revealed that these global scales were generally internally consistent, although reliability was initially lower for the Punitive scale (Support = .88, Magnify = .80, Override = .77, Punitive = .59, and Neglect = .68). Reliability for the punitive scale was improved to alpha = .65 by removing three items (“Showed him/her you did not like them being sad,” “Told him/her not to be a ‘fraidy-cat,’ and “Told him/her that they should be ashamed (for anger)”. The revised 6 item punitive scale was used for subsequent analyses. T1 data were used for the EAC scales.
Child Behavior Checklist (CBCL)
Children’s internalizing symptoms were assessed using mothers’ reports on two versions of the Child Behavior Checklist, for ages 2–3 and 4–16, respectively (CBCL; Achenbach, 1991, 1992). The CBCL is a well-validated measure that assesses behavioral and emotional problems among children. Parents rate each item on a three point scale ranging from “Not True” to “Very True” of the child. Both versions include a broadband factor assessing internalizing symptoms items which was used in the current study. Because the content and quantity of items differed on the two versions, we transformed raw internalizing scores to standardized z scores to facilitate comparability across the two versions. We chose to conduct statistical analyses using raw scores rather than T scores because of evidence of lower sensitivity of T scores in reflecting variation in functioning within the normal range due to compression of scores in the lower range (Drotar, Stein, & Perrin, 1995). As a result of this limitation, Achenbach (1991) recommended that investigators interested in making distinctions among subclinical samples of children for research purposes use raw scores for statistical analyses. Cronbach’s alpha for the Internalizing factor for this study was .82 for the age 2–3 version and .86 for the age 4–16 version. T1 and T2 data were used for the CBCL.
Results
Preliminary Analyses
As shown in Table 1, offspring of COD and NCOD mothers differed significantly in internalizing symptoms at T1 and T2, with COD offspring higher in internalizing symptoms at both time points. In order to interpret the clinical significance of this difference, we examined the percentage of subjects meeting clinical criteria for both groups. At Time 1, 24% of COD offspring scored in the clinical range on internalizing, 7% scored in the borderline range, and 69% scored in the normative range. In contrast, 2% of NCOD offspring scored in the clinical range, 2% scored in the borderline range, and 96% scored in the normative range. Ranges were identical at T2 for the NCOD group (2% clinical, 2% borderline, 96% normative), but lower for the COD group (13% clinical, 5% borderline, 82% normative). Thus, COD youth were 6–12 times more likely to demonstrate clinical levels of internalizing symptoms than NCOD youth.
Table 1.
Mean Scores and Standard Deviations for Maternal Responses to Child Emotions and Internalizing Symptoms by Maternal Diagnostic Group
| Variable | Min | Max | NCOD (n = 57) | COD (n = 55) | t | Cohen’s d | ||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | |||||
| Maternal Response to Emotion | ||||||||
| Support | 6.00 | 15.00 | 13.61 | 1.95 | 12.49 | 2.16 | 2.88** | 0.54 |
| Magnify | 3.00 | 11.00 | 4.54 | 1.66 | 5.72 | 1.81 | −3.61*** | −0.68 |
| Neglect | 3.00 | 10.00 | 4.88 | 1.03 | 5.41 | 1.38 | −2.32* | −0.44 |
| Punitive | 3.00 | 9.50 | 4.12 | 1.46 | 5.13 | 1.53 | −3.50*** | −0.68 |
| Override | 4.33 | 14.00 | 10.05 | 2.41 | 10.12 | 2.13 | −.17 | −0.03 |
| Internalizing Symptoms | ||||||||
| T1 Internalizing | −1.14 | 2.77 | −.52 | .66 | .38 | 1.00 | −5.54*** | −1.06 |
| T2 Internalizing | −.90 | 4.56 | −.35 | .61 | .37 | 1.18 | −4.02*** | −0.77 |
| T1 Internalizing (T score) | 29.00 | 74.00 | 44.20 | 8.64 | 54.94 | 9.90 | −6.01*** | −1.16 |
| T2 Internalizing (T score) | 33.00 | 77.00 | 43.58 | 7.75 | 51.25 | 9.72 | −4.63*** | −.87 |
p < .05;
p < .01;
p < .001; Note: Statistical analyses were conducted using standardized raw scores, but T scores are presented above for descriptive purposes.
Table 2 shows bivariate inter-correlations among key variables. The inter-correlations reveal that mothers who were more likely to punish negative emotions were also more likely to magnify and neglect negative emotions. There was no relationship between support and any of the negative responses. However, mothers who reported engaging in more override responses also reported engaging more in all other responses, including both positive and negative responses.
Table 2.
Bivariate Correlations between Maternal Responses to Child Emotions and Child Internalizing Symptoms
| Support | Magnify | Neglect | Punitive | Override | T1 Internalizing | T2 Internalizing | Maternal BDI | |
|---|---|---|---|---|---|---|---|---|
| 1. Support | 1.0 | |||||||
| 2. Magnify | .02 | 1.0 | ||||||
| 3. Neglect | .05 | .18 | 1.0 | |||||
| 4. Punitive | −.12 | .65*** | .32** | 1.0 | ||||
| 5. Override | .54*** | .34*** | .24* | .29** | 1.0 | |||
| 6. T1 Internalizing | −.14 | .25** | .31** | .27** | .00 | 1.0 | ||
| 7. T2 Internalizing | −.14 | .22* | .36*** | .31** | .04 | .57*** | 1.0 | |
| 8. Maternal BDI | −.24* | .24* | .17 | .26** | −.04 | .46*** | .53*** | 1.0 |
p < .05;
p < .01;
p < .001; N =112.
How does Maternal Depression Relate to Maternal Responses to Negative Emotion?
We hypothesized that mothers with a history of depression would respond to children’s negative emotion with less supportive responses and more negative responses, such as punishing, neglecting, or magnifying children’s negative emotions. As shown in Table 1, COD and NCOD mothers’ reports of responses to children’s negative emotion were compared using independent samples t-tests. COD and NCOD mothers differed significantly on four out of the five categories of responses. As hypothesized, COD mothers were less likely than NCOD mothers to respond to global negative emotion with a supportive response and were more likely to respond with a magnifying, neglectful, or punitive response. There were no group differences in the tendency to respond by overriding the child’s negative emotion.
We also hypothesized that mothers with higher levels of current depressive symptoms would show less supportive responses and more negative responses to children’s negative emotions. As shown in Table 2, this hypothesis was largely supported. Bivariate correlations revealed an inverse relation between maternal depressive symptoms and supportive responses, and positive associations between maternal depressive symptoms and magnifying and punitive responses.
Maternal Responses to Child Emotion and Child Internalizing Symptoms
Our second question was whether maternal responses to negative emotions were associated with children’s internalizing symptoms. We hypothesized that lower supportive responses and higher negative responses would be associated with internalizing symptoms concurrently and at follow-up, especially for offspring of depressed mothers. Bivariate correlations shown in Table 2 indicated that mothers’ tendencies to engage in supportive or override responses were not related to child internalizing symptoms concurrently or one year later. However, as hypothesized, all three negative maternal responses were related to child internalizing symptoms concurrently and longitudinally. Mothers who reported engaging more in magnifying, neglecting, and punitive responses to children’s negative emotion had children who scored higher on internalizing symptoms at both T1 and T2.
To examine whether maternal responses to children’s emotions predicted Time 2 internalizing symptoms above and beyond initial internalizing symptoms or interacted with diagnostic group status, and to control for shared variance among siblings, we computed a series of Mixed Effects Linear Models using Restricted Maximum Likelihood Estimation. Mixed effects models can be used to jointly model the effects of fixed factors with the effects of random factors, such as family membership, in which data exhibit correlated or non-constant variability. Thus, in cases where siblings participated, potential biases created by treating all the subjects as independent are addressed. Mixed effects models were computed with T2 internalizing symptoms as the dependent variable and fixed effects for maternal response (support, punish, magnify, neglect, or override) and maternal diagnostic group. We included covariates for T1 internalizing symptoms, maternal BDI score, child age and gender, mother age, and mother’s education level. We also controlled for child externalizing symptoms at Time 1 given evidence of relations between parental response to children’s emotion and children’s externalizing behavior (Eisenberg et al., 1999; Eisenberg, Losoya et al., 2001) as well as high rates of externalizing behavior in children of depressed mothers (Weissman, Gammon, John, & Merikangas, 1987). We included the interaction between maternal response and diagnostic group to examine whether negative responses were particularly detrimental for COD offspring, and the interaction between maternal response and internalizing symptoms scores at T1 to examine whether negative responses exacerbated initial internalizing symptoms. Family membership was treated as a random effect.
Results of the linear mixed models are summarized in Table 3. There were significant main effects for punish and neglect indicating that both of these negative maternal responses were predictive of T2 internalizing symptoms even after controlling for Time 1 internalizing symptoms, externalizing symptoms, maternal depressive symptoms, and other covariates (maternal education, maternal age, and child age and gender). In addition, there were significant two-way interactions between neglect and T1 internalizing symptoms and between override and T1 internalizing symptoms in predicting T2 internalizing symptoms. There were no interactions between maternal responses to emotion and diagnostic group.
Table 3.
Summary of Mixed Effects Models for T2 Internalizing Symptoms with Maternal Response to Negative Emotion, Diagnostic Group, Covariates and Interactions, as Fixed Effects and Family as a Random Effect
| Support |
Magnify |
Punish |
Neglect |
Override |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| F | d | F | d | F | d | F | d | F | d | |
| Maternal Response | .00 | .00 | 2.27 | .32 | 6.64* | .54 | 7.23** | .57 | 3.65 | .40 |
| Diagnostic Group | .47 | .14 | .39 | .13 | .26 | .10 | 2.20 | .31 | .13 | .08 |
| T1 Internalizing | .42 | .14 | .03 | .04 | .08 | .06 | 6.42* | .53 | 2.41 | .33 |
| Maternal Response | ||||||||||
| × Diagnostic Group | .50 | .15 | .38 | .13 | .38 | .13 | 2.00 | .30 | .15 | .08 |
| Maternal Response | ||||||||||
| × T1 Internalizing | .05 | .05 | .84 | .19 | 1.31 | .24 | 10.70** | .69 | 4.57* | .45 |
| Maternal BDI | 8.31** | .61 | 9.58** | .65 | 6.06* | .52 | 7.93** | .59 | 8.10** | .60 |
| T1 Externalizing | 9.17** | .64 | 9.65** | .65 | 11.02** | .70 | 4.90* | .47 | 8.87** | .63 |
| Child Age | .01 | .02 | .12 | .07 | .03 | .04 | .08 | .06 | .16 | .08 |
| Child Gender | .02 | .03 | .03 | .04 | .06 | .05 | .04 | .04 | .00 | .00 |
| Mom Age | 2.25 | .32 | 2.53 | .34 | 2.31 | .32 | .51 | .15 | 1.99 | .30 |
| Mom Education | 1.70 | .27 | 2.49 | .33 | 2.56 | .34 | 1.81 | .28 | 2.32 | .32 |
p < .05;
p < .01. T1 = Time 1; T2 = Time 2. Note: Maternal response refers to maternal response to child’s negative emotions (specific response noted in column header). Degrees of freedom were 3,90 for maternal education and 1,90 for all other variables.
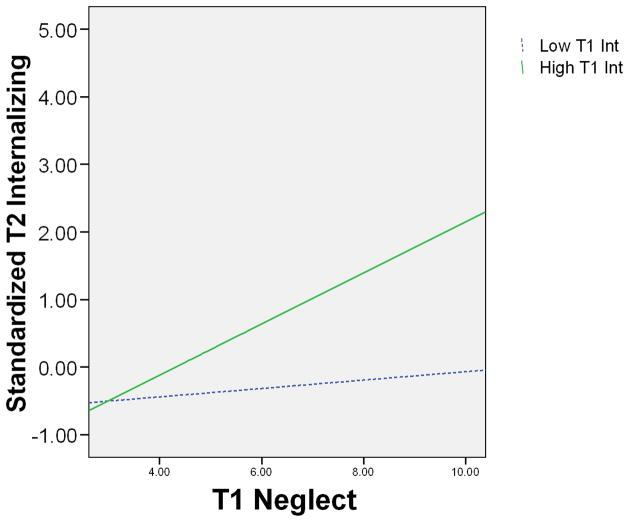
Two-way interactions were probed by computing post-hoc mixed effects models examining the relationship between neglect and override responses and T2 internalizing symptoms within children above and below the median on T1 internalizing symptoms. Consistent with the correlations, post-hoc mixed models predicting T2 internalizing symptoms from override responses were not significant for children with high (F[1,50] = .13; ns) or low (F[1,54] = 1.82; ns) T1 internalizing symptoms. Post-hoc mixed models predicting T2 internalizing symptoms from neglect responses indicated that responding to a child’s negative emotion was not associated with T2 internalizing symptoms for children who were initially low in internalizing symptoms (F[1,54] = 1.21; ns); however, for children who were initially high in internalizing symptoms, maternal neglect of negative emotion was associated with higher internalizing symptoms at T2 (F[1,50] = 10.31, p <.01; see Figure 1).
Figure 1.
The relation between mother’s neglect of child negative emotion and child’s Time 2 internalizing symptoms for children high and low on T1 internalizing symptoms.
There was no main effect of diagnostic group, however, there was a main effect of current maternal depressive symptoms that remained significant in predicting Time 2 internalizing symptoms above and beyond the effects of maternal response to negative emotions in all models. Specifically, higher levels of maternal depressive symptoms were associated with higher levels of T2 child internalizing symptoms. Children’s externalizing symptoms at T1 were also strongly associated with their internalizing at T2.
Discussion
We found that mothers with a history of childhood depression differed from more typical mothers in one critical component of the socialization of emotion—their responses to their young children’s negative emotions. They were less likely than mothers who did not have a history of depression to respond to their children’s negative emotions in a supportive fashion and were also more likely to respond in a negative manner. This included matching or amplifying the child’s negative emotion, punishing or threatening to punish the child for displaying the emotion, or failing to attend to the child’s emotional displays. These findings are consistent with other research on maternal depression which has revealed a pattern of greater negativity in mother-child interactions among dyads of depressed mothers and their offspring (e.g. Cohn et al., 1990; Field et al., 1990; Gordon et al., 1989; Hamilton, Jones, & Hammen, 1993). However, they extend this literature by documenting specific alterations in the socialization of negative emotion in families with depressed mothers. This is particularly important because children learn implicit and explicit messages about how to manage their emotions from the way that their parents respond to their own emotions (Morris et al., 2007). Thus, negative maternal responses to children’s emotions may set the stage for the development of future internalizing symptoms in children.
The present study provides evidence of an association between the socialization of negative emotion and children’s internalizing symptoms. We found that maternal negative responses to children’s emotions were associated with children’s internalizing symptoms concurrently and over a one-year follow-up. Specifically, mothers who were more likely to magnify, neglect, or punish children’s displays of negative emotion had children who exhibited more internalizing symptoms. This is consistent with findings from normative samples showing a link between non-supportive responses to children’s emotions and psychological adjustment (Eisenberg et al., 1996; Eisenberg et al., 1999; Garside & Klimes-Dougan, 2002; Gottman et al., 1996; O’Neal & Magai, 2005), although few previous studies have focused on internalizing symptoms. Importantly, the effects of punishing and neglecting emotions remained significant after controlling for Time 1 internalizing symptoms, indicating that these negative maternal responses were predictive of internalizing symptoms over time above and beyond initial levels.
Negative maternal responses to children’s negative emotions were related to child internalizing symptoms regardless of maternal diagnostic group. This suggests that although mothers with a history of depression were more likely to respond negatively to children’s emotions, these negative responses affected children of depressed and nondepressed mothers in similar ways. This finding suggests that negative responses to children’s emotions may represent a general risk factor for internalizing symptoms. However, given our finding of heightened rates of this risk factor in families of depressed mothers, maternal depression may represent a particularly important context in which to target this risk.
Negative responses to children’s emotions are likely to influence the development of internalizing symptoms by interfering with the development of optimal skills for regulating emotion. When mothers amplify or punish children’s emotional responses, they may increase children’s negative emotions in the short term by increasing arousal. In the long-term, maternal magnification and punishment of children negative emotions could interfere with the development of adaptive emotion regulation strategies. Mothers who respond to children’s emotions with equal or more intense displays of negative emotions may model dysregulated emotional displays for their children. Alternatively, when mothers punish or neglect children’s emotions, they send messages that the expression of negative emotion is not acceptable, thus encouraging children to hide or suppress their emotions. As Buck (1984) argued, emotional experience may become coupled with anxiety about receiving negative consequences for displaying negative emotions. Furthermore, the suppression of emotional displays is often accompanied by increased physiological arousal (Gross & Levenson, 1997). These negative responses also limit opportunities for discussion of emotion and problem solving (Garside & Klimes-Dougan, 2002), approaches that could improve emotion regulation. In turn, a number of studies suggest that failure to regulate negative emotions adaptively is associated with internalizing symptoms among young children and with depressive and anxious symptomatology and disorders among older children and adolescents (Eisenberg, Cumberland et al., 2001; Feng, Shaw, & Silk, 2008; Garber, Braafladt, & Weiss, 1995; Rubin, Coplan, Fox, & Calkins, 1995; Rydell, Berlin, & Bohlin, 2003; Sheeber, Allen, Davis, & Sorensen, 2000; Silk, Steinberg, & Morris, 2003; Suveg, Hoffman, Zeman, & Thomassin, 2008).
Consistent with this model, we have found previous evidence of problems in emotion regulation in this sample of offspring of mothers with childhood onset depression (COD). First, children of mothers with COD, especially behaviorally-inhibited children and girls, were found to be more likely to use passive emotion regulation strategies during emotion-eliciting scenarios than offspring of nondepressed control mothers (Feng, Shaw, Kovacs et al., 2008; Silk, Shaw, Skuban et al., 2006). Second, adaptive emotion regulation strategies, such as focusing on a future reward, were associated with lower levels of internalizing symptoms in children of mothers with childhood-onset depression (Feng, Shaw, Kovacs et al., 2008; Silk, Shaw, Skuban et al., 2006).
Interestingly, the association between neglect of children’s negative emotions and internalizing symptoms at follow-up was qualified by prior level of internalizing symptoms. When children were initially low on internalizing symptoms, there was no association between maternal neglect of negative emotions and later internalizing symptoms. However, maternal neglect of negative emotion was positively associated with later internalizing symptoms for children who already had higher levels of internalizing symptoms at the initial assessment. This suggests that neglecting negative emotion may only be harmful for children who tend to struggle in dealing with their emotions. It is likely that there are times when ignoring a child’s negative emotional display is an adaptive parenting approach and other times when it may be detrimental to the child. This difference may be child-specific as well as situational. Children who are emotionally healthy and have already developed a solid set of skills for regulating emotion may do better when parents ignore negative emotions because they possess greater skills to manage emotion without assistance. In contrast, children who have symptoms of internalizing disorders and related difficulties in managing their emotions may struggle without maternal assistance in managing emotion and may feel hurt or invalidated by the neglecting response, perhaps even resulting in an escalation of the negative emotion. This situation represents a poor match between a child who needs extra help in managing his or her negative emotion and a mother who cannot or would rather not deal with it. Findings may also be driven by child effects (i.e. Burke, Pardini, & Loeber, 2008) such that children with particularly high internalizing symptoms are more likely to elicit maternal neglect of emotions. Mothers may be so used to negative emotional displays in these children that they simply “tune out” or they may by overwhelmed by their children’s emotions and choose to withdraw. Our findings suggest that this combination may predispose youth toward internalizing symptoms. These findings are consistent with evidence that parents may respond more negatively to children’s emotion for children with more difficult temperaments (Yap, Allen, Leve, & Katz, 2008).
We did not find differences between mothers with and without a history of depression in the tendency to override children’s negative emotions. This is not surprising given that the override response includes strategies that likely help children to decrease negative emotion, such as distraction, but is also meant to capture a dismissive style towards the child’s emotions. Consistent with this observation, previous findings for the override scale have been mixed, with some studies finding override to be associated with greater adjustment problems (O’Neal & Magai, 2005), some finding it to be associated with lower adjustment problems (Klimes-Dougan et al., 2007), and some finding no association at all (Garside & Klimes-Dougan, 2002).
It is also notable that mothers’ supportive responses to children’s emotions were not associated with children’s internalizing symptoms concurrently or at follow-up. In this study, maternal negative socialization responses were more highly associated with outcomes than supportive responses. This is consistent with Garside and Klimes-Dougan’s (2002) study based on adults’ retrospective reports of parental socialization of emotion and current psychological distress as well as O’Neal and Magai’s (2005) study of inner-city adolescents. It is possible that negative responses to emotion are more salient to youth and thus exert a stronger influence on the development of psychopathology.
In this report, we chose to focus on children’s global negative affect rather than discrete negative emotions. This focus was based on O’Neal and Magai’s (2005) findings that responses to global emotions were more related to internalizing symptoms than responses to discrete emotions. It is also consistent with evidence that depressive symptoms in youth are associated with general dysregulation of negative emotions (Silk et al., 2003), and with predominant theoretical models of depression which emphasize heightened global negative affect (Watson, Clark, & Carey, 1988). For these reasons, we were interested in the socialization of negative emotions more broadly speaking as a mechanism involved in the intergenerational transmission of internalizing problems. We also believed that this approach was more conservative statistically, as it allowed us to limit the number of statistical tests performed (e.g. from 15 regressions to five regressions), thus significantly reducing type 1 error. We do; however, recognize the utility of the discrete emotion approach in addressing key questions involved in the socialization of emotion (e.g., Shaw et al. 2006).
We also focused exclusively on maternal depression. Two recent meta-analyses indicate that paternal depressive symptoms are associated with children’s internalizing problems (Connell & Goodman, 2002; Kane & Garber, 2004). Goodman and Gotlib (1999) have suggested that paternal depressive symptoms might exacerbate the effects of maternal depression on child internalizing, and a few studies have found that children with two depressed parents are at increased risk for anxiety and depressive disorders compared to children with one depressed parent (Dierker, Merikangas, & Szatmari, 1999; Mezulis, Hyde, & Clark, 2004; Weissman, Prusoff et al., 1984). Evidence also suggests that high father involvement might protect children from the effects of maternal depression (Mezulis et al., 2004). It is likely that socialization mechanisms, such as responses to children’s emotions, play a role in both direct effects of paternal depression on children’s internalizing as well as potential moderating roles that paternal depression may play in attenuating or exacerbating the effects of maternal depression on children’s internalizing outcomes. This is especially important given evidence that mothers and fathers may respond differently to children’s negative emotions (i.e. Cassano, Perry-Parrish, & Zeman, 2007; Cassano & Zeman, 2010; Wong, Diener, & Isabella, 2008). For these reasons, future research on the socialization of emotion in families with depressed fathers would be extremely valuable.
We should also note several limitations to the present investigation. First, findings are based exclusively on maternal self-report and using the same methods for both independent and dependent variable, raising the issue of reporter and method bias. This methodological limitation may have inflated the degree of associations between parent reports of responding to children’s emotions and estimates of child internalizing symptoms, even though these relations persisted when using maternal reports of initial child internalizing and externalizing symptoms. It is also possible that maternal depression could be associated with a negative reporting bias that might inflate perceptions of both one’s own parenting behavior and child internalizing symptoms. However, evidence of a depression-related bias in ratings of child symptomatology has generally been weak or inconclusive (Boyle & Pickles, 1997; Richters, 1992). Although some have argued that it is difficult to capture parental responses to children’s emotions using observational methods given generally low base-rates for emotional displays (e.g. Eisenberg et al., 1999; Garside & Klimes-Dougan, 2002), researchers have recently developed observational paradigms and coding systems to attempt to capture this phenomenon (Chaplin, Cole, & Zahn-Waxler, 2005; Hersh & Hussong, 2009; Hudson, Comer, & Kendall, 2008; Spinrad, Stifter, Donelan-McCall, & Turner, 2004). This is an important area for future methodological development and investigation.
Second, the sample consisted of women whose depression began in childhood, thus findings may not be generalizable to less severe forms of depression. Third, the Time 1 and Time 2 assessments were only separated by approximately 1 year, thus generalizations about change over time are limited to this relatively small interval. Future longitudinal research over longer periods of time would be valuable. Finally, expectations for emotion regulation and the socialization of emotion likely change considerably across the preschool and middle childhood periods covered in the present study (Wong et al., 2008). Evidence also suggests that emotion socialization processes vary by gender (Brody, 1996; Cunningham et al., 2009; Fivush, 1998). For example, several studies suggest that parents preferentially reinforce the display of submissive emotion in girls and disharmonious emotion in boys (Block, 1983; Chaplin et al., 2005; Fuchs & Thelen, 1988). An important next step will be to examine the relationships between parental depressive symptoms, the socialization of emotion, and internalizing symptoms by gender and within narrower age ranges.
Despite these limitations, the study has several notable strengths. It is one of the first studies to extend the growing literature on maternal responses to children’s emotions to a clinically relevant population. The study includes a high-risk sample of offspring of mothers with a history of childhood onset depression identified using rigorous clinical interviews and childhood records. Additionally, the longitudinal design facilitates an examination of internalizing symptoms over time.
Findings from the present study suggest that depressed parents differ from non-depressed parents in their responses to their children’s emotions and that these responses play a role in the development of children’s internalizing symptoms. If replicated, these findings could have implications for the prevention of anxiety and depression. In particular, these findings highlight the potential utility of preventative and intervention approaches that teach depressed parents skills for responding to their children’s emotions in adaptive ways. Providing opportunities for parent education, training, and intervention on emotion socialization techniques may be an effective way to intervene in the cycle of intergenerational transmission of depression for many families. Prevention programs might focus on helping depressed mothers identify and practice less negative responses to children’s emotions as a way to encourage improved emotion regulation in their offspring. The importance of this work is further underscored by the high rates of internalizing problems in the high risk sample. Twenty-four percent of the offspring of depressed mothers scored in the clinical range on the internalizing scale at the initial assessment, suggesting that interventions with the potential to alter trajectories toward mood and anxiety disorders later in childhood and adolescence in this population are critically needed.
Acknowledgments
This research was supported by an NIMH Program Project (#MH56193) awarded to the second and last authors. We would like to thank Charlei George for his assistance in data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jennifer S. Silk, Email: silkj@upmc.edu.
Daniel S. Shaw, Email: casey@pitt.edu.
Joanna T. Prout, Email: jtprout@gmail.com.
Flannery O’Rourke, Email: feo3@pitt.edu.
Tonya J. Lane, Email: tjd50@pitt.edu.
Maria Kovacs, Email: kovacs@pitt.edu.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM. Manual for the Child Behavior Checklist/2–3 and 1992 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1992. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM-III) Washington, D.C.: Author; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, D.C.: Author; 1994. [Google Scholar]
- Anderson KE, Lytton H, Romney DM. Mothers’ interactions with normal and conduct-disordered boys: Who affects whom? Developmental Psychology. 1986;22:604–609. [Google Scholar]
- Beardslee WR, Keller MB, Lavori PW, Staley JE. The impact of parental affective disorder on depression in offspring: A longitudinal follow-up in a nonreferred sample. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:723–730. doi: 10.1097/00004583-199307000-00004. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Versage EM, Gladstone TRG. Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. 1988. [Google Scholar]
- Beidel DC, Turner SM. At risk for anxiety: I. Psychopathology in the offspring of anxious parents. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:918–924. doi: 10.1097/00004583-199707000-00013. [DOI] [PubMed] [Google Scholar]
- Block JH. Differential premises arising from differential socialization of the sexes: Some conjectures. Child Development. 1983;54:1335–1354. [PubMed] [Google Scholar]
- Bornstein MH, Hahn C-S, Suwalsky JTD, Haynes OM. Socioeconomic status, parenting, and child development: The Hollingshead Four-Factor Index of Social Status and The Socioeconomic Index of Occupations. Mahwah, NJ: Lawrence Erlbaum; 2003. [Google Scholar]
- Boyle MH, Pickles AR. Influence of maternal depressive symptoms on ratings of childhood behavior. Journal of Abnormal Child Psychology. 1997;25:399–412. doi: 10.1023/a:1025737124888. [DOI] [PubMed] [Google Scholar]
- Bradley SJ. Affect Regulation and the Development of Psychopathology. New York: Guilford; 2000. [Google Scholar]
- Brody LR. Gender, emotional expression, and parent-child boundaries. In: Kavanaugh RD, editor. Emotion: Interdisciplinary perspectives. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 1996. pp. 139–170. [Google Scholar]
- Buck R. The communication of emotion. New York: Guilford Press; 1984. [Google Scholar]
- Burke JD, Pardini DA, Loeber R. Reciprocal relationships between parenting behavior and disruptive psychopathology from childhood through adolescence. Journal of Abnormal Child Psychology. 2008;36:679–692. doi: 10.1007/s10802-008-9219-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell SB, Cohn JF, Meyers T. Depression in first-time mothers: Mother-infant interaction and depression chronicity. Developmental Psychology. 1995;31:349–357. [Google Scholar]
- Carlson JF. Beck Depression Inventory. In: Impara JC, Plake BS, editors. Mental Measurements Yearbook. Vol. 13. Lincoln, NE: Buros Institute of Mental Measurements; 1998. pp. 100–121. [Google Scholar]
- Cassano MC, Perry-Parrish C, Zeman J. Influence of gender on parental socialization of children’s sadness regulation. Social Development. 2007;16:210–231. [Google Scholar]
- Cassano MC, Zeman JL. Parental socialization of sadness regulation in middle childhood: The role of expectations and gender. Developmental Psychology. 2010;46:1214–1226. doi: 10.1037/a0019851. [DOI] [PubMed] [Google Scholar]
- Chaplin TM, Cole PM, Zahn-Waxler C. Parental socialization of emotion expression: Gender differences and relations to child adjustment. Emotion. 2005;5:80–88. doi: 10.1037/1528-3542.5.1.80. [DOI] [PubMed] [Google Scholar]
- Cohn JF, Campbell SB, Matias R, Hopkins J. Face-to-face interactions of postpartum depressed and nondepressed mothernfant pairs at 2 months. Developmental Psychology. 1990;26:15–23. [Google Scholar]
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: A meta-analysis. Psychological Bulletin. 2002;128:746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Cummings E, Keller PS, Davies PT. Towards a family process model of maternal and paternal depressive symptoms: Exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry. 2005;46:479–489. doi: 10.1111/j.1469-7610.2004.00368.x. [DOI] [PubMed] [Google Scholar]
- Cunningham JN, Kliewer W, Garner PW. Emotion socialization, child emotion understanding and regulation, and adjustment in urban African American families: Differential associations across child gender. Development and Psychopathology. 2009;21:261–283. doi: 10.1017/S0954579409000157. [DOI] [PubMed] [Google Scholar]
- Dickstein S, Seifer R, Hayden LC, Schiller M, Sameroff AJ, Keitner G, Miller I, Rasmussen S, Matzko M, Magee KD. Levels of family assessment: II. Impact of maternal psychopathology on family functioning. Journal of Family Psychology. 1998;12:23–40. [Google Scholar]
- Dierker LC, Merikangas KR, Szatmari P. Influence of parental concordance for psychiatric disorders on psychopathology in offspring. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:280–288. doi: 10.1097/00004583-199903000-00015. [DOI] [PubMed] [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Drotar D, Stein RE, Perrin EC. Methodological issues in using the Child Behavior Checklist and its related instruments in clinical child psychology research. Journal of Clinical Child Psychology. 1995;24:184–192. [Google Scholar]
- Eisenberg N. Mothers’ reactions to children’s negative emotions: Relations to children’s temperament and anger behavior. Merrill Palmer Quarterly. 1994;40:138–156. [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL. Parental socialization of emotion. Psychological Inquiry. 1998;9:241–273. doi: 10.1207/s15327965pli0904_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL, Fabes RA, Shepard SA, Reiser M, Murphy BC, Losoya SH, Guthrie IK. The relations of regulation and emotionality to children’s externalizing and internalizing problem behavior. Child Development. 2001;72:1112–1134. doi: 10.1111/1467-8624.00337. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Carlo G, Karbon M. Emotional responsivity to others: Behavioral correlates and socialization antecedents. In: Eisenberg N, Fabes RA, editors. Emotion and its regulation in early development: New directions in child development. San Francisco: Jossey-Bass; 1992. pp. 57–74. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Murphy BC. Parents’ reactions to children’s negative emotions: Relations to children’s social competence and comforting behavior. Child Development. 1996;67:2227–2247. [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Shepard SA, Guthrie IK, Murphy BC, Reiser M. Parental reactions to children’s negative emotions: Longitudinal relations to quality of children’s social functioning. Child Development. 1999;70:513–534. doi: 10.1111/1467-8624.00037. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Losoya S, Fabes RA, Guthrie IK, Reiser M, Murphy B, Shepard SA, Poulin R, Padgett SJ. Parental socialization of children’s dysregulated expression of emotion and externalizing problems. Journal of Family Psychology. 2001;15:183–205. doi: 10.1037//0893-3200.15.2.183. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Valiente C, Spinrad TL, Liew J, Zhou Q, Losoya SH, Reiser M, Cumberland A. Longitudinal relations of children’s effortful control, impulsivity, and negative emotionality to their externalizing, internalizing, and co-occurring behavior problems. Developmental Psychology. 2009;45:988–1008. doi: 10.1037/a0016213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng X, Shaw DS, Kovacs M, Lane T, O’Rourke FE, Alarcon JH. Emotion regulation in preschoolers: The roles of behavioral inhibition, maternal affective behavior, and maternal depression. Journal of Child Psychology and Psychiatry. 2008;49:132–141. doi: 10.1111/j.1469-7610.2007.01828.x. [DOI] [PubMed] [Google Scholar]
- Feng X, Shaw DS, Silk JS. Developmental trajectories of anxiety symptoms among boys across early and middle childhood. Journal of Abnormal Psychology. 2008;117:32–47. doi: 10.1037/0021-843X.117.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Healy BT, Goldstein S, Guthertz M. Behavior-state matching and synchrony in mothernfant interactions of nondepressed versus depressed dyads. Developmental Psychology. 1990;26:7–14. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders - Patient Edition (SCID-I/P, Version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- Fivush R. Methodological challenges in the study of emotional socialization. Psychological Inquiry. 1998;9:281–283. [Google Scholar]
- Forbes EE, Shaw DS, Dahl RE. Alterations in reward-related decision making in boys with recent and future depression. Biological Psychiatry. 2007;61:633–639. doi: 10.1016/j.biopsych.2006.05.026. [DOI] [PubMed] [Google Scholar]
- Foster CJ, Garber J, Durlak JA. Current and past maternal depression, maternal interaction behaviors, and children’s externalizing and internalizing symptoms. Journal of Abnormal Child Psychology. 2008;36:527–537. doi: 10.1007/s10802-007-9197-1. [DOI] [PubMed] [Google Scholar]
- Frye AA, Garber J. The Relations among maternal depression, maternal criticism, and adolescents’ externalizing and internalizing symptoms. Journal of Abnormal Child Psychology. 2005;33:1–11. doi: 10.1007/s10802-005-0929-9. [DOI] [PubMed] [Google Scholar]
- Fuchs D, Thelen MH. Children’s expected interpersonal consequences of communicating their affective state and reported likelihood of expression. Child Development. 1988;59:1314–1322. doi: 10.1111/j.1467-8624.1988.tb01500.x. [DOI] [PubMed] [Google Scholar]
- Garber J, Braafladt N, Weiss B. Affect regulation in depressed and nondepressed children and young adolescents. Development & Psychopathology. 1995;7:93–115. [Google Scholar]
- Garside RB, Klimes-Dougan B. Socialization of discrete negative emotions: Gender differences and links with psychological distress. Sex Roles. 2002;47:115–128. [Google Scholar]
- Gilboa E, Gotlib IH. Cognitive biases and affect persistence in previously dysphoric and never-dysphoric individuals. Cognition and Emotion. 1997;11:517–538. [Google Scholar]
- Gilliom M, Shaw DS. Codevelopment of externalizing and internalizing problems in early childhood. Development and Psychopathology. 2004;16:313–333. doi: 10.1017/s0954579404044530. [DOI] [PubMed] [Google Scholar]
- Goodman SH. Depression in Mothers. Annual Review of Clinical Psychology. 2007;3:107–135. doi: 10.1146/annurev.clinpsy.3.022806.091401. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Gordon D, Burge D, Hammen C, Adrian C, Jaenicke C, Hiroto D. Observations of interactions of depressed women with their children. American Journal of Psychiatry. 1989;146:50–55. doi: 10.1176/ajp.146.1.50. [DOI] [PubMed] [Google Scholar]
- Gottman JM, Katz LF, Hooven C. Parental meta-emotion philosophy and the emotional life of families: Theoretical models and preliminary data. Journal of Family Psychology. 1996;10:243–268. [Google Scholar]
- Gottman JM, Katz LF, Hooven C. Meta-emotion. Mahwah, N.J.: Lawrence Earlbaum; 1997. [Google Scholar]
- Gross JJ, Levenson RW. Hiding feelings: The acute effects of inhibiting negative and positive emotion. Journal of Abnormal Psychology. 1997;106:95–103. doi: 10.1037//0021-843x.106.1.95. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Munoz RF. Emotion regulation and mental health. Clinical Psychology: Science and Practice. 1995;2:151–164. [Google Scholar]
- Grych JH, Raynor SR, Fosco GM. Family processes that shape the impact of interparental conflict on adolescents. Development and Psychopathology. 2004;16:649–665. doi: 10.1017/s0954579404004717. [DOI] [PubMed] [Google Scholar]
- Hamilton EB, Jones M, Hammen C. Maternal interaction style in affective disordered, physically ill, and normal women. Family Process. 1993;32:329–340. doi: 10.1111/j.1545-5300.1993.00329.x. [DOI] [PubMed] [Google Scholar]
- Hammen C. Interpersonal factors in an emerging developmental model of depression. In: Johnson SL, editor. Stress, coping, and depression. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. pp. 71–88. [Google Scholar]
- Hersh MA, Hussong AM. The association between observed parental emotion socialization and adolescent self-medication. Journal of Abnormal Child Psychology. 2009;37:493–506. doi: 10.1007/s10802-008-9291-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Unpublished manuscript. New Haven: Yale University Sociology Department; 1975. Four Factor Index of Social Status. [Google Scholar]
- Hudson JL, Comer JS, Kendall PC. Parental responses to positive and negative emotions in anxious and nonanxious children. Journal of Clinical Child and Adolescent Psychology. 2008;37:303–313. doi: 10.1080/15374410801955839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagan J, Snidman N, Zentner M, Peterson E. Infant temperament and anxious symptoms in school age children. Development and Psychopathology. 1999;11:209–224. doi: 10.1017/s0954579499002023. [DOI] [PubMed] [Google Scholar]
- Kane P, Garber J. The relations among depression in fathers, children’s psychopathology, and father-child conflict: A meta-analysis. Clinical Psychology Review. 2004;24:339–360. doi: 10.1016/j.cpr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U. Schedule for Affective Disorders and Schizophrenia for School-Age Children-(K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Klimes-Dougan B, Brand A, Garside RB. Factor structure, reliability, and validation of an emotion socialization scale. C. O’Neal (Chair), Multiple approaches to emotion socialization: Methodology and emotional development; Symposium conducted at the annual meeting of the American Psychological Association; San Francisco, CA. 2001. [Google Scholar]
- Klimes-Dougan B, Brand AE, Zahn-Waxler C, Usher B, Hastings PD, Kendziora K, Garside RB. Parental emotion socialization in adolescence: Differences in sex, age and problem status. Social Development. 2007;16:326–342. [Google Scholar]
- Kovacs M, Goldston D. Cognitive and social cognitive development of depressed children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1991;30:388–392. doi: 10.1097/00004583-199105000-00006. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Obrosky S, Gatsonis C, Richards C. First-episode major depressive and dysthymic disorder in childhood: Clinical and sociodemographic factors in recovery. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:777–784. doi: 10.1097/00004583-199706000-00014. [DOI] [PubMed] [Google Scholar]
- Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry. 1982;39:879–883. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- Lunkenheimer ES, Shields AM, Cortina KS. Parental emotion coaching and dismissing in family interaction. Social Development. 2007;16:232–248. [Google Scholar]
- Magai C. Emotions as a child. Long Island University, New York; 1996. [Google Scholar]
- Magai C, O’Neal CR. Emotions as a child (child version) Long Island University, Brooklyn; 1997. [Google Scholar]
- Malatesta-Magai C. Emotional socialization: Its role in personality and developmental psychopathology. In: Cicchetti DET, Sheree L, editors. Rochester Symposium on Developmental Psychopathology: Vol. 3. Internalizing and externalizing expressions of dysfunction. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1991. pp. 203–224. [Google Scholar]
- Maziade M, Roy MA, Fournier JP, Cliche D, Merette C, Caron C, et al. Reliability of best-estimate diagnosis in genetic linkage studies of major psychoses: Results from the Quebec pedigree studies. American Journal of Psychiatry. 1992;149:1674–1686. doi: 10.1176/ajp.149.12.1674. [DOI] [PubMed] [Google Scholar]
- Mezulis AH, Hyde JS, Clark R. Father involvement moderates the effect of maternal depression during a child’s infancy on child behavior problems in kindergarten. Journal of Family Psychology. 2004;18:575–588. doi: 10.1037/0893-3200.18.4.575. [DOI] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the development of emotion regulation. Social Development. 2007;16:361–388. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Sessa FM, Avenevoli S, Essex MJ. Temperamental vulnerability and negative parenting as interacting of child adjustment. Journal of Marriage and Family. 2002;64:461–471. [Google Scholar]
- Nolen Hoeksema S, Wolfson A, Mumme D, Guskin K. Helplessness in children of depressed and nondepressed mothers. Developmental Psychology. 1995;31:377–387. [Google Scholar]
- O’Neal CR, Magai C. Do parents respond in different ways when children feel different emotions? The emotional context of parenting. Development and Psychopathology. 2005;17:467–487. doi: 10.1017/s0954579405050224. [DOI] [PubMed] [Google Scholar]
- Patterson GR, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. American Psychologist. 1989;44:329–335. doi: 10.1037//0003-066x.44.2.329. [DOI] [PubMed] [Google Scholar]
- Puig-Antich J, Lukens E, Davies M, Goetz D, Brennan-Quattrock J, Todak G. Psychosocial functioning in prepubertal major depressive disorders. I. Interpersonal relationships during the depressive episode. Archives of General Psychiatry. 1985;42:500–507. doi: 10.1001/archpsyc.1985.01790280082008. [DOI] [PubMed] [Google Scholar]
- Ramsden SR, Hubbard JA. Family expressiveness and parental emotion coaching: Their role in children’s emotion regulation and aggression. Journal of Abnormal Child Psychology. 2002;30:657–667. doi: 10.1023/a:1020819915881. [DOI] [PubMed] [Google Scholar]
- Richters JE. Depressed mothers as informants about their children: A critical review of the evidence for distortion. Psychological Bulletin. 1992;112:485–499. doi: 10.1037/0033-2909.112.3.485. [DOI] [PubMed] [Google Scholar]
- Roberts W. The socialization of emotional expression: Relations with prosocial behaviour and competence in five samples. Canadian Journal of Behavioural Science. 1999;31:72–85. [Google Scholar]
- Roberts W, Strayer J. Parents’ reponses to the emotional distress of their children: Relations with children’s competence. Developmental Psychology. 1987;23:415–422. [Google Scholar]
- Rubin KH, Coplan RJ, Fox NA, Calkins SD. Emotionality, emotion regulation, and preschoolers’ social adaptation. Development and Psychopathology. 1995;7:49–62. [Google Scholar]
- Rydell AM, Berlin L, Bohlin G. Emotionality, emotion regulation, and adaptation among 5- to 8-year-old children. Emotion. 2003;3:30–47. doi: 10.1037/1528-3542.3.1.30. [DOI] [PubMed] [Google Scholar]
- Sameroff A. Transactional models in early social relations. Human Development. 1975;18:65–79. [Google Scholar]
- Seifer R. Perils and pitfalls of high-risk research. Developmental Psychology. 1995;31:420–424. [Google Scholar]
- Seifer R, Dickstein S, Sameroff AJ, Magee KD, Hayden LC. Infant mental health and variability of parental depression symptoms. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1375–1382. doi: 10.1097/00004583-200112000-00007. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Keenan K, Vondra JI, Delliquadri E, Giovannelli J. Antecedents of preschool children’s internalizing problems: A longitudinal study of low-income families. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1760–1767. [PubMed] [Google Scholar]
- Sheeber L, Allen N, Davis B, Sorensen E. Regulation of negative affect during mother-child problem-solving interactions: Adolescent depressive status and family processes. Journal of Abnormal Child Psychology. 2000;28:467–479. doi: 10.1023/a:1005135706799. [DOI] [PubMed] [Google Scholar]
- Sherrill JT, Kovacs M. Interview Schedule for Children and Adolescents (ISCA) Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:67–75. doi: 10.1097/00004583-200001000-00018. [DOI] [PubMed] [Google Scholar]
- Silk JS, Shaw D, Skuban E, Oland A, Kovacs M. Emotion regulation strategies among offspring of mothers with childhood onset depression. Journal of Child Psychology & Psychiatry. 2006;47:69–78. doi: 10.1111/j.1469-7610.2005.01440.x. [DOI] [PubMed] [Google Scholar]
- Silk JS, Shaw DS, Forbes EE, Lane TJ, Kovacs M. Maternal depression and child internalizing: the Moderating role of child emotion regulation. Journal of Clinical Child and Adolescent Psychology. 2006;35:116–126. doi: 10.1207/s15374424jccp3501_10. [DOI] [PubMed] [Google Scholar]
- Silk JS, Steinberg L, Morris AS. Adolescents’ emotion regulation in daily life: Links to depressive symptoms and problem behavior. Child Development. 2003;74:1869–1880. doi: 10.1046/j.1467-8624.2003.00643.x. [DOI] [PubMed] [Google Scholar]
- Silk JS, Ziegler ML, Whalen DJ, Dahl RE, Ryan ND, Birmaher B, Axelson DA, Williamson DE. Expressed emotion in mothers of children and adolescents with major depressive disorder and at high familial risk for depressive disorder. Journal of Clinical Child & Adolescent Psychology. 2009;38:36–47. doi: 10.1080/15374410802575339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinrad TL, Eisenberg N, Gaertner B, Popp T, Smith CL, Kupfer A, Greving K, Liew J, Hofer C. Relations of maternal socialization and toddlers’ effortful control to children’s adjustment and social competence. Developmental Psychology. 2007;43:1170–1186. doi: 10.1037/0012-1649.43.5.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinrad TL, Stifter CA, Donelan-McCall N, Turner L. Mothers’ regulation strategies in response to toddlers’ affect: Links to later emotion self-regulation. Social Development. 2004;13:40–55. [Google Scholar]
- Suveg C, Hoffman B, Zeman JL, Thomassin K. Common and specific emotion-related predictors of anxious and depressive symptoms in youth. Child Psychiatry and Human Development. 2008;40:223–239. doi: 10.1007/s10578-008-0121-x. [DOI] [PubMed] [Google Scholar]
- Tarullo LB, DeMulder EK, Martinez PE, Radke Yarrow M. Dialogues with preadolescents and adolescents: Mother-child interaction patterns in affectively ill and well dyads. Journal of Abnormal Child Psychology. 1994;22:33–51. doi: 10.1007/BF02169255. [DOI] [PubMed] [Google Scholar]
- Tomkins SS. Negative affects. Vol. 2. New York: Springer; 1963. Affect, imagery, consciousness. [Google Scholar]
- Wachs TD, Black MM, Engle PL. Maternal depression: A global threat to children’s health, development, and behavior and to human rights. Child Development Perspectives. 2009;3:51–59. [Google Scholar]
- Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to anxiety and depressive disorders. Journal of Abnormal Psychology. 1988;97:346–353. doi: 10.1037//0021-843x.97.3.346. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Fendrich M, Warner V, Wickramaratne P. Incidence of psychiatric disorder in offspring at high and low risk for depression. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:640–648. doi: 10.1097/00004583-199207000-00010. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Gammon GD, John K, Merikangas KR. Children of depressed parents: Increased psychopathology and early onset of major depression. Archives of General Psychiatry. 1987;44:847–853. doi: 10.1001/archpsyc.1987.01800220009002. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Prusoff BA, Gammon GD, Merikangas KR, Leckman JF, Kidd KK. Psychopathology in the children (ages 6–18) of depressed and normal parents. Journal of the American Academy of Child Psychiatry. 1984;23:78–84. doi: 10.1097/00004583-198401000-00011. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Warner V, Wickramaratne P, Moreau D, Olfson M. Offspring of depressed parents: 10 years later. Archives of General Psychiatry. 1997;54:932–940. doi: 10.1001/archpsyc.1997.01830220054009. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Merikangas KR, Leckman JF, Prusoff BA, Caruso KA, Kidd KK, Gammon GD. Onset of major depression in early adulthood: Increased familial loading and specificity. Archives of General Psychiatry. 1984;41:1136–1143. doi: 10.1001/archpsyc.1984.01790230022003. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Verdeli H, Pilowsky DJ, Grillon C, Bruder G. Families at high and low risk for depression: a 3-generation study. Arch Gen Psychiatry. 2005;62:29–36. doi: 10.1001/archpsyc.62.1.29. [DOI] [PubMed] [Google Scholar]
- Wickramaratne P, Weissman M. Onset of psychopathology in offspring by developmental phase and parental depression. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:933–942. doi: 10.1097/00004583-199809000-00013. [DOI] [PubMed] [Google Scholar]
- Wong MS, Diener ML, Isabella RA. Parents’ emotion related beliefs and behaviors and child grade: Associations with children’s perceptions of peer competence. Journal of Applied Developmental Psychology. 2008;29:175–186. [Google Scholar]
- Yap MB, Allen NB, Leve C, Katz LF. Maternal meta-emotion philosophy and socialization of adolescent affect: The moderating role of adolescent temperament. Journal of Family Psychology. 2008;22 doi: 10.1037/a0013104. [DOI] [PubMed] [Google Scholar]