Abstract
Problems in diagnosing FM among motor vehicle collision (MVC) patients with whiplash (WL) include: the predominance of tender points (TPs) in the neck/shoulder girdle region; the 3-month duration of widespread pain criterion; and, the stability of diagnosis. The present study examined the prevalence of FM in a cohort (N = 326) with persistent neck pain 3 months following WL injury who were enrolled in a treatment program. Physical examinations were performed at baseline and at the end of treatment. Results indicated that WL patients had a greater proportion of neck/shoulder girdle TPs, relative to distal TPs. Compared to a matched cohort of treatment-seeking FM patients, WL patients indicated less distal TPs (M = 7.3 TPs vs. M = 5.6 TPs, p < 0.001), but were equivalent on neck/shoulder girdle TPs (M = 9.0 TPs vs. 9.2 TPs, ns). Baseline prevalence of FM for the WL cohort based on ACR criteria was 14% (95% CI: 10% – 18%), adjusted TP criterion discounting for neck/shoulder tenderness indicated a prevalence of FM of 8% (95% CI: 5% – 11%). Finally, 63% of patients meeting American College of Rheumatology FM criteria at baseline did not meet this criterion at post-treatment (approx. 6-months post-MVC). In conclusion, present criteria used in determining FM may result in spuriously inflated rates of diagnosis among WL patients due to persistent localized tenderness following MVC. Furthermore, the transient nature of FM “symptoms” among WL patients should be taken into account before making a final diagnosis.
1. Introduction
There is considerable controversy regarding the role of neck injuries in motor vehicle collisions (MVCs) on the etiology of fibromyalgia (FM). Two initial studies that addressed the issue of the causal relationship between MVCs and FM reported results that are diametrically opposed. Buskila et al [4] reported that the probability of FM one year following an accident was 13 times greater in patients with cervical injuries than patients with leg fractures. However, Tishler and colleagues [20] followed a cohort of whiplash (WL) patients for 14 months, and found no increased incidence of FM.
In both the previous studies [4, 20], the 1990 American College of Rheumatology (ACR) criteria for the case definition of FM were used. The ACR defined FM on the basis of two criteria [29]: (1) widespread pain of at least three months duration, and (2) tenderness in at least 11 of 18 specific locations (tender points, TPs). Both of these criteria are problematic in diagnosing FM following MVC and WL injury.
Although TPs identified by the ACR can be construed as measuring generalized hyperalgesia thought to be characteristic of FM, the TPs are located primarily in the neck/shoulder girdle region (ie, 10 of the 18 sites: suboccipital, trapezius, supraspinatus, mid-cervical, and second rib). It is possible that patients with WL injuries experience tenderness in the 10 neck/shoulder girdle sites because of localized hyperalgesia surrounding the site of injury rather than generalized hyperalgesia. These individuals would need to have tenderness in only one of the 8 “distal” sites (lateral epicondyle, gluteal, trochanteric, knee) to meet the TP criterion for FM. Thus, the diagnosis of FM may be spuriously inflated in patients with WL injuries [15; 16; 21].
The 3-month criterion may also be problematic. For example, Holm et al [6] followed patients up to 12 months following a WL injury and found that the cumulative incidence of widespread pain was 21%, but that most participants did not have widespread pain consistently over the course of the follow up. These data suggest that whereas FM is usually viewed as a chronic disorder, people who have recently experienced an MVC might have features of FM that are transient.
The present study examined the prevalence of FM in a cohort of people with persistent neck pain 3 months following a WL injury who were enrolled in a 6-week treatment for their symptoms. FM examinations were performed at baseline and at the end of treatment. Two sets of criteria were used to determine the presence of FM: the standard ACR criteria, and adjusted criteria that discounted TPs in the neck/shoulder girdle region. It was predicted that: (1) participants found to have FM would report tenderness primarily in neck/shoulder girdle region; (2) the apparent prevalence of FM would be lower when modified TP criteria were employed as opposed to standard ACR criteria; and (3) the diagnosis of FM would not be stable over time.
2. Methods
2.1 Participants
2.1.1 Whiplash Sample
The primary cohort in the study was a sample of 326 people with a history of WL following MVCs three months earlier. They were recruited from media and community health care providers for an education-based treatment for persistent neck pain that focused on reduction of fear of movement and patients’ avoidance of activities to prevent increased pain and further injury [25; 26]. Inclusion criteria consisted of: (1) neck pain attributed to a MVC in the past 3 months, and no (2) prior history of FM, (3) hospitalization following MVC, (5) indication of loss of consciousness in MVC, or (6) current substance abuse. All participants met the Quebec Task Force classification of Whiplash Associated Disorders (WADs), grade I (pain, stiffness or tenderness only, no physical signs) or grade II (pain, stiffness, or tenderness with decreased range of motion and point tenderness) [17]. The study was approved by the University of Washington Institutional Review Board.
2.1.2 Comparison Cohort of FM Patients
In order to interpret the distribution of TPs in the study cohort, females in the WL cohort who met criteria for a diagnosis of FM (n=37) were compared to a sample of 37 females with FM. This second comparison cohort was randomly selected from a group of 304 females with chronic FM who had participated in another treatment study performed by the authors [21].
2.2 Procedures
2.2.1 Assessment of FM
FM was assessed by both: (1) ACR methodology [29], and (2) an adjusted criteria for WL patients [21]. Patients completed a diagram consisting of the front and back of a human figure on which they indicated the location of their pain to assess widespread pain status, and a physician completed the standardized Manual Tender Point Survey (MTPS) [11]. The MTPS is a validated method for TP assessment, and its inter-rater reliability has previously been reported in the literature [11, 18]. Moreover, the standardized protocol that has been published was followed [18] and the first author (JR) ensured periodic calibration of the MTPS device to ensure that a consistent amount of pressure during assessments was delivered throughout the duration of the study.
The adjusted criteria distinguished between the 10 TPs involving the neck/shoulder girdle (suboccipital, upper trapezius, supraspinatus, lateral cervical, second rib) and the 8 distal areas (lateral epicondyle, gluteal, trochanteric, and knee). Each participant received a neck/shoulder girdle summary score (number of tender neck/shoulder girdle muscles/10) and a distal site summary score (number of tender distal sites/8). We conceptualized the distal site summary score as an index of a participant’s generalized hyperalgesia, and calculated the expected number of TPs a participant would have if his or her probability of pain in all 18 ACR sites was the same as their probability of tenderness in the distal sites. Thus, for example, an individual whose distal site TP score was 0.5 (i.e., positive for 4 of the 8 distal TPs) would be expected to have 0.5 × 18 = 9 positive TPs. On the other hand, an individual whose distal site TP score was 0.625 (i.e., positive for 5 of the 8 distal TPs) would be expected to have 0.625 × 18 = 11.25 sites. Therefore, by this calculation, any patient scoring positive on five or more distal TPs yielded an index of generalized hyperalgesia that resulted in 11 or more estimated TPs. This adjusted TP criteria was then used in conjunction with the standard determination of widespread pain to determine the presence of an adjusted FM diagnosis. In effect, the adjusted criteria determined whether a participant met the TP criterion for FM strictly on the basis of distal sites. Thus, neck/shoulder girdle sites were discounted completely.
2.2.2 Treatment and Post-Treatment Evaluation
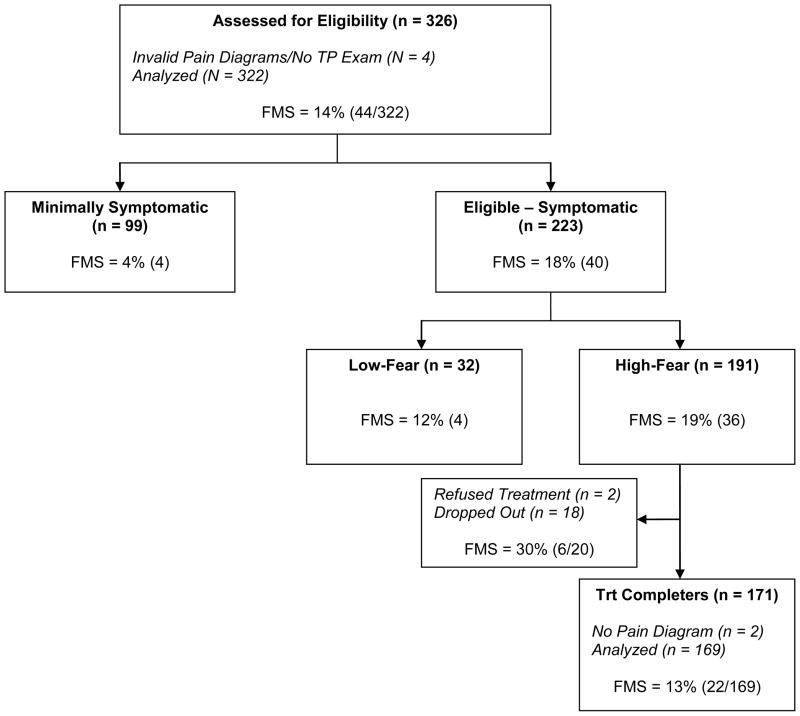
As noted above, the cohort examined in this study consisted of individuals who had sustained WL injuries 3 months previous to study initiation, and were invited to participate in a treatment program for persistent WAD symptoms [14]. In order to be eligible for treatment, potential participants had to meet the following criteria: (1) pain intensity of 4 or more (on an 11-pt scale, 0 = no pain, 10 = worst pain possible) during the week prior to evaluation, and (2) evidence of significant fear of neck movements. As shown in the CONSORT diagram (Figure 1), 223 of the individuals who underwent initial evaluation met the first criterion, and 191 met both criteria. Of these 191 people, 171 completed a 6-week, cognitive-behavioral therapy based treatment targeted for reducing fear and improving outcome following WAD. All treatment completers also participated in post-treatment evaluations, during which the procedures described above for diagnosing FM were repeated. Baseline assessment included the Neck Disability Index (NDI)[23], the Center for Epidemiologic Study Depressive Symptoms scale (CES-D)[12], the pain severity sub-scale of the Multidimensional Pain Inventory (MPI)[8], the Pictorial Fear of Activity Scale (PFACTS-C)[22], the Pain Anxiety Symptoms Scale (PASS)[10], and the Chronic Pain Self-Efficacy Scale (CPSS)[1]. Physical measures included the neck strength and cervical range of motion (CROM) using the Vernon neck muscle test, sphygmomanometer dynamometer, and the CROM section of the Jan Van Breeman Quantification of Pain and Physical Functioning [24].
Figure 1.
CONSORT Diagram for the Whiplash Cohort Meeting the ACR Criteria for FM
2.3 Data Analysis
Preliminary analyses were performed to determine whether females in the WL cohort who met criteria for FM (n=37) were comparable to treatment-seeking FM female patients selected from the cohort in the Turk et al. [21] study with respect to demographic variables. Independent-groups t-tests and Chi-Square tests were utilized for continuous and categorical demographic variables, respectively. When significant differences were observed, effect size statistics in the form of Cohen’s d (small = 0.2; medium 0.5; large = 0.8) for continuous variables and the odds ratio and 95% confidence interval (CI) for categorical variables. In addition, the distribution of TPs among people in the WL cohort who met criteria for FM was compared to that among the comparison cohort of treatment-seeking FM patients. The two groups were compared using an analysis of covariance (ANCOVA) to adjust for the significant difference in age observed between the WL and treatment-seeking FM cohorts. When significant differences were observed, effect size statistics in the form of partial eta-squared (η2) were reported (small = 0.01; medium = 0.09; large = 0.25).
Proportions of participants who, at baseline, (1) met the widespread pain criterion for FM; (2) met the ACR TP criterion for FM; (3) met the adjusted TP criterion for FM; (4) met ACR criteria for FM (ie, met both criterion 1 and criterion 2); and (5) met the adjusted criteria for FM (i.e., met both criterion 1 and criterion 3) were calculated. Proportions were also computed separately for the participants with significant neck pain at baseline evaluation and those who were minimally symptomatic, as well as treatment eligible (high-fear) and ineligible (low-fear) participants. The same five proportions were re-calculated six weeks later for the 171 participants who completed treatment.
Demographic variables as well as functional and psychosocial measures were evaluated to identify differences between those patients who did and did not meet the ACR criteria for FM in the WL cohort. Independent-groups t-tests and Chi-Square tests were utilized for continuous and categorical variables, respectively. Additionally, effect size statistics were reported for all significant group differences, in the form of Cohen’s d for continuous variables and the odds ratio and 95% confidence interval (CI) for categorical variables. Finally, a flow chart illustrating the change in patients meeting ACR criteria for FM at baseline versus post-treatment was reported to document whether FM was a transient phenomenon within sub-acute WAD patients.
Results
3.1 Whiplash Cohort vs. Treatment-Seeking FM Cohort
3.1.1 Demographics
Female patients in both the WL (N = 37) and FM treatment-seeking (N = 37) cohorts were comparable in terms of ethnicity (86% Caucasian in both cohorts). However, patients in the FM treatment-seeking cohort were older on average, relative to the WL cohort [Mean age: 47.9 years (SD = 7.5) vs. 41.8 years (SD = 11.9), p = 0.013, Cohen’s d = 0.6].
3.1.2 Distribution of Tender Points
After adjusting for age as a covariate in an analysis of covariance (ANCOVA), the overall number of TPs in the neck-shoulder region in the WL cohort was equivalent to those in the FM treatment-seeking cohort [Adjusted Mean TPs: 9.2 (SD = 1.2) vs.9.0 (SD = 1.4), p = .404]. However, the WL cohort demonstrated significantly fewer TPs in the distal region compared to the FM treatment-seeking cohort [Adjusted Mean TPs: 5.6 (SD = 1.9) vs. 7.3 (SD = 1.2), p < .001, partial η2 = .21].
3.2 Percentage of WL patients meeting the ACR and the adjusted criteria for FM
The number of patients in the WL cohort meeting the ACR criteria for FM at baseline was 44/322, 14% (95% CI: 10% – 18%). Based on the adjusted criteria, 26/322 patients met criteria for FM, 8% (95% CI: 5% – 11%). Table 1 summarizes the percentage of patients meeting FM using both the ACR and adjusted criteria, at each step of the treatment selection process.
Table 1.
Baseline and Post-Treatment Prevalence of Fibromyalgia in Whiplash Cohort (N = 322)
| Met WP Criterion | Met TP Criterion | Met Adjusted TP Criterion* | Met FMS Criteria | 95% CI FMS | Met Adjusted FMS Criteria** | 95% CI Adjusted FMS | |
|---|---|---|---|---|---|---|---|
| All Patients (N = 322) | 20% (64) | 45% (144) | 24% (76) | 14% (44) | (10%, 18%) | 8% (26) | (5%, 11%) |
| Minimally Symptomatic (N = 99) | 5% (5) | 28% (28) | 17% (17) | 4% (4) | (0%, 8%) | 3% (3) | (0%, 6%) |
| Symptomatic (N = 223) | 26% (59) | 52% (116) | 26% (59) | 18% (40) | (13%, 23%) | 10% (23) | (6%, 14%) |
| Symptomatic Patients (N = 223) | |||||||
| Treatment Ineligible – LoFear (N = 32) | 22% (7) | 31% (10) | 6% (2) | 12% (4) | (1%, 23%) | 3% (1) | (0%, 9%) |
| Treatment Eligible – HiFear (N = 191) | 27% (52) | 55% (106) | 30% (57) | 19% (36) | (13%, 25%) | 11% (22) | (7%, 15%) |
| Treatment Dropouts (N = 20) | 45% (9) | 65% (13) | 45% (9) | 30% (6) | (10%, 50%) | 25% (5) | (6%, 44%) |
| Treatment Completers (N = 171) | |||||||
| At Baseline | 25% (43) | 54% (93) | 28% (48) | 17% (30) | (11%, 23%) | 10% (17) | (6%, 14%) |
| At Post-Treatment (N = 169) | 17% (29) | 39% (66) | 26% (44) | 13% (22) | (8%, 18%) | 7% (12) | (3%, 11%) |
Adjusted TP Criteria: Any individual who scored a probability of p(distal locations) >= 0.625
Adjusted FMS Criteria: Any individual who met both WP Criterion and Adjusted TP Criterion
3.3 Demographic and Baseline Characteristics of WL Cohort
Within the WL cohort evaluated for this study, patients meeting ACR criteria for FM were 2.7 times (95% CI: 1.1, 6.2) more likely to be female, and were 4.2 times (95% CI: 2.1, 8.8) more likely to be planning or currently engaged in a lawsuit for the MVC (see Table 2). Patients meeting criteria for FM also reported a slightly greater proportion of comorbid medical disorders, relative to the non-FM patients [52% vs. 36%, OR (95%CI): 1.9 (1.0, 3.6)]. Collision characteristics, including perceived severity of MVC, seatbelt use, and method of MVC, were equivalent between both the FM and non-FM groups. Patients who met criteria for FM were also significantly worse, with large effect size magnitudes on all self-report measures, and with moderate effect size differences for poorer neck range-of-motion and neck-strength measures, relative to the non-FM group (see Table 3).
Table 2.
Demographic & Accident-related Characteristics of Whiplash Cohort (N = 322)
| Variables | No FMS 86% (N = 278) | FMS 14% (N = 44) | p-value | Odds Ratio (95% CI) |
|---|---|---|---|---|
| % Female | 66% (185) | 84% (37) | .019 | 2.7 (1.1, 6.2) |
| Age (SD) | 35.9 (12.8) | 37.8 (12.9) | .369 | |
| Comorbid Medical Disorders | 36% (101) | 52% (23) | .043 | 1.9 (1.0, 3.6) |
| Prior Surgeries | 58% (161) | 59% (26) | .883 | |
| Hit by other vehicle | 87% (224) | 93% (40) | .273 | |
| Rear-ended | 80% (184) | 76% (32) | .290 | |
| Perceived Severity of Accident [% (n)] | .053 | |||
| Not Severe/Minor | 22% (62) | 9% (4) | ||
| Moderately Severe | 57% (157) | 57% (25) | ||
| Very Severe | 18% (51) | 27% (12) | ||
| Extremely Severe | 2% (6) | 7% (3) | ||
| Wearing Seatbelt During Accident | 93% (255) | 100% | .065 | |
| Planning/Pursuing Lawsuit | 13% (35) | 39% (16) | <.001 | 4.2 (2.1, 8.8) |
Table 3.
Psychosocial & Physical Characteristics of Whiplash Cohort (N = 322)
| Variables | No FMS 86% (N = 278) | FMS 14% (N = 44) | p-value | Cohen’s d |
|---|---|---|---|---|
| Neck Disability Index - NDI (SD) | 23.6 (14.3) | 40.7 (16.0) | <.001 | 1.1 |
| Depressive Symptoms - CESD (SD) | 16.1 (9.3) | 25.6 (10.5) | <.001 | 0.9 |
| Pain Severity - MPI (SD) | 2.2 (1.3) | 3.3 (1.3) | <.001 | 0.8 |
| Fear Level - PFACTS | 213.3 (131.9) | 330.0 (179.5) | <.001 | 0.7 |
| Anxiety - PASS (SD) | 60.1 (25.2) | 81.6 (32.4) | <.001 | 0.7 |
| Self-Efficacy - CPSS (SD) | 228.5 (53.8) | 190.0 (61.1) | <.001 | 0.7 |
| Standardized Neck Range-of-Motion (SD) | 0 (1.0) | −0.5 (1.0) | <.001 | 0.5 |
| Standardized Neck Strength (SD) | 0 (1.0) | −0.4 (0.9) | .002 | 0.4 |
3.4 Meeting Criteria for FM at Post-Treatment
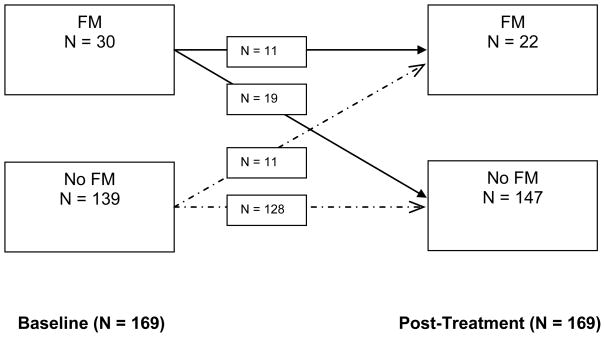
Among those who were eligible for treatment, 171 completed treatment, and 20 either refused or terminated prematurely. For the group of treatment completers, the observed FM rate in the cohort at baseline was 17% (n = 30/171; 95% CI: 11% – 23%), according to the ACR criteria. To determine the course of FM, widespread pain and TP evaluations were conducted again at the end of treatment, to determine a diagnosis for FM. It should be noted that 2 patients who did not meet ACR criteria for FM at baseline, did not have valid pain diagrams filled out at post-treatment, and were therefore excluded from the following discussion. As shown in Figure 2, four trajectories with respect to FM status were identified – 128 participants (FM−−) were FM− at both baseline and post-treatment; only 11 participants (FM++) met criteria both before and after treatment; 19 (FM+−) met criteria at baseline, but not at the end of treatment, and 11 (FM−+) did not meet criteria at baseline, but did meet criteria at the end of treatment. The proportion of patients meeting criteria for FM at post-treatment, based on the ACR criteria, was 13% (22/169; 95% CI: 8% – 18%) (see last row of Table 1). No additional analyses were performed on the sub-groups that fluctuated FM diagnosis at post-treatment, due to restricted sample sizes.
Figure 2.
Pre-to-Post Treatment Changes in the Prevalence of FM based on the ACR Criteria.
3. Discussion
As expected, the participants in our cohort with FM preferentially reported tenderness in neck/shoulder girdle muscles compared to distal muscles, whereas no such predilection was found in FM patients without a history of WL injury. Also, although the initial rate of FM in our cohort was 14% (44/322) when the standard ACR TP criterion was used, this declined to 8% (26/322) when an adjusted TP criterion was used to circumvent participants’ reporting of tenderness specifically in neck/shoulder girdle muscles. Taken together, these findings suggest that FM may be over-diagnosed in WL patients because of the preponderance of TPs in the neck/shoulder girdle region. More generally, our findings raise questions about rigid adherence to the TPs identified by the ACR, and are broadly compatible with concerns that have been raised by other investigators regarding the role that TPs should play in the diagnosis of FM [5; 27]. Moreover, they raise question as to the use of the 3-month criteria since there was considerable reduction in the percentage of patients originally meeting the ACR criteria observed over the course of this study (six months).
In our cohort, FM appeared to be a transient phenomenon rather than the refractory condition that is cited in published literature. Specifically, 19 of the 30 participants diagnosed with FM at treatment baseline (via the standard criteria) showed resolution of their FM by the time of their post-treatment evaluation (approximately six weeks later). Unexpectedly, 11 participants who did not initially meet FM criteria at baseline, did during the post-treatment evaluation approximately six months post MVC. This instability over time challenges the appropriateness of diagnosing FM when features of the condition have been present for only three months as considerable shifting may occur. Our data do not permit us to determine how long people must have symptoms of FM before the symptoms stabilize into a chronic pain disorder that is refractory to treatment. Further research is needed to clarify this point.
Recently Tishler et al, [19] published a 3-year prospective cohort study following the original individuals in the Tishler et al study who had WL following an MVC. These investigators reported a 2.5% prevalence of FM [19], no higher than the established prevalence of FM noted in the general population. On the surface, it might seem that our results fall somewhere between the estimates cited previously by Buskila et al [4] and Tishler et al [19, 20]. However, these studies contain limitations that raise concerns about the validity of the results. For example, the Buskila et al [4] was retrospective and included participants with work-related injuries, recruited from an occupational clinic, who had traumas of various types and not just whiplash associated disorders (WADs). Buskila himself raised concerns about the interpretation and conclusion that could be drawn based of the results of his study [3]. Tishler et al. [19, 20] relied on participants’ reports of symptoms and functioning following MVCs, and follow-up physical examinations were only conducted if patients reported elevated symptoms during telephone interviews.
In the context of the present study, caution is advised against interpreting any causal association between WL and FM. The present study was designed as a treatment study for patients with WADs approximately three months following an MVC rather than as a study of the natural history of WL injuries. Although the prevalence of FM was higher in our symptomatic patients than is generally observed in the population (approximately 2%) [28], we have no information about how typical or atypical the participants were of individuals who sustained WL injuries and importantly, volunteer to participate in a clinical trial. It is important to keep in mind the prevalence of non-fatal MVCs in the population when extrapolating the numbers observed in this study; e.g. the prevalence of MVCs in King County (Seattle, Washington, population 2.0 million) reported during the duration of this study was approximately 36,000/yr. Thus, our study cannot provide definitive information about the causal role that WL injuries may play in the development of FM, because it suffers from the “denominator problem” that often plagues epidemiologic research [7; 9; 13]. It is impossible to know how representative the volunteer sample of 322 was of the 144,000 MVCs that occurred in the time frame of participant recruitment.
In this context, however, our data do suggest that clinicians who treat patients with persistent neck pain following WL injuries are likely to misdiagnose FM in a significant percentage of them, and to conclude on the basis of their clinical experience that WL injuries are a risk factor for the development of FM [2]. This conclusion may be in error for at least two reasons: (1) the ACR TPs are over-represented in the cervical region and therefore may bias toward the diagnosis of FM and (2) because clinicians almost never have information relevant to the entire cohort of individuals who experience WL following MVCs.
A limitation of the present study is that since we recruited volunteers who had sustained WL injuries from the media and community health care providers. Consequently, our sample was not a random sample of people with persistent neck pain following a WL injury and we have no information about the nature or magnitude of the biases introduced by our recruitment methods. Another limitation is that we relied on participants’ reports that they did not have pre-accident FM or significant pre-accident neck pain. We had no independent information to verify the accuracy of their reports.
Despite the limitations noted, the results reported serve as a caution. The standard location of the ACR TPs may bias the diagnosis of FM in WL injury and the 3 month criterion for diagnosing FM may be premature as the presence of TPs appears to fluctuate even up to 6 months post MVC. Diagnosing FM with the accompanying suggestion of chronicity may be a disservice to individuals raising concerns about the long-term consequences of their symptoms.
Acknowledgments
Support for this study were provided in part from a grant from the National Institutes of Health, National Institute of Arthritis and Musculoskeletal and Skin Diseases, grants no R01AR 47298 and R01 AR044724. There is no conflict of interest associated with any of the authors of this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Anderson KO, Dowds BN, Pelletz RE, Edwards WT, Peeters-Asdourian C. Development and initial validation of a scale to measure self-efficacy beliefs in patients with chronic pain. Pain. 1995;63:77–84. doi: 10.1016/0304-3959(95)00021-J. [DOI] [PubMed] [Google Scholar]
- 2.Bennett RM, Jacobsen S. Muscle function and origin of pain in fibromyalgia. Baillieres Clin Rheumatol. 1994;8:721–46. doi: 10.1016/s0950-3579(05)80045-7. [DOI] [PubMed] [Google Scholar]
- 3.Buskila D, Neumann L. Musculoskeletal injury as a trigger for fibromyalgia/posttraumatic fibromyalgia. Curr Rheumatol Rep. 2000;2:104–8. doi: 10.1007/s11926-000-0049-z. [DOI] [PubMed] [Google Scholar]
- 4.Buskila D, Neumann L, Vaisberg G, Alkalay D, Wolfe F. Increased rates of fibromyalgia following cervical spine injury. A controlled study of 161 cases of traumatic injury. Arthritis Rheum. 1997;40:446–52. doi: 10.1002/art.1780400310. [DOI] [PubMed] [Google Scholar]
- 5.Hauser W, Hayo S, Biewer W, Gesmann M, Kuhn-Becker H, Petzke F, von Wilmoswky H, Langhorst J. Diagnosis of fibromyalgia syndrome-a comparison of Association of the Medical Scientific Societies in Germany, survey, and American College of Rheumatology criteria. Clin J Pain. 2010;26:505–11. doi: 10.1097/AJP.0b013e3181d92a6c. [DOI] [PubMed] [Google Scholar]
- 6.Holm LW, Carroll LJ, Cassidy JD, Skillgate E, Ahlbom A. Widespread pain following whiplash-associated disorders: incidence, course, and risk factors. J Rheumatol. 2007;34:193–200. [PubMed] [Google Scholar]
- 7.Kardooni S, Haut ER, Chang DC, Pierce CA, Efron DT, Haider AH, Pronovost PJ, Cornwell EE., 3rd Hazards of benchmarking complications with the National Trauma Data Bank: numerators in search of denominators. J Trauma. 2008;64(2):273–277. doi: 10.1097/TA.0b013e31816335ae. discussion 277–9. [DOI] [PubMed] [Google Scholar]
- 8.Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23:345–56. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- 9.Kibele E, Scholz R, Shkolnikov VM. Low migrant mortality in Germany for men aged 65 and older: fact or artifact? Eur J Epidemiol. 2008;23:389–93. doi: 10.1007/s10654-008-9247-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCracken LM, Zayfert C, Gross RT. The Pain Anxiety Symptoms Scale: development and validation of a scale to measure fear of pain. Pain. 1992;50:67–73. doi: 10.1016/0304-3959(92)90113-P. [DOI] [PubMed] [Google Scholar]
- 11.Okifuji A, Turk DC, Sinclair JD, Starz TW, Marcus DA. A standardized manual tender point survey. I. Development and determination of a threshold point for the identification of positive tender points in fibromyalgia syndrome. J Rheumatol. 1997;24:377–83. [PubMed] [Google Scholar]
- 12.Radloff L. A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–92. [Google Scholar]
- 13.Rempel OR, Laupland KB. Surveillance for antimicrobial resistant organisms: potential sources and magnitude of bias. Epidemiol Infect. 2009;137:1665–73. doi: 10.1017/S0950268809990100. [DOI] [PubMed] [Google Scholar]
- 14.Robinson JP, Theodore BR, Wilson HD, Turk DC. Efficacy of an early intervention combining graded exercise progression and targeted desensitization procedures in the treatment of whiplash-associated disorders, grades I and II: a randomized-controlled trial. Proceedings of the 13th World Congress on Pain; Montreal, QC: IASP Press; 2010. [Google Scholar]
- 15.Robinson JP, Turk DC, Aulet MR, Langmaid GC. Fibromyalgia (FM) syndrome following whiplash (WL) injury. Abstracts of the 10th World Congress on Pain; San Diego, CA: IASP Press; 2002. [Google Scholar]
- 16.Smith MD. Relationship of fibromyalgia to site and type of trauma: comment on the articles by Buskila et al. and Aaron et al. Arthritis Rheum. 1998;41:378–9. doi: 10.1002/1529-0131(199802)41:2<378::AID-ART27>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 17.Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine. 1995;20(8 Suppl):1S–73S. [PubMed] [Google Scholar]
- 18.Starz TW, Sinclair JD, Okifuji A, Turk DC. Putting the finger on fibromyalgia: the tender point survey. J Musculoskeletal Med. 1997;14:61–67. [Google Scholar]
- 19.Tishler M, Levy O, Amit-Vazina M. Can fibromyalgia be associated with whiplash injury? A 3-year follow-up study. Rheumatol Int. 2010 doi: 10.1007/s00296-010-1412-7. [DOI] [PubMed] [Google Scholar]
- 20.Tishler M, Levy O, Maslakov I, Bar-Chaim S, Amit-Vazina M. Neck injury and fibromyalgia-- are they really associated? J Rheumatol. 2006;33:1183–5. [PubMed] [Google Scholar]
- 21.Turk DC, Robinson JP, Burwinkle T. Prevalence of fibromyalgia tender points following whiplash injury. J Pain. 2006;7(Suppl 2):S27. [Google Scholar]
- 22.Turk DC, Robinson JP, Sherman JJ, Burwinkle T, Swanson K. Assessing fear in patients with cervical pain: development and validation of the Pictorial Fear of Activity Scale-Cervical (PFActS-C) Pain. 2008;139:55–62. doi: 10.1016/j.pain.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409–15. [PubMed] [Google Scholar]
- 24.Vernon HT, Aker P, Aramenko M, Battershill D, Alepin A, Penner T. Evaluation of neck muscle strength with a modified sphygmomanometer dynamometer: reliability and validity. J Manipulative Physiol Ther. 1992;15:343–9. [PubMed] [Google Scholar]
- 25.Vlaeyen JW, Haazen IW, Schuerman JA, Kole-Snijders AM, van Eek H. Behavioural rehabilitation of chronic low back pain: comparison of an operant treatment, an operant-cognitive treatment and an operant-respondent treatment. Br J Clin Psychol. 1995;34 (Pt 1):95–118. doi: 10.1111/j.2044-8260.1995.tb01443.x. [DOI] [PubMed] [Google Scholar]
- 26.Vlaeyen JW, Kole-Snijders AM, Boeren RG, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62:363–72. doi: 10.1016/0304-3959(94)00279-N. [DOI] [PubMed] [Google Scholar]
- 27.Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB, Yunus MB. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken) 2010;62:600–10. doi: 10.1002/acr.20140. [DOI] [PubMed] [Google Scholar]
- 28.Wolfe F, Ross K, Anderson J, Russell IJ, Hebert L. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38:19–28. doi: 10.1002/art.1780380104. [DOI] [PubMed] [Google Scholar]
- 29.Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33:160–72. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]