Abstract
Transpedicular screw fixation has been accepted worldwide since Harrington et al. first placed pedicle screws through the isthmus. In vivo and in vitro studies indicated that pedicle screw insertion accuracy could be significantly improved with image-assisted systems compared with conventional approaches. The O-arm is a new generation intraoperative imaging system designed without compromise to address the needs of a modern OR like no other system currently available. The aim of our study was to check the accuracy of O-arm based and S7-navigated pedicle screw implants in comparison to free-hand technique described by Roy-Camille at the lumbar and sacral spine using CT scans. The material of this study was divided into two groups, free-hand group (group I) (30 patients; 152 screws) and O-arm group (37 patients; 187 screws). The patients were operated upon from January to September 2009. Screw implantation was performed during PLIF or TLIF mainly for spondylolisthesis, osteochondritis and post-laminectomy syndrome. The accuracy rate in our work was 94.1% in the free-hand group compared to 99% in the O-arm navigated group. Thus it was concluded that free-hand technique will only be safe and accurate when it is in the hands of an experienced surgeon and the accuracy of screw placement with O-arm can reach 100%.
Keywords: Pedicle screws, Image-guided surgery, Spine navigation, O-arm
Introduction
Transpedicular screw fixation has been accepted worldwide since Harrington et al. [5] first placed pedicle screws through the isthmus. Studies have reported that transpedicular screw fixation has gained an advantage over other forms of spinal instrumentation [6, 20]. Safety concerns on the violation of the spinal canal leading to potential harm to neurovascular structures have been encouraging surgeons to improve the accuracy of pedicle screw placement by trying various approaches [1, 11, 12]. Through many conventional methods, usually relying on anatomical landmarks, pedicle screws were inserted with or without fluoroscopy to localise the pedicle. However, studies have reported high rates of cortical perforation [13, 19].
In vivo and in vitro studies indicated that pedicle screw insertion accuracy could be significantly improved with image-assisted systems compared with conventional approaches [14]. Among them, computed tomography-based navigation was the most popular. CT navigation could provide precise anatomy of the pedicle as well as reduced radiation exposure. However, new concerns about system arose with a steep learning curve and excessive preoperative preparation including computed tomography with a specific protocol, data acquisition and transfer, and patient registration [3, 4]. The development of intraoperative two-dimensional and three-dimensional fluoroscopy-based navigation appeared to tackle such issues [15, 22]. The equipment did not require registration; it reduced imaging time and radiation dosage, and avoided repeated C-arm movements during surgery, because visualization of the surgical instruments in relation to the patient’s anatomy in the entire desired image plane was determined from the beginning. Though a few studies implied that the accuracy of fluoroscopy-assisted pedicle screw insertion was comparable with that of CT navigation [3, 4], different population characteristics and assessment methods of placement accuracy in various studies resulted in inconsistent conclusions.
The O-arm is a mobile 2D and 3D imaging platform designed to improve intraoperative decision making. It allows supporting a multitude of applications in spine, orthopaedics, neurosurgery ENT, maxillofacial and vascular surgery in the close future.
The telescoping gantry section of the O-arm enables lateral patient access and as this gantry system is enclosed, the operative field remains sterile and safe. The iso-centric positioning eliminates need to reposition the gantry for off-axis imaging. The O-arm has high precision robotics for real-time and preset positioning, as well as self propulsion. The parking and imaging positions can be preset, resulting in lower dose of radiation and faster imaging. The multiplane imaging eliminates manual repositioning and need for a second system.
The O-arm interfaces seamlessly with the Medtronic Navigation System eliminating time consuming registration steps and transferring acquired scans automatically which greatly enhances navigation workflow providing the surgeon with unprecedented visualization depth and capabilities for complex orthopaedic and spine surgeries. Surgeons are not dependent on a preoperative CT where the patient position may vary from surgical position in the OR. The O-arm allows the surgeon to scan the patient in the operative position and to obtain an updated scan whenever needed. This ensures the most accurate imaging and navigation possible ensuring the best possible surgical outcome for the patient.
The aim of our study is to check the accuracy of O-arm based and S7-navigated pedicle screw implants in comparison to free-hand technique described by Roy-Camille at the lumbar and sacral spine using CT scans.
Materials and methods
One hundred and fifty-two pedicle screws were implanted in 30 patients (15 males and 15 females) using the free-hand technique (group I) and 187 screws were implanted in 37 patients (21 males and 16 females) using the O-arm navigated technique (group II). The mean age was 60.1 years in group I and 64.41 years in group II. Both groups were operated upon in our spine centre in the period between January and September 2009. This was performed during PLIF or TLIF mainly for spondylolisthesis, osteochondritis and post-laminectomy syndrome. Distribution of screws with regard to the lumbo-sacral vertebrae in both groups is shown in Table 1. All surgeries were done by two senior surgeons (Silbermann and Allam).
Table 1.
Distribution of screws with regard to the lumbo-sacral vertebrae in both groups
| Level | Free-hand group | O-arm group |
|---|---|---|
| S1 | 22 | 28 |
| L5 | 42 | 67 |
| L4 | 35 | 54 |
| L3 | 30 | 28 |
| L2 | 14 | 8 |
| L1 | 9 | 2 |
| Total | 152 | 187 |
In the free-hand group (group I), the screws were implanted according to the technique of Roy-Camille [16–18]: identification of the entry point, opening with the awl then drilling of the pedicle and probing of the drill canal. After tapping and screw placement, the position of screws was assessed by C-arm (AP and lateral). When the position of one or more of the screws was not optimal, the screw will be revised and the new position will be checked again by the C-arm. All the patients were subjected to postoperative CT scan to evaluate the position of the screws. The CT examination was carried out using the Briliance CT 64-channel scanner (Philips medical systems, PC Best, Netherlands).
In the O-arm group (group II), after the reference clamp was screwed to one of the spinous processes in the area of fixation, 2D (AP and lateral) as well as 3D fluoroscopy were done. This was followed by screws placement using the O-arm navigation system. After insertion of all screws, control 2D (AP and lateral) as well as 3D fluoroscopies were done to evaluate screw position. When the position of all screws was optimal, the 3D scans were transferred to the hospital own PACS system to evaluate the position of every single screw.
The CT scans (axial and sagittal) of both groups were examined independently by a surgeon and a radiologist to evaluate the position of screws according to the classification of Learch [10] and Wiesner [23]. In this classification, there are four main categories for screw misplacement:
Encroachment If the pedicle cortex could not be visualised.
Minor penetration When the screw trajectory was <3 mm outside the pedicular boundaries.
Moderate penetration When the screw trajectory was 3–6 mm outside the pedicular boundaries.
Severe penetration When the screw trajectory was >6 mm outside the pedicular boundaries.
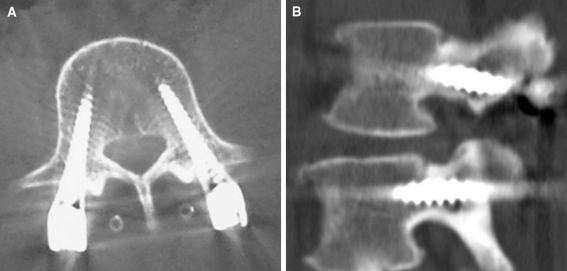
It is worthy to mention that the ideal position of the screw is achieved when the screw lies in the middle of the pedicle in both axial and sagittal reconstruction CT scans (Fig. 1)
Fig. 1.
Ideal position of the screw (a) axial (b) sagittal CT images
Results
Overall inter-observer agreement in the free-hand group was 93.6% compared to 96.3% in the O-arm group including both axial and sagittal reconstruction images.
In the axial images (Table 2), 34 (22.4%) screws showed medial (Fig. 2) and 14 (9.2%) screws showed lateral encroachment in Group I in comparison to 2 (1.1%) and 7 (3.7%) screws, respectively in group II (Fig. 3). The difference was proved to be statistically significant (p < 005). Frank penetration <3 mm was found in 8 (5.2%) screws in group I, in comparison to group II which showed no frank penetration <3 mm either medial or lateral. One screw (0.7%) in group I showed medial frank penetration 3–6 mm but with no symptoms, that is why there was no need to revise it.
Table 2.
Comparison between the two groups regarding screw malplacement
| Screw malplacement | Free-hand group (n = 152) | O-arm group (n = 187) | p | ||
|---|---|---|---|---|---|
| No. | Percent | No. | Percent | ||
| Lateral axial | |||||
| Encroachment | 14 | 9.2 | 7 | 3.7 | 9.56 |
| FP < 3 mm | 4 | 2.6 | 0 | 0.0 | 0.008* |
| Medial axial | |||||
| Encroachment | 34 | 22.4 | 2 | 1.1 | |
| FP < 3 mm | 4 | 2.6 | 0 | 0.0 | 22.65 |
| FP 3–6 mm | 1 | 0.7 | 0 | 0.0 | 0.0001* |
| Anterior axial | |||||
| Encroachment | 10 | 6.6 | 10 | 5.3 | |
| FP < 3 mm | 4 | 2.6 | 0 | 0.0 | |
| FP 3–6 mm | 1 | 0.7 | 1 | 0.5 | 0.65 |
| FP > 6 mm | 1 | 0.7 | 1 | 0.5 | 0.31 |
| Caudal sagittal | |||||
| Encroachment | 23 | 15.1 | 12 | 6.4 | |
| FP < 3 mm | 4 | 2.6 | 0 | 0.0 | |
| FP 3–6 mm | 2 | 1.3 | 0 | 0.0 | 1.32 |
| FP > 6 mm | 0 | 0.0 | 0 | 0.0 | 0.108 |
| Cranial sagittal | 0.99 | ||||
| Encroachment | 10 | 6.6 | 11 | 5.9 | 0.388 |
* Statistical significance
Fig. 2.
Axial CT image showing medial encroachment in the free-hand group
Fig. 3.
Axial O-arm image showing lateral encroachment in the O-arm group
Regarding anterior encroachment and penetration in axial images, in each group 10 screws showed encroachment which was intended to get better screw purchase (S1). Frank penetration was found in 6 (4%) screws in group I in comparison to 2 (1%) screws in group II. One screw (0.7%) in group I showed frank penetration in S1 >6 mm (Fig. 4) and was accompanied by L5 radiculopathy (pain and hypoesthesia). The screw was revised the second day after surgery with no residual neurological deficits.
Fig. 4.
Axial CT image showing anterior frank penetration of the left S1 screw in the free-hand group
In the sagittal images (Table 2), 23 (15.1%) screws showed caudal and 10 screws (6.6%) showed cranial encroachment in Group I in comparison to 12 (6.4%) and 11 (5.9%) screws, respectively in group II (Fig. 5). The difference was proved to be statistically insignificant. Frank penetration was found in 6 (4%) screws in group I in comparison to group II which showed no frank penetration either caudal or cranial.
Fig. 5.
O-arm sagittal reconstruction image showing caudal encroachment of the left L4 screw in the O-arm group
In group I, 4 (2.6%) screws were revised intraoperatively after making the C-arm control. After screw revision, the C-arm control showed good position of the screws. Of these 4 screws, 3 (2%) screws were lateral in L5 and one screw (0.7%) was encroaching on the upper end plate of L2. These patients did not suffer from any neurological deficits postoperatively.
In our study, encroachment and frank penetration <3 mm in axial and sagittal images were considered to be still in the safe zone for implanting the pedicular screws because they do not endanger the efficacy of spine stabilization as well as the neurovascular structures. Accordingly, the screw penetration more than 3 mm in any direction was considered as a screw malposition.
The accuracy rate in our work was 94.1% in the free-hand group compared to 99% in the O-arm navigated group. No residual neurological deficits were reported in both groups (Table 3).
Table 3.
Comparison between the two groups regarding accuracy of screw positioning
| Malplacement | Free-hand technique (152 screws) | O-arm (187 screws) |
|---|---|---|
| Encroachment | 91 | 42 |
| Minor penetration (<3 mm) | 16 | 0 |
| Moderate penetration (3–6 mm) | 4 | 1 |
| Severe penetration (>6 mm) | 1 | 1 |
| Intraoperative screw revision | 4 | 0 |
| Accuracy | 94.1% | 99% |
Discussion
Insertion of pedicle screws is a demanding technique and carries the potential risks of neurological structures injury. The accuracy of placing pedicle screws using the classical open techniques has been the subject of several imaging studies.
Our accuracy rate in the free-hand technique was 94.1% which is better than the rates reported for screw misplacement that range from 10 [18] to 40% [2]. We did not report a single case of severe medial penetration (>6 mm) in comparison to Castro et al. [2] who reported 5.7% in a series of 123 lumbar pedicle screws. In this series, the incidence of neurological deficit attributed to screw malposition was 16.6% (5 out of 30 patients) in comparison to 3.3% (one out of 30 patients) in our study.
In comparison to the free-hand technique, the O-arm based navigation technique showed an accuracy of 99%. Only two out of 187 screws showed anterior penetration more than 3 mm. This was not accompanied by any neurological or vascular injury and both screws were screwed backward after making the intraoperative control 3D scan. Although we have a long experience with the free-hand technique and our accuracy rate approaches the results of 2D fluoroscopy-based navigation technique, the O-arm based navigation technique showed a high better accuracy rate.
The O-arm based navigation technique showed also a higher accuracy rate compared to the CT and 2D fluoroscopy-based navigation techniques and a comparable accuracy rate to the 3D fluoroscopy-based navigation technique. In a meta-analysis of image-guided pedicle screw insertion accuracy in lumbar spine including 7,533 pedicle screws [21], the 2D fluoroscopy-based navigation showed a median accuracy of 86.96% (maximum 90.74% and minimum 72.73%) while the CT-based navigation showed a median accuracy of 90.32% (maximum 95.68% and minimum 72.03%). The 3D fluoroscopy-based navigation had a median accuracy of 97.16% (maximum 99.29% and minimum 80.85%) which is comparable to our results. However, the O-arm is an interesting alternative as it interfaces seamlessly with the Medtronic Navigation System eliminating time consuming registration steps and transferring acquired scans automatically which greatly enhances navigation workflow providing the surgeon with unprecedented visualization depth and capabilities for complex spine surgeries. Surgeons are not dependent on a preoperative CT where the patient position may vary from surgical position in the OR. The O-arm allows the surgeon to scan the patient in the operative position and to obtain an updated scan whenever needed. This ensures the most accurate imaging and navigation possible ensuring the best possible surgical outcome for the patient. On the other hand, the robotic control of the O-arm and the presetting of imaging and parking positions save time and lower the dose of radiation.
To our knowledge, this is the first in the literature that compares the accuracy of screw placement between free-hand and O-arm navigated technique. There is no question that the O-arm navigation-based technique has the best accuracy of pedicle screw placement. On the other hand, it is known that the CT navigation-based techniques prolong the operative time [7–9] as well as the hazards of radiation compared to the C-arm control after the free-hand technique.
We have calculated the time from putting the patient in the prone position till the skin incision (Fig. 6) and there was a statistical difference between the two groups (34.5 min in the free-hand group and 53 min in the O-arm group). In the O-arm group more time was required to adjust the O-arm to the patient, presetting the imaging and parking position, together with draping of the O-arm. We have also calculated the operative time for a single-level PLIF in the two groups (Fig. 7). The mean operative time in the free-hand technique was 183 min in comparison to 193 min in the O-arm group and this was not statistically significant. It is clear that the operative time is more prolonged in the O-arm group but when the team is familiar with the computer system and instruments, the screw navigation time can be reduced and be insignificant when compared to screw placement by the free-hand technique.
Fig. 6.
Comparison between free-hand and O-arm techniques regarding the presurgical patient positioning
Fig. 7.
Comparison between free-hand and O-arm techniques regarding the operative time
Regarding the radiation hazards, each O-arm 3D scan is equal to 60% of an ordinary CT scan according to the radiation measurement carried by the manufactured company (Medtronic, USA). For the operative team, the exposure in nearly zero because the whole surgical team leaves the theatre during the 3D scan.
We think that implanting the screws using the free-hand technique in the lumbar spine is accurate and safe but O-arm based navigation is more accurate and accordingly safer. Further studies are needed to evaluate the efficacy of O-arm based navigation technique in implanting the pedicle screws in the thoracic as well as the cervical spine.
Conclusions
Pedicle screw placement with the free-hand technique is accurate, reliable and safe. Free-hand technique will only be safe and accurate when it is in the hands of an experienced surgeon. The accuracy of screw placement with O-arm can reach 100%. The learning curve of O-arm is high when compared to the free-hand technique which has a steep learning curve and needs a lot of training to get a high accuracy rate.
Conflict of interest
None.
References
- 1.Amiot LP, Lang K, Putzier M, Zippel H, Labelle H. Comparative results between conventional and computer assisted pedicle screw installation in the thoracic, lumbar, and sacral spine. Spine. 2000;25:606–614. doi: 10.1097/00007632-200003010-00012. [DOI] [PubMed] [Google Scholar]
- 2.Castro WH, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S. Accuracy of pedicle screw placement in lumbar vertebrae. Spine. 1996;21:1320–1324. doi: 10.1097/00007632-199606010-00008. [DOI] [PubMed] [Google Scholar]
- 3.Choi WW, Green BA, Levi AD. Computer assisted fluoroscopic targeting system for pedicle screw insertion. Neurosurgery. 2000;47:872–878. doi: 10.1097/00006123-200010000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Fu TS, Wong CB, Tsai TT, Liang YC, Chen LH, Chen WJ. Pedicle screw insertion: computed tomography versus fluoroscopic image guidance. Int Orthop. 2008;32:517–521. doi: 10.1007/s00264-007-0358-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harrington PR, Tullos HS. Reduction of severe spondylolisthesis in children. South Med J. 1969;62:1–7. doi: 10.1097/00007611-196901000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Karatoprak O, Unay K, Tezer M, Ozturk C, Aydogan M, Mirzanli C. Comparative analysis of pedicle screw versus hybrid instrumentation in adolescent idiopathic scoliosis surgery. Int Orthop. 2008;32:523–528. doi: 10.1007/s00264-007-0359-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D. Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J. 2000;9:235–240. doi: 10.1007/s005860000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laine T, Makitalo K, Schlenzka D, Tallroth K, Poussa M, Alho A. Accuracy of pedicle screw insertion: a prospective CT study in 30 low back patients. Eur Spine J. 1997;6:402–405. doi: 10.1007/BF01834068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laine T, Schlenzka D, Makitalo K, Tallroth K, Nolte LP, Visarius H. Improved accuracy of pedicle screw insertion with computer assisted surgery. A prospective clinical trial of 30 patients. Spine. 1997;22:1254–1258. doi: 10.1097/00007632-199706010-00018. [DOI] [PubMed] [Google Scholar]
- 10.Learch TJ, Massie JB, Pathria MN, Ahlgren BA, Garfin SR. Assessment of pedicle screw placement utilizing conventional radiography and computed tomography: a proposed systematic approach to improve accuracy of interpretation. Spine. 2004;29:767–773. doi: 10.1097/01.BRS.0000112071.69448.A1. [DOI] [PubMed] [Google Scholar]
- 11.Lee TC, Yang LC, Liliang PC, Su TM, Rau CS, Chen HJ. Single versus separate registration for computer assisted lumbar pedicle screw placement. Spine. 2004;29:1585–1589. doi: 10.1097/01.BRS.0000131438.68071.6C. [DOI] [PubMed] [Google Scholar]
- 12.Lim MR, Girardi FP, Zoon SC, Huang RC, Cammisa FP. Accuracy of computerized frameless stereotactic image-guided pedicle screw placement into previously fused lumbar spines. Spine. 2005;30:1793–1898. doi: 10.1097/01.brs.0000171905.38459.b7. [DOI] [PubMed] [Google Scholar]
- 13.Merloz P, Tonetti J, Pittel L, Coulomb M, Lavallee S, Sautot P. Pedicle screw placement using image guided techniques. Clin Orthop Relat Res. 1998;354:39–48. doi: 10.1097/00003086-199809000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Merloz P, Troccaz J, Vouillat H, Vasile C, Tonetti J, Eid A, Plaweski S. Fluoroscopy based navigation system in spine surgery. Proc Inst Mech Eng [H] 2007;221(7):813–820. doi: 10.1243/09544119JEIM268. [DOI] [PubMed] [Google Scholar]
- 15.Nottmeier EW, Seemer W, Young PM. Placement of thoracolumbar pedicle screws using three-dimensional image guidance: experience in a large patient cohort. J Neurosurg Spine. 2009;10:33–39. doi: 10.3171/2008.10.SPI08383. [DOI] [PubMed] [Google Scholar]
- 16.Roy-Camille R. Osteosynthesis du rachis dorsal, lombaire et lombo-sacre par plaques metalliques vissees dans les pedicules vertebraux et les apophyses articulaires. Presse Med. 1970;578:1447. [PubMed] [Google Scholar]
- 17.Roy-Camille R, Saillant G, Berteaux D, Salgado V. Osteosynthesis of thoraco-lumbar spine fractures with metal plates screwed through the vertebral pedicles. Reconstr Surg Traumatol. 1976;15:2–16. [PubMed] [Google Scholar]
- 18.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986;203:7–17. [PubMed] [Google Scholar]
- 19.Sakai Y, Matsuyama Y, Nakamura H, Katayama Y, Imagama S, Ito Z, Ishiguro N. Segmental pedicle screwing for idiopathic scoliosis using computer-assisted surgery. J Spinal Disord Tech. 2008;21:181–186. doi: 10.1097/BSD.0b013e318074d388. [DOI] [PubMed] [Google Scholar]
- 20.Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994;18:341–346. doi: 10.1007/BF00187077. [DOI] [PubMed] [Google Scholar]
- 21.Tian NF, Xu HZ. Image guided pedicle screw insertion accuracy: a meta-analysis. Int Orthop. 2009;33:895–903. doi: 10.1007/s00264-009-0792-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wendl K, Recum J, Wentzensen A, Gruetzner PA. Iso-C (3 D-assisted) navigated implantation of pedicle screws in thoracic and lumbar vertebrae. Unfallchirug. 2003;106:907–913. doi: 10.1007/s00113-003-0683-9. [DOI] [PubMed] [Google Scholar]
- 23.Wiesner L, Kothe R, Ruther W. Anatomic evaluation of two different techniques for the percutaneous insertion of pedicle screws in the lumbar spine. Spine. 1999;24:1599–1603. doi: 10.1097/00007632-199908010-00015. [DOI] [PubMed] [Google Scholar]