Abstract
Rationale
Lung function measures are heritable traits that predict population morbidity and mortality and are essential for the diagnosis of chronic obstructive pulmonary disease (COPD). Variations in many genes have been reported to affect these traits, but attempts at replication have provided conflicting results. Recently, we undertook a meta-analysis of Genome Wide Association Study (GWAS) results for lung function measures in 20,288 individuals from the general population (the SpiroMeta consortium).
Objectives
To comprehensively analyse previously reported genetic associations with lung function measures, and to investigate whether single nucleotide polymorphisms (SNPs) in these genomic regions are associated with lung function in a large population sample.
Methods
We analysed association for SNPs tagging 130 genes and 48 intergenic regions (+/−10 kb), after conducting a systematic review of the literature in the PubMed database for genetic association studies reporting lung function associations.
Results
The analysis included 16,936 genotyped and imputed SNPs. No loci showed overall significant association for FEV1 or FEV1/FVC traits using a carefully defined significance threshold of 1.3×10−5. The most significant loci associated with FEV1 include SNPs tagging MACROD2 (P = 6.81×10−5), CNTN5 (P = 4.37×10−4), and TRPV4 (P = 1.58×10−3). Among ever-smokers, SERPINA1 showed the most significant association with FEV1 (P = 8.41×10−5), followed by PDE4D (P = 1.22×10−4). The strongest association with FEV1/FVC ratio was observed with ABCC1 (P = 4.38×10−4), and ESR1 (P = 5.42×10−4) among ever-smokers.
Conclusions
Polymorphisms spanning previously associated lung function genes did not show strong evidence for association with lung function measures in the SpiroMeta consortium population. Common SERPINA1 polymorphisms may affect FEV1 among smokers in the general population.
Introduction
Pulmonary function is usually assessed by measurement of forced expiratory volume in one second (FEV1), forced vital capacity (FVC), and the ratio of FEV1 to FVC. The measurements are integral to the diagnosis of chronic obstructive pulmonary disease (COPD), and also are important long term predictors of population morbidity and mortality [1]. Reduced FEV1/FVC defines airways obstruction; whereas reduced FEV1 grades the severity of obstruction [2].
Pulmonary function is determined by both environmental and genetic factors. Tobacco smoking is the major environmental risk factor for the development of COPD. A genetic contribution to pulmonary function is well established with heritability estimates reaching 77 percent for FEV1 [3]. Linkage analyses within families have previously identified multiple genomic regions associated with spirometry measures and respiratory diseases. In addition, candidate gene studies have identified more than 100 genes which have been suggested to contribute to variability in lung function. The majority have been studied because of their potential pathophysiological role in the development of COPD. Some genes have been examined for association with lung function measurements in individuals with other specific respiratory diseases (most commonly asthma), or to a lesser extent, in the general population. With the exception of SERPINA1, which is the best documented genetic risk factor to influence the development of COPD [4], these genes have not shown consistent associations across different studies [5], [6].
Recently, we established the SpiroMeta consortium and published a large collective meta-analysis of lung function genome-wide association studies (GWAS) in 20,288 individuals of European origin, with follow-up of top SNPs in a further 54,276 individuals [7], [8]. Our study confirmed the hedgehog interacting protein (HHIP) association previously published [9], [10] and identified five new loci associated with FEV1 or FEV1/FVC ratio including tensin 1 gene (TNS1), glutathione S-transferase, C-terminal domain containing (GSTCD), 5-hydroxytryptamine receptor 4 (HTR4), advanced glycosylation end product-specific receptor (AGER), and thrombospondin, type I, domain containing 4 (THSD4). A study with similar design by the CHARGE consortium also identified HHIP, AGER, HTR4, and GSTCD, and in addition suggested a potential role of five additional genes (G protein-coupled receptor 126 (GPR126), a disintegrin and metalloproteinase domain 19 (ADAM19), family with sequence similarity 13, member A (FAM13A), patched homolog 1 (PTCH1), and phosphotyrosine interaction domain containing (PID1) [8].
The identification of these genes offers potential insight into the pathophysiology of altered lung function. The SpiroMeta consortium provides a powerful resource in which to study genetic associations with lung function. We aimed to comprehensively evaluate whether genes studied in candidate gene or small genome-wide association studies, and reported to be associated with lung function or COPD in these studies, were associated with lung function measures in this large general population sample.
Results
Literature search
The literature search identified 1719 publications. Of these, 104 reported one or more genetic associations: these are listed in text S1 in the online supporting information. These publications varied according to their study designs and the populations studied. 47 papers reported association with COPD using case control or family based designs. The remaining literature reported association with lung function traits within populations with specific respiratory diseases (asthma (26) and COPD (17)), or in general population cohorts (14). Nine publications studied other populations which included patients with cystic fibrosis (2), SERPINA1 deficiency (2), cotton and grain workers (2), lung cancer (1), fire fighters (1) and post myocardial infarction (MI) patients (1). Some papers reported more than one endpoint.
These 104 relevant publications identified 130 genes and 48 intergenic SNPs. We investigated association between FEV1 and FEV1/FVC and each of the 16,936 genotyped and imputed SNPs spanning these regions in the SpiroMeta dataset.
Contribution of all tested genes to lung function measures in SpiroMeta
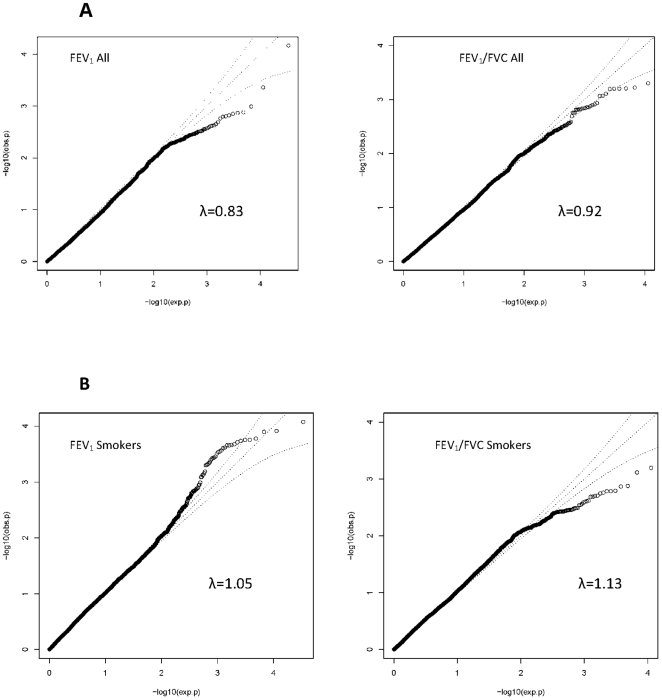
Quantile-quantile (Q-Q) plots did not show large deviations between observed and expected P values for FEV1 and FEV1/FVC in all participants and for FEV1/FVC in ever-smokers (Figure 1). The plot of FEV1 in ever-smokers, however, shows slight deviations for high signal SNPs. The genomic inflation factor, λ for FEV1 is 0.83 in all individuals and 1.05 in smokers; λ for FEV1/FVC in all individuals is 0.92 and 1.13 in smokers.
Figure 1. Quantile-quantile (Q-Q) plots of association results for FEV1 and FEV1/FVC.
The Q-Q plot of association is shown for all individuals in Panel A, and separately for ever-smokers only in panel B. Q-Q plots compare the observed P values (obs.p) to expected P values (exp.p) on the logarithmic scale under the null hypothesis of no significant association. λ: Lambda.
Using the Bonferroni corrected P value threshold of 1.3×10−5, none of the tested SNPs demonstrated significant association with either FEV1 or FEV1/FVC.
Association results in all individuals
In order to examine possible signals in greater detail, we also explored region plots for the top SNPs identified (SNPs with the lowest P values). The three top loci with the most significant P values for all regions tested in all individuals are presented in table 1.
Table 1. Association results for the three most significantly associated loci.
| Gene | Locus | SNP | SNP function | coded allele | Coded allele frequency | N eff | Beta | Se | P |
| FEV1 All individuals | |||||||||
| MACROD2 | 20p12.1 | rs204652 | Intron | G | 0.983 | 13551 | −0.187 | 0.047 | 6.81×10−5 |
| CNTN5 | 11q21-q22.2 | rs17133553 | Intron | T | 0.966 | 13669 | −0.100 | 0.029 | 4.37×10−4 |
| MTHFD1L | 6q25.1 | rs803450 | Intron | G | 0.625 | 18497 | 0.036 | 0.011 | 1.03×10−3 |
| FEV1 Smokers | |||||||||
| SERPINA1 | 14q32.13 | rs3748312 | Intron | T | 0.167 | 9338 | 0.085 | 0.022 | 8.41×10−5 |
| PDE4D | 5q12 | rs298028 | Intron | T | 0.283 | 10829 | −0.069 | 0.018 | 1.22×10−4 |
| MACROD2 | 20p12.1 | rs204652 | Intron | G | 0.983 | 6872 | −0.251 | 0.067 | 1.67×10−4 |
| FEV1/FVC All individuals | |||||||||
| ABCC1 | 16p13.1 | rs3887893 | Intron | T | 0.625 | 15509 | −0.043 | 0.012 | 4.38×10−4 |
| ESR1 | 6q25.1 | rs11155818 | Intron | G | 0.992 | 12571 | 0.185 | 0.053 | 5.02×10−4 |
| CNTN5 | 11q21-q22.2 | rs1216170 | Intron | C | 0.284 | 18863 | 0.039 | 0.011 | 6.02×10−4 |
| FEV1/FVC Smokers | |||||||||
| ESR1 | 6q25.1 | rs9322335 | Intron | T | 0.217 | 9495 | −0.061 | 0.018 | 5.42×10−4 |
| RHBDD1 | 2q36.3 | rs1864271 | Intron | G | 0.708 | 7385 | 0.066 | 0.019 | 6.40×10−4 |
| MTHFD1L | 6q25.1 | rs1738567 | Intron | C | 0.367 | 10668 | 0.046 | 0.014 | 1.33×10−3 |
The table shows the three most significant loci associated with FEV1 and FEV1/FVC ratio in all individuals and ever-Smokers. N eff: the effective sample size. Beta: regression coefficient on a transformed scale. Se: standard error. P: P value. Coded allele frequency based on HapMap Release 24. MACROD2: MACRO domain containing 2. CNTN5: Contactin 5. MTHFD1L Methylenetetrahydrofolate dehydrogenase (NADP+ dependent) 1-like. SERPINA1: serpin peptidase inhibitor, clade A, member 1 (alpha-1 antitrypsin AAT). PDE4D: Phosphodiesterase 4D, cAMP-specific (phosphodiesterase E3 dunce homolog, Drosophila). ABCC1: ATP-binding cassette, sub-family C, member 1. ESR1: estrogen receptor 1. RHBDD1: rhomboid domain containing 1.
Among all individuals, the strongest association with FEV1 was with rs204652 in MACRO domain containing 2 (MACROD2) on chromosome 20. SNP rs17133553 in Contactin 5 (CNTN5) on chromosome 11 was the second top locus for association with FEV1 and third for FEV1/FVC ratio. SNP rs803450 in Methylenetetrahydrofolate dehydrogenase (NADP+ dependent) 1-like (MTHFD1L) on chromosome 6 showed association with FEV1 in all individuals. For FEV1/FVC ratio in all individuals the strongest association was with rs3887893 in ATP-binding cassette, sub-family C, member 1 (ABCC1) on chromosome 16, the second strongest signal was for rs11155818 in estrogen receptor 1(ESR1) on chromosome 6.
The region association plots around the most significant SNPs associated with FEV1 and FEV1/FVC in all individuals provide little evidence from supporting SNPs to suggest strong regions of association in MACROD2, CNTN5, MTHFD1L, and ESR1, and ABCC1 in these data (See figure S1 in the online supporting information).
Association results in ever-smokers
To study the impact of smoking on potential genetic associations with lung function, we repeated the analysis restricted to individuals who had ever smoked (ever-smokers). The most significant loci identified are shown in table 1.
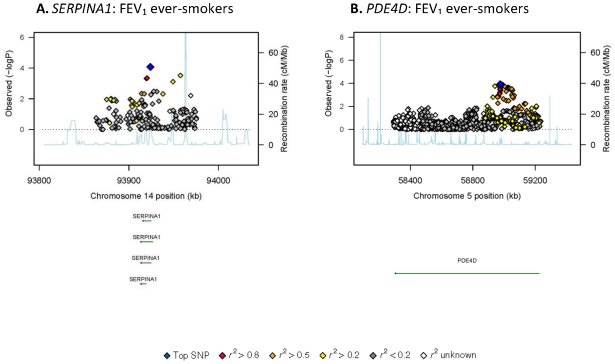
Among ever-smokers, rs3748312 in serpin peptidase inhibitor, clade A, member 1 (SERPINA1) on chromosome 14, also known as alpha-1 antitrypsin (AAT) showed the strongest association with FEV1. SNP rs298028 in Phosphodiesterase 4D, cAMP-specific (phosphodiesterase E3 dunce homolog, Drosophila) (PDE4D) on chromosome 5 showed the second strongest association with FEV1, followed by MACROD2.
The strongest association with FEV1/FVC ratio among smokers was observed with rs9322335 in 1(ESR1) on chromosome 6. The second strongest association was rs1864271 in with rhomboid domain containing 1 (RHBDD1) on chromosome 2, followed by rs1738567 in (MTHFD1L) on chromosome 6. The region association plots for SERPINA1 and PDE4D among ever-smokers (figure 2) show some supportive evidence for the association of these two loci. The region association plots for the additional loci among ever-smokers reported in table 1 are shown in figure S2 in the online supporting information.
Figure 2. Regional association plots for SERPINA1 (A) and PDE4D among ever-smokers (B) in SpiroMeta.
Statistical significance of each SNP on the −log10 scale as a function of chromosome position (NCBI build 36). The sentinel SNP at each locus is shown in blue; the correlations (r 2) of each of the surrounding SNPs to the sentinel SNP are shown in the indicated colours. The relevant trait (FEV1 or FEV1/FVC ratio) is indicated for each plot. Recombination rate is shown in pale blue.
Association results excluding loci identified in previous GWAS
Because some of the regions identified were observed in the previously published small GWAS studies included in our literature search, we also present the top three genes for the relevant end points after excluding GWAS hits (Table 2).
Table 2. Association results for the most significant loci excluding genes identified in GWAS.
| gene | locus | SNP | SNP function | coded allele | Coded allele Frequency | N eff | Beta | se | P |
| FEV1 All | |||||||||
| PDE4D | 5q12 | rs172362 | Intron | C | 0.133 | 18929 | −0.048 | 0.015 | 1.36×10−3 |
| TRPV4 | 12q24.1 | rs3742030 | Missense | G | 0.992 | 17591 | −0.110 | 0.035 | 1.58×10−3 |
| NAT2 | 8p22 | rs6988857 | Intergenic | T | 0.241 | 20080 | 0.035 | 0.011 | 2.37×10−3 |
| FEV1 Smokers | |||||||||
| SERPINA1 | 14q32.13 | rs3748312 | Intron | T | 0.167 | 9338 | 0.085 | 0.022 | 8.41×10−5 |
| PDE4D | 5q12 | rs298028 | Intron | T | 0.283 | 20829 | −0.069 | 0.018 | 1.22×10−4 |
| BCL2 | 18q21.3 | rs2850760 | Intron | T | 0.425 | 10888 | 0.050 | 0.014 | 4.66×10−4 |
| FEV1/FVC All | |||||||||
| ABCC1 | 16p13.1 | rs3887893 | Intron | T | 0.625 | 15509 | −0.043 | 0.012 | 4.38×10−4 |
| ESR1 | 6q25.1 | rs11155818 | Intron | G | 0.992 | 12571 | 0.185 | 0.053 | 5.02×10−4 |
| AIF1 | 6p21.3 | rs3132451 | 5′near gene | G | 0.883 | 19889 | 0.045 | 0.014 | 7.84×10−4 |
| FEV1/FVC Smokers | |||||||||
| ESR1 | 6q25.1 | rs9322335 | Intron | T | 0.217 | 9495 | −0.061 | 0.018 | 5.42×10−4 |
| ABCC1 | 16p13.1 | rs3887893 | Intron | T | 0.625 | 8156 | −0.054 | 0.017 | 1.36×10−3 |
| CD22 | 19q13.1 | rs7251526 | Intron | T | 0.246 | 8328 | −0.054 | 0.018 | 2.00×10−3 |
The table shows association results for the three most significant loci associated with FEV1 and FEV1/FVC, in all individuals and in ever-smokers after excluding genes identified in GWAS. N eff: the effective sample size. Beta: regression coefficient on a transformed scale. Se: standard error. P: P value. Coded allele frequency based on HapMap Release 24. PDE4D: Phosphodiesterase 4D, cAMP-specific (phosphodiesterase E3 dunce homolog, Drosophila). TRPV4: transient receptor potential cation channel, subfamily V, member 4. NAT2: N-acetyltransferase 2. SERPINA1: serpin peptidase inhibitor, clade A, member 1 (alpha-1 antitrypsin AAT). BCL2: B-cell CLL/lymphoma 2. ABCC1: ATP-binding cassette, sub-family C, member 1. AIF1: allograft inflammatory factor 1. ESR1: estrogen receptor 1. CD22: cluster of differentiation; CD22 molecule.
The additional genes identified in this analysis for association with FEV1 among all individuals were the transient receptor potential cation channel, subfamily V, member 4 (TRPV4) on chromosome 12, and N-acetyltransferase 2 (NAT2) on chromosome 8. Among ever-smokers, association results for FEV1 identified B-cell CLL/lymphoma 2 (BCL2) on chromosome 18. Association results for FEV1/FVC ratio identified allograft inflammatory factor 1(AIF1) on chromosome 6 among all individuals, and cluster of differentiation; CD22 molecule (CD22) on chromosome 19 among ever-smokers. The region association plots for the most significant loci in table 2 and not presented earlier are shown in figure S3 in the online supporting information. The plots show some additional support for all presented loci except for ABCC1 among ever-smokers.
Discussion
In the SpiroMeta study, we generated a comprehensive dataset to analyse associations between genetic variants and lung function in the general population [7]. There have been many small previous studies, mostly of individual candidate genes examining association with lung function, which have produced conflicting results. Therefore, in this paper, we undertook a comprehensive literature review to identify relevant gene regions and analysed potential associations with FEV1 and FEV1/FVC ratio in all individuals within SpiroMeta. In addition, given the impact of smoking on lung function, we also analysed the associations separately in ever-smokers. There were no strong association signals in never-smokers group (data available on request).
The main conclusion from this study is that, within 178 previously reported regions, we found no SNP associations which exceeded the significance threshold (P<1.3×10−5) we employed after correction for multiple testing. Our results suggest these regions do not constitute major genetic determinants of lung function measures at the general population level. The lack of replication and sometimes contradicting results in previous studies may reflect the fact that many previously reported associations came from studies with small sample sizes, possibly leading to false positive results.
Despite the failure to identify any overall significant contribution of a single SNP from previously reported genes to lung function, there are some potentially interesting signals apparent from the region plots suggesting that there may be a small signal from variants in some of the genes of interest.
SERPINA1 showed the strongest association with FEV1 among smokers (8.41×10−5). It encodes alpha-1 Antitrypsin protein (AAT), mainly produced in the liver and has the primary role of inhibiting neutrophil elastase in the lungs [11]. Protein variants of this gene have been classified based on their migration in an isoelectric pH gradient from A to Z. Among Caucasians, the M allele is the most common allele with six subtypes: M1–M6 with allele frequencies greater than 95 percent and associated with normal AAT levels. The common deficiency variants; S (frequency 0.02–0.03) and Z (frequency 0.01–0.03), are associated with mild and severe reductions in serum AAT levels, respectively [11], [12]. The r 2 between the Z allele rs28929474 and rs3748312 is 0.08 (based on 1000 Genomes Project pilot 1 data from 120 CEU individuals). Our top SNP, rs3748312, is in LD (r 2 = 0.603) with the M1 allele SNP rs6647, but is in very weak LD with M2 rs709932 (r 2 = 0.033) and M3 rs1303 (r 2 = 0.051). The S allele SNP rs45551939 (merged into rs17580) was not found in HapMap (version24). It is possible that the signal observed in our data is due to variants with effects on gene expression and/or protein levels, and this idea is supported by a previous study showing novel variants in SERPINA1 to be associated with increased susceptibility to COPD independently of the Z allele [13]. The relatively strong signal observed in our study suggests a possible role for variants in SERPINA1 in smokers at the general population level beyond that observed in carriers of known deficient alleles.
The PDE4D gene encodes the type 4D phosphodiesterase, which degrades cyclic adenosine monophosphate (cAMP), an important signal transduction molecule in all cell types. Polymorphisms within PDE4D have been associated with stroke [14], and bone mineral density [15]. PDE4D is the most dominant phosphodiesterase in the lungs and plays an important role in regulating airway smooth muscle contractility [16] demonstrated by PDE4D knockout mice lacking response to methacholine [17]. A study in a Japanese population reported association of one PDE4D SNP (rs829259) and a haplotype consisting of rs10075508 and one interleukin 13 (IL13) SNP with COPD [18]. SNP rs829259 was not associated with FEV1 in all individuals (P = 0.68) and in smokers (P = 0.21) in our study, and SNP rs10075508 was not genotyped or imputed in SpiroMeta. A recent GWAS has also identified PDE4D as an asthma susceptibility gene [19], however, none of the top 5 SNPs associated with asthma is present in our dataset, and the linkage disequilibrium (LD) with SNPs in SpiroMeta is low, so it is difficult to comment on their contribution to lung function measures in our study.
Our study has a number of strengths. First, we have power to detect associations of small magnitude, with data on 20,288 individuals from 14 European studies with more than 2.5 million genotyped and imputed SNPs. Second, we aimed to minimise Type 1 error whilst taking appropriate account of the correlation between neighbouring SNPs. Finally, the literature search was designed to be comprehensive to include all reported genetic variants with effect on lung function irrespective of disease status or ethnicity. To our knowledge, this is the first study to comprehensively evaluate the role of previously associated genes in a large genome-wide association study.
However, it is important to recognise the limitations of our study. We have tested for association in a general population sample; the magnitude of effect of these genetic variants may be greater in populations enriched with individuals with respiratory diseases such as asthma and COPD. Second, we have tested with cross sectional lung function measures. Some of the variants tested might affect longitudinal changes by accelerating or decelerating the decline in lung function, although this would still be expected to result in effects evident in cross sectional data. Third, the power of our study to detect associations of SNPs with modest effect sizes on lung function was limited given our relatively conservative approach to multiple testing, therefore we cannot rule out a real but modest effect of some of these loci on lung function and susceptibility to respiratory diseases in the general population. Alternative approaches could be to utilise a priori evidence about the reported direction of effect and a priori assumptions about the likely presence of multiple causal variants. Fourth, we tested for association with lung function measures among individuals of European ancestry, and the contribution of these variants to lung function in other populations may vary. Finally, the coverage of tested genetic regions varies depending on the genome-wide arrays used and imputation quality metrics.
In conclusion, we have shown that none of the SNPs tagging the genes previously reported to determine lung function were significantly associated with FEV1 or FEV1/FVC ratio in the SpiroMeta general population study. We found some evidence to suggest a possible contribution for the SERPINA1 and PDE4D loci to lung function in smokers which warrant further study. As a resource to the scientific community we have provided the complete association results (Dataset S1) in the online supporting information.
Methods
Systematic Literature search
We conducted a literature search in PubMed in October 2009 for genetic association studies of lung function measurements and/or COPD. The search terms used were: “Lung function” OR “pulmonary function” OR “FEV1” OR “FEV1/FVC” OR “Forced Expiratory Volume” OR “Forced Vital Capacity” OR “ASTHMA” OR “COPD” OR “BRONCHIAL HYPERRESPONSIVENESS” OR “BHR” OR “obstructive lung disease” AND “SNP” OR “single nucleotide polymorphism” OR “polymorphism” OR “gene” OR “genetic” OR “genom*” OR “variation” AND “Linkage” OR “association”
From the search results, we included relevant papers reporting only positive association results. For the three GWAS papers identified, we took a more inclusive approach and included all loci presented in the publication body, and not just those meeting genome-wide significance. We excluded papers reporting associations with respiratory diseases (e.g. asthma) without association with lung function measurements.
Statistical analysis
The genes and intergenic SNPs identified in the relevant literature were evaluated in the SpiroMeta dataset using an extended region of +/−10 kilobases (kb) from the gene coordinates downloaded from the UCSC genome browser (we used the SNP coordinate +/−10 kb for intergenic SNPs). Meta-analysis association results for SNPs in these (+/−10 kb extended) regions were extracted from the SpiroMeta dataset for both FEV1 and FEV1/FVC in all individuals and separately in ever–smokers. The complete cohort descriptions, study design and methods have been previously reported [7], but we provide here a brief summary. At study level, non-genotyped SNPs were imputed using standard approaches [18], [20] to facilitate meta-analysis of studies employing different genotyping platforms. Thus up to 2,705,257 SNPs were tested for association with FEV1 and FEV1/FVC using additive models and adjusting for age, sex, height and ancestry principal components. Then, the results were meta-analysed across studies using inverse variance weighting. Genomic control was applied at the study level and after the meta-analysis to correct for test inflation due to population stratification [21]. We excluded SNPs which were not well measured or imputed in the study (identifiable by an “effective sample size” of <50% of the total sample size) [7]. In all, we identified 16,936 genotyped and imputed SNPs in the gene and intergenic regions described above which met our inclusion criteria.
In order to correct for multiple testing of SNPs in linkage disequilibrium we used Li and Ji's [22] method for calculating the effective number of independent tests from pairwise SNP correlations. Pairwise SNP correlations were obtained from reference genotypes of 1468 subjects in the Busselton study [23]. We estimated that the association tests for the 16,936 highly correlated SNPs we selected in the regions of interest equated to 3,891 independent tests.
To maintain a Type 1 error rate of 5%, we adjusted the significance threshold using a Bonferroni correction (0.05/3891). Thus a threshold of 1.3×10−5 was used to determine statistical significance.
Supporting Information
Regional association plots of the most significant lung function–associated loci among all individuals in SpiroMeta (A–F). Statistical significance of each SNP on the −log10 scale as a function of chromosome position (NCBI build 36). The sentinel SNP at each locus is shown in blue; the correlations (r 2) of each of the surrounding SNPs to the sentinel SNP are shown in the indicated colours. The relevant trait (FEV1 or FEV1/FVC ratio) is indicated for each plot. Recombination rate is shown in pale blue.
(TIFF)
Regional association plots of the most significant lung function–associated loci among ever-smokers in SpiroMeta (A–D). Statistical significance of each SNP on the −log10 scale as a function of chromosome position (NCBI build 36). The sentinel SNP at each locus is shown in blue; the correlations (r 2) of each of the surrounding SNPs to the sentinel SNP are shown in the indicated colours. The relevant trait (FEV1 or FEV1/FVC ratio) is indicated for each plot. Recombination rate is shown in pale blue.
(TIF)
Regional association plots of the most significant lung function–associated loci (A–G) after excluding genes identified in GWAS. Statistical significance of each SNP on the −log10 scale as a function of chromosome position (NCBI build 36). The sentinel SNP at each locus is shown in blue; the correlations (r 2) of each of the surrounding SNPs to the sentinel SNP are shown in the indicated colours. The relevant trait (FEV1 or FEV1/FVC ratio) and whether it is in all individuals or ever-smokers is indicated for each plot. Recombination rate is shown in pale blue.
(TIF)
The 104 relevant publications identified in the literature search.
(DOC)
Complete FEV1 and FEV1/FVC association results for all individuals and separately for ever-smokers.
(XLS)
Acknowledgments
ALSPAC
We thank the Sample Logistics and Genotyping Facilities at the Wellcome Trust Sanger Institute for generating the ALSPAC GWA data.
B58C – T1DGC
We acknowledge use of the DNA from the British 1958 Birth Cohort collection, funded by the Medical Research Council and Wellcome Trust. We thank the Avon Longitudinal Study of Parents and Children laboratory in Bristol and the British 1958 Birth Cohort team, including S. Ring, R. Jones, M. Pembrey, W. McArdle, D.P.Strachan and P. Burton for preparing and providing the control DNA samples.
NFBC1966
We thank Professor Paula Rantakallio (launch of NFBC1966 and 1986), Ms Outi Tornwall and Ms Minttu Jussila (DNA biobanking).
ORCADES
As a EUROSPAN partner, we thank Yurii Aulchenko, Department of Epidemiology, Erasmus University Medical Center and Anatoly V. Kirichenko, Institute of Cytology and Genetics, Siberian Division of Russian Academy of Sciences, Novosibirsk, Russia for respectively performing imputation of the genotypic data and providing IT facilities. The ORCADES study would like to acknowledge the invaluable contributions of Lorraine Anderson (lorraine.anderson@ed.ac.uk) and the research nurses in Orkney.
Vis
The Vis study would like to acknowledge the staff of several institutions in Croatia that supported the field work, including but not limited to The University of Split and Zagreb Medical Schools, Institute for Anthropological Research in Zagreb and Croatian Institute for Public Health.
BHS
The Busselton Health Study acknowledges the generous support for the 1994/5 follow-up study from Healthway, Western Australia. The Busselton Health Study is supported by The Great Wine Estates of the Margaret River region of Western Australia. The BHS gratefully acknowledges the assistance of the Western Australian DNA Bank (NHMRC Enabling Facility) with DNA samples and the support provided by the Western Australian Genetic Epidemiology Resource (NHMRC Enabling Facility) for this study.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: Cohort funding: ALSPAC: The UK Medical Research Council (Grant number: G990146), the Wellcome Trust and the University of Bristol provide core support for ALSPAC. B58C - WTCCC: The British 1958 Birth Cohort DNA collection was funded by the Medical Research Council grant G0000934 and the Wellcome Trust grant 068545/Z/02. Genotyping for the Wellcome Trust Case Control Consortium was funded by the Wellcome Trust grant 076113/B/04/Z. B58C - T1DGC: This research utilizes resources provided by the Type 1 Diabetes Genetics Consortium, a collaborative clinical study sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute of Allergy and Infectious Diseases (NIAID), National Human Genome Research Institute (NHGRI), National Institute of Child Health and Human Development (NICHD), and Juvenile Diabetes Research Foundation International (JDRF) and supported by U01 DK062418. T1DGC GWAS data were deposited by the Diabetes and Inflammation Laboratory, Cambridge Institute for Medical Research (CIMR), University of Cambridge (John Todd, Helen Stevens and Neil Walker), which is funded by Juvenile Diabetes Research Foundation International, the Wellcome Trust and the National Institute for Health Research Cambridge Biomedical Research Centre; the CIMR is in receipt of a Wellcome Trust Strategic Award (079895). EPIC: The EPIC Norfolk Study is funded by Cancer Research United Kingdom and the Medical Research Council.. I.B. received funding from the Wellcome Trust (077016/Z/05/Z) and from the United Kingdom NIHR Cambridge Biomedical Research Centre. FTC: Academy of Finland Centre of Excellence in Complex Disease Genetics. Finnish Twin Study on Aging was funded by Academy of Finland and Finnish Ministry of Education. ENGAGE project grant agreement HEALTH-F4-2007-201413 and the European Union FP-5 GenomEUtwin Project (QLG2-CT-2002-01254). KORA S3: The KORA Augsburg studies were financed by the Helmholtz Zentrum München, German Research Center for Environmental Health, Neuherberg, Germany and supported by grants from the German Federal Ministry of Education and Research (BMBF) in the context of the German National Genome Research Network (NGFN-2 and NGFN-plus). The authors research was supported within the Munich Center of Health Sciences (MC Health) as part of LMUinnovativ. Genotyping for the KORA F3/500K Study which included the lung function characterized KORA C sample was partly funded by UBS Wealth Foundation Grant BA29s8Q7-DZZ. Korcula: The Korcula study (Croatia) was funded by grants from the Medical Research Council (UK) and Republic of Croatia Ministry of Science, Education and Sports research grants to I.R. (Vis) (108-1080315-0302). NFBC1966: Financial support was received from the Academy of Finland (project grants 104781, 1114194, 120315 and Center of Excellence in Complex Disease Genetics), Oulu University Hospital, Biocenter Oulu, University of Oulu, Finland, the European Commission (EURO-BLCS, Framework 5 award QLG1-CT-2000-01643), NHLBI grant 5R01HL087679-02 through the STAMPEED program (1RL1MH083268-01), ENGAGE project and grant agreement HEALTH-F4-2007-201413, and the Medical Research Council (studentship grant G0500539). The DNA extractions, sample quality controls, biobank up-keeping and aliquotting was performed in the National Institute for Health and Welfare, Biomedicum Helsinki, Finland and supported financially by the Academy of Finland and Biocentrum Helsinki. A.R. was supported by the European Commission as part of GABRIEL (a multidisciplinary study to identify the genetic and environmental causes of asthma in the European Community) contract number 018996 under the Integrated Program LSH-2004-1.2.5-1 Post genomic approaches to understand the molecular basis of asthma aiming at a preventive or therapeutic control. NSPHS: EUROSPAN (European Special Populations Research Network) was supported by European Commission FP6 STRP grant number 01947 (LSHG-CT-2006-01947). The Northern Swedish Population Health Study (NSPHS) was funded by the Swedish Medical Research Council (project number K2007-66X-20270-01-3). The computations were performed on UPPMAX (http://www.uppmax.uu.se) resources under Project p2008027. ORCADES: The ORCADES study was funded by the Chief Scientist Office of the Scottish Government, the Royal Society and the MRC Human Genetics Unit. DNA extraction was performed at the Wellcome Trust Clinical Research Facility in Edinburgh. Genotyping was funded by the European Union Framework Programme 6 EUROSPAN project. SHIP: SHIP is part of the Community Medicine Research net of the University of Greifswald, Germany, which is funded by the Federal Ministry of Education and Research (grants no. 01ZZ9603, 01ZZ0103, and 01ZZ0403), the German Asthma and COPD Network (COSYCONET; BMBF grant 01GI0883), the Ministry of Cultural Affairs as well as the Social Ministry of the Federal State of Mecklenburg-West Pomerania. Genome-wide data have been supported by the Federal Ministry of Education and Research (grant no. 03ZIK012) and a joint grant from Siemens Healthcare, Erlangen, Germany and the Federal State of Mecklenburg- West Pomerania. The University of Greifswald is a member of the ‘Center of Knowledge Interchange’ program of the Siemens AG. TwinsUK: TwinsUK is funded by the Wellcome Trust; the Arthritis Research Campaign; European Community's Seventh Framework Programme (FP7/2007–2013)/grant agreement HEALTH-F2-2008-201865-GEFOS and Seventh Framework Programme (FP7/2007–2013), ENGAGE project grant agreement HEALTH-F4-2007-201413 and the European Union FP-5 GenomEUtwin Project (QLG2-CT-2002-01254). The study also receives support from the National Institute for Health Research (NIHR) comprehensive Biomedical Research Centre award to Guy's & St Thomas' NHS Foundation Trust in partnership with King's College London. TDS is an NIHR senior Investigator. The project also received support from a Biotechnology and biological Sciences Research Council (BBSRC) project grant. Vis: The Vis study (Croatia) was funded by grants from the Medical Research Council (UK), European Commission Framework 6 project EUROSPAN (Contract No. LSHG-CT-2006-018947) and Republic of Croatia Ministry of Science, Education and Sports research grants to I.R. (108-1080315-0302). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Schunemann HJ, Dorn J, Grant BJ, Winkelstein W, Jr, Trevisan M. Pulmonary function is a long-term predictor of mortality in the general population: 29-year follow-up of the Buffalo Health Study. Chest. 2000;118:656–664. doi: 10.1378/chest.118.3.656. [DOI] [PubMed] [Google Scholar]
- 2.Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. American Journal of Respiratory & Critical Care Medicine. 2007;176:532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 3.Hubert HB, Fabsitz RR, Feinleib M, Gwinn C. Genetic and environmental influences on pulmonary function in adult twins. American Review of Respiratory Disease. 1982;125:409–415. doi: 10.1164/arrd.1982.125.4.409. [DOI] [PubMed] [Google Scholar]
- 4.Laurell C-B, Eriksson S. The Electrophoretic alpha 1-Globulin Pattern of Serum in alpha 1-Antitrypsin Deficiency. Scandinavian Journal of Clinical and Laboratory Investigation. 1963;15:132–140. [Google Scholar]
- 5.Hersh CP, Demeo DL, Lange C, Litonjua AA, Reilly JJ, et al. Attempted replication of reported chronic obstructive pulmonary disease candidate gene associations. American Journal of Respiratory Cell & Molecular Biology. 2005;33:71–78. doi: 10.1165/rcmb.2005-0073OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smolonska J, Wijmenga C, Postma DS, Boezen HM. Meta-analyses on suspected chronic obstructive pulmonary disease genes: a summary of 20 years' research. American Journal of Respiratory & Critical Care Medicine. 2009;180:618–631. doi: 10.1164/rccm.200905-0722OC. [DOI] [PubMed] [Google Scholar]
- 7.Repapi E, Sayers I, Wain LV, Burton PR, Johnson T, et al. Genome-wide association study identifies five loci associated with lung function. Nature Genetics. 2010;42:36–44. doi: 10.1038/ng.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hancock DB, Eijgelsheim M, Wilk JB, Gharib SA, Loehr LR, et al. Meta-analyses of genome-wide association studies identify multiple loci associated with pulmonary function. Nature Genetics. 2010;42:45–52. doi: 10.1038/ng.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilk JB, Chen T-H, Gottlieb DJ, Walter RE, Nagle MW, et al. A genome-wide association study of pulmonary function measures in the Framingham Heart Study. PLoS Genetics. 2009;5:e1000429. doi: 10.1371/journal.pgen.1000429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pillai SG, Ge D, Zhu G, Kong X, Shianna KV, et al. A genome-wide association study in chronic obstructive pulmonary disease (COPD): identification of two major susceptibility loci. PLoS Genetics. 2009;5:e1000421. doi: 10.1371/journal.pgen.1000421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalsheker NA. alpha1-Antitrypsin deficiency: best clinical practice. Journal of Clinical Pathology. 2009;62:865–869. doi: 10.1136/jcp.2008.063495. [DOI] [PubMed] [Google Scholar]
- 12.DeMeo DL, Silverman EK. Alpha1-antitrypsin deficiency. 2: genetic aspects of alpha(1)-antitrypsin deficiency: phenotypes and genetic modifiers of emphysema risk. Thorax. 2004;59:259–264. doi: 10.1136/thx.2003.006502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chappell S, Daly L, Morgan K, Guetta Baranes T, Roca J, et al. Cryptic haplotypes of SERPINA1 confer susceptibility to chronic obstructive pulmonary disease. Human Mutation. 2006;27:103–109. doi: 10.1002/humu.20275. [DOI] [PubMed] [Google Scholar]
- 14.Gretarsdottir S, Thorleifsson G, Reynisdottir ST, Manolescu A, Jonsdottir S, et al. The gene encoding phosphodiesterase 4D confers risk of ischemic stroke.[Erratum appears in Nat Genet. 2005 May;37(5):555]. Nature Genetics. 2003;35:131–138. doi: 10.1038/ng1245. [DOI] [PubMed] [Google Scholar]
- 15.Reneland RH, Mah S, Kammerer S, Hoyal CR, Marnellos G, et al. Association between a variation in the phosphodiesterase 4D gene and bone mineral density. BMC Medical Genetics. 2005;6:9. doi: 10.1186/1471-2350-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mehats C, Jin SLC, Wahlstrom J, Law E, Umetsu DT, et al. PDE4D plays a critical role in the control of airway smooth muscle contraction. FASEB Journal. 2003;17:1831–1841. doi: 10.1096/fj.03-0274com. [DOI] [PubMed] [Google Scholar]
- 17.Hansen G, Jin S, Umetsu DT, Conti M. Absence of muscarinic cholinergic airway responses in mice deficient in the cyclic nucleotide phosphodiesterase PDE4D. Proceedings of the National Academy of Sciences of the United States of America. 2000;97:6751–6756. doi: 10.1073/pnas.97.12.6751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Homma S, Sakamoto T, Hegab AE, Saitoh W, Nomura A, et al. Association of phosphodiesterase 4D gene polymorphisms with chronic obstructive pulmonary disease: relationship to interleukin 13 gene polymorphism. International Journal of Molecular Medicine. 2006;18:933–939. [PubMed] [Google Scholar]
- 19.Himes BE, Hunninghake GM, Baurley JW, Rafaels NM, Sleiman P, et al. Genome-wide association analysis identifies PDE4D as an asthma-susceptibility gene. American Journal of Human Genetics. 2009;84:581–593. doi: 10.1016/j.ajhg.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marchini J, Howie B, Myers S, McVean G, Donnelly P. A new multipoint method for genome-wide association studies by imputation of genotypes. Nat Genet. 2007;39:906–913. doi: 10.1038/ng2088. [DOI] [PubMed] [Google Scholar]
- 21.Devlin B, Roeder K. Genomic control for association studies. Biometrics. 1999;55:997–1004. doi: 10.1111/j.0006-341x.1999.00997.x. [DOI] [PubMed] [Google Scholar]
- 22.Li J, Ji L. Adjusting multiple testing in multilocus analyses using the eigenvalues of a correlation matrix. Heredity. 2005;95:221–227. doi: 10.1038/sj.hdy.6800717. [DOI] [PubMed] [Google Scholar]
- 23.Palmer LJ, Knuiman MW, Divitini ML, Burton PR, James AL, et al. Familial aggregation and heritability of adult lung function: results from the Busselton Health Study. European Respiratory Journal. 2001;17:696–702. doi: 10.1183/09031936.01.17406960. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Regional association plots of the most significant lung function–associated loci among all individuals in SpiroMeta (A–F). Statistical significance of each SNP on the −log10 scale as a function of chromosome position (NCBI build 36). The sentinel SNP at each locus is shown in blue; the correlations (r 2) of each of the surrounding SNPs to the sentinel SNP are shown in the indicated colours. The relevant trait (FEV1 or FEV1/FVC ratio) is indicated for each plot. Recombination rate is shown in pale blue.
(TIFF)
Regional association plots of the most significant lung function–associated loci among ever-smokers in SpiroMeta (A–D). Statistical significance of each SNP on the −log10 scale as a function of chromosome position (NCBI build 36). The sentinel SNP at each locus is shown in blue; the correlations (r 2) of each of the surrounding SNPs to the sentinel SNP are shown in the indicated colours. The relevant trait (FEV1 or FEV1/FVC ratio) is indicated for each plot. Recombination rate is shown in pale blue.
(TIF)
Regional association plots of the most significant lung function–associated loci (A–G) after excluding genes identified in GWAS. Statistical significance of each SNP on the −log10 scale as a function of chromosome position (NCBI build 36). The sentinel SNP at each locus is shown in blue; the correlations (r 2) of each of the surrounding SNPs to the sentinel SNP are shown in the indicated colours. The relevant trait (FEV1 or FEV1/FVC ratio) and whether it is in all individuals or ever-smokers is indicated for each plot. Recombination rate is shown in pale blue.
(TIF)
The 104 relevant publications identified in the literature search.
(DOC)
Complete FEV1 and FEV1/FVC association results for all individuals and separately for ever-smokers.
(XLS)