Abstract
Justice-involved adolescents engage in high levels of risky sexual behavior, underscoring the need for targeted, effective, prevention interventions geared toward this population. In a randomized controlled trial, 484 detained adolescents received a theory-based intervention or an information-only control. We have previously demonstrated that the theory-based intervention was superior to the control condition in changing theoretical mediators and in producing longitudinal decreases in risky sexual behavior. In the present study, we examined differential response to the intervention based on the adolescents’ level of positive outlook (composed of self-esteem, perceived control over the future and optimism toward the future). Changes to putative theoretical mediators (attitudes, perceived norms, self-efficacy and intentions) were measured immediately post-intervention, and behavioral data were obtained 3, 6, 9 and 12 months later. Positive outlook significantly moderated program effects both in the context of the mediational path model and in the context of the longitudinal growth model. Specifically, intervention effects were strongest for those scoring relatively lower on the positive outlook dimension, whereas adolescents high in positive outlook demonstrated greater attitudes and self-efficacy and decreased risky sexual behavior, regardless of condition. Findings are discussed in terms of targeting and tailoring of intervention content.
Introduction
While the incidence of HIV and other sexually transmitted infections (STIs) has decreased among many demographic groups in the United States, adolescents and emerging adults remain among the subgroups at relatively higher risk for HIV infection and STI [1, 2]. These rates are even more striking among justice-involved youth. Justice-involved adolescents tend to engage in high levels of sexual risk behavior [3–6], resulting in high rates of STIs and/or pregnancy [7–10]. From a practical standpoint, justice involvement presents an important opportunity to access these high-risk adolescents [11] as many are not in the traditional systems, such as public school, where prevention activities traditionally occur. It is imperative to develop effective sexual risk reduction interventions for this population and to determine the factors that maximize positive intervention response.
Individual difference factors that confer resilience in the context of high-risk environments may be particularly important for predicting and mitigating HIV/STI risk in at-risk youth [12–13]. A proportion of adolescents who have grown up in disadvantaged backgrounds may respond by believing that it is unlikely for them to have a healthy and prosperous future. Conversely, those who maintain a positive self-evaluation may be characterized as resilient youth who attempt to engage in healthy behavior regardless of the circumstances [14]. Research on resiliency factors for HIV risk has often emphasized self-esteem and future orientation or the degree to which adolescents think about, plan for and are optimistic about the future. Higher self-esteem appears protective against risky sexual behavior in various populations [14–16] and findings suggest a reliable negative relationship between future orientation and problem behaviors [17]. The influence of these resiliency factors may be explained through their influence on traditional social cognitive constructs. For example, self-esteem and hopefulness predict stronger positive attitudes toward safe sex [18], and perceived control over the future is likely relevant for self-efficacy, a critical construct according to social cognitive theory [19].
Drawing from these perspectives, our group has developed and refined a conceptual model of HIV risk in high-risk adolescents in which self esteem, optimism about the future and perceived control over the future (referred to collectively as ‘positive outlook’) constitute protective factors for engaging in sexual risk behavior. Support for this theoretical model has been demonstrated across several distinct cohorts of disadvantaged adolescents, ranging from incarcerated and probated youth [20–21] to adolescents in sub-Saharan Africa [22]. These studies indicate that stronger positive outlook predicts reduced sexual risk behavior both directly and through its influence on traditional social cognitive constructs (e.g. attitudes, norms and self-efficacy related to condom use). A consistent finding across these studies is that self-efficacy is strongly related to positive outlook and partly mediates its association with safe sex intentions [20–22]. Additionally, there is evidence that positive outlook might mitigate the influence of individual risk factors (e.g. impulsivity, alcohol use) on other health risk behaviors [13, 15]. Collectively, these findings may provide evidence for a ‘subpopulation-specific’ resiliency factor that appears particularly important in predicting HIV risk among disadvantaged youth [20–21]. These studies also address the need to integrate theoretically relevant individual difference factors within traditional social cognitive models of health behavior [23] and to tailor traditional models to include subpopulation-relevant risk or protective factors [20–21, 24–25].
In recent work, our group has tested a theory-based intervention to increase safer sexual behavior among high-risk detained adolescents [26–27]. The intervention consisted of a group-based, interactive psychoeducation program grounded in the theory of planned behavior (TPB) and targeted toward theoretical constructs demonstrated to predict condom use in at-risk youth. In general, we showed that two theory-based interventions (one including alcohol content and one not including alcohol content) were superior to the information-only control intervention both in changing putative mediators of program efficacy and in producing changes in condom use and risky sexual behavior. However, the effects on behavior, while statistically significant and maintained up to 12 months post-intervention, were not large, as is common in other studies of HIV prevention trials targeting the general adolescent population [28–29] as well as justice-involved youth specifically [30]. This leads to the important question of whether the intervention was more successful for some adolescents than for others.
Recent randomized trials and meta-analytic reviews of HIV interventions emphasize the importance of identifying moderators of intervention response [31–32]. Ideally, the identification of an efficacious HIV risk intervention is followed by an evaluation of its differential impact across subgroups of individuals [31]. In a review of meta-analyses in the HIV prevention literature [32], the most commonly studied moderators included demographic factors, aspects of HIV status and baseline risk behavior. Less common is the evaluation of individual difference factors that might moderate intervention efficacy (although see ref. [33] for an evaluation of baseline depression status as a moderator in the context of an HIV intervention geared toward justice-involved youth). Once identified, such moderating factors could aid in identifying higher risk individuals and/or anticipating intervention response, with the ultimate goal of enhancing the efficacy of interventions [34]. Additionally, the identification of modifiable resiliency factors could lead to interventions that aim to reduce HIV risk by targeting these constructs [12, 35].
The goal of the current study was to extend our prior work demonstrating the association of positive outlook with social cognitive constructs relevant to condom use and to examine positive outlook as a resiliency factor that might predict differential response to our HIV risk intervention [26–27]. Positive outlook was examined as a moderator in the context of the path model of TPB-based mediators previously found to drive intervention efficacy [26] and in the context of the longitudinal growth model demonstrating decreased risky sexual behavior over time [27]. Consistent with past research [20–21], it was expected that youth high on the positive outlook dimension would demonstrate lower levels of sexual risk. However, it remained unclear how, or even whether, positive outlook would influence response to the intervention. On the one hand, those highest in positive outlook may be most motivated to adopt health protective behaviors and thus be more engaged in intervention content; on the other hand, those low in positive outlook may be in greatest need of the intervention and may be in a position to improve the most from the intervention content.
Methods
Participants
Participants were 484 adolescents recruited from three detention facilities in the Denver, CO, judicial district from January 2004 to July 2006. The mean age of the participants was 15.8 (SD = 1.1) and the majority (82.7%) was male. The sample was racially and ethnically diverse: 36.6% Caucasian, 28.5% Hispanic, 12.9% African American, 4.8% Native American, 3.5% Asian, 2.1% other ethnicity and 12.6% biracial/mixed ethnicity. Most participants (92.7%) reported ever having had sex. The mean age of first intercourse was 13.0 (SD = 1.7), and the median number of sexual partners was 6.0 (mode was 4). At baseline, only 27.1% reported condom use in ‘all’ sexual encounters.
Procedures
All study procedures were approved by an institutional review board at the University of Colorado at Boulder, a federal certificate of confidentiality was obtained for this research and approval was obtained from the federal Office for Human Research Protections. To be eligible, adolescents had to be between 14 and 17 years old, English speaking, current residents at one of the three detention facilities, have fully informed consent from a parent or legal guardian and give their own fully informed assent. The facilities involved were secure detention facilities that predominantly serve pre-adjudicated youth and those with short sentences.
Random assignment was determined using a random numbers table blocked on gender of participant. The intervention conditions were administered by masters-level intervention leaders who were trained to criterion in the presentation of each manualized intervention. Sex of intervention leader was matched to sex of the participants. Interventions were conducted in classrooms within each facility and were administered in same-sex groups with an average group size of four participants. All interventions were conducted in one session, with the active interventions lasting 3–4 hours and the information-only control condition lasting approximately 1 hour. Fidelity of intervention delivery was confirmed, consistent with procedures used in the previous intervention research [24, 36]. The two active group-level psychosocial interventions were based on previously successfully published HIV/STD risk reduction interventions conducted with young people [10, 24, 36]. Each component targeted constructs from the theoretical models previously shown to relate to condom use in this population [20–21] through group activities, videos and condom use demonstrations. The two active conditions were identical in psychoeducation content, with the only difference being that one intervention included an alcohol-specific motivational enhancement component [26]. Because we did not find statistically significant differences between the two interventions in predicting condom use over the 12 months following the interventions [27], we collapsed across active intervention groups for the current analyses. Participants in the information-only control condition received several components that were also covered in the two active interventions, including basic STI information and definitions and modes and body fluids of HIV transmission, but the control condition did not include content focused on the putative theoretical mediators (e.g. self-efficacy, attitudes, norms). Greater detail of the intervention content is provided in Schmiege et al. [26].
Participants were assessed just prior to and immediately following the intervention, as well as at 3-, 6-, 9- and 12-month follow-ups. All measures were completed on laptop computers via audio computer-assisted self-interview (ACASI). Participants received $25 (US) for completing the intervention and baseline assessments, $25 for each of the 3-, 6- and 9-month follow-ups and $50 for the 12-month follow-up. Retention rates ranged from 65.3% to 69.8% across follow-up waves.
Measures
Positive outlook
‘Self-esteem’ [37] was calculated as the mean of eight statements (e.g. ‘In general, I am satisfied with myself’), each measured on a 4-point scale from 1 = ‘disagree a lot’ to 4 = ‘agree a lot’ (M = 3.23, SD = 0.51, α = 0.79). ‘Control over the future’ [38] was assessed as the mean of seven items (e.g. ‘My future is what I make of it’), measured on the same 4-point scale as self-esteem (M = 3.30, SD = 0.48, α = 0.71). ‘Optimism about the future’ [20] was assessed as the mean of four items (e.g. ‘How likely do you think it is that you will get a good job someday?’), measured on a 4-point scale ranging from 1 = ‘will not happen’ to 4 = ‘will definitely happen’ (M = 3.493, SD = 0.48, α = 0.76). The mean values observed here are consistent with prior studies examining these constructs in other samples of incarcerated adolescents [20–21]. In the prior work, these three measures were treated as indicators of a latent variable that provided excellent fit to the data and were strongly related to TPB-based mediators [20–21]. In order to make the variable amenable to the moderational analyses performed here, we formed a positive outlook index wherein each of the three variables was standardized and these standardized scores were averaged (α = 0.87).
Mediational constructs
Putative mediators (validated in refs [20–21, 24–25]) were measured just prior to and immediately following the intervention. The range of these scales was 1–4, and response options varied from ‘disagree a lot’ to ‘agree a lot’ (or ‘will not happen’ to ‘will definitely happen’ for the intention measures) with higher numbers indicating more positive endorsement of the construct. Scale scores were calculated as a mean of the items comprising each scale. Measured scales included ‘attitudes toward condom use’ [23 items; M = 3.06, SD = 0.45, α = 0.87; e.g. ‘Condoms can ruin the sexual mood’ (reversed)]; ‘perceived norms for condom use’ (8 items; M = 2.78, SD = 0.75, α = 0.91; e.g. ‘Most of my friends use condoms when they have sex’) [The eight-item norm scale originally included four items designed to distinguish injunctive norms measuring perceptions of what close others think one ought to do (e.g. ‘Most of my friends think people should always use a condom when having sex with a new person’) from descriptive norms measuring perceptions of what those around the adolescent actually do (e.g. ‘Most of my friends use condoms when they have sex’). However, the two scales were psychometrically indistinguishable in the current sample (r = 0.70) and were thus collapsed for all analyses.]; ‘self-efficacy for condom use’ [21, 39–40] (33 items; M = 3.47, SD = 0.44, α = 0.93; e.g. ‘I am confident in my ability to use a condom correctly’; ‘I could stop to use a condom even in the heat of passion’) and ‘intentions to practice safer sexual behavior’ (12 items; M = 2.85, SD = 0.64, α = 0.88; e.g. ‘How likely is it that you will use a condom every time you have sexual intercourse?’).
Risky sexual behavior
A risky sexual behavior index was assessed at baseline and at each follow-up assessment. Risky sexual behavior was measured as a multiplicative combination of condom use (reverse scored) and frequency of intercourse. This index was utilized because condom use may be more or less meaningful as an indicator of risky sexual behavior depending on frequency of intercourse. Condom use behavior was measured on a 5-point scale from 0 to 4 with the question ‘In the past three months, how much of the time did you use condoms when you had sexual intercourse?’ with response options of ‘never’, ‘almost never’, ‘sometimes’, ‘almost always’ and ‘always’. Frequency of intercourse was assessed on a 6-point scale from 0 to 5 with the item ‘On average, how often have you had sexual intercourse in the past 3 months?’ Response options ranged from ‘none’ to ‘more than ten times’. Condom use behavior was reverse coded and the resulting risky sex index was calculated such that higher scores indicated more risky sexual behavior (i.e. greater frequency of intercourse and lower condom use, with a potential range from 0 to 20).
Results
Overview of analyses
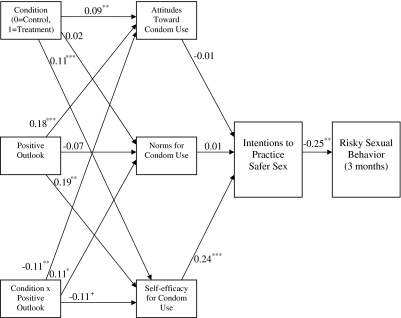
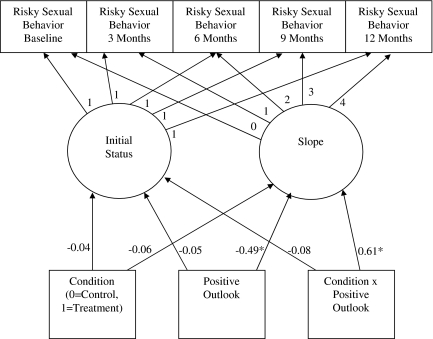
Our analytic approach flowed from our work examining the mediational pathways through which the interventions had their impact on intentions and short-term behavior [26] and the trajectories of longer term behavioral effects [27]. First, we examined the role of the positive outlook index as a moderator of the TPB-based mediators previously found to drive intervention efficacy in the active versus information-only interventions [26]. In addition to a contrast comparing the active interventions with the information-only intervention, we included the main effect of positive outlook and the intervention by positive outlook interaction term as additional exogenous variables in a mediational model (see Fig. 1). To explore the role of positive outlook on long-term behavioral outcomes, we included the main effect of positive outlook and the intervention by positive outlook interaction term in addition to the main effect of condition (active versus information only) as fixed effects in a conditional latent growth model [41] examining risky sexual behavior over time (see Fig. 2).
Fig. 1.
Positive outlook as a moderator of the effects of intervention condition on theoretical predictors in the context of a TPB-based mediational model. Note: ***P < 0.001, **P < 0.01, *P < 0.05, +P = 0.06.
Fig. 2.
Positive outlook as a moderator of the effects of intervention condition on the trajectory of risky sexual behavior over time. Note: *P < 0.05.
Moderation of mediational model
The estimated model examining positive outlook as a moderator in the context of the mediational model [26] is depicted in Fig. 1. This model fit the data adequately [χ2 (29, N = 484) = 72.43, P < 0.001, Root Mean Square Error of Approximation (RMSEA) =0.06, Standardized Root Mean Square Residual (SRMR) =0.05], and accounted for 21% of the variance in risky sexual behavior and 58% of the variance in intentions to practice safer sexual behavior. Although not shown for ease of presentation, pretest scores on each construct were included as covariates predicting their respective construct to decrease error variance due to high correlations between pretest and post-test scores [42]. Consistent with past work [26], participation in either of the two active interventions predicted more positive attitudes toward condom use and higher self-efficacy for condom use relative to participation in the control group. Self-efficacy, in turn, was related to behavioral intentions and greater intentions to practice safer sex predicted lower levels of risky sexual behavior 3 months later. Unique to these analyses was the evidence of a direct effect of positive outlook on attitudes and self-efficacy where higher scores on the positive outlook construct predicted more positive attitudes toward condom use and higher self-efficacy for condom use. These main effects were qualified by significant interactions between condition and positive outlook on attitudes, norms and self-efficacy, providing evidence that positive outlook moderates the impact of the intervention.
To interpret the moderator relationships, supplementary regression analyses examined the simple slope of the outcome on condition at three levels of the predictor to capture high, average and low levels of positive outlook: 1 SD above the positive outlook mean, at the mean and 1 SD below the mean [43]. These analyses revealed the following interpretations of the three interactions: (i) participation in an active intervention significantly predicted increased favorable post-intervention attitudes toward condom use among those with low [β = 0.14 (0.03), P < 0.001] and average [β = 0.08 (0.03), P < 0.01] positive outlook scores but not among those with high positive outlook scores [β = 0.02 (0.04), non-significant (n.s.)]; (ii) participation in an active intervention also significantly predicted increased post-intervention self-efficacy toward condom use among those low [β = 0.13 (0.03), P < 0.001] and average [β = 0.08 (0.02), P < 0.001] in positive outlook but not among those with high positive outlook [β = 0.03 (0.03), n.s.]; (iii) in contrast, intervention condition significantly predicted more supportive post-intervention norms for condom use among those with high [β = 0.15 (0.07), P < 0.05] positive outlook but not for those with low [β = −0.07 (0.07), n.s.] or average [β = 0.04 (0.05), n.s.] scores. We thus have evidence that the mediational pathways through which the intervention had its effects were moderated by level of positive outlook. Of particular interest was the evidence of effects on self-efficacy for those scoring low and moderately on positive outlook, given that self-efficacy had indirect links to behavior, via intentions.
Moderation of longitudinal model
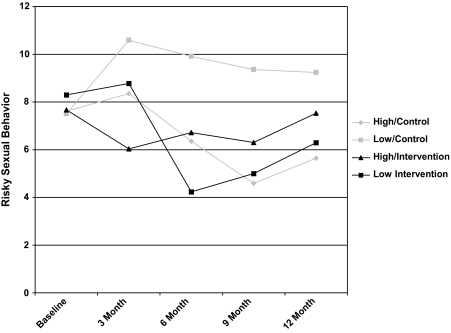
Figure 2 presents positive outlook as a moderator in the context of a longitudinal latent growth model of risky sexual behavior over time. This model demonstrated adequate fit to the data [χ2 (19, N = 484) = 59.64, P < 0.001, RMSEA = 0.06, SRMR = 0.08] and accounted for 2% of the variance in the intercept and 15% of the variance in the slope, representing small and medium effect sizes, respectively. None of the three constructs uniquely predicted the intercept, but there was a main effect of positive outlook on the slope [β = −0.49 (0.25), P < 0.05] where the negative direction indicates that higher positive outlook scores predicted decreasing risky sexual behavior over time. This main effect was qualified by a significant condition by positive outlook interaction [β = 0.61 (0.28), P < 0.05]. Interpretation of this interaction revealed that, in the absence of intervention, high positive outlook served as a buffer against increased risky sexual behavior over time. This interaction can be further understood by the observed risky sexual behavior means, presented by condition and high/low positive outlook, in Fig. 3. For illustrative purposes only, a median split was conducted on positive outlook scores with n = 88 and n = 74 participants scoring low and high on positive outlook, respectively, in the control condition and n = 152 and n = 169 participants scoring low and high, respectively, in the active interventions. Those high in positive outlook demonstrated decreased risky sexual behavior over time, regardless of condition. In contrast, those who were low on positive outlook but were also in the active intervention conditions demonstrated decreased risky sex, whereas those in the information-only control condition did not demonstrate decreases over time.
Fig. 3.
Observed risky sexual behavior means across all waves of data by intervention condition and high versus low positive outlook.
Discussion
We examined the role of an individual difference factor as a moderator of the effects of two theory-based sexual risk reduction interventions versus an information-only control with a sample of justice-involved (detained) youth. Our findings highlight the potential role of a component of resilience termed ‘positive outlook’ in predicting intervention response. We first evaluated whether positive outlook would moderate the previously supported [26] mediational model of intervention effects on risky sexual behavior. Positive outlook had significant main effects on attitudes toward condom use and condom use self-efficacy. The strong linkage between positive outlook and condom use self-efficacy is consistent with our prior work [20–21], suggesting the robustness of this factor with justice involved high-risk adolescents. Further, intervention effects were stronger for those with limited levels of this protective factor, such that adolescents with low levels of positive outlook increased both their positive attitudes toward condom use and their perceptions of condom use self-efficacy in response to the theory-based versus information-only interventions. In contrast, those high in positive outlook did not show differential response to the intervention because attitudes and self-efficacy were relatively high among these adolescents regardless of intervention condition. Interestingly, the effect of the intervention on perceptions of supportive norms for condom use was stronger for those with ‘higher’ positive outlook. In past work [26], intervention condition exhibited the lowest effect size for norms relative to all other theoretical mediators; the present analyses suggest that the impact of condition on norms may be bolstered by high levels of positive outlook.
Next we investigated the influence of positive outlook in the context of a latent growth model examining sexual risk behavior over time up to 12 months post-intervention. The findings were largely consistent with the mediational model, wherein higher positive outlook scores at baseline predicted decreased levels of risky behavior over time and adolescents with low levels of positive outlook responded better to the active intervention conditions. Specifically, adolescents low on positive outlook showed decreased levels of risk behavior in the active interventions but did not evidence the same decreases following the information-only control condition. In contrast, adolescents who were high in positive outlook responded equally well, with decreasing levels of risky sexual behavior over time, regardless of intervention condition.
These findings suggest that it is critical to foster and/or bolster general optimism factors among high-risk adolescents [12]. Methods for doing so with high-risk youth have been delineated by Feldstein Ewing et al. [44, 45] and include approaches such as the characteristics of successful adolescents exercise and the success stories exercise. These strategies focus on having adolescents identify positive attributes about themselves, as well as times they were able to successfully overcome obstacles. The ultimate goal of these exercises is to engender a sense of autonomy and ability to enact positive behavioral changes (see Feldstein Ewing et al. [45] for greater detail). This approach is highly consonant with the resilience literature [46] and substantially overlaps with the recent movement toward strength-based approaches both within the sexual risk [26] and within the broader risk intervention literature [47–48]. Adolescence is a time where many emotional and behavioral symptoms (internalizing/externalizing) as well as negative self-image tend to emerge due to real and/or perceived negative scrutiny by self and peers. Thus, the key for effective interventions may be to maintain the existence of this protective factor for adolescents who may initially have it; this question is a focus of our ongoing work.
While it would be ideal to be able to foster and promote positive outlook, there is also a reasonable literature that suggests that this factor may be dispositional [49] and relatively unresponsive to intervention. It might also be ideal to explore the broader context of development, targeting the families of high-risk children and adolescents in order to foster the longer term development of positive outlook constructs. For example, studies have found that skillful parenting may be able to temper the potential negative trajectory of adolescent temperamental risks [50], and several adolescent risk prevention groups have subsequently approached health risk intervention through parents and families of general, as well as justice-involved youth, with promising results [30, 51–52].
The results should be interpreted with the following limitations in mind. First, data were gathered by self-report and therefore social desirability, self-report biases and poor recall could have contributed to measurement error; however, we share this limitation with virtually all other intervention work [11] and the ACASI technology was employed to assist with truthfulness and accuracy of the self-report data. We were unfortunately unable to obtain information about any adolescents who refused to offer assent due to logistical constraints within the juvenile justice system. That the retention rates were somewhat low (i.e. less than 70%) is a limitation of this study, although attrition analyses reported elsewhere [26, 27] demonstrated no significant differences by condition between retained participants and those lost to attrition in baseline demographic and behavioral variables. The high proportion of male participants could be considered a limitation of this study; however, the sample is consistent with the demographics of this and other juvenile justice populations [6] with respect to gender and ethnicity. Finally, we chose an index of risky sexual behavior that assessed condom use while controlling for frequency of sexual intercourse. Although such an index was consistent with the harm reduction approach of our intervention message and was easily understood by our participants, more precise ways of quantifying self-reported sexual risk (e.g. event-level analyses, timeline follow back assessments) could be useful in future studies.
In sum, this study highlights the robust role of positive outlook as both an initial protective factor for engaging in risky sex and a moderator of response to an HIV/STI prevention intervention among high-risk youth. These findings suggest that youth with high levels of this protective factor evidence better intentions and condom use behavior both immediately and in the longer term following intervention of even the most minimal education-based content. However, youth with lower levels of positive outlook appear to respond more favorably to a more active, theory-based intervention than an information-only intervention. These findings suggest the critical importance of targeting our theory-based intervention to those scoring low positive outlook dimension and/or bolstering positive outlook among at-risk youth and maintaining it among those youth who already appear to have this protective factor. Extensive strides have been made in the design, implementation and evaluation of interventions to increase safer sexual behavior among adolescents. In a recent editorial, Dr Bonita Stanton [53] noted that among general adolescent populations, ‘Multiple trials and numerous meta-analyses have clearly established that behavioral prevention programs can reduce sexual risk behaviors and that such reductions can persist for 1 year or longer’ (p. 1162). However, much work remains in evaluating how HIV prevention interventions work among juvenile justice-involved populations; this study and the intervention trial findings that stem from it take one important step toward addressing this issue. Furthermore, it is the case that successful interventions have key characteristics in common, including a focus on skill building and a strong grounding in established theories of health behavior [54–55]. We must now move beyond these broad findings to explore individual difference characteristics that render our interventions more or less successful and how this informs the development of interventions with broader applicability, as well as those that target subgroups of adolescents at elevated risk, such as justice-involved youth.
Funding
National Institute on Alcoholism and Alcohol Abuse at the National Institutes of Health (R01 AA013844-01 to A.D.B., F32 AA018629 to C.S.H.).
Conflict of interest statement
None declared.
Acknowledgments
We wish to thank the detention facilities (Marvin Foote, Mount View and Gilliam), the young people who participated in our study and our contacts at each of the facilities, Sally Anderson, JoAnn Meeks, Diane Stohner and Vera Candy-Dominguez. We would also like to thank the Colorado Department of Youth Corrections for their cooperation and support. Finally, we wish to thank our research assistants Katy Seals, Sarah Taylor, Michael Levin, Roger Martin-Pressman, Helaine Powell, Patrick Finan, Justin Corrocher, Neil Cline, Ashleigh Golub, Jacob Lee and Angela Hendricks.
References
- 1.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance, 2008. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2009. Available at: http://www.cdc.gov/std/stats08/main.htm. Accessed: 23 June 2010. [Google Scholar]
- 2.Hall HI, Song R, Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–9. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barthlow DJ, Horan PF, DiClemente RJ, et al. Correlates of condom use among incarcerated adolescents in a rural state. Crim Justice Behav. 1995;22:295–306. [Google Scholar]
- 4.Lux KM, Petosa R. Preventing HIV infection among juvenile delinquents: educational diagnosis using the health belief model. Int Q Community Health Educ. 1995;15:145–63. doi: 10.2190/WTBA-HVC1-R16N-RRT5. [DOI] [PubMed] [Google Scholar]
- 5.Morris RE, Harrison EA, Knox GW, et al. Health risk behavioral survey from 39 juvenile correctional facilities in the United States. J Adolesc Health. 1995;17:334–44. doi: 10.1016/1054-139X(95)00098-D. [DOI] [PubMed] [Google Scholar]
- 6.Teplin LA, Mericle AA, McClelland GM, et al. HIV and AIDS risky behaviors in juvenile detainees: implications for public health policy. Am J Public Health. 2003;93:906–12. doi: 10.2105/ajph.93.6.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Canterbury RJ, Clavet GJ, McGarvey EL, et al. HIV risk-related attitudes and behaviors of incarcerated adolescents: implications for public school students. High School J. 1998;82:1–10. [Google Scholar]
- 8.Morris RE, Baker CJ, Valentine M, et al. Variations in HIV risk behaviors of incarcerated juveniles during a four-year period: 1989–1992. J Adolesc Health. 1998;23:39–48. doi: 10.1016/s1054-139x(97)00268-1. [DOI] [PubMed] [Google Scholar]
- 9.Pack RP, DiClemente RJ, Hook EW. High prevalence of asymptomatic STD in incarcerated minority male youth: a case for screening. Sex Transm Dis. 2000;27:175–7. doi: 10.1097/00007435-200003000-00011. [DOI] [PubMed] [Google Scholar]
- 10.St Lawrence JS, Crosby RA, Belcher L, et al. Sexual risk reduction and anger management interventions for incarcerated male adolescents: a randomized controlled trial of two interventions. J Sex Educ Ther. 1999;24:9–17. [Google Scholar]
- 11.Hurd NM, Valerio MA, Garcia NM, et al. Adapting an HIV prevention intervention for high-risk, incarcerated adolescents. Health Educ Behav. 2010;37:37–50. doi: 10.1177/1090198109335655. [DOI] [PubMed] [Google Scholar]
- 12.DiClemente RJ, Wingood GM, Rose E, et al. Evaluation of an HIV/STD sexual risk-reduction intervention for pregnant African American adolescents attending a prenatal clinic in an urban public hospital: preliminary evidence of efficacy. J Pediatr Adolesc Gynecol. 2010;23:32–8. doi: 10.1016/j.jpag.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Broaddus MR, Bryan AD. Consistent condom use among juvenile detainees: the role of individual differences, social bonding, and health beliefs. AIDS Behav. 2008;12:59–67. doi: 10.1007/s10461-007-9260-5. [DOI] [PubMed] [Google Scholar]
- 14.Ethier KA, Kershaw TS, Lewis JB, et al. Self-esteem, emotional distress and sexual behavior among adolescent females: inter-relationships and temporal effects. J Adolesc Health. 2006;38:268–74. doi: 10.1016/j.jadohealth.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 15.Schmiege SJ, Levin M, Bryan A. Regression mixture models of alcohol use and risky sexual behavior among criminally-involved adolescents. Prev Sci. 2009;10:335–44. doi: 10.1007/s11121-009-0135-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stein JA, Rotheram-Borus MJ, Swendeman D, et al. Predictors of sexual transmission risk behaviors among HIV-positive young men. AIDS Care. 2005;17:433–42. doi: 10.1080/09540120412331291724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nurmi J-E. How do adolescents see their future? A review of the development of future orientation and planning. Dev Rev. 1991;11:1–59. [Google Scholar]
- 18.Chang VY, Bendel TL, Koopman C, et al. Delinquents' safe sex attitudes—relationships with demographics, resilience factors, and substance use. Crim Justice Behav. 2003;30:210–29. [Google Scholar]
- 19.Bandura A. A social cognitive approach to the exercise of control over AIDS infection. In: DiClemente RJ, editor. Adolescents and AIDS: A Generation in Jeopardy. Newbury Park, CA: Sage; 1992. pp. 89–116. [Google Scholar]
- 20.Bryan A, Aiken LS, West SG. HIV/STD risk among incarcerated adolescents: optimism about the future and self-esteem as predictors of condom use self-efficacy. J Appl Soc Psychol. 2004;34:912–36. [Google Scholar]
- 21.Bryan A, Rocheleau CA, Robbins RN, et al. Condom use among high-risk adolescents: testing the influence of alcohol use on the relationship of cognitive correlates of behavior. Health Psychol. 2005;24:133–42. doi: 10.1037/0278-6133.24.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bryan AD, Kagee A, Broaddus MR. Condom use among South African adolescents: developing and testing theoretical models of intentions and behavior. AIDS Behav. 2006;10:387–97. doi: 10.1007/s10461-006-9087-5. [DOI] [PubMed] [Google Scholar]
- 23.Noar SM, Zimmerman RS, Palmgreen P, et al. Integrating personality and psychosocial theoretical approaches to understanding safer sexual behavior: implications for message design. Health Commun. 2006;19:165–74. doi: 10.1207/s15327027hc1902_8. [DOI] [PubMed] [Google Scholar]
- 24.Bryan AD, Aiken LS, West SG. Increasing condom use: evaluation of a theory-based intervention to prevent sexually transmitted diseases in young women. Health Psychol. 1996;15:371–82. doi: 10.1037//0278-6133.15.5.371. [DOI] [PubMed] [Google Scholar]
- 25.Bryan AD, Aiken LS, West SG. Young women's condom use: the impact of perceived susceptibility, acceptance of sexuality and control over the sexual encounter. Health Psychol. 1997;16:468–79. doi: 10.1037//0278-6133.16.5.468. [DOI] [PubMed] [Google Scholar]
- 26.Schmiege SJ, Broaddus MR, Levin M, et al. Randomized trial of group interventions to reduce HIV/STD risk and change theoretical mediators among detained adolescents. J Consult Clin Psychol. 2009;77:38–50. doi: 10.1037/a0014513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bryan AD, Schmiege SJ, Broaddus MR. HIV risk reduction among detained adolescents: a randomized, controlled trial. Pediatrics. 2009;124:1180–8. doi: 10.1542/peds.2009-0679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.DiClemente RJ, Salazar LF, Crosby RA. A review of STD/HIV preventive interventions for adolescents: sustaining effects using an ecological approach. J Pediatr Psychol. 2007;32:888–906. doi: 10.1093/jpepsy/jsm056. [DOI] [PubMed] [Google Scholar]
- 29.Stanton B, Kim N, Galbraith J, et al. Design issues addressed in published evaluations of adolescent HIV-risk reduction interventions: a review. J Adolesc Health. 1996;18:387–96. doi: 10.1016/1054-139X(95)00169-S. [DOI] [PubMed] [Google Scholar]
- 30.Tolou-Shams M, Steward A, Fasciano J, et al. A review of HIV prevention interventions for juvenile offenders. J Pediatr Psychol. 2010;35:250–61. doi: 10.1093/jpepsy/jsp069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lightfoot M, Tevendale H, Comulada WS, et al. Who benefited from an efficacious intervention for youth living with HIV: a moderator analysis. AIDS Behav. 2007;11:61–70. doi: 10.1007/s10461-006-9174-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Noar SM. Behavioral interventions to reduce HIV-related sexual risk behavior: review and synthesis of meta-analytic evidence. AIDS Behav. 2008;12:335–53. doi: 10.1007/s10461-007-9313-9. [DOI] [PubMed] [Google Scholar]
- 33.Rosengard C, Stein LAR, Barnett NP, et al. Randomized clinical trial of motivational enhancement of substance use treatment among incarcerated adolescents: post-release condom non-use. J HIV AIDS Prev Child Youth. 2007;8:45–64. doi: 10.1300/J499v08n02_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bancroft J, Janssen E, Carnes L, et al. Sexual activity and risk taking in young heterosexual men: the relevance of sexual arousability, mood, and sensation seeking. J Sex Res. 2004;41:181–92. doi: 10.1080/00224490409552226. [DOI] [PubMed] [Google Scholar]
- 35.O'Leary A, Hoff CC, Purcell DW, et al. What happened in the SUMIT trial? Mediation and behavior change. AIDS. 2005;19(Suppl 1):S111–21. doi: 10.1097/01.aids.0000167357.94664.10. [DOI] [PubMed] [Google Scholar]
- 36.Fisher JD, Fisher WA, Bryan AD, et al. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychol. 2002;21:177–86. [PubMed] [Google Scholar]
- 37.Rosenberg M. Society and the Adolescent Self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 38.Whitaker DJ, Miller KS, Clark LF. Reconceptualizing adolescent sexual behavior: beyond did they or didn't they? Fam Plann Perspect. 2000;32:111–7. [PubMed] [Google Scholar]
- 39.Brien TM, Thombs DL, Mahoney CA, et al. Dimensions of self-efficacy among three distinct groups of condom users. J Am Coll Health. 1994;42:167–74. doi: 10.1080/07448481.1994.9939665. [DOI] [PubMed] [Google Scholar]
- 40.Brafford LJ, Beck KH. Development and validation of a condom self-efficacy scale for college students. Coll Health. 1991;39:219–25. doi: 10.1080/07448481.1991.9936238. [DOI] [PubMed] [Google Scholar]
- 41.Curran PJ. A latent curve framework for the study of developmental trajectories in adolescent substance abuse. In: Rose JS, Chassin L, editors. Multivariate Applications in Substance Use Research: New Methods for New Questions. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2000. pp. 1–42. [Google Scholar]
- 42.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4th edn. Needham Heights, MA: Allyn & Bacon; 2001. [Google Scholar]
- 43.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- 44.Feldstein SW, Ginsburg JID. Sex, drugs, and rock ‘n’ rolling with resistance: motivational interviewing in juvenile justice setting. In: Roberts AR, Springer DW, editors. Handbook of Forensic Mental Health with Victims and Offenders: Assessment, Treatment, and Research. New York, NY: Springer Publishing; 2007. pp. 247–271. [Google Scholar]
- 45.Feldstein Ewing SW, Walters S, Baer JS. Approaching group MI with adolescents and young adults: strengthening the developmental fit. In: Wagner CCI, Ingersoll KS, editors. Motivational Interviewing in Groups. New York, NY: The Guildford Press, in press; [Google Scholar]
- 46.Masten AS. Ordinary magic: resilience processes in development. Am Psychol. 2001;56:227–38. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- 47.Dishion TJ, McCord J, Poulin F. When interventions harm: peer groups and problem behavior. Am Psychol. 1999;54:755–64. doi: 10.1037//0003-066x.54.9.755. [DOI] [PubMed] [Google Scholar]
- 48.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd edn. New York: Guilford Press; 2002. [Google Scholar]
- 49.Werner EE, Smith RS. Journeys from Childhood to Midlife: Risk, Resilience, and Recovery. Ithaca, NY: Cornell University Press; 2001. [DOI] [PubMed] [Google Scholar]
- 50.Hetherington EM, Kelly J. For Better or for Worse: Divorce Reconsidered. New York: W.W. Norton & Company; 2002. [Google Scholar]
- 51.Prado G, Pantin H, Briones E, et al. A randomized control trial of parent-centered intervention in preventing substance use and HIV risk behaviors in Hispanic adolescents. J Consult Clin Psychol. 2007;75:914–26. doi: 10.1037/0022-006X.75.6.914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Marvel F, Rowe CL, Colon-Perez L, et al. Multidimensional family therapy HIV/STD risk-reduction intervention: an integrative family-based model for drug-involved juvenile offenders. Fam Process. 2009;48:69–84. doi: 10.1111/j.1545-5300.2009.01268.x. [DOI] [PubMed] [Google Scholar]
- 53.Stanton B. Adolescent human immunodeficiency virus prevention: what we have accomplished and what still needs to be done. Arch Pediatr Adolesc Med. 2009;163:1162–3. doi: 10.1001/archpediatrics.2009.226. [DOI] [PubMed] [Google Scholar]
- 54.Albarracin D, Durantini MR, Earl A. Empirical and theoretical conclusions of an analysis of outcomes of HIV-prevention interventions. Curr Dir Psychol Sci. 2006;15:73–8. [Google Scholar]
- 55.Robin L, Dittus P, Whitaker D, et al. Behavioral interventions to reduce incidence of HIV, STD, and pregnancy among adolescents: a decade in review. J Adolesc Health. 2004;34:3–26. doi: 10.1016/s1054-139x(03)00244-1. [DOI] [PubMed] [Google Scholar]