Histoplasmosis is often disseminated in patients with cell-mediated immunity defects.1 Primary intestinal involvement is rare, predominantly involves the ileocecal region, and is mainly reported in patients with AIDS.2,3 We report the case of a renal transplant recipient who presented with chronic diarrhea and was diagnosed with colonic histoplasmosis. This is the first reported case of colonic histoplasmosis in a renal transplant recipient from a nonendemic region.
Case Report
A 42-year-old woman presented with 4 weeks of watery diarrhea, intermittent fevers, and weight loss. She had undergone renal transplantation 3 years prior and was on immunosuppressants (tacrolimus and mycophenolate). The patient denied having respiratory symptoms or traveling recently. On examination, she was febrile and had mild diffuse abdominal tenderness. Blood tests revealed a normal white blood cell count and a hemoglobin of 10 g/dL. Stool studies for ova and parasites, Giardia lamblia, and Clostridium difficile were negative. Abdominal computed tomography scan showed cecal and sigmoid wall thickening.
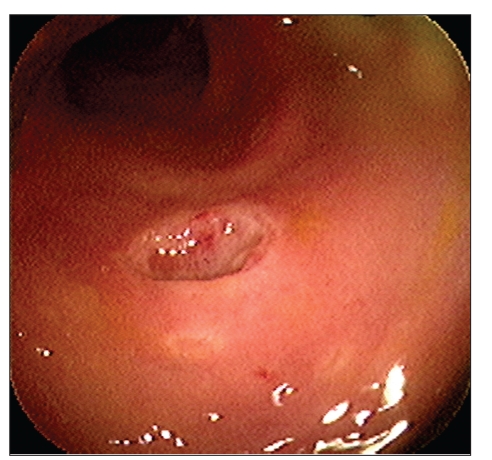
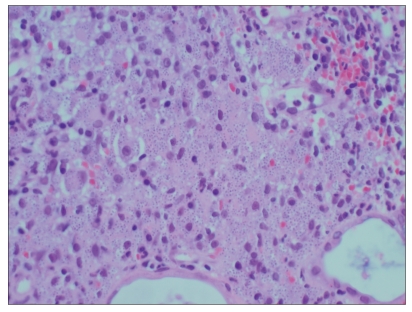
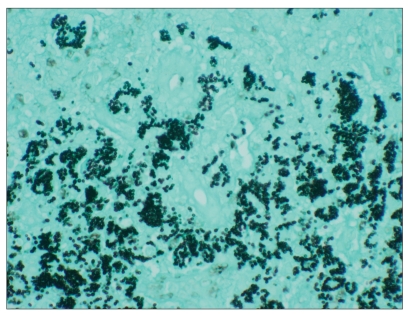
Colonoscopy revealed multiple scattered ulcers (1–3 cm in diameter) throughout the colon (Figure 1). Biopsies from the margins of an ulcer demonstrated diffuse collections of histiocytes with rounded intracytoplasmic structures (1–4 pm in diameter), consistent with Histoplasma capsulatum (Figure 2). Histochemical staining with Gomori methenamine silver highlighted numerous small budding yeasts (Figure 3). Subsequently, intravenous amphotericin B was initiated, and the symptoms resolved within 1 week. Her medication was then switched to oral itraconazole.
Figure 1.
Colonoscopic view of an ulcer in the sigmoid colon.
Figure 2.
Photomicrograph revealed histiocytes with small rounded intracytoplasmic organisms (hematoxylin and eosin stain, 1000x).
Figure 3.
Photomicrograph demonstrated numerous yeast forms (Gomori silver stain, 1000x).
Discussion
Histoplasmosis is mainly encountered in endemic areas (eg, the Ohio and Mississippi River valleys), and is generally either asymptomatic or causes a self-limited respiratory illness in immunocompetent patients.4 In contrast, in up to 80% of immunocompromised patients, histoplasmosis manifests as disseminated disease with multiorgan involvement, including the gastrointestinal system.5 The incidence of infection is reported to be as high as 2–5% in AIDS patients.2
Symptoms of gastrointestinal histoplasmosis may include anorexia, fever, abdominal pain, diarrhea, melena, constipation, and weight loss.6 Gastrointestinal involvement predominantly affects extraluminal organs, such as the liver, spleen, and mesenteric lymph nodes, and is seen in up to 20%, with disseminated disease in autopsy series.3
Primary, symptomatic luminal histoplasmosis in immunocompromised patients is thought to be rare and usually involves the ileocecal region.3 Reports of gastrointestinal histoplasmosis in renal allograft recipients in the United States have come uniformly from centers located in endemic regions.1,3,5,7–9 However, none of these reports has described chronic diarrhea as a presenting symptom, and the diagnoses were established through nonendoscopic means (eg, bone marrow, liver, and lymph node biopsies).
Histologic and fungal cultures of involved tissue are a sensitive means of diagnosis.10 Submucosal and mucosal macrophages with intracytoplasmic round eosinophilic organisms (1–4 pm) with clear halos can be seen. Gomori methenamine silver nitrate staining may aid in the diagnosis. Fungal cultures require 4–6 weeks for definitive identification and thus are rarely helpful in the initial diagnosis. Colonization with histoplasmosis does not occur; therefore, the visualization of organisms in tissue ensures the correct diagnosis of active infection.11
The initial treatment of severely ill patients usually involves intravenous antifungal therapy with amphotericin B.12 Patients usually respond rapidly and can subsequently be switched to oral itraconazole for 6–18 months.12 Prompt diagnosis and initiation of antifungal treatment is of utmost importance, as several case series report a 100% mortality rate in patients who did not receive antifungal agents.1
We report the first case of colonic histoplasmosis in a renal allograft recipient living in a nonendemic area. Although extraluminal involvement is more common, this patient had predominantly luminal disease and presented with chronic diarrhea. Endoscopy with biopsy was instrumental in establishing the diagnosis. Gastroenterologists caring for transplant recipients should be aware of the varied presentations of infectious diseases in immunosuppressed individuals and should consider uncommon etiologies in this population, even from nonendemic geographic regions.
References
- 1.Kauffman CA, Israel KS, Smith JW, et al. Histoplasmosis in immunosuppressed patients. Am J Med. 1978;64:923–932. doi: 10.1016/0002-9343(78)90445-x. [DOI] [PubMed] [Google Scholar]
- 2.Anand A. Diagnosis of systemic histoplasmosis in AIDS patients. South Med J. 1993;86:844–845. doi: 10.1097/00007611-199307000-00030. [DOI] [PubMed] [Google Scholar]
- 3.Cappell MS, Mandell W, Grimes MM, Neu HC. Gastrointestinal histoplasmosis. Dig Dis Sci. 1988;33:353–360. doi: 10.1007/BF01535762. [DOI] [PubMed] [Google Scholar]
- 4.Medoff G, Kobayashi GS. Systemic fungal infections: an overview. Hosp Pract. 1991;26:41–52. doi: 10.1080/21548331.1991.11704143. [DOI] [PubMed] [Google Scholar]
- 5.Wheat LJ, Smith EJ, Sathapatayavongs B, et al. Histoplasmosis in renal allograft recipients. Arch Intern Med. 1983;143:703–707. [PubMed] [Google Scholar]
- 6.Miller DP, Everett ED. Gastrointestinal histoplasmosis. J Clin Gatroenterol. 1979;1:233–236. doi: 10.1097/00004836-197909000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Peddi VR, Hariharan S, First MR. Disseminated histoplasmosis in renal allograft recipients. Clin Transplant. 1996;10:160–165. [PubMed] [Google Scholar]
- 8.Superdock KR, Dummer JS, Koch MO, et al. Disseminated histoplasmosis presenting as urinary tract obstruction in a renal transplant recipient. Am J Kidney Dis. 1994;23:600–604. doi: 10.1016/s0272-6386(12)80386-6. [DOI] [PubMed] [Google Scholar]
- 9.Davies SF, Sarosi GA, Peterson PK, et al. Disseminated histoplasmosis in renal transplant recipients. Am J Surg. 1979;137:686–691. doi: 10.1016/0002-9610(79)90050-3. [DOI] [PubMed] [Google Scholar]
- 10.Temesgeni Z. Histoplasma capsulatum. In: Wilson RW, Sande MA, editors. Current Diagnosis and Treatment in Infectious Diseases. New York: McGraw-Hill; 2001. pp. 721–725. [Google Scholar]
- 11.Bradsher RW. Histoplasmosis and blastomycosis. Clin Infect Dis. 1996;22(suppl 2):S102–S111. doi: 10.1093/clinids/22.supplement_2.s102. [DOI] [PubMed] [Google Scholar]
- 12.Wheat J, Sarosi G, McKinsey D, et al. Practice guidelines for the management of patients with histoplasmosis. Infectious Diseases Society of America. Clin Infect Dis. 2000;30:688–695. doi: 10.1086/313752. [DOI] [PubMed] [Google Scholar]