Abstract
Cancer immunotherapy aims to establish immune-mediated control of tumor growth by priming T-cell responses to target tumor-associated antigens. Three signals are required for T-cell activation: (i) presentation of cognate antigen in self MHC molecules; (ii) costimulation by membrane-bound receptor-ligand pairs; and (iii) soluble factors to direct polarization of the ensuing immune response. The ability of dendritic cells (DCs) to provide all three signals required for T-cell activation makes them an ideal cancer vaccine platform. Several strategies have been developed to enhance and control antigen presentation, costimulation, and cytokine production. In this review, we discuss progress toward developing DC-based cancer vaccines by genetic modification using RNA, DNA, and recombinant viruses. Furthermore, the ability of DC-based vaccines to activate natural killer (NK) and B-cells, and the impact of gene modification strategies on these populations is described. Clinical trials using gene-modified DCs have shown modest results, therefore, further considerations for DC manipulation to enhance their clinical efficacy are also discussed.
Introduction
The idea of treating cancer patients with antigen-specific immunotherapy has matured over the past 120 years. At the end of the 19th century, Coley noticed that some tumors could regress in cancer patients who contracted bacterial infections.1 About 15 years later Ehrlich suggested that transformed cells continuously arise in our bodies which the immune system is able to recognize and eliminate before they are clinically detectable.2 In the mid-20th century, Burnet and Thomas provided experimental evidence for the concept of immune surveillance, showing that tumors could be repressed by the immune system in tumor transplantation models.3 This concept was later substantiated by the identification of tumor-associated antigens (TAAs)4 and the isolation of TAA-specific tumor-infiltrating lymphocytes.5 These findings logically led to the hypothesis that the immune system could be further primed for the treatment of cancer.
The induction of antigen-specific immune responses requires potent interactions between antigen-specific T-cells and professional antigen-presenting cells (APCs), including monocytes, macrophages, and dendritic cells (DCs). It is generally accepted that three signals are required for the induction of robust T-cell responses; all three can be delivered by DCs. The first signal consists of the recognition of an antigenic peptide in the context of MHC molecules on APCs through a specific T-cell receptor.6 The second signal is given by interactions between costimulatory ligands on the T-cells and their receptors on APCs.7 In the absence of signal two, antigen-specific T-cells will become anergic. The third signal, established by the local cytokine milieu, influences T-cell polarization.8,9 When all the necessary signals are present, the interaction between DCs and T-cells leads to T-cell activation, clonal expansion, and differentiation into effector and memory cells.
Immature DCs residing in the peripheral tissues are specialized in antigen capture and processing from invading pathogens. In the presence of ongoing inflammatory immune responses, immature DCs respond to inflammatory and pathogen-derived signals by differentiating into a mature state. At this stage, DCs reduce their antigen uptake/processing capacity and transform into efficient APCs capable of stimulating both CD4+ and CD8+ T-cells. To this end, DCs undergo several morphological, phenotypical, and functional changes: (i) they become more motile and increase their CCR7 expression, which controls the migration from the periphery to the lymphoid organs; (ii) they increase their expression of MHC class I and II molecules and of costimulatory molecules (CD40, CD80, CD83, CD86); (iii) upon arrival in the secondary lymphoid organs, they secrete chemokines to recruit macrophages, natural killer (NK) cells, B-cells, additional DC subsets, and specific T-cell subsets to the local environment; and (iv) they secrete cytokines which are critical for determining the nature of the ensuing immune response. Over the years, multiple protocols have been developed for in vitro generation of mature DCs10 and for their genetic modification,11 both through viral and nonviral approaches.
DCs are being modified to express TAAs or immune-potentiating molecules, or to downregulate negative modulators of DC functioning, with the goal of strengthening the three distinct signals required for CD4+ and CD8+ T-cell activation. This review will focus on the genetic modification of DCs to enhance each of these three pathways.
Genetic Modification to Enhance Antigen Delivery for T-Cell Receptor Stimulation (Signal 1)
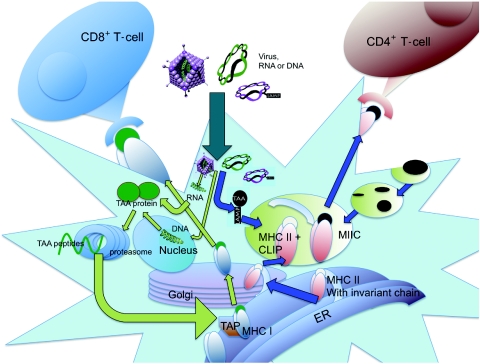
A major advantage of engineering DCs for expression of TAAs is that it allows multi-epitope presentation of full-length TAAs without requiring knowledge of the patient's human leukocyte antigen (HLA) type, unlike widely used peptide vaccination strategies. Secondly, presentation of TAA-derived peptides might be intrinsically enhanced due to their endogenous expression within DCs. Finally, high-efficiency of gene transfer ensures a sufficient, continuous supply of natively processed antigen. Besides these inherent enhancements, several approaches have been utilized to further improve antigen delivery for T-cell receptor stimulation. They can be subdivided into methods that enhance CD8+ T-cell stimulation or CD4+ T-cell stimulation (Figure 1).
Figure 1.
Pathways of antigen processing and presentation. Endogenous proteins are degraded in the cytoplasm by the proteasome. Cleaved peptides are ushered into the endoplasmic reticulum by TAP (transporter associated with antigen processing), where they are loaded onto preformed MHC I/β2m complexes. Stable MHC I:peptide binding allows the complexes to traffic via the Golgi to the cell surface for antigen presentation to CD8+ T-cells. MHC II molecules are formed in the endoplasmic reticulum (ER) and traffic through the Golgi. The invariant chain is used to prevent binding of “self” peptides and to stabilize the MHC II complex. Upon entry into the MHC II compartments (MIIC), the invariant chain is degraded, leaving a small, class II-associated peptide (CLIP). Within the MIIC, the CLIP is replaced with peptides resulting from degradation of endocytosed pathogens. For ectopic expression, genes can be introduced by virus infection or RNA/DNA transfection. Unless otherwise modified, proteins expressed by either strategy are typically processed by the proteasome and presented on MHC I molecules. However, proteins can be also targeted to the MHC II pathway by tagging with sorting signals, including lysosome-associated membrane protein-1 (LAMP-1). TAA, tumor-associated antigen.
When DCs are genetically modified for TAA production, these proteins are generated in the cytoplasm. In order to obtain presentation of TAA derived peptides to CD8+ T-cells, these proteins must be degraded by the proteasome (Figure 1). In most cases, this occurs through protein ubiquitinylation and subsequent targeting to the proteasome. Several proteins such as ornithine decarboxylase, p53, and thymidylate synthase can additionally target proteins for proteasomal degradation through an ubiquitinylation-independent system.12 Antigens are degraded by the proteasome into short peptides which are subsequently transported into the endoplasmic reticulum (ER) by transporter associated with antigen processing. There, newly synthesized HLA class I heavy chains assemble with β2m and peptide and this complex is transported to the cell surface for presentation to CD8+ T-cells, as depicted in Figure 1.
The MHC I pathway has been exploited to enhance antigen presentation. For instance, linking the mRNA for pp65 to ubiquitin or ornithine decarboxylase to enhanced stimulation of CD8+ T-cells. Moreover, when the antigen was linked to both ubiquitin and ornithine decarboxylase, immunogenicity was further increased.13 Recently, we have observed that the immunogenicity of a given TAA can be greatly enhanced by deleting its nuclear localization signal (D. Benteyn, S. Anguille, A.M.T. Van Nuffel, C. Heirman, J. Corthals and W. Waelput, unpublished results), demonstrating that further manipulation of the TAA-encoding sequence can result in favorable induction of potent antitumor immune responses.
It is generally believed that the induction of CD4+ T-cells is necessary to obtain robust and long-lasting CD8+ T-cell responses, especially against weakly immunogenic antigens like TAAs. However, the transgenic proteins produced by genetically modified DCs are located in the cytoplasm and they are less efficient at accessing the endocytic pathway to be processed for presentation to CD4+ T-cells. Consequently, additional measures must be taken to obtain presentation of the introduced gene in the context of MHC II molecules.
In the ER, MHC II molecules are assembled with invariant chain (Ii) bound to the antigen binding groove to stabilize the MHC class II complexes and prevent binding of self-peptides present in the ER (Figure 1). Ii contains two sorting signals in its cytoplasmic tail which regulate the transport of the MHC/Ii complexes from the ER through the Golgi network into the endosomal and lysosomal compartments, called MHC class II compartments (MIIC).14 Ii is degraded in the MIIC, leaving the MHC class II binding groove free to bind peptides derived from antigens present in the endocytic compartments (derived from exogenous antigens). Besides Ii, many other proteins, including lysosome-associated membrane protein-1 (LAMP-1), DC-LAMP and lysosomal acid protease reach the MIIC by virtue of a targeting sequence. A number of studies have appended these sequences to TAA-coding regions to target whole antigens to the MIIC for presentation to CD4+ T-cells (reviewed previously15).
For DC modification strategies, the most extensively used signal is the sorting sequence of LAMP-1. Lin et al. demonstrated that modification with the LAMP-1 sorting signal directs antigens to the endolysosomal compartments.16 Wu and colleagues confirmed that targeting the HPV16 E7 protein to the endolysosomal compartments with the LAMP-1 sorting indeed results in an enhanced presentation of MHC class II/E7 derived peptide complexes.17 Since then, the LAMP-1 sorting signal has been coupled to gene modification vectors, including vaccina virus encoding pp65,18 retrovirus coexpressing HPV16 E7,19 and through mRNA electroporation with carcinoembryonic antigen,20 human telomerase reverse transcriptase (hTERT),21 and Mage-A3.22 DCs electroporated with the chimeric LAMP-1 hTERT were used to immunize patients with metastatic prostate cancer; these patients developed significantly higher frequencies of hTERT-specific CD4+ T-cells than subjects receiving DC transfected with the unmodified hTERT template. Moreover, cytotoxic T-lymphocyte (CTL)-mediated killing of hTERT targets was enhanced in the LAMP-1 hTERT group.21
Improved CTL induction after vaccination with antigens linked to an MHC II targeting sequence has often been observed18,19,23 and can be interpreted as a mechanism mediated by concomitant stimulation of CD4+ cells. Nevertheless, several CD4+ T-cell independent models also showed that enhanced MHC class I presentation of antigens can be observed when the antigen is linked to an MHC class II targeting sequence.22,24 For instance, degradation of misfolded chimeric proteins after retranslocation from the ER into the cytosol could enhance their availability for presentation on MHC I.24
Genetic Modification to Enhance Costimulation (Signal 2)
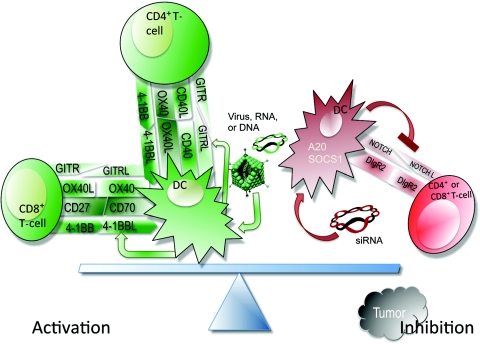
T-cell activation and inhibition are calibrated by surface-bound costimulatory molecules. Therefore, the genetic modification strategies for costimulatory molecules can be divided into two categories: modifications aiming at the enhanced expression of activating molecules, and modifications aiming at the downregulation of inhibitory molecules (Figure 2 and Table 1).
Figure 2.
Pathways of activation and inhibition via costimulatory molecules. Dendritic cell (DC)-mediated T-cell activation requires a second, antigen nonspecific signal. Costimulatory molecules are not constitutively expressed by DCs; they are upregulated during maturation and as a consequence of environmental conditions. Similarly, DCs can inhibit T-cell activation or suppress T-cell activity, especially in the context of pre-existing tumors. Gene modification of DCs has been utilized both to enhance expression of activating costimulatory molecules and to inhibit expression of inhibitory molecules shown in this figure. As described in the text, costimulatory molecules can be delivered by gene transfection or recombinant viruses; inhibitory molecules can be knocked-down using siRNA. SOCS, suppressors of cytokine signaling.
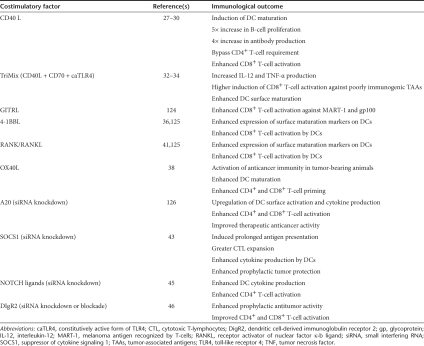
Table 1. Genetic modification of dendritic cells (DCs) for manipulation of costimulatory factors and their immunological outcomes.
Enhancing expression of costimulatory molecules
CD40-CD40L is the costimulatory receptor/ligand pair whose expression has been most often enhanced for the purpose of improving DC function. Ligation of CD40 on DCs is normally provided by activated CD4+ T-cells.25 This “licensing” interaction is the mechanism through which CD4+ type 1 T helper (Th1) cells provide help in generating primary CD8+ T-cell responses, especially to noninflammatory antigens.26 This process leads to DC maturation with upregulation of other costimulatory molecules and enhanced production of cytokines/chemokines. Licensing has been mimicked by engineering DCs to express CD40L through transduction with adenovirus,27 lentivirus,28 vaccinia virus,29 or through mRNA electroporation.30 These studies indeed provided evidence that CD40L-engineered DCs express higher CD80 and CD86, and produce more IL-12p70. Furthermore, T-cell responses against weak tumor antigens such as glycoprotein (gp)100 and MelanA were significantly enhanced when CD40L expressing DCs were used as antigen-presenting cells.31,32
In conjunction with delivering CD40L for licensing, modifying DCs to express a constitutively active form of toll-like receptor 4 (caTLR4) has been evaluated by Cisco et al. They have shown that electroporating DCs with mRNA encoding the caTLR4 mimics binding of lipopolysaccharide to TLR4, enhances DC maturation and IL-12p70 secretion, and leads to potent induction of MelanA specific T cells.33 Further, we have combined CD40L and caTLR4 together with CD70 (called TriMix). TriMix DCs are matured through caTLR4 and CD40L signaling, and additionally provide stimulation to naive T-cells, via CD27-CD70 interactions, to inhibit activated T-cell apoptosis and support T-cell activation and proliferation. When loaded with an HLA-A2 restricted MelanA epitope or coelectroporated with full-length MelanA encoding mRNA, TriMix DCs are better in stimulating MelanA specific CD8+ T-cells than cytokine cocktail matured DCs.34 Moreover, TriMix DCs can induce T-cells against TAA with a lower precursor frequency, such as Mage-A3, Mage-C2, and tyrosinase.32
Besides CD40L and CD70, other members of the tumor necrosis factor (TNF) superfamily or their ligands have been introduced into DCs to enhance their function. Our group has introduced GITRL into DCs through mRNA electroporation.35 Consistent with mouse data, we showed that human GITRL functions as a costimulator for responder T-cells, and priming with GITRL-expressing DCs increases the number of Melan-A-specific CD8+ T-cells. However, in contrast to data obtained in mice, no significant abrogation of Treg suppression by GITRL-expressing human DC could be observed.35 Grünebach et al. have shown that mRNA electroporation with 4-1BBL increased expression of CD80 and CD40.36 Furthermore, cotransfection of 4-1BBL with HER-2/neu resulted in an increased specific lysis of target cells by in vitro induced CTL lines, indicating that 4-1BBL enhances the ability of DCs to elicit primary CTL responses.36 These data confirmed results obtained by Wiethe et al. in a murine model where DCs were adenovirally transduced with 4-1BBL and the E7 oncoprotein of human papillomavirus.37 Using the same model, this group also showed that adenoviral transduction with the costimulatory molecule receptor-ligand pair RANK/RANKL augmented E7-specific, interferon-γ (IFN-γ)-secreting effector and memory T-cells. Similar T-cell enhancement was observed upon cotransduction of DCs for coexpression of T-cell costimulatory molecules, receptor activator of nuclear factor κ-b ligand (RANKL) and CD40L, or for the coexpression of DC costimulatory molecules, RANK, and CD40.37
Another frequently studied costimulatory molecule is OX40L, which enhances stimulation of antigen-specific CD4+ T-cells.38 DCs transfected with OX40L mRNA facilitate generation of antigen-specific CD4+ T-cell response and Th1 polarization, and as a result, improve the induction of antigen-specific CTL responses in vitro. Moreover, mice carrying pre-established B16 melanomas and vaccinated with OX40L-expressing DCs showed an enhancement of antitumor activity due to in vivo priming of Th1-type CD4+ T-cells.38
Downregulating inhibitory molecules
DCs are capable of priming both proinflammatory and regulatory/suppressive T-cell responses based on the complement of costimulatory receptors (or lack thereof) that they express. The downregulation of suppressive molecules in DCs is therefore an attractive approach for generating therapeutic immunity against cancer. Although many molecules qualify for this purpose (reviewed by Mao et al.39), only a few have been investigated by genetic modification of DCs.
The zinc-finger protein, A20, is an ubiquitin-editing enzyme with de-ubiquitinase activity in its amino-terminal region and ubiquitinase activity in the zinc-finger domain of its carboxy-terminal region. Through this dual ubiquitin-editing function, A20 can negatively regulate the TLR and TNF receptor signaling pathways. It has been shown that A20-silenced murine DCs showed enhanced expression of costimulatory molecules and proinflammatory cytokines. These DCs were refractory to Treg-mediated suppression and effectively activated tumor-infiltrating CTLs and CD4+ T-cells.40 Our group subsequently reported that A20 silencing in human DCs results in activation of the transcription factors nuclear factor κ-B (NFκB) and activator protein-1, leading to increased and sustained production of interleukin (IL)-6, IL-10, and IL-12p70. Moreover, A20 downregulated DCs skew naive CD4+ T-cells toward IFN-γ producing Th1 cells and have an enhanced capacity to prime MelanA/melanoma antigen recognized by T-cells (MART-1) specific CD8+ T cells.41
SOCS1 (suppressor of cytokine signaling 1) is an immunosuppressive protein mediating negative-feedback inhibition of cytokine signaling. It is induced by cytokines such as IFN-γ, IL-12, IL-2, IL-7, and granulocyte-macrophage colony stimulating factor (GM-CSF), and subsequently inhibits their function by suppressing signal transducer and activator of transcription (STAT) molecules.42 Vaccination of mice with SOCS1-silenced DCs strongly enhances antigen-specific antitumor immunity in in vivo murine models, likely due to the prolonged antigen presentation permitted by SOCS1 silencing.43
Surface molecules that have direct suppressive effects on T-cells are also attractive targets for silencing. To date, two surface molecules have been evaluated for this purpose: the Notch ligands and DC-derived immunoglobulin receptor 2 (DIgR2). The expression of Notch ligands (Delta1, Jagged1, or Jagged2) has been shown to deliver suppressive signals to T-cells.44 Knockdown by small interfering RNA (siRNA) in human DCs leads to enhanced IFN-γ production in allogeneic mixed lymphocyte reaction. Moreover, Delta1 siRNA leads to enhanced cytokine production by CD4+ T-cells in response to polyclonal T-cell receptor activation.45
The second inhibitory molecule that has been targeted in DCs, DIgR2, is a member of the immunogobulin superfamily. This family includes several molecules with key roles in the biology of innate and adaptive immune responses, some of which—like DIgR2—act as inhibitory receptors. Silencing of DIgR2 in murine DCs with specific siRNA enhances T-cell proliferation and antigen-specific T-cell responses.46 Furthermore, immunization of mice with antigen-pulsed, DIgR2-silenced DCs elicits more potent antigen-specific CD4+ and CD8+ T-cell responses, thus protecting the vaccinated mice from tumor challenge more effectively.46
Genetic Modification to Enhance the Immune Environment (Signal 3)
In addition to cognate antigen recognition and costimulation, DC-derived soluble factors create a critical third signal to condition the immune environment. The cytokine and chemokine milieu established during early innate reactions directs immune polarization and induces recruitment of accessory leukocyte populations. Priming and activity of anticancer T-cell responses occur ideally in Th1-polarized microenvironments, which are established by type I IFN (IFN I), IFN-γ, and IL-12p70, characterized by the presence of CD8+ T-cells, Th1-polarized CD4+ helper T-cells, and NK cells.47,48 To facilitate development and maintenance of Th1 signaling after vaccination, DCs can be modified for constitutive production of Th1 cytokines and chemokines (Summarized in Table 2).
Table 2. Manipulation of chemokine and cytokine secretion and sensitivity in dendritic cell (DC)-based cancer vaccines.
Manipulating Th1 cytokine secretion
IL-12p70, produced by DCs after stimulation, initiates Th1 polarization by inducing upregulation of TNF-α, IFN-γ, IL-2, and IL-18 from neighboring leukocytes.49,50,51 On its own, IL-12 has potent anticancer effects attributable to its ability to activate T- and NK cells, and has been used in clinical trials.47,50 Repeated systemic delivery of IL-12 has potent anticancer effects, unfortunately, however, it is also associated with severe toxicity.47 Modification of DCs for cytokine production provides a continuous supply of IL-12 that is restricted to the immune environment and eliminates the requirement for systemic administration. DCs transduced using recombinant adenovirus carrying IL-12 demonstrate increased antigen presentation and costimulatory molecule expression, and induce increased numbers of activated T-cells.52,53 Similarly, modification of DCs for coexpression of antigens and Th1 cytokines downstream of IL-12, including IL-2 or IL-18, supports development of CTL responses to prevent tumor growth.54,55 Finally, DCs transduced for IL-12 production can reprogram primed T-cells isolated from melanoma patients to produce IFN-γ,56 suggesting that IL-12-engineered DCs can induce Th1 immune polarization and favor the development of tumoricidal T-cell responses, even in tumor-bearing hosts.
Inhibiting responsiveness to regulatory cytokines
Tumor growth is associated with establishment of an immunosuppressive environment, characterized by the presence of regulatory cytokines including transforming growth factor-β (TGF-β) and IL-10. These conditions favor recruitment of immature myeloid suppressor cells and support in situ priming of regulatory T-cells.57 Moreover, TGF-β and IL-10 can induce apoptosis of cytotoxic T-cells and DCs.57,58 T-cells primed in the periphery, including those activated by DC vaccines, demonstrate diminished cytotoxic activity within the tumor environment.52,59 Using genetically modified DCs, it may be possible to overcome the suppression imposed by pre-existing tumors (Table 2). Transduction for expression of GM-CSF induced upregulation of the anti-apoptotic molecule, B-cell lymphoma-extra large (Bcl-xL), in DCs and increased their resistance against TGF-β-induced apoptosis.60 To directly reduce DCs' sensitivity to TGF-β, Wang and colleagues infected DCs using a retrovirus encoding a dominant-negative mutant of the TGF-β receptor.58 Consequently, DCs became less sensitive to TGF-β and produced greater concentrations of IL-12.58 In vivo, TGF-β receptor knocked-down DCs induced significantly stronger CTL activity and effected greater tumor rejection than green fluorescent protein-transduced controls.58 DCs producing proinflammatory cytokines may also be useful to directly establish a proinflammatory microenvironment when injected intratumorally. For instance, intratumoral delivery of DCs overexpressing IFN I recruited and maintained cytotoxic T-cells and extended survival of their hosts.61
Manipulation of chemokine secretion and responsiveness
Upon sensing pathogens, DCs upregulate chemokine production and receptor expression to facilitate T-cell recruitment and homing to draining lymph nodes. However, following subcutaneous injection of ex vivo cultured DCs, fewer than 5% of inoculated DCs can be recovered from the draining lymph node.62,63 To enhance their recruitment to the lymph node, DCs have been modified to respond to chemokines that are constitutively expressed in the lymphatic system, including chemokine (C-C motif) ligand 21 (CCL21).64 For example, following transduction with adenovirus encoding CCR7, the receptor for CCL21, DCs accumulated in draining lymph nodes 5.5 times more efficiently than those infected with control adenovirus.64 Similarly, DCs have also been modified by retroviral transduction to extend their natural production of C-X-C motif chemokine 10 (CXCL10), a chemoattractant for naive T cells.65 CXCL10-producing DCs could induce recruitment of T-cells in in vitro cultures and enhanced CD8+ T-cell priming in vivo.65
The elimination of established tumors will require recruitment of cytotoxic effectors, however, the chemokine milieu within the tumor environment favors recruitment of Treg. Accordingly, DCs can be modified for controlled chemokine expression prior to intratumoral inoculation. Activated DCs express an array of chemokines, including CCL17 and CCL22, which favor recruitment of primed Th2 and Treg T-cells, and CCL23, which favors CD8+ T-cell recruitment.65,66 When CCL17 and CCL22 were knocked-down using siRNA, DCs became potent recruiters of CD8+ T-cells, and intratumoral injection of these DCs lowered the ratio of Treg:CTL within the tumor environment.65 Similarly, the inoculation of DCs transduced using adenovirus expressing CCL21 led to enhanced recruitment and activation of T-cells and increased concentrations of Th1 cytokines within the tumor microenvironment.67
Genetic Modification of DCs to Induce Recruitment of Other Cell Types
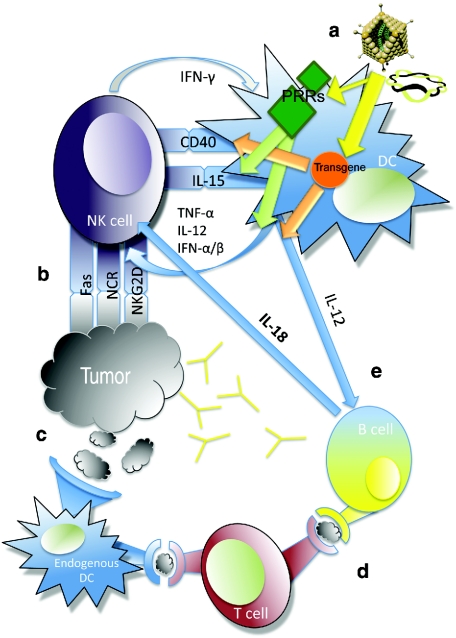
The development of a Th1 immune environment is not only conducive to cytotoxic T-cell priming; recapitulation of a Th1 scenario actually facilitates recruitment and activation of additional effector cell populations. Whether intentionally or collaterally targeted, B-cells and NK cells can contribute significantly to the outcome of DC-based cancer vaccines.68,69,70,71,72,73,74 A schematic representation of DCs' interaction with these cell types is shown in Figure 3.
Figure 3.
Complex interactions between dendritic cells (DCs) and other cell populations. (a) DCs are modified by RNA or DNA transfection, or infection using recombinant viruses. In addition to supporting T-cell priming, these factors can additionally support natural killer (NK) and B-cell activation. Viral components or foreign DNA/RNA can activate pattern recognition receptor, leading to upregulation of DC maturation factors and cytokine production, which, in turn, support NK cell activation. Bidirectional interaction between DCs and NK cells leads to interferon (IFN)-γ production and cytotoxicity from NK cells, and additional interleukin-12 (IL-12) from DCs. (b) NK cells initiate direct tumor cell lysis and additionally support T-cell activation by releasing tumor components. (c) Released tumor antigens can be processed and presented by endogenous DCs. This process facilitates further T-cell priming against an array of tumor-associated antigens. (d) Activated T-cells can additionally support B-cell activation. (e) Additionally, B-cells can support NK cell activation by releasing IL-18 in response to DC-derived IL-12.
Activation of B cells by DC-based vaccines
Because most of the identified TAAs are intracellular antigens, cancer immunotherapies have primarily aimed at generating T-cell responses. However, several extracellular TAAs have been identified, therefore, B-cells and antibodies can provide an additional avenue for tumor targeting. In fact, monoclonal antibody therapies, including herceptin and rituxumab are among the most successful immunotherapeutic drugs available for clinical use.74 B-cell activation and production of antibodies is not directly stimulated by DCs, however, their capacity to deliver antigen and support CD4+ T-cell priming are critical for B-cell activation. Therefore, strategies to prime T-cell responses may collaterally activate B-cells. For instance, vaccination using DCs transduced for production of erbB2 (the murine homologue of HER2/neu), led to antibody production and T-cell activation which mediated downstream tumor protection.75
Few investigations have targeted DCs to initiate interaction with B-cells, however, proof-of-principle does exist to demonstrate that genetically modified DCs can activate B-cells for cytokine and antibody production. For instance, DCs transduced with recombinant adenovirus encoding the HER-2/neu oncogene delayed the onset of spontaneous mammary tumor growth in neuT transgenic mice in a manner dependent on antibodies and CD4+ T-cells.73,76 Surprisingly, B-cells can also contribute to polarization of the Th1 immune environment by producing IL-18 in response to DC-derived IL-12.49 In turn, IL-18 has been shown to activate NK cells for IFN-γ production and cytotoxicity.49
Recently, Boczkowski et al. have reported on a novel approach that might circumvent the need of B-cell activation by DC vaccines: they have engineered the DCs to secrete antibodies.77 By electroporating murine DCs with genes for the heavy and light chains of a rat anti-mouse GITR mAb, they engineered DCs to secrete anti-GITR antibodies. They showed that treatment with DCs secreting anti-GITR and expressing TAA was comparable to administering TAA-expressing DCs plus systemic delivery of 1 mg of anti-GITR mAb, even though the DCs that were injected secreted only 2–3 ng of antibody.
Activation of NK cells by DC-based vaccines
Without prior stimulation, NK cells provide critical immunosurveillance for elimination of transformed, precancerous cells. NK cells are important as a major source of IFN-γ and for direct lysis of tumor cells through cytotoxicity receptors, including NKG2D, Fas, and the natural cytotoxicity receptor families.78 Activated NK cells additionally provide help for B- and T-cell activation, bypassing their requirement for CD4+ T-cell-mediated help.73,79,80 In fact, the presence of activated NK cells in cancer patients correlates with improved prognosis, and may actually be a better predictor of DC vaccine efficacy than T-cells.81,82,83 DCs support the development and activation of NK cells in vivo through bidirectional interactions,84,85,86 and NK cells activated by DC vaccination can provide protection against tumor challenge, even when adoptively transferred to naive hosts.69,70,79,86 Therefore, it is important to consider the impact of DC-based vaccines on NK cell activation and function.
NK cells can be primed beyond their “natural” state to provide enhanced antitumor activity by a variety of stimuli.69,70,86,87 In response to inoculation with DCs, IFN-γ and granzyme B expression is upregulated by NK cells in the spleen and draining lymph node, and is indispensible for tumor protection.53,60,69,70 Protocols for genetic modification of DCs may amplify NK cell activation and improve the overall outcome of DC-based vaccines. For example, modifications of DCs for Th1 cytokine production, including IL-12 or GM-CSF, have been demonstrated to induce NK recruitment and activation.53,56,60 Similarly, DCs differentiated in the presence of polyI:C and IFN-β induce recruitment of activated NK cells, which support Th1 T-cell development.87
Creating a Strong Inflammatory Environment
Maturation of DCs can be accomplished by exposure to cytokine cocktails, TLR ligands or virus infection, however, these stimulations activate different pathways.88 TLR ligands and virus infection induce maturation by agonizing pathogen sensing pathways through activation of pattern recognition receptors, including the toll (TLR)-, NOD (NLR)-, and RIG-I (RLR)-like pathways [pattern recognition receptor (PRRs)].89 In contrast, cytokine cocktails, which are most frequently used in clinical trials, actually recapitulate events that occur downstream of pathogen sensing in DCs by binding to cytokine receptors and inducing activation of STAT molecules. PRR or cytokine receptor engagement triggers downstream signaling that can lead to activation of AP-1, NFκB, and the innate interferon, MAP kinase, and inflammasome pathways.89 Although cytokine cocktails, TLR ligands and virus infection can each induce upregulation of costimulatory molecules and cytokines conducive to T-cell activation, they may differentially influence the longevity of immune responses or the activation of additional cell populations.
Similar to cytokine cocktails, TLR ligands are generally washed from DC preparations before inoculation. The extension of TLR signaling, however, may assist in generating immune responses. As mentioned earlier, transfection of constitutively active mRNA for TLR4 alongside costimulatory molecules and TAAs enhanced T-cell activation in vivo by providing continuous stimulation.32,34 Transfection with RNA or infection with recombinant, replication-incompetent viruses provides a continuous supply of cytoplasmic RNA and DNA which is sensed by RLRs and TLRs 3, 7, 8, and 9.48,70,87,90,91 This continued stimulation leads to upregulation of prototypical DC maturation markers, including CD83 and CD86.92,93
Engagement of multiple receptors can synergize to tailor DC maturation, migration, and cytokine production against a given pathogen.89,94 Recombinant viruses activate components of multiple pathways, and lead to potent, persistent DC activation. For instance, DCs infected with vesicular stomatitis virus activate tumoricidal NK cells in cancer-bearing mice, in a mechanism dependent on IFN I signaling and IL-15 signaling.95 Similarly, DCs infected with adenovirus activate NK cells in vivo via cooperative TNF-α and IL-15 pathways.96 Recombinant canarypox virus also elicits activation of the innate interferon signaling pathway in DCs, upregulates NFκB activity, induces CXCL10 production from DCs and primes IFN-γ production by NK cells.97,98 Taken together, these experiments demonstrate that virus infection of DCs indeed leads to prolonged Th1 immune activation, which assists in activating NK cells in addition to T cells.
Current Progress in Clinical Trials
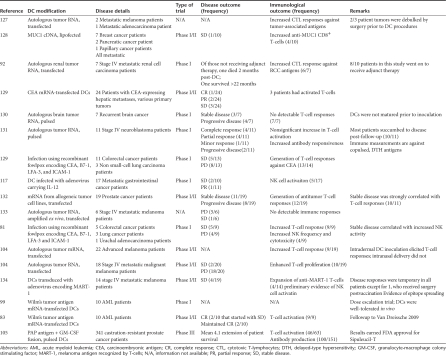
Preclinical models of DC-based cancer vaccines provided significant optimism for translation to clinical application. Protocols for deriving DCs from CD14+ and CD34+ monocytes are established, and DCs are well-tolerated in phase I clinical trials.92,99,100,101,102,103,104 DCs modified for expression of TAAs have been shown to activate antitumor T-cell responses in cancer patients and in therapeutic animal models.48,70,105 A summary of a number of clinical trials using genetically modified DCs is shown in Table 3. Unfortunately, the success of experimental models of DC-based cancer vaccines has generally not translated into clinical efficacy.88 Improvements in DCs' migration, immune polarization and ability to engage effector populations despite tumor-induced immunosuppression will likely be required to facilitate the widespread clinical use of DC-based vaccines. One of the strategies to accomplish this is to manipulate the microenvironment during DC differentiation or following in vivo injection. Recently, a DC-based vaccine for prostate cancer became the first FDA-approved cellular vaccine after reporting a 4.1-month extension of patient survival,105 generating significant optimism for DC-based cancer vaccines. This vaccine, Sipuleucil-T, utilizes DCs pulsed with a fusion protein of a prostate cancer-associated antigen and GM-CSF,105 reinforcing the notion that the combination of DC-based vaccines and cytokines may improve therapeutic outcomes.
Table 3. Summary of outcomes from a number of clinical trials employing gene-modified dendritic cell (DCs).
To date, the majority of clinical trials have used DCs pulsed with TAAs, and matured by exposure to cytokine cocktails that include PGE-2, IL-1β, IL-6, and TNF-α. PGE-2 is required for DC migration to lymph nodes,106,107 however it also impairs DCs' production of IL-12,108 and induces Th2 cytokine production, including IL-5.56 More recently, protocols using IFN I have been established that favor development of “DC1” DCs. DC1 DCs upregulate CXCL10, recruit and activate NK cells, instruct Th1 cytokine production, and reduce Treg frequency.9,87,109,110,111 Compared with standard myeloid DC culture protocols, DC1 DCs induce greater CTL activation and support superior antigen cross priming.9,112 Moreover, DC1 DCs can induce primary antibody immune responses.113 When DCs were transduced for IFN-α prior to in vivo inoculation, their ability to migrate and survive was enhanced compared with control-transduced DCs in human clinical trials.114 Together, these findings support the use of type I IFN during DC differentiation.
IL-12 and TNF-α are also candidates for cytokine gene therapy with DCs, owing to their ability to polarize Th1 immune environments. The clinical utility of DCs genetically modified for IL-12 or TNF-α production is currently under investigation.115,116 Intratumoral administration of DCs infected with adenovirus encoding IL-12 mediates increased recruitment of CD8+ T-cells and activation of NK cells, however, objective clinical response rates remained low.117 This failure may be attributable to impaired DC migration from the tumor to present antigen in draining lymph nodes. Indeed, Feijoó and colleagues have reported that the migration of IL-12-producing DCs was inhibited by tumor-derived IL-8, and their migratory capacity could be restored using an anti-IL-8 antibody.118 An alternative strategy is to control DC interaction with naive T-cells by modifying DCs for expression of CCL21. This chemokine leads to the formation of lymphoid-like structures in vivo, where naive T-cells can be primed extranodally, eliminating the requirement for DCs to traffic to the local lymph nodes. DCs modified for CCL21 expression are the subject of an ongoing clinical trial.115
We have performed a clinical trial with DCs genetically modified through mRNA electroporation with TriMix mRNA, coelectroporated with Mage-A3, Mage-C2, gp100, or tyrosinase mRNA (S. Wilfenhof, A.M.T. Van Nuffel, J. Corthals, C. Heirman, S. Tuyaerts and D. Benteyn, unpublished results). Thirty-five metastatic melanoma patients received four biweekly vaccinations. Thereafter they could initiate interferon-α2b therapy and receive additional TriMix-DC vaccines every 8 weeks. Immune monitoring of T-cells infiltrating a delayed-type hypersensitivity reaction showed that almost 60% of the patients tested after the 4th vaccine had mounted an immune response against one or more of the vaccine antigens. Furthermore, disease control for >6 months with regression of metastases was observed in 7 of 20 patients (35%) with evaluable disease at baseline. For 15 patients without evaluable disease at baseline, recurrence-free survival is 23.0 months.
Clinical trials have demonstrated that the presence of activated NK cells correlates with improved anticancer activity following DC vaccination, and may actually be a better prognostic indicator than T-cell activation.81,83 NK cells can kill tumor cells directly and support T-cell activity, both via cytokine secretion and through release of TAAs by tumor cell lysis. These TAA can subsequently be scavenged and presented by endogenous DCs.78,119 Thus, future efforts may benefit from a focus on developing conditions conducive to NK cell activation and in situ T-cell priming, rather than focusing on selection of TAAs.
Conclusions and Future Directions
DC-based vaccines have shown excellent promise in preclinical studies, but further improvements are required to amplify their therapeutic utility. Clinical trials have mainly employed DCs pulsed with TAAs and matured by exposure to cytokine cocktails. These DCs are sufficient for T-cell activation, but they may not be adequate to provide continuous costimulation to mount and maintain a proinflammatory immune environment and to recruit additional effector components. Since an existing tumor creates an immunosuppressive immune environment, successful DC-based cancer vaccines should be prepared to prime strong and persistent immune responses after immunization. Genetic modification of DCs will allow for a continuous supply of natively processed antigen and immune-stimulating molecules, and might therefore provide more robust and persistent anticancer immunity in vivo.
Several investigations have demonstrated that DCs can be simultaneously modified with multiple genes and/or immune factors.11,33,34,48,108 It is unlikely that modification of DCs for a single factor, or engagement of a single effector population will be sufficient for successful cancer immunotherapy. Not only must DCs activate anticancer immune responses, they must also resist tumor-induced immunosuppression. Thus, DCs should be rationally engineered to simultaneously deliver the three signals required for T-cell activation, along with neutralizing factors for inhibitory components. To accomplish this, DCs can be genetically modified as described in this manuscript, and/or used in combination with other treatment approaches. For example, anthracyclin chemotherapy will facilitate tumor cell apoptosis conducive to DC-mediated antigen cross presentation to T-cells.120 Moreover, DC immunization in combination with antibody therapies, such as anti-IL-8 or anti-CTLA4, will facilitate DC migration and presentation of tumor-derived antigens, or inhibit tumor-induced immunosuppression, respectively.118,121
Clinical trials of DC-based cancer vaccines have revealed that activated NK cells are better predictive of vaccine efficacy than CTL responses.81,82,83 Accordingly, future clinical trials may benefit from the inclusion of strategies to target NK cells in addition to CTL. We, and others, have demonstrated that tumoricidal NK cells can be activated by DC-based vaccines, especially those modified by virus infection.69,70,96 This success has been attributed to IL-15 and membrane-bound TNF-α.96 Similarly, other cytokines, including GM-CSF or IL-12, have been shown to participate in recruitment and activation of NK cells following DC-based cancer vaccination.53,56,122 In addition, delivery of ligands for NK-activating receptors, (i.e., those that bind to NKG2D family receptors), could facilitate the activation of NK cells for IFN-γ production and cytotoxicity.123 Existing DC-based vaccines would likely benefit from additional modification to provide NK-activating cytokines and molecules. Further investigation will be required to determine the optimal combination of these factors to provide NK cell activation and support for CTL-mediated rejection of tumors.
Genetic modification is safe and sufficient for delivery of TAAs, costimulatory molecules, and the environmental signals. The use of DNA, mRNA, or viruses to introduce TAAs allows for endogenous expression and processing of full-length proteins, including tumor antigens and immune response factors. Moreover, chemokine, cytokine, and costimulatory molecule expression can be made continuous by delivering the relevant genes under the control of constitutive promoters.
REFERENCES
- Coley W. The treatment of malignant tumors by repeated inoculations of erysipelas: with a report of ten original cases. Clin Orthop Relat Res. 1893;262:3–11. [PubMed] [Google Scholar]
- Ehrlich, P. Ueber den jetzigen stand der Karzinomforschung. Ned Tijdschr Geneeskd. 1909;5:273. [Google Scholar]
- Burnet FM. The concept of immunological surveillance. Prog Exp Tumor Res. 1970;13:1–27. doi: 10.1159/000386035. [DOI] [PubMed] [Google Scholar]
- van der Bruggen P, Traversari C, Chomez P, Lurquin C, De Plaen E, Van den Eynde B.et al. (1991A gene encoding an antigen recognized by cytolytic T lymphocytes on a human melanoma Science 2541643–1647. [DOI] [PubMed] [Google Scholar]
- Muul LM, Spiess PJ, Director EP., and, Rosenberg SA. Identification of specific cytolytic immune responses against autologous tumor in humans bearing malignant melanoma. J Immunol. 1987;138:989–995. [PubMed] [Google Scholar]
- Zinkernagel RM., and, Doherty PC. Restriction of in vitro T cell-mediated cytotoxicity in lymphocytic choriomeningitis within a syngeneic or semiallogeneic system. Nature. 1974;248:701–702. doi: 10.1038/248701a0. [DOI] [PubMed] [Google Scholar]
- Lafferty KJ, Warren HS., and, Woolnough JA. A mediator acting as a costimulator for the development of cytotoxic responses in vitro. Adv Exp Med Biol. 1979;114:497–501. doi: 10.1007/978-1-4615-9101-6_82. [DOI] [PubMed] [Google Scholar]
- Curtsinger JM, Schmidt CS, Mondino A, Lins DC, Kedl RM, Jenkins MK.et al. (1999Inflammatory cytokines provide a third signal for activation of naive CD4+ and CD8+ T cells J Immunol 1623256–3262. [PubMed] [Google Scholar]
- Kalinski P, Nakamura Y, Watchmaker P, Giermasz A, Muthuswamy R., and, Mailliard RB. Helper roles of NK and CD8+ T cells in the induction of tumor immunity. Polarized dendritic cells as cancer vaccines. Immunol Res. 2006;36:137–146. doi: 10.1385/IR:36:1:137. [DOI] [PubMed] [Google Scholar]
- Breckpot K, Bonehill A, Aerts JL., and, Thielemans K.Dendritic cells: subtypes, life cycle, activation and biological functions Dendritic Cells: Types, Life Cycles and Biological Functions Welles LC.Ed). Nova Science Publishers. Hauppage, NY.In press. [Google Scholar]
- Breckpot K, Heirman C, Neyns B., and, Thielemans K. Exploiting dendritic cells for cancer immunotherapy: genetic modification of dendritic cells. J Gene Med. 2004;6:1175–1188. doi: 10.1002/jgm.615. [DOI] [PubMed] [Google Scholar]
- Jariel-Encontre I, Bossis G., and, Piechaczyk M. Ubiquitin-independent degradation of proteins by the proteasome. Biochim Biophys Acta. 2008;1786:153–177. doi: 10.1016/j.bbcan.2008.05.004. [DOI] [PubMed] [Google Scholar]
- Park MJ, Kim EK, Han JY, Cho HW, Sohn HJ, Kim SY.et al. (2010Fusion of the Human Cytomegalovirus pp65 antigen with both ubiquitin and ornithine decarboxylase additively enhances antigen presentation to CD8+ T cells in human dendritic cells Hum Gene Ther 21957–967. [DOI] [PubMed] [Google Scholar]
- Cresswell P. Invariant chain structure and MHC class II function. Cell. 1996;84:505–507. doi: 10.1016/s0092-8674(00)81025-9. [DOI] [PubMed] [Google Scholar]
- Bonehill A, Heirman C., and, Thielemans K. Genetic approaches for the induction of a CD4+ T cell response in cancer immunotherapy. J Gene Med. 2005;7:686–695. doi: 10.1002/jgm.713. [DOI] [PubMed] [Google Scholar]
- Lin X, Dashti A, Schinazi RF., and, Tang J. Intracellular diversion of glycoprotein GP160 of human immunodeficiency virus to lysosomes as a strategy of AIDS gene therapy. FASEB J. 1993;7:1070–1080. doi: 10.1096/fasebj.7.11.8370478. [DOI] [PubMed] [Google Scholar]
- Wu TC, Guarnieri FG, Staveley-O'Carroll KF, Viscidi RP, Levitsky HI, Hedrick L.et al. (1995Engineering an intracellular pathway for major histocompatibility complex class II presentation of antigens Proc Natl Acad Sci USA 9211671–11675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonini C, Lee SP, Riddell SR., and, Greenberg PD. Targeting antigen in mature dendritic cells for simultaneous stimulation of CD4+ and CD8+ T cells. J Immunol. 2001;166:5250–5257. doi: 10.4049/jimmunol.166.8.5250. [DOI] [PubMed] [Google Scholar]
- Kang TH, Lee JH, Bae HC, Noh KH, Kim JH, Song CK.et al. (2006Enhancement of dendritic cell-based vaccine potency by targeting antigen to endosomal/lysosomal compartments Immunol Lett 106126–134. [DOI] [PubMed] [Google Scholar]
- Nair SK, Boczkowski D, Morse M, Cumming RI, Lyerly HK., and, Gilboa E. Induction of primary carcinoembryonic antigen (CEA)-specific cytotoxic T lymphocytes in vitro using human dendritic cells transfected with RNA. Nat Biotechnol. 1998;16:364–369. doi: 10.1038/nbt0498-364. [DOI] [PubMed] [Google Scholar]
- Su Z, Vieweg J, Weizer AZ, Dahm P, Yancey D, Turaga V.et al. (2002Enhanced induction of telomerase-specific CD4+ T cells using dendritic cells transfected with RNA encoding a chimeric gene product Cancer Res 625041–5048. [PubMed] [Google Scholar]
- Bonehill A, Heirman C, Tuyaerts S, Michiels A, Breckpot K, Brasseur F.et al. (2004Messenger RNA-electroporated dendritic cells presenting MAGE-A3 simultaneously in HLA class I and class II molecules J Immunol 1726649–6657. [DOI] [PubMed] [Google Scholar]
- Ji H, Wang TL, Chen CH, Pai SI, Hung CF, Lin KY.et al. (1999Targeting human papillomavirus type 16 E7 to the endosomal/lysosomal compartment enhances the antitumor immunity of DNA vaccines against murine human papillomavirus type 16 E7-expressing tumors Hum Gene Ther 102727–2740. [DOI] [PubMed] [Google Scholar]
- Kreiter S, Selmi A, Diken M, Sebastian M, Osterloh P, Schild H.et al. (2008Increased antigen presentation efficiency by coupling antigens to MHC class I trafficking signals J Immunol 180309–318. [DOI] [PubMed] [Google Scholar]
- Schönbeck U., and, Libby P. The CD40/CD154 receptor/ligand dyad. Cell Mol Life Sci. 2001;58:4–43. doi: 10.1007/PL00000776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevan MJ. Helping the CD8+ T-cell response. Nat Rev Immunol. 2004;4:595–602. doi: 10.1038/nri1413. [DOI] [PubMed] [Google Scholar]
- Kikuchi T, Moore MA., and, Crystal RG. Dendritic cells modified to express CD40 ligand elicit therapeutic immunity against pre-existing murine tumors. Blood. 2000;96:91–99. [PubMed] [Google Scholar]
- Koya RC, Kasahara N, Favaro PM, Lau R, Ta HQ, Weber JS.et al. (2003Potent maturation of monocyte-derived dendritic cells after CD40L lentiviral gene delivery J Immunother 26451–460. [DOI] [PubMed] [Google Scholar]
- Feder-Mengus C, Schultz-Thater E, Oertli D, Marti WR, Heberer M, Spagnoli GC.et al. (2005Nonreplicating recombinant vaccinia virus expressing CD40 ligand enhances APC capacity to stimulate specific CD4+ and CD8+ T cell responses Hum Gene Ther 16348–360. [DOI] [PubMed] [Google Scholar]
- Tcherepanova IY, Adams MD, Feng X, Hinohara A, Horvatinovich J, Calderhead D.et al. (2008Ectopic expression of a truncated CD40L protein from synthetic post-transcriptionally capped RNA in dendritic cells induces high levels of IL-12 secretion BMC Mol Biol 990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knippertz I, Hesse A, Schunder T, Kämpgen E, Brenner MK, Schuler G.et al. (2009Generation of human dendritic cells that simultaneously secrete IL-12 and have migratory capacity by adenoviral gene transfer of hCD40L in combination with IFN-γ J Immunother 32524–538. [DOI] [PubMed] [Google Scholar]
- Bonehill A, Van Nuffel AM, Corthals J, Tuyaerts S, Heirman C, François V.et al. (2009Single-step antigen loading and activation of dendritic cells by mRNA electroporation for the purpose of therapeutic vaccination in melanoma patients Clin Cancer Res 153366–3375. [DOI] [PubMed] [Google Scholar]
- Cisco RM, Abdel-Wahab Z, Dannull J, Nair S, Tyler DS, Gilboa E.et al. (2004Induction of human dendritic cell maturation using transfection with RNA encoding a dominant positive toll-like receptor 4 J Immunol 1727162–7168. [DOI] [PubMed] [Google Scholar]
- Bonehill A, Tuyaerts S, Van Nuffel AM, Heirman C, Bos TJ, Fostier K.et al. (2008Enhancing the T-cell stimulatory capacity of human dendritic cells by co-electroporation with CD40L, CD70 and constitutively active TLR4 encoding mRNA Mol Ther 161170–1180. [DOI] [PubMed] [Google Scholar]
- Tuyaerts S, Aerts JL, Corthals J, Neyns B, Heirman C, Breckpot K.et al. (2007Current approaches in dendritic cell generation and future implications for cancer immunotherapy Cancer Immunol Immunother 561513–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grünebach F, Kayser K, Weck MM, Müller MR, Appel S., and, Brossart P. Cotransfection of dendritic cells with RNA coding for HER-2/neu and 4-1BBL increases the induction of tumor antigen specific cytotoxic T lymphocytes. Cancer Gene Ther. 2005;12:749–756. doi: 10.1038/sj.cgt.7700842. [DOI] [PubMed] [Google Scholar]
- Wiethe C, Debus A, Mohrs M, Steinkasserer A, Lutz M., and, Gessner A. Dendritic cell differentiation state and their interaction with NKT cells determine Th1/Th2 differentiation in the murine model of Leishmania major infection. J Immunol. 2008;180:4371–4381. doi: 10.4049/jimmunol.180.7.4371. [DOI] [PubMed] [Google Scholar]
- Dannull J, Nair S, Su Z, Boczkowski D, DeBeck C, Yang B.et al. (2005Enhancing the immunostimulatory function of dendritic cells by transfection with mRNA encoding OX40 ligand Blood 1053206–3213. [DOI] [PubMed] [Google Scholar]
- Mao CP., and, Wu T. Inhibitory RNA Molecules in Immunotherapy for Cancer. Methods Mol Biol. 2010;623:325–339. doi: 10.1007/978-1-60761-588-0_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song XT, Evel-Kabler K, Shen L, Rollins L, Huang XF., and, Chen SY. A20 is an antigen presentation attenuator, and its inhibition overcomes regulatory T cell-mediated suppression. Nat Med. 2008;14:258–265. doi: 10.1038/nm1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breckpot K, Aerts-Toegaert C, Heirman C, Peeters U, Beyaert R, Aerts JL.et al. (2009Attenuated expression of A20 markedly increases the efficacy of double-stranded RNA-activated dendritic cells as an anti-cancer vaccine J Immunol 182860–870. [DOI] [PubMed] [Google Scholar]
- Palmer DC., and, Restifo NP. Suppressors of cytokine signaling (SOCS) in T cell differentiation, maturation, and function. Trends Immunol. 2009;30:592–602. doi: 10.1016/j.it.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen L, Evel-Kabler K, Strube R., and, Chen SY. Silencing of SOCS1 enhances antigen presentation by dendritic cells and antigen-specific anti-tumor immunity. Nat Biotechnol. 2004;22:1546–1553. doi: 10.1038/nbt1035. [DOI] [PubMed] [Google Scholar]
- McKenzie GJ, Khan M, Briend E, Stallwood Y., and, Champion BR. Notch: a unique therapeutic target for immunomodulation. Expert Opin Ther Targets. 2005;9:395–410. doi: 10.1517/14728222.9.2.395. [DOI] [PubMed] [Google Scholar]
- Stallwood Y, Briend E, Ray KM, Ward GA, Smith BJ, Nye E.et al. (2006Small interfering RNA-mediated knockdown of notch ligands in primary CD4+ T cells and dendritic cells enhances cytokine production J Immunol 177885–895. [DOI] [PubMed] [Google Scholar]
- Shi L, Luo K, Xia D, Chen T, Chen G, Jiang Y.et al. (2006DIgR2, dendritic cell-derived immunoglobulin receptor 2, is one representative of a family of IgSF inhibitory receptors and mediates negative regulation of dendritic cell-initiated antigen-specific T-cell responses Blood 1082678–2686. [DOI] [PubMed] [Google Scholar]
- Colombo MP., and, Trinchieri G. Interleukin-12 in anti-tumor immunity and immunotherapy. Cytokine Growth Factor Rev. 2002;13:155–168. doi: 10.1016/s1359-6101(01)00032-6. [DOI] [PubMed] [Google Scholar]
- Yang Y, Huang CT, Huang X., and, Pardoll DM. Persistent Toll-like receptor signals are required for reversal of regulatory T cell-mediated CD8 tolerance. Nat Immunol. 2004;5:508–515. doi: 10.1038/ni1059. [DOI] [PubMed] [Google Scholar]
- Haddad E, Senger L., and, Takei F. An accessory role for B cells in the IL-12-induced activation of resting mouse NK cells. J Immunology. 2009;183:3608–3615. doi: 10.4049/jimmunol.0901391. [DOI] [PubMed] [Google Scholar]
- Del Vecchio M, Bajetta E, Canova S, Lotze MT, Wesa A, Parmiani G.et al. (2007Interleukin-12: biological properties and clinical application Clin Cancer Res 134677–4685. [DOI] [PubMed] [Google Scholar]
- Trinchieri G., and, Gerosa F. Immunoregulation by interleukin-12. J Leukoc Biol. 1996;59:505–511. doi: 10.1002/jlb.59.4.505. [DOI] [PubMed] [Google Scholar]
- Okada N, Iiyama S, Okada Y, Mizuguchi H, Hayakawa T, Nakagawa S.et al. (2005Immunological properties and vaccine efficacy of murine dendritic cells simultaneously expressing melanoma-associated antigen and interleukin-12 Cancer Gene Ther 1272–83. [DOI] [PubMed] [Google Scholar]
- Ojima T, Iwahashi M, Nakamura M, Matsuda K, Naka T, Nakamori M.et al. (2006The boosting effect of co-transduction with cytokine genes on cancer vaccine therapy using genetically modified dendritic cells expressing tumor-associated antigen Int J Oncol 28947–953. [PubMed] [Google Scholar]
- Iinuma H, Okinaga K, Fukushima R, Inaba T, Iwasaki K, Okinaga A.et al. (2006Superior protective and therapeutic effects of IL-12 and IL-18 gene-transduced dendritic neuroblastoma fusion cells on liver metastasis of murine neuroblastoma J Immunol 1763461–3469. [DOI] [PubMed] [Google Scholar]
- Ogawa F, Iinuma H., and, Okinaga K. Dendritic cell vaccine therapy by immunization with fusion cells of interleukin-2 gene-transduced, spleen-derived dendritic cells and tumour cells. Scand J Immunol. 2004;59:432–439. doi: 10.1111/j.0300-9475.2004.01411.x. [DOI] [PubMed] [Google Scholar]
- Minkis K, Kavanagh DG, Alter G, Bogunovic D, O'Neill D, Adams S.et al. (2008Type 2 Bias of T cells expanded from the blood of melanoma patients switched to type 1 by IL-12p70 mRNA-transfected dendritic cells Cancer Res 689441–9450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghiringhelli F, Ménard C, Terme M, Flament C, Taieb J, Chaput N.et al. (2005CD4+CD25+ regulatory T cells inhibit natural killer cell functions in a transforming growth factor-β-dependent manner J Exp Med 2021075–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang FL, Qin WJ, Wen WH, Tian F, Song B, Zhang Q.et al. (2007TGF-β insensitive dendritic cells: an efficient vaccine for murine prostate cancer Cancer Immunol Immunother 561785–1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinshtein N, Ventresca M, Margl R, Bernard D, Yang TC, Millar JB.et al. (2009High-dose chemotherapy augments the efficacy of recombinant adenovirus vaccines and improves the therapeutic outcome Cancer Gene Ther 16338–350. [DOI] [PubMed] [Google Scholar]
- Ojima T, Iwahashi M, Nakamura M, Matsuda K, Nakamori M, Ueda K.et al. (2007Benefits of gene transduction of granulocyte macrophage colony-stimulating factor in cancer vaccine using genetically modified dendritic cells Int J Oncol 31931–939. [PubMed] [Google Scholar]
- Yamaguchi T, Kawabata K, Koizumi N, Sakurai F, Nakashima K, Sakurai H.et al. (2007Role of MyD88 and TLR9 in the innate immune response elicited by serotype 5 adenoviral vectors Hum Gene Ther 18753–762. [DOI] [PubMed] [Google Scholar]
- Luketic L, Delanghe J, Sobol PT, Yang P, Frotten E, Mossman KL.et al. (2007Antigen presentation by exosomes released from peptide-pulsed dendritic cells is not suppressed by the presence of active CTL J Immunol 1795024–5032. [DOI] [PubMed] [Google Scholar]
- Verdijk P, Aarntzen EH, Lesterhuis WJ, Boullart AC, Kok E, van Rossum MM.et al. (2009Limited amounts of dendritic cells migrate into the T-cell area of lymph nodes but have high immune activating potential in melanoma patients Clin Cancer Res 152531–2540. [DOI] [PubMed] [Google Scholar]
- Okada N, Mori N, Koretomo R, Okada Y, Nakayama T, Yoshie O.et al. (2005Augmentation of the migratory ability of DC-based vaccine into regional lymph nodes by efficient CCR7 gene transduction Gene Ther 12129–139. [DOI] [PubMed] [Google Scholar]
- Kang TH, Bae HC, Kim SH, Seo SH, Son SW, Choi EY.et al. (2009Modification of dendritic cells with interferon-γ-inducible protein-10 gene to enhance vaccine potency J Gene Med 11889–898. [DOI] [PubMed] [Google Scholar]
- Bayry J, Tchilian EZ, Davies MN, Forbes EK, Draper SJ, Kaveri SV.et al. (2008In silico identified CCR4 antagonists target regulatory T cells and exert adjuvant activity in vaccination Proc Natl Acad Sci USA 10510221–10226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang SC, Hillinger S, Riedl K, Zhang L, Zhu L, Huang M.et al. (2004Intratumoral administration of dendritic cells overexpressing CCL21 generates systemic antitumor responses and confers tumor immunity Clin Cancer Res 102891–2901. [DOI] [PubMed] [Google Scholar]
- Kim A, Noh YW, Kim KD, Jang YS, Choe YK., and, Lim JS. Activated natural killer cell-mediated immunity is required for the inhibition of tumor metastasis by dendritic cell vaccination. Exp Mol Med. 2004;36:428–443. doi: 10.1038/emm.2004.55. [DOI] [PubMed] [Google Scholar]
- Karimi K, Boudreau JE, Fraser K, Liu H, Delanghe J, Gauldie J.et al. (2008Enhanced antitumor immunity elicited by dendritic cell vaccines is a result of their ability to engage both CTL and IFN γ-producing NK cells Mol Ther 16411–418. [DOI] [PubMed] [Google Scholar]
- Boudreau JE, Bridle BW, Stephenson KB, Jenkins KM, Brunellière J., and, Bramson JL.et al. (2010Recombinant vesicular stomatitis virus transduction of dendritic cells enhances their ability to prime innate and adaptive antitumor immunity Mol Ther 171465–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Broeke LT, Daschbach E, Thomas EK, Andringa G., and, Berzofsky JA. Dendritic cell-induced activation of adaptive and innate antitumor immunity. J Immunol. 2003;171:5842–5852. doi: 10.4049/jimmunol.171.11.5842. [DOI] [PubMed] [Google Scholar]
- Ribas A, Wargo JA, Comin-Anduix B, Sanetti S, Schumacher LY, McLean C.et al. (2004Enhanced tumor responses to dendritic cells in the absence of CD8-positive cells J Immunol 1724762–4769. [DOI] [PubMed] [Google Scholar]
- Steel JC, Ramlogan CA, Yu P, Sakai Y, Forni G, Waldmann TA.et al. (2010Interleukin-15 and its receptor augment dendritic cell vaccination against the neu oncogene through the induction of antibodies partially independent of CD4 help Cancer Res 701072–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green MC, Murray JL., and, Hortobagyi GN. Monoclonal antibody therapy for solid tumors. Cancer Treat Rev. 2000;26:269–286. doi: 10.1053/ctrv.2000.0176. [DOI] [PubMed] [Google Scholar]
- Mossoba ME, Walia JS, Rasaiah VI, Buxhoeveden N, Head R., and, Ying C.et al. (2008Tumor protection following vaccination with low doses of lentivirally transduced DCs expressing the self-antigen erbB2 Mol Ther 16607–617. [DOI] [PubMed] [Google Scholar]
- Sakai Y, Morrison BJ, Burke JD, Park JM, Terabe M, Janik JE.et al. (2004Vaccination by genetically modified dendritic cells expressing a truncated neu oncogene prevents development of breast cancer in transgenic mice Cancer Res 648022–8028. [DOI] [PubMed] [Google Scholar]
- Boczkowski D, Lee J, Pruitt S., and, Nair S. Dendritic cells engineered to secrete anti-GITR antibodies are effective adjuvants to dendritic cell-based immunotherapy. Cancer Gene Ther. 2009;16:900–911. doi: 10.1038/cgt.2009.39. [DOI] [PubMed] [Google Scholar]
- Luci C., and, Tomasello E. Natural killer cells: detectors of stress. Int J Biochem Cell Biol. 2008;40:2335–2340. doi: 10.1016/j.biocel.2008.05.001. [DOI] [PubMed] [Google Scholar]
- Wargo JA, Schumacher LY, Comin-Anduix B, Dissette VB, Glaspy JA., and, McBride WH.et al. (2005Natural killer cells play a critical role in the immune response following immunization with melanoma-antigen-engineered dendritic cells Cancer Gene Ther 12516–527. [DOI] [PubMed] [Google Scholar]
- Morandi B, Mortara L, Carrega P, Cantoni C, Costa G, Accolla RS.et al. (2009NK cells provide helper signal for CD8+ T cells by inducing the expression of membrane-bound IL-15 on DCs Int Immunol 21599–606. [DOI] [PubMed] [Google Scholar]
- Osada T, Clay T, Hobeika A, Lyerly HK., and, Morse MA. NK cell activation by dendritic cell vaccine: a mechanism of action for clinical activity. Cancer Immunol Immunother. 2006;55:1122–1131. doi: 10.1007/s00262-005-0089-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo CY, Clay TM, Lyerly HK, Morse MA., and, Osada T. Role of natural killer cell function in dendritic cell-based vaccines. Expert Rev Vaccines. 2006;5:66–65. doi: 10.1586/14760584.5.1.55. [DOI] [PubMed] [Google Scholar]
- Van Tendeloo VF, Van de Velde A, Van Driessche A, Cools N, Anguille S, Ladell K.et al. (2010Induction of complete and molecular remissions in acute myeloid leukemia by Wilms' tumor 1 antigen-targeted dendritic cell vaccination Proc Natl Acad Sci USA 10713824–13829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas M, Schachterle W, Oberle K, Aichele P., and, Diefenbach A. Dendritic cells prime natural killer cells by trans-presenting interleukin 15. Immunity. 2007;26:503–517. doi: 10.1016/j.immuni.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochweller K, Striegler J, Hämmerling GJ., and, Garbi N. A novel CD11c.DTR transgenic mouse for depletion of dendritic cells reveals their requirement for homeostatic proliferation of natural killer cells. Eur J Immunol. 2008;38:2776–2783. doi: 10.1002/eji.200838659. [DOI] [PubMed] [Google Scholar]
- Walzer T, Dalod M, Robbins SH, Zitvogel L., and, Vivier E. Natural-killer cells and dendritic cells: “l'union fait la force”. Blood. 2005;106:2252–2258. doi: 10.1182/blood-2005-03-1154. [DOI] [PubMed] [Google Scholar]
- Gustafsson K, Ingelsten M, Bergqvist L, Nyström J, Andersson B., and, Karlsson-Parra A. Recruitment and activation of natural killer cells in vitro by a human dendritic cell vaccine. Cancer Res. 2008;68:5965–5971. doi: 10.1158/0008-5472.CAN-07-6494. [DOI] [PubMed] [Google Scholar]
- Gilboa E. DC-based cancer vaccines. J Clin Invest. 2007;117:1195–1203. doi: 10.1172/JCI31205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benko S, Magyarics Z, Szabó A., and, Rajnavölgyi E. Dendritic cell subtypes as primary targets of vaccines: the emerging role and cross-talk of pattern recognition receptors. Biol Chem. 2008;389:469–485. doi: 10.1515/bc.2008.054. [DOI] [PubMed] [Google Scholar]
- Drillien R, Spehner D., and, Hanau D. Modified vaccinia virus Ankara induces moderate activation of human dendritic cells. J Gen Virol. 2004;85 Pt 8:2167–2175. doi: 10.1099/vir.0.79998-0. [DOI] [PubMed] [Google Scholar]
- Ahmed M, Mitchell LM, Puckett S, Brzoza-Lewis KL, Lyles DS., and, Hiltbold EM. Vesicular stomatitis virus M protein mutant stimulates maturation of Toll-like receptor 7 (TLR7)-positive dendritic cells through TLR-dependent and -independent mechanisms. J Virol. 2009;83:2962–2975. doi: 10.1128/JVI.02030-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su Z, Dannull J, Heiser A, Yancey D, Pruitt S, Madden J.et al. (2003Immunological and clinical responses in metastatic renal cancer patients vaccinated with tumor RNA-transfected dendritic cells Cancer Res 632127–2133. [PubMed] [Google Scholar]
- Breckpot K, Aerts JL., and, Thielemans K. Lentiviral vectors for cancer immunotherapy: transforming infectious particles into therapeutics. Gene Ther. 2007;14:847–862. doi: 10.1038/sj.gt.3302947. [DOI] [PubMed] [Google Scholar]
- Napolitani G, Rinaldi A, Bertoni F, Sallusto F., and, Lanzavecchia A. Selected Toll-like receptor agonist combinations synergistically trigger a T helper type 1-polarizing program in dendritic cells. Nat Immunol. 2005;6:769–776. doi: 10.1038/ni1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boudreau JE, Stephenson KB, Wang F, Ashkar AA, Mossman KL, Lenz LL.et al. (2011IL-15 and type I interferon are required for activation of tumoricidal NK cells by virus-infected dendritic cells Cancer Resin press. [DOI] [PubMed]
- Vujanovic L, Szymkowski DE, Alber S, Watkins SC, Vujanovic NL., and, Butterfield LH. Virally infected and matured human dendritic cells activate natural killer cells via cooperative activity of plasma membrane-bound TNF and IL-15. Blood. 2010;116:575–583. doi: 10.1182/blood-2009-08-240325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harenberg A, Guillaume F, Ryan EJ, Burdin N., and, Spada F. Gene profiling analysis of ALVAC infected human monocyte derived dendritic cells. Vaccine. 2008;26:5004–5013. doi: 10.1016/j.vaccine.2008.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan EJ, Harenberg A., and, Burdin N. The Canarypox-virus vaccine vector ALVAC triggers the release of IFN-γ by Natural Killer (NK) cells enhancing Th1 polarization. Vaccine. 2007;25:3380–3390. doi: 10.1016/j.vaccine.2006.12.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Driessche A, Van de Velde AL, Nijs G, Braeckman T, Stein B, De Vries JM.et al. (2009Clinical-grade manufacturing of autologous mature mRNA-electroporated dendritic cells and safety testing in acute myeloid leukemia patients in a phase I dose-escalation clinical trial Cytotherapy 11653–668. [DOI] [PubMed] [Google Scholar]
- Van Camp K, Cools N, Stein B, Van de Velde A, Goossens H, Berneman ZN.et al. (2010Efficient mRNA electroporation of peripheral blood mononuclear cells to detect memory T cell responses for immunomonitoring purposes J Immunol Methods 3541–10. [DOI] [PubMed] [Google Scholar]
- Mellman I., and, Steinman RM. Dendritic cells: specialized and regulated antigen processing machines. Cell. 2001;106:255–258. doi: 10.1016/s0092-8674(01)00449-4. [DOI] [PubMed] [Google Scholar]
- Heiser A, Maurice MA, Yancey DR, Coleman DM, Dahm P., and, Vieweg J. Human dendritic cells transfected with renal tumor RNA stimulate polyclonal T-cell responses against antigens expressed by primary and metastatic tumors. Cancer Res. 2001;61:3388–3393. [PubMed] [Google Scholar]
- Heiser A, Maurice MA, Yancey DR, Wu NZ, Dahm P, Pruitt SK.et al. (2001Induction of polyclonal prostate cancer-specific CTL using dendritic cells transfected with amplified tumor RNA J Immunol 1662953–2960. [DOI] [PubMed] [Google Scholar]
- Kyte JA, Mu L, Aamdal S, Kvalheim G, Dueland S, Hauser M.et al. (2006Phase I/II trial of melanoma therapy with dendritic cells transfected with autologous tumor-mRNA Cancer Gene Ther 13905–918. [DOI] [PubMed] [Google Scholar]
- Tanimoto T, Hori A., and, Kami M. Sipuleucel-T immunotherapry for castration-resistant prostate cancer. N Engl J Med. 2010;363:411–422. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- Scandella E, Men Y, Gillessen S, Förster R., and, Groettrup M. Prostaglandin E2 is a key factor for CCR7 surface expression and migration of monocyte-derived dendritic cells. Blood. 2002;100:1354–1361. doi: 10.1182/blood-2001-11-0017. [DOI] [PubMed] [Google Scholar]
- Luft T, Jefford M, Luetjens P, Toy T, Hochrein H, Masterman KA.et al. (2002Functionally distinct dendritic cell (DC) populations induced by physiologic stimuli: prostaglandin E(2) regulates the migratory capacity of specific DC subsets Blood 1001362–1372. [DOI] [PubMed] [Google Scholar]
- Boczkowski D., and, Nair S. RNA as performance-enhancers for dendritic cells. Expert Opin Biol Ther. 2010;10:563–574. doi: 10.1517/14712591003614749. [DOI] [PubMed] [Google Scholar]
- Papewalis C, Jacobs B, Wuttke M, Ullrich E, Baehring T, Fenk R.et al. (2008IFN-α skews monocytes into CD56+-expressing dendritic cells with potent functional activities in vitro and in vivo J Immunol 1801462–1470. [DOI] [PubMed] [Google Scholar]
- Czerniecki BJ, Koski GK, Koldovsky U, Xu S, Cohen PA, Mick R.et al. (2007Targeting HER-2/neu in early breast cancer development using dendritic cells with staged interleukin-12 burst secretion Cancer Res 671842–1852. [DOI] [PubMed] [Google Scholar]
- Padovan E, Spagnoli GC, Ferrantini M., and, Heberer M. IFN-α2a induces IP-10/CXCL10 and MIG/CXCL9 production in monocyte-derived dendritic cells and enhances their capacity to attract and stimulate CD8+ effector T cells. J Leukoc Biol. 2002;71:669–676. [PubMed] [Google Scholar]
- Di Pucchio T, Pilla L, Capone I, Ferrantini M, Montefiore E, Urbani F.et al. (2006Immunization of stage IV melanoma patients with Melan-A/MART-1 and gp100 peptides plus IFN-α results in the activation of specific CD8+ T cells and monocyte/dendritic cell precursors Cancer Res 664943–4951. [DOI] [PubMed] [Google Scholar]
- Parlato S, Santini SM, Lapenta C, Di Pucchio T, Logozzi M, Spada M.et al. (2001Expression of CCR-7, MIP-3β, and Th-1 chemokines in type I IFN-induced monocyte-derived dendritic cells: importance for the rapid acquisition of potent migratory and functional activities Blood 983022–3029. [DOI] [PubMed] [Google Scholar]
- Kuwashima N, Nishimura F, Eguchi J, Sato H, Hatano M, Tsugawa T.et al. (2005Delivery of dendritic cells engineered to secrete IFN-α into central nervous system tumors enhances the efficacy of peripheral tumor cell vaccines: dependence on apoptotic pathways J Immunol 1752730–2740. [DOI] [PubMed] [Google Scholar]
- Mulé JJ. Dendritic cell-based vaccines for pancreatic cancer and melanoma. Ann N Y Acad Sci. 2009;1174:33–40. doi: 10.1111/j.1749-6632.2009.04936.x. [DOI] [PubMed] [Google Scholar]
- Butterfield LH., and, Vujanovic L. New approaches to the development of adenoviral dendritic cell vaccines in melanoma. Curr Opin Investig Drugs. 2010;11:1399–1408. [PMC free article] [PubMed] [Google Scholar]
- Mazzolini G, Alfaro C, Sangro B, Feijoó E, Ruiz J, Benito A.et al. (2005Intratumoral injection of dendritic cells engineered to secrete interleukin-12 by recombinant adenovirus in patients with metastatic gastrointestinal carcinomas J Clin Oncol 23999–1010. [DOI] [PubMed] [Google Scholar]
- Feijoó E, Alfaro C, Mazzolini G, Serra P, Peñuelas I, Arina A.et al. (2005Dendritic cells delivered inside human carcinomas are sequestered by interleukin-8 Int J Cancer 116275–281. [DOI] [PubMed] [Google Scholar]
- Adam C, King S, Allgeier T, Braumüller H, Lüking C, Mysliwietz J.et al. (2005DC-NK cell cross talk as a novel CD4+ T-cell-independent pathway for antitumor CTL induction Blood 106338–344. [DOI] [PubMed] [Google Scholar]
- Obeid M, Tesniere A, Ghiringhelli F, Fimia GM, Apetoh L, Perfettini JL.et al. (2007Calreticulin exposure dictates the immunogenicity of cancer cell death Nat Med 1354–61. [DOI] [PubMed] [Google Scholar]
- Kirkwood JM, Tarhini AA, Panelli MC, Moschos SJ, Zarour HM, Butterfield LH.et al. (2008Next generation of immunotherapy for melanoma J Clin Oncol 263445–3455. [DOI] [PubMed] [Google Scholar]
- Ojima T, Iwahashi M, Nakamura M, Matsuda K, Nakamori M, Ueda K.et al. (2007Successful cancer vaccine therapy for carcinoembryonic antigen (CEA)-expressing colon cancer using genetically modified dendritic cells that express CEA and T helper-type 1 cytokines in CEA transgenic mice Int J Cancer 120585–593. [DOI] [PubMed] [Google Scholar]
- Ebihara T, Masuda H, Akazawa T, Shingai M, Kikuta H, Ariga T.et al. (2007Induction of NKG2D ligands on human dendritic cells by TLR ligand stimulation and RNA virus infection Int Immunol 191145–1155. [DOI] [PubMed] [Google Scholar]
- Tuyaerts S, Van Meirvenne S, Bonehill A, Heirman C, Corthals J, Waldmann H.et al. (2007Expression of human GITRL on myeloid dendritic cells enhances their immunostimulatory function but does not abrogate the suppressive effect of CD4+CD25+ regulatory T cells J Leukoc Biol 8293–105. [DOI] [PubMed] [Google Scholar]
- Wiethe C, Dittmar K, Doan T, Lindenmaier W., and, Tindle R. Provision of 4-1BB ligand enhances effector and memory CTL responses generated by immunization with dendritic cells expressing a human tumor-associated antigen. J Immunol. 2003;170:2912–2922. doi: 10.4049/jimmunol.170.6.2912. [DOI] [PubMed] [Google Scholar]
- Song SY., and, Kim HS. Strategies to improve dendritic cell-based immunotherapy against cancer. Yonsei Med J. 2004;45 Suppl:48–52. doi: 10.3349/ymj.2004.45.Suppl.48. [DOI] [PubMed] [Google Scholar]
- Nair SK, Morse M, Boczkowski D, Cumming RI, Vasovic L, Gilboa E.et al. (2002Induction of tumor-specific cytotoxic T lymphocytes in cancer patients by autologous tumor RNA-transfected dendritic cells Ann Surg 235540–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pecher G, Häring A, Kaiser L., and, Thiel E. Mucin gene (MUC1) transfected dendritic cells as vaccine: results of a phase I/II clinical trial. Cancer Immunol Immunother. 2002;51:669–673. doi: 10.1007/s00262-002-0317-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse MA, Clay TM, Hobeika AC, Osada T, Khan S, Chui S.et al. (2005Phase I study of immunization with dendritic cells modified with fowlpox encoding carcinoembryonic antigen and costimulatory molecules Clin Cancer Res 113017–3024. [DOI] [PubMed] [Google Scholar]
- Caruso DA, Orme LM, Neale AM, Radcliff FJ, Amor GM, Maixner W.et al. (2004Results of a phase 1 study utilizing monocyte-derived dendritic cells pulsed with tumor RNA in children and young adults with brain cancer Neuro-oncology 6236–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caruso DA, Orme LM, Amor GM, Neale AM, Radcliff FJ, Downie P.et al. (2005Results of a Phase I study utilizing monocyte-derived dendritic cells pulsed with tumor RNA in children with Stage 4 neuroblastoma Cancer 1031280–1291. [DOI] [PubMed] [Google Scholar]
- Mu LJ, Kyte JA, Kvalheim G, Aamdal S, Dueland S, Hauser M.et al. (2005Immunotherapy with allotumour mRNA-transfected dendritic cells in androgen-resistant prostate cancer patients Br J Cancer 93749–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markovic SN, Dietz AB, Greiner CW, Maas ML, Butler GW, Padley DJ.et al. (2006Preparing clinical-grade myeloid dendritic cells by electroporation-mediated transfection of in vitro amplified tumor-derived mRNA and safety testing in stage IV malignant melanoma J Transl Med 435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butterfield LH, Comin-Anduix B, Vujanovic L, Lee Y, Dissette VB, Yang JQ.et al. (2008Adenovirus MART-1-engineered autologous dendritic cell vaccine for metastatic melanoma J Immunother 31294–309. [DOI] [PMC free article] [PubMed] [Google Scholar]