Abstract
Background
Acupuncture is often used for migraine prophylaxis but its effectiveness is still controversial. This review (along with a companion review on ’Acupuncture for tension-type headache’) represents an updated version of a Cochrane review originally published in Issue 1, 2001, of The Cochrane Library.
Objectives
To investigate whether acupuncture is a) more effective than no prophylactic treatment/routine care only; b) more effective than ’sham’ (placebo) acupuncture; and c) as effective as other interventions in reducing headache frequency in patients with migraine.
Search strategy
The Cochrane Pain, Palliative & Supportive Care Trials Register, CENTRAL, MEDLINE, EMBASE and the Cochrane Complementary Medicine Field Trials Register were searched to January 2008.
Selection criteria
We included randomized trials with a post-randomization observation period of at least 8 weeks that compared the clinical effects of an acupuncture intervention with a control (no prophylactic treatment or routine care only), a sham acupuncture intervention or another intervention in patients with migraine.
Data collection and analysis
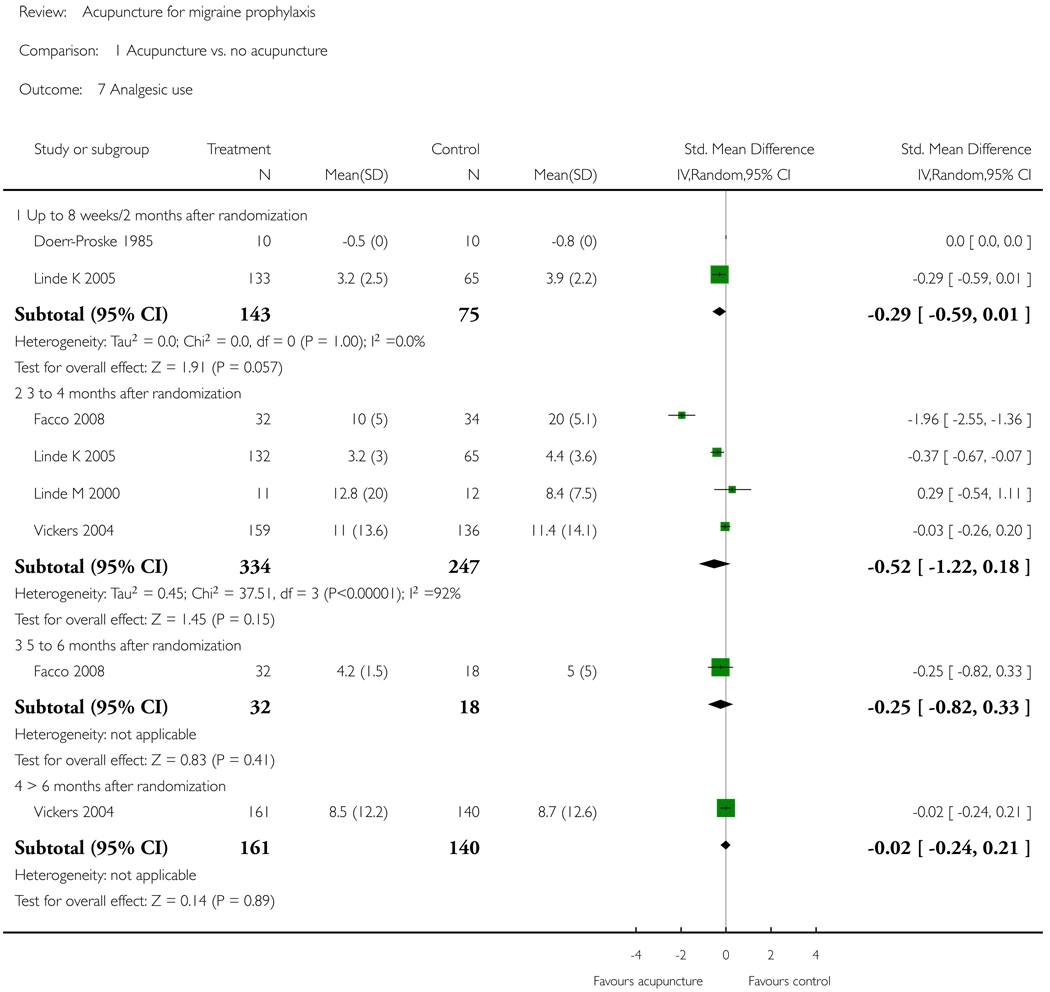
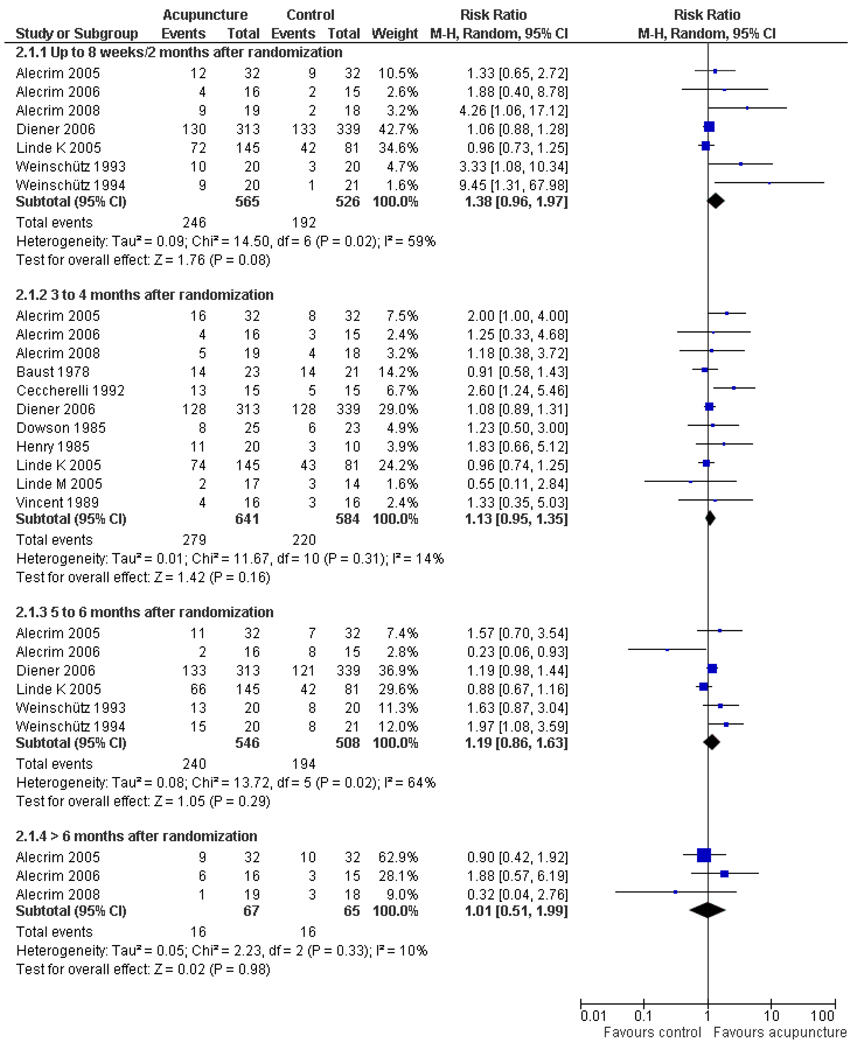
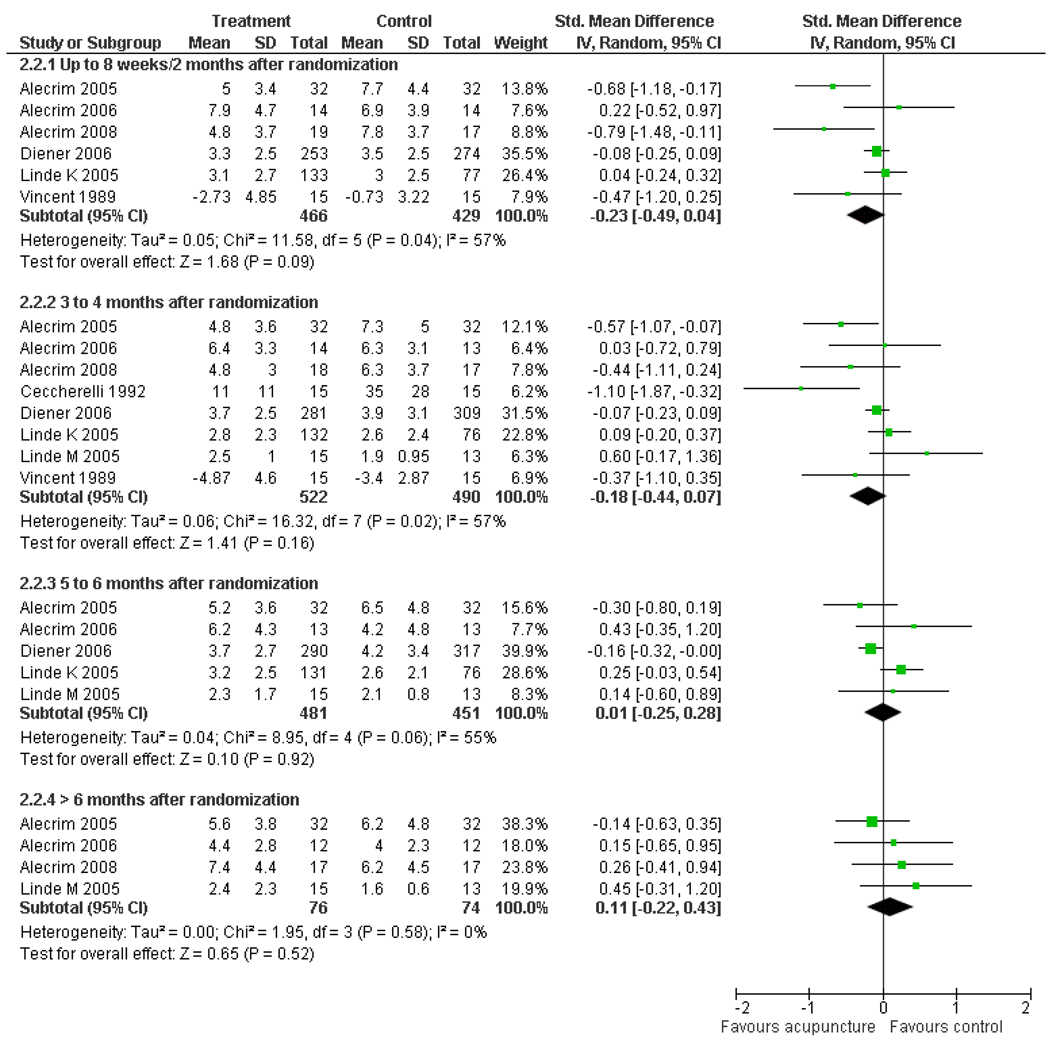
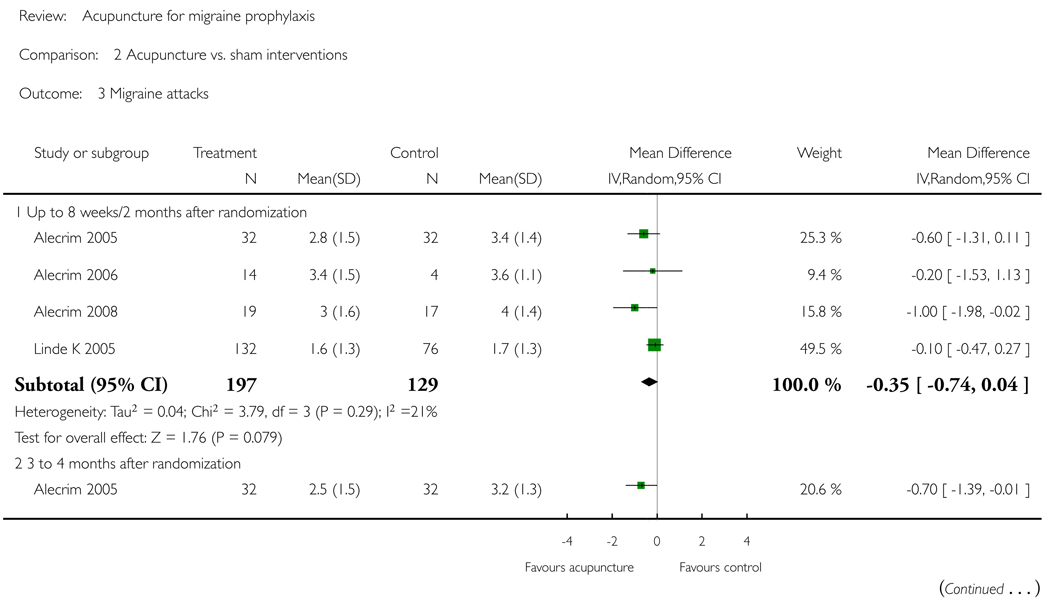
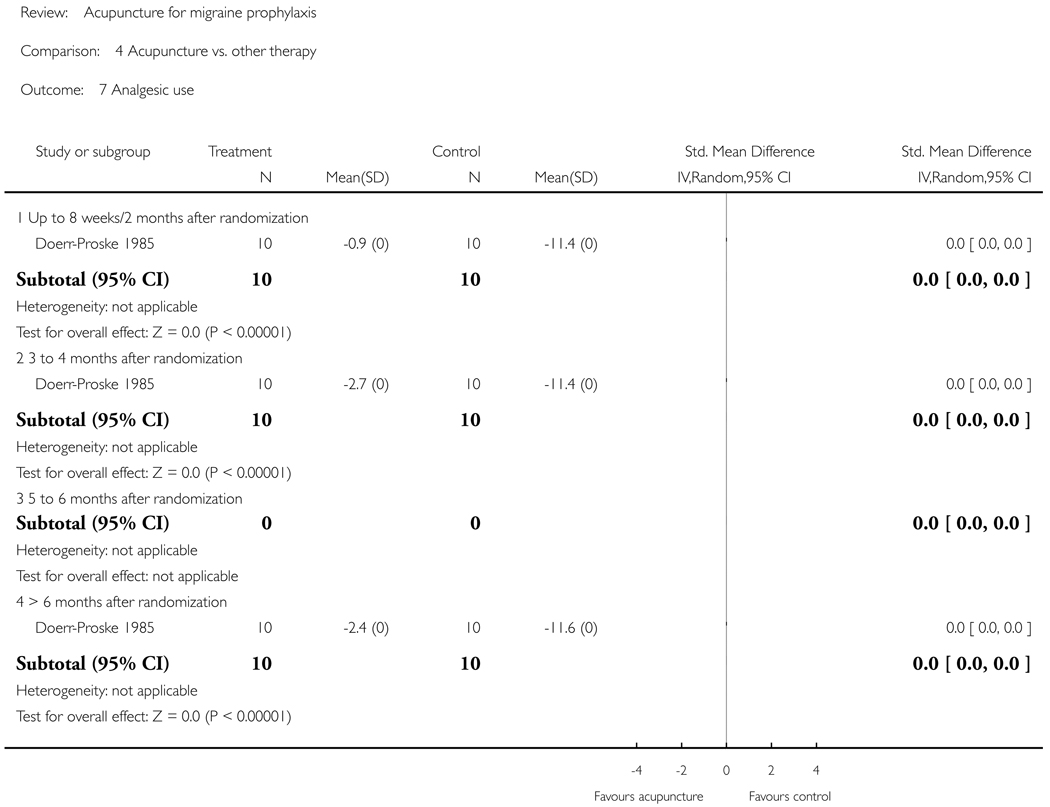
Two reviewers checked eligibility; extracted information on patients, interventions, methods and results; and assessed risk of bias and quality of the acupuncture intervention. Outcomes extracted included response (outcome of primary interest), migraine attacks, migraine days, headache days and analgesic use. Pooled effect size estimates were calculated using a random-effects model.
Main results
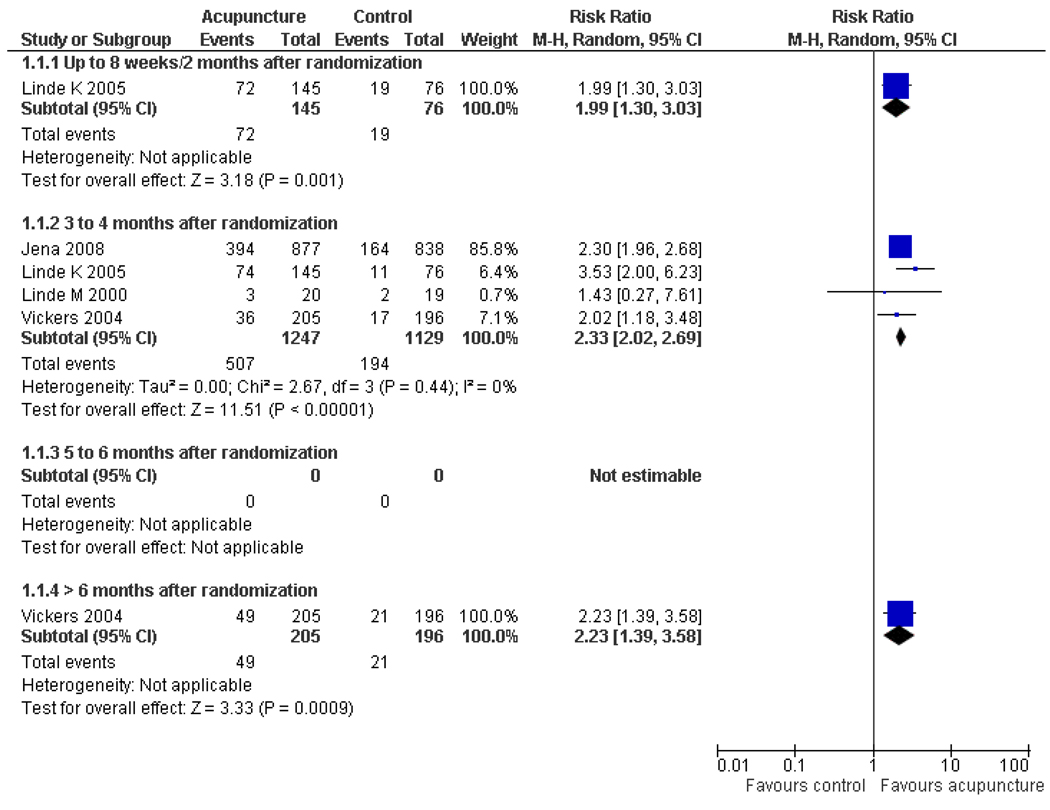
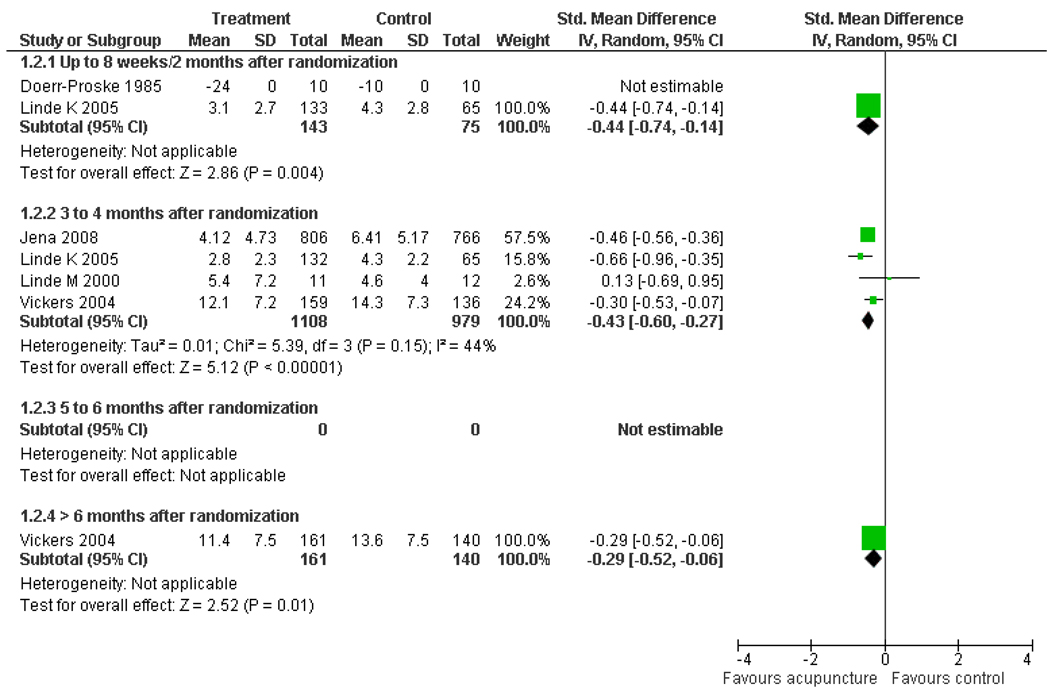
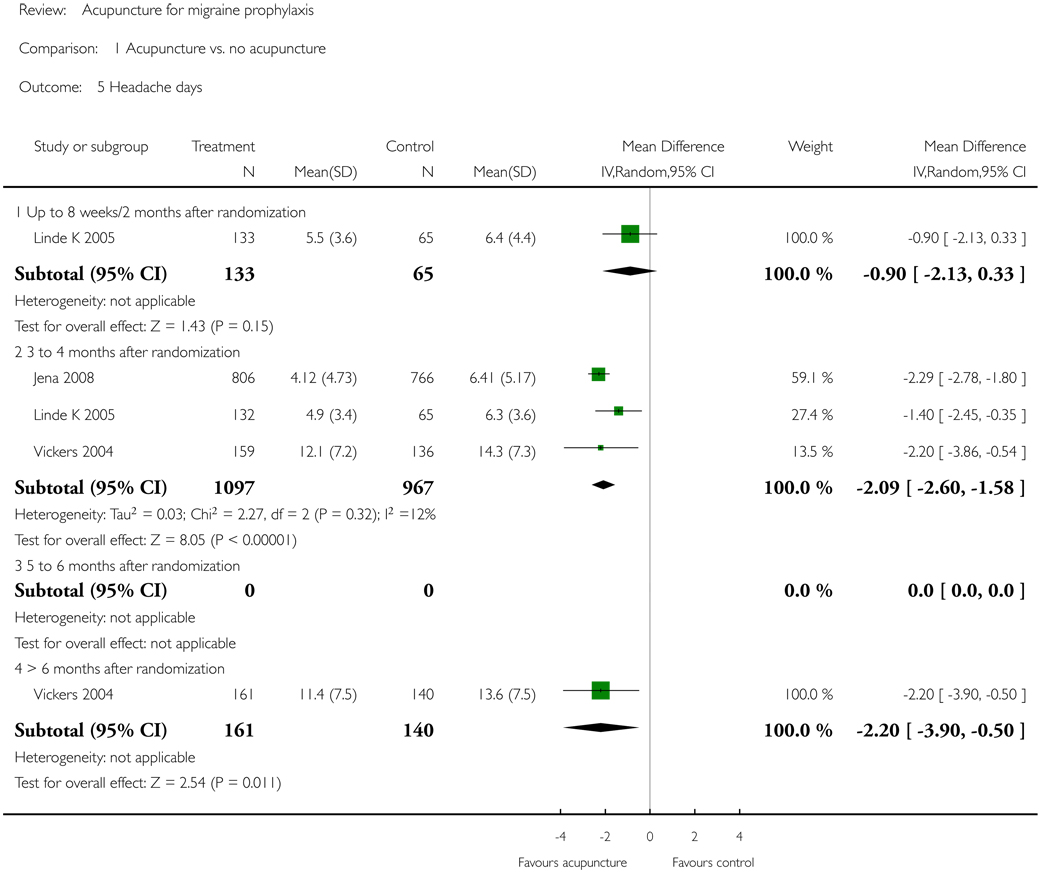
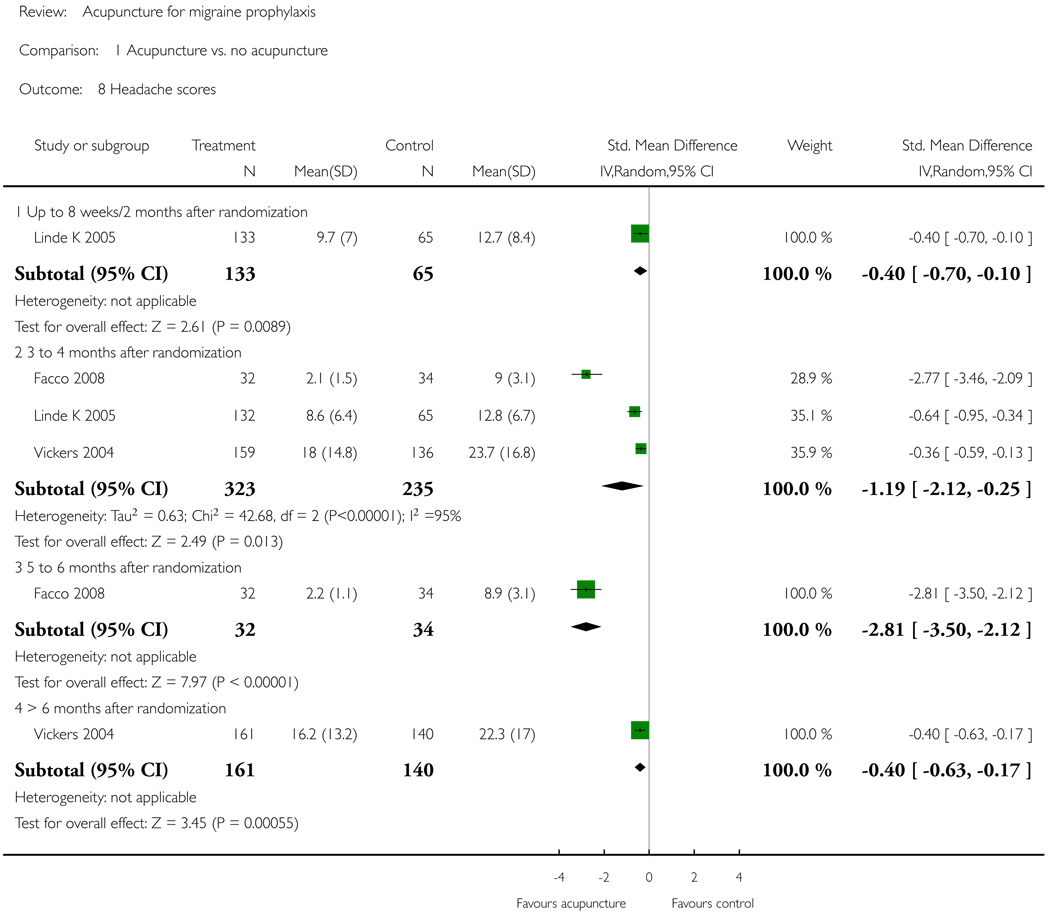
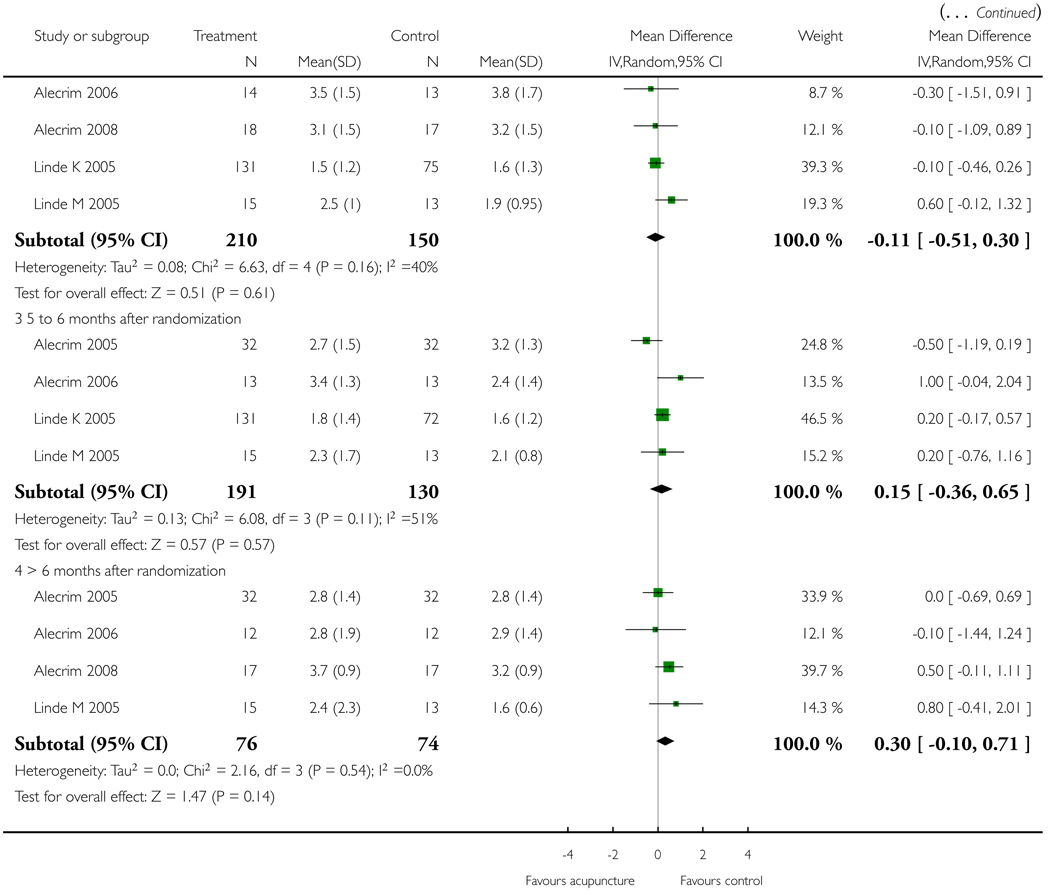
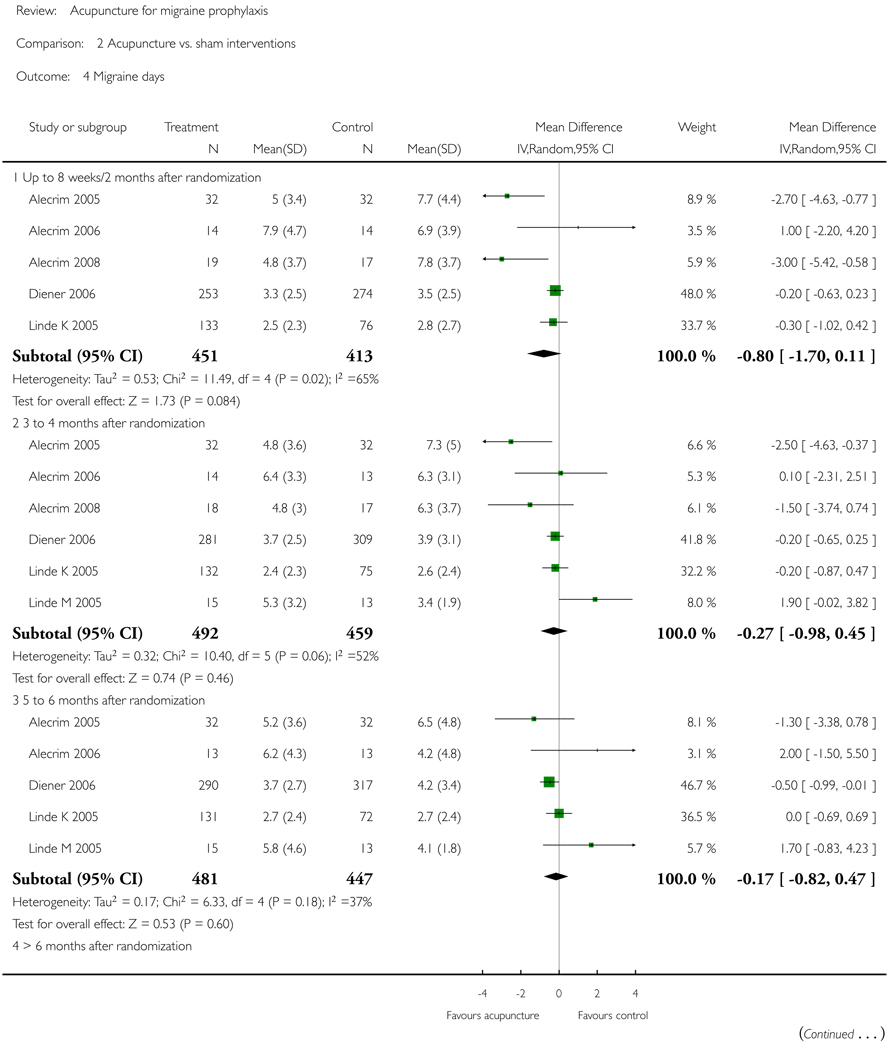
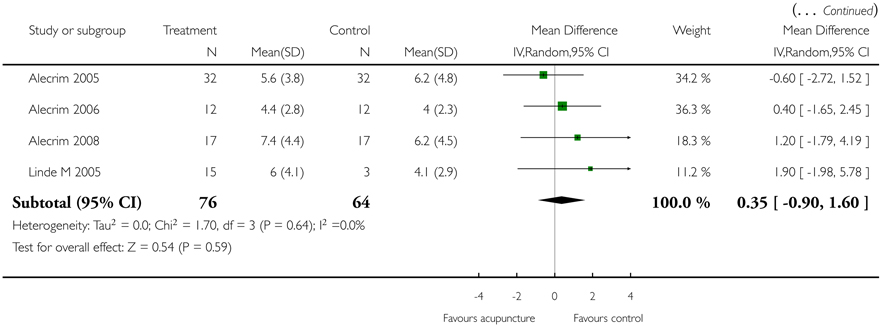
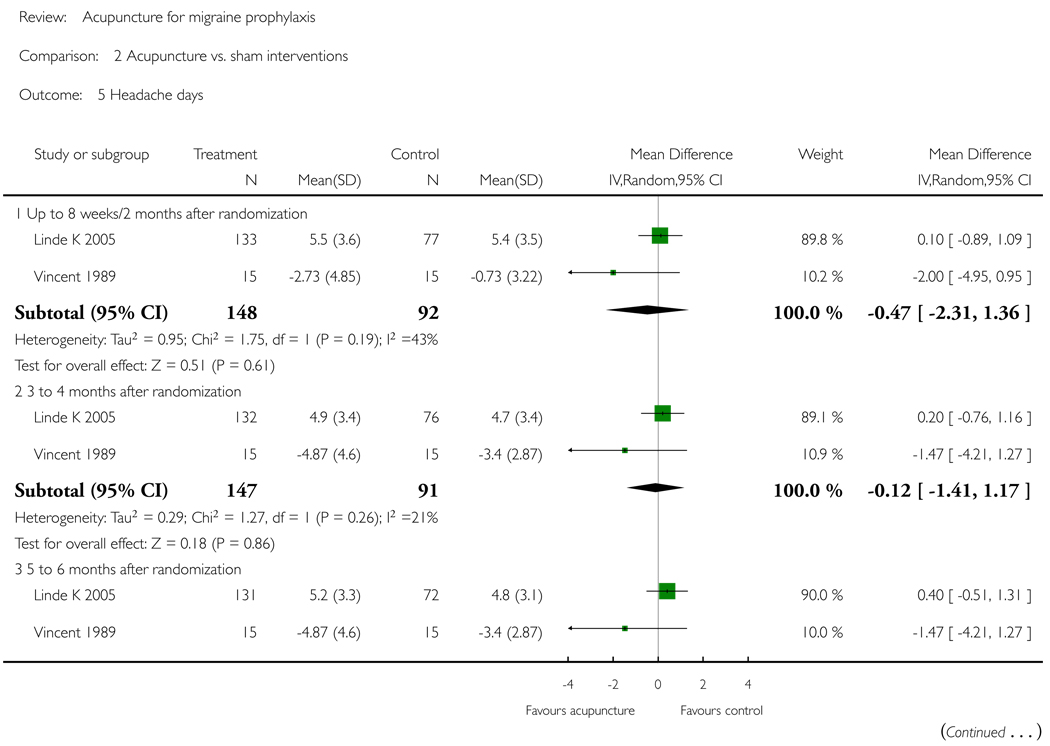
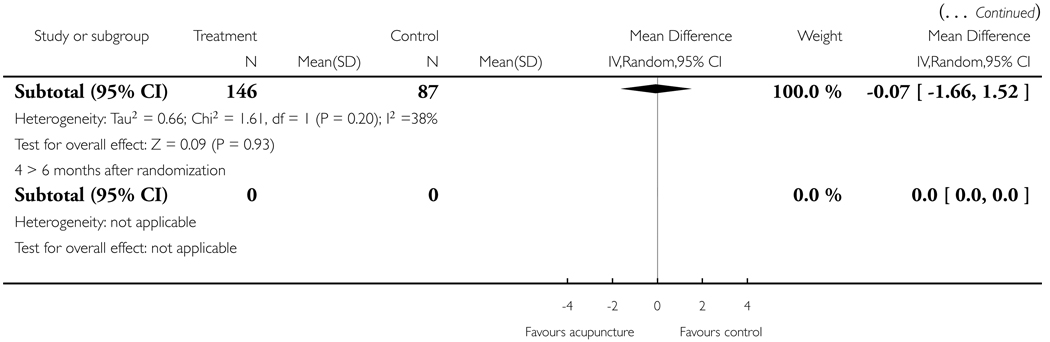
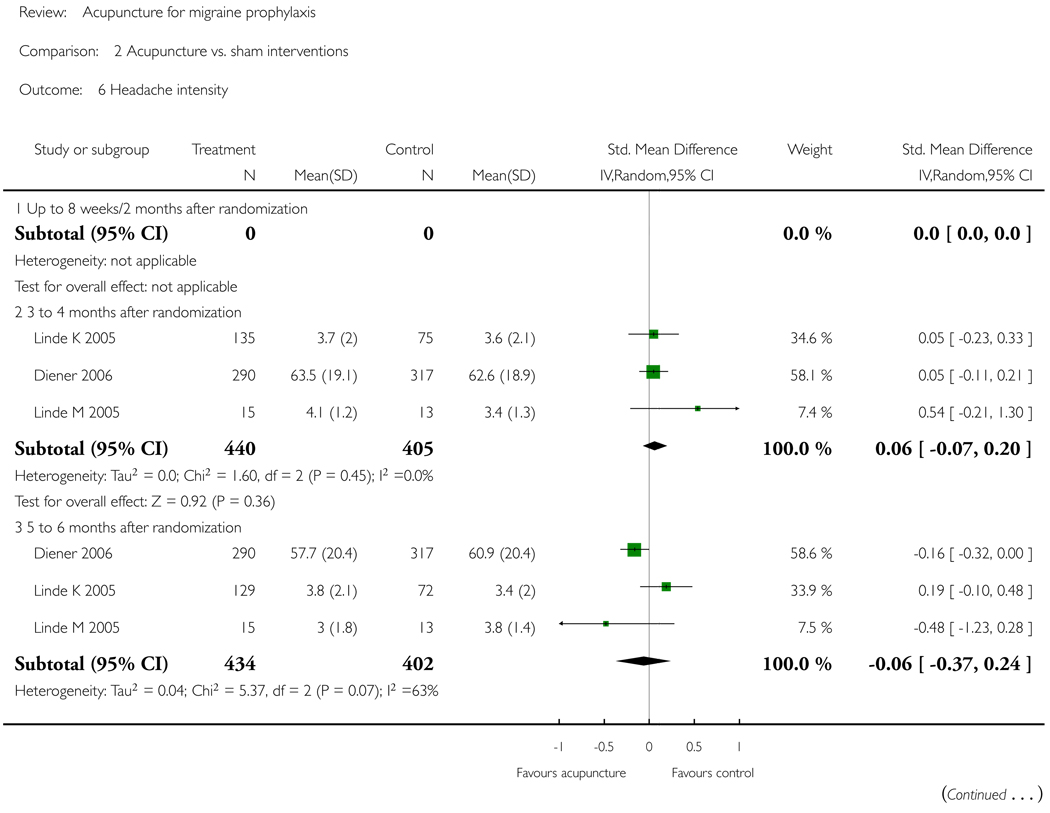
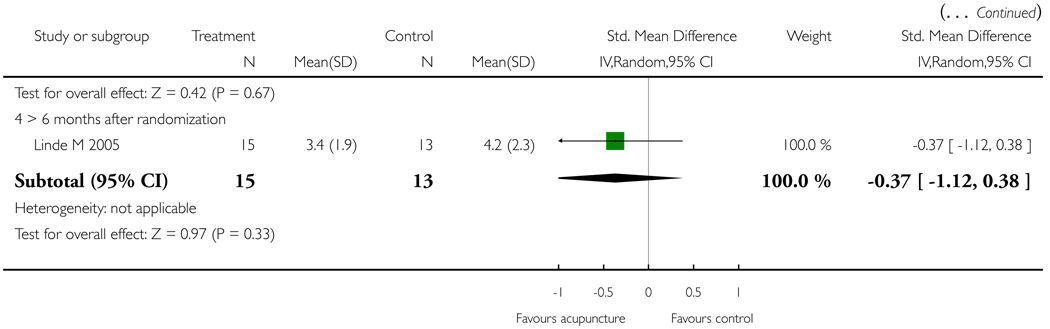
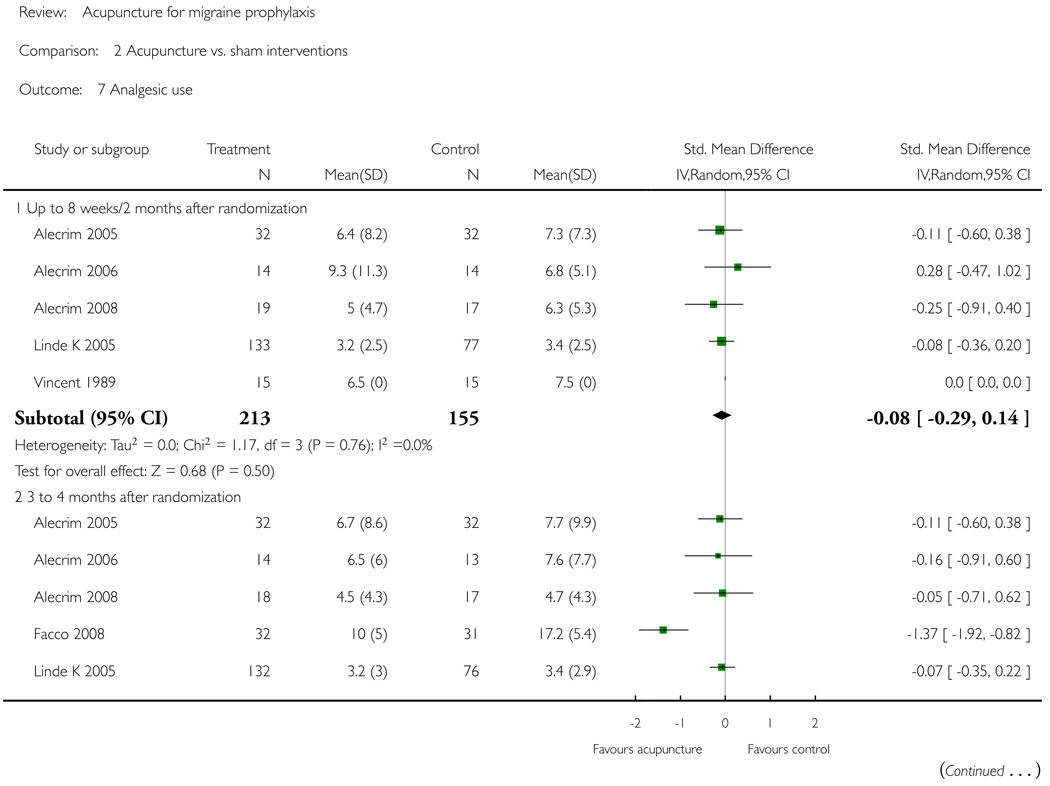
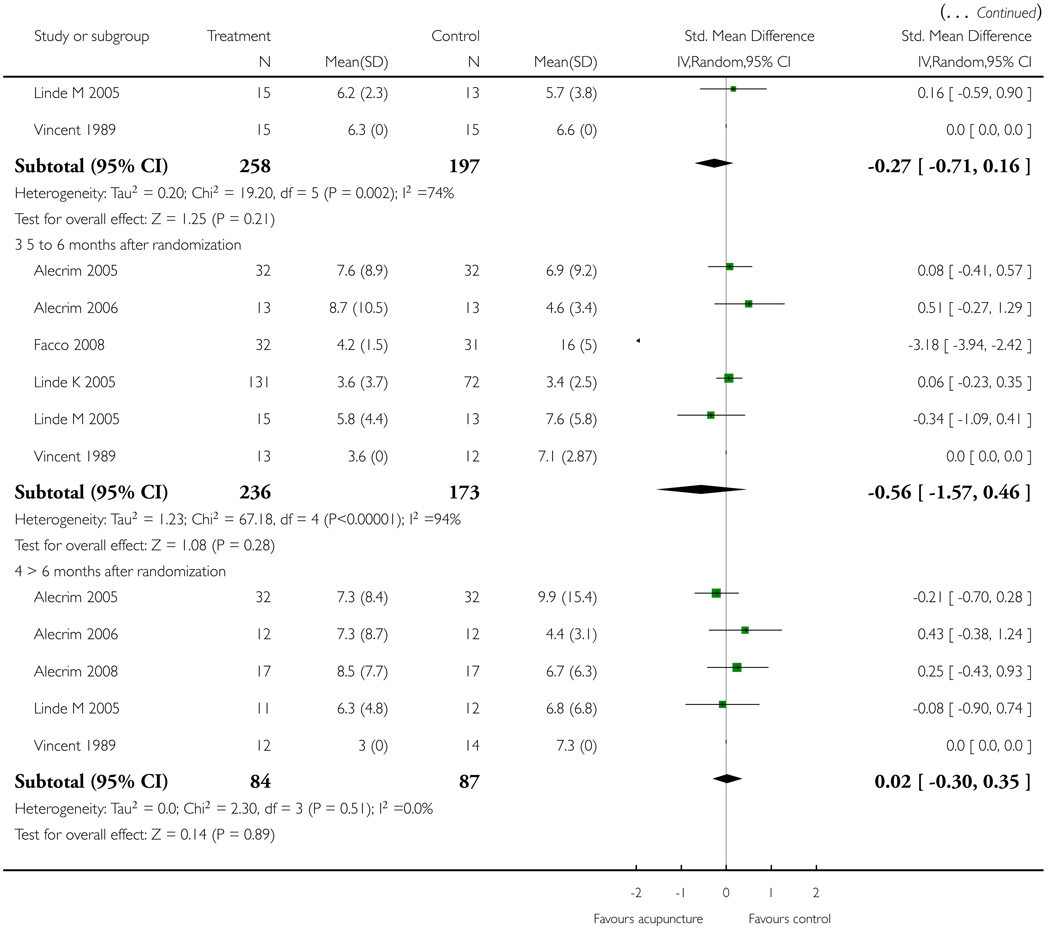
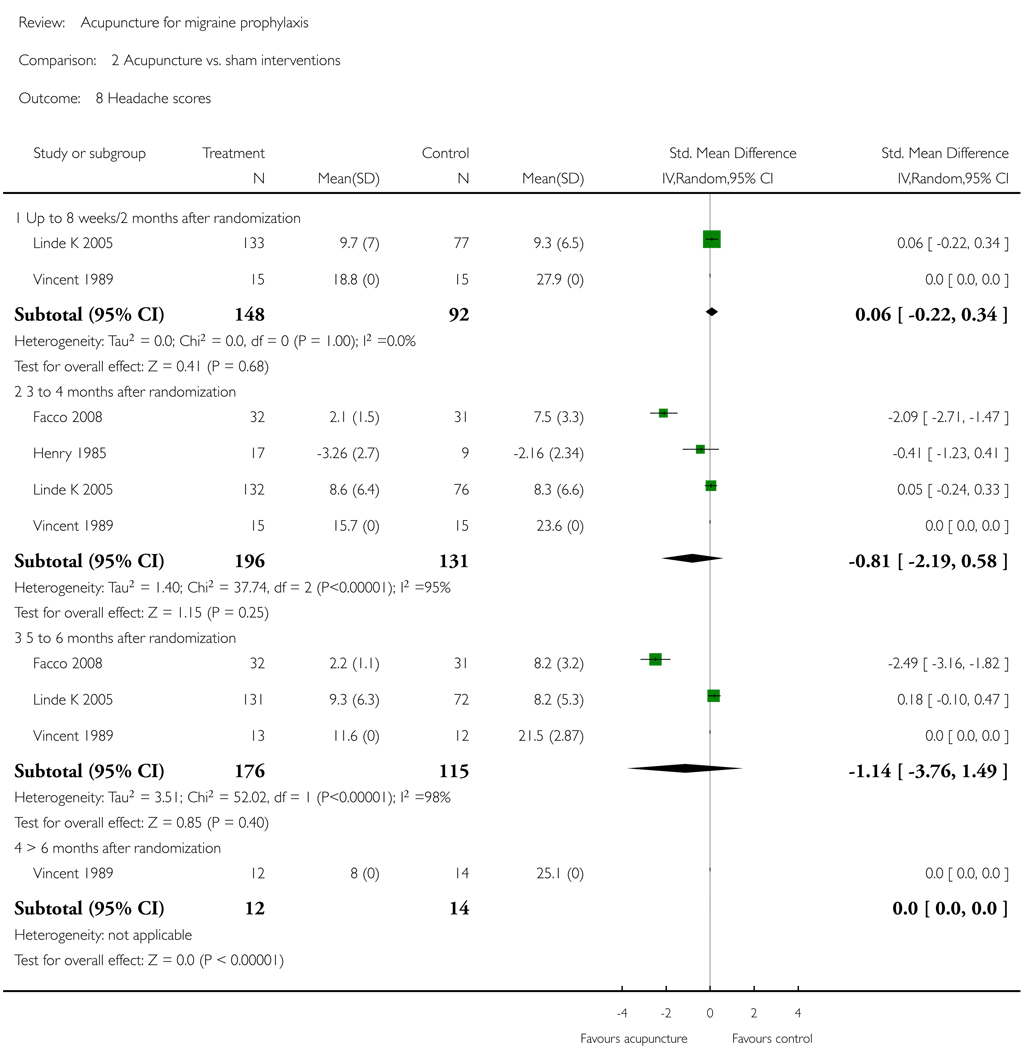
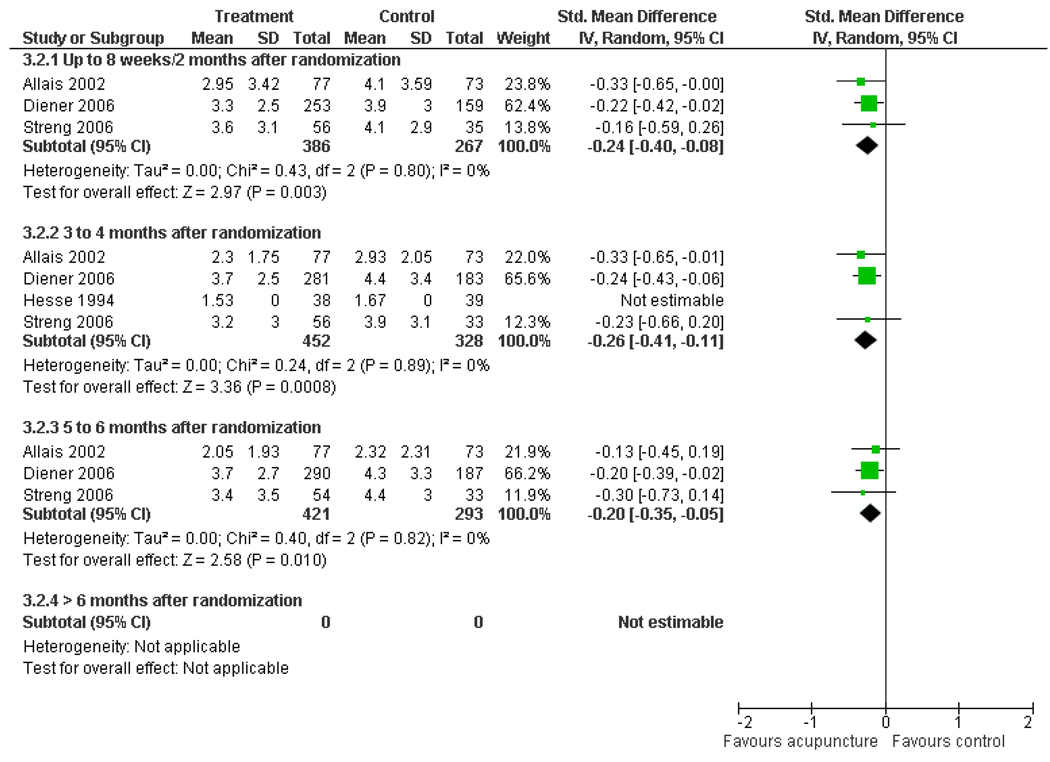
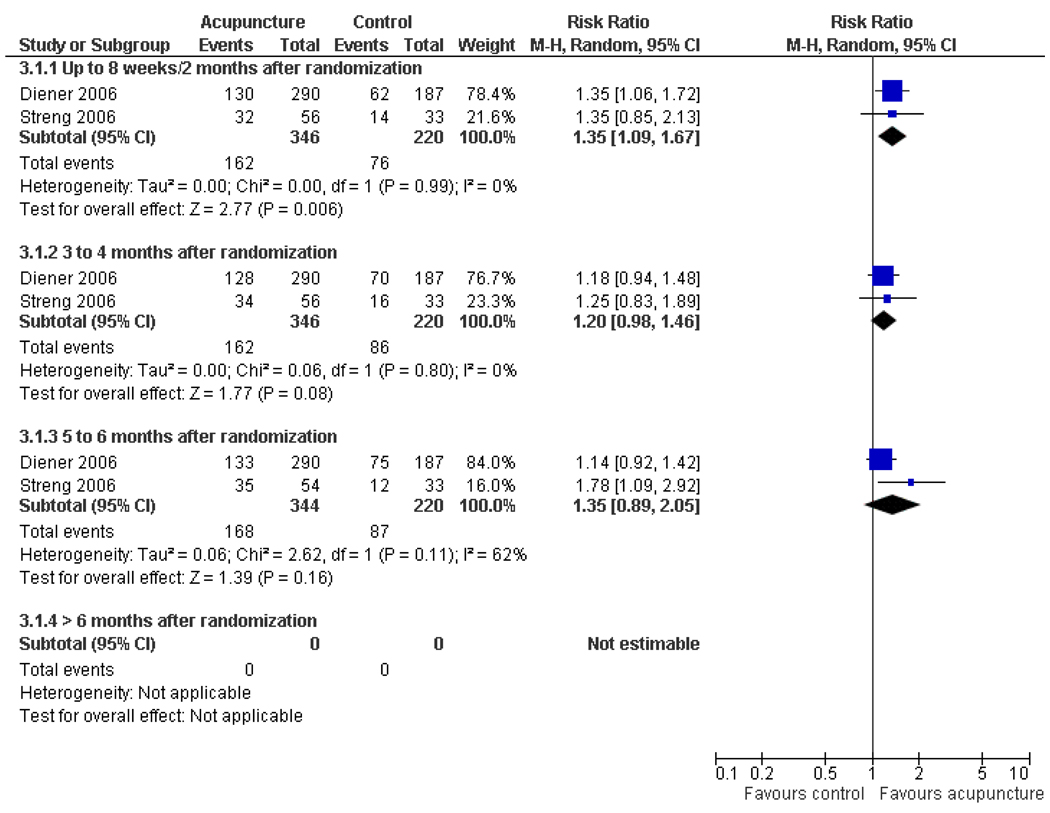
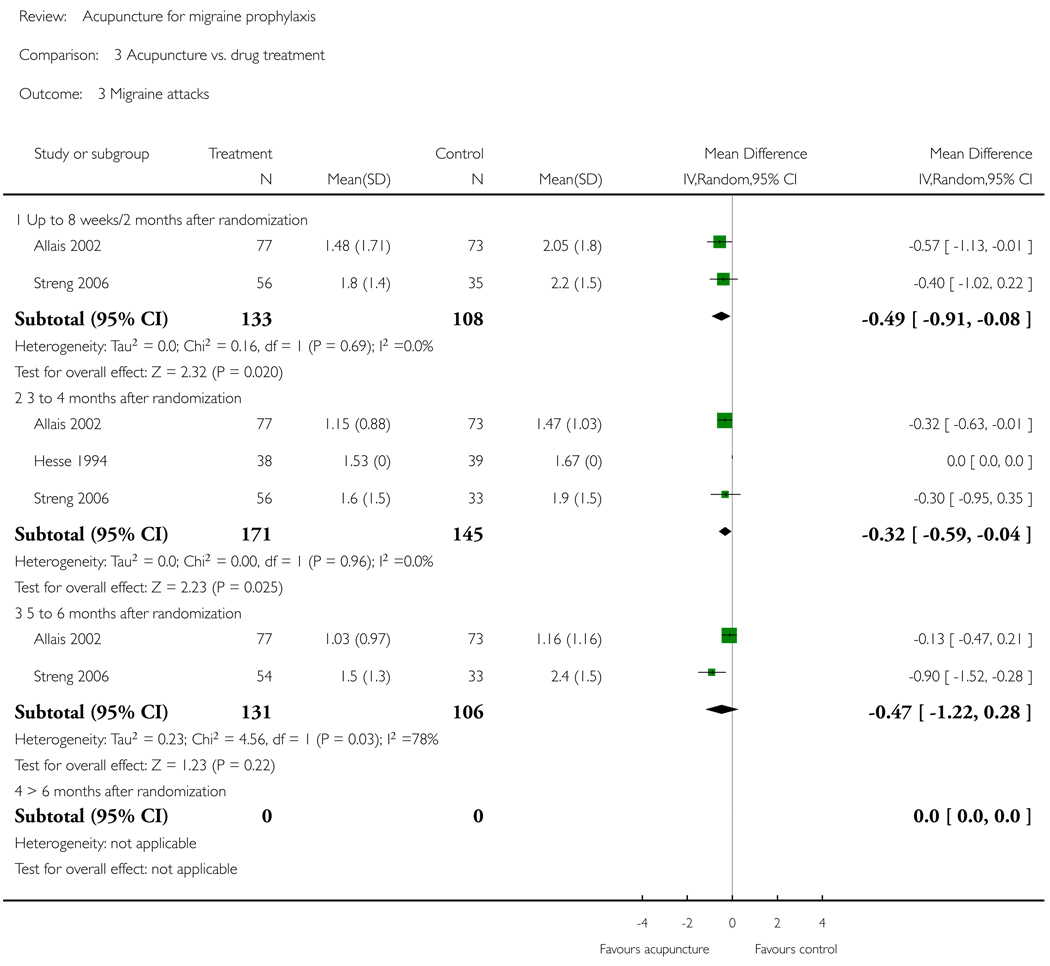
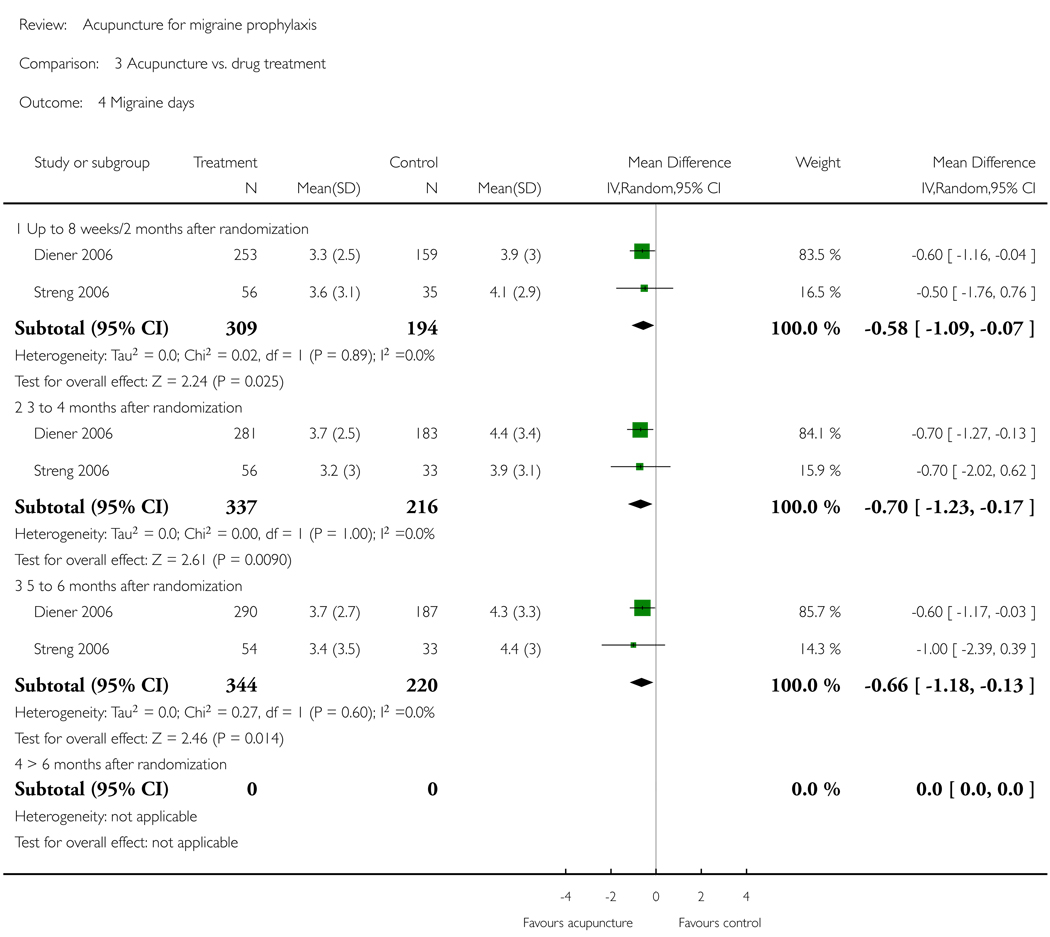
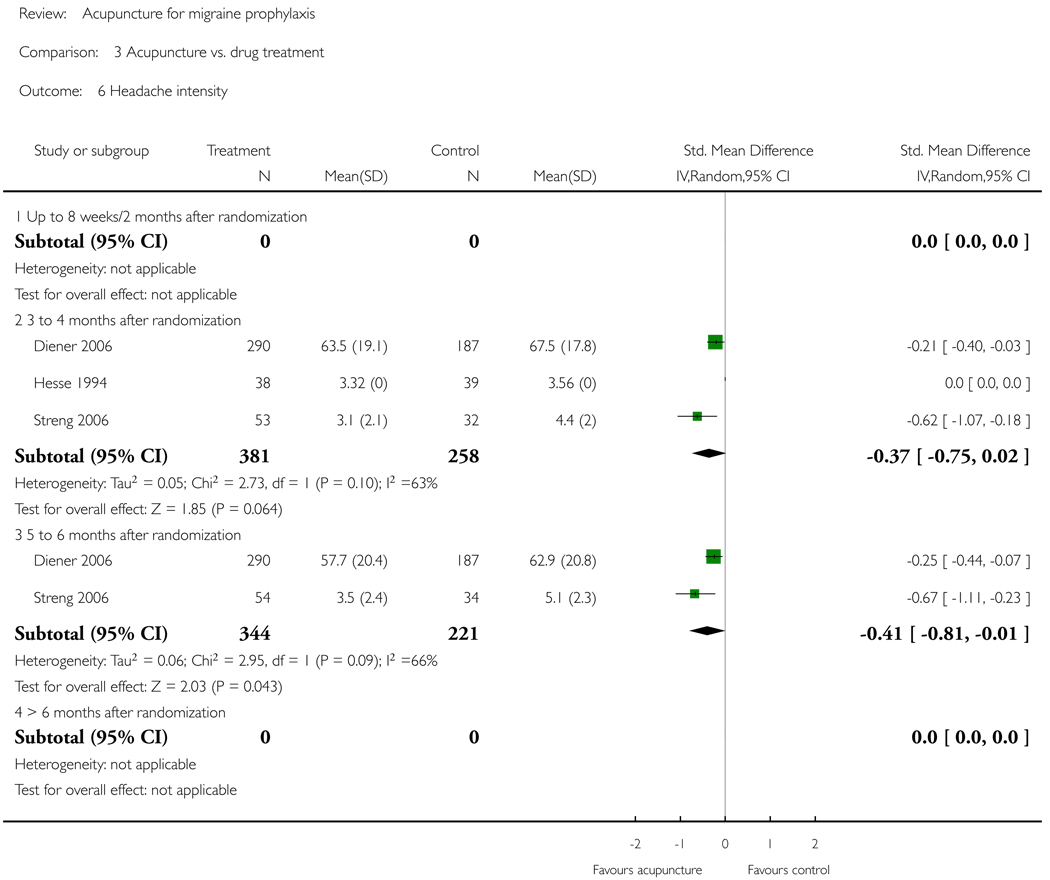
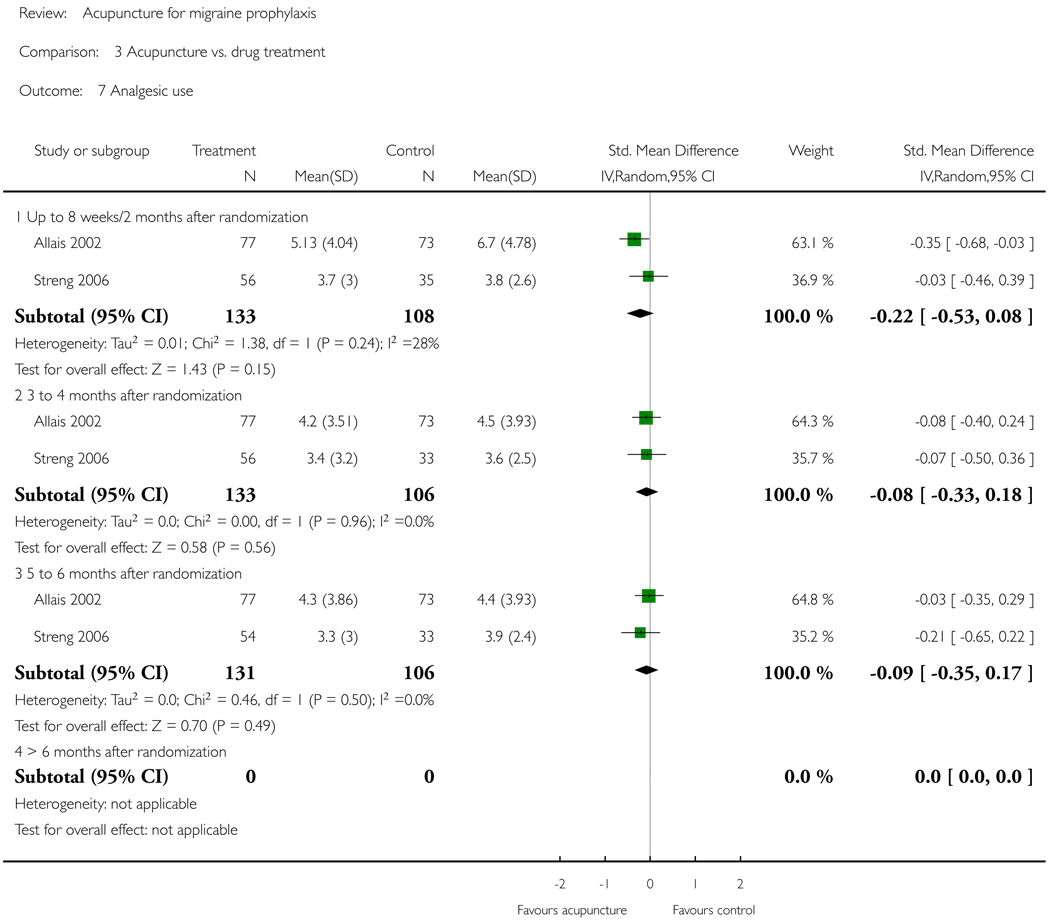
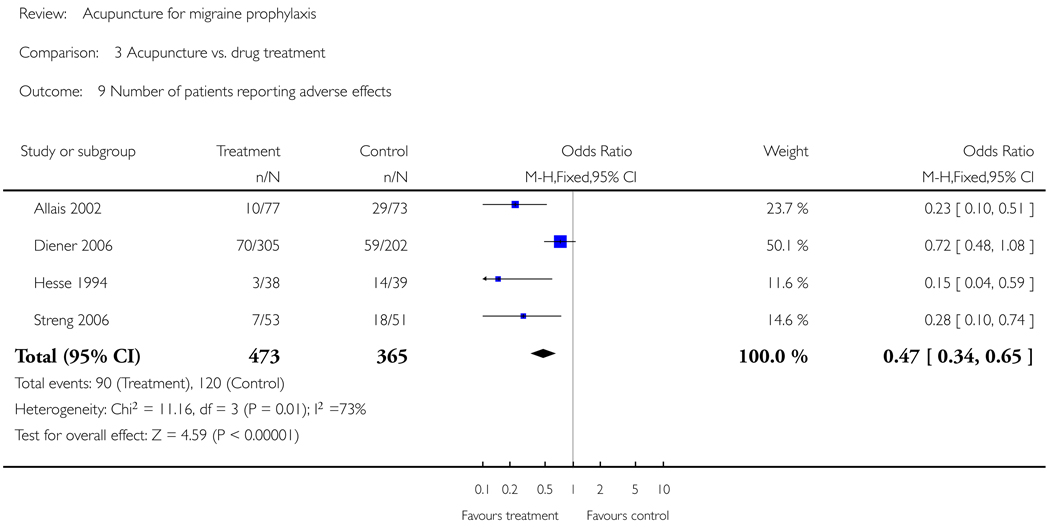
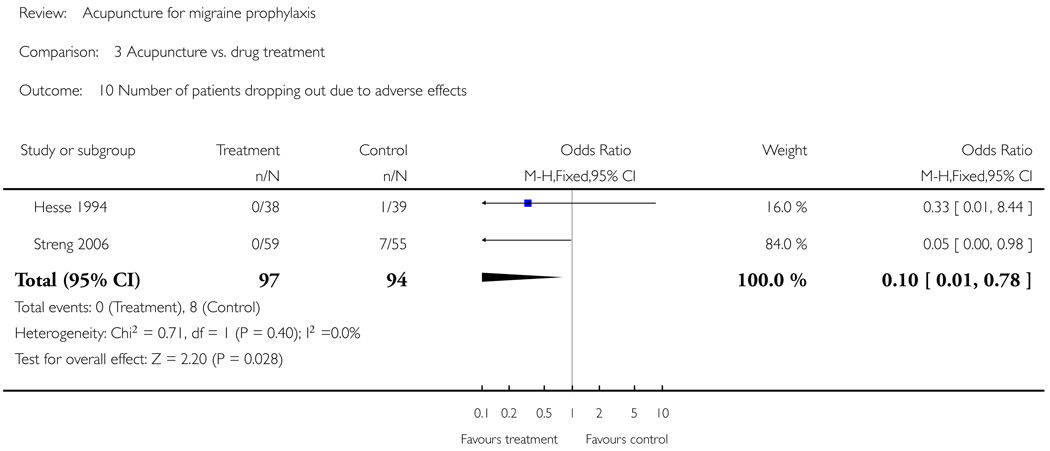
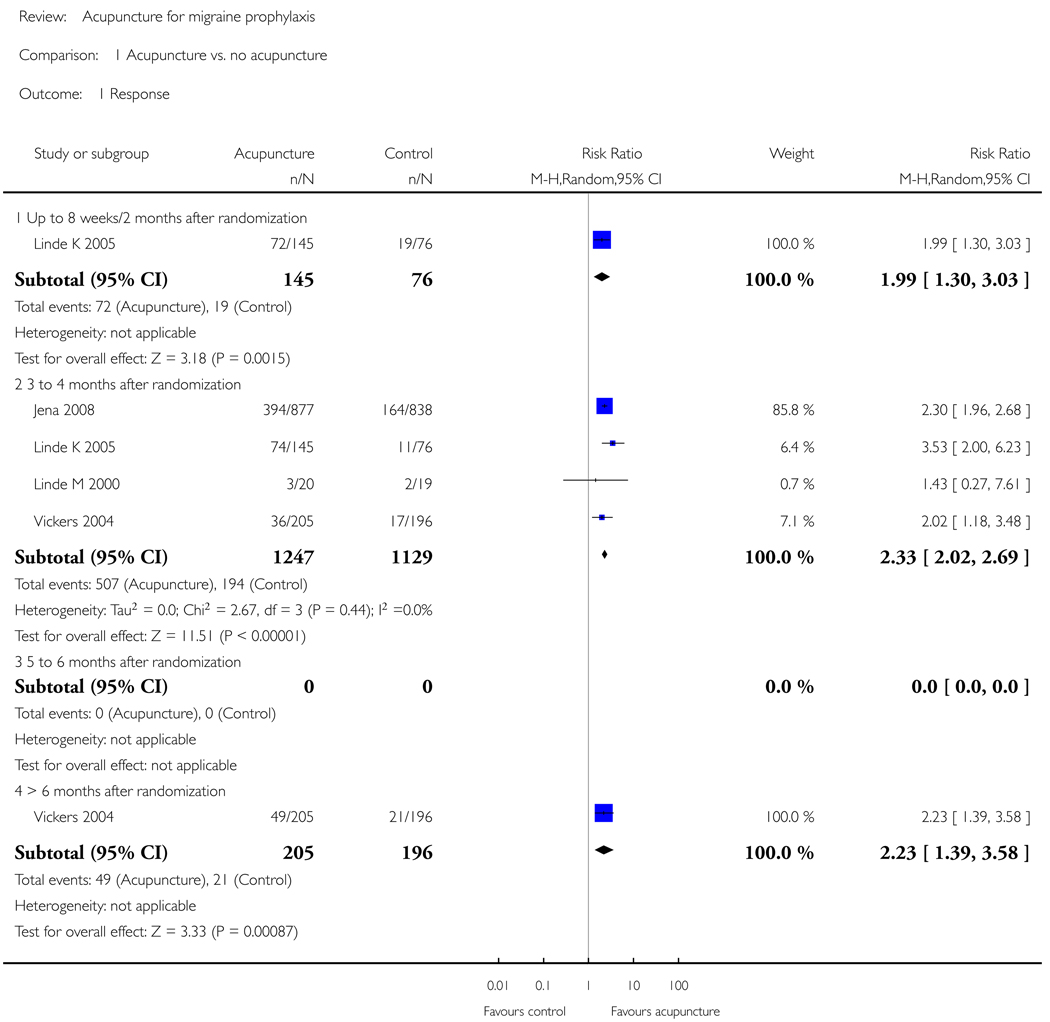
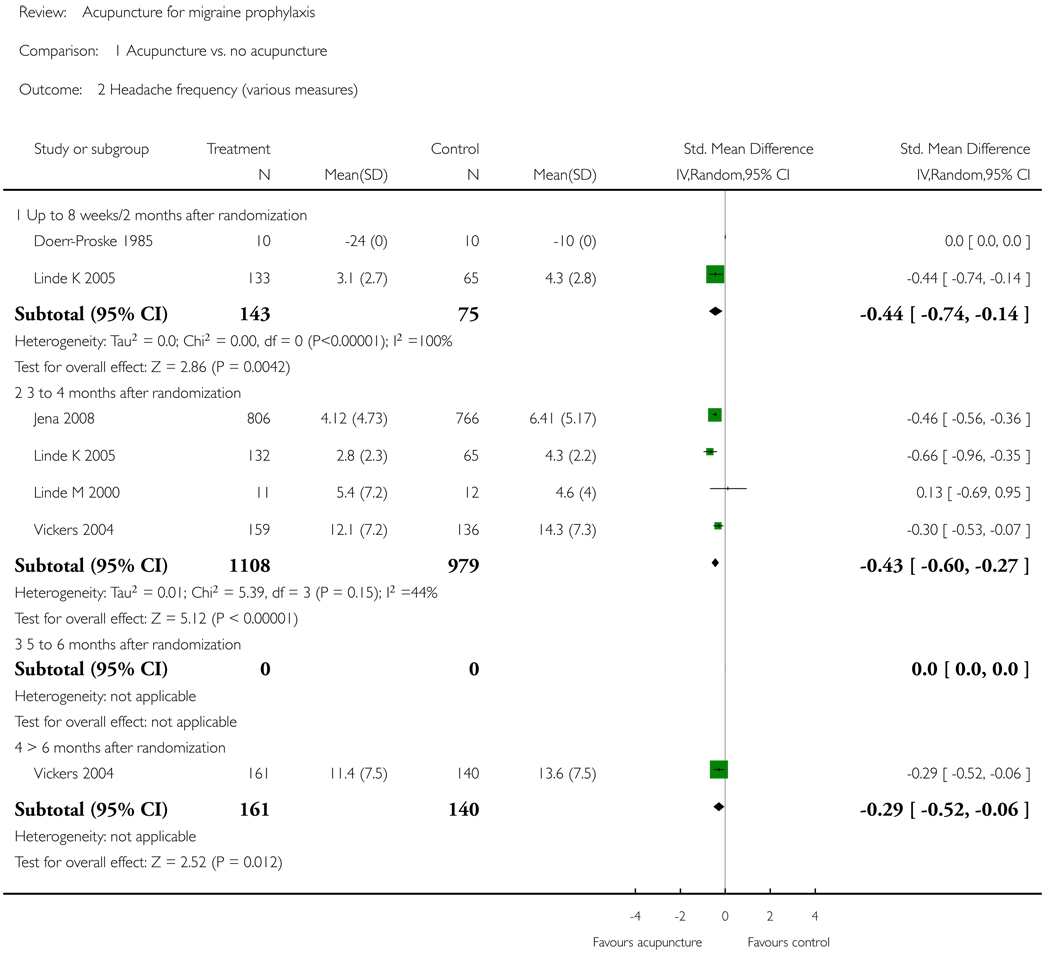
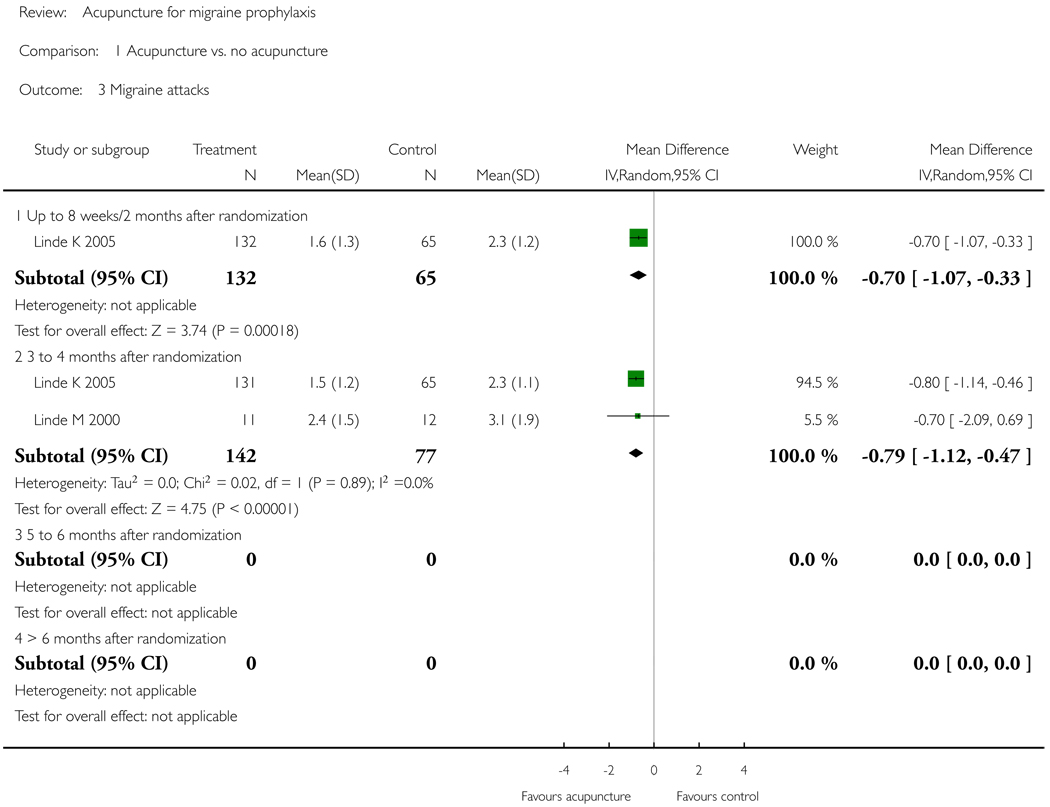
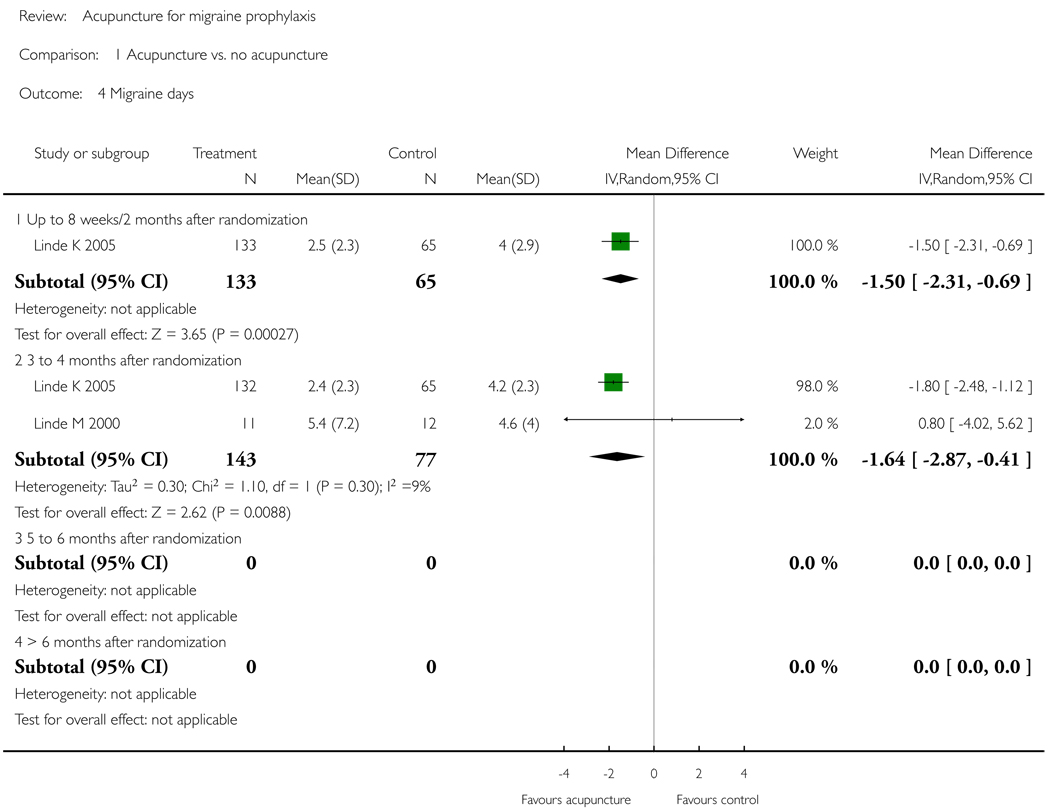
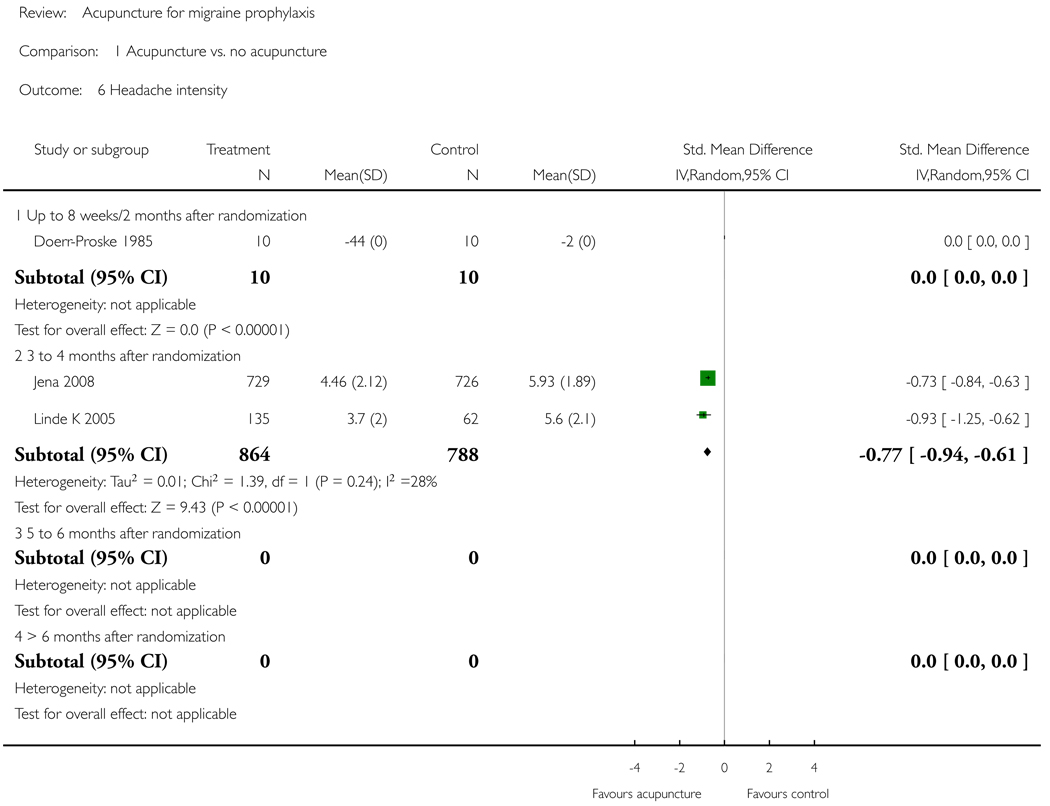
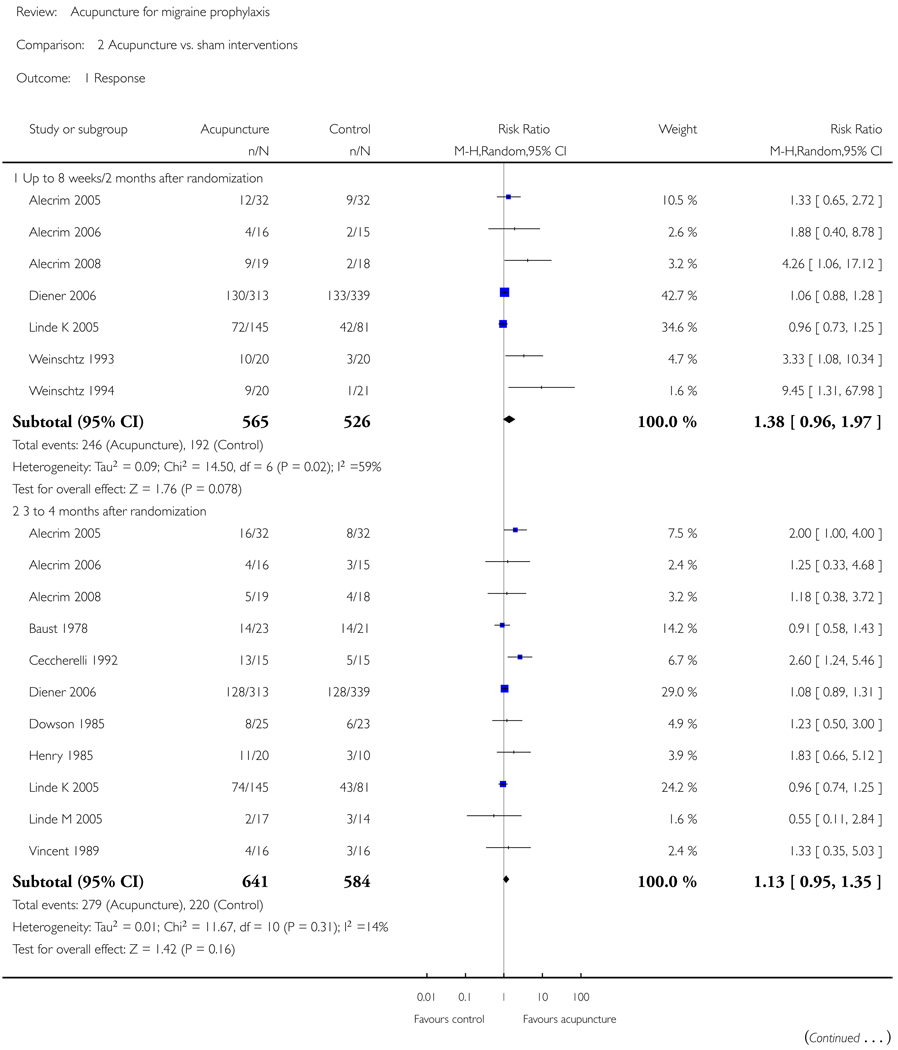
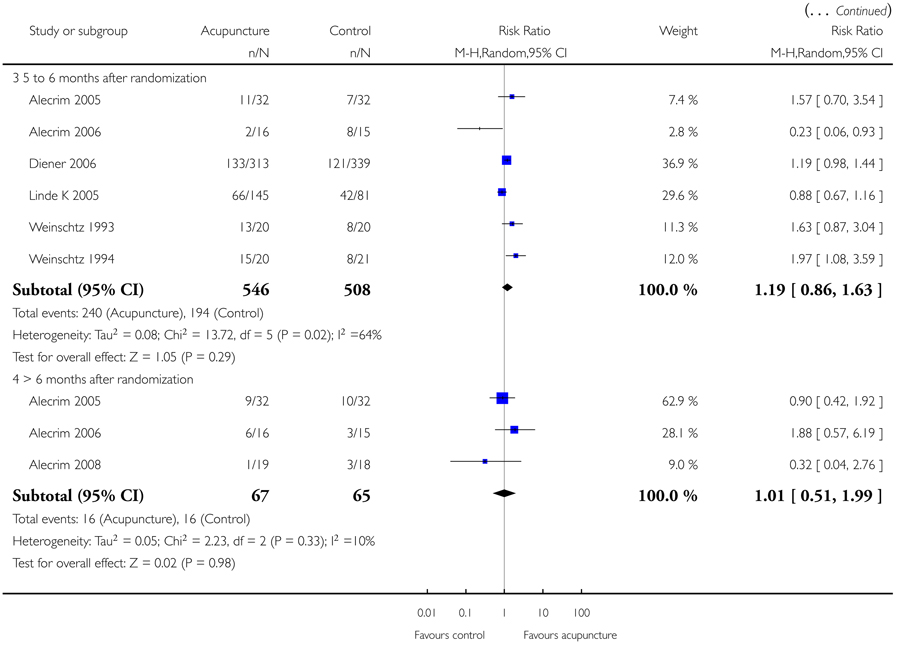
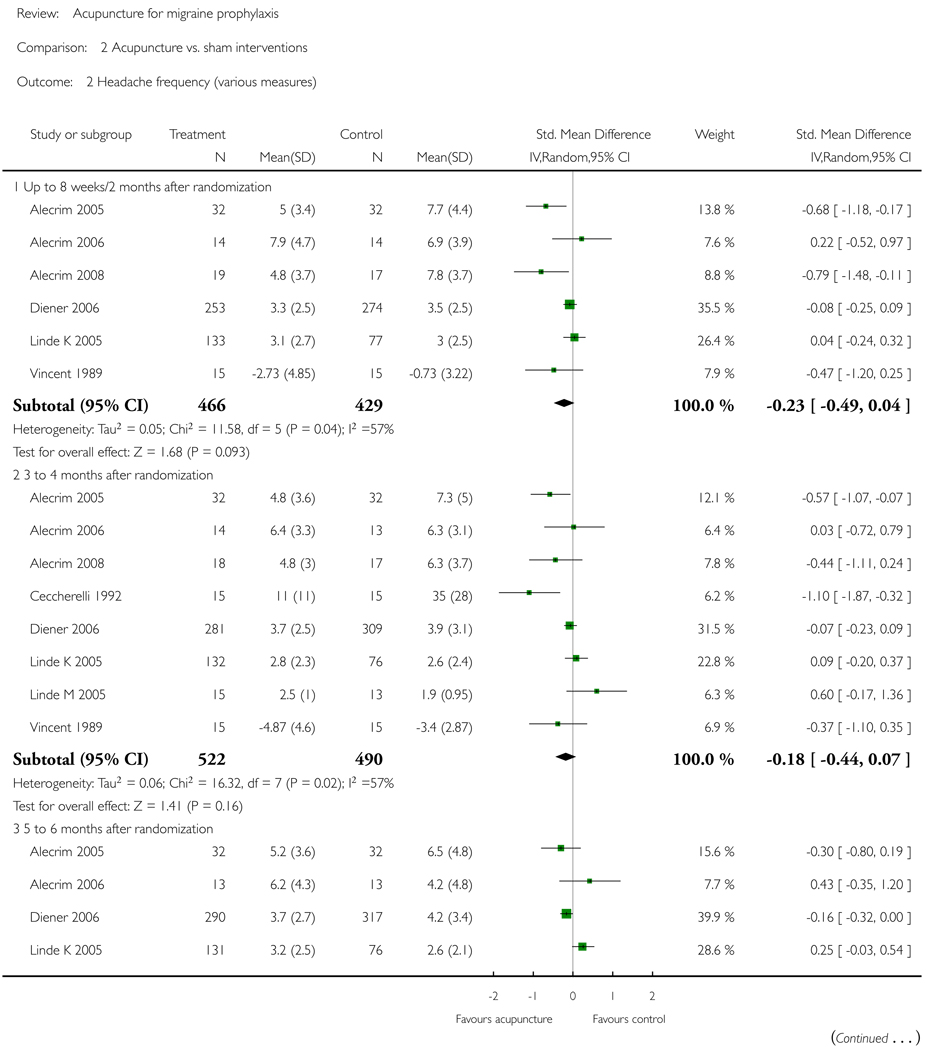
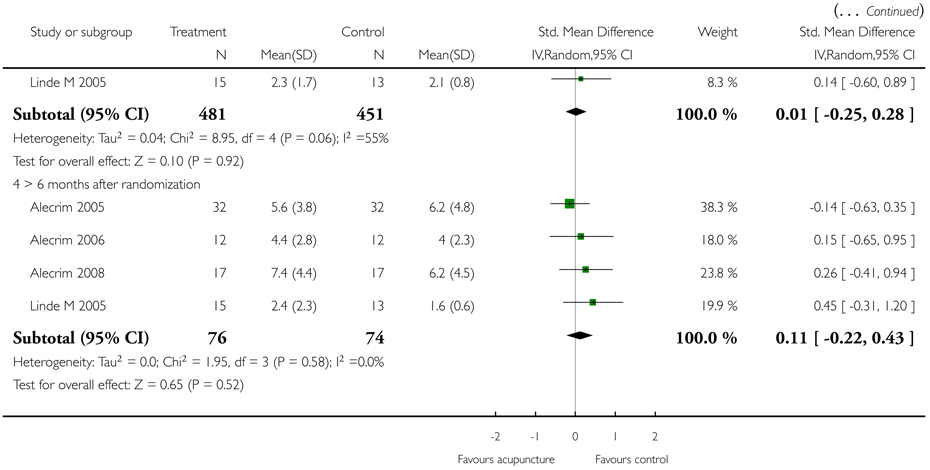
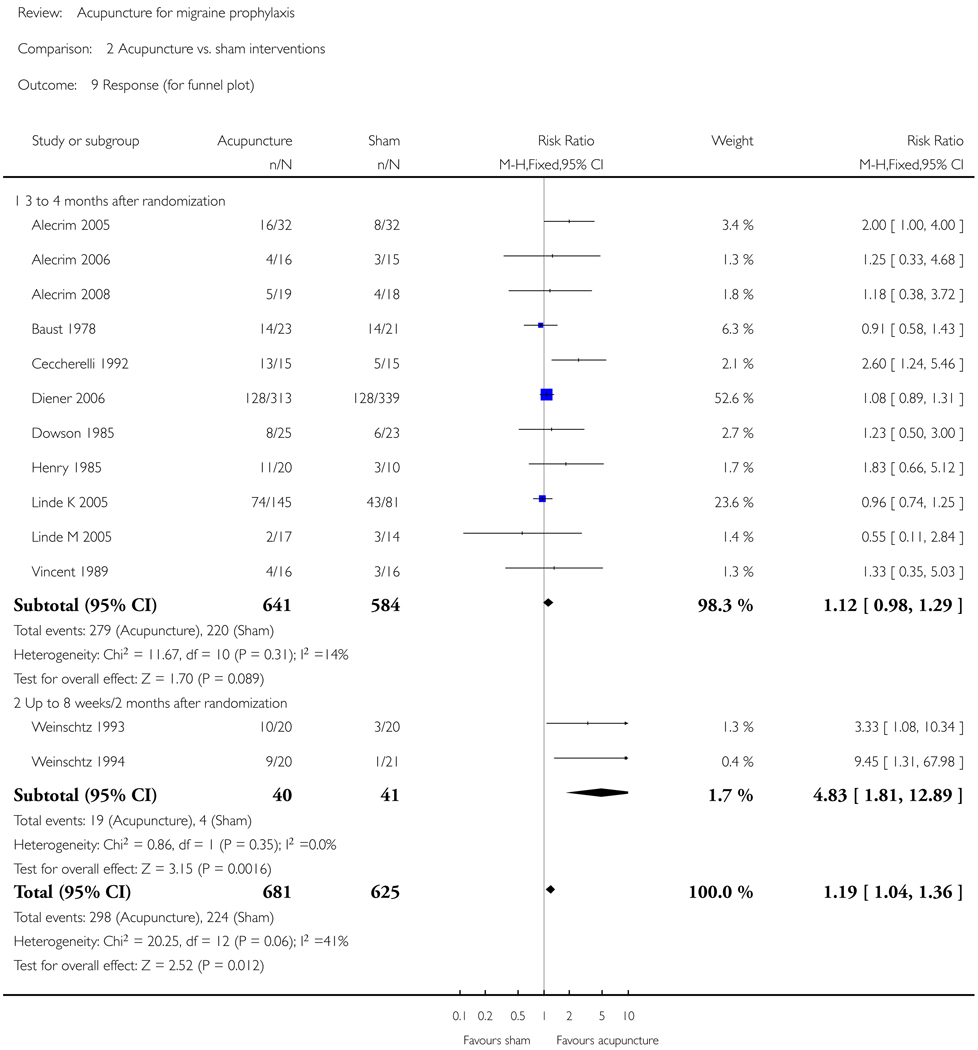
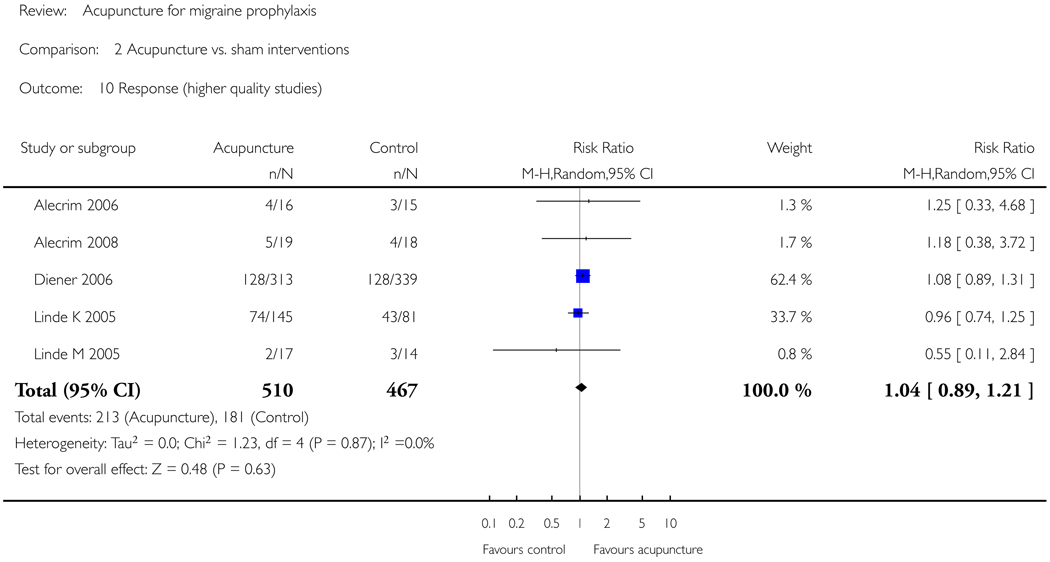
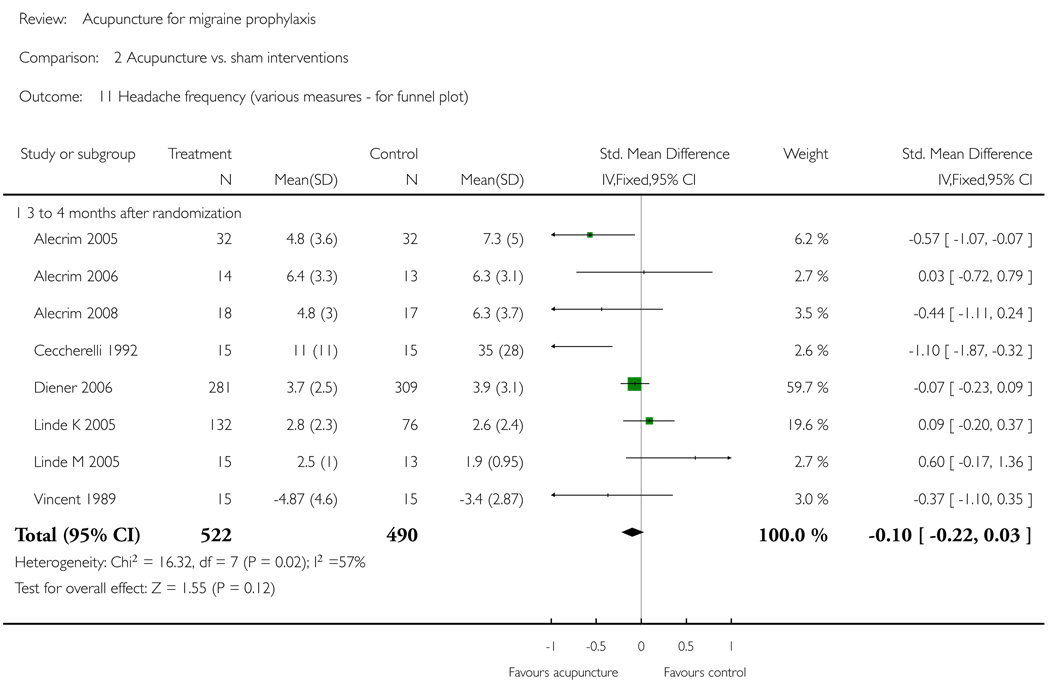
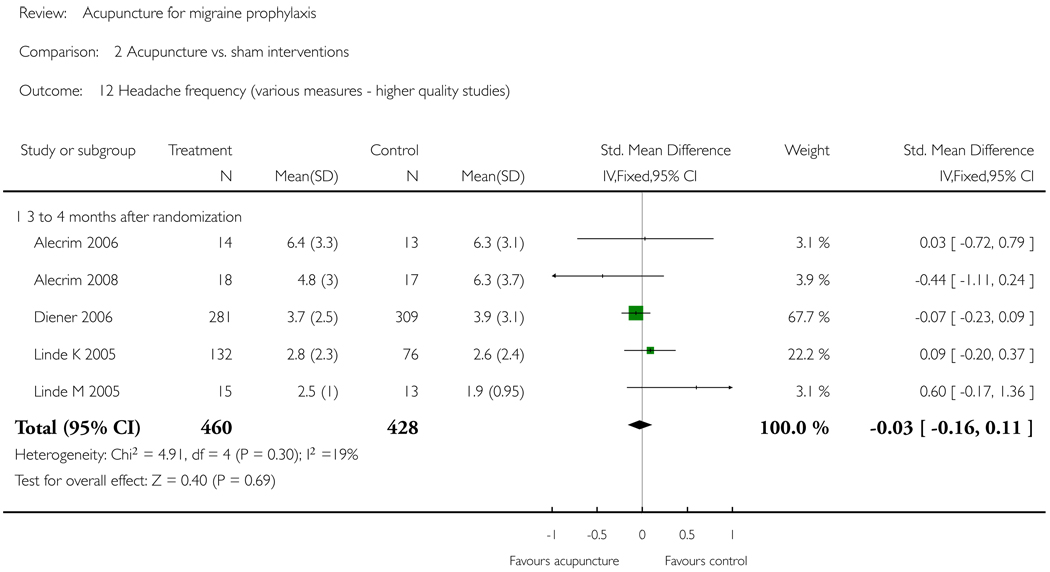
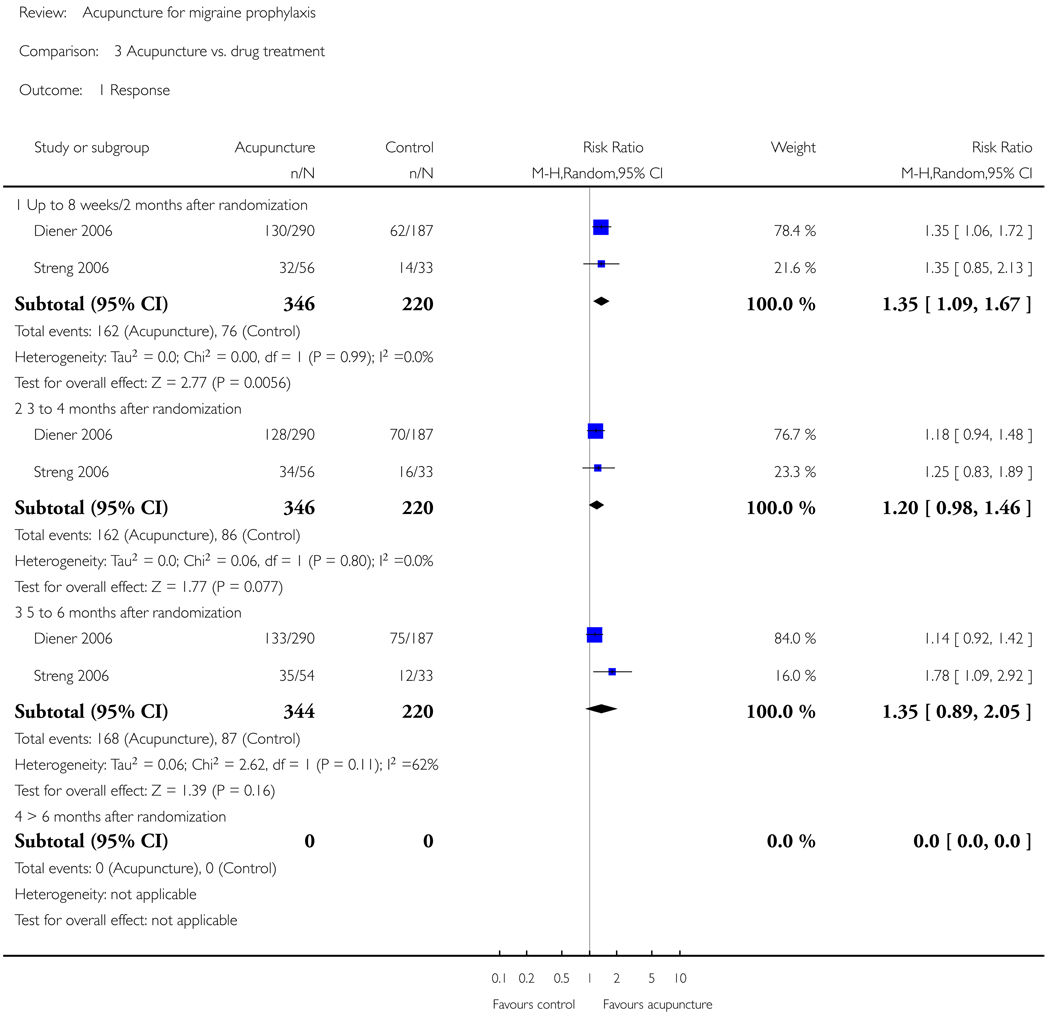
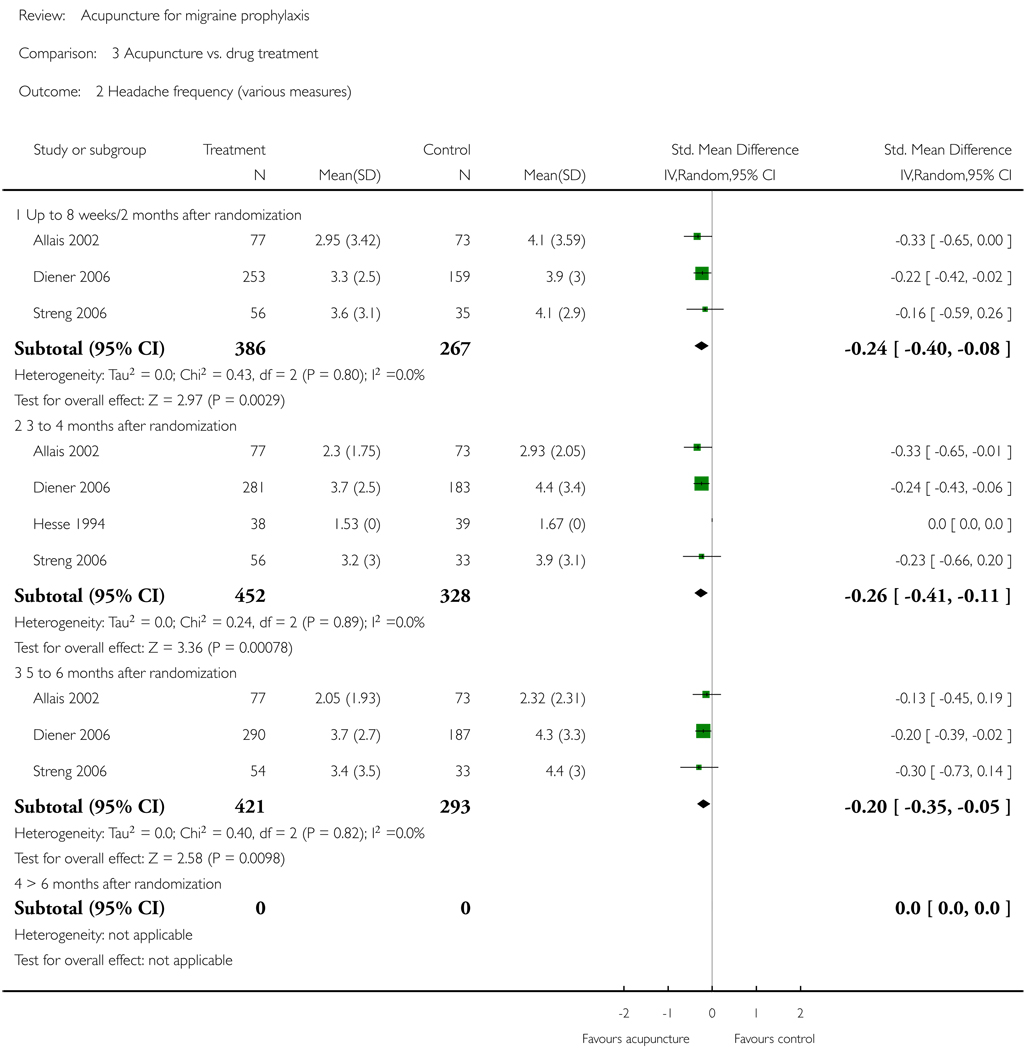
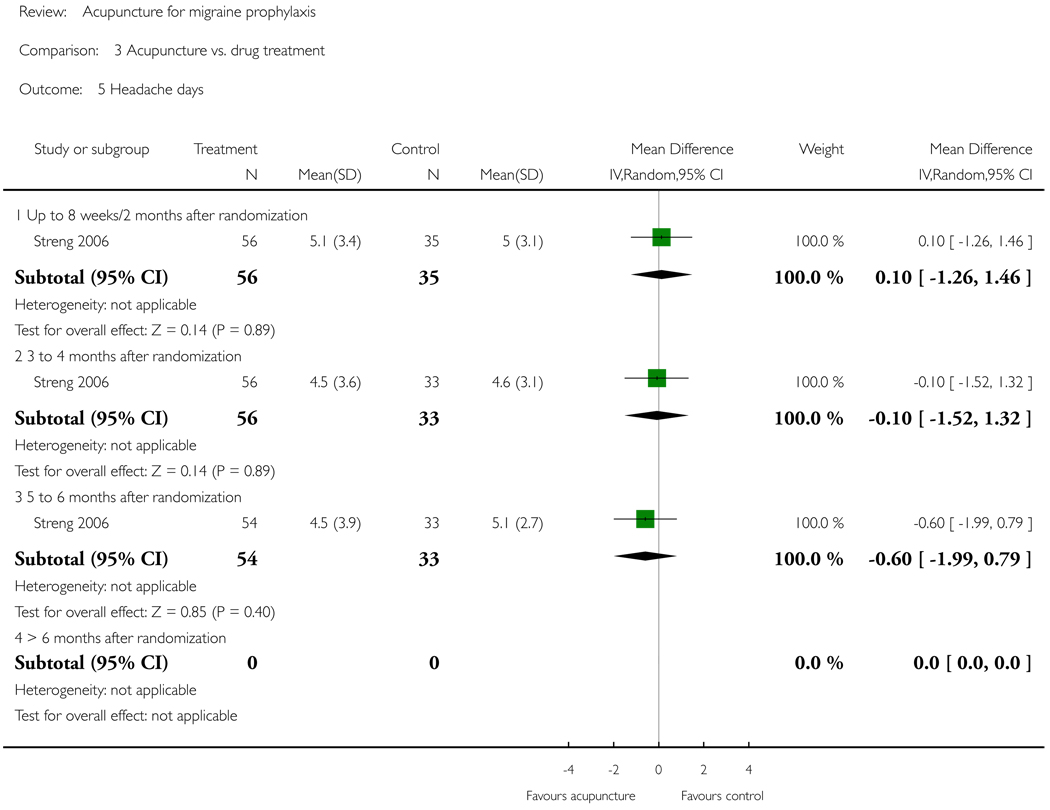
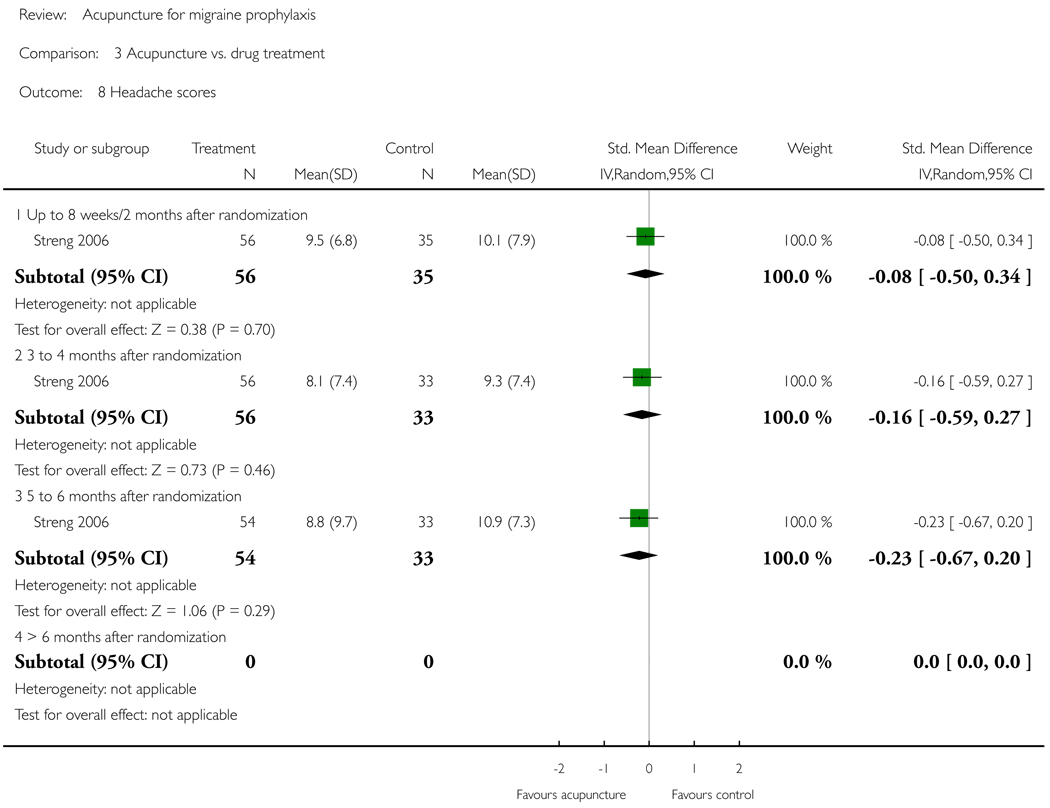
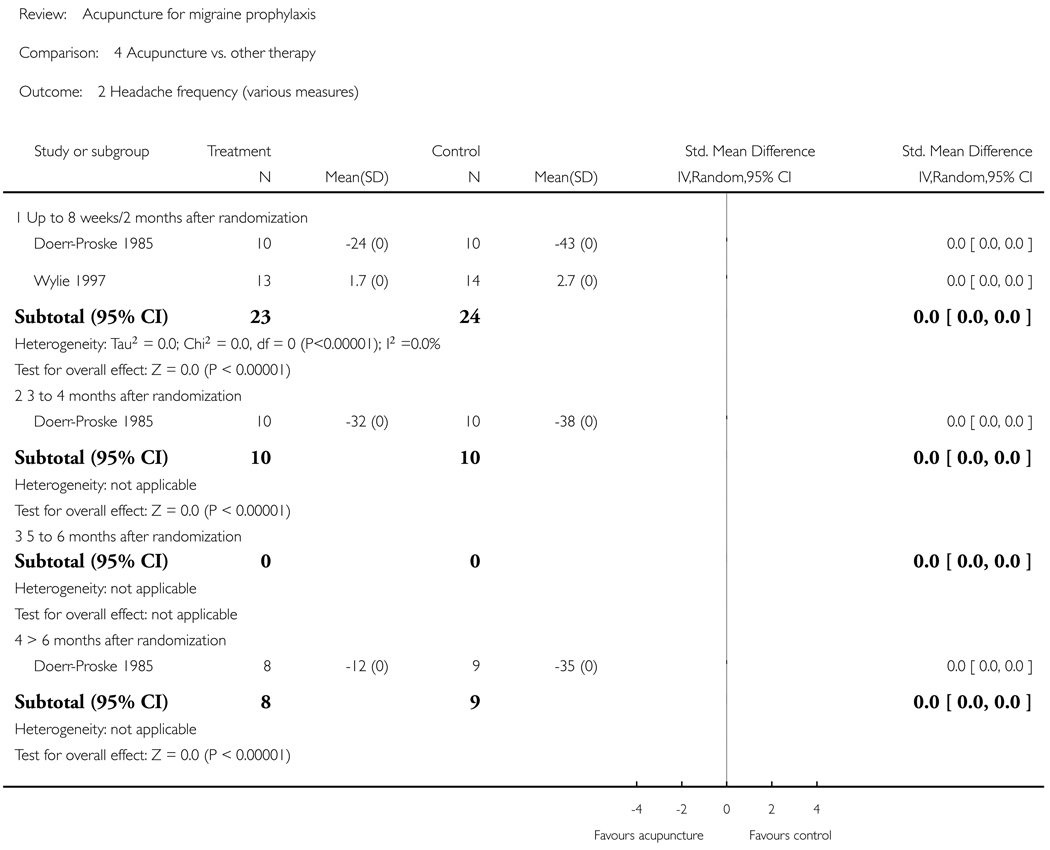
Twenty-two trials with 4419 participants (mean 201, median 42, range 27 to 1715) met the inclusion criteria. Six trials (including two large trials with 401 and 1715 patients) compared acupuncture to no prophylactic treatment or routine care only. After 3 to 4 months patients receiving acupuncture had higher response rates and fewer headaches. The only study with long-term follow up saw no evidence that effects dissipated up to 9 months after cessation of treatment. Fourteen trials compared a ’true’ acupuncture intervention with a variety of sham interventions. Pooled analyses did not show a statistically significant superiority for true acupuncture for any outcome in any of the time windows, but the results of single trials varied considerably. Four trials compared acupuncture to proven prophylactic drug treatment. Overall in these trials acupuncture was associated with slightly better outcomes and fewer adverse effects than prophylactic drug treatment. Two small low-quality trials comparing acupuncture with relaxation (alone or in combination with massage) could not be interpreted reliably.
Authors’ conclusions
In the previous version of this review, evidence in support of acupuncture for migraine prophylaxis was considered promising but insufficient. Now, with 12 additional trials, there is consistent evidence that acupuncture provides additional benefit to treatment of acute migraine attacks only or to routine care. There is no evidence for an effect of ’true’ acupuncture over sham interventions, though this is difficult to interpret, as exact point location could be of limited importance. Available studies suggest that acupuncture is at least as effective as, or possibly more effective than, prophylactic drug treatment, and has fewer adverse effects. Acupuncture should be considered a treatment option for patients willing to undergo this treatment.
Medical Subject Headings (MeSH): *Acupuncture Therapy, Migraine Disorders [*prevention & control], Randomized Controlled Trials as Topic
MeSH check words: Humans
PLAIN LANGUAGE SUMMARY
Acupuncture for migraine prophylaxis
Migraine patients suffer from recurrent attacks of mostly one-sided, severe headache. Acupuncture is a therapy in which thin needles are inserted into the skin at defined points; it originates from China. Acupuncture is used in many countries for migraine prophylaxis - that is, to reduce the frequency and intensity of migraine attacks.
We reviewed 22 trials which investigated whether acupuncture is effective in the prophylaxis of migraine. Six trials investigating whether adding acupuncture to basic care (which usually involves only treating acute headaches) found that those patients who received acupuncture had fewer headaches. Fourteen trials compared true acupuncture with inadequate or fake acupuncture interventions in which needles were either inserted at incorrect points or did not penetrate the skin. In these trials both groups had fewer headaches than before treatment, but there was no difference between the effects of the two treatments. In the four trials in which acupuncture was compared to a proven prophylactic drug treatment, patients receiving acupuncture tended to report more improvement and fewer side effects. Collectively, the studies suggest that migraine patients benefit from acupuncture, although the correct placement of needles seems to be less relevant than is usually thought by acupuncturists.
BACKGROUND
Description of the condition
Migraine is a disorder with recurrent headaches manifesting in attacks lasting 4 to 72 hours. Typical characteristics of the headache are unilateral location, pulsating quality, moderate or severe intensity, aggravation by routine physical activity and association with nausea and/or photophobia and phonophobia (IHS 2004). Epidemiological studies have consistently shown that migraine is a common disorder with a 1-year prevalence of around 10% to 12% and a lifetime prevalence of between 15% and 20% (Oleson 2007). In Europe, the economic cost of migraine is estimated at 27 billion Euro per year (Andlin-Sobocki 2005). Most migraine patients can be adequately treated with treatment of acute headaches alone, but a relevant minority need prophylactic interventions, as their attacks are either too frequent or are insufficiently controlled by acute therapy. Several drugs, such as propranolol, metoprolol, flunarizine, valproic acid and topiramate, have been shown to effectively reduce attack frequency in some patients (Dodick 2007). However, all these drugs are associated with adverse effects. Dropout rates in most clinical trials are high, suggesting that the drugs are not well accepted by patients. There is some evidence that behavioral interventions such as relaxation or biofeedback are beneficial (Holroyd 1990; Nestoriuc 2007), but additional effective, low-risk treatments are clearly desirable.
Description of the intervention
Acupuncture in the context of this review is defined as the needling of specific points of the body. It is one of the most widely used complementary therapies in many countries (Bodeker 2005). For example, according to a population-based survey in the year 2002 in the United States, 4.1% of respondents reported lifetime use of acupuncture, and 1.1% recent use (Burke 2006). A similar survey in Germany performed in the same year found that 8.7% of adults between 18 and 69 years of age had received acupuncture treatment in the previous 12 months (Härtel 2004). Acupuncture was originally developed as part of Chinese medicine wherein the purpose of treatment is to bring the patient back to the state of equilibrium postulated to exist prior to illness (Endres 2007). Some acupuncture practitioners have dispensed with these concepts and understand acupuncture in terms of conventional neurophysiology. Acupuncture is often used to treat headache, especially migraine. For example, 9.9% of the acupuncture users in the U.S. survey mentioned above stated that they had been treated for migraine or other headaches (Burke 2006). Practitioners typically claim that a short course of treatment, such as 12 sessions over a 3-month period, can have a long-term impact on the frequency and intensity of headache episodes.
How the intervention might work
Multiple studies have shown that acupuncture has short-term effects on a variety of physiological variables relevant to analgesia (Bäcker 2004; Endres 2007). However, it is unclear to what extent these observations from experimental settings are relevant to the long-term effects reported by practitioners. It is assumed that a variable combination of peripheral effects; spinal and supraspinal mechanisms; and cortical, psychological or ’placebo’ mechanisms contribute to the clinical effects in routine care (Carlsson 2002). While there is little doubt that acupuncture interventions cause neurophysiological changes in the organism, the traditional concepts of acupuncture involving specifically located points on a system of ’channels’ called meridians are controversial (Kaptchuk 2002).
Why it is important to do this review
As in many other clinical areas, the findings of controlled trials of acupuncture for migraine and other headaches have not been conclusive in the past. In 1999 we published a first version of our review on acupuncture for idiopathic headache (Melchart 1999), and in 2001 we published an updated version in The Cochrane Library (Melchart 2001). In our 2001 update, we concluded that “overall, the existing evidence supports the value of acupuncture for the treatment of idiopathic headaches. However, the quality and the amount of evidence are not fully convincing.” In recent years several rigorous, large trials have been undertaken. Due to the increasing number of studies, and for clinical reasons, we decided to split our previous review on idiopathic headache into two separate reviews on migraine and tension-type headache (Linde 2009) for the present update.
OBJECTIVES
We aimed to investigate whether acupuncture is a) more effective than no prophylactic treatment/routine care only; b) more effective than ’sham’ (placebo) acupuncture; and c) as effective as other interventions in reducing the frequency of headaches in patients with migraine.
METHODS
Criteria for considering studies for this review
Types of studies
We included controlled trials in which allocation to treatment was explicitly randomized, and in which patients were followed up for at least 8 weeks after randomization. Trials in which a clearly inappropriate method of randomization (for example, open alternation) was used were excluded.
Types of participants
Study participants had to be diagnosed with migraine. Studies focusing on migraine but including patients with additional tension-type headache were included. Studies including patients with headaches of various types (for example, some patients with migraine, some with tension-type headache) were included only if findings for migraine patients were presented separately or if more than 90% of patients suffered from migraine.
Types of interventions
The treatments considered had to involve needle insertion at acupuncture points, pain points or trigger points, and had to be described as acupuncture. Studies investigating other methods of stimulating acupuncture points without needle insertion (for example, laser stimulation or transcutaneous electrical stimulation) were excluded.
Control interventions considered were:
no treatment other than treatment of acute migraine attacks or routine care (which typically includes treatment of acute attacks, but might also include other treatments; however, trials normally require that no new experimental or standardized treatment be initiated during the trial period);
sham interventions (interventions mimicking ’true’ acupuncture/true treatment, but deviating in at least one aspect considered important by acupuncture theory, such as skin penetration or correct point location);
other treatment (drugs, relaxation, physical therapies, etc.).
Trials that only compared different forms of acupuncture were excluded.
Types of outcome measures
Studies were included if they reported at least one clinical outcome related to headache (for example, response, frequency, pain intensity, headache scores, analgesic use). Trials reporting only physiological or laboratory parameters were excluded, as were trials with outcome measurement periods of less than 8 weeks (from randomization to final observation).
Search methods for identification of studies
(See also: Pain, Palliative & Supportive Care Group methods used in reviews.)
For our previous versions of the review on idiopathic headache (Melchart 1999; Melchart 2001), we used a very broad search strategy to identify as many references on acupuncture for headaches as possible, as we also aimed to identify non-randomized studies for an additional methodological investigation (Linde 2002). The sources searched for the 2001 version of the review were:
MEDLINE 1966 to April 2000;
EMBASE 1989 to April 2000;
Cochrane Complementary Medicine Field Trials Register;
Cochrane Central Register of Controlled Trials (CENTRAL; Issue 1, 2000);
individual trial collections and private databases;
bibliographies of review articles and included studies.
The search terms used for the electronic databases were ’(acupuncture or acupressure)’ and ’(headache ormigraine)’. In the years following publication of the 2001 review, the first authors regularly checked PubMed and CENTRAL using the same search terms. For the present update, detailed search strategies were developed for each database searched (see Appendix 1). These were based on the search strategy developed for MEDLINE, revised appropriately for each database. The MEDLINE search strategy combined a subject search strategy with phases 1 and 2 of the Cochrane Sensitive Search Strategy for RCTs (as published in Appendix 5b2 of the Cochrane Handbook for Systematic Reviews of Interventions, version 4.2 6 (updated Sept 2006)). Detailed strategies for each database searched are provided in Appendix 1.
The following databases were searched for this update:
Cochrane Pain, Palliative & Supportive Care Trials Register to January 2008;
Cochrane Central Register of Controlled Trials (CENTRAL; Issue 4, 2007);
MEDLINE updated to January 2008;
EMBASE updated to January 2008;
Cochrane Complementary Medicine Field Trials Register updated to January 2008.
In addition to the formal searches, one of the reviewers (KL) regularly checked (last search 15 April 2008) all new entries in PubMed identified by a simple search combining acupuncture AND (migraine OR headache), checked available conference abstracts and asked researchers in the field about new studies. Ongoing or unpublished studies were identified by searching three clinical trial registries (http://clinicaltrials.gov/, http:// www.anzctr.org.au/, and http://www.controlled-trials.com/mrct/; last update 15 April 2008).
Data collection and analysis
Selection of studies
All abstracts identified by the updated search were screened by one reviewer (KL), who excluded those that were clearly irrelevant (for example, studies focusing on other conditions, reviews, etc.). Full texts of all remaining references were obtained and were again screened to exclude clearly irrelevant papers. All other articles and all trials included in our previous review of acupuncture for idiopathic headache were then formally checked by at least two reviewers for eligibility according to the above-mentioned selection criteria. Disagreements were resolved by discussion.
Data extraction
Information on patients, methods, interventions, outcomes and resultswas extracted independently by at least two reviewers using a specially designed form. In particular, we extracted exact diagnoses; headache classifications used; number and type of centers; age; sex; duration of disease; number of patients randomized, treated and analyzed; number of, and reasons for dropouts; duration of baseline, treatment and follow-up periods; details of acupuncture treatments (such as selection of points; number, frequency and duration of sessions; achievement of de-chi (an irradiating feeling considered to indicate effective needling); number, training and experience of acupuncturists); and details of control interventions (sham technique, type and dosage of drugs). For details regarding methodological issues and study results, see below.
Where necessary, we sought additional information from the first or corresponding authors of the included studies.
Assessment of risk of bias in included studies
For the assessment of study quality, the new risk of bias approach for Cochrane reviews was used (Higgins 2008). We used the following six separate criteria:
Adequate sequence generation;
Allocation concealment;
Blinding;
Incomplete outcome data addressed (up to 3 months after randomization);
Incomplete follow-up outcome data addressed (4 to 12 months after randomization);
Free of selective reporting.
We did not include the item ’other potential threats to validity’ in a formal manner, but noted if relevant flaws were detected.
In a first step, information relevant for making a judgment on a criterion was copied from the original publication into an assessment table. If additional information from study authors was available, this was also entered in the table, along with an indication that this was unpublished information. At least two reviewers independently made a judgment whether the risk of bias for each criterion was considered low, high or unclear. Disagreements were resolved by discussion.
For the operationalization of the first five criteria, we followed the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). For the ’selective reporting’ item, we decided to use a more liberal definition following discussion with two persons (Julian Higgins and Peter Jüni) involved in the development of the Handbook guidelines. Headache trials typically measure a multiplicity of headache outcomes at several time points using diaries, and there is a plethora of slightly different outcome measurement methods. While a single primary end-point is sometimes predefined, the overall pattern of a variety of outcomes is necessary to get a clinically interpretable picture. If the strict Handbook guidelines had been applied, almost all trials would have been rated ’unclear’ for the ’selective reporting’ item. We considered trials as having a low risk of bias for this item if they reported the results of the most relevant headache outcomes assessed (typically a frequency measure, intensity, analgesic use and response) for the most relevant time points (end of treatment and, if done, follow-up), and if the outcomes and time points reported made it unlikely that study investigators had picked them out because they were particularly favorable or unfavorable.
Trials that met all criteria, or all but one criterion, were considered to be of higher quality. Some trials had both blinded sham control groups and unblinded comparison groups receiving no prophylactic treatment or drug treatment. In the risk of bias tables, the ’Judgement’ column always relates to the comparison with sham interventions. In the ’Description’ column, we also include the assessment for the other comparison group(s). As the risk of bias table does not include a ’not applicable’ option, the item ’ incomplete follow-up outcome data addressed (4 to 12 months after randomization)?’ was rated as ’unclear’ for trials that did not follow patients longer than 3 months.
Assessment of the adequacy of the acupuncture intervention
We also attempted to provide a crude estimate of the quality of acupuncture. Two reviewers (mostly GA and BB, or, for trials in which one of these reviewers was involved, AW) who are trained in acupuncture and have several years of practical experience answered two questions. First, they were asked how they would treat the patients included in the study. Answer options were ’exactly or almost exactly the same way’, ’similarly’, ’differently’, ’completely differently’ or ’could not assess’ due to insufficient information (on acupuncture or on the patients). Second, they were asked to rate their degree of confidence that acupuncture was applied in an appropriate manner on a 100-mm visual scale (with 0% = complete absence of evidence that the acupuncture was appropriate, and 100% = total certainty that the acupuncture was appropriate). The latter method was proposed by a member of the review team (AW) and has been used in a systematic review of clinical trials of acupuncture for back pain (Ernst 1998). In the Characteristics of included studies table, the acupuncturists’ assessments are summarized under ’Methods’ (for example, ’similarly/70%’ indicates a trial where the acupuncturist-reviewer would treat ’similarly’ and is ’70%’ confident that acupuncture was applied appropriately).
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Alecrim 2005 | ||
| Methods | This trial is only available as an abstract publication so far. A full publication is in preparation. On request the first author informed us that sequence generation, allocation concealment and blinding were performed as in Alecrim 2008. Both intention-to-treat analyses and analyses based on available data were performed. | |
| Participants | Number of patients included/analyzed: 64/64 (in intention-to-treat analysis; information from author) Condition: migraine with or without aura Demographics: not reported Setting: outpatient headache clinic of a neurology department of State University of Campinas, Brasil Time since onset of headaches: not reported |
|
| Interventions | Acupuncture points: individualized selection according to traditional Chinese medicine DeChi achieved?: yes (information from author) Number of treatment sessions: 16 Frequency of sessions: 2/week for first 4 weeks, then 1/week for 8 weeks (information from author) Information on acupuncturists: 1 acupuncturist trained in Spain and 12 years of practical experience (information from author) Control intervention: sham acupuncture (superficial needling without manipulation at non-indicated points) |
|
| Outcomes | Method for outcome measurement: diary | |
| Notes | This trial is the third in a series performed by the authors. The trials Alecrim 2006 and 2008 were performed before this study. The authors provided data for effect size calculations (50% response rates, migraine days, attacks, rescue medication use). | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Only published abstract is now available, therefore, the study was not yet assessed formally. According to authors methods are the same as in Alecrim 2006 and Alecrim 2008. |
| Allocation concealment? | Unclear | Only published abstract is now available, therefore, the study was not yet assessed formally. According to authors methods are the same as in Alecrim 2006 and Alecrim 2008. |
| Blinding? All outcomes |
Unclear | Only published abstract is now available, therefore, the study was not yet assessed formally. According to authors methods are the same as in Alecrim 2006 and Alecrim 2008. |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Unclear | Only published abstract is now available, therefore, the study was not yet assessed formally. According to authors methods are the same as in Alecrim 2006 and Alecrim 2008. |
| Free of selective reporting? | Unclear | Only published abstract is now available, therefore, the study was not yet assessed formally. According to authors methods are the same as in Alecrim 2006 and Alecrim 2008. |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Unclear | Only published abstract is now available, therefore, the study was not yet assessed formally. According to authors methods are the same as in Alecrim 2006 and Alecrim 2008. |
| Alecrim 2006 | ||
| Methods | Blinding: patients, research assistants, neurologist; blinding tested and successful Dropout/withdrawals: substantial bias is unlikely in the first 3 months, but it cannot be ruled out for late follow-up (< 10% attrition (3/31) in the first 3 months, 5/31 until end of month 5, 7 /31 until end of month 9; similar rates in both groups; no intention-to-treat analysis) Observation period: 4 weeks baseline, 12 weeks treatment, 24 weeks follow Acupuncturists’ assessments: GA similarly/70% |
|
| Participants | Number of patients included/analyzed: 31/28 Condition: migraine with or without aura (IHS 1988) Demographics: mean age 32.5 (acupuncture) and 39.1 (sham) years, 79% female Setting: outpatient headache clinic of a neurology department of State University of Campinas, Brasil Time since onset of headaches: mean 16.9 (acupuncture) and 20.0 (sham) years |
|
| Interventions | Acupuncture points: semistandardized point selection (GB12/20/21 and BL10 in all patients + individualized additional points from a selection); point selection for a patient was not changed over treatment sessions Information on acupuncturists: 1 acupuncturist trained in Spain and 12 years of practical experience (information from author) De-Chi achieved?: yes Number of sessions: 16 (30 minutes each) Frequency of treatment sessions: 2/week for first 4 weeks, then 1/week for 8 weeks Control intervention: sham(superficial needling without manipulation at non-indicated points Ex-B1, SJ17/20, Sp7, St37, Lu5) |
|
| Outcomes | Method for outcome measurement: diary Primary outcomes: at least 40% reduction in attack frequency, at least 50% attack reduction and total migraine days during treatment period Other outcomes: frequency of migraine attacks, duration of attacks, severity, migraine hours, rescue medication, nausea and vomiting frequency |
|
| Notes | Rigorous but small trial; selection of existing acupuncture points in the sham group problematic Authors provided additional information on methods and data for effect size calculations (50% response rates, migraine days, attacks, rescue medication use) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | “Random digits (reference 14) were used to define the sequence” |
| Allocation concealment? | Yes | Opaque, numbered and sealed envelopes |
| Blinding? All outcomes |
Yes | Patients blinded; test of blinding suggests successful blinding |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Yes | Low attrition unlikely to cause major bias: 3 of 31 patients (2 of 16 acupuncture, 1 of 15 sham) did not complete the 12-week treatment phase |
| Free of selective reporting? | Yes | Relevant outcomes described in publication and additional data provided on request |
| Incomplete follow-up outcome data addressed? All outcomes later than 3months after randomisation |
Unclear | 13 patients in both groups at 2 month follow-up after treatment (5 months after randomisation) and 12 in both groups at 6 months after treatment (9 months after randomisation); no intention-to-treat analysis |
| Alecrim 2008 | ||
| Methods | Blinding: patients, research assistants, neurologist; blinding tested and successful Dropouts/withdrawals: bias unlikely - during the first 3 months only one patient in sham group without diary data, at late follow-up one exclusion and one lacking diary in the acupuncture group Observation period: 4 weeks baseline, 12 weeks treatment, 24 weeks follow-up Acupuncturists’ assessments: GA can’t tell |
|
| Participants | Number of patients included/analyzed: 37/36 Condition: migraine with or without aura (IHS 1988) Demographics: mean age 35 years, 89% female Setting: outpatient headache clinic of a neurology department of State University of Campinas, Brasil Time since onset of headaches: mean 20.6 (acupuncture) and 14.5 (sham) years |
|
| Interventions | Acupuncture points: individualized selection based on principles of traditional Chinese medicine DeChi achieved?: yes Number of treatment sessions: 16 (30 minutes each) Frequency of sessions: 2/week for first 4 weeks, then 1/week for 8 weeks (not reported in paper) Information on acupuncturists: 1 acupuncturist trained in Spain and 12 years of practical experience (information from author) Control intervention: very superficial insertion of 10 to 15 needles at acupuncture points considered irrelevant for headache (some on the head) |
|
| Outcomes | Method for outcome measurement: diary Primary outcome: at least 50% attack reduction (each month) Other outcomes: at least 40% attack reduction, attack frequency, number of migraine days, migraine hours, duration per attack, severity, amount and type of rescuemedication, nausea and vomiting frequency |
|
| Notes | Rigorous but small trial; selection of existing acupuncture points in the sham group problematic First author provided additional information on methods and data for effect size calculations (50% response rates, migraine days, attacks, rescue medication use) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Use of random digits as in Alecrim 2006 |
| Allocation concealment? | Yes | Opaque and sealed envelopes; inclusion by independent neurologist |
| Blinding? All outcomes |
Yes | Patients blinded; test of blinding suggests successful blinding |
| Incomplete outcome data addressed? All outcomes up to 3month after randomisation |
Yes | 36 of 37 randomized patients (1 drop out sham group) included in analysis |
| Free of selective reporting? | Yes | Relevant outcomes described in publication and additional data provided on request |
| Incomplete follow-up outcome data addressed? All outcomes later than 3months after randomisation |
Yes | 34 of 37 patients with data at long-term follow-up (2 vs. 1 dropouts/withdrawals) |
| Allais 2002 | ||
| Methods | Blinding: diary evaluator Dropouts/withdrawals: substantial bias unlikely (attrition only 10 of 160 patients in 6 months) Observation period: baseline 2 months; treatment 6 months, no follow-up Acupuncturists’ assessments: BB different/65% |
|
| Participants | Number of patients included/analyzed: 160/150 Condition: migraine without aura (IHS) Demographics: mean age 38 years; all female Setting: Women’s Headache Center, University of Turin, Italy Age at onset of headaches: mean 18 years |
|
| Interventions | Acupuncture points: LR3, SP6, ST36, CV12, LI4, PC6, GB20, GB14, Taiyang, GV20 Information on acupuncturists; n = 3, “experienced and qualified” DeChi achieved?: yes Number of treatment sessions: 12 Frequency of treatment sessions: 1/week for 2 months, then 1/month for 4 months Control intervention: Flunarizine 10 mg (2 months daily, then 20 days per month for 4 months) |
|
| Outcomes | Method for outcome measurement: headache diary Primary outcome: attack frequency Other outcomes: intensity, use of rescue medication |
|
| Notes | Unblinded, but otherwise rigorous trial; additional information provided from author The paper presents data on attack frequency and analgesics use for 2-month intervals. For calculating weigthed mean differences in this review the means for attack frequency presented in the publication were divided by 2, as all other trials refer to 4-week periods. The same was done with the standard deviations provided by the author. For calculation of standardized mean differences the 2-month means presented in the publication were used. |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer program |
| Allocation concealment? | Yes | Central telephone procedure (information from author) |
| Blinding? All outcomes |
No | Patients not blinded; diary evaluation blinded |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Yes | Only 10 (3 acupuncture, 7 flunarizine) of 160 patients did not complete the study |
| Free of selective reporting? | Yes | Relevant outcomes presented |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Yes | Only 10 (3 acupuncture, 7 flunarizine) of 160 patients did not complete the study |
| Baust 1978 | ||
| Methods | Blinding: patient, evaluating physician (patients not informed that a sham treatment was involved) Dropouts/withdrawals: no information in publication, according to the author’s memory 6 of 50 patients included dropped out Observation period: individualized period of observation (10 intervals between migraine attacks in the baseline period) Acupuncturists’ assessments: GA similarly/35% - BB differently/30% |
|
| Participants | Number of patients included/analyzed: 44?/44? Condition: migraine (’therapy-resistant’) Demographics: no information Setting: unclear, Germany Time since onset of headaches: 75% of patients > 5 years |
|
| Interventions | Acupuncture points: if pain mainly frontal: GB 14, Ex3, LI 4; temporal: Ex9, GB 20, TE5; occipital: GV 15, BL 10, BL 60 Information on acupuncturists: n = 2, no information on experience and qualification DeChi achieved?: no information Number of treatment sessions: 6 Frequency of treatment sessions: every 2 days Control group intervention: placebo points 2–3 cm distant from true points |
|
| Outcomes | Method for outcome measurement: patient diary Outcomes: all analyses focus on a categorized index (integrating frequency, intensity and duration) although other aspects were also documented in the diary |
|
| Notes | Insufficient data presentation; variable observation period; patients were not told that they could get a sham intervention Limited additional information provided from author (patient files and reports were destroyed 10 years after completion of the study) Available responder data included in analysis for response after 3 to 4 months |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Unclear (author confirmed it was randomized) |
| Allocation concealment? | Unclear | No description |
| Blinding? All outcomes |
Yes | Patients and evaluating physicians were blinded (patients not informed that a sham treatment was involved) |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
No | No dropouts mentioned in publication. Author reports on request that according to his memory 6 patients dropped out |
| Free of selective reporting? | No | Only responder data reported |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Unclear | No follow-up |
| Ceccherelli 1992 | ||
| Methods | Blinding: patients, statistician (information from author) Dropout/withdrawals: no dropouts mentioned in the publication (first author remembers that there were a few more patients but does not remember the exact number) Observation period: baseline unclear; treatment 10 weeks; follow-up only in patients with good response Acupuncturists’ assessments: GA similarly/70% - BB differently/45% |
|
| Participants | Number of patients included/analyzed: 30?/30 Condition: migraine without aura Demographics: mean age 40 years; 9 female, 6 male in acupuncture group; 15 female in sham group Setting: unclear, Italy Time since onset of headaches: 179 +/− 127 months (control group: 226 +/− 140) |
|
| Interventions | Acupuncture points: BL 2, BL10, BL 60, GB 3, GB 20, GV 11, GV 20, LR 3, CV 13 Ex HN1, ST 8 (on non-painful side) Information on acupuncturist: n = 1, trained 3 years DeChi achieved?: no information Number of treatment sessions: 10 Frequency of treatment sessions: 1/week Control intervention: placebo acupuncture (complex procedure without real needling suggesting superficial anesthesia to the patient) |
|
| Outcomes | Method for outcome measurement: headache diary Primary outcome: at least 50% score reduction Other outcomes: headache hours, intensity |
|
| Notes | Patients were not informed that they might get a placebo; unusual sham technique; sex differences between groups; no interpretable follow-up data (only follow-up of responders) | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Random number table (information from author) |
| Allocation concealment? | Yes | Numbered envelopes, inclusion and random allocation by different persons (information from author) |
| Blinding? All outcomes |
Yes | Patients were blinded. The sham procedures differed from true acupuncture but patients were not informed that they might get a placebo. |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Unclear | No dropouts mentioned. The author reports on request that there were a few patients who did not complete the study. |
| Free of selective reporting? | Yes | Relevant outcomes reported |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Unclear | Follow-up only performed in treatment responders |
| Diener 2006 | ||
| Methods | Blinding: patients (comparison acupuncture vs. sham), telephone interviewers; blinding acupuncture vs. sham tested and successful Dropouts/withdrawals: no bias for comparison with sham acupuncture, major bias possible for comparison with medication (8 of 313 patients allocated to acupuncture with-drew consent before the first treatment, 11 of 339 allocated to sham acupuncture and 106 of 308 allocated to standard treatment; after start of treatment 15 of 305 in the acupuncture group did not reach the primary endpoint, 11 of 328 in the sham acupuncture group and 15 of 202 in the standard treatment group) Acupuncturists assessment: GA similarly/85% - BB similarly/70% |
|
| Participants | Number of participants included/analyzed: 960/794 Condition: migraine (IHS) Demographics: mean age 37 years, 83% female Observation period: 4 weeks baseline, 6 weeks treatment (+ optionally 2 further weeks), 20 weeks follow-up Setting: 149 primary care physicians in Germany Time since onset of headaches: mean 16 years |
|
| Interventions | Acupuncture points: semistandardized - depending on Chinese syndrome diagnosis pre-defined collections of obligatory and flexible points Information on acupuncturists: 149 physicians with at least 140 hours acupuncture training and 2 years professional experience DeChi achieved?: yes Number of treatment sessions: 10 (if moderate response further 5 sessions possible) Frequency of treatment sessions: 2/week Control intervention 1: shamacupuncture (superificial needling at distant non-acupuncture points) Control intervention 2: guideline-based individualized standard treatment - 1. preference beta-blockers, 2. preference flunarizine, 3. preference valproic acid |
|
| Outcomes | Method for outcome measurement: diary and interviews Primary outcome: difference in migraine days between baseline and weeks 23 to 26 after randomization Other outcomes: migraine days, medication use, at least 50% reduction of migraine days, pain intensity, impairment, pain days, quality of life, global assessments |
|
| Notes | Very large, rigorous multicenter trial. The interpretation of the comparison with standard treatment is compromised by the fact that more than a third of patients allocated to standard treatment withdrew consent. No information is given on dosage and compliance in the standard treatment group. Authors provided biometrical report. Data on migraine days at the different time points were taken from this report instead from the publication which presented differences to baseline only. | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer program |
| Allocation concealment? | Yes | Central fax procedure |
| Blinding? All outcomes |
Yes | Patients and telephone interviewers were blinded for the comparison with sham acupuncture. Test of blinding suggests successful blinding. The comparison with drug treatment was not blinded. |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Yes | Very low attrition and intention-to-treat analysis for comparison with sham acupuncture. For the comparison with drug treatment the risk of bias is high as a large proportion of patients allocated to drug treatment withdrew consent immediately after randomization or discontinued treatment. |
| Free of selective reporting? | Yes | Relevant outcomes reported and additional data provided on request |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Yes | Very low attrition and intention-to-treat analysis for comparison with sham acupuncture. For the comparison with drug treatment the risk of bias is high as a large proportion of patients allocated drug treatment withdrew consent immediately after randomization or dropped out. |
| Doerr-Proske 1985 | ||
| Methods | Blinding: not blinded Dropouts/withdrawals: no explicit information, results suggest that all patients completed the treatment period and 17/20 the follow-up period (waiting list group without follow-up) Observation period: 2 months diagnostic; baseline 1 month; treatment 2 months; follow-up 20 months Acupuncturists’ assessments: GA completely different/20% - BB completely different/5% |
|
| Participants | Number of patients included/analyzed: 30?/30? Condition: migraine (therapy-resistant; 18 migraine with aura, 7 vasomotoric headache, 5 common migraine; 2 had additional cluster headache) Demographics: mean age 39 years; 77% female Setting: unclear, Germany Time since onset of headaches: > 2 years (inclusion criterion); 23/30 > 10 years |
|
| Interventions | Acupuncture points: Extra 2 (Yintang), GB2, TE5 Information on acupuncturist: n = 1; anesthesiologist trained in acupuncture DeChi achieved?: no information Number of treatment sessions: 10 Frequency of treatment sessions: 1/week? Control 1: waiting-list (2 months) Control 2: psychological biobehavioral treatment program focusing on relaxation |
|
| Outcomes | Method for outcome measurement: diary Outcomes: frequency, intensity, duration, impairment, medication use |
|
| Notes | Very small sample size; no explicit information on whether there were dropouts/ with-drawals; very unusual point selection | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Not described |
| Allocation concealment? | Unclear | Not described |
| Blinding? All outcomes |
Unclear | No blinding |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Yes | No mentioning of dropouts and with-drawals. Table 5 in Wittchen & Lässle publication suggests that 30/30 patients completed the 8 weeks treatment period, 20/20 (the 10 waiting list patients then were treated after 8 weeks) the first follow-up (1 month later), and 17/20 the 20 month follow-up. |
| Free of selective reporting? | Yes | Relevant outcomes reported |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Unclear | See above |
| Dowson 1985 | ||
| Methods | Blinding: patients Dropouts/withdrawals: all patients with data after treatment, 9/44 (5 vs. 4) did not complete the follow-up Observation period: baseline 4 weeks; treatment 6 weeks; follow-up 24 weeks Acupuncturists’ assessments: GA insufficient information for an assessment - BB similarly/70% |
|
| Participants | Number of patients included/analyzed: 48/48 (after treatment) and 39 (follow-up) Condition: migraine, migrainous headaches (recurrent headache with 2 of 3main symptoms (aura, unilateral distribution and nausea/vomiting)) Demographics: mean age 39 years in the acupuncture and 42 years in the sham group; 83% female Setting: practice, UK Time since onset of headaches: not reported |
|
| Interventions | Acupuncture points: point selection according to location of pain (modified after 2–3 sessions if no response) No information on acupuncturist(s) DeChi achieved?: yes Number of treatment sessions: 6 sessions of 10 minutes each Frequency of sessions: 1/week Information on acupuncturists: none Control intervention: mock transcutaneous nerve stimulation |
|
| Outcomes | Method for outcome measurement: diary, but only presentation of dichotomized data (50% reduction) | |
| Notes | Insufficient presentation of results (no data on follow-up at all); unusual (probably not very sensitive) method of analysis; patients probably not fully informed about use of placebo | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer program |
| Allocation concealment? | Unclear | Sealed envelopes (further information not available) |
| Blinding? All outcomes |
Unclear | The sham procedure (mock transcutaneous nerve stimulation) was distinguishable from acupuncture. The method of obtaining informed consent is not described, but probably patients were not informed that a sham procedure was involved. |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Yes | All patients completed the early phase of the study |
| Free of selective reporting? | No | Only responder data after treatment and results of inferential statistics presented. Reporting seems more insufficient than biased. Headache duration and analgesic requirement not reported; primary outcome not actually stated but was clearly pain relief. |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
No | 4 patients in the mock TNS group and 5 patients in the acupuncture group failed to complete follow-up (24 weeks after completion of treatment). No intention-to-treat analysis. |
| Facco 2008 | ||
| Methods | Blinding: patients (no blinding for the comparison with Rizatriptan only). Patients were informed that stronger (for true acupuncture group) and milder (for mock acupuncture control groups) acupuncture treatments would be applied (information from author) Dropouts/withdrawals: 17 of 160 in the first 3 months (5, 5, 5, and 2 in the 4 groups), further 16 in the following 3 months (3, 5, 4, 4); no intention-to-treat analysis - bias cannot be ruled out with certainty but does not seem likely Observation period: no baseline period, treatment 11 weeks, follow-up 3 months Quality scores: Acupuncturists’ assessments: GA similarly/80% - BB similarly/60% |
|
| Participants | Number of patients included/analyzed: 160/127 Condition: migraine without aura (IHS) Demographics: mean age 36 years 54% female Setting: unclear, Italy Time since onset of headaches: not reported |
|
| Interventions | All patients treated acute attacks with rizatriptan Acupuncture points: depending on the Chinese diagnosis (3 external and 4 internal syndromes) predefined point selection DeChi achieved?: yes Number of treatment sessions: 20 (2 courses of 10 sessions with 1-week rest between the courses) of 30 minutes each Frequency of sessions: 2/week Information on acupuncturists: n = 3, at least 560 hours training and 5 years clinical experience (information from authors) Control intervention 1: non-penetrating sham (non-penetrating needles with manipulation) at correct, individualized points with full process of Chinese diagnosis (“ritualized mock acupuncture” Control intervention 2: non-penetrating sham (non-penetrating needles with manipulation) at standardized points (ST8, GB5, GB20, GV14, LU7) without the process of Chinese diagnosis (“standard mock acupuncture”) Control group 3: attack treatment with rizatriptan only |
|
| Outcomes | Method for outcome measurement:Migraine Disability questionnaire (MIDAS) at baseline and after 3 and 6 months + number of rizatriptan wafers per 3-month period | |
| Notes | Only MIDAS score and rizatriptan intake measured, poor description of the sample, surprisingly little variability in several post-treatment and follow-up measures | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Computer program |
| Allocation concealment? | Yes | Sealed, opaque, consecutively numbered envelopes (information from author) |
| Blinding? All outcomes |
Yes | Patients were blinded for the comparison with the two sham groups; no blinding for the comparison with Rizatriptan only. Patients were informed that stronger and milder acupuncture treatments would be applied (information from author). |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
No | 33 of 160 dropped out; reasons were not reported; no intention-to-treat analysis |
| Free of selective reporting? | Yes | Very limited outcome measurement; outcomes measured were adequately reported |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
No | 33 of 160 dropped out; reasons were not reported; no intention-to-treat analysis |
| Henry 1985 | ||
| Methods | Blinding: patient, evaluating neurologist Dropouts/withdrawals: major bias unlikely until end of treatment phase, high attrition rate at follow-up Observation period: baseline unclear; treatment probably 3 months; follow-up 3 months after therapy (second follow-up after 6 months) Acupuncturists’ assessments: GA differently/45% - BB completely different/5% |
|
| Participants | Number of patients included/analyzed: 30/26 Condition: migraine (Ad Hoc) Demographics: mean age 34 years; 73% female; Setting: unclear, France Time since onset of headaches: 12.6 ± 1.5 years (placebo: 13.8 ± 10.6) |
|
| Interventions | Acupuncture points: LI 4, ST36, BL 2, BL 10, BL 60, LR3 needling with electrostimulation Information on acupuncturist: n = 1, no further information DeChi achieved?: no information Number of treatment sessions: 8 sessions of 30 minutes each Frequency of treatment sessions: 6× one/week, 2× one/month Control intervention: needling 1 cm away from points used in acupuncture group |
|
| Outcomes | Method for outcome measurement: migraine index (by blinded neurologist; no diary), global assessments (after 3 months) | |
| Notes | Insufficiently reported study, no use of a diary;many losses to follow-up, therefore follow-up data uninterpretable | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | No description |
| Allocation concealment? | Unclear | No description |
| Blinding? All outcomes |
Unclear | Study described as double-blind test. Needling in sham group 1 cm from true points, “not connected to the low frequency current”, duration and frequency as in acupuncture group, neurologist blinded. Very short description only, unclear how patients were informed and whether needles were connected with the electrostimulation device. |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Unclear | Data at 3 months reported for 17 of 20 patients in the acupuncture group and 9 of 10 patients in the sham group 2 (3 + 1 dropouts, no intention-to-treat analysis) |
| Free of selective reporting? | Yes | Very limited outcome measurement; outcomes measured were adequately reported |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
No | Data for 6/20 and 4/10 patients at 3 months reported suggesting very high attrition |
| Hesse 1994 | ||
| Methods | Blinding: patients and evaluators Dropouts/withdrawals: bias unlikely (8 of 85 patients dropped out) Observation period: baseline 4 weeks; treatment 17 weeks; no follow-up Acupuncturists’ assessments: GA completely differently/50% - BB different /30% |
|
| Participants | Number of patients included/analyzed: 85/77 Condition: migraine with or without aura (IHS) Demographics: mean age 45 years; 84% female Setting: outpatient pain clinic in Denmark Time since onset of headaches: mean 23 years |
|
| Interventions | Acupuncture points: needling individual trigger points together with placebo tablets Information on acupuncturist: n = 1, no further information DeChi achieved?: no information Number of treatment sessions: individualized Duration of treatment sessions: needling for a few seconds only Control intervention: beta blocker metoprolol 100 mg and placebo stimulation (touch with blunt end of the needle) |
|
| Outcomes | Method for outcome measurement: diary Primary outcome: probably attack frequency Other outcomes: severity, duration, global rating, consumption of analgesics |
|
| Notes | Rigorous trial; sham acupuncture procedure possibly distinguishable; non-traditional acupuncture technique (brief needling at trigger points); mean frequency and mean severity of attacks in the last 4 weeks were recalculated from raw data in Figure 1. | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | No description |
| Allocation concealment? | Unclear | No description |
| Blinding? All outcomes |
Unclear | “Blinding was obtained through a double-dummy technique and by keeping the therapist blinded to the results, whilst both investigator and statistician were blinded to the treatment”. Dry needling of individual trigger point was used in the acupuncture group compared to a superficial touch with the blunt end of the needle in the medication/sham acupuncture group at a random selection of points. The success of blinding is not discussed. The way of informing patients about interventions si not reported.No details on the drug placebo reported |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Yes | 8 of 85 patients dropped out. Analysis according to intention-to-treat principle. |
| Free of selective reporting? | Yes | Relevant outcomes reported |
| Incomplete follow-up outcome data addressed? All outcomes later than 3months after randomisation |
Unclear | Probably rigorous trial with data presented in a manner not feasible for effect size calculation. Authors could not be contacted. Trial ended 17 weeks after randomization. |
| Jena 2008 | ||
| Methods | Blinding: none Dropouts/withdrawals: 1479 of 1613 included in the acupuncture group with 3 month data vs. 1456 of 1569 in the control group; sensitivity analyses with missing values replaced confirm main analysis based on available data Observation period: no baseline period; treatment 3 months; no follow-up (for randomized comparison) Acupuncturists’ assessments: GA can’t tell - AW can’t tell |
|
| Participants | Number of patients included/analyzed: 3182/2935 with migraine or tension-type headache (of those included 1715 with migraine, 167 with migraine and TTH, no information on numbers of migraine patients analyzed) Condition: migraine and/or tension-type headache (IHS) Demographics: mean age 44 years, 77% female (for total group) Setting: several thousand practices in Germany Time since onset of headaches: 10.8 years (for total group) |
|
| Interventions | Acupuncture points: individualized selection Information on acupuncturists: at least 140 hours acupuncture training DeChi achieved?: no information Number of treatment sessions: up to a maximum of 15 (mean 10) Frequency of treatment sessions: individualized Control intervention: waiting list received “usual care” |
|
| Outcomes | Method for outcome measurement: questionnaires, no diary Primary outcome: headache days in the third month Other outcomes: intensity, quality of life |
|
| Notes | Large, very pragmatic study including both patients with migraine and tension-type headache; treating physicians were completely free to choose points, number of sessions (upper limit allowed 15) etc. Unclear what usual care consisted of. Some diagnostic misclassification likely. Authors provided raw means, standard deviations and number of observations for headache days and headache intensity for patients suffering from migraine. | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer program |
| Allocation concealment? | Yes | Central telephone randomization |
| Blinding? All outcomes |
No | No blinding |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Yes | 1711 patients were allocated to acupuncture and 1693 to control, but consent forms were available for only 1613 and 1569, respectively; baseline questionnaires were available for 1572 and 1522 (all numbers refer to both patients with migraine and patients with tension-type headache). 3-month data were available for 1479 and 1456 patients. Sensitivity analyses with replacing missing values confirmed main analyses. |
| Free of selective reporting? | Yes | Limited outcome measurement. Data on relevant outcomes for migraine subgroup provided by authors. |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Unclear | No randomized comparison after 3 months |
| Linde K 2005 | ||
| Methods | Blinding: patients, diary evaluators Dropouts/withdrawals: major bias unlikely Observation period: baseline 4 weeks; treatment 8 weeks; follow-up 16 weeks Acupuncturists’ assessments: AW similarly/80% - GA exactly as in the study/90% |
|
| Participants | Number of patients included/analyzed: 302/302 Condition: Migraine (IHS) Demographics: mean age 43 years, 88% female Setting: 18 primary care practices in Germany Time since onset of headaches: mean 20 years |
|
| Interventions | Acupuncture points: in all patients recommended GB20, GB40 or 41 or 42, DU20, LIV3, SJ3 or 5, Taiyang; additional optional points recommended according to individual symptoms Information on acupuncturists: n = 30, at least 160 hs of training DeChi achieved?: yes Number of treatment sessions: 12 of 30 minutes Frequency of treatment sessions: 2/week for 4 weeks, then 1/week for 4 weeks Control intervention: minimal acupuncture (superficial needling at non-acupuncture points) Control 2: waiting list (attack treatment only) for 12 weeks |
|
| Outcomes | Method for outcome measurement: diary and pain questionnaire Primary outcome: Number of days with moderate or severe headache in weeks 9 to 12 Other outcomes: migraine days, attacks, headache days; days with nausea, vomiting, disability, analgesics, headache score, intensity; quality of life, pain disability, depressive symptoms |
|
| Notes | Additional information from unpublished study report used for 8-week data, migraine days and headache scores | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer program |
| Allocation concealment? | Yes | Central telephone procedure |
| Blinding? All outcomes |
Yes | Patients and diary evaluators were blinded for the comparison with sham acupuncture. Patients were informed that two different types of acupuncture were compared. Early tests of blinding indicate successful blinding, but at follow-up guesses of allocation status were different between groups (although the sham group reported slightly better outcomes). Comparison with no treatment waiting list not blinded. |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Yes | Low attrition and intention-to-treat analysis |
| Free of selective reporting? | Yes | Relevant outcomes reported and additional data available for analyses |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Yes | Low attrition and intention-to-treat analysis |
| Linde M 2000 | ||
| Methods | Blinding: none Dropouts/withdrawals: substantial bias possible (16 of 39 patients dropped out/not included in analysis) Observation period: baseline 4 weeks; treatment 4–6 weeks; follow-up 12 weeks Acupuncturists’ assessments: GA differently/45% |
|
| Participants | Number of patients included/analyzed: 39/23 Condition: migraine without aura (IHS) Demographics: mean age 41 years, 82% female Setting: Gothenburg Migraine Clinic, Sweden Time since onset of headaches: more than 20 years on average |
|
| Interventions | Acupuncture points: GB40, GB14, DU20, LI4 and ST44 in all patients + additional points selected according to symptoms Information on acupuncturists: 1 experienced physiotherapist DeChi achieved?: yes Number of treatment sessions: 7–10 Frequency of treatment sessions: 1–2 sessions/week Control intervention: no acupuncture All patients received pharmacological acute treatment as before the study |
|
| Outcomes | Method for outcome measurement: diary Primary outcome: migraine days Other outcomes: attack frequency, medication use |
|
| Notes | Pilot study hardly interpretable due to very high dropout rate; one patient in the acupuncture group had no migraine days during the baseline period and 26 during follow-up; some additional information provided by authors (M Linde and C+ Dahlöf). The trial originally had a third arm(relaxation) but results were not reported and are not available. | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Random number list |
| Allocation concealment? | No | Inadequate method, although bias seems unlikely (random list was openly accessible to the physician including the patient; this physician was, however, not involved further - information from author) |
| Blinding? All outcomes |
No | No blinding |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
No | 16/39 patients (9 acupuncture, 7 control) dropped out early or could not be analyzed. Detailed description, no intention-to-treat analysis. |
| Free of selective reporting? | Yes | Relevant outcomes reported |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
No | See above |
| Linde M 2005 | ||
| Methods | Blinding: patients, statistical analysis Dropouts/withdrawals: 3 during treatment, further 5 during follow-up, major bias unlikely Observation period: baseline at least 2 months; treatment 3 months; 6 months follow-up Acupuncturists’ assessments: GA completely differently/20% - BB differently/45% |
|
| Participants | Number of patients included/analyzed: 31/28 Condition: menstrually related migraine without aura (IHS) Demographics: mean age 36 years, all female Setting: Gothenburg Migraine Clinic, Sweden (information provided by author) Time since onset of headaches: not reported |
|
| Interventions | Acupuncture points: in all patients GB8, GB20, LI4, LR3, SP6 + either GB14, Taiyang or UB10 depending on site of maximum pain Information on acupuncturists: 2 experienced physiotherapists DeChi achieved?: yes Number of treatment sessions: 9 sessions Frequency of treatment sessions: 8, 5, and 3 days before expected date of menstruation in three cycles Control intervention: Non-penetrating sham needles at the same points All patients wore a cap on the head to allow fixation of plaster holders through which both true and sham needles were applied |
|
| Outcomes | Method for outcome measurement: diary Primary outcome: migraine attack frequency Other outcomes: migraine days, intensity, medication use, intensity |
|
| Notes | Rigorous but small study; use of non-penetrating sham needles at true points; additional information provided by author | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Random number table (information from author) |
| Allocation concealment? | Unclear | Method not optimal, but bias seems unlikely: inclusion of patients by a neurologist, then a research nurse randomly took a twice folded card from a collection of six cards prepared by the neurologist; the opened card was forwarded to the acupuncturist who met the prescheduled patients (information provided by author) |
| Blinding? All outcomes |
Yes | Patients and data analysis blinded. Test suggests that blinding was successful. |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Yes | Low attrition rate and intention-to-treat analysis |
| Free of selective reporting? | Yes | Relevant outcome reported |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Yes | Acceptable attrition rate and intention-to-treat analysis |
| Streng 2006 | ||
| Methods | Blinding: diary evaluators Dropouts/withdrawals: substantial bias possible Observation period: baseline 4 weeks; treatment 12 weeks; follow-up 12 weeks Acupuncturists’ assessments: BB similarly/80% - GA similarly/90% |
|
| Participants | Number of patients included/analyzed: 114/89 Condition: migraine (IHS) Demographics: mean age 40 years, 88% female Setting: 17 primary care practices in Germany Time since onset of headaches: mean 16 years |
|
| Interventions | Acupuncture points: individualized Information on acupuncturists: n = 21, at least 160 hours acupuncture training DeChi achieved?: yes Number of treatment sessions: on average 13.4 Frequency of treatment sessions: 1–2/week Control intervention: Metoprolol 100 to 200mg daily for 3 months |
|
| Outcomes | Method for outcome measurement: diary and pain questionnaires Primary outcome: migraine days (in weeks 9 to 12) Other outcomes: migraine attacks, headache days, days with rescue medication, at least 50% attack/migraine days reduction, days with nausea, vomiting, disability; intensity, headache score; quality of life, pain disability, depressive symptoms |
|
| Notes | Additional information available from full study report; more dropout in metoprolol group Data on number of patients with side effects taken from full study report (patient questionnaire) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer program |
| Allocation concealment? | Yes | Central telephone randomization |
| Blinding? All outcomes |
No | Patients not blinded; diary evaluators blinded |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
No | Unequal attrition in the two groups: very low in acupuncture group while a relevant proportion of patients in the metoprolol group either withdrew consent immediately after randomization or dropped out later |
| Free of selective reporting? | Yes | Relevant outcomes reported |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
No | See above |
| Vickers 2004 | ||
| Methods | Blinding: none Dropouts/withdrawals: careful handling of dropouts and withdrawals - substantial bias unlikely Observation period: 4 weeks baseline; 3 months treatment; 9 months follow-up Acupuncturists’ assessments: GA can’t tell - BB exactly as in the trial 90% |
|
| Participants | Number of patients included/analyzed: 401/326 at 3 months and 301 at 12 months Condition: 94% migraine, 6% tension-type headache (IHS) Demographics: mean age 46 years, 84% female Setting: 12 separate sites consisting of a single acupuncture practice and 2 to 5 general practices in the UK Time since onset of headaches: mean 21 years |
|
| Interventions | Acupuncture points: individualized Information on acupuncturists: 12 practices, members of the Acupuncture Association of Chartered Physiotherapists with at least 250 hours acupuncture training (median 12 years acupuncture practice) DeChi achieved?: not reported Number of treatment sessions: median 9, (25th and 75th percentiles 6 and 11) in 3 months Frequency of treatment sessions: median 1/week Control intervention: usual care by general practitioner |
|
| Outcomes | Method for outcome measurement: diary and questionnaires Primary outcome measure: headache score (at 1 year) Other outcomes: headache days, severity,% improvement, medication use, at least 50% reduction of headache days, quality of life |
|
| Notes | Pragmatic trial with additional cost-effectiveness analysis | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer generated minimization procedure (gender, age, chronicity, severity, diagnoses and number per group as minimized variables) |
| Allocation concealment? | Yes | Secure, password protected database |
| Blinding? All outcomes |
No | No blinding |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Yes | Acceptable attrition rates and sensitivity analyses (several imputations for missing values) confirming primary analysis |
| Free of selective reporting? | Yes | Relevant outcomes reported |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Yes | See above |
| Vincent 1989 | ||
| Methods | Blinding: patients Dropouts and withdrawals: bias unlikely for treatment and early follow-up (only 2/32 patients did not complete this phase), for late follow-up attrition is also comparably low (6/32) but bias cannot be ruled out completely Observation period: baseline 4 weeks; treatment 6 weeks; follow-up 1 year Acupuncturist’s GA assessment: similarly/75% - BB similarly/70% |
|
| Participants | Number of patients included/analyzed: 32/30 (6-week follow-up)/26 (1-year follow-up) Condition: classical or common migraine Demographics: mean 37 years; 84% female Setting: university outpatient department, UK Time since onset of headaches: mean 20 years |
|
| Interventions | Acupuncture points: classical points chosen individually by tenderness; 8 both local and distant points used No information on acupuncturist(s) DeChi achieved?: no information Number of treatment sessions: 6 sessions of 15 minutes each Frequency of treatment sessions: 1/week Control group intervention: superficial needling only, 2–3 cm from classical points |
|
| Outcomes | Method for outcome measurement: diary Primary outcome: total weekly pain score Outcomes: pain-free days, intensity, medication use |
|
| Notes | Significant effect on intensity, but no relevant effect on number of pain-free days; credibility of blinding tested; rigorous trial; author provided individual patient data which allowed calculation of responders and number of headache days | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | No description |
| Allocation concealment? | Unclear | Sealed envelopes (information from author) |
| Blinding? All outcomes |
Yes | Patients blinded. Test suggests successful blinding. |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Yes | Very low attrition rate (3/32 patients) in early phase of the trial |
| Free of selective reporting? | Yes | Most important outcomes presented and individual patient data for headache days provided |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Unclear | 25/32 patients completed the follow-up 4 months after treatment and 26/32 patients after 12 months; no intention-to-treat analysis |
| Weinschütz 1993 | ||
| Methods | Blinding: patients Dropouts/withdrawals: unclear Observation period: baseline 6 weeks; treatment 8 weeks; follow-up 12 months Acupuncturists’ assessments: GA exactly the same way/95% - BB differently/45% |
|
| Participants | Number of patients included/analyzed: 40?/40? Condition: migraine with or without aura (IHS) Demographics: mean age 41 years; 90% female Setting: pain outpatient department of a university hospital, Germany Time since onset of headaches: mean 18 years |
|
| Interventions | Acupuncture points: up to 10 points chosen according to pain localization and modalities Information on acupuncturist: n = 1, experienced and qualified DeChi achieved?: yes Number of treatment sessions: 8 sessions of 15 minutes each Frequency of treatment sessions: 1/week Control intervention: sham acupuncture (superficial needling 1–2 cm distant from true points) |
|
| Outcomes | Method for outcome measurement: diary Primary outcomes: attack frequency and migraine hours (data mainly presented as responder rate evaluated by time-series analysis) |
|
| Notes | Probably rigorous, but insufficiently reported (in spite of multiple publication); no information on whether there were dropouts/withdrawals Additional information could not be obtained despite of several requests |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | No description |
| Allocation concealment? | Unclear | No description |
| Blinding? All outcomes |
Yes | Patients were blinded, sham acupuncture with superficial needling of the same number of needles 1 to 2 cm from true points without DeChi |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Unclear | No statements on whether any attrition or exclusions from analyses occurred |
| Free of selective reporting? | No | Only responder data derived from single-case statistics reported |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Unclear | See above |
| Weinschütz 1994 | ||
| Methods | Blinding: patients Dropouts/withdrawals: unclear Observation period: baseline 6 weeks; treatment 8 weeks; follow-up 12 months Acupuncturists’ assessments: GA exactly the same way/95% - BB differently/45% |
|
| Participants | Number of patients included/analyzed: 41?/41? Condition: migraine with or without aura (IHS) Demographics: mean age 38 years; 90% female Setting: pain outpatient department of a university hospital, Germany Time since onset of headaches: mean 18 years |
|
| Interventions | Acupuncture points: up to 10 points chosen according to pain localization and modalities Information on acupuncturist: n = 1, experienced and qualified DeChi achieved?: yes Number of treatment sessions: 8 sessions of 15 minutes each Frequency of treatment sessions: 1/week Control intervention: sham acupuncture (superficial needling 1–2 cm distant from true points) |
|
| Outcomes | Method for outcome measurement: diary Primary outcomes: attack frequency and migraine hours (data mainly presented as responder rate evaluated by time-series analysis) |
|
| Notes | Probably rigorous, but insufficiently reported (in spite of multiple publication); no information on whether there were dropouts/withdrawals; replication of Weinschütz 1993 (with additional needling of foot points) | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | No description |
| Allocation concealment? | Unclear | No description |
| Blinding? All outcomes |
Yes | Patients were blinded, sham acupuncture with superficial needling of the same number of needles 1 to 2 cm from true points without DeChi |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Unclear | No statements on whether any attrition or exclusions from analyses occurred |
| Free of selective reporting? | Unclear | Only responder data derived from single-case statistics reported |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Unclear | See above |
| Wylie 1997 | ||
| Methods | Blinding: post-treatment care Dropouts/withdrawals: unclear Observation period: baseline 4 weeks; treatment/follow-up unclear (probably 8 weeks) Acupuncturists’ assessments: GA can’t tell - BB similarly/70% |
|
| Participants | Number of patients included/analyzed: 67/? Condition: 27 migraine or migraine + tension-type headache, 40 tension-type headache (IHS) Demographics: mean age 38 years; 67% female Setting: headache outpatient department, UK Time since onset of headaches: mean 10 years |
|
| Interventions | Acupuncture points: chosen individually according to traditional Chinese medicine No information on acupuncturist(s) DeChi achieved?: no information Number of treatment sessions: 6 Frequency of treatment sessions: unclear Control intervention: massage and relaxation |
|
| Outcomes | Method for outcome measurement: diary Outcomes: two scores, migraine days, psychological measures |
|
| Notes | Results seem to differ considerably among subgroups: in migraine, results favor acupuncture; in tension-type headache, massage + relaxation; patients in the control group had a higher headache index at baseline Insufficiently reported |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | No description |
| Allocation concealment? | Unclear | No description |
| Blinding? All outcomes |
No | Patients unblinded. Follow-up assessments carried out by blinded clinician. |
| Incomplete outcome data addressed? All outcomes up to 3 month after randomisation |
Unclear | 82 patients agreed to enter study, 67 started treatment and seem to have completed the study |
| Free of selective reporting? | Yes | Outcome measurement and presentation of results not very good but data on major outcome measures basically presented |
| Incomplete follow-up outcome data addressed? All outcomes later than 3 months after randomisation |
Unclear | Trial had no follow-up |
DeChi = irradiating sensation said to indicate effective needling
IHS = International Headache Society
Comparisons for analysis
For the purposes of summarizing results, the included trials were categorized according to control groups: 1) comparisons with no acupuncture (acute treatment only or routine care); 2) comparisons with sham acupuncture interventions; 3) comparisons with prophylactic drug treatment; and 4) comparisons with other treatments.
Outcomes for effect size estimation
We defined four time windows for which we tried to extract and analyze study findings:
Up to 8 weeks/2 months after randomization;
3 to 4 months after randomization;
5 to 6 months after randomization; and
More than 6 months after randomization.
In all included studies acupuncture treatment started immediately or very soon after randomization.
If more than one data point were available for a given time window, we used: for the first time window, preferably data closest to 8 weeks; for the second window, data closest to the 4 weeks after completion of treatment (for example, if treatment lasted 8 weeks, data for weeks 9 to 12); for the third window, data closest to 6 months; and for the fourth window, data closest to 12 months.
We extracted data for the following outcomes:
Proportion of ’responders’. For trials investigating the superiority of acupuncture compared to no acupuncture or sham intervention, we used, if available, the number of patients with an attack frequency reduction of at least 50% and divided it by the number of patients randomized to the respective group. In studies comparing acupuncture with drug treatment or other therapies, we used for the denominator the number of patients receiving an adequate amount of treatment. If the number of responders regarding attack frequency was not available we used, in descending order of preference, the following outcomes: at least 50% reduction in number of migraine days; at least 50% reduction in number of headache days; at least 50% headache score reduction; and global assessment by patients or physicians. We calculated responder rate ratios (relative risk of having a response) and 95% confidence intervals as effect size measures.
Frequency of migraine attacks (means and standard deviations) per 4-week period. (Weighted) mean differences were calculated as effect size measures.
Number of migraine days (means and standard deviations) per 4-week period (weighted mean differences).
Number of headache days (means and standard deviations) per 4-week period (weighted mean differences).
Headache frequency (means and standard deviations). As many studies only reported either attacks, migraine days, headache days or absolute or percent reductions from baseline for one of these measures, we decided also to include a measure where various frequency measures could be used. As available, we used (in descending order of preference) absolute values from 4-week periods, other periods, differences from baseline or percentage change from baseline for (again, in descending order of preference) migraine days, migraine attacks or headache days. Due to the variability of outcomes, standardized mean differences were calculated as effect size measures.
Headache intensity (any measures available, extraction of means and standard deviations, calculation of standardized mean differences).
Frequency of analgesic use (any continuous or rank measures available, extraction of means and standard deviations, calculation of standardized mean differences).
For continuous measures we used, if available, the data from intention-to-treat analyses with missing values replaced; otherwise, we used the presented data on available cases.
All these outcomes rely on patient reports, mainly collected in headache diaries.
Post hoc we decided also to extract the number of patients reporting adverse effects and dropping out due to adverse effects for the trials comparing acupuncture and prophylactic drug treatment.
Main outcome measure
Although we consider measures such as number of migraine days to be preferable - because they are more informative and less subject to random variation - we decided to use the proportion of responders as the main outcome measure simply because this was most often reported in the studies in a manner that allowed effect size calculation. We chose the 3- to 4-month time window as the primary measure because this a) is typically close to the end of the treatment cycle, and b) is a time point for which outcome data are often available.
Meta-analysis
Pooled random-effects estimates, their 95% confidence intervals, the Chi2-test for heterogeneity and the I2-statistic were calculated for each time window for each of the outcomes listed above. Given the strong clinical heterogeneity, pooled effect size estimates can be considered to be only very crude indicators of the overall evidence. For this reason we also refrained from calculating numbers needed to treat to benefit (NNTBs).
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
Characteristics of excluded studies [ordered by study ID]
| Allais 2003 | Intervention: transcutaneous electrical nerve stimulation and laser therapy at acupuncture points in patients with transformed migraine |
| Annal 1992 | Intervention: transcutaneous electrical nerve stimulation not at acupuncture points |
| Borglum-Jensen 1979 | Methods: random allocation unlikely |
| Bäcker 2004 | Neurophysiological study comparing migraine patients and non-migraine subjects |
| Coeytaux 2005 | Patients: patients with chronic daily headaches |
| Domzal 1980 | Design: not controlled trial |
| Dong 1994 | Intervention: acupuncture vs. acupuncture |
| Gao 1999 | Patients/intervention: randomized study of acupuncture vs. traditional Chinese drugs. Included patients with migraine with a headache history < 6 months. |
| Gottschling 2008 | Intervention/patients: RCT investigating laser acupuncture in children with migraine or tension-type headache (no presentation of subgroup results) |
| Hansen 1983 | Patients: condition chronic facial pain |
| Heydenreich 1989a | Intervention: transcutaneous electrical stimulation (TENS) at acupuncture points without skin penetration vs. TENS at sham points |
| Heydenreich 1989b | Randomized study of acupuncture, transcutaneous electrical nerve stimulation at acupuncture points and medication.Reason for exclusion:medication (dihydroergotamine and ipraazochrom) considered contraindicated today. Insufficiently reported, hardly credible (no dropouts reported in spite of inadequate medication and long duration) trial. |
| Ho 1999 | Intervention: laser acupuncture (no skin penetration) vs. sham laser |
| Johansson 1991 | Patients: condition facial pain |
| Junnilla 1983 | Patients: study included patients with various chronic pain syndromes, including headache; however, headache patients were not presented as a separate subgroup, but only together with all other patients |
| Kubiena 1992 | Rigorously planned RCT comparing acupuncture and sham in patients with migraine. Reason for exclusion: trial uninterpretable due to extreme attrition/missing data (diary data for only 15 of 30 patients after completion of treatment and for only 4 patients at follow-up). |
| Lavies 1998 | Intervention/patients: laser acupuncture (no skin penetration) vs. sham laser in patients with migraine or tension-type headache |
| Lehmann 1991 | Insufficiently reported study with highly questionable validity (inconsistent reporting on proceedings in case of lack of response; extremely positive results claimed; no report on dropouts in a study lasting 18 months) comparing acupuncture, electro-acupuncture and propranolol in patients with “frequent”migraine. Reasons for exclusion: diagnosis of migraine not compatible with an average of 22 migraine days per months; strong doubts about validity. |
| Lenhard 1983 | Intervention: acupuncture + naloxone vs. acupuncture + placebo |
| Liguori 2000 | Study comparing acupuncture and medical treatment with highly questionable validity. Reasons for exclusion: 1) Doubts whether the study is truly randomized (only 2 of the 4 study centers used acupuncture); 2) It is stated that acupuncture patients never treated attacks with medication - this seems hardly credible with a study duration of 12 months; 3) no mentioning of dropouts and protocol deviations - hardly credible for a observation period of 12 months with daily documentation; 4) medication therapy highly different in two centers. |
| Loh 1984 | Patients: RCT including both patients with migraine and tension-type headache without reporting results for subgroups |
| Lundeberg 1988 | Report of a series of studies with RCTs on other pain syndromes; only uncontrolled trial in headache patients |
| Melchart 2003 | Patients/outcomes: RCT in acute migraine |
| Melchart 2004 | Intervention: Acupuncture provided together with other Chinese treatments (herbal medicine, Qi Gong or Tuina) compared to waiting list |
| Okazaki 1975 | Intervention: acupuncture vs. acupuncture |
| Pikoff 1989 | Patients/outcome measures: study on acute headache |
| Pintov 1997 | Design: Controlled trial with alternating allocation (not truly randomized) to deep acupuncture vs. sham (unclear whether this was superficial needling at the same or other points) in children with migraine |
| Shi 2000 | Patients: patients with “therapy-resistant headache” (exact headache diagnoses not reported) |
| Sold-Darseff 1986 | Methods: probably not randomized, only a subgroup had headache |
| Sun 2004 | Patients/outcome measures: RCT in migraine patients (“duration of illness over three months in all groups, and the longest was 12 months”) treated “in the acute period” for 10 days with daily acupuncture or indomethacin |
| Tekeoglu 1995 | Intervention: electroacupuncture vs. music sound electroacupuncture |
| Turk 1990 | Methods/intervention/outcomes: unclear method of allocation/acupuncture vs. laser-acupuncture/follow-up < 4 weeks |
Characteristics of ongoing studies [ordered by study ID]
| Liang | |
| Trial name or title | Randomized controlled trial of treating migraine with acupuncture |
| Methods | Sham-controlled, single blind |
| Participants | Adult migraine patients; estimated enrollment: 360 |
| Interventions | 4 acupuncture and 1 sham acupuncture arm |
| Outcomes | Primary outcome measure visual analogue scale |
| Starting date | November 2007 |
| Contact information | Liang F, Chengdu University of Traditional Chinese Medicine |
| Notes | Possibly this trial has only 4-week post-randomization observation |
| Vas | |
| Trial name or title | Pragmatic randomised controlled trial in general practice investigating the effectiveness of acupuncture against migraine |
| Methods | Multicentre, three-armed |
| Participants | Adult migraine patients; estimated enrollment: 270 |
| Interventions | Acupuncture, sham acupuncture and conventional treatment |
| Outcomes | Migraine days |
| Starting date | February 2008 |
| Contact information | Vas J, Pain Ceter, Dos Hermanos, Spain |
| Notes | |
| Wang | |
| Trial name or title | Efficacy and safety of acupuncture for migraine prophylaxis - a multicenter, randomized, controlled clinical trial |
| Methods | Single-blind, double-dummy |
| Participants | Adult migraine patients; estimated enrollment: 140 |
| Interventions | Acupuncture + drug placebo vs. sham acupuncture + flunarizine |
| Outcomes | Visual analogue scale, McGill Pain Questionnaire, change in frequency and duration of migraine attacks |
| Starting date | June 2007 |
| Contact information | Wang L, Beijing, China |
| Notes | |
| Zheng | |
| Trial name or title | Effectiveness and safety of acupuncture for migraine: a randomised, single blind and sham controlled trial |
| Methods | single blind |
| Participants | Adult migraine patients; estimated enrollment: 78 |
| Interventions | Acupuncture vs. sham acupuncture |
| Outcomes | Frequency of migraine attacks |
| Starting date | December 2005 |
| Contact information | Zheng ZRMIT University, Bundoora, Australia |
| Notes | |
Selection process
In our previous review on idiopathic headache (Melchart 2001), we evaluated 26 trials that included 1151 participants with various types of headaches. The search update identified a total of 251 new references. Full reports for three migraine trials (Alecrim 2005; Alecrim 2008; Jena 2008) that were reported only as abstracts at the time of completion of the literature search (January 2008) were later identified through personal contacts with study authors.
Most of the references identified by the search update were excluded at the first screening step by one reviewer, as they were clearly irrelevant. The most frequent reasons for exclusion at this level were: article was a review or a commentary; studies of non-headache conditions; clearly non-randomized design; and investigation of an intervention which was not true acupuncture involving skin penetration.
A total of 70 full-text papers were then formally assessed by at least two reviewers for eligibility. Thirty-two studies reported in 33 publications did not meet the selection criteria (see Characteristics of excluded studies). Common reasons for exclusion included: study group had non-migraine headache or included mixed pain populations without reporting data separately for the migraine subgroup (8 trials); interventions did not meet our definition of acupuncture (for example, laser acupuncture or transcutaneous electrical stimulation at acupuncture points; 6 trials); comparison of acupuncture with laser acupuncture or other acupuncture-like interventions (5 trials); and questionable random allocation (5 trials).
Twenty-two trials described in 37 publications (including published protocols, abstracts of trials otherwise not available at all or not available in English language, papers reporting additional aspects such as treatment details or cost-effectiveness analyses) met all selection criteria and were included in the review. The total number of study participants was 4419. One large study (n = 401) in which 6% of patients suffered from tension-type headache only was included, as 94% patients had migraine as a primary diagnosis (Vickers 2004). Two studies with a larger proportion of patients with tension-type headache were also included because separate subgroup data for migraine patients were available (Jena 2008; Wylie 1997). Patients included in these two studies who had only tension-type headache are not included in the number of patients and other figures below. Ten of the 22 included trials (Baust 1978; Ceccherelli 1992; Doerr-Proske 1985; Dowson 1985; Henry 1985; Hesse 1994; Vincent 1989; Weinschütz 1993; Weinschütz 1994; Wylie 1997) had been included in our previous review; the remaining 12 trials (Alecrim 2005; Alecrim 2006; Alecrim 2008; Allais 2002; Diener 2006; Facco 2008; Jena 2008; Linde K 2005; Linde M 2000; Linde M 2005; Streng 2006; Vickers 2004) are new.
Searches in the clinical trial registers identified four ongoing trials (Liang; Vas; Wang; Zheng; see Characteristics of ongoing studies).
General study characteristics
A total of 4419 migraine patients participated in the included studies. The mean number of patients in each trial was 201, with a median of 42. The smallest trial included 27 patients and the largest 1715. Five trials had between 114 and 401 participants (Allais 2002; Facco 2008; Linde K 2005; Streng 2006; Vickers 2004); the two largest trials had 960 (Diener 2006) and 1715 participants (Jena 2008). Five of the larger trials were multicenter studies; all others were performed in a single center. The 10 older trials included in the previous version of our review had included a total of 407 migraine patients.
Eight trials originated from Germany, four from the UK, three each from Italy and Brazil, two from Sweden and one each from Denmark and France. We were able to obtain additional information from the authors of 16 trials; however, for most older trials the amount of additional information was very limited. Detailed additional data relevant for the calculation of effect size measures were received for eight trials (Alecrim 2005; Alecrim 2006; Alecrim 2008; Diener 2006; Jena 2008; Linde K 2005; Streng 2006; Vincent 1989).
Design and comparisons
All trials used parallel-group designs; no trial had a cross-over design. Eighteen trials had two groups (one acupuncture group and a control group), three trials were three-armed (Diener 2006; Doerr-Proske 1985; Linde K 2005) and one trial had four groups (Facco 2008). Six trials included a group which either received treatment of acute attacks only (Doerr-Proske 1985; Facco 2008; Linde K 2005; Linde M 2000) or ’routine care’ that was not specified by protocol (Jena 2008; Vickers 2004), while the experimental group received acupuncture in addition. Fourteen trials had a sham control group. Sham techniques varied considerably. In three trials existing acupuncture points considered inadequate for the treatment of migraine were needled superficially (Alecrim 2005; Alecrim 2006; Alecrim 2008); in five trials superficial needling of non-acupuncture points at variable distance from true points was used (Diener 2006; Linde K 2005; Vincent 1989; Weinschütz 1993; Weinschütz 1994); and in a further two trials close non-acupuncture points were needled without indication of needling depth (Baust 1978; Henry 1985). In two trials (Linde M 2005; Facco 2008) ’placebo’ needles (telescope needles with blunt tips not penetrating the skin) were used. In Linde M 2005 these were placed at the same predefined points as in the true treatment group. Facco 2008 had two sham groups: in one group the placebo needles were placed at correct, individualized points after the same full process of Chinese diagnosis as in the true treatment group. In the second group placebo needles were placed at standardized points without the ’Chinese ritual’ (to investigate whether the different interaction and process affected outcomes). In the remaining two trials (Ceccherelli 1992; Dowson 1985) other sham interventions without skin penetration were applied. Four trials compared acupuncture to prophylactic drug treatment with metoprolol (Hesse 1994; Streng 2006), flunarizine (Allais 2002) or individualized treatment according to guidelines (Diener 2006). In three of these trials participants were unblinded, while one blinded trial used a double-dummy approach (true acupuncture + metoprolol placebo vs. metoprolol + sham acupuncture; Hesse 1994). One trial compared acupuncture to a specific relaxation program (and a waiting list; Doerr-Proske 1985), and one to a combination of massage and relaxation (Wylie 1997).
Included patients
Most trials included patients diagnosed as having migraine with or without aura, or reported only that they included patients with migraine. One trial was restricted to women with migraine without aura (Allais 2002), one recruited only women with menstrually related migraine (Linde M 2005) and a third recruited only patients with migraine without aura (Linde M 2000). Two older, small trials explicitly stated that included patients had been non-responders to previous treatments (Baust 1978; Doerr-Proske 1985).
It is likely that there is some diagnostic inaccuracy in several trials. In two older trials (Dowson 1985; Vincent 1989) the high number of headache days during the baseline phase makes it seem likely that a relevant proportion of participants had additional tension-type headache. In two large, recent pragmatic, multicenter trials investigating the addition of acupuncture to routine care in primary care (Jena 2008; Vickers 2004), baseline headache frequency and the reported diagnoses make it likely that, in spite of the use of the criteria of the International Headache Society, there was some diagnostic misclassification. This applies to a minor extent also to three other recent multicenter trials (Diener 2006; Linde K 2005; Streng 2006). In the two large, pragmatic, routine care studies (Jena 2008; Vickers 2004), which left non-acupuncture treatment completely to the individual practitioner, it also seems likely that treatment of acute attacks was suboptimal in a relevant proportion of patients.
Treatment interventions
The acupuncture interventions tested in the included trials also varied to a great extent. In four trials (Allais 2002; Ceccherelli 1992; Doerr-Proske 1985; Henry 1985) acupuncture treatments were standardized (all patients were treated at the same points); in six (Alecrim 2006; Baust 1978; Diener 2006; Linde K 2005; Linde M 2000; Linde M 2005) treatments were semi-standardized (either all patients were treated at some basic points and additional individualized points, or there were different predefined needling schemes depending on symptom patterns); and in 12 trials the selection of acupuncture points was individualized (Alecrim 2005; Alecrim 2008; Dowson 1985; Facco 2008; Hesse 1994; Jena 2008; Streng 2006; Vickers 2004; Vincent 1989; Weinschütz 1993; Weinschütz 1994; Wylie 1997). In four trials treatment consisted of six acupuncture sessions (Baust 1978; Dowson 1985; Vincent 1989; Wylie 1997), which must be considered a low number for a chronic condition. In four trials 16 to 20 sessions were provided (Alecrim 2005; Alecrim 2006; Alecrim 2008; Facco 2008), while the remaining trials included between 7 and 15 sessions. In most trials reporting the duration of sessions, needles were left in place between 20 and 30 minutes; in one trial (Dowson 1985) needles were inserted for 10 minutes only, and one trial (Hesse 1994) investigated brief needling for a few seconds. In the case of one trial (Doerr-Proske 1985), both assessing acupuncturists had very little confidence that acupuncture was performed in an adequate manner and would have treated the patients in a completely different manner.
Outcome measurement
All but three trials (Facco 2008; Henry 1985; Jena 2008) used a headache diary for measuring primary outcomes. Two trials (Baust 1978; Ceccherelli 1992) did not include a pre-treatment baseline period. Twelve trials followed patients for 6 months or more after randomization. The complex headache data on frequency, intensity, medication use and response were presented in a highly variable manner, making systematic extraction difficult. Particularly, most small, older trials (Baust 1978; Ceccherelli 1992; Doerr-Proske 1985; Henry 1985; Hesse 1994; Weinschütz 1993; Weinschütz 1994; Wylie 1997) presented the findings in a way precluding effect size estimation for migraine days, migraine attacks, headache days, intensity and analgesic use.
Risk of bias in included studies
We discuss the methodological quality of trials (risk of bias) for the four comparisons separately, as problems differ according to control groups.
Comparisons with no acupuncture (acute treatment only or routine care)
The four largest trials (Facco 2008; Jena 2008; Linde K 2005; Vickers 2004) all used adequate methods for allocation sequence generation and concealment of allocation. For one trial (Linde M 2000) sequence generation was adequate but concealment was in-adequate. One trial (Doerr-Proske 1985) did not report any details on randomization, and we were not able to obtain additional information. Given the comparison between acupuncture and no acupuncture, the patients (who were also assessing all relevant outcomes) were unblinded in all six trials. In consequence, bias cannot be ruled out. The use of headache diaries to monitor symptoms closely over a long period of time (in Doerr-Proske 1985; Linde K 2005; Linde M 2000; Vickers 2004) might be less prone to bias than the use of questionnaires with retrospective assessment of symptoms for the preceding weeks. Attrition in the first 3 months was high in Linde M 2000 and minor to moderate in the remaining trials. The analyses of Jena 2008, Linde K 2005 and Vickers 2004 took account of attrition (primary or sensitivity analysis with missing values replaced that confirmed available data analyses), suggesting a low risk of bias. This applies also to the long-term follow-up in Vickers 2004, while Facco 2008 presented only a per protocol analysis. Although presentation of results was not always optimal, we considered the risk of selective reporting to be low as the most important outcome measures were always presented and consistent.
While comparisons with no acupuncture cannot be blinded and, therefore, bias cannot be ruled out in the patient assessment of the (subjective) headache outcomes in any trial, we consider the trials of Jena 2008, Linde K 2005 and Vickers 2004 to have a lower risk of bias compared to the other three trials.
Comparisons with sham interventions
We did not formally assess the quality of Alecrim 2005, for which only an abstract and additional unpublished information provided by the authors were available. Unpublished information provided by the authors and published information from the two other trials (Alecrim 2006; Alecrim 2008) conducted by the same group suggest that the risk of bias in this trial is low. Among the 13 trials formally assessed, the risk of bias regarding sequence generation was low for eight (Alecrim 2006; Alecrim 2008; Ceccherelli 1992; Diener 2006; Dowson 1985; Facco 2008; Linde K 2005; Linde M 2005) and unclear in five. Publications for four trials reported adequate methods of allocation concealment (Alecrim 2006; Alecrim 2008; Diener 2006; Linde K 2005); for a further two trials, such information was provided by the authors (Ceccherelli 1992; Facco 2008). In all trials there were attempts to blind patients. Several trials that used sham interventions which were not strictly indistinguishable from ’true’ acupuncture’ (Ceccherelli 1992; Diener 2006; Facco 2008; Linde K 2005) did not mention the use of a sham or placebo control in the informed consent procedure. This is ethically problematic, but enhances the credibility of the sham interventions. Taking into account also the results of the trials, we considered the risk of bias to be low in all trials except in one that used an distinguishable sham procedure and for which we could not obtain information on the method of informed consent (Dowson 1985). Reporting of dropouts was insufficient in several older trials. We considered the risk of bias to be low regarding short-term outcomes (up to 3 months) in seven trials, (Alecrim 2006; Alecrim 2008; Diener 2006; Dowson 1985; Linde K 2005; Linde M 2005; Vincent 1989), and low regarding long-term outcomes in four (Alecrim 2008; Diener 2006; Linde K 2005; Linde M 2005). For four trials (Baust 1978; Dowson 1985; Weinschütz 1993; Weinschütz 1994) outcomes were reported so insufficiently that selective reporting cannot be ruled out.
Five trials (Alecrim 2006; Alecrim 2008; Diener 2006; Linde K 2005; Linde M 2005) met all or all but one criteria and were therefore considered to be of higher quality.
Comparisons with prophylactic drug treatment
One trial (Hesse 1994) did not describe the methods for sequence generation and concealment, while these were adequate in the other three trials (Allais 2002; Diener 2006; Streng 2006). These three trials compared acupuncture and drug treatment in an open manner, which implies that bias on this level cannot be ruled out. The use of a double-dummy technique allowed patient blinding in Hesse 1994, but this approach might be associated with other problems (see Discussion). While there is little risk of bias due to low attrition rates in Allais 2002 and Hesse 1994, a relevant problem occurred in the two German trials (Diener 2006; Streng 2006). The recruitment situation for these trials made it likely that participants had a preference for acupuncture. This resulted in a high proportion of patients allocated to drug treatment withdrawing informed consent immediately after randomization (34% in Diener 2006 and 13% in Streng 2006), as well as high treatment discontinuation (18% in Diener 2006) or dropout rates due to adverse effects (16% in Streng 2006). These trials did not include patients refusing informed consent immediately after randomization in analyses, and one (Streng 2006) also excluded early dropouts. Such analyses should normally tend to favor drug treatment. Both trials presented additional analyses restricted to patients complying with the protocol. All four trials presented the most important outcomes measured, so we considered the risk of bias of selective reporting to be low.
Comparisons with other treatments
The two small trials comparing acupuncture with relaxation (Doerr-Proske 1985) or a combination of relaxation and massage (Wylie 1997) did not report on the methods used for generation of the allocation sequence, on concealment or on dropouts. Therefore, the risk of bias is unclear for these aspects. Patients were not blinded. Although the reporting of outcomes was suboptimal (no standard deviations, etc.), the most relevant outcomes measured were presented, and we considered the risk of bias of selective reporting to be low.
Effects of interventions
Comparisons with no acupuncture (acute treatment only or routine care)
The six trials comparing acupuncture with a control group receiving either treatment of acute migraine attacks only or routine care are clinically very heterogeneous. Doerr-Proske 1985 is a very small older trial investigating a probably inadequate acupuncture treatment (see assessments by acupuncturists in Characteristics of included studies) compared to both a relaxation control and a waiting list control. Facco 2008 performed a four-armed trial in which patients in the control group all received acute treatment with rizatriptan. Linde M 2000 was a small pilot trial (n = 39) performed in a specialized migraine clinic in Sweden in which control patients continued with their individualized treatment of acute attacks but did not receive additional acupuncture. A similar approach was used for the waiting-list control group in the three-armed (also sham control group) Linde K 2005 (n = 302) trial. Jena 2008 is a very large, highly pragmatic study which included a total of 15,056 headache patients recruited by more than 4000 physicians in Germany. A total of 11,874 patients not giving consent to randomization received up to 15 acupuncture treatments within 3 months and were followed for an additional 3 months. This was also the case for 1613 patients randomized to immediate acupuncture, while the remaining 1569 patients remained on routine care (not further defined) for 3 months and then received acupuncture. The published analysis of this trial is on all randomized patients, but the authors provided us with unpublished results of subgroup analyses on the 1715 patients with migraine. Finally, in the Vickers 2004 trial (n = 401), acupuncture in addition to routine care in the British National Health Service was compared to a strategy, ’avoid acupuncture.’ In addition to the strong clinical heterogeneity, the methods and timing of outcome measurement in these trials also differed considerably. Therefore, any pooled effect size measures in the forest plots should be interpreted only as very crude indicators of the overall direction of the findings. Nevertheless, the findings clearly show that response, headache frequency, headache days and headache scores 3 to 4 months after randomization are more favorable in patients receiving acupuncture (see Figure 1; Figure 2; Analysis 1.5; Analysis 1.8). Responder rate ratios 3 to 4 months after randomization in the four trials reporting this outcome varied between 1.43 and 3.53. For analgesic use, the findings differed strongly across studies (Analysis 1.7). Migraine attacks and migraine days were adequately measured in only two trials (Linde K 2005; Linde M 2000). Only Vickers 2004 included a long-term follow-up. In this study, patients who had received acupuncture still did significantly better than those receiving routine care 9 months after completion of treatment.
Figure 1.
Forest plot of comparison: 1 Acupuncture vs. no acupuncture, outcome: 1.1 Response.
Figure 2.
Forest plot of comparison: 1 Acupuncture vs. no acupuncture, outcome: 1.2 Headache frequency (various measures).
Analysis 1.5.
Comparison 1 Acupuncture vs. no acupuncture, Outcome 5 Headache days.
Analysis 1.8.
Comparison 1 Acupuncture vs. no acupuncture, Outcome 8 Headache scores.
Analysis 1.7.
Comparison 1 Acupuncture vs. no acupuncture, Outcome 7 Analgesic use.
Comparisons with sham interventions
The clinical heterogeneity of the 14 sham-controlled trials is less extreme than in the case of comparisons with no acupuncture, but is still considerable. Due to the variability of treatment and sham interventions, here too any pooled effect size estimates must be interpreted with caution. Furthermore, despite the very limited power (low number of trials), the Chi2-test for statistical heterogeneity was statistically significant (P < 0.05) in 9 of the 25 analyses and was close to significance (0.05 < p < 0.1) in a further three. I2-values were above 50% (indicating strong statistical heterogeneity) in 13 comparisons, and between 25% and 50% in a further four. Response measures were reported by 7 trials for the period up to 2 months after randomization, by 11 for 3 to 4 months, by 6 at 5 to 6 months, and by 3 after 6 months. Pooled responder rate ratios were not statistically significant at any period (see Figure 3). The same applies to mixed headache frequency measures (six, eight, five and four trials at the four different periods; see Figure 4), migraine attacks (four, five, four and four trials; Analysis 2.3), migraine days (five, six, five and four trials; Analysis 2.4), headache days (two, two, two and zero trials; Analysis 2.5), headache intensity (zero, three, three and 1 trials; Analysis 2.6), analgesic use (four, six, five and four trials; Analysis 2.7) and headache scores (one, three, two and zero trials; Analysis 2.8). There was some evidence of group differences (0.05 < p < 0.1) in four analyses (responder rate ratio, headache frequency, migraine days and migraine attacks up to 2 months after randomization).
Figure 3.
Forest plot of comparison: 2 Acupuncture vs. sham interventions, outcome: 2.1 Response.
Figure 4.
Forest plot of comparison: 2 Acupuncture vs. sham interventions, outcome: 2.2 Headache frequency (various measures).
Analysis 2.3.
Comparison 2 Acupuncture vs. sham interventions, Outcome 3 Migraine attacks.
Analysis 2.4.
Comparison 2 Acupuncture vs. sham interventions, Outcome 4 Migraine days.
Analysis 2.5.
Comparison 2 Acupuncture vs. sham interventions, Outcome 5 Headache days.
Analysis 2.6.
Comparison 2 Acupuncture vs. sham interventions, Outcome 6 Headache intensity.
Analysis 2.7.
Comparison 2 Acupuncture vs. sham interventions, Outcome 7 Analgesic use.
Analysis 2.8.
Comparison 2 Acupuncture vs. sham interventions, Outcome 8 Headache scores.
When restricted to the five studies of higher quality (Alecrim 2006; Alecrim 2008; Diener 2006; Linde K 2005; Linde M 2005), analyses of response and headache frequency also failed to yield significant differences between acupuncture and sham acupuncture.
Comparisons with prophylactic drug treatment
The results of Hesse 1994 regarding treatment effectiveness were not reported in amanner that allowed effect size estimation. Overall, the findings of this trial, which used a double-dummy design (true acupuncture + metoprolol placebo vs. metoprolol + sham acupuncture), show similar improvements in both groups, slightly favouring the metoprolol + sham acupuncture group. The acupuncture technique used in this trial (very brief needling of individual trigger points) is rather unusual. The remaining three trials all reported at least some frequency data (migraine attacks and/or migraine days). Findings were consistent among trials, and the pooled standardized mean differences were statistically significant in favour of acupuncture in the first three time periods (none of the trials had a follow-up beyond 6 months; see Figure 5). For response (see Figure 6), migraine attacks (Analysis 3.3), migraine days (Analysis 3.4), headache intensity (Analysis 3.6) and analgesic use (Analysis 3.7), effect size estimates could be calculated for at least two trials. The reduction of analgesic use was similar in patients receiving acupuncture and prophylactic drug treatment, but for several time windows, results for response, migraine attacks, migraine days and intensity were statistically significant in favour of the acupuncture groups.
Figure 5.
Forest plot of comparison: 3 Acupuncture vs. drug treatment, outcome: 3.2 Headache frequency (various measures).
Figure 6.
Forest plot of comparison: 3 Acupuncture vs. drug treatment, outcome: 3.1 Response.
Analysis 3.3.
Comparison 3 Acupuncture vs. drug treatment, Outcome 3 Migraine attacks.
Analysis 3.4.
Comparison 3 Acupuncture vs. drug treatment, Outcome 4 Migraine days.
Analysis 3.6.
Comparison 3 Acupuncture vs. drug treatment, Outcome 6 Headache intensity.
Analysis 3.7.
Comparison 3 Acupuncture vs. drug treatment, Outcome 7 Analgesic use.
All four trials described the number of patients reporting adverse effects. In all four, more patients receiving drug treatment reported adverse effects than patients receiving acupuncture, but the difference was less pronounced in the largest trial (Diener 2006) compared to the other three trials (test for heterogeneity P = 0.01, I2 = 73.1%). The pooled odds ratio was 0.47 (95% confidence interval 0.34 to 0.65; Analysis 3.9). In the two trials reporting the number of dropouts due to adverse effects, this was lower in patients receiving acupuncture (Analysis 3.10).
Analysis 3.9.
Comparison 3 Acupuncture vs. drug treatment, Outcome 9 Number of patients reporting adverse effects.
Analysis 3.10.
Comparison 3 Acupuncture vs. drug treatment, Outcome 10 Number of patients dropping out due to adverse effects.
Comparisons with other treatments
The two small trials comparing acupuncture with relaxation (Doerr-Proske 1985) and a combination of relaxation and massage (Wylie 1997) did not report any outcome measures in a manner usable for calculation of effect size estimates. In Doerr-Proske 1985 overall results suggest short- and long-term superiority of the relaxation program compared to the probably inadequate acupuncture intervention. Wylie 1997 reported a significantly larger short-term (no follow-up beyond 2 months) reduction of pain total and headache scores in the group receiving massage and relaxation, but baseline values were much lower in the acupuncture group (189 vs. 326 for the pain total score, and 23 vs. 38 for the headache index). The mean number of migraine days decreased from 7.1 to 1.7 in the acupuncture group, and from 7.5 to 2.7 in the massage and relaxation group.
DISCUSSION
Summary of main results
In recent years, the evidence base for acupuncture as a prophylactic treatment for headache has grown considerably due to the publication of several large trials of high quality. Still, the results are challenging and not easy to interpret. Several trials using quite variable methods and interventions consistently show that the addition of acupuncture to treatment of acute migraine attacks or to routine care is beneficial for at least 3 months. Compared to routine care, which includes treatment of acute migraine attacks and possibly other interventions, the size of the effect seems to be small to moderate (according to usual standards for classifying effect size measures such as standardized mean differences); it seems to be larger compared to acute treatment only. The only trial which investigated long-term effects showed a sustained moderate response to acupuncture in addition to routine care provided by a GP. There is currently no evidence that the acupuncture interventions tested had relevant effects over their sham comparators, although a number of single trials report significant findings. At the same time, the pooled analyses of the available trials comparing acupuncture interventions with evidence-based prophylactic drug treatment found a superiority of acupuncture. The findings from two small older trials comparing acupuncture and relaxation interventions are not reliably interpretable.
Possible explanations for the findings
The findings of our review seem contradictory: on the one hand, the available evidence suggests that acupuncture is an effective adjunct to routine care and at least as effective as prophylactic treatment with drugs that have been shown to be superior to placebo (Schürks 2008). On the other hand, ’true’ acupuncture interventions do not seem to be superior to sham interventions. Three factors could explain these findings (possibly in combination): 1) Acupuncture might be a particularly potent placebo; 2) sham acupuncture might have direct physiological effects affecting mechanisms relevant for migraine symptoms; 3) due to the lack of blinding, comparisons with routine care and prophylactic drug treatment might be biased.
We consider each of these possible explanations in turn:
Although the average effect of placebo interventions seems to be small (Hróbjartsson 2004), there is evidence that more complex placebos are associated with larger effects (Kaptchuk 2000). There is also some direct evidence that a sham acupuncture intervention is associated with a larger response than a pill (Kaptchuk 2006). A recent trial has shown that the size of the effect associated with a sham acupuncture intervention can vary with the amount and charactersitics of the patient-provide interaction (Kaptchuk 2008). According to the available evidence, the most important mechanisms for placebo effects are expectations, conditioning, anxiety reduction and social support (Crow 1999; Benedetti 2008). These elements are likely to be influenced by the treatment setting, its context and its meaning. Acupuncture - with its repeated sessions, intense provider contact, slightly painful procedure, an often ’exotic’ model of symptom explanation and associated relaxation during sessions - might maximize such effects.
Many sham acupuncture procedures involve needling locations that are not traditional points with the same frequency and duration as in the true acupuncture group. In some studies needles are inserted into classical acupuncture points not indicated in migraine. Most physiological mechanisms proposed for acupuncture do not necessarily imply point specificity (Bäcker 2004). Even the non-penetrating ’placebo’ needles might activate unmyelinated (C ’tactile’) afferent nerves which can influence pain perception (Lund 2006). Several researchers have argued that some effects of acupuncture might not be point-specific (Han 1997; Lundeberg 2007), and that these might be particularly relevant for treating conditions other than localized nociceptive pain (Thomas 1996). Both explanation 1 and 2 would also imply that it would be difficult to detect any small, point-specific effects in addition to potent placebo effects and non-specific needling effects.
While patients in the sham-controlled trials were blinded, this was (with the exception of the trial by Hesse 1994) not the case for the comparisons with treatment of acutemigraine attacks only, routine care or other treatments. All clinically relevant outcome measures in clinical trials in migraine are patient-reported (IHS 2000). Preferably outcomes are documented in diaries at least for 4 weeks before treatment and for longer time periods during and after treatment. It cannot be ruled out that patients allocated to acupuncture reported positively biased outcomes, while patients allocated to control reported negatively biased outcomes. However, response rates in patients allocated to drug treatment in the trials included in this review were comparable to those reported in drug trials (Van der Kuy 2002). Also, in groups receiving acute treatment only, response rates were within the range of placebo groups in drug trials (Van der Kuy 2002). In two trials comparing acupuncture and drug treatment (Diener 2006; Streng 2006), a relevant proportion of patients withdrew informed consent immediately after allocation to drug treatment. Additional patients dropped out during the study. This indicates that study participants had a preference for acupuncture. These problems could severely bias the findings. However, patients not starting treatment were not included in the analyses, and per-protocol analyses confirmed the study findings. Still, these trials must be interpreted with caution.
A fourth possible explanation for the lack of effects of true acupuncture over sham comes from the perspective of acupuncture practitioners. The quality of acupuncture interventions in clinical trials is often disputed. Study protocols often limit the flexibility of treatment procedures, particularly in sham-controlled trials, and it is argued that better acupuncturists would have achieved better results. However, response rates in sham-controlled trials were on average similar to those in pragmatic trials with flexible treatments. Furthermore, while there is always the possibility that some expert acupuncturists are particularly successful, in several of the larger trials included in this review the training of treatment providers was at least comparable to that of the average acupuncturists in their country. Still, it cannot be ruled out that inadequate study interventions contribute to the lack of differences compared to sham interventions.
It should be noted that a statistically significant difference between ’true’ and sham acupuncture interventions was found in our systematic review on trials in patients with tension-type headache (Linde 2009). This review, however, included a smaller number of studies, and pooled effect estimates were stronly influenced by one large trial.
Quality of the evidence
The quality of clinical trials of acupuncture for headache has clearly improved since the last version of our review. Methods for sequence generation, allocation concealment, handling of dropouts and withdrawals and reporting of findings were adequate in most of the recent trials. Still, designing and performing clinical trials of acupuncture is a challenge, particularily with respect to blinding and selection of control interventions. We have mentioned that bias cannot be ruled out in the unblinded studies, and that comparisons with prophylactic drug treatment have to be interpreted with caution due to high dropout rates in two of the trials. Blinding in comparisons with drug treatment could be achieved by double-dummy designs (drug + sham acupuncture vs. acupuncture + drug placebo) as in the trials by Hesse 1994. However, if it is the case that sham acupuncture interventions might be strong placebos and not physiologically inert, this approach would also be problematic.
Overall completeness and applicability of the evidence
Acupuncture is a therapy which is applied in a variable manner in different countries and settings. For example, in Germany, where the majority of the large trials included in this review were performed, acupuncture is mainly provided by general practitioners and other physicians. Their approach to acupuncture is based on the theories of traditional Chinese medicine, although the amount of training they receive in traditional Chinese medicine is limited (Weidenhammer 2007). In the UK, the providers are likely to be non-medical acupuncturists with a comparatively intense traditional training, physiotherapists or medical doctors with a more ’Western’ approach (Dale 1997). The trials included in our review come from a variety of countries, and study designs range from very pragmatic (Jena 2008; Vickers 2004) to more experimental (Linde M 2005). Despite this strong heterogeneity, within comparisons the findings are quite consistent. Large-scale observational studies (Jena 2008; Melchart 2006), a review of smaller observational studies (Linde 2002) and a systematic comparison of findings from a randomized and an observational study (Linde 2007a) suggest that the response rates observed in clinical trials are also seen in conditions similar to routine practice. However, as the overall evidence also suggests that factors other than the correct selection of acupuncture points and needling procedures play an important role in outcomes, treatment setting and patient selection could have a strong impact and might vary considerably. For example, a pooled analysis of four trials on chronic pain (including Linde K 2005) found that even 4 months after completion of treatment, patients who had started acupuncture with a positive attitude and expectation had significantly better outcomes than patients with lower expectations (Linde 2007b).
Potential biases in the review process
We are confident that we have identified the existing large clinical trials relevant to our question, but we cannot rule out the possibility that there are additional small trials which are unpublished or published in sources not accessible to our search. We have not systematically searched Chinese databases for this version of the review, but we assume that Chinese trials meeting our selection criteria exist. The few Chinese trials identified through our literature search did not meet the inclusion criteria. There is considerable skepticism toward clinical trials from China, as in the past results were almost exclusively positive (Vickers 1998). However, the quality and number of randomized trials published in Chinese have improved over the last years (Wang 2007), and it seems in-adequate to neglect this evidence without examining it critically. For the next update of this review we plan to include researchers and evidence from China to overcome this shortcoming.
A relevant problem for systematic reviews on prophylactic treatments of migraine is the highly variable outcome measurement and the often insufficient reporting of results. Various measures of frequency, intensity, analgesic use and other outcomes are used, and as these measures have to be observed over longer time periods, the amount of data needed to obtain a good overview of the course of symptoms is considerable. Most trials in our review reported several outcome measures at different time points without evidence that these were selected in a biased way. Nevertheless, we were confronted with a complex mosaic of data. Several authors kindly provided unpublished data. Some sort of response and frequency measure was available for almost all trials, although the timing of the measurement and details of the measure often differed. As overall results are rather consistent, it seems unlikely that our results would have changed in a relevant manner if missing data had been available.
Four members of the review team were involved in at least one of the included trials. These trials were assessed by other members of the review team. All reviewers currently have affiliations to a CAM (complementary and alternative medicine) research center, or have had such an affiliation in the past.
Agreements and disagreements with other studies and reviews
Our findings are in good accordance with a recent systematic review published in an acupuncture journal (Scott 2006). Using slightly wider inclusion criteria regarding methodology and condition, the Scott review summarized a total of 25 trials. Another systematic review published in 2006 (Griggs 2006) did not include trials published after 2004, excluded trials published in languages other than English, and included trials on other headaches, although the title suggests a focus on migraine. The conclusion that large trials are needed is not based on the most current evidence. Only five of the trials included in our review were included in the Griggs 2006 review. The remaining trials included in Griggs 2006 were either on tension-type headache (n = 6) or mixed populations (n = 1) or, in one case, a migraine trial that was excluded by us (Liguori 2000) because we had severe doubts that allocation was truly randomized. A large narrative review focusing on recent trials (Endres 2007) also draws conclusions similar to ours.
Safety and cost-effectiveness
The assessment of safety was not a predefined objective of this review. Post-hoc analyses for comparisons with prophylactic drug treatments found fewer patients reporting adverse effects and fewer dropouts due to adverse effects in the acupuncture groups. We will include a more formal assessment of safety in future versions of this review. Several large-scale observational studies have provided good evidence that acupuncture is a comparatively safe intervention (White 2001; MacPherson 2001; Weidenhammer 2007; Witt 2006). Severe adverse effects such as pneumothorax are very rare. However, between 8% and 11% of patients report minor adverse effects such as fatigue or temporary aggravations (Witt 2006; Melchart 2006).
For the two large pragmatic trials included in our review (Vickers 2004; Jena 2008), detailed cost-effectiveness analyses are available (Wonderling 2004; Witt 2008). Both analyses show that costs within the study periods (12 months in Vickers 2004 and 3 months in Jena 2008) were higher in the groups receiving acupuncture than in those receiving routine care because of acupuncture practitioners’ costs. Cost-effectiveness was assessed by calculating incremental costs per quality-adjusted life year. The resulting estimates were 13.600 Euro in the analysis by Wonderling 2004 and 11.700 Euro in the analysis by Witt 2008. Both groups concluded that according to international threshold values, acupuncture seems to be a cost-effective treatment.
AUTHORS’ CONCLUSIONS
Implications for practice
Although the available results suggest that the selection of specific points is not as important as had been thought by providers, acupuncture should be considered as a treatment option for migraine patients needing prophylactic treatment due to frequent or insufficiently controlled migraine attacks, particularly in patients refusing prophylactic drug treatment or experiencing adverse effects from such treatment.
Implications for research
There is a clear need for further studies. A priority, in our opinion, should be to investigate whether the high response rates observed in conditions similar to routine care in Germany and the UK are reproducible elsewhere. As migraine is a chronic condition, it would be important for clinicians to know how long improvements associated with acupuncture treatment last and whether a further treatment cycle again leads to improvement. These latter questions might be best investigated in cohort studies. Available studies have been rather unsuccessful at identifying reliable predictors for treatment response (Jena 2008; Weidenhammer 2006); these issues could also be investigated in observational studies. For decision makers it would be important to know who is sufficiently qualified to deliver acupuncture. Studies from Germany did not find an association between factors such as amount of training or professional experience and treatment response (Jena 2008; Weidenhammer 2006), but these studies were limited to physicians. Randomized trials comparing outcomes after treatment by different types of practitioners are desirable, although large sample sizes would be needed. Such studies would also be interesting from a more scientific perspective because it is unclear to what extent the effects of acupuncture are mainly mediated by context variables and generalised (i.e., not specific to traditional points) needling effects, and what contribution correct point location makes. Although future sham-controlled trials might find ’specific’ effects over sham interventions, we think that such studies should not have the highest priority unless they also address other important questions. Other aspects that deserve further research include questions such as which types of acupuncture work best, what is the optimal frequency and duration of sessions, and so on. Future comparisons with other non-drug interventions (such as relaxation) should have sufficient sample size. To facilitate future meta-analyses, it would be helpful if some standards for reporting outcome data were established.
Supplementary Material
Analysis 1.1.
Comparison 1 Acupuncture vs. no acupuncture, Outcome 1 Response.
Analysis 1.2.
Comparison 1 Acupuncture vs. no acupuncture, Outcome 2 Headache frequency (various measures).
Analysis 1.3.
Comparison 1 Acupuncture vs. no acupuncture, Outcome 3 Migraine attacks.
Analysis 1.4.
Comparison 1 Acupuncture vs. no acupuncture, Outcome 4 Migraine days.
Analysis 1.6.
Comparison 1 Acupuncture vs. no acupuncture, Outcome 6 Headache intensity.
Analysis 2.1.
Comparison 2 Acupuncture vs. sham interventions, Outcome 1 Response.
Analysis 2.2.
Comparison 2 Acupuncture vs. sham interventions, Outcome 2 Headache frequency (various measures).
Analysis 2.9.
Comparison 2 Acupuncture vs. sham interventions, Outcome 9 Response (for funnel plot).
Analysis 2.10.
Comparison 2 Acupuncture vs. sham interventions, Outcome 10 Response (higher quality studies).
Analysis 2.11.
Comparison 2 Acupuncture vs. sham interventions, Outcome 11 Headache frequency (various measures - for funnel plot).
Analysis 2.12.
Comparison 2 Acupuncture vs. sham interventions, Outcome 12 Headache frequency (various measures - higher quality studies).
Analysis 3.1.
Comparison 3 Acupuncture vs. drug treatment, Outcome 1 Response.
Analysis 3.2.
Comparison 3 Acupuncture vs. drug treatment, Outcome 2 Headache frequency (various measures).
Analysis 3.5.
Comparison 3 Acupuncture vs. drug treatment, Outcome 5 Headache days.
Analysis 3.8.
Comparison 3 Acupuncture vs. drug treatment, Outcome 8 Headache scores.
Analysis 4.2.
Comparison 4 Acupuncture vs. other therapy, Outcome 2 Headache frequency (various measures).
Analysis 4.7.
Comparison 4 Acupuncture vs. other therapy, Outcome 7 Analgesic use.
ACKNOWLEDGEMENTS
We would like to thank the study authors who provided additional information on their trials.
Dieter Melchart, Patricia Fischer and Brian Berman were involved in previous versions of the review. Eva Israel helped assess eligibility. Lucia Angermayer helped with data checks and quality assessments. Sylvia Bickley performed search updates, and Becky Gray helped in various ways.
SOURCES OF SUPPORT
Internal sources
No sources of support supplied
External sources
NIAMS Grant No 5 U24-AR-43346-02, USA.
-
International Headache Society, Not specified.
For administrative costs associated with editorial review and peer review of the original version of this review.
-
National Center for Complementary and Alternative Medicine (NCCAM), USA.
Eric Manheimer’s work was funded by Grant Number R24 AT001293 from the National Center for Complementary and Alternative Medicine (NCCAM)
Appendix 1
Search strategies
PaPaS trials register search strategy
((acupunctur* OR electroacupunct* or electro-acupunct*) AND (headache* OR migrain* OR hemicrania OR cephalgi* or cephalalgi*))
CENTRAL search strategy
-
#1
ACUPUNCTURE THERAPY/ Single MeSH
-
#2
ELECTROACUPUNCTURE/ Single MeSH
-
#3
(acupunct* or electroacupunct* or electro-acupunct*)
-
#4
#1 or #2 or #3
-
#5
exp HEADACHE DISORDERS/
-
#6
HEADACHE/ Single MeSH
-
#7
(headache* or migraine* or cephalgi* or cephalalgi*)
-
#8
#5 or #6 or #7
-
#9
#4 and #8
MEDLINE via OVID subject search strategy
ACUPUNCTURE THERAPY/
ELECTROACUPUNCTURE/
(acupunct$ or electroacupunct$ or electro-acupunct$).mp. [mp=title, original title, abstract, name of substance word, subject heading word]
or/ 1–3
exp HEADACHE DISORDERS/
HEADACHE/
(headache$ or migrain$ or cephalgi$ or cephalalgi$).mp. [mp=title, original title, abstract, name of substance word, subject heading word]
or/ 5–7
4 and 8
The above subject search was linked to the following MEDLINE via OVID Cochrane sensitive search strategy for RCTs
(Revised SRB Jan 07)
randomized controlled trial.pt.
controlled clinical trial.pt.
randomized controlled trials as topic/
random allocation.sh.
double blind method.sh.
single blind method.sh.
or/ 1–6
(ANIMALS not HUMANS).sh.
7 not 8
clinical trial.pt.
exp clinical trials as topic/
(clin$ adj25 trial$).ti,ab.
((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).ti,ab.
placebos.sh.
placebo$.ti,ab.
random$.ti,ab.
research design.sh.
or/ 10–17
18 not 8
19 not 9
9 or 19
EMBASE via OVID subject search strategy
ACUPUNCTURE/
ELECTROACUPUNCTURE/
(acupunct$ or electroacupunct$ or electro-acupunct$).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name]
or/ 1–3
HEADACHE/
(headache$ or migrain$ or cephalgi$ or cephalalgi$).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name]
or/5–6
4 and 7
The above subject search was linked to the following Study design filter for EMBASE via OVID
random$.ti,ab.
factorial$.ti,ab.
(crossover$ or cross over$ or cross-over$).ti,ab.
placebo$.ti,ab.
(doubl$ adj blind$).ti,ab.
(singl$ adj blind$).ti,ab.
assign$.ti,ab.
allocat$.ti,ab.
volunteer$.ti,ab.
CROSSOVER PROCEDURE.sh.
DOUBLE-BLIND PROCEDURE.sh.
RANDOMIZED CONTROLLED TRIAL.sh.
SINGLE BLIND PROCEDURE.sh.
or/1–3
ANIMAL/ or NONHUMAN/ or ANIMAL EXPERIMENT/
HUMAN/
16 and 15
15 not 17
14 not 18
COCHRANE Complementary Medicine Field trials register
This register was searched via CENTRAL using the search strategy described above.
Footnotes
CONTRIBUTIONS OF AUTHORS
All reviewers participated in the development of the protocol, the extraction and assessment of the primary studies and the review of the final manuscript. KL coordinated the review process and wrote the draft of the review.
DECLARATIONS OF INTEREST
This review includes trials in which some of the reviewers were involved, as follows: Allais 2002 - Gianni Allais; Jena 2008 - Benno Brinkhaus; Linde K 2005 - Benno Brinkhaus and Klaus Linde; Streng 2006 - Klaus Linde; and Vickers 2004 - Andrew Vickers. These trials were reviewed by at least two other members of the review team. Gianni Allais, Benno Brinkhaus and Adrian White use acupuncture in their clinical work. Gianni Allais receives fees for teaching acupuncture in private schools. Klaus Linde has received travel reimbursement and, in two cases, fees from acupuncture societies (British, German and Spanish Medical Acupuncture Societies; Society of Acupuncture Research) for speaking about research at conferences. Eric Manheimer and Andrew Vickers both received an honorarium for preparing and delivering presentations on acupuncture research at the 2007 meeting of the Society for Acupuncture Research. Adrian White is employed by the British Medical Acupuncture Society as journal editor and has received fees and travel reimbursements for lecturing on acupuncture on several occasions. Benno Brinkhaus has received travel reimbursement and fees for presenting research findings at meetings of acupuncture societies (British, German and Spanish Medical Acupuncture Societies).
REFERENCES
References to studies included in this review
- Alecrim-Andrade J, Maciel-Júnior JA, Carne i Cladellas X, Correa-Filho HR, Machado HC, Vasconcelos GMS. Efficacy of acupuncture in migraine attack prophylaxis: a randomized sham-controlled trial. Cephalalgia. 2005;25(10):942. doi: 10.1111/j.1468-2982.2006.01062.x. [DOI] [PubMed] [Google Scholar]
- Alecrim-Andrade J, Maciel-Júnior JA, Carne i Cladellas X, Correa-Filho HR, Machado HC, Vasconcelos GMS. The long-lasting response of acupuncture treatment for migraine prophylaxis: 44 weeks' post-treatment follow-up. Cephalalgia. 2005;25(10):942–943. [Google Scholar]
- Alecrim-Andrade J, Maciel-Júnior JA, Cladellas XC, Correa-Filho HR, Machado HC. Acupuncture in migraine prophylaxis: a randomized sham-controlled trial. Cephalalgia. 2006;26(5):520–529. doi: 10.1111/j.1468-2982.2006.01062.x. [MEDLINE: 16674760] [DOI] [PubMed] [Google Scholar]
- Alecrim-Andrade J, Maciel-Júnior JA, Carnè X, Severino Vasconcelos GM, Correa-Filho HR. Acupuncture in migraine prevention: a randomized sham controlled study with 6-months posttreatment follow-up. Clinical Journal of Pain. 2008;24(2):98–105. doi: 10.1097/AJP.0b013e3181590d66. [MEDLINE: 18209514] [DOI] [PubMed] [Google Scholar]
- Alecrim-Andrade J, Maciel-Júnior JA, Carnè X, Vascocelos GMS, Correa-Filho HR. Acupuncture in migraine prevention: a randomized sham controlled study with 6-months post-treatment follow-up. Journal of Alternative and Complementary Medicine. 2007;13(8):891. [Google Scholar]
- Allais G, De Lorenzo C, Quirico PE, Airola G, Tolardo G, Mana O, et al. Acupuncture in the prophylactic treatment of migraine without aura: a comparison with flunarizine. Headache. 2002;42(9):855–861. doi: 10.1046/j.1526-4610.2002.02203.x. [MEDLINE: 12390610] [DOI] [PubMed] [Google Scholar]
- Baust W, Stürtzbecher KH. Management of migraine using acupuncture in a double-blind study [Akupunkturbehandlung der Migräne im Doppelblindversuch] Medizinische Welt. 1978;29(16):669–673. [MEDLINE: 347221] [PubMed] [Google Scholar]
- Ceccherelli F, Ambrosio F, Avila M, Duse G, Munari A, Giron GP. Acupuncture vs. placebo in the common migraine: a double-blind study. Cephalalgia. 1987;7 Suppl 6:499–500. [Google Scholar]
- Ceccherrelli F, Altafini L, Rossato M, Meneghetti O, Duse G, Donolato C, et al. Acupuncture in migraine without aura. Double blind placebo controlled study [Trattamento agopunturale dell’ emicrania senz’aura. Studio in doppio cieco vs. placebo] Atti - XV Congresso Nazionale A.I.S.D. S. Margherita Ligure: Associazione Italiana per lo Studio del Dolore. 1992:310–318.
- Diener HC, Kronfeld K, Boewing G, Lungenhausen M, Maier C, Molsberger A, et al. GERAC Migraine Study Group. Efficacy of acupuncture for the prophylaxis of migraine: a multicentre randomised controlled clinical trial. Lancet Neurology. 2006;5(4):310–316. doi: 10.1016/S1474-4422(06)70382-9. [MEDLINE: 16545747] [DOI] [PubMed] [Google Scholar]
- Molsberger AF, Boewing G, Diener HC, Endres HG, Kraehmer N, Kronfeld K, et al. Designing an acupuncture study: the nationwide, randomized, controlled German acupuncture trials on migraine and tension-type headache. Journal of Alternative and Complementary Medicine. 2006;12(3):237–245. doi: 10.1089/acm.2006.12.237. [MEDLINE: 16646722] [DOI] [PubMed] [Google Scholar]
- Doerr-Proske H, Wittchen HU. A muscle and vascular oriented relaxation program for the treatment of chronic migraine patients. A randomized clinical comparative study [Ein muskel– und gefässorientiertes Entspannungsprogramm (SEP) zur Behandlung chronischer Migränepatienten. Eine randomisierte klinische Vergleichsstudie] Zeitschrift für Psychosomatische Medizin und Psychoanalyse. 1985;31(3):247–266. [MEDLINE: 3898645] [PubMed] [Google Scholar]
- Wittchen HU, Lässle R. The situation-specific relaxation program for patients with chronic migraine - stability and specificity of the therapeutic effects [Das situationsspezifische Entspannungsprogramm (SEP) für chronische Migränepatienten – Stabilität und Spezifität der therapeutischen Veränderungen] In: Wittchen HU, Brengelmann JC, editors. Psychologische Therapie chronischer Schmerzen. Berlin: Springer; 1985. pp. 24–49. [Google Scholar]
- Dowson DI, Lewith GT, Machin D. The effects of acupuncture versus placebo in the treatment of headache. Pain. 1985;21(1):35–42. doi: 10.1016/0304-3959(85)90074-0. [MEDLINE: 3982837] [DOI] [PubMed] [Google Scholar]
- Facco E, Liguori A, Petti F, Zanette G, Coluzzi F, De Nardin M, et al. Traditional acupuncture in migraine: a controlled, randomized study. Headache. 2008;48(3):398–407. doi: 10.1111/j.1526-4610.2007.00916.x. [MEDLINE: 17868354] [DOI] [PubMed] [Google Scholar]
- Henry P, Baille H, Dartigues F, Jogeix M. Headaches and acupuncture. In: Pfaffenrath V, Lundberg PO, Sjaastad O, editors. Updating in headache. Berlin: Springer; 1985. pp. 208–216. [Google Scholar]
- Hesse J, Mogelvang B, Simonsen H. Acupuncture versus metoprolol in migraine prophylaxis: a randomized trial of trigger point inactivation. Journal of Internal Medicine. 1994;235(5):451–456. doi: 10.1111/j.1365-2796.1994.tb01102.x. [MEDLINE: 8182401] [DOI] [PubMed] [Google Scholar]
- Jena S, Becker-Witt C, Brinkhaus B, Selim D, Willich S. Effectiveness of acupuncture treatment for headache - the Acupuncture in Routine Care Study (ARC-Headache) Focus on Alternative and Complementary Therapies. 2004;9 Suppl:17. [Google Scholar]
- Jena S, Witt CM, Brinkhaus B, Wegscheider K, Willich SN. Acupuncture in patients with headache. Cephalalgia. 2008;Vol. 28(issue 9):969–979. doi: 10.1111/j.1468-2982.2008.01640.x. [DOI] [PubMed] [Google Scholar]
- Linde K, Streng A, Hoppe A, Brinkhaus B, Witt CM, Hammes M, et al. Treatment in a randomized multicenter trial of acupuncture for migraine (ART migraine) Forschende Komplementärmedizin. 2006;13(2):101–108. doi: 10.1159/000091999. [MEDLINE: 16645290] [DOI] [PubMed] [Google Scholar]
- Linde K, Streng A, Jürgens S, Hoppe A, Brinkhaus B, Witt C, et al. Acupuncture for patients with migraine: a randomized controlled trial. JAMA. 2005;293(17):2118–2125. doi: 10.1001/jama.293.17.2118. [MEDLINE: 15870415] [DOI] [PubMed] [Google Scholar]
- Melchart D, Linde K, Streng A, Reitmayr S, Hoppe A, Brinkhaus B, et al. Acupuncture Randomized Trials (ART) in patients with migraine or tension-type headache - design and protocols. Forschende Komplementärmedizin und Klassische Naturheilkunde. 2003;10:179–184. doi: 10.1159/000073473. [MEDLINE: 12972722] [DOI] [PubMed] [Google Scholar]
- Linde MA, Carlsson JY, Dahlöf CG. Impact of acupuncture as add-on therapy to pharmacological treatment of migraine: a pilot study. Pain Clinic. 2000;12:247–252. [Google Scholar]
- Linde M, Fjell A, Carlsson J, Dahlöf C. Role of the needling per se in acupuncture as prophylaxis for menstrually related migraine: a randomized placebo-controlled study. Cephalalgia. 2005;25(1):41–47. doi: 10.1111/j.1468-2982.2004.00803.x. [MEDLINE: 15606569] [DOI] [PubMed] [Google Scholar]
- Streng A, Linde K, Hoppe A, Pfaffenrath V, Hammes M, Wagenpfeil S, et al. Effectiveness and tolerability of acupuncture compared with metoprolol in migraine prophylaxis. Headache. 2006;46(10):1492–1502. doi: 10.1111/j.1526-4610.2006.00598.x. [MEDLINE: 17115982] [DOI] [PubMed] [Google Scholar]
- Vickers A, Rees R, Zollman C, Smith C, Ellis N. Acupuncture for migraine and headache in primary care: a protocol for a pragmatic, randomized trial. Complementary Therapies in Medicine. 1999;7(1):3–18. doi: 10.1016/s0965-2299(99)80053-3. [MEDLINE: 10361566] [DOI] [PubMed] [Google Scholar]
- Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al. Acupuncture for chronic headache in primary care: large, pragmatic, randomised trial. BMJ. 2004;328(7442):744–747. doi: 10.1136/bmj.38029.421863.EB. [MEDLINE: 15023828] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al. Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis. Health Technology Assessment. 2004;8(48):1–50. doi: 10.3310/hta8480. [MEDLINE: 15527670] [DOI] [PubMed] [Google Scholar]
- Vincent CA. A controlled trial of the treatment of migraine by acupuncture. Clinical Journal of Pain. 1989;5(4):305–312. doi: 10.1097/00002508-198912000-00006. [MEDLINE: 2520420] [DOI] [PubMed] [Google Scholar]
- Weinschütz T. Acupuncture in headache therapy [Akupunktur bei Kopfschmerzen] Schmerz. 1996;10(3):149–155. doi: 10.1007/s004829600044. [DOI] [PubMed] [Google Scholar]
- Weinschütz T, Lindner V, Niederberger U, Schreiber J, Soyka D. Potentials and limitations of acupuncture in a neurological pain outpatient unit: re-evaluation of therapeutic efficacy in the case of migraine [Möglichkeiten und Grenzen der Akupunktur in einer neurologischen Schmerzambulanz: Reevaluierung der klinischen Wirkung am Beispiel der Migränebehandlung] In: Schimrigk K, editor. Verhandlungen der Deutschen Gesellschaft für Neurologie. Band 7. Berlin: Springer; 1993. pp. 533–534. [Google Scholar]
- Weinschütz T, Niederberger U. The value of acupuncture in migraine therapy [Zum Stellenwert der Akupunktur in der Migränetherapie] Nervenheilkunde. 1995;14:295–301. [Google Scholar]
- Weinschütz T, Niederberger U, Johnsen S, Schreiber J, Kropp P. The neuroregulative effects of acupuncture in patients with headache [Zur neuroregulativen Wirkung der Akupunktur bei Kopfschmerzpatienten] Deutsche Zeitschrift für Akupunktur. 1994;37:106–117. [Google Scholar]
- Weinschütz T. Acupuncture in headache therapy [Akupunktur bei Kopfschmerzen] Schmerz. 1996;10(3):149–155. doi: 10.1007/s004829600044. [DOI] [PubMed] [Google Scholar]
- Weinschütz T, Niederberger U. The value of acupuncture in migraine therapy [Zum Stellenwert der Akupunktur in der Migränetherapie] Nervenheilkunde. 1995;14:295–301. [Google Scholar]
- Weinschütz T, Niederberger U, Johnsen S, Schreiber J, Kropp P. The neuroregulative effects of acupuncture in patients with headache [Zur neuroregulativen Wirkung der Akupunktur bei Kopfschmerzpatienten] Deutsche Zeitschrift für Akupunktur. 1994;37:106–117. [Google Scholar]
- Wylie KR, Jackson C, Crawford PM. Does psychological testing help to predict the response to acupuncture or massage/relaxation therapy in patients presenting to a general neurology clinic with headache? Journal of Traditional Chinese Medicine. 1997;17(2):130–139. [MEDLINE: 10437184] [PubMed] [Google Scholar]
References to studies excluded from this review
- Allais G, De Lorenzo C, Quirico PE, Lupi G, Airola G, Mana O, et al. Non-pharmacological approaches to chronic headaches: transcutaneous electrical nerve stimulation, laser therapy and acupuncture in transformed migraine treatment. Neurological Sciences. 2003;24 Suppl 2:S138–S142. doi: 10.1007/s100720300062. [DOI] [PubMed] [Google Scholar]
- Annal N, Soundappan SV, Subbu Palaniappan KMC, Chandrasekar S. Introduction of transcutaneous, low-voltage, non-pulsatile direct current (DC) therapy for migraine and chronic headaches. A comparison with transcutaneous electrical nerve stimulation (TENS) Headache Quarterly. 1992;3(4):434–437. [Google Scholar]
- Borglum-Jensen L, Melsen B, Borglum-Jensen S. Effect of acupuncture on headache measured by reduction in number of attacks and use of drugs. Scandinavian Journal of Dental Research. 1979;87(5):373–380. doi: 10.1111/j.1600-0722.1979.tb00696.x. [MEDLINE: 395626] [DOI] [PubMed] [Google Scholar]
- Bäcker M, Hammes M, Sander D, Funke D, Deppe M, Tölle TR, et al. Changes of cerebrovascular response to visual stimulation in migraineurs after repetitive sessions of somatosensory stimulation (acupuncture): a pilot study. Headache. 2004;44(1):95–101. doi: 10.1111/j.1526-4610.2004.04017.x. [MEDLINE: 14979891] [DOI] [PubMed] [Google Scholar]
- Coeytaux RR, Kaufman JS, Kaptchuk TJ, Chen W, Miller WC, Callahan LF, et al. A randomized controlled trial of acupuncture for chronic daily headache. Headache. 2005;45(9):1113–1123. doi: 10.1111/j.1526-4610.2005.00235.x. [MEDLINE: 16178942] [DOI] [PubMed] [Google Scholar]
- Domzal T, Kwasucki J, Zaleska B. Acupuncture in headache and radicular syndromes [Akupunktura w bolach glowy i zespolach korzeniowych] Neurologia i Neurochirurgia Polska. 1980;14(3):259–262. [MEDLINE: 7412983] [PubMed] [Google Scholar]
- Dong Z. Treating vascular migraine with deep puncture at Fengchi: a report of 240 cases. International Journal of Clinical Acupuncture. 1994;5:455–458. [Google Scholar]
- Gao S, Zhao D, Xie Y. A comparative study on the treatment of migraine headache with combined distant and local acupuncture points versus conventional drug therapy. American Journal of Acupuncture. 1999;27(1–2):27–30. [MEDLINE: 10513096] [PubMed] [Google Scholar]
- Gottschling S, Meyer S, Gribova I, Distler L, Berrang J, Gortner L, et al. Laser acupuncture in children with headache: a double-blind, randomized, bicenter, placebo-controlled trial. Pain. 2008;137(2):405–412. doi: 10.1016/j.pain.2007.10.004. [DOI] [PubMed] [Google Scholar]
- Hansen PE, Hansen JH. Acupuncture treatment of chronic facial pain - a controlled cross-over trial. Headache. 1983;23(2):66–69. doi: 10.1111/j.1526-4610.1983.hed2302066.x. [MEDLINE: 6853155] [DOI] [PubMed] [Google Scholar]
- Heydenreich A. Transcutaneous electrical nerve stimulation at acupuncture points (PuTENS) compared to placebo in migraine [Punktförmige transkutane elektrische Nervenstimulation (PuTENS) im einfachen Placebovergleich bei der Migräne] Zeitschrift für ärztliche Fortbildung und Qualitätssicherung. 1989;83(17):881–883. [PubMed] [Google Scholar]
- Heydenreich A, Thiessen M. Comparison of the effectiveness of drug treatment, invasive and non-invasive acupuncture in migraine [Effektivitätsvergleich zwischen medikamentöser Therapie, invasiver und nichtinvasiver Akupunktur bei der Migräne] Zeitschrift für ärztliche Fortbildung und Qualitätssicherung. 1989;83(17):877–879. [PubMed] [Google Scholar]
- Ho H, Kropp P, Wallasch T, Niederberger U, Weinschütz T. Laser-acupuncture in migraine therapy - methodological considerations and results of a randomized, controlled clinical and electrophysical study [Zur Intervalltherapie der Migräne mit Laserakupunktur – klinische und elektrophysiologische Parameter] Akupunktur und Traditionelle Chinesische Medizin. 1999;27:159–170. [Google Scholar]
- Schütz H, Bruhn HD, Kropp P, Niederberger U, Weinschütz T. Laser acupuncture in migraine therapy and its effects on humoral parameters [Modulation humoraler Parameter durch Laserakupunktur – das Beispiel Migräne] Akupunktur und Traditionelle Chinesische Medizin. 2000;28:32–43. [Google Scholar]
- Johansson A, Wenneberg B, Wagersten C, Haraldson T. Acupuncture in treatment of facial muscular pain. Acta Odontologica Scandinavica. 1991;49(3):153–158. doi: 10.3109/00016359109005900. [MEDLINE: 1882649] [DOI] [PubMed] [Google Scholar]
- Junnilla S. Acupuncture treatment for chronic pain. Acupuncture in Medicine. 1983;1:6–8. [Google Scholar]
- Kubiena G, Nissel H, Porenta G, Veitl M, Wessely P. Acupuncture in migraine. Follow-up study [Akupunktur bei Migräne. Follow-up Studie] Deutsche Zeitschrift für Akupunktur. 1992;35:140–148. [Google Scholar]
- Lavies NG. Laser acupuncture for migraine and muscle tension headache: a double-blind controlled trial. Acupuncture in Medicine. 1998;16:73–76. [Google Scholar]
- Lehmann V, Banzhaf E, Kunze E, Stube G, Theil G, Schilling C, et al. Randomized clinically controlled study of the efficacy of acupuncture in comparison with electroacupuncture as well as drug therapy with propanolol in patients with recurrent migraine [Randomisierte klinisch kontrollierte Studie der Effizienz der Akupunktur im Vergleich zur Elektroakupunktur sowie zur Pharmakotherapie mit Propanolol bei Patienten mit häufiger Migräne] Deutsche Zeitschrift für Akupunktur. 1991;34:27–30. [Google Scholar]
- Lenhard L, Waite PM. Acupuncture in the prophylactic treatment of migraine headaches: pilot study. New Zealand Medical Journal. 1983;96(738):663–666. [MEDLINE: 6576263] [PubMed] [Google Scholar]
- Liguori A, Petti F, Bangrazi A, Camaioni D, Guccione G, Pitari GM, et al. Comparison of pharmacological treatment versus acupuncture treatment for migraine without aura - analysis of socio-medical parameters. Journal of Traditional Chinese Medicine. 2000;20(3):231–240. [MEDLINE: 11038990] [PubMed] [Google Scholar]
- Loh L, Nathan PW, Schott GD, Zilkha KJ. Acupuncture versus medical treatment for migraine and muscle tension headaches. Journal of Neurology, Neurosurgery and Psychiatry. 1984;47(4):333–337. doi: 10.1136/jnnp.47.4.333. [MEDLINE: 6726258] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundeberg T, Hurtig T, Lundeberg S, Thomas M. Long-term results of acupuncture in chronic head and neck pain. Pain Clinic. 1988;2:15–31. [Google Scholar]
- Melchart D, Thormaehlen J, Hager S, Liao J, Linde K, Weidenhammer W. Acupuncture versus placebo versus sumatriptan for early treatment of migraine attacks: a randomized controlled trial. Journal of Internal Medicine. 2003;253(2):181–188. doi: 10.1046/j.1365-2796.2003.01081.x. [MEDLINE: 12542558] [DOI] [PubMed] [Google Scholar]
- Melchart D, Hager S, Hager U, Liao J, Weidenhammer W, Linde K. Treatment of patients with chronic headaches in a hospital for traditional Chinese medicine on Germany. A randomised, waiting list controlled trial. Complementary Therapies in Medicine. 2004;12(2–3):71–78. doi: 10.1016/j.ctim.2004.05.001. [MEDLINE: 15561516] [DOI] [PubMed] [Google Scholar]
- Okazaki K, Sadove MS, Kim SI, Lee MH, Cheng D. Ryodoraku therapy for migraine headache. American Journal of Chinese Medicine. 1975;3(1):61–70. doi: 10.1142/s0192415x75000074. [MEDLINE: 1119438] [DOI] [PubMed] [Google Scholar]
- Pikoff H. The effects of acupressure on headache pain: a placebo-controlled group outcome study [dissertation] Buffalo, NY: State University of New York at Buffalo; 1989. [Google Scholar]
- Pintov S, Lahat E, Alstein M, Vogel Z, Barg J. Acupuncture and the opioid system: implications in management of migraine. Pediatric Neurology. 1997;17(2):129–133. doi: 10.1016/s0887-8994(97)00086-6. [MEDLINE: 9367292] [DOI] [PubMed] [Google Scholar]
- Shi J, Flemming M, Stehr-Zirngibl S, Taeger K. Treating chronic headache by means of acupuncture. A clinical trial [Schmerztherapie mit Akupunktur bei chronischen Kopfschmerzen. Eine klinische Studie] Chinesische Medizin. 2000;15:14–25. [Google Scholar]
- Sold-Darseff J, Leydhecker W. Acupuncture as a treatment for pain in the cranial region and for blepharospasm without organic cause [Akupunktur bei Schmerzen im Kopfbereich sowie bei Blepharospasmus ohne organische Ursache] Klinische Monatsblätter für Augenheilkunde. 1986;189:167–169. doi: 10.1055/s-2008-1050778. [DOI] [PubMed] [Google Scholar]
- Sun ZR, Wu YJ, Li XJ. Study on the clinical effect of acupuncture and its biochemical mechanism. Zhongguo Linchuang Kangfu. 2004;8:1994–1995. [Google Scholar]
- Tekeoglu I. Introduction of a new therapy method: music sound electroacupuncture stimulation. Acupunture in Medicine. 1995;13:71–73. [Google Scholar]
- Turk Z, Moser I. Curing chronic headache with acupuncture [Heilung des chronischen Kopfschmerzes durch Akupunktur] Erfahrungsheilkunde. 1990;11:724–726. [Google Scholar]
References to ongoing studies
- Liang F. Randomized controlled trial of treating migraine with acupuncture. ClinicalTrials.gov.
- Vas J. ISRCTN register; Study protocol for a pragmatic randomised controlled trial in general practice investigating thre effectiveness of acupuncture against migraine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L. ISRCTN Register; Efficacy and safety of acupuncture for migraine prophylaxis - a multicenter, randomized controlled trial. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Z, Xue C. Australian New Zealand Clinical Trials Registry; Effectiveness and safety of acupuncture for migraine: a randomised, single blind and sham controlled trials. [Google Scholar]
Additional references
- Andlin-Sobocki P, Jonsson B, Wittchen HU, Olesen J. Cost of disorders of the brain in Europe. European Journal of Neurology. 2005;12 Suppl 1:1–27. doi: 10.1111/j.1468-1331.2005.01202.x. [MEDLINE: 15877774] [DOI] [PubMed] [Google Scholar]
- Benedetti F. Mechanism of placebo and placebo-related effects across diseases and treatments. Annual Review of Pharmacology and Toxicology. 2008;48:33–60. doi: 10.1146/annurev.pharmtox.48.113006.094711. [MEDLINE: 17666008] [DOI] [PubMed] [Google Scholar]
- Bodeker G, Ong CK, Grundy C, Burford G, Shein K. Kobe, Japan: WHO Center for Health Development; 2005. WHO global atlas of traditional, complementary and alternative medicine. [Google Scholar]
- Burke A, Upchurch DM, Dye C, Chyu L. Acupuncture use in the United States: findings from the National Health Interview Study. Journal of Alternative and Complementary Medicine. 2006;12(7):639–648. doi: 10.1089/acm.2006.12.639. [MEDLINE: 16970534] [DOI] [PubMed] [Google Scholar]
- Bäcker M, Gareus IK, Knoblauch NTM, Michalsen A, Dobos G. Acupuncture in the treatment of pain - hypothesis to adaptive effects [Akupunktur in der Schmerztherapie – Hypothese zu adaptiven Prozessen] Forschende Komplementärmedizin und Klassische Naturheilkunde. 2004;11(6):335–345. doi: 10.1159/000082815. [MEDLINE: 15604624] [DOI] [PubMed] [Google Scholar]
- Carlsson C. Acupuncture mechanisms for clinically relevant long-term effects - reconsideration and a hypothesis. Acupuncture in Medicine. 2002;20(2–3):82–99. doi: 10.1136/aim.20.2-3.82. [MEDLINE: 12216606] [DOI] [PubMed] [Google Scholar]
- Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H. The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review. Health Technology Assessment. 1999;3(3):1–96. [MEDLINE: 10448203] [PubMed] [Google Scholar]
- Dale J. Acupuncture practice in the UK. Part I: report of a survey. Complementary Therapies in Medicine. 1997;5:215–220. [Google Scholar]
- Dodick DW, Silberstein SD. Migraine prevention. Practical Neurology. 2007;7(6):383–393. doi: 10.1136/jnnp.2007.134023. [MEDLINE: 18024778] [DOI] [PubMed] [Google Scholar]
- Endres HG, Diener HC, Molsberger A. Role of acupuncture in the treatment of migraine. Expert Review of Neurotherapeutics. 2007;7(9):1121–1134. doi: 10.1586/14737175.7.9.1121. [MEDLINE: 17868011] [DOI] [PubMed] [Google Scholar]
- Ernst E, White A. Acupuncture for back pain. A meta-analysis of randomized controlled trials. Archives of Internal Medicine. 1998;158(20):2235–2241. doi: 10.1001/archinte.158.20.2235. [MEDLINE: 9818803] [DOI] [PubMed] [Google Scholar]
- Griggs C, Jensen J. Effectiveness of acupuncture for migraine: critical literature review. Journal of Advanced Nursing. 2006;54(4):491–501. doi: 10.1111/j.1365-2648.2006.03837.x. [MEDLINE: 16671978] [DOI] [PubMed] [Google Scholar]
- Han JS. Physiology of acupuncture: review of thirty years of research. Journal of Alternative and Complementary Medicine. 1997;3 Suppl 1:S101–S108. [Google Scholar]
- Higgins JPT, Altman DG. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0. The Cochrane Collaboration; 2008. [updated February 2008]. Available from www.cochrane-handbook.org. [Google Scholar]
- Holroyd KA, Penzien DB. Pharmacological versus non-pharmacological prophylaxis of recurrent migraine headache: a meta-analytic review of clinical trials. Pain. 1990;42(1):1–13. doi: 10.1016/0304-3959(90)91085-W. [MEDLINE: 2146583] [DOI] [PubMed] [Google Scholar]
- Hróbjartsson A, Gøtzsche PC. Placebo interventions for all clinical conditions. Cochrane Database of Systematic Reviews. 2004;(Issue 2) doi: 10.1002/14651858.CD003974.pub2. [DOI] [PubMed] [Google Scholar]
- Härtel U, Volger E. Use and acceptance of classical and alternative medicine in Germany - findings of a representative population-based survey [Inanspruchnahme und Akzeptanz klassischer Naturheilverfahren und alternativer Heilmethoden in Deutschland – Ergebnisse einer repräsentativen Bevölkerungsstudie] Forschende Komplementärmedizin und Klassische Naturheilkunde. 2004;11(6):327–334. doi: 10.1159/000082814. [MEDLINE: 15604623] [DOI] [PubMed] [Google Scholar]
- International Headache Society Clinical Trials Subcommittee. Guidelines for controlled trials of drugs in migraine: second edition. Cephalalgia. 2000;20(9):765–786. doi: 10.1046/j.1468-2982.2000.00117.x. [MEDLINE: 11167908] [DOI] [PubMed] [Google Scholar]
- Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24 Suppl 1:1–160. doi: 10.1111/j.1468-2982.2003.00824.x. [MEDLINE: 14979299] [DOI] [PubMed] [Google Scholar]
- Kaptchuk TJ, Goldman P, Stone DA, Stason WB. Do medical devices have enhanced placebo effects? Journal of Clinical Epidemiology. 2000;53(8):786–792. doi: 10.1016/s0895-4356(00)00206-7. [MEDLINE: 10942860] [DOI] [PubMed] [Google Scholar]
- Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Annals of Internal Medicine. 2002;136(5):374–383. doi: 10.7326/0003-4819-136-5-200203050-00010. [MEDLINE: 11874310] [DOI] [PubMed] [Google Scholar]
- Kaptchuk TJ, Stason WB, Davis RB, Legezda ATR, Schnyer RN, Kerr CE, et al. Sham device v inert pill: randomised controlled trial of two placebo treatments. BMJ. 2006;332(7538):391–397. doi: 10.1136/bmj.38726.603310.55. [MEDLINE: 16452103] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaptchuk TJ, Kelley JM, Conboy LA, Davis RB, Kerr CE, Jacobson EE, et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ. 2008;336(7651):999–1003. doi: 10.1136/bmj.39524.439618.25. [MEDLINE: 18390493] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linde K, Scholz M, Melchart D, Willich SN. Should systematic reviews include non-randomized and uncontrolled studies? The case of acupuncture for chronic headache. Journal of Clinical Epidemiology. 2002;55(1):77–85. doi: 10.1016/s0895-4356(01)00422-x. [MEDLINE: 11781125] [DOI] [PubMed] [Google Scholar]
- Linde K, Streng A, Hoppe A, Weidenhammer W, Wagenpfeil S, Melchart D. Randomized trial vs. observational study of acupuncture for migraine found that patient characteristics differed but outcomes were similar. Journal of Clinical Epidemiology. 2007;60(3):280–287. doi: 10.1016/j.jclinepi.2006.06.014. [MEDLINE: 17292022] [DOI] [PubMed] [Google Scholar]
- Linde K, Witt CM, Streng A, Weidenhammer W, Wagenpfeil S, Brinkhaus B, et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture with chronic pain. Pain. 2007;128(3):264–271. doi: 10.1016/j.pain.2006.12.006. [MEDLINE: 17257756] [DOI] [PubMed] [Google Scholar]
- Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White A. Acupuncture for tension-type headache. Cochrane Database of Systematic Reviews. 2009;(Issue 1) doi: 10.1002/14651858.CD007587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupuncture in Medicine. 2006;24(1):13–15. doi: 10.1136/aim.24.1.13. [MEDLINE: 16618044] [DOI] [PubMed] [Google Scholar]
- Lundeberg T, Lund I, Naslund J. Acupuncture - self-appraisal and the reward system. Acupuncture in Medicine. 2007;25(3):87–99. doi: 10.1136/aim.25.3.87. [MEDLINE: 17906602] [DOI] [PubMed] [Google Scholar]
- MacPherson H, Thomas K, Walters S, Fitter M. A prospective survey of adverse events and treatment reactions following 34,000 consultations with professional acupuncturists. Acupuncture in Medicine. 2001;19(2):93–102. doi: 10.1136/aim.19.2.93. [MEDLINE: 11829165] [DOI] [PubMed] [Google Scholar]
- Melchart D, Weidenhammer W, Streng A, Hoppe A, Pfaffenrath V, Linde K. Acupuncture for chronic headaches - an epidemiological study. Headache. 2006;46(4):632–641. doi: 10.1111/j.1526-4610.2006.00365.x. [MEDLINE: 16643558] [DOI] [PubMed] [Google Scholar]
- Nestoriuc Y, Martin A. Efficacy of biofeedback for migraine: a meta-analysis. Pain. 2007;128(1–2):111–127. doi: 10.1016/j.pain.2006.09.007. [MEDLINE: 17084028] [DOI] [PubMed] [Google Scholar]
- Olesen J, Lekander I, Andlin-Sobocki P, Jönsson B. Funding of headache research in Europe. Cephalalgia. 2007;27(9):995–999. doi: 10.1111/j.1468-2982.2007.01397.x. [MEDLINE: 17727472] [DOI] [PubMed] [Google Scholar]
- Schürks M, Diener HC, Goadsby P. Update on the prophylaxis of migraine. Current Treatment Options in Neurology. 2008;10(1):20–29. doi: 10.1007/s11940-008-0003-3. [DOI] [PubMed] [Google Scholar]
- Scott SW, Deare JC. Acupuncture for migraine: a systematic review. Australian Journal of Acupuncture and Chinese Medicine. 2006;1:3–14. [Google Scholar]
- Thomas M, Lundeberg T. Does acupuncture work? Pain Clinical Update. 1996;4:1–4. [Google Scholar]
- Van der Kuy PH, Lohmann JJ. A quantification of the placebo response in migraine prophylaxis. Cephalalgia. 2002;22(4):265–270. doi: 10.1046/j.1468-2982.2002.00363.x. [MEDLINE: 12100088] [DOI] [PubMed] [Google Scholar]
- Vickers A, Goyal N, Harland R, Rees R. Do certain countries produce only positive results? A systematic review of controlled trials. Controlled Clinical Trials. 1998;19(2):159–166. doi: 10.1016/s0197-2456(97)00150-5. [MEDLINE: 9551280] [DOI] [PubMed] [Google Scholar]
- Wang G, Mao B, Xiong ZY, Fan T, Chen XD, Wang L, et al. CONSORT Group for Traditional Chinese Medicine. The quality of reporting of randomized controlled trials of traditional Chinese medicine: a survey of 13 randomly selected journals from mainland China. Clinical Therapeutics. 2007;29(7):1456–1467. doi: 10.1016/j.clinthera.2007.07.023. [MEDLINE: 17825697] [DOI] [PubMed] [Google Scholar]
- Weidenhammer W, Menz G, Streng A, Linde K, Melchart D. Acupuncture for chronic pain patients. Treatment outcomes - the role of the acupuncturist [Akupunktur bei chronischen Schmerzpatienten. Behandlungsergebnisse – Rolle des Akupunkteurs] Schmerz. 2006;20(5):418–431. doi: 10.1007/s00482-006-0471-x. [DOI] [PubMed] [Google Scholar]
- Weidenhammer W, Streng A, Linde K, Hoppe A, Melchart D. Acupuncture for chronic pain within the research program of 10 German Health Insurance Funds - basic results from an observational study. Complementary Therapies in Medicine. 2007;15(4):238–246. doi: 10.1016/j.ctim.2006.09.005. [MEDLINE: 18054725] [DOI] [PubMed] [Google Scholar]
- White A, Hayhoe S, Hart A, Ernst E. Adverse events following acupuncture: prospective survey of 32 000 consultations with doctors and physiotherapists. BMJ. 2001;323(7311):485–486. doi: 10.1136/bmj.323.7311.485. [MEDLINE: 11532840] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witt CM, Brinkhaus B, Reinhold T, Willich SN. Efficacy, effectiveness, safety and costs of acupuncture for chronic pain - results of a large research initiative. Acupuncture in Medicine. 2006;24 Suppl:S33–S39. [Google Scholar]
- Witt CM, Reinhold T, Jena S, Brinkhaus B, Willich SN. Cost-effectiveness of acupuncture treatment in patients with headache. Cephalalgia. 2008;28(4):334–345. doi: 10.1111/j.1468-2982.2007.01504.x. [MEDLINE: 18315686] [DOI] [PubMed] [Google Scholar]
- Wonderling D, Vickers AJ, Grieve R, McCarney R. Cost effectiveness analysis of a randomised trial of acupuncture for chronic headache in primary care. BMJ. 2004;328(7442):744–749. doi: 10.1136/bmj.38033.896505.EB. [MEDLINE: 15023830] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
- Melchart D, Linde K, Fischer P, White A, Allais G, Vickers A, et al. Acupuncture for recurrent headaches: a systematic review of randomized controlled trials. Cephalalgia. 1999;19(9):779–786. doi: 10.1046/j.1468-2982.1999.1909779.x. [erratum appears in Cephalalgia 2000 Oct;20(8):762-3] [MEDLINE: 10595286] [DOI] [PubMed] [Google Scholar]
- Melchart D, Linde K, Berman B, White A, Vickers A, Allais G, et al. Acupuncture for idiopathic headache. Cochrane Database of Systematic Reviews. 2001;(Issue Issue 1) doi: 10.1002/14651858.CD001218. [Art. No.: CD001218. DOI: 10.1002/14651858.CD001218] * Indicates the major publication for the study
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.