Abstract
Objective
To assess trends in hospital births in China during 1988–2008 in an effort to determine if efforts to overcome financial barriers to giving birth in hospital have reduced the access gap between the rich and the poor.
Methods
Cross-sectional data obtained from four National Health Service Surveys were used to determine trends in hospital births during 1988–2008. Crude and adjusted annual rates were calculated by means of Poisson regression and were used to define trends across socioeconomic regions and households in different income quintiles.
Findings
In 2008 women throughout China were giving birth in hospital almost universally except in region IV, the most remote rural region, where the percentage of hospital births was only 60.8. Hospital births in this region had increased steadily before 2002, but after that year the upward trend slowed down. During 1988–2001 the average yearly increase had been 21%, but in 2002–2008 it dropped to 10% (P = 0.0031). Inequalities between socioeconomic regions were greater than among individual households belonging to different income strata. By 2008 the difference between low- and high-income households in the proportion of hospital births had become very small (96.1% and 87.7% of high- and low-income households, respectively, gave birth in hospital that year).
Conclusion
Most Chinese women now give birth in hospital, but the poorest rural region is still lagging behind. A more active and comprehensive approach will be needed to increase hospital births in these remote, hard-to-reach populations.
ملخص
الغرض
تقييم اتجاهات الولادة في المستشفيات في الصين أثناء الأعوام 1988-2008 سعياً لتحديد جدوى الجهود المبذولة للتغلب على العوائق المالية أمام الولادة في المستشفى وهل نجحت في سد الفجوة بين الأغنياء والفقراء.
الطريقة
جُمِعَت معطيات مقطعية من أربعة مسوحات وطنية عن الخدمات الصحية لتحديد اتجاهات الولادات في المستشفيات خلال الأعوام 1988-2008. وجرى حساب المعدلات السنوية الخام والمُصحَحَة عن طريق تحوّف بواسون Poisson، ثم استُخْدِمت في تحديد الاتجاهات عبر المناطق الاجتماعية والاقتصادية، وعبر الأسر في مختلف الشرائح المئوية للدخل.
النتائج
كانت النساء في عام 2008 يلدن في المستشفيات على نطاق واسع ما عدا في المنطقة الرابعة، وهي منطقة ريفية نائية، حيث كانت نسبة الولادة في المستشفيات 60.8 فقط. وقد ازدادت الولادات في المستشفيات على نحو ثابت في هذه المنطقة من قبل عام 2002، ولكن بعد هذا العام تباطأ هذا الاتجاه الصاعد. وخلال الأعوام 1988-2001 بلغ متوسط الزيادة السنوية 21%، لكن في الأعوام 2002-2008 انخفض إلى 10% (قوة الاحتمالP= 0.0031)) وكان التباين بين المناطق الاجتماعية والاقتصادية أكبر من التباين بين الأسر التي تنتمي إلى طبقات دخل مختلفة. وبحلول عام 2008 كان الفرق بين الأسر المنخفضة الدخل والأسر المرتفعة الدخل في نسبة الولادة في المستشفيات قد أصبح ضئيلاً للغاية (حيث كانت نسبة الولادة في المستشفيات في هذا العام هي96.1% للأسر ذات الدخل المرتفع، و 87.7% للأسر ذات الدخل المنخفض).
الاستنتاج
غالبية الصينيات يدلن الآن في المستشفيات، إلا أن المناطق الريفية الفقيرة مازالت متأخرة في هذا الصدد. وهناك حاجة إلى أسلوب فعّال وشامل لزيادة الولادات في المستشفيات بين السكان في المناطق النائية التي يصعب الوصول إليها.
摘要
Abstract
目的
旨在评价1988至2008年间中国住院分娩的趋势以分析消除住院分娩经济障碍的努力是否起到了降低住院分娩利用贫富差距的作用。
方法
利用四次国家卫生服务调查的横断面数据来分析1988至2008年间住院分娩的趋势。计算年住院分娩率,通过泊松回归调整其他因素和分析不同社会经济地区和不同收入家庭的趋势。
结果
2008年,除最偏远的农村四类地区住院分娩率仅为60.8%外,中国的产妇都普遍接受了住院分娩服务。2002年之前四类农村地区的住院分娩率一直稳步增加,而2002年后增长趋势减缓。1988至2001年间,平均年增涨为21%,而2002至2008年间仅为10%(P = 0.0031)。社会经济地区之间的不平等比不同收入分组的个体家庭之间的不平等更大。截至2008年,高收入和低收入家庭在住院分娩比例方面的差别已经变得很小(高收入和低收入家庭2008年住院分娩比例分别为96.1%和87.7%)。
结论
大多数中国产妇都能接受到住院分娩服务,然而最贫困的农村地区仍然滞后。因而需要更积极、更全面的方法来提高这些偏远、交通不方便地区人群的住院分娩率。
Résumé
Objectif
Évaluer les tendances des accouchements à l'hôpital en Chine sur la période 1988-2008, afin de déterminer si les efforts pour surmonter les obstacles financiers à l'accouchement à l'hôpital ont réduit la différence d'accès entre riches et pauvres.
Méthodes
Les données transversales obtenues de quatre études nationales des services de santé ont été utilisées pour déterminer les tendances des accouchements à l'hôpital de 1988 à 2008. Les taux annuels bruts et ajustés ont été calculés par régression de Poisson et ont été utilisés pour définir les tendances sur les régions socioéconomiques et les ménages dans différents quintiles de revenu.
Résultats
En 2008, les femmes ont accouché à l'hôpital presque partout en Chine, sauf dans la région IV, la région la plus rurale et éloignée, où le pourcentage d’accouchements à l'hôpital a atteint seulement 60,8. Les accouchements à l'hôpital dans cette région ont augmenté régulièrement avant 2002, mais après cette année, la tendance a ralenti. Sur la période 1988-2001, l’augmentation baisse moyenne annuelle était de 21%, mais entre 2002 et 2008, elle a atteint 10% (P = 0,0031). Les inégalités entre les régions socioéconomiques étaient plus importantes qu'entre les ménages individuels appartenant à des strates de revenu différents. En 2008, la différence entre les ménages à faible et haut revenus en termes de proportion d’accouchements à l'hôpital était devenue très faible (96,1% et 87,7%, respectivement, des ménages à haut et bas revenus ont accouché à l'hôpital cette année-là).
Conclusion
La plupart des femmes chinoises accouchent maintenant à l'hôpital, mais la région rurale la plus pauvre est toujours à la traîne. Une approche plus active et globale sera nécessaire pour augmenter le nombre d’accouchements à l'hôpital de ces populations éloignées et difficiles d'accès.
Резюме
Цель
Оценить тенденции показателя родов, принятых в больнице, в Китае за период 1988–2008 годов с тем, чтобы определить, способствовали ли меры по преодолению финансовых барьеров, препятствующих проведению родов в медицинском учреждении, сокращению разрыва в доступе к медицинской помощи между богатыми и бедными.
Методы
Для определения тенденций показателя родов, принятых в больнице, за период 1988–2008 годов использовались кросс-секционные данные Национальных обследований в области здравоохранения. С помощью регрессии Пуассона производился расчет грубых и уточненных годовых показателей, которые были использованы для определения тенденций по социально-экономическим регионам и домохозяйствам, относящимся к разным квинтилям распределения доходов.
Результаты
В 2008 году китаянки рожали почти исключительно в больницах, за исключением региона IV – наиболее отдаленного сельского региона, где процент родов, принятых в больнице, составлял лишь 60,8. В этом регионе процентная доля родов, принятых в больнице, неуклонно повышалась вплоть до 2002 года, после чего повышательная тенденция замедлилась. В период с 1988 по 2001 год среднегодовой прирост составлял 21%, но в 2002–2008 годах он сократился до 10% (P = 0,0031). Неравенство сильнее проявлялось между социально-экономическими регионами, чем между домохозяйствами, принадлежащими к стратам с различными уровнями дохода. К 2008 году разница в процентной доле родов, принятых в больнице, между домохозяйствами с низким и высоким доходом стала весьма незначительной (в тот год роды в больнице были приняты у 96,1 и 87,7% домохозяйств с высоким и низким доходом, соответственно).
Вывод
В настоящее время большинство китаянок рожают в больнице, однако беднейший сельский регион по-прежнему отстает в этом отношении. Для увеличения доли родов, принятых в больнице, среди этих отдаленных и труднодоступных групп населения потребуется применить более активный и всеобъемлющий подход.
Resumen
Objetivo
Evaluar las tendencias de los nacimientos en los hospitales de China entre 1998 y 2008, con el fin de determinar si los esfuerzos realizados para superar las barreras económicas del alumbramiento en un hospital habían conseguido reducir las diferencias en el acceso entre ricos y pobres.
Métodos
Se emplearon datos aleatorios y representativos procedentes de cuatro Encuestas del Servicio Nacional de Salud para determinar las tendencias de los nacimientos en hospitales entre 1988 y 2008. Se calcularon las tasas anuales brutas y ajustadas con una regresión de Poisson y éstas se utilizaron para definir las tendencias en las diversas regiones socioeconómicas y unidades domésticas dentro de los diferentes quintiles de ingresos.
Resultados
En 2008, la gran mayoría de las mujeres de toda China dieron a luz en el hospital, exceptuando la región IV, la región rural más remota, en la que el porcentaje de nacimientos en hospitales fue de un 60,8%. Los nacimientos en hospitales de esta región aumentaron progresivamente antes de 2002, pero dicha tendencia se ralentizó poco después. Durante el periodo comprendido entre 1998 y 2001, el ascenso anual medio fue de un 21%, pero entre 2002 y 2008 cayó hasta un 10% (p = 0,0031). Las desigualdades entre las regiones socioeconómicas fueron superiores a las existentes entre las unidades domésticas pertenecientes a diversos niveles de ingresos. Antes de 2008, la diferencia entre las unidades domésticas con ingresos bajos y altos en la proporción de nacimientos en hospitales se había reducido en gran medida (un 96,1% y un 87,7% de las unidades domésticas con ingresos altos y bajos, respectivamente, dieron a luz en hospitales durante ese año).
Conclusión
En la actualidad, la mayoría de las mujeres de China dan a luz en el hospital, si bien la región rural más pobre del país sigue quedándose rezagada. Será necesario aplicar un enfoque mucho más activo y global para que aumenten los nacimientos en los hospitales entre la población de estas regiones lejanas y de difícil acceso.
Introduction
China has made remarkable progress in reducing maternal mortality, and several studies indicate that it may be close to achieving the fifth Millennium Development Goal (MDG 5).1–3 China’s success has been largely attributed to the strategy of improving hospital delivery: institutional deliveries have risen dramatically, even in the most remote rural areas.2,3 However, the government is now concerned about a widening gap between the rich and the poor in access to health care, including obstetric care.4,5
The boom in China’s economy has reduced poverty overall, but economic reforms have also triggered worry over rising inequalities in access to health care.5–9 The market reforms introduced in the 1980s have led to a deterioration of preventive health services and a dramatic increase in health-care expenditure.4,10–16 The central government decentralized fiscal responsibility to local government, and central government transfers in the health sector have declined.4,14–17 As a result, health insurance coverage has decreased sharply and an inability to pay is considered to be the main obstacle for the uptake of maternity care, especially for poor rural households.5,6,18
Over the last fifteen years the government has responded to these concerns in several ways. In 1995 it passed the Law on Maternal and Infant Health Care, which guarantees a woman’s right to institutional delivery. Targets for the proportion of hospital births are imposed by district authorities. In 2000, the government launched a comprehensive safe motherhood programme,19,20 the National Programme to Reduce Maternal Mortality and Eliminate Neonatal Tetanus, targeted at poor rural areas. The programme involved improved infrastructure; enhanced staff training and supervision in township and lower-level hospitals; the establishment of channels for referral to tertiary hospitals equipped to deal with emergency obstetric care; and the provision of subsidies to women and/or hospitals to encourage hospital delivery. By 2008 coverage had increased to more than half of all counties in China. In 2003, the government launched the New Cooperative Medical Scheme (NCMS), which provided further subsidies to encourage hospital delivery.21 The reimbursement policy for maternity care is decentralized and varies by county but, in general, normal deliveries are reimbursed for a flat fee and caesarean sections are reimbursed as a proportion of total expenditure, with a ceiling.18
Whether these policies have reduced the gap between the rich and the poor in access to maternal health care is uncertain. There is no evidence of widening regional disparities in maternal mortality and access to obstetric care over time,2,3 but the evidence on disparities between rich and poor households is inconsistent. Liu et al.5 reported an increase in income-related inequality in hospital delivery rates in rural areas between 1993 and 2003, whereas Long et al.18 found a decrease in the gap in hospital deliveries between the richest and poorest income groups in rural western China between 2002 and 2007. The evidence regarding the impact of the NCMS on the economic burden imposed by health care is also inconclusive.18,22–24 According to some studies, the NCMS has not decreased out-of-pocket expenditure;21,24 according to others, it has reduced the out-of-pocket costs of delivery.18,22
The objective of this paper is to examine trends in hospital births in China between 1988 and 2008, especially among the poor. We specifically examine whether trends have changed in the poorest regions and among the poorest households from 2002 onwards, when subsidies for hospital birth were gradually implemented. By focusing our analysis on equity in access to hospital birth, we provide insights into the ways in which the safe motherhood strategy in China may have served the poor.
Methods
We used data from four cross-sectional National Health Service Surveys conducted in urban and rural China in 1993, 1998, 2003 and 2008. All surveys were conducted on the same sample of villages, with minor modifications over time, and all used four-stage stratified cluster random sampling to select households. In the first stage, cities/counties were randomly selected from five socioeconomic strata developed by the Ministry of Health.25 This system divides China into socioeconomic regions based on a range of social and economic indicators derived from the 1982 census. The indicators include the employment rate, the percent of the population less than 14 and more than 65 years of age, educational achievements and illiteracy rate, crude birth rate and death rate, infant mortality rate and gross domestic product (GDP) per capita. Each survey sampled a similar number of cities/counties (92, 95, 95 and 94 in the 1993, 1998, 2003 and 2008 surveys, respectively). Within each city/county five districts/townships were sampled, and two villages were surveyed within each district/township. Each survey randomly sampled around 60 households from each village. The total number of households sampled in each survey was 54 984, 56 994, 57 023 and 56 456, respectively.
Locally trained health personnel interviewed household members using a structured questionnaire. All women of reproductive age were questioned about the characteristics of the most recent birth before the survey, including the place of delivery and the number of antenatal visits attended. The recall period was six years for the 1993 survey, two years for the 1998 survey, and five years for the 2003 and 2008 surveys. Data were missing for births in 1994 and 1995.
The questionnaires included a comprehensive list of sociodemographic indicators. Because many of these variables were correlated (data not shown), we selected the following for analysis: socioeconomic region of residence, annual household income, the educational attainment of the mother in the household, access to health insurance, maternal age and parity. Socioeconomic regions were categorized as urban (combining large, medium and small cities) and rural (types I, II, III and IV, this last being the poorest). In each survey households were categorized into five quintiles in accordance with their annual income per capita (gross household income divided by the number of individuals in the household). Thus, the income ranges varied by survey. Per capita income in the poorest quintile, for example, ranged from less than 320 yuan in 1993 to less than 2125 yuan in 2008. Per capita income in the richest quintile, on the other hand, ranged from more than 1200 yuan in 1993 to more than 7500 yuan in 2008. Access to health insurance was defined as any self report of being covered by either a social or a private health insurance plan.
Our analysis was restricted to live births. The outcome of interest was the per cent of births in hospital, including township, county, provincial or national hospitals, including county-level maternal and child care centres. To make our findings representative of the whole country, the data was weighted for the probability of an individual’s inclusion in the sample. We calculated the probability of sample selection at the city or county level by dividing the sampled population by the total population in each city or county, using the census data closest to the date of the survey to calculate the total population.
We used multilevel Poisson regression with allowance for clustering at the city/county and village level and sample stratification to assess crude and adjusted relative risks (RRs) of hospital births over time and in various groups. We chose Poisson regression because the outcome of interest was common and we wanted to compute RRs rather than odds ratios (ORs).26,27 We adjusted the RRs for year, region, household income quintile, mother’s education, health insurance, antenatal visits (4 or more), parity and mother’s age. We modelled year as a linear variable (assuming a constant change per year) and allowed for changes in trend in 1996, when the Law on Maternal and Infant Health Care went into effect, and in 2002, when the major subsidy policies were initiated. We explored yearly trend interactions with socioeconomic region, income quintile, health insurance and parity to determine whether births in hospitals were changing at the same rate over time in all socioeconomic regions and all income, insurance and parity subgroups.
Results
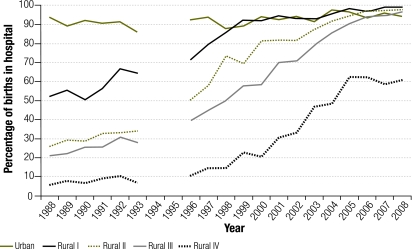
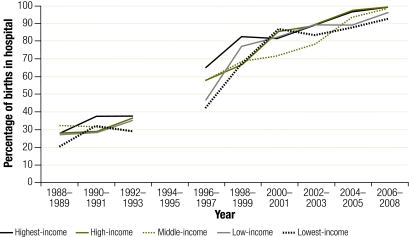
Information on the place of delivery was available for 34 482 live births between 1988 and 2008 (13 727 in 1993; 3981 in 1998; 9006 in 2003 and 7768 in 2008). Trends over time and by region in the proportion of births in hospital are shown in Fig. 1. Hospital births increased from 44.3% of all live births in 1988 to 94.7% in 2008. By 2008, nearly all women in urban and rural China were giving birth in hospital except in the most remote rural region (IV), where only about 60.8% of all live births took place in hospital in 2008. These trends resulted in a reduced gap in hospital births between urban residents and residents of rural region IV (Fig. 1).
Fig. 1.
Trends in hospital births by socioeconomic region, China, 1988–2008
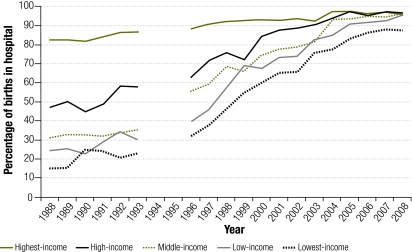
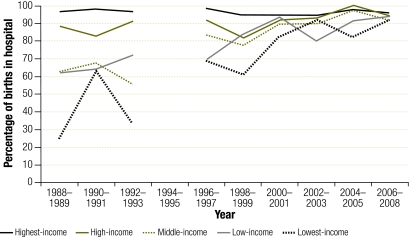
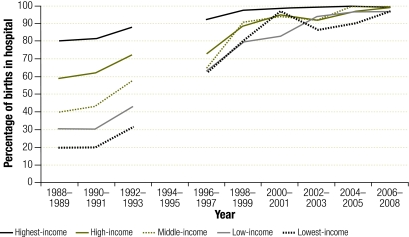
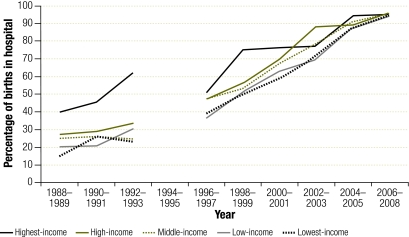
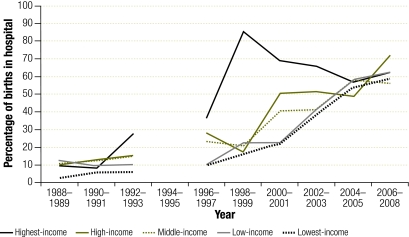
Fig. 2 shows trends over time in the proportion of hospital births by income group. The gap between low- and high-income households nearly disappeared: in 2008, 96.1% and 87.7% of high- and low-income households, respectively, gave birth in hospital. The distribution of income groups was not uniform across regions: in urban areas only 2.3% of births were from households having the lowest income, compared with 54.1% in rural region IV. Similarly, 57.6% of urban births were from households with the highest income, compared with 1.9% of births in remote rural region IV. Fig. 3, Fig. 4, Fig. 5, Fig. 6 and Fig. 7 shows trends over time in the proportion of hospital births by region and income group. Data for two-year periods were pooled to improve the precision of the estimates. All income groups in urban and rural regions I, II and III converged towards nearly universal coverage of hospital births. In rural region IV, trends were remarkably similar among the different income groups, with 58.8–62.3% of the women giving birth in hospital in 2008.
Fig. 2.
Trends in hospital births by household income group, China, 1988–2008
Fig. 3.
Trends in hospital births by income group in urban socioeconomic region, China, 1988–2008
Fig. 4.
Trends in hospital births by income group in rural I socioeconomic region, China, 1988–2008
Fig. 5.
Trends in hospital births by income group in rural II socioeconomic region, China, 1988–2008
Fig. 6.
Trends in hospital births by income group in rural III socioeconomic region, China, 1988–2008
Fig. 7.
Trends in hospital births by income group in rural IV socioeconomic region, China, 1988–2008
The results of the Poisson regression are shown in Table 1. The proportion of hospital births increased by 6% per year during 1988–1993 (crude RR: 1.06; 95% CI: 1.04–1.09), and this trend was sustained during 1996–2001 (crude RR: 1.06; 95% CI: 1.03–1.09). After 2001, hospital births continued to rise by 4% per year (crude RR: 1.04; 95% CI: 1.03–1.05), although part of this increase was accounted for by sociodemographic change (2% annual trend adjustment). However, the upward trend slowed down significantly between 1996–2001 and 2002–2008 (P-value for change in trend = 0.0076).
Table 1. Hospital births in China: time trends and sociodemographic determinants, 1988–2008.
| Trend/Determinant | No. of births | Births in hospital (%) | Crude RR (95% CI) | Adjusted RR (95% CI) |
|---|---|---|---|---|
| Linear trends within time periods | ||||
| Annual trend, 1988–1993 | 13 727 | 45.0 | 1.06 (1.04–1.09) | 1.05 (1.03–1.07) |
| Annual trend, 1996–2001 | 10 194 | 70.4 | 1.06 (1.03–1.09) | 1.06 (1.04–1.08) |
| Annual trend, 2002–2008 | 10 561 | 90.0 | 1.04 (1.03–1.05) | 1.02 (1.01–1.03) |
| Region | ||||
| Urban | 6 398 | 92.2 | 3.90 (2.96–5.13) | 2.57 (2.00–3.29) |
| Rural I | 5 537 | 75.9 | 3.21 (2.39–4.30) | 2.42 (1.91–3.06) |
| Rural II | 8 263 | 58.0 | 2.45 (1.78–3.38) | 2.10 (1.60–2.74) |
| Rural III | 9 333 | 51.9 | 2.19 (1.59–3.02) | 1.92 (1.49–2.48) |
| Rural IV | 4 982 | 23.7 | 1.00 | 1.00 |
| Household income | ||||
| Highest | 6 472 | 90.0 | 1.88 (1.59–2.23) | 1.12 (1.03–1.23) |
| High | 7 156 | 69.9 | 1.47 (1.25–1.73) | 1.07 (0.98–1.16) |
| Middle | 5 874 | 62.6 | 1.31 (1.13–1.52) | 1.03 (0.95–1.12) |
| Low | 7 975 | 51.9 | 1.09 (0.96–1.23) | 0.99 (0.93–1.06) |
| Lowest | 6 998 | 47.6 | 1.00 | 1.00 |
| Education | ||||
| College and above | 1 453 | 97.4 | 2.86 (2.29–3.57) | 1.02 (0.90–1.16) |
| Secondary | 3 924 | 89.2 | 2.61 (2.11–3.24) | 1.20 (1.06–1.36) |
| Primary | 23 962 | 64.3 | 1.88 (1.56–2.28) | 1.18 (1.04–1.33) |
| None (illiterate) | 5 093 | 34.1 | 1.00 | 1.00 |
| Health insurance | ||||
| Yes | 11 999 | 87.7 | 1.66 (1.50–1.84) | 1.20 (1.11–1.29) |
| No | 22 514 | 52.8 | 1.00 | 1.00 |
| Antenatal visits, 4 or more | ||||
| Yes | 15 120 | 88.5 | 1.94 (1.72–2.19) | 1.29 (1.21–1.38) |
| No | 19 393 | 45.6 | 1.00 | 1.00 |
| Age (years) at delivery | ||||
| ≤ 19 | 1 444 | 52.4 | 0.79 (0.71–0.88) | 0.91 (0.85–0.98) |
| 20–34 | 30 935 | 66.1 | 1.00 | 1.00 |
| 35–49 | 2 134 | 62.7 | 0.95 (0.89–1.02) | 1.04 (0.99–1.10) |
| Paritya | ||||
| 3+ | 4 833 | 31.7 | 0.41 (0.36–0.47) | 0.69 (0.62–0.76) |
| 2 | 11 010 | 57.4 | 0.74 (0.69–0.80) | 0.90 (0.87–0.94) |
| 1 | 18 636 | 77.2 | 1.00 | 1.00 |
CI, confidence interval; RR, relative risk.
a Defined as the total number of stillbirths and live births.
The percentage of hospital births differed substantially between regions. Urban women were four times more likely to give birth in hospital than women in rural region IV (crude RR: 3.90; 95% CI: 2.96–5.13) (Table 1). Birth in hospital was much more common among the richest women and those with a college education or higher, but this variation was largely explained by other factors (adjusted RR for lowest versus highest income households: 1.12; 95% CI: 1.03–1.23); adjusted RR for illiterate women versus women with a college education or higher: 1.02; 95% CI: 0.90–1.16). Women with health insurance were more likely to give birth in hospital, but the effect was small (adjusted RR: 1.20; 95% CI: 1.11–1.29). Nearly half (45.9%) of all live births occurred among multiparas (parity of 2 or higher), and such women were less likely to give birth in hospital than women delivering for the first time.
Results of time trends in hospital births by sociodemographic group are shown in Table 2. We pooled the data for 1988–2001 because trends were similar during 1988–1993 and 1996–2001 (data not shown). The yearly increase in hospital births was most pronounced among women living in the poorest region; among the poorest households; among women with insurance and among multiparous women. For example, in rural region IV the average yearly increase in the proportion of hospital births was 21% during 1988–2001 and 10% during 2002–2008. The trends are different across regions (P < 0.0001 for 1988–2001; P < 0.0001 for 2002–2008), and no upward trend was noted in urban areas. The rise in hospital births was more pronounced among multiparas than among primiparas.
Table 2. Time trends in hospital births by socioeconomic region, household income, health insurance and parity, China, 1988–2008.
| Annual trends | Hospital births |
|
|---|---|---|
| Crude RR (95% CI) | Adjusted RRa (95% CI) | |
| Model 1: By socioeconomic region | ||
| 1988–2001 | ||
| Urban | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) |
| Rural I | 1.06 (1.02–1.10) | 1.05 (1.02–1.07) |
| Rural II | 1.12 (1.05–1.19) | 1.10 (1.04–1.17) |
| Rural III | 1.13 (1.08–1.17) | 1.12 (1.07–1.17) |
| Rural IV | 1.21 (1.09–1.34) | 1.17 (1.05–1.30) |
| 2002–2008 | ||
| Urban | 1.01 (1.00–1.02) | 1.00 (1.00–1.01) |
| Rural I | 1.02 (1.00–1.03) | 1.00 (0.98–1.01) |
| Rural II | 1.05 (1.02–1.07) | 1.06 (1.02–1.10) |
| Rural III | 1.06 (1.04–1.09) | 1.03 (1.01–1.05) |
| Rural IV | 1.10 (1.02–1.19) | 1.07 (0.99–1.16) |
| Model 2: By household income | ||
| 1988–2001 | ||
| Highest income | 1.01 (1.00–1.02) | 1.01 (1.00–1.02) |
| High income | 1.07 (1.04–1.09) | 1.05 (1.03–1.07) |
| Middle income | 1.09 (1.06–1.12) | 1.08 (1.05–1.11) |
| Low income | 1.13 (1.09–1.17) | 1.11 (1.07–1.15) |
| Lowest income | 1.15 (1.11–1.20) | 1.13 (1.09–1.17) |
| 2002–2008 | ||
| Highest income | 1.01 (1.00–1.02) | 1.01 (1.00–1.01) |
| High income | 1.02 (1.01–1.04) | 1.01 (0.99–1.03) |
| Middle income | 1.06 (1.04–1.07) | 1.03 (1.01–1.05) |
| Low income | 1.05 (1.03–1.06) | 1.03 (1.01–1.05) |
| Lowest income | 1.05 (1.03–1.08) | 1.03 (1.01–1.05) |
| Model 3: By health insurance | ||
| 1988–2001 | ||
| Health insurance | 1.09 (1.06–1.12) | 1.08 (1.05–1.10) |
| No health insurance | 1.00 (0.98–1.02) | 1.01 (1.00–1.03) |
| 2002–2008 | ||
| Health insurance | 1.07 (1.05–1.08) | 1.01 (1.00–1.03) |
| No health insurance | 1.02 (1.01–1.03) | 1.02 (1.01–1.04) |
| Model 4: By parity | ||
| 1988–2001 | ||
| Parity 1 | 1.03 (1.01–1.05) | 1.04 (1.02–1.05) |
| Parity 2+ | 1.09 (1.06–1.13) | 1.08 (1.05–1.12) |
| 2002–2008 | ||
| Parity 1 | 1.03 (1.02–1.04) | 1.01 (1.00–1.02) |
| Parity 2+ | 1.07 (1.05–1.08) | 1.05 (1.02–1.07) |
CI, confidence interval; RR, relative risk.
a Relative risk adjusted for all other variables in the table.
The annual increase in hospital births in rural region IV slowed down after 2002 (from 21% per year during 1988–2001 to 10% per year during 2002–2008; P = 0.0031). The annual increase in hospital births among the poorest quintile also slowed down (from 15% during 1988–2001 to 5% per year during 2002–2008; P < 0.0001). Hospital births rose dramatically among women with health insurance during 1988–2001 and 2002–2008, but the increase during 2002–2008 was entirely accounted for by sociodemographic factors.
Discussion
Using data from four National Health Service Surveys, we reported nationally representative rates of uptake of hospital birth in China between 1988 and 2008. We found that China has made great progress towards ensuring that all women, irrespective of their economic status, give birth in hospital. The gaps between urban regions and poor rural regions and between high- and low-income households are closing fast, and nearly two thirds of women in the most remote rural region now give birth in hospital.
The rising institutional birth rates in rural areas are corroborated by findings from other studies.2,3,11,15,18,28,29 The gap in institutional birth rates between urban and rural regions is narrowing, which suggests that China’s safe motherhood strategy, with its regional focus, is working. However, in recent years the upward trend has been slowing down among those living in rural region IV. In this region, the percentage of institutional births has levelled at around 60% since 2005. This is a cause for concern, particularly since these regions continue to have high maternal mortality.3
The most remote rural region is lagging behind for several reasons. Despite the fact that by 2008 68% of all counties in rural region IV were covered by the national safe motherhood programme19 (this programme targeted counties that had some capacity, even if minimal),19 the most remote counties with poor infrastructure and scarce human resources may have been left behind. Women in remote areas travel long distances to reach a hospital, but smaller township hospitals in these areas may be poorly equipped for deliveries.30,31 The absence of caesarean section and blood transfusion in some of these hospitals may deter women from delivering there.30 Some evidence also suggests that women in the most remote counties, particularly those from ethnic minorities, are reluctant to deliver in hospital because of the discomfort and embarrassment associated with modern birthing practices.31–33
According to many studies, inability to pay is one of the main obstacles to the uptake of maternity care in China, especially among poor rural households.10,15,18,34 Our analysis suggests that inequalities between socioeconomic regions are more pronounced than between individual households. It did not show household income to be an important determinant of hospital delivery, since the gap between high- and low-income households has nearly disappeared. The NCMS, which had achieved nearly universal coverage by 2007,24 may have reduced the financial barriers affecting rural households. The NCMS covers only a modest part of the actual cost of institutional deliveries,18,31 and the mean out-of-pocket expenditure reported for institutional births among low-income groups in western rural China is still a substantial burden for the poor in the most remote regions.18,35 Most families now probably recognize the need to give birth in hospital and are willing to bear the additional costs involved.
Lower institutional birth rates among women giving birth for the second or third time have also been found in other studies. This suggests that fear of disapproval or chastisement among multiparas for not complying with government policy on family size may be a deterrent to institutional delivery11,36,37. However, in rural areas and among ethnic minorities the one-child policy is relaxed11,38,39 and higher order births are far from negligible. Encouragingly, the rate at which higher order births are attended in hospital increased by 7% per year between 2002 and 2008.
The data in this study are nationally representative and the sample size is large, but there are limitations. First, births not approved by the family planning system or among rural migrants who were temporarily away from home when the surveys were conducted may have been missed. Migration from rural to urban areas has increased dramatically since 1992, when the sampling frame for the surveys was designed.40 The exclusion of migrants from National Health Service Surveys may have biased the results by affecting trends and income inequalities in institutional births in urban areas. Since migrant women usually belong to the lowest income group and seldom use formal services,41,42 we may have overestimated the proportion of institutional births among the urban poor. Second, rural counties were classified into socioeconomic strata more than 15 years ago and their status could have changed. Nonetheless, the latest National Health Services Survey report suggests that few counties would be re-classified if more recent data were used.43 Third, we used a modified Poisson regression to compute RRs. Logistic regression tends to be the natural choice when the outcome is binary, but the OR overestimates the RR when the outcome is common. To estimate RR directly, binomial regression and Poisson regression with robust standard errors are usually recommended.26,27 We used Poisson regression because the maximum likelihood estimation of the binomial model did not converge.
Institutional deliveries are not a guarantee of good obstetric care. Consequently, one must be cautious when inferring that institutional births have reduced maternal or perinatal mortality.44,45 Institutional births are more conducive to caesarean sections, although the rise in institutional birth rates in China does not explain the rise in caesareans.28 Some studies suggest that obstetric practice is becoming more evidence-informed in county hospitals and higher-level hospitals,46 whereas the quality of care in some rural township hospitals may still be alarmingly poor.30 However, previous research in China has shown that the observed reductions in maternal mortality can be attributed in large measure to increasing institutional birth rates.2,3 Using two different national databases, the authors showed independently that variations in the coverage of hospital deliveries fully explained the declining trends in maternal mortality in China. China’s safe motherhood programme has focused almost exclusively on the promotion of hospital delivery, with doctors rather than midwives attending the deliveries. Midwifery care has been marginalised in China32,33,47 to the extent that very few women give birth with a trained midwife.
China’s sustained commitment to safe motherhood has resulted in impressive improvements in access to institutional birth across all socioeconomic groups, and most Chinese women now give birth in hospital. However, the poorest rural region is still lagging behind and this is causing concern because maternal mortality remains persistently high.3 Ensuring access to hospital delivery in this region is an enormous challenge: roads are poor, distances are long, populations are dispersed, township hospitals are under-resourced and some women may be reluctant to give birth in hospital. A more active mobilization of communities and additional professional and financial resources will be needed to ensure that women in remote regions are transferred to county hospitals where better quality obstetric care can be offered.
Acknowledgements
We thank the China Medical Board and the Centre for Statistics and Information, Ministry of Health of China, directed by Keqin Rao. We also thank Yanqiu Gao from the Department of Maternal and Child Health, Peking University; Guisheng Liu from the Department of Rural Health, Ministry of Health; and Yaoguang Zhang from the Centre for Statistics and Information, Ministry of Health of China .
Funding:
Xing Lin Feng is funded by the China Medical Board.
Competing interests:
None declared.
References
- 1.Hogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, Makela SM, et al. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet. 2010;375:1609–23. doi: 10.1016/S0140-6736(10)60518-1. [DOI] [PubMed] [Google Scholar]
- 2.Yanqiu G, Ronsmans C, Lin A. Time trends and regional differences in maternal mortality in China from 2000 to 2005. Bull World Health Organ. 2009;87:913–20. doi: 10.2471/BLT.08.060426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feng XL, Zhu J, Zhang L, Song L, Hipgrave D, Guo S, et al. Socio-economic disparities in maternal mortality in China between 1996 and 2006. BJOG. 2010;117:1527–36. doi: 10.1111/j.1471-0528.2010.02707.x. [DOI] [PubMed] [Google Scholar]
- 4.Wagstaff A, Yip W, Lindelow M, Hsiao WC. China’s health system and its reform: a review of recent studies. Health Econ. 2009;18(Suppl 2):S7–23. doi: 10.1002/hec.1518. [DOI] [PubMed] [Google Scholar]
- 5.Liu Y, Rao K, Wu J, Gakidou E. China’s health system performance. Lancet. 2008;372:1914–23. doi: 10.1016/S0140-6736(08)61362-8. [DOI] [PubMed] [Google Scholar]
- 6.Tang S, Meng QY, Chen L, Bekedam H, Evans T, Whitehead M. Tackling the challenges to health equity in China. Lancet. 2008;372:1493–501. doi: 10.1016/S0140-6736(08)61364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao Z. Income Inequality, Unequal Health Care Access, and Mortality in China. Popul Dev Rev. 2006;32:461–83. doi: 10.1111/j.1728-4457.2006.00133.x. [DOI] [Google Scholar]
- 8.Bloom G, Xingyuan G. Health sector reform: lessons from China. Soc Sci Med. 1997;45:351–60. doi: 10.1016/S0277-9536(96)00350-4. [DOI] [PubMed] [Google Scholar]
- 9.Fang P, Dong S, Xiao J, Liu C, Feng X, Wang Y. Regional inequality in health and its determinants: evidence from China. Health Policy. 2010;94:14–25. doi: 10.1016/j.healthpol.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Kaufman J, Jing F. Privatisation of health services and the reproductive health of rural Chinese women. Reprod Health Matters. 2002;10:108–16. doi: 10.1016/S0968-8080(02)00090-3. [DOI] [PubMed] [Google Scholar]
- 11.Short S, Zhang F. Use of maternal health services in rural China. Popul Stud (Camb) 2004;58:3–19. doi: 10.1080/0032472032000175446. [DOI] [PubMed] [Google Scholar]
- 12.Yip WC, Hsiao W, Meng Q, Chen W, Sun X. Realignment of incentives for health-care providers in China. Lancet. 2010;375:1120–30. doi: 10.1016/S0140-6736(10)60063-3. [DOI] [PubMed] [Google Scholar]
- 13.Blumenthal D, Hsiao W. Privatization and its discontents–the evolving Chinese health care system. N Engl J Med. 2005;353:1165–70. doi: 10.1056/NEJMhpr051133. [DOI] [PubMed] [Google Scholar]
- 14.Yip W, Hsiao WC. The Chinese health system at a crossroads. Health Aff (Millwood) 2008;27:460–8. doi: 10.1377/hlthaff.27.2.460. [DOI] [PubMed] [Google Scholar]
- 15.Bogg L, Wang K, Diwan V. Chinese maternal health in adjustment: claim for life. Reprod Health Matters. 2002;10:95–107. doi: 10.1016/S0968-8080(02)00076-9. [DOI] [PubMed] [Google Scholar]
- 16.Jing F. Health sector reform and reproductive health services in poor rural China. Health Policy Plan. 2004;19(Suppl 1):i40–9. doi: 10.1093/heapol/czh044. [DOI] [PubMed] [Google Scholar]
- 17.Hu S, Tang SL, Liu YL, Zhao YX, Escobar ML, de Ferranti D. Reform of how health care is paid for in China: challenges and opportunities. Lancet. 2008;372:1846–53. doi: 10.1016/S0140-6736(08)61368-9. [DOI] [PubMed] [Google Scholar]
- 18.Long Q, Zhang T, Xu L, Tang S, Hemminki E. Utilisation of maternal health care in western rural China under a new rural health insurance system (New Co-operative Medical System). Trop Med Int Health. 2010;15:1210–7. doi: 10.1111/j.1365-3156.2010.02602.x. [DOI] [PubMed] [Google Scholar]
- 19.Feng XL, Shi G, Wang Y, Xu L, Luo H, Shen J, et al. An impact evaluation of the Safe Motherhood Program in China. Health Econ. 2010;19(Suppl):69–94. doi: 10.1002/hec.1593. [DOI] [PubMed] [Google Scholar]
- 20.Liu X, Yan H, Wang D. The evaluation of “Safe Motherhood” program on maternal care utilization in rural western China: a difference in difference approach. BMC Public Health. 2010;10:566. doi: 10.1186/1471-2458-10-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wagstaff A, Lindelow M, Jun G, Ling X, Juncheng Q. Extending health insurance to the rural population: an impact evaluation of China’s new cooperative medical scheme. J Health Econ. 2009;28:1–19. doi: 10.1016/j.jhealeco.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 22.Babiarz KS, Miller G, Yi H, Zhang L, Rozelle S. New evidence on the impact of China’s New Rural Cooperative Medical Scheme and its implications for rural primary healthcare: multivariate difference-in-difference analysis. BMJ. 2010;341:c5617. doi: 10.1136/bmj.c5617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feng Z. Chinese health care in rural areas. BMJ. 2010;341:c5254. doi: 10.1136/bmj.c5254. [DOI] [PubMed] [Google Scholar]
- 24.Lei X, Lin W. The New Cooperative Medical Scheme in rural China: does more coverage mean more service and better health? Health Econ. 2009;18(Suppl 2):S25–46. doi: 10.1002/hec.1501. [DOI] [PubMed] [Google Scholar]
- 25.The guideline manual for the Fourth National Health Services Survey. Beijing: Ministry of Health of China; 2008. Chinese.
- 26.Schmidt CO, Kohlmann T. When to use the odds ratio or the relative risk? Int J Public Health. 2008;53:165–7. doi: 10.1007/s00038-008-7068-3. [DOI] [PubMed] [Google Scholar]
- 27.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 28.Sufang G, Padmadas SS, Fengmin Z, Brown JJ, Stones RW. Delivery settings and caesarean section rates in China. Bull World Health Organ. 2007;85:755–62. doi: 10.2471/BLT.06.035808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anson O. Utilization of maternal care in rural HeBei Province, the People’s Republic of China: individual and structural characteristics. Health Policy. 2004;70:197–206. doi: 10.1016/j.healthpol.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 30.Gao Y, Barclay L. Availability and quality of emergency obstetric care in Shanxi Province, China. Int J Gynaecol Obstet. 2010;110:181–5. doi: 10.1016/j.ijgo.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Harris A, Zhou Y, Liao H, Barclay L, Zeng W, Gao Y. Challenges to maternal health care utilization among ethnic minority women in a resource-poor region of Sichuan Province, China. Health Policy Plan. 2010;25:311–8. doi: 10.1093/heapol/czp062. [DOI] [PubMed] [Google Scholar]
- 32.Cheung NF. Chinese midwifery: the history and modernity. Midwifery. 2009;25:228–41. doi: 10.1016/j.midw.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 33.Harris A, Belton S, Barclay L, Fenwick J. Midwives in China: ‘jie sheng po’ to ‘zhu chan shi’. Midwifery. 2009;25:203–12. doi: 10.1016/j.midw.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 34.Wu Z, Viisainen K, Li X, Hemminki E. Maternal care in rural China: a case study from Anhui province. BMC Health Serv Res. 2008;8:55. doi: 10.1186/1472-6963-8-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Long Q, Zhang Y, Raven J, Wu Z, Bogg L, Tang S, et al. Giving birth at a health-care facility in rural China: is it affordable for the poor? Bull World Health Organ. 2011;89:144–52. doi: 10.2471/BLT.10.079434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen J, Xie Z, Liu H. Son preference, use of maternal health care, and infant mortality in rural China, 1989–2000. Popul Stud (Camb) 2007;61:161–83. doi: 10.1080/00324720701340194. [DOI] [PubMed] [Google Scholar]
- 37.Li J. Gender inequality, family planning, and maternal and child care in a rural Chinese county. Soc Sci Med. 2004;59:695–708. doi: 10.1016/j.socscimed.2003.11.041. [DOI] [PubMed] [Google Scholar]
- 38.Hesketh T, Lu L, Xing ZW. The effect of China’s one-child family policy after 25 years. N Engl J Med. 2005;353:1171–6. doi: 10.1056/NEJMhpr051833. [DOI] [PubMed] [Google Scholar]
- 39.Winckler EA. Chinese reproductive policy at the turn of the millennium: dynamic stability. Popul Dev Rev. 2002;28:379–418. doi: 10.1111/j.1728-4457.2002.00379.x. [DOI] [Google Scholar]
- 40.Hu X, Cook S, Salazar MA. Internal migration and health in China. Lancet. 2008;372:1717–9. doi: 10.1016/S0140-6736(08)61360-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhao Q, Kulane A, Gao Y, Xu B. Knowledge and attitude on maternal health care among rural-to-urban migrant women in Shanghai, China. BMC Womens Health. 2009;9:5. doi: 10.1186/1472-6874-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shaokang Z, Zhenwei S, Blas E. Economic transition and maternal health care for internal migrants in Shanghai, China. Health Policy Plan. 2002;17(Suppl):47–55. doi: 10.1093/heapol/17.suppl_1.47. [DOI] [PubMed] [Google Scholar]
- 43.Centre for Health Statistics and Information, Ministry of Health of China. An analysis report of national health services survey in China, 2008 Beijing: Chinese Academy of Medical Science & Peking Union Medical College Press; 2009. Chinese. [Google Scholar]
- 44.Wax JR, Lucas FL, Lamont M, Pinette MG, Cartin A, Blackstone J. Maternal and newborn outcomes in planned home birth vs planned hospital births: a metaanalysis. Am J Obstet Gynecol 2010;203:e1-243.e8. [DOI] [PubMed]
- 45.Ronsmans C, Chowdhury ME, Koblinsky M, Ahmed A. Care seeking at time of childbirth, and maternal and perinatal mortality in Matlab, Bangladesh. Bull World Health Organ. 2010;88:289–96. doi: 10.2471/BLT.09.069385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Qian X, Smith H, Liang H, Liang J, Garner P. Evidence-informed obstetric practice during normal birth in China: trends and influences in four hospitals. BMC Health Serv Res. 2006;6:29. doi: 10.1186/1472-6963-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cheung NF, Zhang L, Mander R, Xu X, Wang X. Proposed continuing professional education programme for midwives in China: New mothers’ and midwives’ views. Nurse Educ Today. 2010 doi: 10.1016/j.nedt.2010.08.014. [DOI] [PubMed] [Google Scholar]