Abstract
Root perforation repair has historically been an unpredictable treatment modality, with an unacceptably high rate of clinical failure. Recent developments in the techniques and materials utilized in root perforation repair have dramatically enhanced the prognosis of both surgical and nonsurgical procedures. Mineral Trioxide Aggregate is a relatively new material that is being successfully used to repair perforations. Technological advancements such as the use of a Dental Operating Microscope for correction of these inevitable procedural errors are a major breakthrough in dentistry today. This article presents one clinical case of nonsurgical root perforation repair by Mineral Trioxide Aggregate, using the Dental Operating Microscope.
Keywords: Perforation, mineral trioxide aggregate, microscope
INTRODUCTION
Root perforations are undesired complications of endodontic treatment. Once a perforation has been diagnosed, treatment must be rendered to seal the perforation site effectively to minimize injury and prevent contamination of the surrounding periodontal attachment apparatus. Although successful treatment and prognosis depend on many factors, the location of the perforation and the time lapse between exposure and repair are the two most important factors for determining the treatment and prognosis of the tooth.[1,4] Perforations have been treated mainly through surgical means earlier. However, now, with the introduction and widespread use of the operating microscope, together with the power of ultrasonics, the nonsurgical repair of perforation is more predictable, safe, and easy.[1,2]
This present case illustrates concepts and techniques of using the operating microscope to visualize and repair the perforation nonsurgically.
CASE REPORT
A 35-year-old female patient reported to the Department of Conservative Dentistry and Endodontics, Dr. R. Ahmed Dental College and Hospital, Kolkata, with pain in tooth No 11. She gave a history of root canal treatment (RCT) having been attempted elsewhere on that tooth, about one month prior.
Clinical examination revealed that access preparation had been attempted in the grossly carious maxillary right central incisor. Under rubber dam isolation, the access opening was carefully examined under a Dental Operating Microscope (FS – 1-11; MOELLER – WEDDEL INTERNATIONAL, Germany) (16X Magnification). Distolateral midroot perforation with ledge formation was clearly visualized under the microscope [Figure 1].
Figure 1.
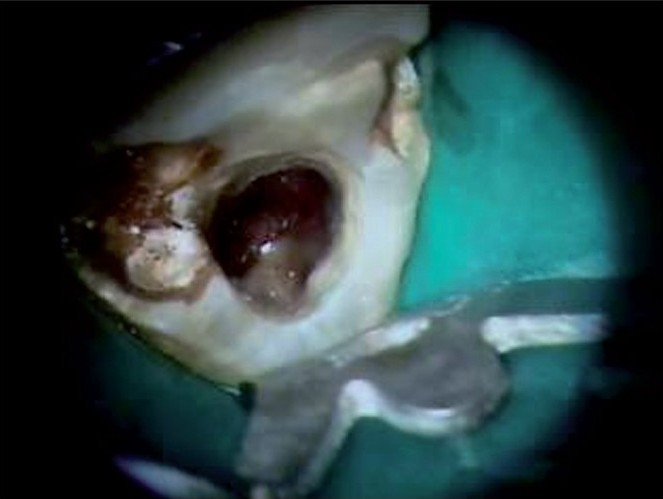
Perforation site in disto-lateral mid-root area of tooth 11 under Microscope in 16X magnification
An intraoral periapical radiograph was taken with a #60 size gutta percha (GP) point placed in the perforation, which aided in further localizing the site of the perforation, and it was confirmed that the defect was subcrestal [Figure 2]. A slight periodontal ligament (PDL) widening was seen.
Figure 2.
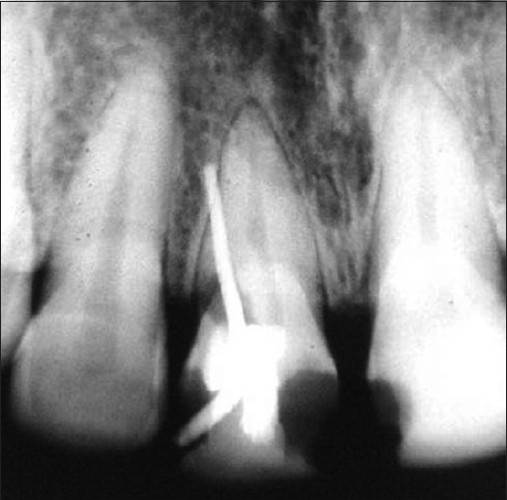
IOPA radiograph of tooth 11 with GP point placed through the perforation
The decision to nonsurgically manage the perforation using Mineral Trioxide Aggregate, under a Dental Operating Microscope, was taken with the patient's consent.
The lateral walls of the perforation were refined and cleaned with light brushing strokes using an Endo 4 ultrasonic tip (Dentsply Tulsa Dental, Tulsa, Oklahoma). Hemostasis was achieved. A #60 size gutta percha point was used to establish the length from the incisal reference point up to the perforation site inside the root canal.[1] Healiguide (ENCOLL, Fremont, CA, USA), an absorbable collagen material was chosen to provide complete hemostasis and a controlled barrier, to pack the restorative material against it. Working length was established and a #40 size GP point was placed in the canal [Figure 3]. Pieces of healiguide were appropriately cut and carried out into the access cavity [Figure 4]. These were progressively placed into the chamber with an appropriate plugger and firmly pressed through the perforation defect. A solid barrier was established [Figure 5]. The access cavity and perforation defect were flushed thoroughly with normal saline and dried. Mineral trioxide aggregate (MTA – ANGELUS; Peterborough, UK) was mixed and carried to the perforation site with the help of a carrier and packed with an appropriately fitted plugger. Repair of the perforation was carried out by progressive placement and packing of small increments of the Mineral Trioxide Aggregate. The gutta percha point was removed and moist cotton pellets were placed over the Mineral Trioxide Aggregate, and closed with noneugenol temporary restoration (Cavit, 3MESPE). The Mineral Trioxide Aggregate was allowed to set for approximately four hours and the patient was recalled after four hours. The canal was opened and it was found that the well-adapted, hard Mineral Trioxide Aggregate had sealed the perforation site and ledge area [Figure 6]. Biomechanical preparation was carried out using the step back method. Apical preparation was performed up to size #60 and obturation was done by lateral condensation of the gutta percha [Figure 7].
Figure 3.

GP point placed in the canal
Figure 4.

Piece of Healiguide resorbable collagen matrix carried out into the access cavity
Figure 5.

Collagen matrix placed corresponding to the cavosurface of the root
Figure 6.

After 48 hours well adapted hard MTA visible under 24X magnification - completely filled the perforation defect
Figure 7.
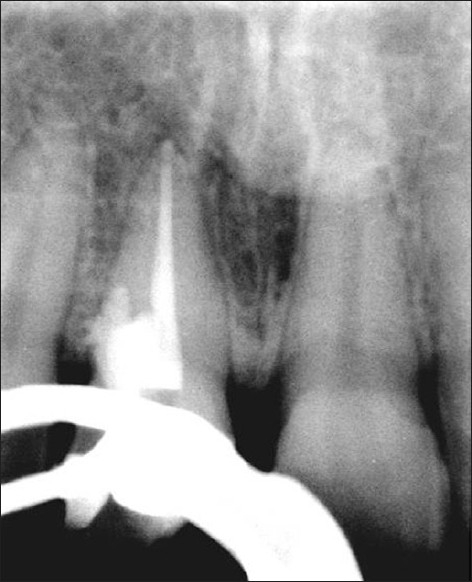
Obturation done in tooth 11
After one month the patient was recalled and was found to be asymptomatic. The glass fiber post was cemented by dual cure resin cement (Calibra - DENTSPLY). The crown was restored by a light cure composite resin [Figure 8]. A one-year recall examination, clinically demonstrated an asymptomatic tooth, with normal attachment and architecture of the soft tissues. A radiographic analysis at this recall evaluation revealed no development of a periapical lesion and no further widening of the PDL [Figure 9]. The patient was advised to put in a crown, but she did not report back, as she had migrated.
Figure 8.

Light Cure Composite build up done in tooth 11
Figure 9.

1 year postoperative radiograph of tooth 11
DISCUSSION
A perforation is defined as the pathological or iatrogenic communication between the root canal space and the periodontal tissue.[7] In the present case, the perforation was present in the distolateral midroot area of the upper right central incisor, which might have been caused during access preparation. To avoid such an occurrence, preparation of the access cavity should be carried out with regard to the anatomy of the tooth, and help of the microscope should be taken, to locate the canal orifice. In the present case the Dental Operating Microscope was used to repair the perforation defect. A midrange magnification (16×) was used because it was the recommended magnification for any surgical purpose.[1,10]
The increased magnification and dual light source of the microscope is invaluable to diagnose and locate accurately the exact perforation site.[2,3] Incremental placement of restorative material like the Mineral Trioxide Aggregate over the perforation site can be carried out successfully and precisely under a microscope.
As the perforation was in the middle third of the root and sufficient access was available through the pulp chamber, the perforation was repaired nonsurgically.[4] The perforation site was cleaned and refined by Endo 4 ultrasonic tip (Dentsply Tulsa Dental, Tulsa, Oklahoma) to ensure an environment free of microbial contamination and necrotic tissue.
The internal matrix concept, in conjunction with the microscope, is an efficient and effective technique for treating accessible perforations nonsurgically.[1] In the present case we placed a sterile, resorbable, and biocompatible collagen material Healiguide into the perforation site, to control hemostasis and prevent overfills, and it acted as an internal matrix.
The Mineral Trioxide Aggregate forms a colloidal gel upon hydration, which solidifies in approximately four hours. Therefore, when used as a root repair material, moisture must be provided from the internal aspect of the root (using a moist cotton pellet).[7] The Mineral Trioxide Aggregate was initially introduced as a root end filling material, however, because of its biocompatibility it is now also considered as a material of choice to seal perforations.[8,9,11,12,14] Although Mineral Trioxide Aggregate is an expensive material, it has become indispensible in procedures such as perforation repair.[13,15]
The location of the perforation is an important factor for its successful repair. More apical the perforation, the better the prognosis.[7] In the present case the perforation was in the midroot, but yet prognosis was favorable even after one year.
CONCLUSION
Training, practice, and technology allow clinicians to expand their abilities greatly in endodontic treatment. Correction of procedural errors can now be performed with a higher degree of clinical confidence by using a Dental Operating Microscope. The use of the microscope and its inherent precision is closing the gap between theoretical possibility and clinical reality.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Microscopes in Endodontics. DCNA. 1997:41–3. [Google Scholar]
- 2.Ingle, Bakland . 6th. Baumgartner: Ingle's Endodontics; [Google Scholar]
- 3.Stephen C, Kenneth M. 9th. Hargreaves: Pathways of the Pulp; [Google Scholar]
- 4.Roda RS. Root perforation repair: Surgical and nonsurgical management. Pract Proced Aesthet Dent. 2001;13:467–72. [PubMed] [Google Scholar]
- 5.Birte Nikolaisen. University of OSLO Dental Faculty. Myrvang: Case Book; 2006. [Google Scholar]
- 6.Ghoddusi J, Sanaan A, Shahrami F. Clinical and radiographic evaluation of root perforation repair using MTA. N Y State Dent J. 2007;73:46–9. [PubMed] [Google Scholar]
- 7.Aziz S, Ali AK, Moeen F. Two successful cases of root perforation repair using mineral trioxide aggregate. Pak Oral Dent J. 2008;28:103–6. [Google Scholar]
- 8.Silveira CM, Sánchez-Ayala A, Lagravère MO, Pilatti GL, Gomes OM. Repair of furcal perforation with mineral trioxide aggregate: long-term follow-up of 2 cases. J Can Dent Assoc. 2008;74:729–33. [PubMed] [Google Scholar]
- 9.Schwartz RS, Mauger M, Clement DJ, Walker WA 3rd. Mineral trioxide aggregate: A new material for endodontics. J Am Dent Assoc. 1999;130:967–75. doi: 10.14219/jada.archive.1999.0337. [DOI] [PubMed] [Google Scholar]
- 10.Castellucci A. Magnification in endodontics: The use of the operating microscope. Pract Proced Aesthet Dent. 2003;15:377–84. [PubMed] [Google Scholar]
- 11.Vajrabhaya LO, Korsuwannawong S, Jantarat J, Korre S. Biocompatibility of furcal perforation repair material using cell culture technique: Ketac Molar versus ProRoot MTA. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:48–50. doi: 10.1016/j.tripleo.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 12.Koulaouzidou EA, Economides N, Beltes P, Geromichalos G, Papazisis K. In vitro evaluation of the cytotoxicity of ProRoot MTA and MTA Angelus. J Oral Sci. 2008;50:397–402. doi: 10.2334/josnusd.50.397. [DOI] [PubMed] [Google Scholar]
- 13.Juárez Broon N, Bramante CM, de Assis GF, Bortoluzzi EA, Bernardineli N, de Moraes IG, et al. Healing of root perforations treated with Mineral Trioxide Aggregate (MTA) and Portland cement. J Appl Oral Sci. 2006;14:305–11. doi: 10.1590/S1678-77572006000500002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moghaddame-Jafari S, Mantellini MG, Botero TM, McDonald NJ, Nör JE. In vitro Effect of ProRoot MTA on pulp cell apoptosis and proliferation. J Endod. 2005;31:389–91. doi: 10.1097/01.don.0000145423.89539.d7. [DOI] [PubMed] [Google Scholar]
- 15.Qatharni HA. In vitro Effect of root perforation repair materials on morphology and attachment behavior of human PDL fibroblasts. Saudt Dent J. 2004;16:113–7. [Google Scholar]


