Abstract
Introduction
This study examined the longitudinal association between adolescent psychological problems following cancer treatment and obesity, limited exercise, smoking, and excess sun exposure during adulthood in the Childhood Cancer Survivor Study cohort.
Methods
Participants included 1,652 adolescent survivors of childhood cancer and 406 siblings of cancer survivors, initially evaluated at 12-17 years of age and ≥ 5 years post-diagnosis. A follow-up survey of these participants was conducted roughly 7 years later and included assessment of health status and health behaviors. Logistic regression models were used to assess the association between adolescent psychological problems and adult health behavior outcomes.
Results
During adolescence, survivors demonstrated higher rates of attention deficits, emotional problems, externalizing behavior and social withdrawal compared to sibling controls. Social withdrawal was associated with adult obesity (OR = 1.5, 95% CI = 1.1 - 2.1) and physical inactivity (OR = 1.7, 1.1 - 2.5). Use of stimulant medication during adolescence was also associated with adult obesity (OR = 1.9, 1.1 – 3.2), while antidepressant use was associated with physical inactivity (OR = 3.2, 1.2 – 8.2).
Discussion/Conclusions
Adolescent survivors of childhood cancer display higher rates of psychological problems compared to siblings of cancer survivors. These psychological problems are associated with an increased risk for obesity and poor heath behavior in adulthood, which may increase future risk for chronic health conditions and secondary neoplasms.
Implications
In order to decrease risk of future health problems, adolescent survivors of childhood cancer should be routinely screened and treated for psychological problems following cancer therapy.
Keywords: Adolescence, Cancer, Psychological problems, Obesity, Oncology, Childhood Cancer Survivor Study
Introduction
Adult survivors of childhood cancer are at increased risk for late effects and secondary neoplasms.[1,2] Risk for these late effects is significantly increased by health status and behavior, including obesity, physical inactivity, smoking, and unprotected sun exposure.[3,4] Psychological problems during adolescence have been identified as important risk factors of poor health status and behavior in non-cancer populations. For example, depression and social withdrawal increase risk for obesity[5,6] and physical inactivity,[7-9] while attention deficits and antisocial behavior also increase risk for obesity.[10-13] However, an association between adolescent psychological problems and poor health status and behaviors has not been demonstrated in survivors or childhood cancer.
Adolescent survivors of childhood cancer are at increased risk for psychological problems. In a recent report of over 2,979 long-term survivors between 12-17 years of age, compared to 649 sibling controls, survivors demonstrated increased rates of depression/anxiety, attention deficits, oppositional behavior, and social withdrawal.[14] Survivors of pediatric leukemia and central nervous system (CNS) tumors were at significantly higher risk for these psychological problems compared to other diagnostic groups.
Given the increased prevalence of psychological problems in adolescent cancer survivors, and the association between these problems and poor health status and behaviors in the general population, it is reasonable to expect that psychological problems during adolescence may predict future adverse health outcomes in adult survivors of childhood cancer. The impact of these health behaviors in cancer survivors may be more dramatic than those observed in the general population, given this group's increased risk for late effects, including chronic health conditions.[1,15] The current study aimed to address this issue by examining the association between parent-reported psychological problems in adolescents and self-reported health status and behavior after these adolescents reached adulthood. We hypothesized that symptoms of depression/anxiety, attention deficits, and social problems during adolescence would predict future health status and behaviors in young adulthood.
Method
Participants included 1,652 cancer survivors and a control group of 406 siblings of cancer survivors from the Childhood Cancer Survivor Study (CCSS). The CCSS is a cohort study designed to evaluate the impact of childhood cancer and its treatment on long-term health and function.[16-18] Eligible participants were treated for one of eight childhood cancer diagnoses at 26 institutions between 1970 and 1986 when younger than 21 years of age. Cohort entry was limited to those individuals who survived for at least five years after their original diagnosis. Siblings were recruited from a randomly selected subset of adolescent and adult survivors. The human subjects committee at each of the collaborating institutions approved the study protocol before participant enrollment. Participants provided informed consent for the questionnaires and medical record abstraction. Study participants completed a 24-page Baseline questionnaire between 1995 and 1996, at least five years post their original diagnosis. This questionnaire surveyed sociodemographic information, medical history, and functional limitations. A second Follow-Up questionnaire was initiated in 2003 (the full survey questionnaires are available at http://www.stjude.org/CCSS).
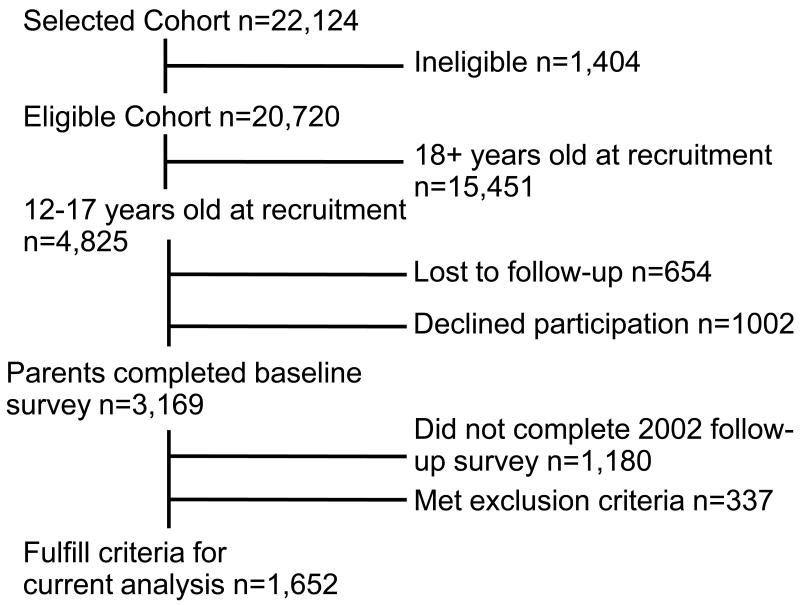
The study population for the current analyses included (1) all cancer survivors and siblings whose parents participated in the Baseline survey when the survivor or sibling was 12-17 years of age, and (2) survivors or siblings who also completed the 2003 Follow-Up survey as adults approximately seven years later. Exclusion criteria included survivors and siblings who were over 17 years of age at the Baseline survey. Participants who reported experiencing a cerebrovascular abnormality, cerebral palsy, paralysis, mental retardation, or epilepsy were also excluded as these neurological conditions were perceived to have the potential to impact health status and behaviors independent of the predictor variables (e.g. requiring parents to regulate health behaviors). In addition, given the inclusion of physical activity and body mass index (BMI) outcomes in this study, four additional survivors with lower limb amputations were also excluded. See Figure 1 for a schematic of patient recruitment.
Figure 1.
Schematic of recruitment of adolescents used in the analyses of this longitudinal study.
The Behavior Problem Index (BPI) was completed by parents as part of the Baseline survey. The BPI is a standardized questionnaire developed for the National Health Survey, and has been normed on a large nationally representative sample.[19] This rating scale was developed as a shortened version of the Child Behavior Checklist,[20] and has been widely used in medical populations and epidemiological studies. For each of the 32 items, parents are asked to rate their child's behavioral and/or emotional functioning using a Likert scale ranging from 1 (“Not True”) to 3 (“Often True”). Factor analyses in the normative sample resulted in five scales: depression/anxiety, headstrong behavior, attention deficit, social withdrawal, and antisocial behavior.[19] This original factor structure has been cross-validated in a large cohort of adolescent survivors of childhood cancer.[14] For the current study, participants were classified according to whether or not they displayed impairment on each of these factors, with impairment defined as having a level of problematic symptoms that occur in ≤ 10% of the original normative standardization sample.[19]
Adult weight status and health behavior outcomes were collected during the 2003 Follow-Up survey. Body mass index (BMI) was calculated to indicate weight status. In order to adjust for adolescent BMI, height and weight was also obtained during the Baseline survey and was compared to national norms,[21] and classified as follows: underweight = BMI < 5th percentile, normal weight = BMI 5th–84th percentile, overweight = BMI 85th–94th percentile; and obese = BMI ≥ 95th percentile. During adulthood BMI classifications were defined as follows: underweight = BMI < 18.5, normal weight = BMI 18.5–24.9; overweight = BMI 25–29.9; obese = BMI ≥ 30. Health behavior variables included physical activity, smoking, and sunscreen use. Health behaviors were selected based on those behaviors associated with increased risk for chronic health impairment and/or secondary neoplasm. Physical activity was measured in weekly minutes of moderate and vigorous physical exercise, and was dichotomized according to whether or not the participant met national standards established by the Centers for Disease Control (CDC), with “Inactivity” defined as falling below the recommended guidelines.[22]. Adult participants were identified as a smoker if they reported currently smoking and smoking at least 100 cigarettes over their lifetime. Poor sunscreen use was defined as reporting “never”, “rarely”, or only “sometimes” using sunscreen when exposed to the sun for more than 15 minutes.
Logistic regression models formed the basis for all statistical approaches. A multinomial logit model was used to assess the association between the five BPI factors and BMI categories as adults. Given the small number of survivors in the underweight category, this group was combined with the normal weight category to examine predictors of obesity. Logistic regression models were used to assess the association between the five BPI factors and each of the three health behavior outcomes (i.e. physical activity, smoking, and sunscreen). Models were constructed using both survivor and sibling data to compare participant status. Separate models were then constructed for survivors only in order to include diagnosis and treatment variables. Full models for the survivor group comprise the majority of the results discussed below. For all survivor analyses, covariates included cancer diagnosis (i.e. leukemia vs. CNS tumor vs. other cancers [Hodgkin's disease, non-Hodgkin's lymphoma, Wilms' tumor, neuroblastoma, and soft tissue sarcoma]), cancer therapy (i.e. cranial radiation vs. non-cranial radiation; CNS chemotherapy vs. no CNS chemotherapy), sex, and psychotropic medication history (i.e. antidepressants, stimulants). For the BMI outcome model, BMI at adolescence was also included as a covariate. The presence of adult chronic health conditions was included as a covariate for the physical activity outcome. Avoidance of sun exposure (e.g. wearing protective clothing, staying in the shade) was used as a covariate for use of sunscreen.
Results
Table I presents the characteristics of the survivor and sibling samples. Significantly more survivors than siblings were classified as having attention deficits, antisocial behavior, depression/anxiety, headstrong behavior, and social withdrawal. Noted in these percentages is the fact that the rate of impairment in the siblings does not substantially differ from the 10% rate determined in the original normative standardization sample. A similar small percentage of survivors and siblings were reported to be taking stimulant medication (2.9% of survivors and 2.0% of siblings) or anti-depressants (1.9% of survivors and 1.7% of siblings). This similarity in rate of medication usage is surprising in light of the nearly two-fold increase in rates of survivor attention and emotional problems. Although the rate of stimulant and anti-depressant medication use is low, a closer examination reveals that use did not correspond to adolescent symptoms of specific behavioral problems (see Table II). A substantial proportion of survivors using stimulants were also reported to demonstrate internalizing and externalizing problems, while a majority of adolescent survivors using anti-depressants were reported to demonstrate social withdrawal as well as depression/anxiety.
Table I.
Characteristics of adolescent survivor and sibling samples.
| Survivors (N=1652) |
Siblings (N=406) |
P-value | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Sex | 0.59 | ||||
| Male | 814 | 49.3 | 194 | 47.8 | |
| Female | 838 | 50.7 | 212 | 52.2 | |
| Attention deficit* | <.01 | ||||
| Yes | 313 | 19.0 | 46 | 11.3 | |
| No | 1339 | 81.0 | 360 | 88.7 | |
| Antisocial behaviors* | <.01 | ||||
| Yes | 203 | 12.3 | 30 | 7.4 | |
| No | 1449 | 87.7 | 376 | 92.6 | |
| Depression/Anxiety* | <.01 | ||||
| Yes | 282 | 17.1 | 37 | 9.1 | |
| No | 1370 | 82.9 | 369 | 90.9 | |
| Headstrong behavior* | <.01 | ||||
| Yes | 218 | 13.2 | 33 | 8.1 | |
| No | 1434 | 86.8 | 373 | 91.9 | |
| Social withdrawal* | <.01 | ||||
| Yes | 348 | 21.1 | 40 | 9.9 | |
| No | 1304 | 78.9 | 366 | 90.2 | |
| Stimulant | 0.30 | ||||
| Yes | 48 | 2.9 | 8 | 2.0 | |
| No | 1604 | 97.1 | 398 | 98.0 | |
| Anti-depressants | 0.78 | ||||
| Yes | 32 | 1.9 | 7 | 1.7 | |
| No | 1620 | 98.1 | 399 | 98.3 | |
| Diagnosis | NA | ||||
| Leukemia | 790 | 47.8 | NA | NA | |
| CNS tumor | 150 | 9.1 | NA | NA | |
| Other | 712 | 43.1 | NA | NA | |
| Cranial Radiation | NA | ||||
| Yes | 452 | 27.4 | NA | NA | |
| No | 1084 | 65.6 | NA | NA | |
| Unknown | 116 | 7.0 | NA | NA | |
| Chronic Disease Status** | <.01 | ||||
| Grade 0 | 880 | 53.3 | 336 | 82.8 | |
| Grade 1 & 2 | 569 | 34.4 | 62 | 15.3 | |
| Grade 3 & 4 | 203 | 12.3 | 8 | 2.0 | |
| Age at 2003 Follow-up | Mean (SD) | Range | Mean (SD) | Range | |
| 22.8 (1.9) | 18-27 | 22.2 (1.8) | 18-26 | ||
Yes category represents a symptom level reported in ≤10% of a national normative sample.
chronic disease at baseline (severity determined using the scoring system used by Oeffinger, et al. based on the Common Terminology Criteria for Adverse Events (CTCAE) version 3 and the scoring system developed by the National Cancer Institute).
Table II.
Percent of adolescents demonstrating impairment on scales from the Behavior Problem Inventory who were reported to be taking stimulant and/or anti-depressants.
| Stimulants | Anti-depressants | |||
|---|---|---|---|---|
| Survivors (n=48) |
Siblings (n=8) |
Survivors (n=32) |
Siblings (n=7) |
|
| Adolescent Behavior Problems | N (%) | N (%) | N (%) | N (%) |
| Attention Deficit | 39 (81.3) | 6 (75.0) | 18 (56.3) | 4 (57.1) |
| Antisocial Behavior | 21 (43.8) | 0 (0.0) | 10 (31.3) | 2 (28.6) |
| Depression/Anxiety | 26 (54.2) | 3 (37.5) | 22 (68.8) | 3 (42.9) |
| Headstrong Behavior | 27 (56.3) | 2 (25.0) | 11 (34.4) | 3 (42.9) |
| Social Withdrawal | 31 (64.6) | 2 (25.0) | 23 (71.9) | 2 (28.6) |
The percentage of survivors falling within each BMI classe changed from adolescence to adulthood. Although during adolescence 73.7% of survivors and 82.7% of siblings exhibited a BMI in the normal range, this number decreased to 56.9% for survivors and 64.6% for siblings during follow-up as adults. At adolescence, 14.8% of survivors and 10.5% of siblings fell in the overweight range and 11.5% of survivors and 6.8% of siblings were in the obese BMI range. As adults, 25.6% of survivors and 23.4% siblings were overweight and 17.5% of survivors and 12.1% of siblings were obese. After controlling for adolescent weight status, no significant differences were observed between survivors and siblings in risk of adult obesity (OR=1.1, 95% CI=0.9-1.5). Table III presents the results of the Multinomial logit model used to predict the increase in BMI from adolescence to adulthood for the survivor group. Social withdrawal during adolescence increased the risk for adult obesity. This 50% increased risk was present after adjusting for the increased risk associated with being overweight or obese as an adolescent. Use of stimulant medication during adolescence was associated with an increased risk for obesity in adulthood.
Table III.
Multi-variable model to predict the likelihood of being overweight or obese as an adult.
| Overweight** | Obese** | P-value | |||
|---|---|---|---|---|---|
| OR | 95%CL | OR | 95%CL | ||
| Adolescent Behavior Problem* | |||||
| Attention deficit | 1.0 | 0.8-1.3 | 1.0 | 0.7-1.3 | 0.98 |
| Social Withdrawal | 1.3 | 1.0-1.6 | 1.5 | 1.1-2.1 | 0.04 |
| Antisocial behaviors | 0.9 | 0.7-1.3 | 0.8 | 0.5-1.2 | 0.53 |
| Depression/anxiety | 0.8 | 0.6-1.0 | 0.8 | 0.6-1.2 | 0.18 |
| Headstrong behaviors | 1.0 | 0.7-1.3 | 1.1 | 0.7-1.6 | 0.80 |
| Adolescent Medication Use | |||||
| Stimulant Mediation | 1.3 | 0.9-2.0 | 1.9 | 1.2-3.2 | 0.04 |
| Sex (Female) | 0.7 | 0.6-0.8 | 1.1 | 0.9-1.3 | <.01 |
| Cranial Radiation | 1.0 | 0.9-1.2 | 1.2 | 0.9-1.5 | 0.48 |
| Diagnosis | 0.25 | ||||
| Leukemia vs. Other | 1.2 | 1.0-1.5 | 0.9 | 0.6-1.3 | |
| CNS tumor vs. Other | 0.9 | 0.6-1.2 | 0.8 | 0.6-1.1 | |
| Baseline BMI*** | <.01 | ||||
| Overweight vs. Normal | 1.6 | 1.1-2.3 | 1.5 | 1.1-2.2 | |
| Obese vs. Normal | 2.6 | 1.6-4.2 | 10.0 | 6.2-15.9 | |
| Chronic Disease Score**** | 0.12 | ||||
| Grade 1&2 vs. Grade 0 | 0.9 | 0.7-1.1 | 0.8 | 0.6-1.1 | |
| Grade 3&4 vs. Grade 0 | 1.0 | 0.8-1.3 | 0.9 | 0.6-1.3 | |
Yes category represents a symptom level reported in ≤10% of a national normative sample.
Defined during adulthood as Normal weight = BMI < 25, Overweight = BMI 25 to < 30, Obese = BMI ≥ 30.
Defined during adolescence as: Normal weight ≤ 84th percentile, Overweight = 85th - 94th percentile, Obese ≥ 95th percentile.
chronic disease at baseline (severity determined using the scoring system used by Oeffinger, et al. based on the Common Terminology Criteria for Adverse Events (CTCAE) version 3 and the scoring system developed by the National Cancer Institute).
A substantial percentage of adult survivors reported physical inactivity. Although survivors were not at increased risk compared to siblings (OR=0.9, 95% CI=0.7-1.1), physical inactivity in survivors carries increased risk for late effects. Table IV presents the results of a multiple variable logistic regression model for prediction of physical inactivity in the adult survivors of childhood cancer. Social withdrawal and use of anti-depressants were associated with increased risk for physical inactivity as an adult. These risks were significant even when controlling for other demographic and disease factors, including adolescent obesity and having a chronic disease during adulthood.
Table IV.
Multi-variable model to predict the likelihood of physical inactivity as an adult.
| OR | 95% CI | P-value | |
|---|---|---|---|
| Adolescent Behavior Problem* | |||
| Attention Deficit | 0.9 | 0.7-1.3 | 0.71 |
| Antisocial Behavior | 0.9 | 0.5-1.4 | 0.56 |
| Depression/Anxiety | 0.8 | 0.5-1.2 | 0.26 |
| Headstrong Behavior | 1.1 | 0.7-1.8 | 0.64 |
| Social Withdrawal | 1.7 | 1.1-2.5 | 0.01 |
| Adolescent Medication Use | |||
| Anti-depressants | 3.2 | 1.2-8.3 | 0.02 |
| Stimulant | 1.2 | 0.6-2.4 | 0.54 |
| Sex (Female) | 1.4 | 1.1-1.7 | <.01 |
| Cranial Radiation | 1.1 | 0.8-1.4 | 0.72 |
| Diagnosis | 0.14 | ||
| Leukemia vs. Other | 0.8 | 0.7-1.1 | |
| CNS tumor vs. Other | 1.2 | 0.8-1.8 | |
| BMI** | <.01 | ||
| Underweight vs. Normal | 2.5 | 1.5-4.1 | |
| Overweight vs. Normal | 1.0 | 0.7-1.2 | |
| Obese vs. Normal | 1.6 | 1.2-2.1 | |
| Chronic Disease*** | 0.10 | ||
| Grade 1&2 vs. Grade 0 | 1.3 | 1.0-1.6 | |
| Grade 3&4 vs. Grade 0 | 1.3 | 0.9-1.8 |
Yes category represents a symptom level reported in ≤10% of a national normative sample.
Defined during adolescence as: Underweight <5th percentile, Normal weight 5th- 84th percentile, Overweight 85th - 94th percentile, Obese ≥ 95th percentile.
chronic disease at baseline (severity determined using the scoring system used by Oeffinger, et al. based on the Common Terminology Criteria for Adverse Events (CTCAE) version 3 and the scoring system developed by the National Cancer Institute).
More than half of the survivors reported limited or no sunscreen use as an adult. Again, although survivors were not at increased risk compared to siblings (OR=0.9, 95% CI=0.7-1.2), limited sunscreen use in cancer survivors may carry a greater relative risk given the already higher risk of skin cancer in survivors. Table V presents the results of a multiple variable logistic regression model for prediction of unhealthy sun exposure. Although none of the five categories of adolescent behavioral problems were associated with lower sunscreen use as an adult, adolescents who were treated with stimulant medication were less likely to engage in unprotected sun exposure.
Table V.
Multi-variable model to predict the likelihood of poor sunscreen use as an adult.
| OR | 95% CI | P-value | |
|---|---|---|---|
| Adolescent Behavior Problem* | |||
| Attention Deficit | 1.4 | 1.0-2.0 | 0.06 |
| Antisocial Behavior | 1.6 | 1.0-2.5 | 0.06 |
| Depression/Anxiety | 1.1 | 0.7-1.7 | 0.67 |
| Headstrong Behavior | 1.1 | 0.7-1.8 | 0.65 |
| Social Withdrawal | 0.8 | 0.6-1.2 | 0.33 |
| Adolescent Medication Use | |||
| Anti-depressants | 2.2 | 0.9-5.5 | 0.09 |
| Stimulant | 0.4 | 0.2-0.8 | 0.01 |
| Sex (Female) | 0.5 | 0.4-0.7 | <.01 |
| Cranial Radiation | 0.8 | 0.6-1.0 | 0.07 |
| Diagnosis | 0.85 | ||
| Leukemia vs. Other | 0.9 | 0.7-1.2 | |
| CNS tumor vs. Other | 1.0 | 0.7-1.6 | |
| Other Sun Protection | <.01 | ||
| Sometimes vs. often/always | 1.7 | 1.3-2.2 | |
| Never/rarely vs. often/always | 5.0 | 3.4-7.3 |
Yes category represents a symptom level reported in ≤10% of a national normative sample.
Although the rate of smoking in adult survivors was lower than that reported in siblings (OR=0.6, 95% CI=0.5-0.8), the potential risk associated with smoking is magnified by virtue of the history of childhood cancer. Table VI presents the results of a model for prediction of being classified as a regular adult smoker. Adolescent antisocial behavior increased the risk for smoking during adulthood. This increased risk was significant even when controlling for risks associated with other demographic and disease characteristics. Survivors with a history of cranial radiation therapy were less likely to report smoking as an adult compared to survivors not treated with cranial radiation.
Table VI.
Multi-variable model to predict the likelihood of smoking as an adult.
| OR | 95% CI | P-value | |
|---|---|---|---|
| Adolescent Behavior Problem* | |||
| Attention Deficit | 1.4 | 1.0-2.1 | 0.07 |
| Antisocial Behavior | 2.6 | 1.6-4.2 | <.01 |
| Depression/Anxiety | 1.4 | 0.8-2.3 | 0.19 |
| Headstrong Behavior | 1.3 | 0.8-2.2 | 0.30 |
| Social Withdrawal | 0.7 | 0.4-1.1 | 0.10 |
| Adolescent Medication Use | |||
| Anti-depressants | 2.0 | 0.9-4.5 | 0.10 |
| Stimulant | 0.8 | 0.4-1.6 | 0.50 |
| Sex (Female) | 0.8 | 0.6-0.9 | 0.03 |
| Cranial Radiation | 0.6 | 0.4-0.8 | <.01 |
| Diagnosis | 0.30 | ||
| Leukemia vs. Other | 1.2 | 0.9-1.6 | |
| CNS tumor vs. Other | 0.8 | 0.5-1.4 |
Yes category represents a symptom level reported in ≤10% of a national normative sample.
Discussion
Long-term survivors of childhood cancer that experience psychological problems during adolescence, following cancer therapy, are at increased risk for obesity and poor health behaviors as young adults. A previous report from CCSS identified adolescent survivors of leukemia and CNS tumors at highest risk for psychological problems following cancer therapy.[14] The current results extend those findings to suggest that the increased rates of psychological problems during adolescence place the adult survivors at increased risk for chronic health problems as they age. The association between adolescent psychological problems and adult health status in long-term survivors of childhood cancer is similar to that seen in non-cancer populations. However, the impact of such behaviors in cancer survivors is potentially more problematic.[3] Compared to siblings and the general population, survivors of childhood cancer are already at increased risk for heart disease and second malignant neoplasms.[1] The additional risk associated with obesity and poor health behaviors may be cumulative and further increase risk in these individuals. Early identification and treatment of the adolescent psychological problems that predict adult obesity and poor health behaviors may be a strategy for overall risk reduction.
Adolescents who are long-term survivors of childhood cancer demonstrate significantly higher rates of inattention, social withdrawal, emotional problems, and externalizing problems compared to their siblings. However, relatively few of the survivors are reported to be treated with stimulant medication or anti-depressants. This reduced reliance on medication management of psychological problems may reflect the limited available information on efficacy of such treatment in child survivors of chronic disease. Few randomized controlled trials provide support for successful medication management in child cancer survivors, or other populations of chronically ill children.[23] Furthermore, as evident in Table II, adolescent survivors of childhood cancer who are prescribed either stimulants or anti-depressants demonstrate a complex symptom pattern. Significant problems with social withdrawal were reported in roughly 65% of the adolescents prescribed stimulants and 72% of those prescribed anti-depressants. In addition, nearly half of the stimulant users were reported to experience significant emotional problems and externalizing behaviors, and over half of the adolescents using anti-depressants were reported to have significant attention problems. This co-morbid symptom profile combined with the history of cancer and chemotherapy may be associated with a relative under reliance on typical treatment options.
Survivors of childhood cancer are at increased risk for adult obesity, specifically those that are treated with cranial radiation.[24] However, in the current study, the increased rate of change in BMI of survivors was not significantly different from the rates seen in siblings. This apparent discrepancy is likely due to the fact that previous studies focused on outcome of therapy, while the current study examined longitudinal change from adolescence to young adulthood. Thus, the effect of cranial radiation is present in the adolescent BMI, which was used as a covariate in the current analyses. Significant social withdrawal during adolescence was associated with a 50% increased risk for adult obesity. Although the rate of stimulant medication use during adolescence was small, such use was associated with a 90% increase in adult obesity. However, as noted earlier 65% of the adolescents who were reported to be using stimulant medication were also reported to display significant symptoms of social withdrawal.
Social withdrawal during adolescence was also associated with a 70% increased risk for not meeting CDC exercise guidelines. Similar to the impact on adult obesity, adolescent medication use was associated with this physical inactivity. Specifically, use of anti-depressants was associated with a three-fold increased risk of being physically inactive as an adult. However, readers should be cautioned that this risk is based on a very small number of adolescents who used anti-depressants. Again, the impact of social withdrawal and use of medication during adolescence was significant even when controlling for cancer diagnosis, cranial radiation therapy, adolescent BMI and the presence of a chronic disease during adulthood. Existing research does support the link between use of anti-depressants and increased risk for obesity and physical inactivity in depressed populations.[5,6] Current results extend this finding to survivors of a chronic disease of childhood. Furthermore, as the risk factors appear present during childhood, early intervention to prevent adverse health outcomes in adulthood may be possible.
Individuals that experience internalizing psychological problems, including social withdrawal, are also reported to be at increased risk for cardiovascular disease.[25,26] Although this cardiac outcome was not assessed in the current study, the association between cardiovascular disease, obesity, and physical inactivity warrants follow-up examination in these individuals with social withdrawal. Furthermore, given the evaluated rate of social withdrawal previously reported in survivors of pediatric leukemia,[14] and the fact that these survivors are treated with anthracyclines that may place them are additional risk for cardiomyopathy,[27] the interaction between specific chemotherapy treatment exposure and problems with social withdrawal should be further examined.
Survivors who displayed antisocial behavior during adolescence had a nearly three-fold increase risk of adult smoking. Again, this pattern did not significantly differ from siblings and is similar to that seen in adolescents in the general population.[28] Although many of these adult survivors were likely to be smoking as an adolescent, the accuracy of adolescent report of smoking is unreliable,[29] particularly in cancer survivors who are repeatedly educated about the risks associated with such behavior. Given the strong association between smoking and parent reported antisocial behavior, this behavior may be a good marker to identify those in need of smoking prevention or cessation interventions.
Adolescent behavior problems did not significantly predict future frequency of sunscreen use. Adolescents who used stimulant medication and females were more likely to engage in appropriate sun protection. As little information is available about this risky behavior category, it deserves attention in future studies.
Implications
These results reinforce the need for routine screening for psychological problems in survivors of childhood cancer and the need for development of intervention approaches. Undiagnosed and untreated psychological problems during adolescence appear to increase the risk for poor health status and poor health behavior outcomes. Targeted interventions for psychological problems may not only increase adolescent quality of life, but may also decrease the risk for development of negative health behaviors that are associated with future chronic disease and subsequent cancers. For example, cognitive and behavior therapy has been demonstrated to improve emotional and attention problems in adolescents,[30,31] while social skills training has demonstrated efficacy in reversing social withdrawal.[32] Delivery of these interventions during early survivorship may improve long-term health and quality of life among survivors of childhood cancer.
Acknowledgments
This work was supported by the National Cancer Institute (U24-CA55727, L. L. Robison) and the American Lebanese-Syrian Associated Charities (ALSAC).
Footnotes
No authors report conflict of interest.
References
- 1.Bassal M, Mertens AC, Taylor L, et al. Risk of selected subsequent carcinomas in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2006;24(3):476–483. doi: 10.1200/JCO.2005.02.7235. [DOI] [PubMed] [Google Scholar]
- 2.Oeffinger KC, Mertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355(15):1572–1582. doi: 10.1056/NEJMsa060185. [DOI] [PubMed] [Google Scholar]
- 3.Hudson MM, Findlay S. Health-risk behaviors and health promotion in adolescent and young adult cancer survivors. Cancer. 2006;107(7 Suppl):1695–1701. doi: 10.1002/cncr.22103. [DOI] [PubMed] [Google Scholar]
- 4.Nathan PC, Ford JS, Henderson TO, et al. Health behaviors, medical care, and interventions to promote healthy living in the Childhood Cancer Survivor Study cohort. J Clin Oncol. 2009;27(14):2363–2373. doi: 10.1200/JCO.2008.21.1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cuijpers P, Schoevers RA. Increased mortality in depressive disorders: a review. Curr Psychiatry Rep. 2004;6(6):430–437. doi: 10.1007/s11920-004-0007-y. [DOI] [PubMed] [Google Scholar]
- 6.Lauder W, Mummery K, Jones M, et al. A comparison of health behaviours in lonely and non-lonely populations. Psychol Health Med. 2006;11(2):233–245. doi: 10.1080/13548500500266607. [DOI] [PubMed] [Google Scholar]
- 7.Mental health in the United States: health risk behaviors and conditions among persons with depression--new Mexico, 2003. MMWR Morb Mortal Wkly Rep. 2005;54(39):989–991. [PubMed] [Google Scholar]
- 8.Vickers KS, Nies MA, Patten CA, et al. Patients with diabetes and depression may need additional support for exercise. Am J Health Behav. 2006;30(4):353–362. doi: 10.5555/ajhb.2006.30.4.353. [DOI] [PubMed] [Google Scholar]
- 9.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32(5):963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Campbell BC, Eisenberg D. Obesity, attention deficit-hyperactivity disorder and the dopaminergic reward system. Coll Antropol. 2007;31(1):33–38. [PubMed] [Google Scholar]
- 11.Hubel R, Jass J, Marcus A, et al. Overweight and basal metabolic rate in boys with attention-deficit/hyperactivity disorder. Eat Weight Disord. 2006;11(3):139–146. doi: 10.1007/BF03327559. [DOI] [PubMed] [Google Scholar]
- 12.Johnson JG, Cohen P, Kasen S, et al. Personality disorder traits evident by early adulthood and risk for eating and weight problems during middle adulthood. Int J Eat Disord. 2006;39(3):184–192. doi: 10.1002/eat.20223. [DOI] [PubMed] [Google Scholar]
- 13.Pickering RP, Grant BF, Chou SP, et al. Are overweight, obesity, and extreme obesity associated with psychopathology? Results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2007;68(7):998–1009. doi: 10.4088/jcp.v68n0704. [DOI] [PubMed] [Google Scholar]
- 14.Schultz KA, Ness KK, Whitton J, et al. Behavioral and social outcomes in adolescent survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol. 2007;25(24):3649–3656. doi: 10.1200/JCO.2006.09.2486. [DOI] [PubMed] [Google Scholar]
- 15.Hudson MM, Mulrooney DA, Bowers DC, et al. High-Risk Populations Identified in Childhood Cancer Survivor Study Investigations: Implications for Risk-Based Surveillance. J Clin Oncol. 2009 doi: 10.1200/JCO.2008.21.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robison LL, Mertens AC, Boice JD, et al. Study design and cohort characteristics of the Childhood Cancer Survivor Study: a multi-institutional collaborative project. Med Pediatr Oncol. 2002;38(4):229–239. doi: 10.1002/mpo.1316. [DOI] [PubMed] [Google Scholar]
- 17.Robison LL, Armstrong GT, Boice JD, et al. The Childhood Cancer Survivor Study: A National Cancer Institute-Supported Resource for Outcome and Intervention Research. J Clin Oncol. 2009 doi: 10.1200/JCO.2009.22.3339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leisenring WM, Mertens AC, Armstrong GT, et al. Pediatric Cancer Survivorship Research: Experience of the Childhood Cancer Survivor Study. J Clin Oncol. 2009 doi: 10.1200/JCO.2008.21.1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zill N, Peterson J. Behavior Problems Index. Washington, DC: Child Trends Inc.; 1986. [Google Scholar]
- 20.Achenbach TM. Manual for the Child Behavior Checklist. Burlington: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 21.National Center for Health Statistics. Centers for Disease Control; [Accessed October 15, 2008]. 2000 CDC Growth Charts: United States. http://www.cdc.gov/growthcharts. [Google Scholar]
- 22.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. Jama. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 23.Butler RW, Mulhern RK. Neurocognitive interventions for children and adolescents surviving cancer. J Pediatr Psychol. 2005;30(1):65–78. doi: 10.1093/jpepsy/jsi017. [DOI] [PubMed] [Google Scholar]
- 24.Garmey EG, Liu Q, Sklar CA, et al. Longitudinal changes in obesity and body mass index among adult survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2008;26(28):4639–4645. doi: 10.1200/JCO.2008.16.3527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Urizar GG, Jr, Sears SF., Jr Psychosocial and cultural influences on cardiovascular health and quality of life among Hispanic cardiac patients in South Florida. J Behav Med. 2006;29(3):255–268. doi: 10.1007/s10865-006-9050-y. [DOI] [PubMed] [Google Scholar]
- 26.Luttik ML, Jaarsma T, Moser D, et al. The importance and impact of social support on outcomes in patients with heart failure: an overview of the literature. J Cardiovasc Nurs. 2005;20(3):162–169. doi: 10.1097/00005082-200505000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Krischer JP, Epstein S, Cuthbertson DD, et al. Clinical cardiotoxicity following anthracycline treatment for childhood cancer: the Pediatric Oncology Group experience. J Clin Oncol. 1997;15(4):1544–1552. doi: 10.1200/JCO.1997.15.4.1544. [DOI] [PubMed] [Google Scholar]
- 28.Faraone SV, Biederman J, Spencer T, et al. Attention-deficit/hyperactivity disorder in adults: an overview. Biol Psychiatry. 2000;48(1):9–20. doi: 10.1016/s0006-3223(00)00889-1. [DOI] [PubMed] [Google Scholar]
- 29.Klosky JL, Tyc VL, Garces-Webb DM, et al. Emerging issues in smoking among adolescent and adult cancer survivors: a comprehensive review. Cancer. 2007;110(11):2408–2419. doi: 10.1002/cncr.23061. [DOI] [PubMed] [Google Scholar]
- 30.Munoz-Solomando A, Kendall T, Whittington CJ. Cognitive behavioural therapy for children and adolescents. Curr Opin Psychiatry. 2008;21(4):332–337. doi: 10.1097/YCO.0b013e328305097c. [DOI] [PubMed] [Google Scholar]
- 31.Butler RW, Copeland DR, Fairclough DL, et al. A multicenter, randomized clinical trial of a cognitive remediation program for childhood survivors of a pediatric malignancy. J Consult Clin Psychol. 2008;76(3):367–378. doi: 10.1037/0022-006X.76.3.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blakeney P, Thomas C, Holzer C, 3rd, et al. Efficacy of a short-term, intensive social skills training program for burned adolescents. J Burn Care Rehabil. 2005;26(6):546–555. doi: 10.1097/01.bcr.0000185455.81677.a2. [DOI] [PubMed] [Google Scholar]