Abstract
Background
Health care providers will increasingly encounter information about the genetics of obesity as genetics research progresses.
Purpose
This study explores whether information about the genetics of obesity reduces medical student stigmatization of obese patients, and how it affects rates of health behavior-related referral.
Methods
One hundred and ten third and fourth year medical students were randomly assigned to read about genetic or behavioral mechanisms of obesity, or a control topic. Students interacted with an obese virtual patient in a virtual clinic and completed a battery of measures.
Results
Rates of most health behavior screening recommendations (weight loss, exercise, and diet consultations) were lower among participants exposed to genetic causal information than control. The genetic causal information group exhibited less negative stereotyping of the patient than control, F(1,105)=5.00, p=0.028, but did not differ in anticipated patient adherence, F(1,105)=3.18, p=0.077.
Conclusions
Information highlighting genetic contributions to obesity may lead to both positive and negative outcomes. Communication about the genetics of obesity should discuss the multi-factorial and non-deterministic nature of genetic risk.
Keywords: Obesity, Genetics, Stigma, Provider attitudes, Health behavior, Virtual reality
Introduction
Obesity is a condition with strong genetic underpinnings; twin studies have shown heritability of weight to be between 0.50 and 0.80 [1]. Research has identified hundreds of candidate genes that may be involved in physiological and behavioral pathways related to obesity, particularly as they interact with one another and with the environment [2–4]. Scientists anticipate that future research efforts will supply information needed to take a genomic approach to obesity prevention and treatment [5]. As a result, it is expected that health care providers will frequently encounter information about the genetics of obesity, and that such information will become integrated into clinical contexts [6].
Though information about obesity genetics will undoubtedly be used to improve patient care, there are additional ways that this information will impact the interaction between providers and patients. Many providers believe that the contribution of personal behavior to body weight greatly exceeds that of genetics [7, 8]. Emerging information that highlights the substantial genetic contributions to obesity and the interplay between genes and environment has the capacity to change providers’ beliefs about mechanisms that cause obesity. In turn, this may reduce the likelihood of stigmatizing obese patients and alter, either positively or negatively, providers’ inclination to counsel patients about health-promoting behaviors. On one hand, effects of genetic information may be uniformly positive; in addition to informing targeting and tailoring of treatment, genetic information may also bring reduction in stigma and increased attention to health behavior. However, genetic information could bring positive effects with respect to treatment and possibly stigma, but decreased attention to and lower rates of referral related to health behavior. The objective of the current study is to explore these possibilities.
Health Behavior Promotion
Behaviors like eating a healthful diet and performing adequate physical activity are crucial in promoting health for every individual. Screening and recommendations with respect to lifestyle behaviors are especially important for patients who are obese, as these individuals are at higher risk for co-morbid health conditions [9]. Several studies have demonstrated that providers address weight and health behavior with their overweight and obese patients at suboptimal rates [10–13]. Physicians cite several barriers to discussion of weight management (e.g., low confidence in patients’ ability to change behavior, the perception of weight counseling as a futile task; 14–17], many of which are likely to be influenced by beliefs about obesity causes.
Increasing genetic causal attributions for obesity could reduce the rate at which providers screen for and encourage health-promoting behaviors among obese patients. Genetic information could suggest to providers that obesity is primarily caused by uncontrollable factors, and thus diet and physical activity may not be efficacious for weight management. Mental models of illness tend to be structured such that beliefs about causes and solutions match one another [18]. If providers believe that obesity has a primarily genetic or biological cause, they may also tend to believe that the appropriate response should be biological in nature [19].
Alternatively, behavioral recommendations could be perceived to be more important for individuals at genetic risk, and thus could increase providers’ rates of health behavior screening and referral. Although this possibility has not been explored in the context of obesity, Grant and colleagues [20] found that physicians believed they would increase time spent counseling patients about lifestyle habits in response to a high risk result from a genetic test for diabetes. The literature therefore suggests competing hypotheses as to the impact of genetic causal information on health behavior recommendations.
Weight Stigma and Bias
A sizeable literature demonstrates that health care providers report stigmatizing attitudes toward and bias against obese patients [21]. Many physicians perceive individuals who are obese to be personally responsible for causing their condition, [7, 8, 22] and endorse stereotypes that these individuals are lazy and lacking in self-control [7, 23]. Stigmatizing attitudes can lead to clinical encounters that are more negative in tone and more uncomfortable for patients who are obese [24–26]. In turn, this may have important consequences for health care utilization and disease prevention [27]. There is clearly a need for reduction of bias against obese patients. It is unclear, however, whether genetic causal information will be a means to that end.
Genetic explanations challenge a primary tenant upon which obesity stigma rests, i.e., the idea that obese individuals simply lack self-control [28]. Consequently, genetic explanations have the potential to reduce stigma-related attitudes and behavior. In previous work, when individuals are described as having a condition or situation in which their weight is less controllable (e.g., genetic predisposition; thyroid condition), stigmatizing attitudes and discriminatory behavior have sometimes, but not always been reduced [29–33]. In addition, two studies focusing specifically on medical and public health students demonstrate at least partial effectiveness of stigma reduction interventions that incorporate provision of genetic causal information [34, 35].
Though these findings are encouraging, there are still several open questions about how genetics information impacts stigma and bias, particularly among medical students and providers. In previous work, the mechanisms of bias reduction (e.g., genetic causal explanations versus empathy) are unclear. Furthermore, studies have only examined generalized attitudes rather than effects of interventions on attitudes and behaviors displayed toward individual patients in clinical contexts. Therefore, there is a need to examine the specific effect of genetic information on stigmatization among providers.
Finally, it is important to consider the impact of information implicating personal behavior as the cause of obesity as a counterpoint to genetic causal information. Information about personal behavior is ubiquitous in media and in public health messages. Encountering messages about personal behavior could have little or no effect on health behavior recommendation or social stigma because it aligns with preexisting beliefs [7, 8] and thus may be effectively neutral. Alternatively, these messages could reinforce or strengthen providers’ beliefs about personal responsibility and exacerbate stigmatizing attitudes.
Immersive Virtual Environment Platform
In this study, participants’ behavior toward a target patient was examined in an immersive virtual environment (IVE). In IVEs, users are immersed in a computer-generated three-dimensional “world” that they can navigate in a natural way (e.g., by walking; Fig. 1). Use of this technology eliminates the tradeoff between experimental control and realism typically inherent in experimental research [36]. Therefore, unlike traditional research, in IVEs one can maintain standardization of a target patient between participants while still situating the encounter in a realistic clinical context [37, 38]. By employing a virtual patient, it also ensures that no real patient or individual suffers any negative effects of an experimental manipulation. Thus, participants’ attitudes, behavior, and recommendations toward a totally standardized, individual patient can be assessed without any of the drawbacks associated with human patients or actors.
Fig. 1.
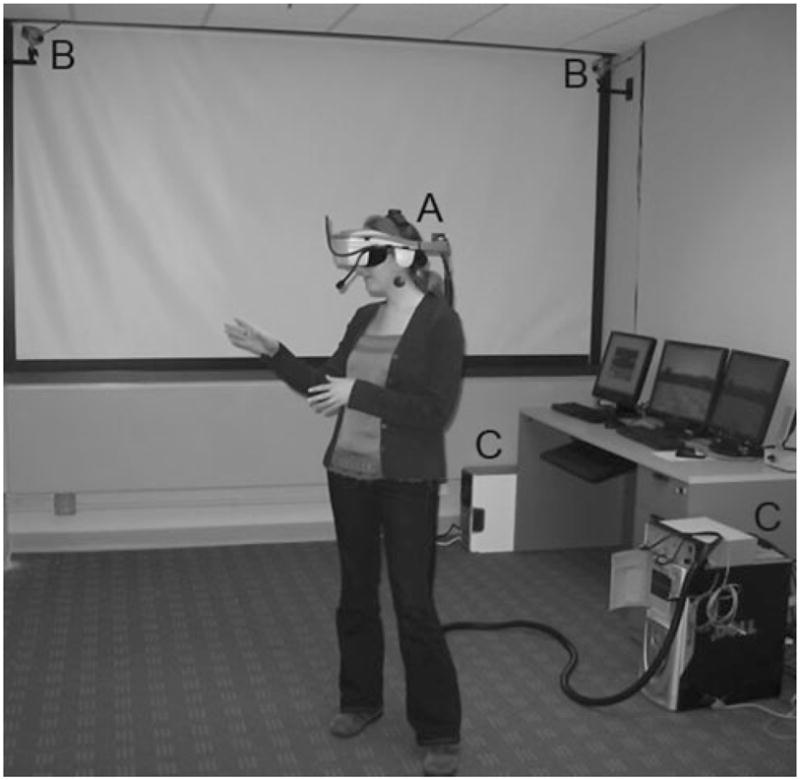
Illustration of IVE set-up. a Head-mounted display; b tracking cameras; c) tracking and rendering computers
Previous research suggests that experiences in virtual environments are psychologically compelling and that findings in the virtual clinical IVE are applicable to real-life situations [37, 39]. A small number of previous studies have used virtual patients to explore clinical interactions [26, 40, 41]. Virtual patient simulations are also being developed for medical student training. In this area, work has demonstrated that virtual patients generally elicit reactions similar to standardized patients in training scenarios [42, 43]. Furthermore, behavior in these simulations has been shown to translate to behavior in real clinical interactions [43, 44].
Hypotheses
We hypothesized that participants who receive information about genetic causal mechanisms of obesity would demonstrate lower rates of stigma-related attitudes than those who receive no causal information and those who receive behavioral causal information. In contrast, we did not anticipate a significant difference between participants who receive information about personal behavior as a primary cause of obesity and those who receive no causal information. As noted above, the literature suggests competing hypotheses related to the impact of genetic causal information on health behavior recommendations. This information could either reduce or increase the rate at which participants recommend screening for health behaviors. We anticipated that behavioral causal information might increase recommendation rates from control and from the genetic condition. These hypotheses were explored using a medical student population. Although medical students are not yet providers, they are an important group for study because they are in the process learning how patients should be viewed and treated [45]. Thus, they are a likely target for future intervention work.
Methods
Design
This study was a controlled experiment in which medical students were randomly assigned to one of three information conditions. Students read information positing that obesity is primarily caused by genetic factors (the genetic condition), is primarily caused by behavioral factors (the behavioral condition), or information about an unrelated medical topic (the control condition). Data for this study were obtained from a larger experimental project.
Participants
Participants were 110 third and fourth year medical students recruited from the Washington, DC and Baltimore, Maryland metropolitan areas. Recruitment efforts consisted primarily of posting flyers, sending emails to medical student groups, and word-of-mouth. Thirty-nine medical students were randomly assigned to the genetic condition, 35 to the behavioral condition, and 36 to the control condition. Due to the use of IVE technology, exclusion criteria included having a seizure or vestibular disorder, being highly prone to motion sickness, and having poor, uncorrected hearing or vision. Participants were compensated for their participation. This study was approved by the National Human Genome Research Institute Institutional Review Board.
Procedure
Participants were run through the study individually. All participants first gave their informed consent to participate in the study. Students then received one of the three types of information depending upon randomly assigned condition. The information was contained in a short article, formatted to appear as if it had been photocopied from a scientific journal. Genetic and behavioral condition articles contained scientific information collected from actual review articles on the etiology of obesity. Passages from multiple published articles were excerpted and combined so as to support the central premise of each experimental article. For example, the genetic article included information about high heritability rates associated with obesity, common and rare gene discovery, and the mechanisms through which genetic factors are posited to influence body weight. The control article related to chronic headache pain and was created in a fashion analogous to the other articles. Articles were approximately equal in length and formatting was consistent across all three. Excerpts are available in the Appendix. After reading their assigned article, students completed a short questionnaire with items related to the information they had read.
Students next engaged in an IVE-based interaction with a female virtual patient who was obese (Fig. 2). Students wore a head-mounted display to interface with the virtual environment. Their head and body movements were tracked to render the appropriate scene in real time. The virtual world was rendered stereoscopically, and in three dimensions. The virtual encounter with the patient was a primary care-type clinical encounter. Communication and interactions were constrained so that each student would receive the same type and amount of information from the patient.
Fig. 2.
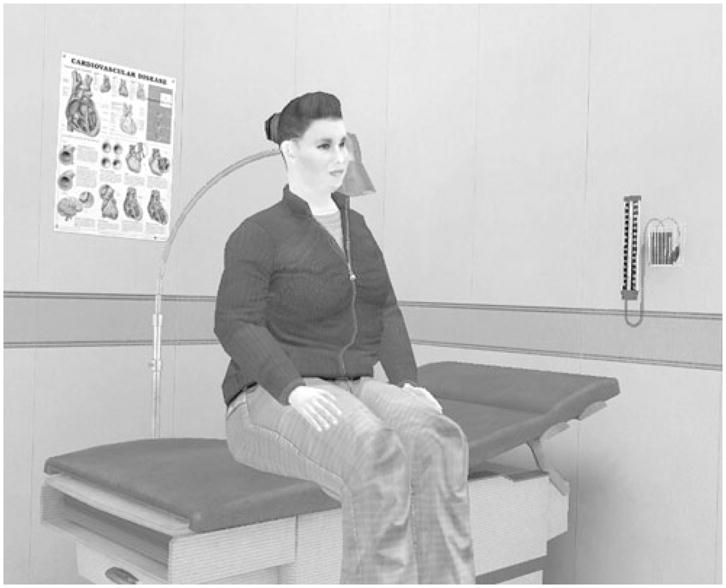
View of the virtual clinic room with the patient
Students “entered” the virtual clinic room by wearing the head-mounted display and were given instructions to guide them though the interaction. Information from the virtual patient’s health record was then displayed (Fig. 3). When students were finished reviewing the patient information, they saw the patient for the first time.
Fig. 3.
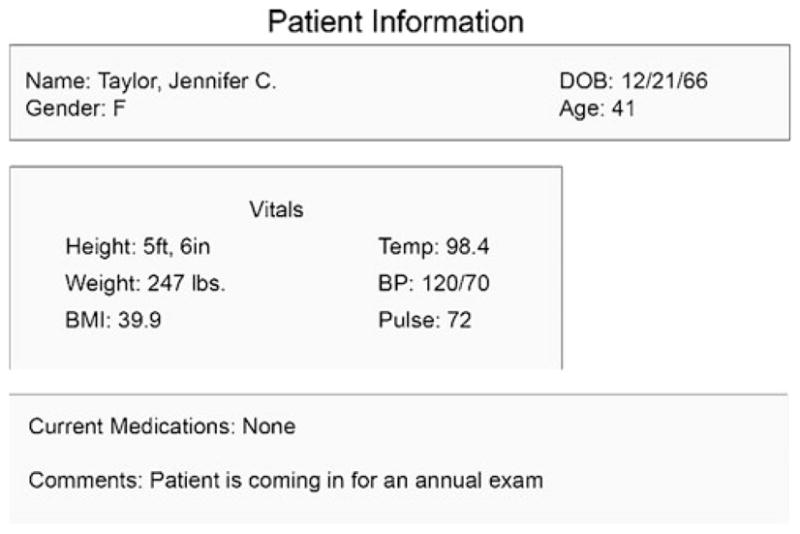
Electronic health record information for the patient
A clinical interaction between the student and the patient took place in a turn-taking fashion. The student introduced him or herself to the virtual patient. The patient then verbalized information about her current health symptoms and concerns. Specifically, the patient reported that she currently had a rash on her hand that she believed to be eczema, that she was experiencing knee pain previously diagnosed as osteoarthritis, and that she had been experiencing some intermittent shortness of breath. After the patient finished speaking, the student had an opportunity to visually examine the patient (e.g., taking a closer look at the eczema rash on her hand). The student responded verbally to the patient with whatever he or she felt was appropriate, and the interaction was ended.
Following the virtual encounter, students completed a battery of computerized questionnaires. A subset of the measures that were assessed (those related to bias and health behavior promotion) is reported here. Each measure was assessed at a single time point. Finally, students were weighed and measured for height, and fully debriefed.
Measures
Belief in Article Premise
After reading their assigned article, but before interacting with the virtual patient, participants were asked to choose on a multiple choice question what they thought was the article’s main message regarding the primary cause of obesity. Response options included: genes, behavior, gene-behavior interaction, or none. This item was scored as to whether a participant’s response matched or mis-matched the intended article premise.
Causal Beliefs
All other self-report measures were assessed following interaction with the virtual patient. Students’ self-reported beliefs about the extent to which genetic factors cause body weight were measured. Participants were asked to indicate what percentage of body weight (from 0–100%) they believed to be caused by genetic factors.
Perceptions of Patient’s Responsibility
The extent to which students believed the patient was responsible for causing her body weight was assessed with a single item, “how responsible is your patient for causing her weight?” Perceptions were measured on a seven-point scale with endpoints “not at all responsible” and “entirely responsible”.
Health Behavior Recommendations
Students were provided with a list of 25 potential clinical recommendations related to routine health maintenance, adapted from Hebl and Xu [46]. Three of these were directly related to health behavior: recommending a “consultation about diet”, a “consultation about exercise”, and a “dietary intake evaluation”. One item was indirectly related to health behavior: recommending a “consultation about weight loss”. Students indicated whether or not they would recommend each item for the patient at this time.
Negative Stereotyping
Students’ attitudes about the patient were measured using a negative stereotype scale based on the Obese Persons Trait Survey [47] (Cronbach’s alpha in this study=0.87). The scale consists of ten negative traits (e.g., laziness). Students were asked to indicate on a seven-point scale, from “strongly agree” to “strongly disagree”, the extent to which each trait described the patient.
Patient’s Anticipated Adherence
Students’ perceptions of the patient’s likelihood to adhere to their advice were assessed with a single item [46], “this patient would follow my advice.” Responses were indicated on a 7-point scale with endpoints “not at all” and “extremely”.
Demographics
Students’ weight and height were measured directly using a scale and tape measure. Body mass index (kg/m2) was calculated from these measurements. Demographic variables such as gender, age, race and ethnicity, year in medical school, and family history of obesity were collected via self-report questionnaire.
Statistical Analysis
Analyses were performed using SPSS version 17.0 (SPSS Inc., Chicago IL). Descriptive analyses of all variables were performed. Dummy-coded variables were created to represent the three experimental conditions. Each dummy-coded variable represents a partial effect, and thus the presence of both dummy-coded variables in an analysis is necessary in analyses to reflect all three conditions [48]. Comparisons between the control condition and each of the other conditions, and between the genetic condition and each of the other conditions were performed by entering dummy-coded variables into an ANCOVA. Participants’ sex, body mass index, and the belief in article premise measure were entered into the ANCOVAs as covariates.
Results
Demographics
Student demographics are reported in Table 1. None of the demographic factors varied significantly by condition.
Table 1.
Participant characteristics by condition, means and standard deviations or frequency and percentage
| Characteristic | Total (N=110) | Genetic condition (N=39) | Behavioral condition (N=35) | Control condition (N=36) |
|---|---|---|---|---|
| Age, years mean (SD) | 26.22 (2.54) | 26.54 (3.24) | 26.11 (2.34) | 25.97 (1.78) |
| BMI, kg/m2 mean (SD) | 23.92 (2.54) | 23.70 (3.24) | 24.59 (4.33) | 23.52 (3.35) |
| Female gender | 56 (50.1%) | 18 (46.2%) | 17 (48.6%) | 21 (58.3%) |
| Whitea | 62 (56.4%) | 24 (61.5%) | 17 (48.6%) | 21 (58.3%) |
| Asian | 24 (21.8%) | 7 (17.9%) | 6 (17.1%) | 11 (30.6%) |
| Black/African American | 24 (21.8%) | 6 (15.4%) | 10 (28.6%) | 8 (22.2%) |
| Hispanic/Latino | 4 (3.6%) | 3 (7.7%) | 0 (0%) | 1 (2.8%) |
| Third year medical student | 54 (49.1%) | 17 (43.6%) | 19 (54.3%) | 18 (50%) |
| Overweight or obese BMI | 38 (34.5%) | 12 (30.8%) | 14 (40%) | 12 (33.3%) |
| Family history of obesity | 40 (36.4%) | 13 (33.3%) | 14 (40%) | 13 (36.1%) |
Numbers represent frequencies and percentages unless otherwise noted
Racial percentages add up to >100% because participants were allowed to select more than one race category
Belief in Article Premise
Of the participants in the genetic condition, 12 (30.8%) provided a “mis-match” response to the belief in article premise item, indicating that they did not accept or understand the main point of the article. Seven participants in the behavioral condition (20%) provided a mis-match response. For all mis-matches, participants reported that the article posited that weight is due to an interaction between genes and behavior. Participants who read the control article were all coded as a match because the control article contained no obesity-related information. Although some participants indicated beliefs that did not wholly agree with the intended article premise, they may have nonetheless been affected by exposure to the information. Therefore, this measure was included as a covariate in analyses.
Causal Beliefs
Relative to students in the control condition (M=20.88%, SD=2.1%), students in the genetic condition indicated that genetics was responsible for causing a significantly higher percentage of body weight (M=42.87%, SD=2.0%), F(1,105)=54.06, p<0.0001. In contrast, relative to the control condition, participants in the behavioral condition attributed a significantly lower percentage of body weight to genetics (M=5.64%, SD=2.1%), F(1,105)=23.17, p<0.0001. The difference between the genetic and behavioral conditions was also significant, F(1,105)=166.74, p<0.0001.
Perceptions of the Patient’s Responsibility
Compared to the control condition, participants in the genetic condition held the patient significantly less responsible for causing her weight, F(1,105)=4.14 p= 0.044 (see Table 2). Participants in the control condition were not significantly different from those in the behavioral condition in their perception of the patient’s responsibility for her weight, F(1,105)=3.35, p=0.070. However, the genetic and behavioral conditions were significantly different from one another, F(1,105)=16.02, p<0.0001.
Table 2.
Attitudes and beliefs about patient and visual behavior (covariate-adjusted meansa and standard error), and health behavior recommendations by condition (frequencies and percentages)
| Genetic condition (N=39) | Behavioral condition (N=35) | Control condition (N=36) | p values genetic vs. control/behavioral vs. control/genetic vs. behavioral | |
|---|---|---|---|---|
| Attitudes and beliefs | ||||
| Responsibility | 4.43 (0.17) | 5.39 (0.17) | 4.94 (0.17) | 0.044/0.070/<0.0001 |
| Negative stereotypes | 3.55 (0.12) | 3.75 (0.13) | 3.96 (0.13) | 0.028/0.26/0.25 |
| Anticipated adherence | 4.62 (0.17) | 4.32 (0.18) | 4.17 (0.18) | 0.077/0.56/0.22 |
| Recommendations | ||||
| Weight loss consultation | 34 (87.2%) | 35 (100%) | 36 (100%) | 0.005/0.81/0.007 |
| Exercise consultation | 34 (87.2%) | 33 (94.3%) | 36 (100%) | 0.009/0.22/0.15 |
| Diet consultation | 33 (84.6%) | 32 (91.4%) | 35 (97.2%) | 0.022/0.25/0.23 |
| Dietary intake evaluation | 31 (79.5%) | 33 (92.3%) | 32 (88.9%) | 0.26/0.49/0.059 |
Covariates include sex, body mass index, and belief in article premise
Health Behavior Recommendations
Rates of health behavior recommendation were high overall. However, compared to those in the control condition, participants in the genetic condition recommended weight loss consultation, exercise consultation, and diet consultation significantly less frequently, F(1,105)=8.28, p=0.005; F(1,105)=7.01, p=0.009; F(1,105)=5.43, p=0.022, respectively (see Table 2). Rates of recommending dietary intake evaluation did not differ between the control condition and the genetic condition, F(1,105)=1.31, p=0.26. In comparing the control condition and the behavioral condition, there were no differences in rates of recommendations for any of the four items, F(1,105)=0.058, p=0.81; F(1,105)=1.54, p= 0.22; F(1,105)=1.37, p=0.25; F(1,105)=0.49, p=0.49 for weight loss consultation, exercise consultation, diet consultation, and dietary intake evaluation respectively. Participants recommended weight loss consultation significantly more frequently in the behavioral than the genetic condition, F(1,105)=7.49, p=0.007. Rates of recommending exercise consultation, nutrition consultation, and dietary intake evaluation did not significantly differ between the genetic and behavioral conditions; F(1,105)=2.14, p=0.15; F(1,105)=1.46, p=0.23; F(1,105)=3.65, p=0.059.
Stigma-Related Variables
Relative to participants in the control condition, there was significantly less stereotyping of the patient among participants in the genetic condition, F(1,105)=5.00, p=0.028; however, participants in the genetic condition did not expect the patient to be significantly more adherent, F(1,105)=3.18, p=0.077. Comparisons between the control and behavioral conditions revealed no difference in levels of negative stereotyping, F(1,105)=1.27, p=0.26, nor in anticipated adherence, F(1,105)=0.34 p=0.56. Comparisons between the genetic and control conditions also revealed no difference in levels of negative stereotyping, F(1,105)=1.33, p= 0.25, or anticipated adherence, F(1,105)=1.55, p=0.22.
Discussion
We found that information highlighting genetic contributions to obesity may be a double-edged sword when it comes to medical student attitudes and behavior. Although exposure to genetic causal information in comparison to control led to some reduction in social stigma-related attitudes among medical students, it also reduced health behavior screening recommendations.
Reduction in recommendation rates for health behavior assessments related to diet and exercise may be a concerning, unintended consequence of focusing on genetics as a primary cause of obesity. Information positing that obesity and body weight are primarily caused by genetic factors led to less frequent recommendation of dietary consultation, exercise consultation, and weight loss consultation to the obese patient. Though not significant, means for dietary intake evaluation recommendations also demonstrated a similar pattern. Thus, obesity genetics information could give clinicians an additional reason to avoid a task that is often viewed as aversive or futile [14–17].
Lifestyle behaviors have wide-ranging consequences for individuals’ health beyond their relationship to body weight. It is therefore particularly important that these behaviors be addressed by providers whether or not they produce successful or maintained weight loss. It may therefore be beneficial to include information about the multi-factorial causal nature of obesity and the nondeterministic nature of genes when conveying obesity genetics information to medical students and providers. This area is ripe for further research.
Information advancing personal behavior explanations for obesity did not change rates of health behavior recommendations from control. Though this information was expected to increase these recommendations, recommendation rates were already near or at ceiling among the control condition. In contrast to patterns described in previous literature [10–13], participants in the current study made recommendations related to health behavior and weight loss at very high rates. This could be due to the fact that medical students are sensitive to evaluation or because they knew they would not actually have to deliver health behavior counseling. In either case, the high rate of behavior-related recommendations overall makes the reduction in recommendations among the genetic group all the more striking.
Information positing that obesity is primarily genetic reduced negative stereotyping compared with the control condition. Though it did not significantly increase perceptions that the patient would be adherent to recommendations, the means were in the anticipated direction and the effect approached significance. For this question, participants were asked to imagine having a continuing relationship with the patient; this may have been difficult for participants to do with a virtual patient. Information that attributes obesity and body weight primarily to personal behavior did not lead to differences in stigmatizing attitudes from the other conditions. It may therefore be the case that because messages about personal behavior are ubiquitous in modern culture, they are less carefully considered and thus have less impact.
Obesity genetics information may have some ability to attenuate weight stigma among medical students, although the effects are small in magnitude. The genetic information we provided may have been too weak a manipulation as demonstrated by the large number of participants who did not endorse the intended article premise. In considering interventions to reduce stigma among medical students, a stronger, more detailed presentation of these concepts or a multi-method approach may be necessary to result in meaningful bias reduction.
In addition, providers naturally encounter messages about the etiology of weight in both scientific and public settings. Based on the results of this study, encountering messages advancing personal behavior as a primary cause for obesity may not increase stigmatizing attitudes. Furthermore, encountering information advancing genetic causes could have the positive “side effect” of reducing stigma among medical students and health care providers.
Limitations
The current study has several limitations. Although we opted to focus on medical students as they are a likely intervention target, they are not yet providers and lack clinical experience. Thus, findings may be less generalizable to practicing physicians. In addition, the arguments for genetic or personal behavior causes of obesity presented to students focused on a single cause and did not represent the multi-factorial, interactive nature of obesity etiology. Future research should investigate the impact of information that more fully characterizes complex causal mechanisms related to obesity.
In this study, we opted to keep the clinical interaction simple. Therefore, it lacked a true physical examination or interview. In the future, making the flow of the interaction more similar to reality may increase external validity. In addition, we did not assess the extent to which the participant perceived the patient to be obese. Although perceptions of the patient’s size may have affected participant attitudes, such perceptions are unlikely to differ by condition. If anything, our results may have been stronger if we checked for and eliminated participants who did not perceive the patient as obese. Finally, this study was limited by its sample size. The study was powered to detect medium-sized effects, and some of the hypothesized relationships may have thus failed to reach the significance criterion.
Implications
It is anticipated that scientific findings elucidating genetic mechanisms for obesity will play an important role in prevention and treatment. The current study demonstrates that dissemination of information about genetic causal mechanisms may be able to play a role in reducing provider bias against obese patients. Our findings also suggest, however, that the impact of genetic causal information may not be uniformly positive. It is concerning that provision of this information led to reduction in health behavior screening recommendations. This points to a potential need for communication about genetics of obesity to discuss the multi-factorial and non-deterministic nature of genetic risk. More research on this process is clearly warranted. In addition, research is needed to determine the impact of genetic causal information on patients in weight-related clinical interactions. Timely attention to these issues will ensure that the public reaps the benefits of genetic discovery and genomic medicine without suffering any preventable negative by-products of dissemination.
Acknowledgments
This research was supported by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health. The authors wish to thank Colleen McBride and Alex Cho for their insightful comments on an earlier version of this manuscript, and Lori Bastian, Greg Feero, and Nancy Stevens for their valuable advice. In addition, the authors thank Laura Wagner, Studly Auguste, ShaDonna Jackson, and Shea Lott for their assistance with data collection.
Appendix
Excerpted conclusion from genetic article—material adapted from [49] and [50]
Common forms of obesity may be viewed as disorders with genetic underpinnings that occur most readily among individuals who are predisposed to energy conservation both in terms of metabolic processes and in terms of behavioral phenotypes. Help will come with identification of the genes that predispose to obesity, and a fuller understanding of their function.
Excerpted conclusion from behavioral article —additional material adapted from [51]
Common forms of obesity may be viewed as disorders with possible small genetic influence that occur most readily among individuals who are prone to energy-conserving behaviors consisting of preferential seeking of energy-dense foods and sedentary activities. Current trends in weight-for-height measurements indicate that a major cause of the obesity problem lies in dietary and physical activity patterns.
Excerpted conclusion from control article—material adapted from [52] and [53]
Chronic daily headache is a relatively common condition associated with significant burden of suffering, but we are only just beginning to understand the pathophysiological mechanisms underlying the chronification of primary headaches. As a result, the management of the most common forms of chronic daily headache is currently nonspecific, non evidence-based, and largely unsatisfactory. Some complementary and alternative treatments do offer hope for chronic headache treatment however, it is quite difficult to differentiate hype from hope or hazard in such treatment.
Footnotes
Conflict of Interest Statement The authors have no conflict of interest to disclose
Contributor Information
Susan Persky, Email: perskys@mail.nih.gov, Social and Behavioral Research Branch, National Human Genome Research Institute, NIH, 31 Center Drive, Room B1B36, Bethesda, MD 20892, USA
Collette P. Eccleston, Syracuse University, 430 Huntington Hall, Syracuse, NY 13244, USA
References
- 1.Maes HHM, Neale MC, Eaves LJ. Genetic and environmental factors in relative body weight and human adiposity. Behavior Genetics. 1997;27:325–351. doi: 10.1023/a:1025635913927. [DOI] [PubMed] [Google Scholar]
- 2.Bouchard C. Gene-environment interactions in the etiology of obesity: Defining the fundamentals. Obesity. 2008;16:S5–S10. doi: 10.1038/oby.2008.528. [DOI] [PubMed] [Google Scholar]
- 3.Agurs-Collins T, Khoury MJ, Simon-Morton D, et al. Public health genomics: Translating obesity genomics research into population health benefits. Obesity. 2008;16:S85–S94. doi: 10.1038/oby.2008.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marti A, Martinez-Gonzalez MA, Martinez JA. Interaction between genes and lifestyle factors on obesity. Proceedings of the Nutrition Society. 2008;67:1–8. doi: 10.1017/S002966510800596X. [DOI] [PubMed] [Google Scholar]
- 5.Collins FS. Has the revolution arrived? Nature. 2010;464:674–675. doi: 10.1038/464674a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guttmacher AE, Porteous ME, McInerney JD. Educating health-care professionals about genetics and genomics. Nature Reviews Genetics. 2007;8:151–157. doi: 10.1038/nrg2007. [DOI] [PubMed] [Google Scholar]
- 7.Foster GD, Wadden TA, Makris AP, et al. Primary care physicians’ attitudes about obesity and its treatment. Obesity Research. 2003;11:1168–1177. doi: 10.1038/oby.2003.161. [DOI] [PubMed] [Google Scholar]
- 8.Ogden J, Bandara I, Cohen H, et al. General practicioners’ and patients’ models of obesity: Whose problem is it? Patient Education and Counseling. 2001;44:227–233. doi: 10.1016/s0738-3991(00)00192-0. [DOI] [PubMed] [Google Scholar]
- 9.Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. Journal of the American Medical Association. 1999;282:1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 10.Scott JG, Cohen D, DiCiccio-Bloom B, et al. Speaking of weight: How patients and primary care clinicians initiate weight loss counseling. Preventive Medicine. 2004;38:819–827. doi: 10.1016/j.ypmed.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 11.Thande NK, Hurstak EE, Sciacca RE, Giardina E-GV. Management of obesity: A challenge for medical training and practice. Obesity. 2009;17:107–113. doi: 10.1038/oby.2008.478. [DOI] [PubMed] [Google Scholar]
- 12.Tham M, Young D. The role of the general practitioner in weight management in primary care - a cross sectional study in General Practice. BMC Family Practice. 2008;9 doi: 10.1186/1471-2296-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simkin-Silverman LR, Gleason KA, King WC, et al. Predictors of weight control advice in primary care practices: Patient health and psychosocial characteristics. Preventive Medicine. 2005;40:71–82. doi: 10.1016/j.ypmed.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 14.Jay M, Kalet A, Ark T, et al. Physicians’ attitudes about obesity and their associations with competency and specialty: A cross-sectional study. BMC Health Services Research. 2009;9 doi: 10.1186/1472-6963-9-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Visser F, Hiddink G, Koelen M, et al. Longitudinal changes in GPs’ task perceptions, self-efficacy, barriers, and practices of nutrition education and treatment of overweight. Family Practice. 2008;25:i105–i111. doi: 10.1093/fampra/cmn078. [DOI] [PubMed] [Google Scholar]
- 16.Block JP, DeSalvo KB, Fisher WP. Are physicians equipped to address the obesity epidemic? Knowledge and attitudes of internal medicine residents. Preventive Medicine. 2003;36:669–675. doi: 10.1016/s0091-7435(03)00055-0. [DOI] [PubMed] [Google Scholar]
- 17.Hayden MJ, Dixon JB, Piterman L, O’Brien PE. Physician attitudes, beliefs, and barriers toward the management and treatment of adult obesity: A literature review. Australian Journal of Primary Health. 2008;14:9–18. [Google Scholar]
- 18.Leventhal H, Benyamini Y, Brownlee S. Perceptions of health and illness. Amsterdam: Harwood; 1997. Illness representations: Theoretical foundations; pp. 1–18. [Google Scholar]
- 19.Ogden J, Flanagan Z. Beliefs about the causes and solutions to obesity: A comparison of GPs and lay people. Patient Education and Counseling. 2008;71:72–78. doi: 10.1016/j.pec.2007.11.022. [DOI] [PubMed] [Google Scholar]
- 20.Grant RW, Hivert M, Pandiscio JC, et al. The clinical application of genetic testing in type 2 diabetes: A patient and physician survey. Diabetologia. 2009;52:2299–2305. doi: 10.1007/s00125-009-1512-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Puhl RM, Heuer CA. The stigma of obesity: A review and update. Obesity. 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 22.Harvey EL, Hill AJ. Health professionals’ views of overweight people and smoking. International Journal of Obesity. 2001;25:1253–1261. doi: 10.1038/sj.ijo.0801647. [DOI] [PubMed] [Google Scholar]
- 23.Price JH, Desmond SM, Krol RA, Snyder FF, O’Connell JK. Family practice physicians’ beliefs, attitudes, and practices regarding obesity. American Journal of Preventive Medicine. 1987;3:339–345. [PubMed] [Google Scholar]
- 24.Beach MC, Roter DL, Wang NY, Duggan PS, Cooper LA. Are physicians’ attitudes of respect accurately perceived by patients and associated with more positive communication behaviors? Patient Education and Counseling. 2006;62:347–354. doi: 10.1016/j.pec.2006.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Street RL, Jr, Gordon H, Haidet P. Physicians’ communication and perceptions of patients: Is it how they look, how they talk, or is it just the doctor? Social Science and Medicine. 2007;64:586–598. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Persky S, Eccleston CP. Medical student bias and care recommendations for an obese versus non-obese virtual patient. International Journal of Obesity. doi: 10.1038/ijo.2010.173. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African-American obese women. International Journal of Obesity. 2006;30:147–155. doi: 10.1038/sj.ijo.0803105. [DOI] [PubMed] [Google Scholar]
- 28.Puhl RM, Brownell KD. Psychosocial origins of obesity stigma: Toward changing a powerful and pervasive bias. Obesity Reviews. 2003;4:213–227. doi: 10.1046/j.1467-789x.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- 29.Weiner B, Perry RP, Magnusson J. An attributional analysis of reactions to stigmas. Journal of Personality and Social Psychology. 1988;55:738–748. doi: 10.1037//0022-3514.55.5.738. [DOI] [PubMed] [Google Scholar]
- 30.Crandall CS. Prejudice against fat people: Ideology and self-interest. Journal of Personality and Social Psychology. 1994;66:882–894. doi: 10.1037//0022-3514.66.5.882. [DOI] [PubMed] [Google Scholar]
- 31.Daníelsdóttir S, O’Brien KS, Ciao A. Anti-fat prejudice reduction: A review of published studies. Obesity Facts. 2010;3:47–58. doi: 10.1159/000277067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ross KM, Shivy VA, Mazzeo SE. Ambiguity and judgments of obese individuals: No news could be bad news. Eating Behaviors. 2009;10:152–156. doi: 10.1016/j.eatbeh.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 33.Teachman BA, Gapinski KD, Brownell KD, Jeyaram S. Demonstrations of implicit anti-fat bias: The impact of providing causal information and evoking sympathy. Health Psychology. 2003;22:68–78. doi: 10.1037//0278-6133.22.1.68. [DOI] [PubMed] [Google Scholar]
- 34.Wiese HJC, Wilson JF, Jones RA, Neises M. Obesity stigma reduction in medical students. International Journal of Obesity. 1992;16:859–868. [PubMed] [Google Scholar]
- 35.O’Brien KS, Puhl RM, Latner JD, Mir AS, Hunter JA. Reducing anti-fat prejudice in preservice health students: A randomized trial. Obesity. doi: 10.1038/oby.2010.79. In Press. [DOI] [PubMed] [Google Scholar]
- 36.Loomis JM, Blascovich JJ, Beall AC. Immersive virtual environments as a basic research tool in psychology. Behavior Research Methods, Instruments, and Computers. 1999;31:557–564. doi: 10.3758/bf03200735. [DOI] [PubMed] [Google Scholar]
- 37.Blascovich J, Loomis J, Beall A, et al. Immersive virtual environment technology as a research tool for social psychology. Psychological Inquiry. 2002;13:103–125. [Google Scholar]
- 38.Persky S, McBride CM. Immersive virtual environment technology: a promising tool for future social and behavioral genomics research and practice. Health Communication. 2009;24:677–682. doi: 10.1080/10410230903263982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McCall C, Blascovich J. How, when, and why to use digital experimental virtual environments to study social behavior. Social and Personality Psychology Compass. 2009;3:744–758. [Google Scholar]
- 40.Mast MS, Hall JA, Roter DL. Caring and dominance affect participants’ perceptions and behaviors during a virtual medical visit. Journal of General Internal Medicine. 2008;23:53–527. doi: 10.1007/s11606-008-0512-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mast MS, Hall JA, Roter DL. Disentangling physician sex and physician communication style: Their effects on patient satisfaction in a virtual medical visit. Patient Education and Counseling. 2007;68:16–22. doi: 10.1016/j.pec.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 42.Deladisma AM, Cohen M, Stevens A, et al. Do medical students respond empathetically to a virtual patient? The American Journal of Surgery. 2007;193:756–760. doi: 10.1016/j.amjsurg.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 43.Raij AB, Johnsen K, Dickerson RF, et al. Comparing interpersonal interactions with a virtual human to those with a real human. IEEE Transactions on Visualization and Computer Graphics. 2007;13:1–15. doi: 10.1109/TVCG.2007.1036. [DOI] [PubMed] [Google Scholar]
- 44.Johnsen K, Raij A, Stevens A, Lind DS, Lok B. The validity of a virtual human experience for interpersonal skills education. Proceedings of the SIGCHI conference on Human factors in computing systems; 2007. pp. 1049–1058. [Google Scholar]
- 45.Coulehan J, Williams PC. Vanquishing virtue: The impact of medical education. Academic Medicine. 2001;76:598–605. doi: 10.1097/00001888-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 46.Hebl MR, Xu J. Weighing the care: Physicians’ reactions to the size of a patient. International Journal of Obesity. 2001;25:1246–1252. doi: 10.1038/sj.ijo.0801681. [DOI] [PubMed] [Google Scholar]
- 47.Puhl RM, Schwartz MB, Brownell KD. Impact of perceived consensus on stereotypes about obese people: A new approach for reducing bias. Health Psychology. 2005;24:517–525. doi: 10.1037/0278-6133.24.5.517. [DOI] [PubMed] [Google Scholar]
- 48.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- 49.Friedman JM. Modern science versus the stigma of obesity. Nature Medicine. 2004;10:563–569. doi: 10.1038/nm0604-563. [DOI] [PubMed] [Google Scholar]
- 50.Weinsier RL, Hunter GR, Heini AF, Goran MI, Sell SM. The etiology of obesity: Relative contribution of metabolic factors, diet, and physical activity. The American Journal of Medicine. 1998;105:145–150. doi: 10.1016/s0002-9343(98)00190-9. [DOI] [PubMed] [Google Scholar]
- 51.Martinez JA. Body-weight regulation: Causes of obesity. Proceedings of the Nutrition Society. 2000;59:337–345. doi: 10.1017/s0029665100000380. [DOI] [PubMed] [Google Scholar]
- 52.Ernst E, Canter PH. A systematic review of systematic reviews of spinal manipulation. Journal of the Royal Society of Medicine. 2006;99:192–196. doi: 10.1258/jrsm.99.4.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nappi G, Perrotta A, Rossa P, Sandrini G. Chronic daily headache. Expert Review of Neurotherapeutics. 2008;8:361–384. doi: 10.1586/14737175.8.3.361. [DOI] [PubMed] [Google Scholar]


