Abstract
This case report describes a pulpotomy treatment of a permanent mature molar tooth with established irreversible pulpitis and condensing apical periodontitis, using calcium-enriched mixture (CEM) cement. Clinical examination revealed that the first right lower molar had a large carious lesion with history of spontaneous/lingering pain; radiographic examination showed condensing apical periodontitis. Pulpotomy was opted as the treatment; cervical pulpotomy was carried out. Following hemostasis, the radicular pulp stumps were covered with ~2-mm-thick layer of the prepared CEM cement; the tooth was restored with amalgam. Two-year follow-up showed that the treated tooth had been symptomless, and there were no clinical signs/symptoms of either inflammation or infection. Radiographically, the periradicular lesion was completely healed with reconstruction of bone structures to normal appearance; the root canals were not calcified. According to chemical, physical, and biological properties of the CEM cement, this novel biomaterial may be suitable for endodontic treatment.
Keywords: Apical periodontitis, calcium-enriched mixture, calcium-enriched mixture cement, mature, molar, new endodontic cement, pain, pulpitis, pulpotomy
INTRODUCTION
Currently, more attention is being paid by clinicians to preserve tooth pulp vitality.[1] The aim of vital pulp therapy (VPT) is to use biomaterials in order to safeguard as much vitality as possible for the dental pulp with carious exposure. Direct pulp capping and pulpotomy, the two main VPT procedures, are less invasive than pulpectomy/root canal therapy (RCT).
It is well known that the most common cause of pulp/periapical diseases is the presence of bacteria and their by-products within the involved tooth,[2,3] and the most common pathway of their entrance is through carious lesions; when further bacterial recontamination is prevented with a good biological seal, the exposed dental pulp has the capability to heal and construct a new dentinal bridge[4,5] and periapical tissues have the ability of regeneration.[6]
There is a body of evidence for biocompatibility and sealing ability of mineral trioxide aggregate (MTA).[7] Currently, MTA is as an alternative gold standard for calcium hydroxide, a traditional gold standard, in the field of VPT. This biomaterial creates a biological seal via hydroxyapatite crystal formation which is improved the first physical seal.[8,9] Despite the advantages, MTA has nonpredictable antimicrobial activity, delayed setting time, poor handling characteristics, as well as high cost.[10,11]
The calcium-enriched mixture (CEM) cement is a newly introduced endodontic biomaterial with similar clinical applications as MTA, but different chemical compositions.[12,13] This novel cement has an antibacterial effect comparable to calcium hydroxide and superior to MTA[10] and sealing ability similar to MTA.[14] Recent researches revealed that the biologic response of the pulpal and periapical tissues to the MTA and CEM cement were comparable in dogs‘ teeth.[5,6,15] Hydroxyapatite crystal formation was reported over the set CEM even in normal saline solution.[9] Besides the surface characteristics of the set CEM cement, as well as the distribution pattern of calcium, phosphorus, and oxygen ions, is similar to dentine.[13] Last but not least, the clinical use of CEM has been approved by the Iranian Ministry of Health and Medical Education.
Even after carious pulp exposure of symptomatic permanent molars, the pulp can heal, as it has been shown in several studies using MTA[16,17] and CEM cement[18] as pulp-capping biomaterials. This case report discusses a successful treatment outcome of pulpotomy treatment in a symptomatic mature molar with established irreversible pulpitis associate with condensing apical periodontitis.
CASE REPORT
The patient was a 15-year-old boy with noncontributory medical history. He complained of lingering pain to cold. The dental examination revealed normal soft tissue appearance. The first right lower molar had a large carious lesion.
Diagnostic tests were performed; the involved tooth responded with mild pain to percussion and severe lingering pain to the cold thermal test. It was not responded within normal limits to the electric pulp test (EPT). A radiographic examination showed a large carious lesion associated with condensing apical periodontitis [Figure 1a]. The adjacent and opposing teeth were asymptomatic and responded normally to all diagnostic tests.
Figure 1.
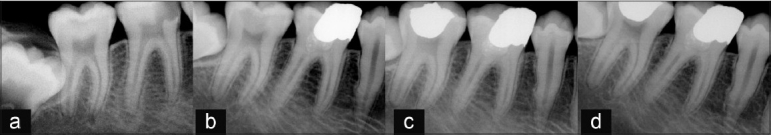
(a) Preoperative radiograph shows a large carious lesion associated with a condensing apical periodontitis. (b–d) Six months, 1 year and 2 years follow-up radiographs, respectively; a complete resolution of condensing apical periodontitis is evident. Note the existence of a dentinal bridge beneath the CEM cement; the remaining pulp canal space does not obliterated
Following clinical and radiographic diagnostic examination, pulpotomy of the first mandibular molar was decided as the treatment. A 0.2% chlorhexidine rinse was carried out. The tooth was anesthetized with 2% lidocaine with 1:80,000 epinephrine (Daroupakhsh, Tehran, Iran), isolated with a rubber damn and then caries was excavated; the exposed coronal pulp tissue was removed with a sterile round diamond bur with water spray. Hemorrhage was controlled with sterile cotton pellets; a ~2 mm layer of the CEM cement (BioniqueDent, Tehran, Iran) was placed without any pressure to cover the exposed pulp stump. The permanent restoration was then completed with amalgam.
The patient was re-examined clinically after 1 and 7 days; tooth mobility was within the normal physiological range, the percussion test was slight positive to negative, and patients were asymptomatic. Six months, one-year, and 2-years follow-ups revealed no clinical or radiographic pathological findings (i.e. inflammation, infection, calcification, and resorption) on the first mandibular molar; radiographs showed normal periodontium apparatus, an evidence of complete periapical healing [Figure 1b–d].
DISCUSSION
The root canal treatment of teeth with irreversible inflamed pulps is basically a prophylactic treatment, since the radicular vital pulp is frequently free of infection and the rationale is to avoid further infection of the root canal system.[19] Improved and more conservative VPT has the potential to reduce the need for more invasive/complicated RCT. However, if this is to be achieved in permanent teeth, there is a need for suitable biomaterials for VPT, particularly pulpotomy. In this report, a case of established irreversible pulpitis associated with condensing apical periodontitis was presented where the CEM cement was used as a pulpotomy biomaterial. Recall examinations revealed that treatment outcomes were successful in preserving pulpal vitality and complete periapical healing of the tooth.
It has been suggested that the existence of a dentinal bridge may at least be an indicator of VPT success, and there are several studies that point to its clinical importance.[20] However, researchers reported the presence of tunnel defects in dentinal bridge under calcium hydroxide in VPT.[5–21,22] They concluded that tunnel defects can serve as pathways for bacterial leakage. Unlike CH, the calcified bridge formed by MTA is continuous and has no evidence of tunnel defects.[5] According to histological evidence from animal/human studies in mature permanent teeth, the CEM cement, like MTA, saves pulp vitality and also induces a hard tissue bridge formation, the both.[5,15,18,23,24] Dentine bridge induced by the CEM cement has been shown to be similar to that induced by MTA in terms of thickness, absence of tunnel defects, presence of adjacent odontoblast-like cells, predentine, and dentinal tubules.[5]
An important finding was the complete healing of the condensing apical periodontitis with reconstruction of bone structures to normal appearance surrounding the involved molar. Endodontic literature supports a direct relationship between pulp inflammations and periapical lesion.[25,26] Mild inflammatory processes may at times cause the formation of condensing apical periodontitis, mostly involving the mandibular first molar.[27] Various studies have suggested that the key factor in success of VPT is the sealing ability of the material;[28] on the other hand, the most important cause of failure is bacterial recontamination.[29] The CEM cement favourably prevents microleakage and has sealing ability comparable to MTA and superior to IRM.[14] In addition, the CEM cement was an effective antibacterial agent.[10] Therefore, when bacterial contamination is removed from the dentin-pulp complex in addition to a creation of tight coronal seal to prevent further bacterial recontamination the inflamed but vital pulp of a permanent molar has a chance to return to a healthy and functional status. All these are resulted in removing the etiologic factor of periapical lesion and complete periapical healing.
Because pulp/periapical healing was achieved without any need for further intervention, it seems that the CEM cement has the required and acceptable properties to be used as a pulp protective biomaterial. The exact biological mechanism by which the CEM cement promotes pulp healing is currently unknown. This characteristic is likely to be the result of several properties such as sealing ability,[14] high alkalinity,[12] antibacterial effect,[10] biocompatibility, i.e. dentinogenesis,[5,15,18,23,24] cementogenesis,[6,30,31] low cytotoxicity,[32,33] pain relief effect,[34] anti-IERR (inflammatory external root resorption) effect,[35] hydroxyapatite formation,[9] and similarity to dentine.[13] Besides, recent interesting studies have established favourable treatment outcomes for the CEM cement when used in pulpotomy of human permanent teeth with irreversible pulpitis.[34,36]
In the future, biomaterials can play an important role in regenerative dentistry; they may completely transform our whole philosophy of endodontic treatment. Endodontics seems to be on the brink of an era when a diseased pulp can be a saved one.[1,36]
There is a realistic biological argument to perform pulpotomy as a promising alternative endodontic treatment in mature permanent teeth; the results of this case clearly show that CEM cement can be used clinically in the treatment of a mature molar associated with irreversible pulpitis and condensing apical periodontitis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Ranly DM, Garcia-Godoy F. Current and potential pulp therapies for primary and young permanent teeth. J Dent. 2000;28:153–61. doi: 10.1016/s0300-5712(99)00065-2. [DOI] [PubMed] [Google Scholar]
- 2.Kakehashi GH, Stanley HR, Fitzgerald RL. The effects of surgical exposure of dental pulps in germ-free and conventional laboratory rats. Oral Surg Oral Med Oral Pathol. 1965;20:340–9. doi: 10.1016/0030-4220(65)90166-0. [DOI] [PubMed] [Google Scholar]
- 3.Torabinejad M, Walton RE. Pulp and Periapical Pathosis. In: Walton R, Torabinejad M, editors. Endodontics: Principles and Practice. Amsterdam: Elsevier Health Sciences; 2008. p. 49. [Google Scholar]
- 4.Asgary S, Parirokh M, Eghbal MJ, Ghoddusi J, Eskandarizadeh A. SEM evaluation of neodentinal bridging after direct pulp protection with mineral trioxide aggregate. Aus Endod J. 2006;32:26–30. doi: 10.1111/j.1747-4477.2006.00004.x. [DOI] [PubMed] [Google Scholar]
- 5.Asgary S, Eghbal MJ, Parirokh M, Ghanavati F, Rahimi H. A comparative study of histologic response to different pulp capping materials and a novel endodontic cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:609–14. doi: 10.1016/j.tripleo.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 6.Asgary S, Eghbal MJ, Ehsani S. Periradicular regeneration after endodontic surgery with calcium-enriched mixture cement in dogs. J Endod. 2010;36:837–41. doi: 10.1016/j.joen.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Torabinejad M, Parirokh M. Mineral trioxide aggregate: A comprehensive literature review Part II: Leakage and biocompatibility investigations. J Endod. 2010;36:190–202. doi: 10.1016/j.joen.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 8.Sarkar NK, Caicedo R, Ritwik P, Moiseyeva R, Kawashima I. Physicochemical basis of the biologic properties of mineral trioxide aggregate. J Endod. 2005;31:97–100. doi: 10.1097/01.don.0000133155.04468.41. [DOI] [PubMed] [Google Scholar]
- 9.Asgary S, Eghbal MJ, Parirokh M, Ghoddusi J. Effect of two storage solutions on surface topography of two root-end fillings. Aust Endod J. 2009;35:147–52. doi: 10.1111/j.1747-4477.2008.00137.x. [DOI] [PubMed] [Google Scholar]
- 10.Asgary S, Kamrani FA. Antibacterial effects of five different root canal sealing materials. J Oral Sci. 2008;50:469–74. doi: 10.2334/josnusd.50.469. [DOI] [PubMed] [Google Scholar]
- 11.Parirokh M, Torabinejad M. Mineral trioxide aggregate: A comprehensive literature review Part III: Clinical applications, drawbacks, and mechanism of action. J Endod. 2010;36:400–13. doi: 10.1016/j.joen.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 12.Asgary S, Shahabi S, Jafarzade T, Amini S, Kheirieh S. The properties of a new endodontic material. J Endod. 2008;34:990–3. doi: 10.1016/j.joen.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 13.Asgary S, Eghbal MJ, Parirokh M, Ghoddusi J, Kheirieh S, Brink F. Comparison of mineral trioxide's composition with Portland cements and a new endodontic cement. J Endod. 2009;35:243–50. doi: 10.1016/j.joen.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 14.Asgary S, Eghbal MJ, Parirokh M. Sealing ability of a novel endodontic cement as a root-end filling material. J Biomed Mater Res A. 2008;87:706–9. doi: 10.1002/jbm.a.31678. [DOI] [PubMed] [Google Scholar]
- 15.Tabarsi B, Parirokh M, Eghbal MJ, Haghdoost AA, Torabzadeh H, Asgary S. A comparative study of dental pulp response to several pulpotomy agents. Int Endod J. 2010;43:565–71. doi: 10.1111/j.1365-2591.2010.01711.x. [DOI] [PubMed] [Google Scholar]
- 16.Eghbal MJ, Asgary S, Ali Baglue R, Parirokh M, Ghoddusi J. MTA pulpotomy of human permanent molars with irreversible pulpitis. Aust Endod J. 2009;35:4–8. doi: 10.1111/j.1747-4477.2009.00166.x. [DOI] [PubMed] [Google Scholar]
- 17.Witherspoon DE, Small JC, Harris GZ. Mineral trioxide aggregate pulpotomies: A case series outcomes assessment. J Am Dent Assoc. 2006;137:610–8. doi: 10.14219/jada.archive.2006.0256. [DOI] [PubMed] [Google Scholar]
- 18.Asgary S, Ehsani S. Permanent molar pulpotomy with a new endodontic cement: A case series. J Conserv Dent. 2009;12:31–6. doi: 10.4103/0972-0707.53340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spangberg LS. Endodontic treatment of teeth without apical periodontitis. In: Orstavik D, Pitt Ford T, editors. Essential Endodontology. Oxford: Blackwell Science Ltd; 1998. pp. 211–41. [Google Scholar]
- 20.Caliskan MK. Clinical reliability of the dentine bridge formed after pulpotomy: A case report. Int Endod J. 1994;27:52–5. doi: 10.1111/j.1365-2591.1994.tb00230.x. [DOI] [PubMed] [Google Scholar]
- 21.Cox C, Bergenholtz G, Heys D, Syed S, Fitzgerald M, Heys R. Pulp capping of dental pulp mechanically exposed to oral microflora: A 1-2-year observation of wound healing in the monkey. J Oral Pathol. 1985;14:156–68. doi: 10.1111/j.1600-0714.1985.tb00479.x. [DOI] [PubMed] [Google Scholar]
- 22.Pitt Ford TR, Roberts GJ. Immediate and delayed direct pulp capping with the use of new visible light-cured calcium hydroxide preparation. Oral Surg Oral Med Oral Pathol. 1991;71:338–42. doi: 10.1016/0030-4220(91)90311-y. [DOI] [PubMed] [Google Scholar]
- 23.Nosrat A, Asgary S. Apexogenesis treatment with a new endodontic cement: A case report. J Endod. 2010;36:912–4. doi: 10.1016/j.joen.2009.11.025. [DOI] [PubMed] [Google Scholar]
- 24.Nosrat A, Asgary S. Apexogenesis of a symptomatic molar with calcium enriched mixture. Int Endod J. 2010;43:940–4. doi: 10.1111/j.1365-2591.2010.01777.x. [DOI] [PubMed] [Google Scholar]
- 25.Yamasaki M, Kumazawa M, Kohsaka T, Nakamura H, Kameyama Y. Pulpal and periapical tissue reactions after experimental pulpal exposure in rats. J Endod. 1994;20:13–7. doi: 10.1016/s0099-2399(06)80020-8. [DOI] [PubMed] [Google Scholar]
- 26.Tani-Ishii N, Wang CT, Tanner A, Stashenko P. Changes in root canal microbiota during the development of rat periapical lesions. Oral Microbiol Immunol. 1994;9:129–35. doi: 10.1111/j.1399-302x.1994.tb00048.x. [DOI] [PubMed] [Google Scholar]
- 27.Marmary Y, Kutiner G. A radiographic survey of periapical jawbone lesions. Oral Surg Oral Med Oral Pathol. 1986;61:405–8. doi: 10.1016/0030-4220(86)90427-5. [DOI] [PubMed] [Google Scholar]
- 28.Tobias RS, plant CG, Browne RM. Reduction in pulpal inflammation beneath surface sealed silicates. Int Endod J. 1982;15:173–80. doi: 10.1111/j.1365-2591.1982.tb01274.x. [DOI] [PubMed] [Google Scholar]
- 29.Massler M. Preserving the exposed pulp. J Pedodont. 1978;2:217–27. [PubMed] [Google Scholar]
- 30.Samiee M, Eghbal MJ, Parirokh M, Abbas FM, Asgary S. Repair of furcal perforation using a new endodontic cement. Clin Oral Investig. 2010;14:653–8. doi: 10.1007/s00784-009-0351-8. [DOI] [PubMed] [Google Scholar]
- 31.Asgary S. Furcal perforation repair using calcium enriched mixture cement. J Conserv Dent. 2010;13:156–8. doi: 10.4103/0972-0707.71650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mozayeni MA, Salem Milani A, Alim Marvasti L, Asgary S. Cytotoxicity of calcium enriched mixture cement compared with mineral trioxide aggregate and intermediate restorative material. Aust Endod J. 2010 Oct 24; doi: 10.1111/j.1747-4477.2010.00269.x. [DOI] [PubMed] [Google Scholar]
- 33.Goddusi J, Tavakol Afshari J, Donyavi Z, Brook A, Disfani R, Esmaeelzade M. Cytotoxic effect of a new endodontic cement and mineral trioxide aggregate on L929 line culture. Iranian Endod J. 2008;3:17–23. [PMC free article] [PubMed] [Google Scholar]
- 34.Asgary S, Eghbal MJ. The effect of pulpotomy using a calcium-enriched mixture cement versus one-visit root canal therapy on postoperative pain relief in irreversible pulpitis: A randomized clinical trial. Odontology. 2010;98:126–33. doi: 10.1007/s10266-010-0127-2. [DOI] [PubMed] [Google Scholar]
- 35.Asgary S, Nosrat A, Seifi A. Management of Inflammatory External Root Resorption by Using Calcium-enriched Mixture Cement: A Case Report. J Endod. 2011;37:411–3. doi: 10.1016/j.joen.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 36.Asgary S, Eghbal MJ. A Clinical Trial of Pulpotomy vs. Root Canal Therapy of Mature Molars. J Dent Res. 2010;89:1080–5. doi: 10.1177/0022034510374057. [DOI] [PubMed] [Google Scholar]


