Abstract
Objective
Metabolic syndrome is associated with elevated risk for cardiovascular disease and diabetes, and has increased prevalence in low-income African-Americans, which constitutes a significant health disparity. The mechanisms responsible for this disparity remain unclear; the current study investigated the relationship between Posttraumatic Stress Disorder (PTSD) and metabolic syndrome.
Method
We assessed childhood and adult trauma history, Major Depressive Disorder (MDD), PTSD, and the components of metabolic syndrome in an urban population. We recruited 245 low socio-economic status (SES), primarily African American subjects from general medical clinics in an inner-city hospital.
Results
Trauma exposure was extremely prevalent, with 90.6% of subjects reporting at least one significant trauma, and 18.8% of subjects meeting criteria for a current PTSD. Metabolic syndrome was also prevalent in this population (33.2%), with significantly higher rates among patients with current PTSD (47.8%, p<.05). After controlling for demographics, smoking history, antipsychotic use, depression, and exercise, current PTSD remained the only significant predictor of metabolic syndrome (p=0.006).
Conclusions
PTSD is associated with increased rates of metabolic syndrome within a traumatized, impoverished urban population. Further studies should investigate if PTSD treatment may reduce the rates of metabolic syndrome, improve overall health outcomes, and decrease healthcare disparities in minority populations.
Keywords: Post-traumatic Stress Disorder, Depression, African-American, Minority, Trauma, Child Abuse, Childhood Maltreatment, Psychiatry
Introduction
The elements of metabolic syndrome, including hyperglycemia, obesity, hyperlipidemia, and hypertension, are among the leading risk factors for cardiovascular morbidity and mortality [1-5]. The increased prevalence of cardiovascular risk factors in African-Americans is well-established, but the mechanisms underlying this important health disparity are unclear [6-10]. Some investigators have found that socioeconomic status (SES) plays an important role in health disparity [11]. One possible explanation that has received little attention is that metabolic syndrome and cardiovascular risk factors develop as a result of high rates of trauma exposure in marginalized populations [12].
Previous studies have reported that many urban, low SES minority populations have extremely high rates of trauma exposure and are at elevated risk for Posttraumatic Stress Disorder (PTSD) [13-16]. Trauma exposure and PTSD are associated with higher rates of physical morbidity and mortality, as well as increased healthcare utilization and expenditures [17-20]. In addition, trauma exposure and/or a diagnosis of PTSD are associated with a variety of metabolic abnormalities [21-26] which may mediate these adverse health outcomes. For example, combat veterans and civilian police officers with a diagnosis of PTSD have been reported to have higher levels of serum lipids [26, 27], as well as a higher rate of metabolic syndrome [18, 20, 23, 25, 26]. Similarly, elevated rates of diabetes and cardiovascular disease have been reported in civilians and combat veterans with PTSD [28, 29]. In addition, an association has been demonstrated between a diagnosis of PTSD and the presence of metabolic syndrome in psychiatric outpatients receiving antipsychotic medications [24]. However, there are no published reports of the relationship between the presence of metabolic syndrome and diagnosis of PTSD in civilian, low SES, minority individuals in an inner city setting.
The high rates of trauma exposure and stress-related psychiatric disorders observed in at-risk low SES urban African-American populations [13, 15] may also be associated with alterations in metabolic functioning that may partially account for observed health disparities within this population. Frequent activation of the body's stress response as a result of trauma and PTSD can cause a cumulative strain on the body. Previous studies have demonstrated that comprehensive measures of physiological function can be more predictive of cumulative biological risk than approaches that assess biological risk factors as individual parameters [30]. Therefore, we focused on the prevalence of metabolic syndrome, which is characterized by the presence of multiple metabolic risk factors in a given individual and is associated with increased risk for cardiovascular disease, diabetes, stroke, and multiple other medical sequellae. To further explore this hypothesis, we examined whether childhood and adult trauma history, as well as Major Depressive Disorder (MDD) and PTSD were associated with metabolic syndrome within individuals recruited from general medical clinic waiting rooms in an urban public hospital.
Methods
Recruitment and General Study Procedures
The data for this study were collected to investigate the effects of PTSD on metabolic function and were drawn from a larger sample of subjects enrolled in a study of risk factors for PTSD in an urban, low-income, predominantly African-American population [15, 31]. Individual subjects were recruited from waiting rooms in multiple primary care clinics at Grady Memorial Hospital, a publicly funded hospital primarily serving individuals of low SES in Atlanta, Georgia. Prospective subjects were invited to complete a screening interview, and a subset of subjects returned for additional study visits to participate in more in-depth psychiatric interviews and physiological assessments. Demographic data were ascertained through subject self-report. As part of the multi-day study, subjects underwent psychological assessments, a physical examination, a fasting morning blood draw, and morphometric measurements. To be eligible for participation, subjects had to be at least age 18 or older, provide informed consent, and be able to speak English. Subjects were excluded if they had active/unstable psychotic symptoms or prominent suicidal ideation at the time of the study, had dementia, were pregnant, or took oral corticosteroids within the past month. All other subjects for whom we collected metabolic data were included from the larger study. A detailed account of the general Grady Trauma Project study methods has been previously published and can be found in Gillespie et al[15]. The final sample size included 245 participants.
Trauma and Psychological Measures
Trauma History
The Traumatic Events Inventory (TEI) [15, 31] is a 14-item instrument for assessing exposure to traumatic events in childhood and adulthood. For each traumatic life event, the TEI assesses experiencing and witnessing of events separately. In addition to assessing the presence and absence of each type of trauma exposure, the TEI also assesses frequency of exposure within each type of trauma. The TEI, which was developed for use with our specific study population, is similar in number of questions and format to other self report assessments of trauma exposure see e.g., [32] and see [33] for a review of self-report instruments of civilian trauma exposure.
PTSD
PTSD symptoms and PTSD diagnosis were assessed using the Clinician Administered PTSD Scale (CAPS) [37, 38]. The CAPS is a structured interview with excellent psychometric properties [39], which provides a diagnosis of PTSD and can also be used as a continuous measure of PTSD symptomatology. A current (last 30 days) or lifetime diagnosis of PTSD was based on the presence/absence of each of the DSM-IV diagnostic criteria using a frequency rating of ≥1 paired with an intensity score of ≥ 2 as the scoring rule.
MDD
The Structured Clinical Interview for DSM-IV (SCID) [40] is a well-validated interview assessment for the diagnosis of clinical psychiatric disorders. Within the context of this study, the SCID was used to determine the presence or absence of current MDD.
Smoking and Substance Abuse
Lifetime history of smoking was assessed using responses from the Kreek-McHugh-Schluger-Kellogg scale. Current and lifetime substance abuse was determined based on SCID diagnosis of alcohol and drug abuse or dependence.
Physiologic Measures
Medical Evaluation and Laboratory Determinations
A study physician determined each subject's eligibility based on a medical examination performed by the study physician at the beginning of the study visit or based on review of records from a medical exam by a Grady physician completed within 2 months of study participation. Blood pressure, weight (kg), height (cm), and waist circumference (cm) were obtained by trained nursing staff at the Grady Hospital Clinical Research Center. Fasting blood samples were obtained by venipuncture between 0800 and 0900 during the baseline study assessment for each subject. Serum samples were obtained, processed, and then stored at −80° C for later processing in batches. Triglyceride (TG) and glucose were measured by enzymatic methods using reagent kits from Beckman Coulter Diagnostics (Fullerton, CA). High Density Lipoprotein (HDL) was ascertained by homogenous enzymatic methods using kits from Equal Diagnostics (Exton, PA).
Prescribed medications from the hospital were recorded and used as covariates when needed. Antipsychotics were prescribed within a subset of the cohort (<30), and these included: risperidone, ziprasidone, quetiapine, aripiprazole, and paliperidone.
Definition of Metabolic Syndrome
Within the context of this study, metabolic syndrome was defined using a modified version of the Adult Treatment Panel (ATP) III guidelines [2, 41]. ATP III guidelines have been widely used in the literature to assess metabolic syndrome in a wide range of racial and ethnic groups in the US and throughout the world, [42-45] and metabolic syndrome as defined by ATP III guidelines has been shown to predict cardiovascular disease and cerebrovascular disease in African American individuals [46].
Subjects who had at least 3 of the 5 risk characteristics were considered to have metabolic syndrome: 1) Fasting glucose ≥ 110 mg/dL , 2) Abdominal obesity based on a waist circumference of >102 cm for men or >88 cm for women, 3) Triglycerides ≥ 150 mg/dL, 4) HDL cholesterol <40 mg/dL for men or <50 mg/dL for women, and 5) Systolic blood pressure ≥ 130 or diastolic blood pressure ≥ 85 mmHg.
Statistical Analyses
We examined the relationship between PTSD, metabolic syndrome, and the individual components of metabolic syndrome by conducting chi square comparisons of the rate of metabolic syndrome in subjects with versus without current PTSD. Additionally, a logistic regression analysis was completed, examining metabolic syndrome as the outcome and current PTSD diagnosis as the predictor variable adjusting for age, sex, race, lifetime smoking history, current antipsychotic use, number and types of trauma exposure, and current diagnosis of MDD. We had full fasting data on all variables needed for establishing presence/absence of metabolic syndrome and PTSD for 245 subjects who were included in the chi-square, and 200 subjects for whom all variables were present for logistic regression analyses. We conducted secondary analyses to control for the effect of medications for diabetes, hypertension, and hyperlipidemia on any association between PTSD and metabolic syndrome.
Results
Patient Characteristics
The mean age of the study population was approximately 45 years, and was similar between those subjects with and without a current diagnosis of PTSD (Table 1). Although not statistically significant, the proportion of female subjects (69.6%) was higher in the group with a current diagnosis of PTSD versus those without that diagnosis (60.3%), reflecting the increased frequency of PTSD amongst women with a history of trauma exposure. As previously reported in this study population, race was primarily African-American (>89%) and did not differ between those subjects with and without PTSD [15]. At the time of the study, approximately 51% of subjects were unemployed with an additional 27% disabled. Unemployment and lower income were more frequent in the PTSD subjects compared to those without PTSD; however, these differences were not statistically significant.
Table 1.
Characteristics of Participants by Current PTSD Status (N=245)
| Measure | No current PTSD (n=199) |
Current PTSD (n=46) |
P value |
|---|---|---|---|
| Age, mean (sd) in years | 46.0 (11.86) | 43.70 (10.98) | 0.252 |
|
| |||
| Sex, No. (%) | 0.243 | ||
| Men | 79 (39.7%) | 14 (30.4%) | |
| Women | 120 (60.3%) | 32 (69.6%) | |
|
| |||
| Race, No. (%) | 0.890 | ||
| African American | 174 (88.8%) | 40 (90.9%) | |
| Caucasian | 15 (7.7%) | 3 (6.8%) | |
| Other | 7 (3.6%) | 1 (2.3%) | |
|
| |||
| Marital Status, No. (%) | 0.170 | ||
| Not Married | 175 (89.3%) | 36 (81.8%) | |
| Married | 21 (10.7%) | 8 (18.2%) | |
|
| |||
| Education, No. (%) | 0.414 | ||
| Less than HS | 41 (20.9%) | 11 (25.0%) | |
| GED or HS Grad | 79 (40.3%) | 13 (29.5%) | |
| ≥ Some College | 76 (38.8%) | 20 (45.5%) | |
|
| |||
| Employment, No. (%) | 0.651 | ||
| Unemployed | 100 (51.0%) | 25 (56.8%) | |
| Disabled | 53 (27.0%) | 12 (27.3%) | |
| Employed | 43 (21.9%) | 7 (15.9%) | |
|
| |||
| Monthly Income, No (%), $ | 0.238 | ||
| Less than $250 | 59 (30.7%) | 16 (38.1%) | |
| $250-$499 | 23 (12.0%) | 2 (4.8%) | |
| $500-$999 | 56 (29.2%) | 16 (38.1%) | |
| $1000 or more | 54 (28.1%) | 8 (19.0%) | |
|
| |||
| Cigarette Smoking, No. (%) | 0.385 | ||
| Never Smoked | 49 (25.8%) | 13 (32.5%) | |
| Lifetime Hx Smoking | 141 (74.2%) | 27 (67.5%) | |
|
| |||
| Current Substance Abuse, No. (%) | 0.244 | ||
| No Current Substance Abuse | 184 (95.3%) | 40 (90.9%) | |
| Current Substance Abuse | 9 (4.7%) | 4 (9.1%) | |
|
| |||
| Currently on Antipsychotics, No. (%) | 17 (8.5%) | 5 (10.9%) | 0.619 |
|
| |||
| Time of Trauma, No. (%) | 0.064 | ||
| None | 26 (14.2%) | 0 (0%) | |
| Adult Only | 71 (38.8%) | 17 (42.5%) | |
| Childhood Only | 30 (16.4%) | 6 (15.0%) | |
| Child and Adult | 56 (30.6%) | 16 (42.5%) | |
|
| |||
| Amount of Trauma, No. (%) | 0.092 | ||
| Not Experienced (but witnessed) | 19 (10.3%) | 2 (4.7%) | |
| 1 type of trauma | 20 (10.8%) | 1 (2.3%) | |
| 2 or more types of trauma | 146 (78.9%) | 40 (93%) | |
|
| |||
| Current MDD, No. (%) | <0.001 | ||
| No Current MDD | 176 (93.6%) | 24 (57.1%) | |
| Current MDD | 12 (6.4%) | 18 (42.9%) | |
Note, N's range from 223-245 due to occasional missing demographic data; All except for age (which was examined with ANOVA) are examined with chi-squared statistics.
Trauma and psychiatric diagnoses
Reported rates of trauma exposure were extremely high within this population. Of the 245 subjects examined for metabolic syndrome (Table 1) 90.6% reported a history of exposure to at least one, with an average of 3.7 criterion A traumatic events. Exposure to trauma during both childhood and adulthood was common, and those with a current diagnosis of PTSD tended to have higher rates compared to those without a current diagnosis of PTSD (42.5% vs. 30.6%, p=0.06). The most common traumas were serious accident or injury (59.5% of subjects), attack with a weapon by someone other than a domestic partner (39.4%), attack by a significant other without a weapon (36.6%), and witnessing domestic violence as a child (37.3%). Regarding childhood trauma exposure, 43.4% of subjects reported physical abuse, 34.0% reported a history of sexual abuse, and 44.6% reported emotional abuse.
Overall, 18.8% of subjects met DSM-IV diagnostic criteria for a current diagnosis of PTSD with the CAPS. Depression was also prominent in this study population, with 13.2% of subjects meeting diagnostic criteria for a current Major Depressive Disorder (MDD) with the SCID. As expected given the high prevalence of comorbid PTSD and MDD, a current diagnosis of MDD was significantly more common amongst those with a current diagnosis of PTSD (42.9%) versus those without a current diagnosis of PTSD (6.4%, p <0.001).
Due to the previous evidence of an association between antipsychotic medications and metabolic syndrome[50], the rate of antipsychotic use was also examined in this population. However, there was no difference between the rate of prescribed antipsychotic use between those without a current diagnosis of PTSD (8.5%) versus those with PTSD (10.9%; p = 0.62).
The self-reported rate of current substance abuse was low (5.3%), and did not differ based upon presence or absence of PTSD diagnosis (p=0.14). However, far higher rates were endorsed for lifetime smoking (73.7% of the population), a known cardiovascular risk factor. There was no difference in lifetime history of smoking between those with versus those without a current diagnosis of PTSD (p=0.39).
Metabolic Syndrome and Components of Metabolic Syndrome
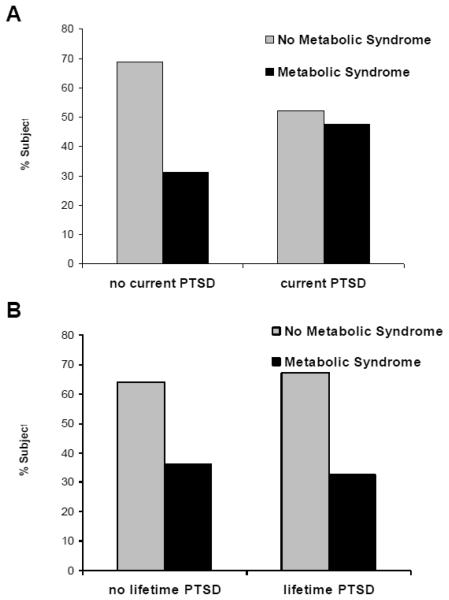
Metabolic syndrome was present at a high rate in this population as a whole, with 33.2% meeting criteria by the ATP III Guidelines. A greater proportion of those with a current diagnosis of PTSD (47.8%) met criteria for metabolic syndrome versus those without current PTSD (31.2%, p < 0.05; Table 2, Figure 1A). Notably, a lifetime diagnosis of PTSD was not found to have any association with presence of metabolic syndrome (p=0.60, Figure 1B).
Table 2.
Metabolic Syndrome and Metabolic Parameters by Current PTSD Status (n=245)
| Measure | No Current PTSD (n = 199) |
Current PTSD (n = 46) |
P value |
|---|---|---|---|
| Metabolic Syndrome (a) | 0.03 | ||
| Metabolic Syndrome Present | 62 (31.2%) | 22 (47.8%) | |
| Metabolic Syndrome Absent | 137 (68.8%) | 24 (52.2%) | |
|
| |||
| Fasting Glucose (mg/dL) (b) | 102.4 (47.0) | 93.9 (19.4) | 0.23 |
|
| |||
| Waist Circumference (cm) (b) | 100.4 (20.0) | 104.0 (16.9) | 0.27 |
|
| |||
| Triglycerides (mg/dL) (b) | 126.4 (130.6) | 116.4 (59.5) | 0.61 |
|
| |||
| HDL Cholesterol (mg/dL) (b) | 48.2 (16.2) | 51.7 (20.5) | 0.22 |
|
| |||
| LDL Cholesterol (mg/dL) (b) | 107.8 (41.1) | 101.2 (26.3) | 0.30 |
|
| |||
| Systolic Blood Pressure (mmHg) | 128.2 (23.2) | 129.8 (24.9) | 0.67 |
|
| |||
| Diastolic Blood Pressure (mmHg) | 76.5 (12.2) | 75.1 (13.2) | 0.49 |
data are presented as number of subjects (percentage)
Values for the individual metabolic parameters are expressed as mean (standard deviation).
Figure 1. Effects of PTSD Status on Prevalence of Metabolic Syndrome.
The percentage of subjects who meet criteria for presence vs. absence of metabolic syndrome are shown. A) Percentage of subjects meeting criteria for Metabolic Syndrome for those without vs. those with current PTSD diagnosis are shown, demonstrating significantly greater metabolic syndrome rates in those with current PTSD (N=245, p<0.05). B) Percentage of subjects meeting criteria for Metabolic Syndrome for those without vs. those with lifetime (but not necessarily current) PTSD diagnosis are shown, demonstrating no difference in metabolic syndrome rates in those with a history of PTSD (N=245, p>0.50).
Interestingly, while a current diagnosis of PTSD was significantly associated with the presence of metabolic syndrome, the association with each individual parameter of metabolic syndrome was not as strong. There were no statistically significant differences in mean waist circumference, fasting glucose, triglyceride or HDL cholesterol concentrations by current PTSD status (Table 2).
Given the significant association between current PTSD and metabolic syndrome, it was of interest to assess the contribution of PTSD to metabolic syndrome while controlling for other demographic, psychiatric, and pharmacologic factors that could moderate this relationship. Therefore, logistic regression modeling was utilized to control for other predictor variables, including age, sex, race, smoking history, antipsychotics, trauma exposure, and a current diagnosis of MDD. In this analysis, only a current diagnosis of PTSD (N=200, Wald χ2= 7.40, p=0.0065) remained a significant predictor of metabolic syndrome (Table 3). Of particular note, the association between current PTSD and metabolic syndrome was not due to use of antipsychotic medication (Wald χ2= 0.79, p=0.38) or comorbid MDD (Wald χ2= 2.70, p=0.10). Finally, we performed an additional regression, including the same predictor variables as above, with the addition of exercise level as a covariate, and current PTSD remained a significant predictor of metabolic syndrome (N=177, Wald χ2= 7.41, p=0.006). Using this logistic regression analyses, a lifetime diagnosis of PTSD was not associated with the presence of metabolic syndrome (p>0.5).
Table 3.
Current PTSD Predicts Metabolic Syndrome After Controlling for Comorbidity (N=200)
| Variable | Wald χ2 | p-value |
|---|---|---|
| Age | 3.59 | 0.058 |
|
| ||
| Sex | 0.087 | 0.77 |
|
| ||
| Race - | ||
| African American | 0.63 | 0.73 |
| Caucasian | 0.62 | 0.43 |
| Other | 0.52 | 0.47 |
|
| ||
| Lifetime Smoking History | 0.087 | 0.77 |
|
| ||
| Current Use of Antipsychotic Medication |
.79 | 0.38 |
|
| ||
| Number of Trauma Types | 0.41 | 0.52 |
|
| ||
| Current MDD | 2.70 | 0.10 |
|
| ||
| Current PTSD | 7.40 | 0.0065 |
Discussion
This study found that a current diagnosis of PTSD was associated with a significantly increased risk for the presence of metabolic syndrome. The rate of metabolic syndrome in this study as a whole (33.2%), and particularly amongst those with current PTSD (47.8%), was much higher than that reported among the general adult population in the National Health and Nutrition Examination Survey (20-31%) [43, 44, 51]. Even after evaluating multiple potentially confounding variables, such as age, sex, race, smoking history, trauma exposure, antipsychotic use, MDD, and exercise this association remained significant. These data suggest that the increased rates of metabolic syndrome and cardiovascular risk factors observed in low income African-Americans [52] may be related to the heightened rates of trauma exposure and subsequent PTSD.
The results are similar to those found in other studies of PTSD and metabolic abnormalities utilizing subjects drawn from populations with high risk for trauma. For example, PTSD related to combat exposure has been associated with elevated lipids [26, 27], diabetes [53], and metabolic syndrome [21, 23, 54, 55]. Additionally, studies of civilian police officers with significant trauma exposure have also identified associations between a diagnosis of PTSD and the presence of lipid abnormalities [25] as well as metabolic syndrome [56]. However, this is the first study that we are aware of in which the role of PTSD has been examined in a civilian population with known health disparities in cardiovascular disease and metabolic syndrome. It is possible that this association may underlie the known correlation between PTSD and adverse cardiovascular events. A prospective study of combat veterans demonstrated that a diagnosis of PTSD predicted subsequent cardiac mortality [18], and multiple cross-sectional studies have reported a correlation between a diagnosis of PTSD and adverse cardiovascular outcomes including higher rates of angina pectoris, diagnosis of coronary artery disease, stroke and myocardial infarctions [57].
Given the frequent use of atypical antipsychotic medications as a pharmacologic augmentation strategy in the treatment of PTSD and/or MDD, and the consistent association between use of these medications and metabolic syndrome, it was plausible that the association between PTSD and metabolic syndrome was mediated by increased use of these medications in subjects with PTSD. However, not only was the rate of antipsychotic use lower within the subjects with a current diagnosis of PTSD versus those without that diagnosis, but also the use of these medications was not associated with metabolic syndrome in this study. Therefore, the use of antipsychotic medications did not mediate the current association between PTSD and metabolic syndrome. Given the relatively small sample that was taking antipsychotic medication, we were not likely powered to demonstrate a true negative finding for this lack of association. Notably, in this study, the rates of antipsychotic use were not significantly different in the PTSD group. We have previously found that PTSD is widely clinically underdiagnosed in this population [16], so that antipsychotic prescription rates may reflect primary psychotic disorders, but are unlikely used frequently for PTSD symptoms. Further, the magnitude of the effect of PTSD diagnosis on predicting the presence of metabolic syndrome was greater than the effect of age, which has been documented to increase the prevalence of each metabolic risk parameter, as well as prevalence of the overall metabolic syndrome [58].
Despite the significant association between current PTSD diagnosis and the presence of metabolic syndrome, PTSD was not associated with each individual metabolic risk parameter. However, the detrimental health impact of metabolic syndrome is significant, with an approximate 2.5 fold increase in the odds of developing cardiovascular disease[58]. The magnitude of this risk highlights the public health impact of PTSD, and demonstrates the need for heightened vigilance for and treatment of metabolic syndrome within this population.
The mechanism by which PTSD mediates the association between trauma exposure and metabolic syndrome in this population is not clear, but may reflect the cumulative detrimental physiological impact of repeated activation of the body's stress response system [58, 59]. In response to stressors, activation of the sympathetic nervous system leads to increased release of catecholamines, which upregulate the production of lipoprotein lipase, ultimately leading to increased concentrations of cholesterol and triglycerides, a key component of metabolic syndrome. Further, stress-induced activation of the hypothalamic-pituitary-adrenal(HPA) axis leads to the release of glucocorticoids, which increase the deposition of abdominal fat, which leads to increased waist circumference and is associated with insulin resistance [60]. The finding that the risk for current PTSD is more strongly associated with a diagnosis of metabolic syndrome than meeting criteria for each individual metabolic risk factor is consistent with previous studies in which a more comprehensive measure is a better predictor of overall health risk than more reductionist approaches that examine biological risks factors as individual parameters [30].
There are a number of potential limitations to this study. First, there is a very high overlap between PTSD and MDD, such that the distinction in a sufficiently traumatized subject may not be important for medical sequellae. Thus, we examined models with and without MDD as a covariate, demonstrating similar results, suggesting that MDD did not account for the relationship between PTSD and metabolic syndrome. It would also be nice to examine the time since index trauma as a potential predictor of metabolic syndrome. Unfortunately, due to the highly traumatized nature of our subjects, with multiple past criterion A traumas, we do not feel that our data would fairly represent this relationship. We recommend that future studies (for example with combat veterans) examine the specific interaction of time since index trauma and metabolic syndrome. Additionally, larger, more well-powered studies may better address whether level of PTSD severity is associated with increased risk of metabolic syndrome.
It is also important to note that correlation does not imply causation. Thus, we cannot be certain that PTSD is causing additional rates of metabolic syndrome as opposed to the other interpretation which is that metabolic syndrome might place people at higher risk for developing PTSD, although we think the preponderance of data would not be consistent with this interpretation. Additionally, both PTSD and metabolic syndrome may both be secondary to a yet undetermined factor, e.g. HPA-axis dysregulation. We should point out that PTSD accounted for 30% of the additional variance in metabolic syndrome in this cohort, and the baseline rate of 48% is still very highly elevated beyond the general population. The additional reasons for this high rate of metabolic syndrome are multifactorial, but may also be due at some level to subsyndromal PTSD and trauma sequelae that were controlled for in these analyses. It is likely that poverty, poor diet selection, lack of exercise and other well-known factors may also be contributing to the high baseline rate of metabolic syndrome.
Interestingly, individuals with a lifetime history of PTSD, but not a current diagnosis of PTSD, did not demonstrate higher rates of metabolic syndrome, suggesting that the metabolic risk associated with PTSD may reflect the acute state of PTSD symptoms. On the other hand, although the diagnostic criteria are identifying ‘current PTSD’, in this population current PTSD is generally of prolonged duration and severity, and is often untreated. It is likely that those with a current diagnosis of PTSD represent individuals with a higher chronic and severe condition than those who meet lifetime, but not current diagnostic criteria. In future studies, it will be important to investigate whether effective treatment of PTSD within this population may reduce the prevalence of metabolic syndrome and ameliorate the adverse cardiovascular outcomes. Overall, these findings point out the importance of screening for PTSD, as well as for metabolic syndrome in this at-risk population, and suggest that active PTSD may play a role in the health disparities seen within traumatized, inner city, minority populations.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hu G, Qiao Q, Tuomilehto J, Balkau B, Borch-Johnsen K, Pyorala K. Prevalence of the metabolic syndrome and its relation to all-cause and cardiovascular mortality in nondiabetic European men and women. Archives of Internal Medicine. 2004;164(10):1066. doi: 10.1001/archinte.164.10.1066. [DOI] [PubMed] [Google Scholar]
- 2.Hunt K, Resendez R, Williams K, Haffner S, Stern M. National Cholesterol Education Program versus World Health Organization metabolic syndrome in relation to all-cause and cardiovascular mortality in the San Antonio Heart Study. Circulation. 2004;110(10):1251. doi: 10.1161/01.CIR.0000140762.04598.F9. [DOI] [PubMed] [Google Scholar]
- 3.Isomaa B, Almgren P, Tuomi T, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes care. 2001;24(4):683. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 4.Lakka H, Laaksonen D, Lakka T, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. Jama. 2002;288(21):2709. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 5.Malik S, Wong N, Franklin S, et al. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation. 2004;110(10):1245. doi: 10.1161/01.CIR.0000140677.20606.0E. [DOI] [PubMed] [Google Scholar]
- 6.Chan P, Nichol G, Krumholz H, et al. Racial Differences in Survival After In-Hospital Cardiac Arrest. Jama. 2009;302(11):1195. doi: 10.1001/jama.2009.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clark L, Ferdinand K, Flack J, et al. Coronary heart disease in African Americans. Heart Disease. 2001;3(2):97–108. doi: 10.1097/00132580-200103000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Cook N, Albert M. Regarding REGARDS: Does Inflammation Explain Racial and Regional Differences in Cardiovascular Disease Risk? Clinical Chemistry. 2009;55(9):1603. doi: 10.1373/clinchem.2009.131185. [DOI] [PubMed] [Google Scholar]
- 9.Duprez D, Jacobs D, Jr, Lutsey P, et al. Race/ethnic and sex differences in large and small artery elasticity--results of the multi-ethnic study of atherosclerosis (MESA) Ethnicity & disease. 2009;19(3):243. [PMC free article] [PubMed] [Google Scholar]
- 10.Mensah G, Mokdad A, Ford E, Greenlund K, Croft J. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 11.Link CL, McKinlay JB. Disparities in the prevalence of diabetes: is it race/ethnicity or socioeconomic status? Results from the Boston Area Community Health (BACH) survey. Ethn Dis. Summer. 2009;19(3):288–292. [PMC free article] [PubMed] [Google Scholar]
- 12.Shonkoff J, Boyce W, McEwen B. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. Jama. 2009;301(21):2252. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 13.Alim T, Graves E, Mellman T, et al. Trauma exposure, posttraumatic stress disorder and depression in an African-American primary care population. Journal of the National Medical Association. 2006;98(10):1630. [PMC free article] [PubMed] [Google Scholar]
- 14.Breslau N, Wilcox H, Storr C, Lucia V, Anthony J. Trauma exposure and posttraumatic stress disorder: A study of youths in urban America. Journal of Urban Health. 2004;81(4):530–544. doi: 10.1093/jurban/jth138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gillespie CF, Bradley B, Mercer K, et al. Trauma exposure and stress-related disorders in inner city primary care patients. Gen Hosp Psychiatry. 2009 Nov-Dec;31(6):505–514. doi: 10.1016/j.genhosppsych.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schwartz A, Bradley R, Sexton M, Sherry A, Ressler K. Posttraumatic stress disorder among African Americans in an inner city mental health clinic. Psychiatric Services. 2005;56(2):212. doi: 10.1176/appi.ps.56.2.212. [DOI] [PubMed] [Google Scholar]
- 17.Boscarino J. Posttraumatic stress disorder and physical illness. Ann. NY Acad. Sci. 2004;1032:141–153. doi: 10.1196/annals.1314.011. [DOI] [PubMed] [Google Scholar]
- 18.Boscarino J. Posttraumatic stress disorder and mortality among US Army veterans 30 years after military service. Annals of epidemiology. 2006;16(4):248–256. doi: 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 19.Krause N, Shaw BA, Cairney J. A descriptive epidemiology of lifetime trauma and the physical health status of older adults. Psychol Aging. 2004 Dec;19(4):637–648. doi: 10.1037/0882-7974.19.4.637. [DOI] [PubMed] [Google Scholar]
- 20.Vieweg WV, Julius DA, Fernandez A, Tassone DM, Narla SN, Pandurangi AK. Posttraumatic stress disorder in male military veterans with comorbid overweight and obesity: psychotropic, antihypertensive, and metabolic medications. Prim Care Companion J Clin Psychiatry. 2006;8(1):25–31. doi: 10.4088/pcc.v08n0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jakovljevic M, Babic D, Crncevic Z, Martinac M, Maslov B, Topic R. Metabolic syndrome and depression in war veterans with post-traumatic stress disorder. Psychiatria Danubina. 2008;20(3):406. [PubMed] [Google Scholar]
- 22.Jakovljevic M, Crncevic Z, Ljubicic D, Babic D, Topic R, Saric M. Mental disorders and metabolic syndrome: a fatamorgana or warning reality? Psychiatria Danubina. 2007;19(1-2):76. [PubMed] [Google Scholar]
- 23.Jakovljevi c M, Šaric M, Nadj S, Topic R, Vuksan- Cusa B. Metabolic syndrome, somatic and psychiatric comorbidity in war veterans with post-traumatic stress disorder: Preliminary findings. Psychiatria Danubina. 2006;18:176. 169. [PubMed] [Google Scholar]
- 24.Jin H, Lanouette N, Mudaliar S, et al. Association of Posttraumatic Stress Disorder With Increased Prevalence of Metabolic Syndrome. Journal of Clinical Psychopharmacology. 2009;29(3):210. doi: 10.1097/JCP.0b013e3181a45ed0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maia D, Marmar C, Mendlowicz M, et al. Abnormal serum lipid profile in Brazilian police officers with post-traumatic stress disorder. Journal of Affective Disorders. 2008;107(1-3):259–263. doi: 10.1016/j.jad.2007.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Solter V, Thaller V, Karlovic D, Crnkovic D. Elevated serum lipids in veterans with combat-related chronic posttraumatic stress disorder. Croatian medical journal. 2002;43(6):685–689. [PubMed] [Google Scholar]
- 27.Kagan B, Leskin G, Haas B, Wilkins J, Foy D. Elevated lipid levels in Vietnam veterans with chronic posttraumatic stress disorder. Biological Psychiatry. 1999;45(3):374–377. doi: 10.1016/s0006-3223(98)00059-6. [DOI] [PubMed] [Google Scholar]
- 28.Schnurr PP, Jankowski MK. Physical health and post-traumatic stress disorder: review and synthesis. Semin Clin Neuropsychiatry. 1999 Oct;4(4):295–304. doi: 10.153/SCNP00400295. [DOI] [PubMed] [Google Scholar]
- 29.Trief PM, Ouimette P, Wade M, Shanahan P, Weinstock RS. Post-traumatic stress disorder and diabetes: comorbidity and outcomes in a male veterans sample. J Behav Med. 2006 Oct;29(5):411–418. doi: 10.1007/s10865-006-9067-2. [DOI] [PubMed] [Google Scholar]
- 30.Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci U S A. 2001 Apr 10;98(8):4770–4775. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Binder EB, Bradley RG, Liu W, et al. Association of FKBP5 polymorphisms and childhood abuse with risk of posttraumatic stress disorder symptoms in adults. JAMA. 2008 Mar 19;299(11):1291–1305. doi: 10.1001/jama.299.11.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cusack K, Frueh B, Brady K. Trauma history screening in a community mental health center. Psychiatric Services. 2004;55(2):157. doi: 10.1176/appi.ps.55.2.157. [DOI] [PubMed] [Google Scholar]
- 33.Norris F, Hamblen J. Standardized self-report measures of civilian trauma and PTSD. Assessing psychological trauma and PTSD/edited by John P. Wilson, Terence M. Keane. 2004:63. [Google Scholar]
- 34.Liebschutz J, Saitz R, Brower V, et al. PTSD in urban primary care: high prevalence and low physician recognition. Journal of general internal medicine. 2007;22(6):719–726. doi: 10.1007/s11606-007-0161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bernstein D, Stein J, Newcomb M, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 36.Bremner J, Vermetten E, Mazure C. Development and preliminary psychometric properties of an instrument for the measurement of childhood trauma: the Early Trauma Inventory. Depression and Anxiety. 2000;12(1):1–12. doi: 10.1002/1520-6394(2000)12:1<1::AID-DA1>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 37.Blake DD, Weathers FW, Nagy LM, et al. The development of a clinician administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 38.Blake DD, Weathers FW, Nagy LM, et al. A clinician rating scale for assessing current lifetime PTSD: the CAPS-1. Behavior Therapy. 1990;13:187–188. [Google Scholar]
- 39.Weathers FW, Keane TM, Davidson JRT. Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- 40.First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview For DSM-IV Axis I Disorders, (Research Version, 2/96 Final) NY Biometrics Research Department, New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- 41.National Cholesterol Education Program (NCEP) Expert Panel on Detection E, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002 Dec 17;106(25):3143–3421. [PubMed] [Google Scholar]
- 42.Cameron AJ, Shaw JE, Zimmet PZ. The metabolic syndrome: prevalence in worldwide populations. Endocrinol Metab Clin North Am. 2004 Jun;33(2):351–375. doi: 10.1016/j.ecl.2004.03.005. table of contents. [DOI] [PubMed] [Google Scholar]
- 43.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002 Jan 16;287(3):356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 44.Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med. 2003 Feb 24;163(4):427–436. doi: 10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Salsberry P, Corwin E, Reagan P. A Complex Web of Risks for Metabolic Syndrome:: Race/Ethnicity, Economics, and Gender. American journal of preventive medicine. 2007;33(2):114–120. doi: 10.1016/j.amepre.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 46.Lehman B, Taylor S, Kiefe C, Seeman T. Relation of childhood socioeconomic status and family environment to adult metabolic functioning in the CARDIA study. Psychosomatic Medicine. 2005;67(6):846. doi: 10.1097/01.psy.0000188443.48405.eb. [DOI] [PubMed] [Google Scholar]
- 47.Appel S, Moore T, Giger J. An overview and update on the metabolic syndrome: implications for identifying cardiometabolic risk among African-American women. J Natl Black Nurses Assoc. 2006;17(2):47–62. [PubMed] [Google Scholar]
- 48.Blevins L, Berry D, Barksdale D. Management of cardiovascular disease inAfrican-American women: utility of the metabolic syndrome guidelines. J Natl Black Nurses Assoc. 2008;19(1):52–62. [PubMed] [Google Scholar]
- 49.Gaillard T, Schuster D, Osei K. Differential impact of serum glucose, triglycerides, and high-density lipoprotein cholesterol on cardiovascular risk factor burden in nondiabetic, obese African American women: implications for the prevalence of metabolic syndrome. Metabolism. 2010 doi: 10.1016/j.metabol.2009.09.035. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 50.Newcomer JW. Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs. 2005;19(Suppl 1):1–93. doi: 10.2165/00023210-200519001-00001. [DOI] [PubMed] [Google Scholar]
- 51.Loucks EB, Magnusson KT, Cook S, Rehkopf DH, Ford ES, Berkman LF. Socioeconomic position and the metabolic syndrome in early, middle, and late life: evidence from NHANES 1999-2002. Ann Epidemiol. 2007 Oct;17(10):782–790. doi: 10.1016/j.annepidem.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 52.Braunschweig C, Gomez S, Liang H, et al. Obesity and risk factors for the metabolic syndrome among low-income, urban, African American schoolchildren: the rule rather than the exception? American Journal of Clinical Nutrition. 2005;81(5):970. doi: 10.1093/ajcn/81.5.970. [DOI] [PubMed] [Google Scholar]
- 53.David D, Woodward C, Esquenazi J, Mellman TA. Comparison of comorbid physical illnesses among veterans with PTSD and veterans with alcohol dependence. Psychiatr Serv. 2004 Jan;55(1):82–85. doi: 10.1176/appi.ps.55.1.82. [DOI] [PubMed] [Google Scholar]
- 54.Babic D, Jakovljevic M, Martinac M, Saric M, Topic R, Maslov B. Metabolic syndrome and combat post-traumatic stress disorder intensity: preliminary findings. Psychiatria Danubina. 2007;19(1/2):68. [PubMed] [Google Scholar]
- 55.Heppner PS, Crawford EF, Haji UA, et al. The association of posttraumatic stress disorder and metabolic syndrome: a study of increased health risk in veterans. BMC Med. 2009;7:1. doi: 10.1186/1741-7015-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Violanti J, Fekedulegn D, Hartley T, et al. Police trauma and cardiovascular disease: association between PTSD symptoms and metabolic syndrome. International journal of emergency mental health. 2006;8(4):227. [PubMed] [Google Scholar]
- 57.Gander ML, von Kanel R. Myocardial infarction and post-traumatic stress disorder: frequency, outcome, and atherosclerotic mechanisms. Eur J Cardiovasc Prev Rehabil. 2006 Apr;13(2):165–172. doi: 10.1097/01.hjr.0000214606.60995.46. [DOI] [PubMed] [Google Scholar]
- 58.Kraja AT, Borecki IB, North K, et al. Longitudinal and age trends of metabolic syndrome and its risk factors: the Family Heart Study. Nutr Metab (Lond) 2006;3:41. doi: 10.1186/1743-7075-3-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Horm Behav. 2003 Jan;43(1):2–15. doi: 10.1016/s0018-506x(02)00024-7. [DOI] [PubMed] [Google Scholar]
- 60.Rosmond R. Role of stress in the pathogenesis of the metabolic syndrome. Psychoneuroendocrinology. 2005 Jan;30(1):1–10. doi: 10.1016/j.psyneuen.2004.05.007. [DOI] [PubMed] [Google Scholar]