Abstract
Study Objectives:
To determine the proportion of adolescents whose bedtime is set by their parents and to evaluate whether parent-set bedtimes are associated with earlier bedtimes, more sleep, and better daytime functioning.
Participants:
385 adolescents aged 13-18 years (mean = 15.6, SD = 0.95; 60% male) from 8 socioeconomically diverse schools in South Australia.
Measurements & Methods:
Adolescents completed the School Sleep Habits Survey during class time and then completed an 8-day Sleep Diary. The Flinders Fatigue Scale was completed on the final day of the study.
Results:
17.5% of adolescents reported a parent-set bedtime as the main factor determining their bedtime on school nights. Compared to adolescents without parent-set bedtimes, those with parent-set bedtimes had earlier bedtimes, obtained more sleep, and experienced improved daytime wakefulness and less fatigue. They did not differ significantly in terms of time taken to fall asleep. When parent-set bedtimes were removed on weekends, sleep patterns did not significantly differ between groups.
Conclusions:
Significant personal and public health issues, such as depression and accidental injury and mortality, are associated with insufficient sleep. Converging biological and psychosocial factors mean that adolescence is a period of heightened risk. Parent-set bedtimes offer promise as a simple and easily translatable means for parents to improve the sleep and daytime functioning of their teens.
Citation:
Short MA; Gradisar M; Wright H; Lack LC; Dohnt H; Carskadon MA. Time for bed: parent-set bedtimes associated with improved sleep and daytime functioning in adolescents. SLEEP 2011;34(6):797-800.
Keywords: Bedtime, sleep, sleepiness, fatigue, adolescence, Sleep Habits Survey
INTRODUCTION
Many adolescents obtain insufficient sleep to maintain optimal functioning during the day.1 Insufficient sleep during adolescence has been associated with sleepiness and fatigue, poor academic outcomes, and risk of depression and anxiety.2–8 Numerous biological and psychosocial factors emerge during adolescence pushing bedtimes later into the evening; however, sleep is curtailed by the need to get up for school.9 Psychosocial factors associated with later bedtimes and insufficient sleep include increased academic workload, increased part-time employment, and use of technology, particularly in the bedroom.10–16 Biological factors include the puberty-related delay of the circadian body clock and reduced homeostatic sleep drive at bedtime.17,18 These factors are all conducive to longer periods of evening wakefulness.
Although risk factors for insufficient sleep and associated negative sequelae have been identified, there remains a paucity of research into protective factors. Parental involvement in regulating adolescent sleep schedules may be one such factor. While the maintenance of parental involvement in adolescents' sleep has support,19 comparison of the impact upon sleep when bedtimes are set by parents compared to self-selected bedtimes is lacking. Research has revealed as children get older, fewer parents set limits around their bedtime.11 Such practice was associated with a decline in total sleep time, though this association may result from uncontrolled covariants, such as general parent limit setting and children's age.
Gangwisch and colleagues recently examined timing of parent-set bedtimes in a nationally representative U.S. sample of 15,659 adolescents in grades 7-12.20 They found that adolescents with later (after 12 midnight) or no parent-set bedtimes were 24% more likely to suffer from depression and were 20% more likely to have reported suicidal ideation in the past year than adolescents with parent-set bedtimes before 10 pm. The authors argue that the relationship between parent-set bedtimes and risk of depression and suicidal ideation is likely to be mediated by decreased sleep duration and the perception of getting insufficient sleep.
The current study seeks to extend this work, which is an important and timely topic of research. While depression and suicidal ideation are significant and important public health concerns, this study focused upon the general day-to-day functioning of adolescents. Specifically, alertness and fatigue of adolescents with parent-set bedtimes were compared to those without. To avoid any social desirability responding that may occur when asking parents about their involvement (or lack thereof) in setting the teens' bedtime, adolescent report was used to identify the main factor determining bedtime on school nights. Lastly, this study measured sleep parameters using an 8-day sleep diary. This offered greater validity as a measure of teens' sleep patterns than survey report, as it is less likely to be sensitive to recall bias than retrospective survey.21
We hypothesized that adolescents with parent-set bedtimes would have earlier bedtimes than those who did not, and that they would obtain more sleep and experience less daytime sleepiness and fatigue. One concern with externally determined bedtimes is that adolescents may attempt to initiate sleep before they are physiologically ready, thus taking longer to fall asleep and heightening the risk of sleep-onset insomnia. Thus, we also assessed whether parental-set bedtimes were associated with longer sleep onset latencies.
METHODS
Participants
Participants were 385 adolescents (60% male) recruited from 8 socioeconomically diverse high schools in South Australia. Schools were selected using stratified random sampling. This was achieved by ranking schools according to the percentage of students receiving a State government benefit to assist low-income families with education costs. The ranked list was then divided into 8 strata, with one school being randomly selected per octile. One class in each of Years 9, 10, and 11 participated per school. Student age ranged from 13 to 18 years (M = 15.6, SD = 0.95). Seventy-seven percent of participants resided with 2 parents. Response rate was 84%. Informed consent was obtained from the adolescent, a parent/guardian and the school principals. The Flinders University Social and Behavioural Research Ethics Committee and the Department of Education and Children's Services of South Australia approved the study. Participants were reimbursed for their time with a $40 gift voucher.
Measures
Parent-set bedtime and maintenance of wakefulness during daily activities, were assessed using items in the School Sleep Habits Survey (SSHS).22 The SSHS is one of the most widely used survey tools in adolescent sleep. Parent-set bedtimes were assessed using the item “What is the main reason that you usually go to bed on school days? (pick one).” Eight possible responses were available, including “My parents have set my bedtime,” “I feel sleepy,” and “I finish my homework,” and “Other (please describe).” All responses other than “My parents have set my bedtime” were combined to form a dichotomous variable. While factors determining bedtime such as, “I finish my homework,” or “I feel sleepy,” do not preclude some parental influence, our focal interest was in determining the primary factor regulating bedtime.
The maintenance of wakefulness scale23 asks adolescents whether they have struggled to stay awake or fallen asleep in the last 2 weeks during 13 daily activities, including while watching television or while in a class at school. As the majority of our sample was aged under 16 (the minimum legal driving age), the question referring to driving was excluded from these analyses. Item responses range from 0 (No) to 3 (Both struggled to stay awake and fallen asleep). Total scores could range from 0 to 36, with higher scores indicating more difficulty maintaining wakefulness (i.e., greater daytime sleepiness). Cronbach α for this sample was 0.77.
An 8-day sleep diary was used to collect information on daily bedtime, sleep onset latency, and total sleep time. Data from school night variables were used in this study. While data were collected on weekend sleep patterns, the proportion of adolescents reporting a weekend parent-set bedtime (< 2%) was too small to support analysis.
The Flinders Fatigue Scale (FFS)24 is a 7-item scale that asks about the experience of fatigue in the previous 2 weeks. The FFS consists of questions, such as “Was fatigue a problem for you?” and “How severe was the fatigue you experienced?” Responses range from 0 (Not at all) to 4 (Extremely). Total scores could range from 0 to 30, with higher scores indicating higher levels of fatigue. Cronbach α for the fatigue scale was 0.91 in this sample.
Procedure
Participants completed the modified SSHS during school class time. A Sleep Diary was completed for 8 days following completion of the SHSS. During this time, participants telephoned the Flinders University Sleep Laboratory morning and night to record their bedtimes and wake times. These calls were time and date stamped and served as a validity check, to ensure that sleep diaries were completed twice daily, rather than retrospectively, when recall is likely to be impaired. On the last day of the study, participants completed the Flinders Fatigue Scale.
Statistical Analyses
Adolescents whose parents set their bedtimes (N = 68) were compared with adolescents without parent-set bedtimes (N = 310) using one-way ANOVAs. Where age or sex was significantly related to the outcome variable, one-way ANCOVA, with age and sex as covariates, was used. Sum of squares II was utilized to adjust for unequal sample size between groups.
RESULTS
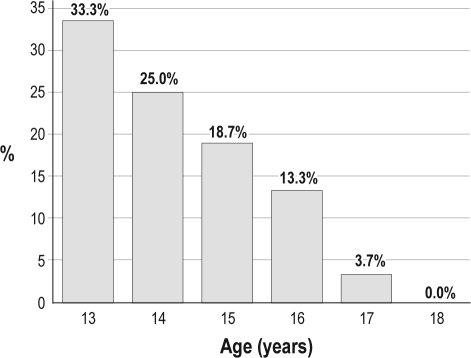
Of adolescents studied, 17.5% reported a parent-set bedtime on school nights. The proportion of boys (23%) who reported a parent-set bedtime was significantly greater than the proportion of girls (11%). Those reporting a parent-set bedtime were also significantly younger. Figure 1 shows the steady decline in the percentage of adolescents whose parents set their bedtime from age 13 to 18 years. To examine any potentially confounding demographic differences between groups, the proportion of adolescents residing in a 2-parent household, maternal education or full-time employment, paternal education or full-time employment, and socioeconomic status, as measured by school stratum, were examined. No differences were found on any of these variables, all P > 0.05. To examine whether any differences in academic or extracurricular commitments occurred between the groups, the number of hours spent per week on homework, sports, or extracurricular activities were compared on both school nights and weekends. The teens with parent-set bedtimes did not differ from those without on any of these variables, all P > 0.05.
Figure 1.
The percentage of adolescents with a parent-set bedtime from ages 13 to 18 years.
Results of inferential tests, together with descriptive statistics, are presented in Table 1. ANCOVA results, after adjusting for age and gender, showed that adolescents with a parent-set bedtime went to bed significantly earlier, with bedtimes occurring an average of 23 minutes earlier. This group also obtained an average of 19 minutes extra sleep per school night. While this increase in sleep quantity was fairly modest, it was nonetheless associated with improvements in daytime functioning. Students with parent-set bedtimes reported less fatigue and had less trouble maintaining wakefulness during daily activities. No significant differences were found between groups for the time taken to fall asleep, indicating that parent-set bedtimes were not associated with increased risk of prolonged sleep latencies and possible sleep-onset insomnia.
Table 1.
Descriptive and inferential statistics comparing those with a parent-set bedtime to those without on sleep and daytime functioning
| Parent-set bedtime on school nights M (SD) |
|||
|---|---|---|---|
| Yes | No | F value | |
| Sex | 75% male | 55% male | X2 = 9.06** |
| Age | 15.2 years (0.85) | 15.6 years (0.97) | 10.73** |
| Bedtime on school nights (Diary) | 10:10 pm (0.11)a | 10:33 pm (0.05) | 8.92** |
| Sleep on school nights (Diary) | 8h 32m (7.1)a | 8h 13m (3.3) | 5.94* |
| Fatigue (FFS) | 5.4 (0.7)a | 8.1 (0.3) | 12.04** |
| Maintaining wakefulness (SSHS) | 2.2 (0.5)a | 4.6 (0.2) | 21.37*** |
| SOL on school nights (Diary) | 20m (15) | 19m (16) | 1.59 |
| Bedtime on weekends (Diary) | 11:44 pm (0.18)a | 11:40 pm (0.08) | 0.07 |
| Sleep on weekends (Diary) | 8h 45m (10.4)a | 8h 39m (4.9) | 0.28 |
P < 0.05
P < 0.01
P < 0.001.
Estimated marginal means and standard error, adjusting for the effect of age and sex.
To further strengthen these findings, group differences on weekend bedtimes and total sleep times were examined, comparing those who had a parent-set bedtime on school nights to those who did not. Because fewer than 2% of the sample reported a parent-set bedtime on weekends, this enabled us to examine the effect of removing parent limit setting. If, as we hypothesized, parent limit setting was putting the brakes on later bedtimes and the truncation of sleep, we would expect to find no significant differences between the 2 groups on weekends, when this restraint was removed. After excluding those participants who had a parent-set bedtime on weekends (N = 7), no significant differences were found for either weekend bedtime or weekend total sleep time.
DISCUSSION
Adolescents with parent-set bedtimes on school nights reported earlier bedtimes on school nights, more sleep on school nights, less fatigue, and had less trouble maintaining wakefulness. These results are consistent with the findings of Gangwisch and colleagues,20 who found that earlier parent-set bedtimes were associated with earlier bedtimes and more sleep, as well as a lower risk of depression and suicidal ideation than parent-set bedtimes that were either late or non-existent. In this study, parent-set bedtimes were determined by parents' response to the question, “What time does {name} have to go to bed on weeknights?” This phrasing may introduce not only social desirability responding, with parents wanting to present themselves in a positive light, but also general response bias because of the implicit assumption that the adolescent has a parent-set bedtime, thus leading the parent to give a compliant response. This may explain why the proportion of adolescents with a parent-set bedtime is substantially higher in the Gangwisch study (over 75%) than in another large-scale study, in which the adolescents themselves reported only 5.1% as having a parent-set bedtime.9 Thus, this method enables the collection of information from the adolescents themselves about exactly what (or who) is determining their bedtimes on school nights.
To the authors' knowledge, this is the first study to compare the sleep and daytime functioning in adolescents with parent-set bedtimes to those without. Participants were adolescents across the socioeconomic spectrum who completed an 8-day sleep diary, both of which are strengths of the study. The findings support the potential protective benefit of parent limit-setting around bedtimes for adolescents. Due to the cross-sectional nature of the study, we could not determine causation or rule out other potential explanations for these findings. It is possible that parents involved in regulating the sleep of their adolescents are more likely to be involved in establishing and helping to maintain good sleep hygiene for the adolescent. They may also be more involved in the lives of their adolescent and apply greater limit setting, generally. However, the finding that differences in sleep parameters disappear on weekends (when parental involvement in sleep is withdrawn) strengthens the argument that parent limit setting is responsible for the school night differences. If other confounding factors between the groups were responsible for these school-night results, we would expect that they would operate similarly across weekends to maintain these differences. These findings suggest that both groups may have had similar sleep patterns if parents in the parent-set bedtime group had not been involved in setting bedtimes. So the school night differences arose, not from intrinsic differences in sleep between the groups, but from parental involvement. Previous studies using polysomnography or actigraphy provide support for the notion that adolescents obtain more sleep when given the opportunity through earlier bedtimes.25,26 Sadeh and colleagues randomly allocated 77 children, aged 9 to 12 years, to either three nights of sleep restriction or three nights of sleep extension. Children in the sleep extension group obtained 35 minutes more sleep per night than their usual amount, which led to improvements in neurobehavioral performance. The researchers remarked that even modest increases in sleep across three nights led to demonstrable benefits. These experimental studies provide support for the idea that earlier bedtimes enable more sleep, irrespective of differing demographic and family factors, and that even small increases in nighttime sleep have positive benefits for children and adolescents in terms of their feeling and functioning.
The benefits of small, but regular, increases in sleep may take on an even greater importance in populations where adolescents' sleep is more restricted. On average, the Australian adolescents in this study obtain more sleep than many adolescents worldwide.27 The study by Gangwisch and colleagues revealed that adolescents with an earlier parent-set bedtime obtained an extra 40 minutes of sleep on school nights and had reduced risk of depression and suicidal ideation. Of interest, the “low-risk” adolescents in the Gangwisch study were obtaining almost the same amount of sleep per night (8h 10m) as the “higher-risk” adolescents in the present study (8h 13m), who did not have a parent-set bedtime and reported less sleep and poorer daytime functioning. While the 19 extra minutes of sleep per night gained by adolescents in this study may seem small, the cumulative effect of this extra sleep was associated with improved daytime functioning and may have further reaching effects in terms of improved emotional regulation and reduced risk of psychopathology. Further research could strengthen these findings by gathering daily reports of the main factor determining each bedtime and validating these findings with objective measures of sleep.
Numerous risk factors serve to push adolescent bedtimes later and shorten sleep. Parent limit-setting may be one simple way to counter these factors and protect sleep, with possible benefits for improved daytime functioning. Adolescents face a multitude of important developmental tasks. These include managing more mature social and intimate relationships, completing secondary school education, and learning to drive. Considering the important “flow-on” effects of insufficient sleep and impaired daytime functioning, including poor emotional regulation, diminished school performance and increased risk of sleep related accidents,2,3,4,6,28 parental involvement in the sleep of adolescents takes on added importance.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This work was conducted at the Flinders University of South Australia and was funded by Australian Research Council grant #DP0881261.
REFERENCES
- 1.Owens JA. Sleep in children: cross-cultural perspectives. Sleep Biol Rhythms. 2004;2:165–73. [Google Scholar]
- 2.Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bogels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: a meta-analytic review. Sleep Med Rev. 2009;14:179–89. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 3.Wolfson AR, Carskadon MA. Understanding adolescents' sleep patterns and school performance: a critical appraisal. Sleep Med Rev. 2003;7:491–506. doi: 10.1016/s1087-0792(03)90003-7. [DOI] [PubMed] [Google Scholar]
- 4.Meijer AM. Chronic sleep reduction, functioning at school and school achievement in preadolescents. J Sleep Res. 2008;17:395–405. doi: 10.1111/j.1365-2869.2008.00677.x. [DOI] [PubMed] [Google Scholar]
- 5.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatric Res. 2006;40:700–8. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Dahl RE, Lewin DS. Pathways to adolescent sleep and behaviour. J Adolesc Health. 2002;31:175–84. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- 7.Lui X. Sleep and adolescent suicidal behaviour. Sleep. 2004;27:1351–8. doi: 10.1093/sleep/27.7.1351. [DOI] [PubMed] [Google Scholar]
- 8.Taylor DJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Epidemiology of insomnia, depression and anxiety. Sleep. 2005;28:1457–64. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- 9.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–87. [PubMed] [Google Scholar]
- 10.Gau SF, Soong WT. Sleep problems of junior high school students in Taipei. Sleep. 1995;18:667–73. doi: 10.1093/sleep/18.8.667. [DOI] [PubMed] [Google Scholar]
- 11.Carskadon MA. Patterns of sleep and sleepiness in adolescents. Pediatrician. 1990;17:5–12. [PubMed] [Google Scholar]
- 12.Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. Circadian preference, sleep and daytime behaviour in adolescence. J Sleep Res. 2002;11:191–9. doi: 10.1046/j.1365-2869.2002.00302.x. [DOI] [PubMed] [Google Scholar]
- 13.Carskadon MA. Factors influencing sleep patterns of adolescents. In: Carskadon MA, editor. Adolescent sleep patterns: biological, social and psychological influences. New York: Cambridge University Press; 2002. pp. 4–26. [Google Scholar]
- 14.Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med. 2010;11:735–42. doi: 10.1016/j.sleep.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 15.Dworak M, Schierl T, Bruns T, Struder HK. Impact of singular excessive computer game and television exposure on sleep patterns and memory performance of school-aged children. Pediatrics. 2007;120:978–85. doi: 10.1542/peds.2007-0476. [DOI] [PubMed] [Google Scholar]
- 16.Knutson KL, Lauderdale DS. Sociodemographic and behavioural predictors of bedtime and wake time among US adolescents aged 15 to 17 years. J Pediatr. 2009;154:426–30. doi: 10.1016/j.jpeds.2008.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carskadon MA, Acebo C, Richardson GS, et al. Long nights protocol: access to circadian parameters in adolescents. J Biol Rhythms. 1997;12:278–89. doi: 10.1177/074873049701200309. [DOI] [PubMed] [Google Scholar]
- 18.Jenni OG, Achermann P, Carskadon MA. Homeostatic sleep regulation in adolescents. Sleep. 2005;28:1446–54. doi: 10.1093/sleep/28.11.1446. [DOI] [PubMed] [Google Scholar]
- 19.Le Bourgios MK, Giannotti F, Wolfson AR, et al. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics. 2005;115:257–65. doi: 10.1542/peds.2004-0815H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gangwisch JE, Babiss LA, Malaspina D, Turner JB, Zammit GK, Posner K. Earlier parental set bedtimes as a protective factor against depression and suicidal ideation. Sleep. 2010;33:97–106. doi: 10.1093/sleep/33.1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155–73. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]
- 22.Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a Sleep Habits Survey for adolescents. Sleep. 2003;26:213–6. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- 23.Carskadon MA, Seifer R, Acebo C. Reliability of six scales in a sleep questionnaire for adolescents. Sleep Res. 1991;20:421. [Google Scholar]
- 24.Gradisar M, Lack L, Richards H, et al. The Flinders Fatigue Scale: Preliminary psychometric properties and clinical sensitivity of a new scale for measuring daytime fatigue associated with insomnia. J Clin Sleep Med. 2007;3:722–8. [PMC free article] [PubMed] [Google Scholar]
- 25.Carskadon MC, Keenan S, Dement WC. Nighttime sleep and daytime sleep tendency in preadolescents. In: Guilleminault C, editor. Sleep and its disorders in children. New York: Raven Press; 1987. pp. 43–52. [Google Scholar]
- 26.Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Dev. 2003;74:444–55. doi: 10.1111/1467-8624.7402008. [DOI] [PubMed] [Google Scholar]
- 27.Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: A review and meta-analysis of age, region, and sleep. Sleep Med. 2010 doi: 10.1016/j.sleep.2010.11.008. In press. [DOI] [PubMed] [Google Scholar]
- 28.Pizza F, Contardi S, Antognini AB, et al. Sleep quality and motor vehicle crashes in adolescents. J Clin Sleep Med. 2010;15:41–5. [PMC free article] [PubMed] [Google Scholar]