Abstract
BACKGROUND AND OBJECTIVES
Patients receiving more information about a new prescription are more adherent to their medication regimens and have better treatment outcomes. Yet it is unclear how much information patients retain when they receive a new prescription. This study aims to describe patient recall of information about new medication prescriptions after an outpatient visit.
METHODS
We used a cross-sectional study of 117 adult outpatient visits to six family physicians. Direct observation of physician-patient encounters by medical students was used to document discussion of information about new prescriptions. Patient recall of specific prescription information was assessed by interviewing patients immediately after the visit.
RESULTS
When prescribing a new medication, physicians most frequently discussed the medication purpose (all visits), how often to take the medication (82%), and how much to take (76%). On average, patients recalled 86% (± 23%) of the information provided, and 64% recalled all information discussed during their visit. Of the 42 patients who failed to recall all of the information, 47% forgot how much to take and 42% forgot potential side effects, but only 24% forgot directions about when to take their medication. Complete recall of information about a new prescription was not associated with the amount of information provided, patient education, race, or duration of relationship with their physician.
CONCLUSIONS
Almost two thirds of patients remember all of the basic information they are given when a new medication is prescribed. Providers should work on improving patient education when prescribing new medications and should not be deterred by worries about poor patient recall.
Numerous studies have shown that patient nonadherence to medication regimens adversely affects treatment outcomes.1–5 This problem affects a broad range of medical conditions and can lead to significant adverse consequences, including poorly controlled asthma attacks,1 higher mortality among heart disease patients,4 and inadequately treated major depression.5 These adverse outcomes can lead to preventable hospitalizations,6 nursing home admissions,7 and increased costs,8 and may create major barriers to the health of the nation.9,10
Inadequate patient knowledge may contribute to medication nonadherence.11,12 Patients who receive more information about their medications have higher rates of adherence and better therapeutic outcomes.9,13,14 But both physicians and pharmacists vary widely in the frequency and types of information they provide about medications.15,16 Studies indicate that they often do not discuss important information when prescribing new medications, such as directions for use and potential side effects.16–24 Some physicians say they do not always educate patients because of worries about patient information overload.25
It is unclear how much information patients actually retain from office visits. Food and Drug Administration (FDA) surveys indicated that there is a great disparity between physician and patient reports of prescription information discussed during office visits.26 Studies have used direct observation techniques to assess a less biased report of new medication-related information discussed during office visits.17–22,27 However, none have combined direct observation of the patient encounter with patient recall of the information provided.
The goals of this study were to (1) use direct observation of physician-patient encounters to assess patient recall of key information about new medication prescriptions and (2) examine whether the amount of information given about a new prescription affected patient recall.
Methods
Study Design and Data Collection
Four medical students from Case Western Reserve University collected data for a cross-sectional observational study of the outpatient visits of six family physicians at four community practices located in Cleveland and Boston. Physicians and patients were told that the students would be conducting a research project involving observation of routine patient care but were not told the specific aims of the study.
Data were collected on 117 visits of patients seen by the six study physicians during 6 weeks from June to July 2000. On randomly selected half days of patient care, students observed consecutive encounters for data collection purposes. When an observed encounter involved a new prescription, the medical student completed a data collection card to note discussion about previously specified medication-related information. Each student aimed to complete 30 data collection cards. Immediately after each encounter, students asked the patients for permission to ask a few follow-up questions regarding the visit (100% agreed). Follow-up questions assessed patient recall of the prescription topics discussed, patient demographics, and duration of the physician-patient relationship. At the conclusion of the data collection period, the student shared the study aims with the physicians and debriefed them about the hypotheses. The study was approved by the University Hospitals of Cleveland Institutional Review Board.
Measures
Information presented by the physician concerning the new prescription was recorded on the front of the card. The information collected was based on recommendations and guidelines concerning key information patients should receive when given a new prescription.28–30 These included medication purpose, how often to take the medication, how much of the medication to take, when to take the medication, duration of regimen, and possible medication side-effects. More knowledge about this information may increase patient medication adherence.
Patients were interviewed immediately after their office visit to collect patient demographics and to assess their recall of the prescription information provided. They were asked about their age, race (Caucasian, African American, or other), educational level (high school graduate or less, some college, college graduate, or graduate/professional school), and duration of relationship with physician. Recall was assessed by asking the patient to provide specific pieces of information about their new prescription. Patient recall was only assessed on the pieces of new prescription information presented by the physician during the visit.
Analysis
Descriptive statistics were calculated to describe patient characteristics, physician provision of information about new prescriptions, and patient recall of information. Bivariate statistics were calculated, using chi-square tests to examine the relationship of patient characteristics (ie, patient gender, age, race, education, and duration of relationship with physician) on complete recall of the information provided. Chi-square tests were also used to test the association of the number of pieces of information provided and complete recall of the information. The final analysis utilized a multiple logistic regression to examine the independent association of patient characteristics and the number of pieces of information provided on complete recall of the information provided. All associations were evaluated with a P value of .05.
Results
Data were collected from 117 patients. A majority of patients were female (65%), and most were Caucasian (65%) or African American (27%). Patients represented a range of educational levels, with 29% having a high school degree or less.
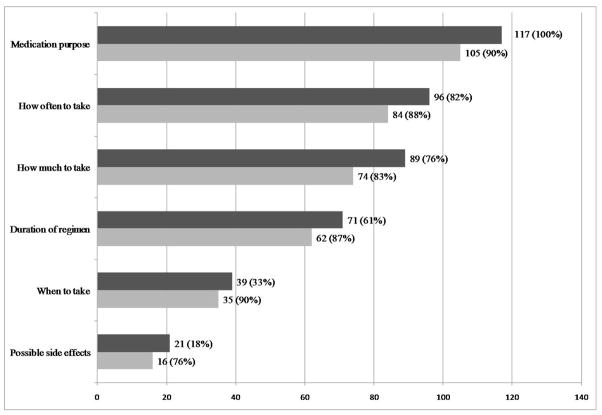
New prescription information discussed during the office visit and patient recall of that information is presented in Figure 1. On average, physicians presented 3.7 (SD=1.2, range 1–6) pieces of information about the new prescription to their patients. Out of 117 discussions of new prescriptions, there were only six in which all six pieces of information were discussed. Physicians presented the medication purpose to every patient observed and frequently provided information about medication directions (eg, how often, how much, and how long to take the new prescription). They discussed other types of information much less frequently; only 33% mentioned when to take the medication, and just 18% talked about possible side effects.
Figure 1. Discussion and Patient Recall of Information About New Prescriptions (n=117).
The top bars correspond to the number of visits in which the information was discussed; the bottom bars correspond to the number of patients recalling the information.
On average, patients recalled 86% (±23%) of the information discussed. Sixty-four percent of patients recalled all of the information provided to them. Patients most frequently remembered conversations about medication purpose, when to take the medication, and how often to take it. Recall ranged from 83%–90% for all pieces of information except for possible medication side effects (76%). Among those that did not recall all of the new medication-related information discussed during the visit, patients most often forgot information about how much medication to take and possible side effects.
Relationship of Patient Characteristics and Information Provision on Patient Recall
The association of patient recall with the patient characteristics was assessed next. As shown in Table 1 (column 4), there were no significant associations between complete patient recall of information and patient age, gender, race, education, or duration of relationship with physician. The amount of information presented was not associated with patient recall. All variables in the table were included in a multivariable model to further examine the relationships and to test for suppressor variables. As shown in the fifth column of Table 1, none of the variables were associated with patient recall.
Table 1.
Association of Patient Characteristics and Recall of New Prescription Information (n=117)*
| n (%) | Complete Recall of Information Provided (%) | Bivariate P Value | Multivariable P Value | |
|---|---|---|---|---|
| Patient Characteristics | ||||
| Age | .68 | .44 | ||
| 19–30 | 34 (29) | 62 | ||
| 31–40 | 26 (23) | 62 | ||
| 41–50 | 23 (20) | 61 | ||
| 51–60 | 15 (13) | 80 | ||
| 61–70 | 9 (8) | 78 | ||
| 71 and over | 8 (7) | 50 | ||
| Female | 75 (65) | 63 | ||
| Race | .26 | .66 | ||
| Caucasian | 76 (65) | 67 | ||
| African American | 32 (27) | 53 | ||
| Other | 9 (8) | 78 | ||
| Education | .18 | .12 | ||
| High school graduate or less | 34 (29) | 62 | ||
| Some college | 38 (32) | 53 | ||
| College graduate | 31 (27) | 74 | ||
| Graduate/professional school | 14 (12) | 79 | ||
| Duration of relationship† | .37 | .64 | ||
| Less than 1 year | 35 (30) | 69 | ||
| 1–3 years | 48 (41) | 50 | ||
| 4–6 years | 16 (14) | 81 | ||
| 7–10 years | 12 (10) | 92 | ||
| 11 or more years | 6 (5) | 50 | ||
| Number of pieces of information discussed | ||||
| 1 | 5 (4) | 80 | .91 | .66 |
| 2 | 12 (10) | 67 | ||
| 3 | 28 (24) | 57 | ||
| 4 | 46 (40) | 67 | ||
| 5 | 20 (17) | 60 | ||
| 6 | 6 (5) | 67 |
Missing data was minimal; age n=2 and sex n=1.
Linear association expected, linear-by-linear association P value reported.
Discussion
This study combines data from direct observation of physician-patient outpatient visits with post-visit patient surveys to demonstrate that most patients have good short-term recall of information about new prescriptions. Almost two thirds of patients remembered all information about the new prescription that was discussed during the visit, and patients recalled 86% of all the information provided. Importantly, there was no association between the amount of information provided and patient recall. This suggests that when initiating a new prescription, physicians should not let worries about information overload deter them from providing all of the key elements of information about a new prescription. These data more accurately portray patient recall than previous studies, which queried whether discussions occurred during the visit or compared patient recall to physician reports or chart reviews.31,32
Of all the information discussed during the visit, patients most frequently failed to recall potential medication side effects. This is particularly interesting because patients routinely say they want their physician to give more information about side effects.33,34 One explanation is that patients may not have recognized that certain discussions were about side effects. For example, a physician may have mentioned the need to follow up if a patient developed hives after taking an antibiotic, but the patient may not have understood that this was a potential medication side effect. Another possibility is that patients may not have focused on the specific side effects discussed because they were planning on getting the information from their pharmacist after the visit. Alternatively, the type of medication prescribed may have influenced patient recall. Those receiving chronic medications may have been more attuned to side effects than those receiving short courses of medication. Future studies should investigate whether the type of medication prescribed influences patient recall of potential side effects and whether it might be more efficient and effective for another health care provider, such as a pharmacist, to review medication side effects.
The findings from this study should be interpreted in light of its limitations. Due to the nature and length of this project, a modest number of patients and physicians were observed, all patients spoke English, 71% had at least some college education, and all physicians were family physicians, thus limiting the generalizability of the findings. Patients in the study were mostly middle aged, and it is unknown whether older patients would have similar recall rates. Further investigation is required to assess whether patient health literacy affects recall of information about new prescriptions and whether patient recall of medication-related information comes at the expense of remembering other information discussed during the visit. Patient information retention may be affected by the content of discussions and by the manner in which information is presented, but these data were not collected in this study. Additional investigations might test patient recall under standardized conditions in which they are presented with uniform comprehensive medication-related counseling.
The Hawthorne effect of having a medical student in the room taking notes when a new medication was prescribed may have inflated rates of physician counseling about medications. Indeed, physicians in this study provided more information about medication purpose and directions for use than seen in other studies based on direct observation.17–21 However, physicians were unaware of the specific aims of the study until data collection was complete, and they may have become attuned to the students’ pattern of data collection after a few visits. It is unknown whether medical student note-taking during the prescribing conversations enhanced or detracted from patient attention to the information discussed.
The results of this study indicate that in general, independent of race and education level, almost two-thirds of patients are able to recall all of the prescription information that is provided to them. In concert with prior studies showing that patients would like more information from their physician or pharmacist,35 these findings should encourage physicians to provide complete information to their patients about new prescriptions. Further studies are needed to assess whether poor recall of medication-related information might be an indicator of suboptimal understanding and to determine how information might be optimally presented so that patients can remember all of the important information discussed. Studies also should investigate how long the recall lasts. In the meantime, health care providers should be reassured that patients have good short-term recall of pertinent information about new prescriptions.
Acknowledgments
Dr Tarn was supported by a UCLA Mentored Clinical Scientist Development Award (5K12AG001004) and by the UCLA Older Americans Independence Center (NIH/NIA Grant P30-AG028748). The manuscript content does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
References
- 1.Mawhinney H, Spector SL, Kinsman RA, et al. Compliance in clinical trials of two non-bronchodilator, antiasthma medications. Ann Allergy. 1991;66:294–9. [PubMed] [Google Scholar]
- 2.Turk DC, Rudy TE. Neglected topics in the treatment of chronic pain patients—relapse, noncompliance, and adherence enhancement. Pain. 1991;44:5–28. doi: 10.1016/0304-3959(91)90142-K. [DOI] [PubMed] [Google Scholar]
- 3.Sumartojo E. When tuberculosis treatment fails. A social behavioral account of patient adherence. Am Rev Respir Dis. 1993;147:1311–20. doi: 10.1164/ajrccm/147.5.1311. [DOI] [PubMed] [Google Scholar]
- 4.Gallagher EJ, Viscoli CM, Horwitz RI. The relationship of treatment adherence to the risk of death after myocardial infarction in women. JAMA. 1993;270:742–4. [PubMed] [Google Scholar]
- 5.Katon W, Von Korff M, Lin E, et al. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. JAMA. 1995;273:1026–31. [PubMed] [Google Scholar]
- 6.McKenney JM, Harrison WL. Drug-related hospital admissions. Am J Hosp Pharm. 1976;33:792–5. [PubMed] [Google Scholar]
- 7.Strandberg L. Drugs as a reason for nursing home admissions. American Health Care Association Journal. 1984;10:20–3. [PubMed] [Google Scholar]
- 8.Stason WB, Weinstein MC, Shepard DS. Obstacles to controlling hypertension. In: Weinstein MC, Stason WB, editors. Hypertension: a policy perspective. Cambridge, MA: Harvard University Press; 1976. pp. 121–39. [Google Scholar]
- 9.Morris LS, Schulz RM. Patient compliance—an overview. J Clin Pharm Ther. 1992;17:283–95. doi: 10.1111/j.1365-2710.1992.tb01306.x. [DOI] [PubMed] [Google Scholar]
- 10.Rogers PG, Bullman WR. Prescription medicine compliance: a review of the baseline knowledge—a report of the National Council on Patient Information and Education. J Pharmacoepidemiology. 1995;3:3–36. [Google Scholar]
- 11.Safran DG, Neuman P, Schoen C, et al. Prescription drug coverage and seniors: findings from a 2003 national survey. Health Aff (Millwood) 2005;(Suppl Web Exclusives):W5-152–W5-66. doi: 10.1377/hlthaff.w5.152. [DOI] [PubMed] [Google Scholar]
- 12.Taylor SA, Galbraith SM, Mills RP. Causes of noncompliance with drug regimens in glaucoma patients: a qualitative study. J Ocul Pharmacol Ther. 2002;18:401–9. doi: 10.1089/10807680260362687. [DOI] [PubMed] [Google Scholar]
- 13.Svarstad BL. Patient-practitioner relationships and compliance with prescribed medical regimens. In: Aiken L, Mechanic D, editors. Applications of social science to clinical medicine and health policy. New Brunswick, NJ: Rutgers University Press; 1986. pp. 438–59. [Google Scholar]
- 14.Hulka BS, Cassel JC, Kupper LL, Burdette JA. Communication, compliance, and concordance between physicians and patients with prescribed medications. Am J Public Health. 1976;66:847–53. doi: 10.2105/ajph.66.9.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Svarstad BL. Physician-patient communication and patient conformity with medical advice. In: Mechanic D, editor. The growth of bureaucratic medicine An inquiry into the dynamics of patient behavior and the organization of medical care. New York: John Wiley and Sons; 1976. pp. 220–38. [Google Scholar]
- 16.Morris LA, Tabak ER, Gondek K. Counseling patients about prescribed medication: 12-year trends. Med Care. 1997;35:996–1007. doi: 10.1097/00005650-199710000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Tarn DM, Heritage J, Paterniti DA, Hays RD, Kravitz RL, Wenger NS. Physician communication when prescribing new medications. Arch Intern Med. 2006;166:1855–62. doi: 10.1001/archinte.166.17.1855. [DOI] [PubMed] [Google Scholar]
- 18.Richard C, Lussier MT. Nature and frequency of exchanges on medications during primary care encounters. Patient Educ Couns. 2006;64:207–16. doi: 10.1016/j.pec.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Cockburn J, Reid AL, Sanson-Fisher RW. The process and content of general-practice consultations that involve prescription of antibiotic agents. Med J Aust. 1987;147:321–4. [PubMed] [Google Scholar]
- 20.Svarstad BL. Sociology: PhD Dissertation. University of Wisconsin; 1974. The doctor-patient encounter: an observational study of communication and outcome; pp. 1–338. [Google Scholar]
- 21.Scherwitz L, Hennrikus D, Yusim S, Lester J, Vallbona C. Physician communication to patients regarding medications. Patient Educ Couns. 1985;7:121–36. doi: 10.1016/0738-3991(85)90003-5. [DOI] [PubMed] [Google Scholar]
- 22.Makoul G, Arntson P, Schofield T. Health promotion in primary care: physician-patient communication and decision making about prescription medications. Soc Sci Med. 1995;41:1241–54. doi: 10.1016/0277-9536(95)00061-b. [DOI] [PubMed] [Google Scholar]
- 23.Svarstad BL, Bultman DC, Mount JK. Patient counseling provided in community pharmacies: effects of state regulation, pharmacist age, and busyness. J Am Pharm Assoc. 2004;44:22–9. doi: 10.1331/154434504322713192. [DOI] [PubMed] [Google Scholar]
- 24.Flynn EA, Barker KN, Berger BA, Lloyd KB, Brackett PD. Dispensing errors and counseling quality in 100 pharmacies. J Am Pharm Assoc. 2009;49:171–80. doi: 10.1331/JAPhA.2009.08130. [DOI] [PubMed] [Google Scholar]
- 25.McGrath JM. Physicians’ perspectives on communicating prescription drug information. Qual Health Res. 1999;9:731–45. doi: 10.1177/104973299129122243. [DOI] [PubMed] [Google Scholar]
- 26.Nightingale SL. Do physicians tell patients enough about prescription drugs? Do patients think so? Postgrad Med. 1983;74:169–75. doi: 10.1080/00325481.1983.11698387. [DOI] [PubMed] [Google Scholar]
- 27.Sleath B, Roter D, Chewning B, Svarstad B. Asking questions about medication: analysis of physician-patient interactions and physician perceptions. Med Care. 1999;37:1169–73. doi: 10.1097/00005650-199911000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Shrank WH, Polinski JM, Avorn J. Quality indicators for medication use in vulnerable elders. J Am Geriatr Soc. 2007;55 (Suppl 2):S373–S382. doi: 10.1111/j.1532-5415.2007.01345.x. [DOI] [PubMed] [Google Scholar]
- 29.Knight EL, Avorn J. Quality indicators for appropriate medication use in vulnerable elders. Ann Intern Med. 2001;135:703–10. doi: 10.7326/0003-4819-135-8_part_2-200110161-00009. [DOI] [PubMed] [Google Scholar]
- 30.Patient fact sheet. AHRQ Publication No. 00-PO38. Rockville, MD: Agency for Healthcare Research and Quality; Feb, 2000. [Accessed February 9, 2010]. 20 tips to help prevent medical errors. ww.ahrq.gov/consumer/20tips.htm. [Google Scholar]
- 31.Jaye C, Hope J, Martin IR. What do general practice patients know about their prescription medications? N Z Med J. 2002;115:U183. [PubMed] [Google Scholar]
- 32.Calkins DR, Davis RB, Reiley P, et al. Patient-physician communication at hospital discharge and patients’ understanding of the postdischarge treatment plan. Arch Intern Med. 1997;157:1026–30. [PubMed] [Google Scholar]
- 33.Berry DC, Michas IC, Gillie T, Forster M. What do patients want to know about their medicines, and what do doctors want to tell them? A comparative study. Psychology and Health. 1997;12:467–80. [Google Scholar]
- 34.Tarn DM, Paterniti DA, Williams BR, Cipri CS, Wenger NS. Which providers should communicate which critical information about a new medication? Patient, pharmacist, and physician perspectives. J Am Geriatr Soc. 2009;57:462–9. doi: 10.1111/j.1532-5415.2008.02133.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gardner ME, Rulien N, McGhan WF, Mead RA. A study of patients’ perceived importance of medication information provided by physicians in a health maintenance organization. Drug Intell Clin Pharm. 1988;22:596–8. doi: 10.1177/106002808802200718. [DOI] [PubMed] [Google Scholar]