Abstract
Ischaemic stroke is a disorder involving multiple mechanisms of injury progression including activation of glutamate receptors, release of proinflammatory cytokines, nitric oxide (NO), free oxygen radicals and proteases. Presently, recombinant tissue plasminogen activator (rtPA) is the only drug approved for the management of acute ischaemic stroke. This drug, however, is associated with limitations like narrow therapeutic window and increased risk of intracranial haemorrhage. A large number of therapeutic agents have been tested including N-methly-D-aspartate (NMDA) receptor antagonist, calcium channel blockers and antioxidants for management of stroke, but none has provided significant neuroprotection in clinical trials. Therefore, searching for other potentially effective drugs for ischaemic stroke management becomes important. Immunosuppressive agents with their wide array of mechanisms have potential as neuroprotectants. Corticosteroids, immunophilin ligands, mycophenolate mofetil and minocycline have shown protective effect on neurons by their direct actions or attenuating toxic effects of mediators of inflammation. This review focuses on the current status of corticosteroids, cyclosporine A, FK506, rapamycin, mycophenolate mofetil and minocycline in the experimental models of cerebral ischaemia.
Keywords: Cerebral ischaemia, immunosuppressants, in vitro and in vivo models, neuroprotection
Introduction
Cerebral stroke (brain attack) is the most life- threatening cerebovascular disorder, the second leading cause of death and principle cause of disability in the world1. Even with advances in treatment of stroke, 20-50 per cent of the patient die within a month or become dependent on others2. Stroke results due to interruption of cerebral blood flow causing irreversible and fatal damage to the affected neurons. There are two main types of strokes, ischaemic and haemorrhagic. Ischaemic stroke accounts nearly for 85 per cent of all reported stroke incidents and is the main focus of the current studies. This type of stroke occurs when a thrombus or embolus blocks cerebral blood flow resulting in cerebral ischaemia and consequently neuronal damage and cell death. Haemorrhagic stroke occurs due to rupture of any blood vessel in the brain resulting in rapid cerebral damage and accounts for the remaining 15 per cent stroke cases.
Intravenous recombinant tissue plasminogen activator (rtPA) is the only approved therapy for management of ischaemic stroke3. Patients who receive this drug within the initial 3 h therapeutic window also have a high risk of intracranial haemorrhage, usually 6-8 per cent against 0.6-2 per cent spontaneous hemorrhages in stroke4–5. Other limitations associated with rtPA therapy like disruption of blood brain barrier; seizures and progression of neuronal damage6–8 are major concerns. Thus, there is a continued need for exploring novel neuroprotective strategies for the management of ischaemic stroke.
Recent studies on immunosuppressive agents have revealed their neuroprotective potential in ischaemic stroke. Immunosuppressive agents have shown promise as being neuroprotective in safeguarding the neurons against excitotoxic insults and also improving neurological functions and infarct volume in experimental models of ischaemic stroke9–13. These agents have direct effect on microglia cells and inhibit mediators of inflammation. In order to appreciate the potential role of immunosuppressive agents in ischaemia, revisiting the pathophysiology of cerebral ischaemia is required. This review briefly focuses on the mechanisms involved in cerebral ischaemic stroke and how the immunosuppressive agents have shown potential in its management.
The aetiopathology and mechanisms of cell death in ischaemia
The interruption in blood flow to the brain results in reduced supply of oxygen and nutrients to the neurons. The lack of blood supply results in two identifiable areas namely the core and penumbra. The core which is a neuronal dead area is not accessible to therapeutic intervention whereas the penumbra is a still salvageable zone and is the target of the most therapeutic interventions (Fig.). The consequence of ischaemia can briefly be described as below.
Fig.
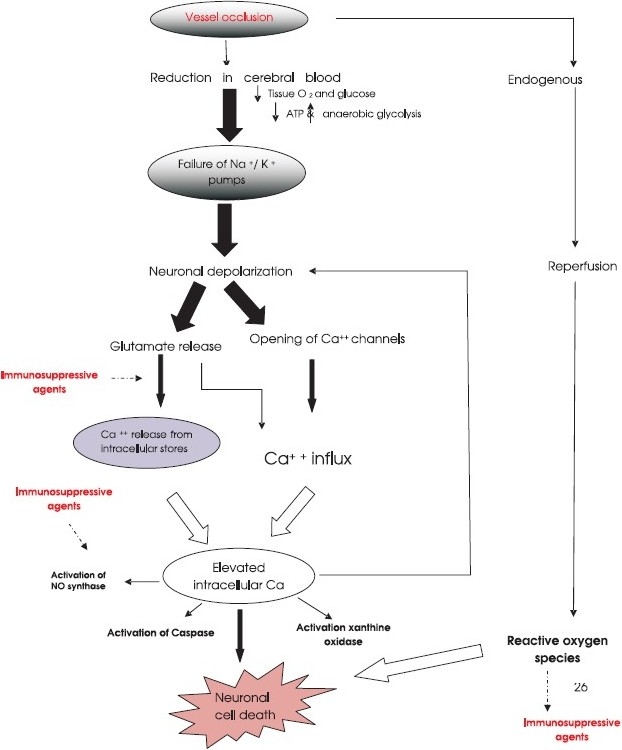
A simplistic presentation of the cascade of events occurring in cerebral ischaemia and possible sites of immunosuppressive agents actions.
Energy depletion: Consequent to reduction/loss of blood supply inside the core, the adenosine triphosphate (ATP) levels are reduced leading to incarceration of cellular metabolism14. The lack of energy results in impaired ion homeostasis.
Calcium overload and activation of glutamate receptors: Disrupted ion homeostasis leads to rapid depolarization, and large influx of calcium and potassium. The intracellular calcium overload results in activation of excitotoxic glutamatergic transmission, nitric oxide (NO) synthase, caspase, xanthine oxidase and release of reactive oxygen species15 (Fig.).
Excess glutamate release leads to activation of phospholipases, phospholipid hydrolysis and arachidonic acid release, ultimately resulting in necrotic as well as apoptotic cell death16–18. Generation of free radicals, lipid peroxidation, inflammatory cascade and activation of immediate early genes such as c-fos, c-jun, leads to progressive ischaemic damage.
The generation of reactive oxygen species in the core area is less as compared to penumbra because there is negligible blood supply to core. The penumbra is still the viable tissue surrounding the core, and receives trivial amount of blood from collateral arteries19. This area is therefore, the target for drug intervention and has potential for recovery. If no quick and effective drug intervention is done, this further progresses to cellular energy failure, release of excitotoxic neurotransmitters and reactive oxygen species and finally, cellular death in the region.
Mechanism of cell death
Neurodegeneration
Neurodegeneration is described by the loss of neuronal functions and cell death20. Neuronal degeneration and cell death occurs through apoptotic as well as necrotic pathways21. Cell death is characterized by imbalance in cellular homeostasis, influx of calcium, mitochondrial dysfunction and generation of reactive free radicals22,23.
(i) Necrotic cell death - Energy depletion leads to release of excitatory amino acids (EAAs) such as glutamate24. Excessive release of glutamate activates α-amino-3-hydroxy-5-methlyl-4-isoxazolone-proprionic acid (AMPA) receptors which increase sodium influx25 and the N-methly-D-aspartate (NMDA) receptors which mediate the influx of calcium26. This increase in calcium overload results in activation of proteases such as caspases and matrix metalloproteases (MMP). The aftermath of this activation is increased proteolytic injury and ultimately cell death27. Many calcium dependent and calcium induced enzymes mediate intracellular calcium induced toxicity like NO synthase, cyclooxygenase, phospholipase A 2 and calpain128. Increased intracellular calcium activates NO synthase and results in release of NO29. The NO then combines with superoxide generated as by- product from cyclooxygenase, or xanthine oxidase to produce highly reactive peroxynitrite, that results in tissue destruction30. Cells are not capable of protecting themselves against excessive reactive oxygen species and ultimately die.
(ii) Apoptotic cell death - In apoptotic cell death there is transcription of immediate early genes such as c-fos, c-jun leading to caspase cascade resulting in increased cytokine levels within hours of initial injury. The released cytokines cause activation of cell surface receptors such as Fas receptor and tumour necrosis factor-alpha receptor (TNF- α) leading to apoptotic cell death31 32. TNF- α stimulates the production of bcl-2 family protein, bid33. Bid activates bax, another bcl-2 family member and increases mitochondrial permeability, resulting in release of cytochrome c, a key component in apoptosis initiation. Cytochrome c forms a complex with apoptotic protease activating factor-1 (APAF -1) and procaspase -9, this complex causes cleavage of procaspase – 9 to caspase 9 and ultimately activation of other caspases including casapase-334. Caspase-3 injury leads to irreversible DNA damage and cell death35. Generation of reactive oxygen species during cerebral ischaemia also activates process of apoptosis36 leading to activation of transcription factor p53 and caspases thus resulting in DNA damage37.
Inflammation and ischaemia - role of microglia cells
The continued ischaemic injury to brain cells results in to a complex inflammatory cascade. It is characterized by infiltration of leukocytes mainly polymorphonuclear (PMN) cells, monocytes/macrophages lymphocytes and the activation of microglia which are the resident immune cells of the brain38. Astrocytes, neuronal support cells, also contribute to inflammation during insult39. Astrocytes under normal conditions perform several functions like, glutamate uptake, glutamate release and maintain cellular and ion homeostasis40. During cerebral injury, astrocytes undergo morphological changes and become activated41. Activated astrocytes release proinflammtory cytokines and chemokines thus results in initiation and progression of inflammation39.
In cerebral ischaemia, microglia, resident brain macrophages become activated and release detrimental neurotoxic mediators like proinflammtory cytokines, superoxide, nitric oxide (NO), TNF- α and proteases 42–44. Many of these mediators can inturn influence the microglia morphology and activate it in a paracrine and autocrine fashion45. Among the proinflammatory cytokines interleukin- 1 (IL-1) is most abundantly expressed in microglia cells46. IL-1 induces the expression of other cytokines such as IL-6 and TNF-α47 which contribute to the progression of ischaemic damage. The inhibition of this pathway of neuronal damage can be considered a logical option.
Other agents that have an important role in stroke injury are proteases. Tissue plasminogen activator, a potential neurotoxicant released by microglia cells is implicated in cerebral ischaemic injury48. Other proteases that play a leading role in disruption of blood brain barrier are matrix metalloproteases which contribute to secondary brain damage in cerebral ischaemia49. NO is a small molecule, secreted by microglia cells, acts directly on neurons as neurotoxin or indirectly by potentiating excitotoxic transmitters50. Inhibition of microglia activation in ischaemia may provide a novel target in management of stroke, the immunosuppressive agents, therefore, may serve the purpose to a greater extent.
Is rtPA good enough in acute stroke?
Currently, recombinant tissue plasminogen activator (rtPA) is the only drug approved by US Food and Drug Administration for management of acute ischaemic stroke51. Several limitations are associated with rtPA including the narrow 3 h therapeutic window, increased risk of intracranial haemorrhage, generation of free oxygen radicals and recurrent stroke5,51. The rtPA has only clot busting activity and this activity is bothersome because it can lead to progression of secondary neuronal damage52.
For developing potent neuroprotective agents two main strategies are focused, clot lysis activity and safeguard of neurons subjected to ischaemic damage. rtPA is adequate for clot lysis, but there have been many unsuccessful attempts in developing effective neuroprotective drugs for management of stroke.
Drugs under investigation for ischaemic stroke
Several studies conducted on drugs of different groups have exhibited neuroprotection in experimental models of cerebral ischaemia. One of these agents is endothelin antagonist (TAK-044), a reported anti-inflammmatory and antioxidant agent53. In oxygen-glucose deprivation model of cerebral ischaemia, TAK-044 showed significant improvement in percentage cell viability as compared to cells in hypoxic condition54. In rat model of focal cerebral ischaemia, TAK-044 significantly improved the neurological parameters, oxidative stress markers and infarct volume53. Several other agents have also shown potential of protecting the ischaemic cerebral injury by antioxidant mechanism. Agents like α-tocopherol55, trans-resveratrol56 and melatonin57 have shown significant improvement in neurobehavioural paradigms, infarct size and oxidative stress markers in experimental model of cerebral ischaemia.
The other group of drugs that showed promise is statins, 3-hydroxy-3-methyglutaryl (3- HMG)- CoA reductase inhibitors. Several studies have reported the beneficial effects of statins in experimental model of cerebral ischaemia58–60. The neuroprotective effects of statins are reported to be mediated by inhibiting inducible NO synthase thus resulting in inhibition of proinflammtory cytokines60. Beside these agents, recent studies have also shown neuroprotection by human umbilical cord cells61,62 in experimental models of cerebral ischaemia.
Recent findings have focused on drugs which can be given as stand alone or in combination with rtPA for management of stroke. One of these agents is imatinib, an anticancer drug. Imatinib is tyrosine kinase inhibitor used in treatment of chronic myeloid leukaemia. The rtPA neurotoxicity is thought to be mediated through platelet derived growth factor–CC (PDGF-CC)63. Recently Su et al63 have shown that administration of imatinib, PDGF-CC antagonist, one hour after vessel occlusion and 5 h later application of rtPA drastically reduced the infarct volume by 34 per cent and incidence of intracranial haemorrhage by 50 per cent as compared to rtPA alone in mouse model of stroke. One single administration of imatinib before the rtPA administration may provide an adequate neuroprotection in stroke patients, but this aspect needs to be validated in clinical settings. Till these agents are tested in clinical trials, no concrete conclusions can be drawn from animal models.
Neuroprotection by immunosuppressive agents: a new dimension
As the ischaemic stroke has a multifactorial aetiopathology, and the mechanisms that are involved are activation of glutamate receptors, release of proinflammatory cytokines, TNF-α, NO, reactive oxygen radicals and proteases, the drugs having combinational neuroprotective and anti-inflammatory activity will be theoretically more effective in its management. Immunosuppressive agents have shown potential as neuroprotectants and anti-inflammatory agents in experimental models of cerebral ischaemia (Fig.). Drugs including steroids, immunophilin ligands and mycophenolate mofetil (MMF) have been in use as immunosuppressants since 1970s and these have been effectively used in avoiding organ rejection in transplant patients. Recent studies have reported their protective effect in microglial and neuronal cell cultures and in animal models of cerebral ischaemia64. Steroids, cyclosporine A, FK506, MMF and minocycline have been reported to have direct inhibitory effects on activation of microglia cells. This effect is mediated by inhibition of secretion of proinflammtory cytokines and NO from microglia cells64 (Table).
Table.
Effects produced by immunosuppressive agents in experimental models of ischaemic stroke
| Immunosuppressive drugs investigated | Experimental model | Effect produced | References |
|---|---|---|---|
| Steroids (Cortisol, corticosterone & dexamethasone) Dexamethasone | Isolated glial cells | Inhibition proliferation and activity of iNOS. | Chao et al, 199269; Drew & Chavis, 200070; |
| Inhibition of release of TNF- α and IL-6. | Jacobsson et al, 200671 | ||
| Suppression of production of MCP-1. | |||
| Permanent middle cerebral artery occlusion model in rats. | Reduction in expression of TNF- α. | Bertorelli et al, 199872 | |
| Permanent middle cerebral artery occlusion model in cats. | Beneficial effect on cerebral oedema. | Fenske et al, 197973 | |
| Occlusion of middle cerebral arteries in hyperglycaemic cat. | Reduce size of infarcts. | de Courten-Myers, 199474 | |
| Cyclosporine A | Rat neuronal cells. | Inhibit caspase activation. | Capano et al, 20029 |
| Human neuroblastoma cells. | Prevents apoptosis and enhance neurite outgrowth. | Sheehan et al, 200684 | |
| Transient forebrain ischaemia in rats. | Reduced brain oedema and infarct size. | Shiga et al, 199285 | |
| Hippocampal CA1 neurons. | Improvement in survival. | Uchino et al, 199586; Miyata et al, 200187 | |
| Global ischaemia rat model. | Inhibit activation of microglia cells secreted proinflammatory substances. | Wakita et al, 199588 | |
| Tacrolimus, FK506 | Cortical cell against excitotoxic neuronal death. | Prevents dephosphorylation of nitric oxide synthase. | Dawson et al, 199392 |
| Rodent model of focal ischaemia. | Neuroprotective effect. | Sharkey and Butcher, 199411 | |
| Transient global ischaemia model in gerbils. | Reduce delayed neuronal death mediated by inhibition of neuronal nitric oxide synthase. | Tokime et al, 199694 | |
| Primate model of cerebral ischaemia. | Improved neurological functions. | Furuichi et al, 200695 | |
| Rapamycin | Microglial cells. | Inhibits expression of inducible nitric oxide synthase. | Lu et al, 2006100 |
| Traumatic injury model in mice. | Improved the functional recovery. | Erlich et al, 2007101 | |
| Mycophenolate Mofetil | Organotypic hippocampal slice cultures. | Attenuated neuronal damage induced by excitotoxic injury. | Dehghani et al, 2003104 |
| Mice model of amyotrophic lateral sclerosis. | Reduced microglial activation, improved stem cell survival and delayed the onset of neurological symptoms. | Yan et al, 2006106 | |
| Minocycline | Mixed SC and pure microglia cultures. | Inhibition of NMDA activated p38 MAPK, No and IL- 1β release. | Tikka et al, 2001112 |
| Global ischaemia in gerbils. | Inhibition of microglial cells. | Yrjanheikki et al, 199812 | |
| Focal ischaemia in rats. | Reduced infarct volume & Inhibition of microglial cells. | Yrjanheikki et al, 199913 |
iNOS, inducible nitric oxide synthase; TNF- α, tumor necrosis factor-alpha; IL-6, interleukin- 1; MCP-1, monocyte chemoattractant protein-1; NMDA, N-methyl-D-aspartate; p38 MAPK, p38 mitogen-activated protein kinase; NO, nitric oxide
Steroids in cerebral ischaemia: an unresolved issue
For many years corticosteroids have been used for the treatment of brain oedema65. Overwhelming evidence has reported the protective effects of corticosteroids, both in vitro as well as in a variety of animal models66,67.
In vitro studies using steroids have shown inhibition of both microglial cell proliferation and activity of NO synthase68 in the isolated microglial cells. Several investigators have reported that treatment of isolated microglial cells with steroid reduce the release of the proinflammatory substances69–71 and thus restricting the inflammation cascade and protecting neurons against the ischaemic insult. Treatment with dexamethasone on gerbil hippocampal regions diminished the ischaemia induced glutamate toxicity and consequently protected the neurons10. Dexamethasone has also been shown to suppress monocyte chemoattractant protein-1 (MCP-1) production via inhibition of jun-N-terminal kinase and p38 mitogen activated protein kinase in activated microglial cells8.
In in vivo studies, application of dexamethasone in permanent middle cerebral artery occlusion model in rats reduced the expression of TNF-α and decreased the inflammatory cascade72. Dexamethasone treatment in a model of permanent occlusion of middle cerebral artery in cats showed neuroprotective effects73. In an interesting experiment by de Courten – Myers et al74 4 h occlusion of middle cerebral arteries in hyperglycaemic cats, and administration of high dose of corticosteroids 30 min after occlusion, significantly reduced the size of infarcts as compared to untreated group.
The mechanism of neuroprotection by corticosteroids is speculated to be either due to activation of membrane receptors on neurons by circulating steroids and hence leading to rapid changes in properties of exposed neuron or their modulation of nuclear transcription of various genes67. The beneficial effects of corticosteroids are largely due to preservation of neuronal structures and improvement in behavioural functions.
Interestingly in contrast to the experimental evidences, in the clinical trials, the steroids have not shown any beneficial effects. In a retrospective study on patients with history of ischaemic stroke, disability and mortality rates were worse in patients taking steroids as compared to those without steroid treatment75. There was no difference between the outcomes i.e., the disability and mortality as well as adverse effects between the two groups. In another study, patients with acute cerebral infarction were treated either with dexamethasone or placebo and the patients in steroid group fared worse than the placebo group76.
In summary, corticosteroids have shown favourable neuroprotective profile in experimental models of ischaemic stroke but failed to provide any significant beneficial effect in ischaemic patients. Thus, the use of corticosteroids as neuroprotective agents still remains controversial and there is a need to re-evaluate these in well planned clinical trials.
How effective are immunophilin ligands in stroke?
A plethora of evidence is available that indicates the role of immunophilin/calcineurin in brain function and development77–79. High levels of immunophilins are expressed in brain and these are believed to be involved in neuronal apoptosis mechanisms80. Cyclosporin, tacrolimus/FK506 and rapamycin are immunophilin binding ligands used in avoiding rejection of transplanted organs.
Cyclosporine A: Cyclosporine A is an 11 amino acid cyclic peptide of fungal origin having effective immunosuppressive action. The mechanism of action of cyclosporine A involves binding to cyclophilin, an intracellular protein belonging to immunophillin family. Cyclosporine A and cyclophillin complex inhibits calcium/calmodulin dependent activation of calcineurin and via this pathway cyclosporine inhibits production of IL-281 and gamma interferon and other lymphokines82. Cyclosporine A can also reduce the expression of an intracellular adhesion molecule and affect subsequent inflammation cascade83.
Cyclosporine A has shown antiapoptotic activity by inhibiting activation of caspase in rat neuronal cells9. It showed protective effect against apoptosis in human neuroblastoma cells by enhancing neurite outgrowth84. Cyclosporine A has shown to reduce brain oedema, infarct size and improved the survival of hippocampal CA1 neurons probably due to enhanced phosphorylation of cAMP response element binding (CREB) protein and increase in production of brain derived neurotrophic factor in experimental model of transient forebrain ischaemia in rats85–87. In the global ischaemia rat model, cyclosporine A showed beneficial effects by inhibiting the activation of microglia cells and thus providing protection against microglia secreted proinflammatory substances88. Till now cyclosporine A has not been tested in clinical trials for the treatment of CNS disorders but it has been tried in autoimmune disorders.
Cyclosporine A treatment in rats with experimental autoimmune myasthenia gravis has shown protective effects by reducing the levels of acetylcholine receptor antibodies by 50 per cent89. Mahattanakul et al90 have reported antinflammatory effect of cyclosporine A in patients suffering from chronic inflammatory demyelinating polyneuropathy. In this study, cyclosporine A treatment was successful in 3 out of 8 patients and the therapy with this agent did not show any serious side effects. In summary, cyclosporine A does have potential in neuroprotective strategy and needs to be evaluated experimentally and in clinical trials.
Tacrolimus/FK506: FK506 is an immunosuppressant introduced in 1990s and the mechanism of action is similar to that of cyclosporine A. FK506 binds with FK506 binding protein (FKBP), an immunophilin, and makes a complex which results in inhibition of downstream activation of nuclear factor of activated T-cells (NFAT), hence controlling relevant immunological genes91.
In in vitro studies, FK506 has shown protection against excitotoxic neuronal death in cortical cell cultures92. In another in vitro study, FK506 protected the cultured cortical neurons against oxygen glucose deprivation. The action was inhibited in the presence of an antibody against FKBP-12 suggesting that FK506 acts via FKBP-1293.
FK506 has been shown to provide protection in rodent model of focal ischaemia and this neuroprotection was thought to be mediated by immunophillins11, but in subsequent study done in gerbils in transient global ischaemia model, FK506 reduced delayed neuronal death and this effect was not mediated by inhibition of neuronal NO synthase, again binding to physiological target was anticipated94.
In primate model of cerebral ischaemia, FK506 showed a significant improvement in neurological deficits95. FK506 has been shown to have neuroprotective effects on cultured neurons and also in experimental models of ischaemic stroke, still a mechanistic pathway for its neuroprotective effect of tacrolimus needs to be explored.
Rapamycin: Rapamycin is a macrolide antibiotic developed as an antifungal agent but was later discovered to have potent immunosuppressive and anti-proliferative properties. Rapamycin is an immunophillin ligand that structurally resembles FK506. Unlike FK506 and cyclosporine A, rapamycin binds to mammalian targets of rapamycin (mTOR) and prevents phosphorylation of p70S6K, 4EBP1 and other proteins involved in transcription, translation and cell cycle control96. Rapamycin also antagonizes the anti-apoptotic signals mediated by mTOR97, and induces autophagy and maintains normal cell metabolism98.
Literature is available stating the benefitting effects of rapamycin in in vitro and in vitro models of cerebral ischaemia. An in vitro study reported that application of rapamycin at different concentrations did not affect the bioelectrical activity and evoked field excitatory post-synaptic potentials magnitude in hippocampal slices99 suggesting an alternative to calcineurin inhibitors in events of neurotoxicity. Rapamycin treatment inhibits the hypoxia induced expression of inducible NO synthase in microglial cells100. In mice after experimental traumatic brain injury, rapamycin significantly improved the functional recovery101. Anti-depressant like effects of rapamycin in rodents have also been reported suggesting a role in treatment of affective disorders102. Effects of rapamycin in experimental models of cerebral ischaemia have not been systematically investigated. More studies have to be undertaken to fully acknowledge the neuroprotective significance of rapamycin.
Does mycophenolate mofetil (MMF) have any potential as neuroprotectant?
MMF is a prodrug converted into active mycophenolic acid in body and inhibits inosine mono phosphate dehydrogenase, a critical enzyme required in de novo purine biosynthesis. Inhibition of this enzyme leads to reduction in purine nucleotides and inhibition of cellular proliferation. MMF suppresses the monocytic production of both pro-inflammatory cytokines and microglial mitogen granulocyte macrophage colony stimulating factor103. It has also shown to prevent microglial activation as well as reduce the neuronal damage induced by excitotoxic injury in the in vitro model of stroke104. The microglial activation is an important pathway of proinflammatory cytokines generation, nitric oxide production and activation and release of proteases, which leads to neuronal damage105.
Studies on the effects of MMF in animal models of CNS disorders are sparse. In mice model of amyotrophic lateral sclerosis, MMF treatment reduced microglial activation, improved stem cell survival and delayed the onset of neurological symptoms106. MMF has also shown protection against experimental autoimmune myasthenia gravis in rats107and has also been used against inflammatory myopathy and chronic inflammatory demylelinating polyradiculoneuropathy108. Thus MMF is an interesting candidate but its use in ischaemic brain diseases needs further exploration.
Effects of minocycline - an approach to ischaemic damages?
Minocycline is semisynthetic tetracycline derivative, which also possesses anti-inflammatory properties that are entirely distinct from its antimicrobial action. Studies have shown its usefulness in management of rheumatoid arthritis and osteoarthritis109. Minocycline has been recognized to have numerous pharmacological effects including ability to inhibit MMP, superoxide production and iNOS expression in human cartilage and murine macrophages110,111. Minocycline has been reported to penetrate blood brain barrier and provide neuroprotection in global ischaemia in gerbils12 and focal ischaemia in rats13. In these studies the neuroprotection by minocycline was associated with reduced activation of microglia and also inhibition of induction of IL-1b-converting enzyme (ICE) mRNA which was expressed mostly in microglia. In nanomolar concentrations it protected neurons in mixed spinal cord (SC) as well as pure microglia cultures against NMDA excititoxicity112. NMDA activated p38 mitogen-activated protein kinase (p38 MAPK), NO and IL- 1β release were effectively inhibited by minocycline in mixed spinal cord and pure microglia cultures113. Thus it indicates the direct effect of monocycline on microglia activation and proliferation.
Minocycline also demonstrated delayed mortality in transgenic R 6/2 model of Huntington disease by inhibiting caspase 1 and 3 expression as well as iNOS activity114. Minocycline treatment exhibited protection in MPTP (1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine) model of Parkinson’s disease, this neuroprotection was mediated by reduction in expression of inducible NO synthase (iNOS) and caspase -1 expression115. Recently a placebo controlled open label clinical trial of minocycline in acute stroke has shown significant beneficial effects116. To the best of our knowledge three clinical trials are under investigation to evaluate the effects of minocycline in acute ischaemic stroke117. In one study, safe and well tolerated doses of minocycline are being evaluated whereas in other study minocycline, enoxaparin or combination of both will be studied on acute ischaemic stroke patients. The effect of minocycline on neurological deficits and functional outcomes in acute ischaemic stroke patients will be assessed in the other enlisted clinical trial117.
Conclusion
Cerebral ischaemia is a multifactorial disorder which includes a number of pathways for progression of injury to brain cells. Activation of glutamate receptors, release of NO, proteases and generation of free radicals are important mechanisms in ischaemia. Inflammation is considered a major component in disseminating the detrimental effects of cerebral ischaemia. Circumscription of inflammatory cascade is an integral part in ameliorating the harmful consequences in cerebral ischaemia. In this respect, immunosuppressive agents can prove to be valuable drugs in attenuating CNS damage following ischaemia.
Immunosuppressive agents have been shown to undermine the CNS damage following ischaemia by improved neuronal survival and inhibition of mediators of inflammation in various experimental models. In vitro experiments using immunosuppressive agents have demonstrated the blockade of excitotoxic insult induced by NMDA as well as inhibition of microglia cells, thus inhibiting inflammatory cascade. In vivo, these have been shown to improve the neurological functions as seen by neurological assessment paradigms and reductions in infarct volume.
More research is required before any definitive conclusion is derived for immunosuppressive agents as neuroprotectants. Minocycline is the only drug which is being evaluated in clinical trials. An important issue that needs to be addressed is: can there be a differential dose that causes neuroprotective effect than that required to cause immunosuppression? If these drugs exhibit neuroprotection at much lower doses than that required for preventing organ transplant rejection, it may be a potential addition to the existing therapeutic armamentarium for ischaemic stroke. This will require well designed clinical trials to evaluate short as well as long term clinical outcomes vis-a-vis side effect profile of each drug and translate it into improvement in quality of life of stroke patients.
References
- 1.Bonita R. Stroke prevention: A global perspective. In: Norris JW, Hachinski V, editors. Stroke prevention. New York: NY: Oxford University Press; 2001. pp. 259–74. [Google Scholar]
- 2.Truelsen T, Begg S, Mathers C. The global burden of cerebrovascular Disease. Available from: http://www.who.int/healthinfo/statistics/bod_cerebrovasculardiseasestroke.pdf, accessed on January 16, 2011.
- 3.Adams HP, Adams R, del Zoppo G, Goldstein LB. Guidelines for the early management of patients with ischaemic stroke: 2005 guidelines update. Stroke. 2005;36:916–21. doi: 10.1161/01.STR.0000163257.66207.2d. [DOI] [PubMed] [Google Scholar]
- 4.Külkens S, Hacke W. Thrombolysis with alteplase for acute ischaemic stroke: review of SITS-MOST and other Phase IV studies. Expert Rev Neurother. 2007;7:783–8. doi: 10.1586/14737175.7.7.783. [DOI] [PubMed] [Google Scholar]
- 5.The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333:1581–7. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 6.Tsirka SE, Rogove AD, Bugge TH, Degen JL, Strickland S. An extracellular proteolytic cascade promotes neuronal degeneration in the mouse hippocampus. J Neurosci. 1997;17:543–52. doi: 10.1523/JNEUROSCI.17-02-00543.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang YF, Tsirka SE, Strickland S, Stieg PE, Soriano SG, Lipton SA. Tissue plasminogen activator (tPA) increases neuronal damage after focal cerebral ischemia in wild-type and tPA-deficient mice. Nat Med. 1998;4:228–31. doi: 10.1038/nm0298-228. [DOI] [PubMed] [Google Scholar]
- 8.Zhuo M, Holtzman DM, Li Y, Osaka H, DeMaro J, Jacquin M, et al. Role of tissue plasminogen activator receptor LRP in hippocampal long-term potentiation. J Neurosci. 2000;20:542–9. doi: 10.1523/JNEUROSCI.20-02-00542.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Capano M, Virji S, Crompton M. Cyclophilin-A is involved in excitotoxin-induced caspase activation in rat neuronal B50 cells. Biochem J. 2002;363:29–36. doi: 10.1042/bj3630029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen J, Adachi N, Tsubota S, Nagaro T, Arai T. Dexamethasone augments ischemia-induced extracellular accumulation of glutamate in gerbil hippocampus. Eur J Pharmacol. 1998;347:67–70. doi: 10.1016/s0014-2999(98)00198-8. [DOI] [PubMed] [Google Scholar]
- 11.Sharkey J, Butcher SP. Immunophilins mediate the neuroprotective effects of FK506 in focal cerebral ischemia. Nature. 1994;371:336–9. doi: 10.1038/371336a0. [DOI] [PubMed] [Google Scholar]
- 12.Yrjänheikki J, Keinänen R, Pellikka M, Hökfelt T, Koistinaho J. Tetracyclines inhibit microglial activation and are neuroprotective in global brain ischemia. Proc Natl Acad Sci USA. 1998;95:15769–74. doi: 10.1073/pnas.95.26.15769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yrjänheikki J, Tikka T, Keinänen R, Goldsteins G, Chan PH, Koistinaho J. A tetracycline derivative, minocycline, reduces inflammation and protects against focal cerebral ischemia with a wide therapeutic window. Proc Natl Acad Sci USA. 1999;96:13496–500. doi: 10.1073/pnas.96.23.13496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lipton P. Ischemic cell death in brain neurons. Physiol Rev. 1999;79:1431–568. doi: 10.1152/physrev.1999.79.4.1431. [DOI] [PubMed] [Google Scholar]
- 15.Dirnagl U, Iadecola C, Moskowitz MA. Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci. 1999;22:391–7. doi: 10.1016/s0166-2236(99)01401-0. [DOI] [PubMed] [Google Scholar]
- 16.Rao AM, Hatcher JF, Kindy MS, Dempsey RJ. Arachidonic acid and leukotriene C4: role in transient cerebral ischemia of gerbils. Neurochem Res. 1999;24:1225–32. doi: 10.1023/a:1020916905312. [DOI] [PubMed] [Google Scholar]
- 17.Phillis JW, O’Regan MH. The role of phospholipases, cyclooxygenases, and lipoxygenases in cerebral ischemic/traumatic injuries. Crit Rev Neurobiol. 2003;15:61–90. doi: 10.1615/critrevneurobiol.v15.i1.30. [DOI] [PubMed] [Google Scholar]
- 18.Mattson MP, Culmsee C, Yu ZF. Apoptotic and antiapoptotic mechanisms in stroke. Cell Tissue Res. 2000;301:173–87. doi: 10.1007/s004419900154. [DOI] [PubMed] [Google Scholar]
- 19.Bandera E, Botteri M, Minelli C, Sutton A, Abrams KR, Latronico N. Cerebral blood flow threshold of ischaemic penumbra and infarct core in acute ischaemic stroke: a systematic review. Stroke. 2006;37:1334–9. doi: 10.1161/01.STR.0000217418.29609.22. [DOI] [PubMed] [Google Scholar]
- 20.Graham SH, Chen J. Programmed cell death in cerebral ischemia. J Cereb Blood Flow Metab. 2001;21:99–109. doi: 10.1097/00004647-200102000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Weinberger JM. Evolving therapeutic approaches to treating acute ischemic stroke. J Neurol Sci. 2006;249:101–9. doi: 10.1016/j.jns.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 22.Chan PH. Reactive oxygen radicals in signaling and damage in the ischaemic brain. J Cereb Blood Flow Metab. 2001;21:2–14. doi: 10.1097/00004647-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Globus MY-T, Busto R, Lin B, Schnippering H, Ginsberg MD. Detection of free radical activity during transient global ischemia and recirculation: effects of intraischemic brain temperature modulation. J Neurochem. 1995;65:1250–6. doi: 10.1046/j.1471-4159.1995.65031250.x. [DOI] [PubMed] [Google Scholar]
- 24.Fonnum F. Glutamate: A neurotransmitter in the mammalian brain. J Neurochem. 1984;42:1–11. doi: 10.1111/j.1471-4159.1984.tb09689.x. [DOI] [PubMed] [Google Scholar]
- 25.Endres M, Dirnagl U. Ischemia and stroke. Adv Exp Med Biol. 2002;513:455–73. doi: 10.1007/978-1-4615-0123-7_17. [DOI] [PubMed] [Google Scholar]
- 26.Choi DW, Koh JY, Peters S. Pharmacology of glutamate neurotoxicity in cortical cell culture: attenuation by NMDA antagonists. J Neurosci. 1988;8:185–9. doi: 10.1523/JNEUROSCI.08-01-00185.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White BC, Sullivan JM, DeGracia DJ, O’Neil BJ, Neumar RW, Grossman LI, et al. Brain ischemia and reperfusion: molecular mechanisms of neuronal injury. J Neurol Sci. 2000;179:1–33. doi: 10.1016/s0022-510x(00)00386-5. [DOI] [PubMed] [Google Scholar]
- 28.Graham SH, Hickey RW. Molecular pathophysiology of stroke. In: Davis KL, Charney D, Coyle JT, Nemeroff C, editors. Neuropsychopharmacology: The Fifth Generation of Progress. Nashville TN: American College of Neuropsychopharmacology; 2002. [Google Scholar]
- 29.Clark GD, Happel LT, Zorumski CF, Bazann NG. Enhancement of hippocampal excitatory synaptic transmission by platelet-activating factor. Neuron. 1992;9:1211–6. doi: 10.1016/0896-6273(92)90078-r. [DOI] [PubMed] [Google Scholar]
- 30.Ying W, Han SK, Miller JW, Swanson RA. Acidosis potentiates oxidative neuronal death by multiple mechanisms. J Neurochem. 1999;73:1549–56. doi: 10.1046/j.1471-4159.1999.0731549.x. [DOI] [PubMed] [Google Scholar]
- 31.Nagata S. Apoptosis regulated by a death factor and its receptor: Fas ligand and Fas. Philos Trans R Soc Lond B Biol Sci. 1994;345:281–7. doi: 10.1098/rstb.1994.0107. [DOI] [PubMed] [Google Scholar]
- 32.Beutler B, Bazzoni F. TNF, apoptosis and autoimmunity: a common thread? Blood Cells Mol Dis. 1998;24:216–30. doi: 10.1006/bcmd.1998.0187. [DOI] [PubMed] [Google Scholar]
- 33.Yin XM, Wang K, Gross A, Zhao Y, Zinkel S, Klocke B, et al. Bid-deficient mice are resistant to Fas-induced hepatocellular apoptosis. Nature. 1999;400:886–91. doi: 10.1038/23730. [DOI] [PubMed] [Google Scholar]
- 34.Li P, Nijhawan D, Budihardjo I, Srinivasula SM, Ahmad M, Alnemri ES, et al. Cytochrome c and DATP-dependent formation of APAF-1/caspase-9 complex initiates an apoptotic protease cascade. Cell. 1997;91:479–89. doi: 10.1016/s0092-8674(00)80434-1. [DOI] [PubMed] [Google Scholar]
- 35.Zukin RS, Jover T, Yokota H, Calderone A, Simionescu M, Lau C-Y. Molecular and cellular mechanisms of ischemiainduced neuronal death. In: Mohr JP, Choi DW, Grotta JC, Weir B, Wolf PA, editors. Stroke: pathophysiology, diagnosis, and management. Philadelphia: The Curtis Center; 2004. pp. 829–54. [Google Scholar]
- 36.Gupta YK, Gupta M, Kohli K. Neuroprotective role of melatonin in oxidative stress vulnerable brain. Indian J Physiol Pharmacol. 2003;47:373–86. [PubMed] [Google Scholar]
- 37.Gupta S, Gupta YK, Sharma SS. Protective effect of pifithrin-alpha on brain ischaemic reperfusion injury induced by bilateral common carotid arteries occlusion in gerbils. Indian J Physiol Pharmacol. 2007;51:62–8. [PubMed] [Google Scholar]
- 38.Kochanek PM, Hallenbeck JM. Polymorphonuclear leukocytes and monocytes/macrophages in the pathogenesis of cerebral ischemia and stroke. Stroke. 1992;23:1367–79. doi: 10.1161/01.str.23.9.1367. [DOI] [PubMed] [Google Scholar]
- 39.Ridet JL, Malhotra SK, Privat A, Gage FH. Reactive astrocytes: cellular and molecular cues to biological function. Trends Neurosci. 1997;20:570–7. doi: 10.1016/s0166-2236(97)01139-9. [DOI] [PubMed] [Google Scholar]
- 40.Swanson RA, Ying W, Kauppinen TM. Astrocyte influences on ischaemic neuronal death. Curr Mol Med. 2004;4:193–205. doi: 10.2174/1566524043479185. [DOI] [PubMed] [Google Scholar]
- 41.Pekny M, Nilsson M. Astrocyte activation and reactive gliosis. Glia. 2005;50:427–34. doi: 10.1002/glia.20207. [DOI] [PubMed] [Google Scholar]
- 42.Danton GH, Dietrich WD. Inflammatory mechanisms after ischemia and stroke. J Neuropathol Exp Neurol. 2003;62:127–36. doi: 10.1093/jnen/62.2.127. [DOI] [PubMed] [Google Scholar]
- 43.Dirnagl U, Iadecola C, Moskowitz MA. Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci. 1999;22:391–7. doi: 10.1016/s0166-2236(99)01401-0. [DOI] [PubMed] [Google Scholar]
- 44.Polazzi E, Contestabile A. Reciprocal interactions between microglia and neurons: from survival to neuropathology. Rev Neurosci. 2002;13:221–42. doi: 10.1515/revneuro.2002.13.3.221. [DOI] [PubMed] [Google Scholar]
- 45.Wirjatijasa F, Dehghani F, Blaheta RA, Korf HW, Hailer NP. Interleukin-4, interleukin-10, and interleukin-1-receptor antagonist but not transforming growth factor-beta induce ramification and reduce adhesion molecule expression of rat microglial cells. J Neurosci Res. 2002;68:579–87. doi: 10.1002/jnr.10254. [DOI] [PubMed] [Google Scholar]
- 46.Woodroofe MN, Sarna GS, Wadhwa M, Hayes GM, Loughlin AJ, Tinker A, et al. Detection of interleukin-1 and interleukin-6 in adult rat brain, following mechanical injury, by in vivo microdialysis: evidence of a role for microglia in cytokine production. J Neuroimmunol. 1991;33:227–36. doi: 10.1016/0165-5728(91)90110-s. [DOI] [PubMed] [Google Scholar]
- 47.Lee SC, Liu W, Dickson DW, Brosnan CF, Berman JW. Cytokine production by human fetal microglia and astrocytes. Differential induction by lipopolysaccharide and IL-1 beta. J Immunol. 1993;150:2659–67. [PubMed] [Google Scholar]
- 48.Tsirka S.E. Clinical implications of the involvement of tPA in neuronal cell death. J Mol Med. 1997;75:341–7. doi: 10.1007/s001090050119. [DOI] [PubMed] [Google Scholar]
- 49.del Zoppo GJ, Milner R, Mabuchi T, Hung S, Wang X, Berg GI, et al. Microglial activation and matrix protease generation during focal cerebral ischemia. Stroke. 2007;38:646–51. doi: 10.1161/01.STR.0000254477.34231.cb. [DOI] [PubMed] [Google Scholar]
- 50.Boje KM, Arora PK. Microglial-produced nitric oxide and reactive nitrogen oxides mediate neuronal cell death. Brain Res. 1992;587:250–6. doi: 10.1016/0006-8993(92)91004-x. [DOI] [PubMed] [Google Scholar]
- 51.Marler JR, Goldstein LB. Medicine. Stroke-tPA and the clinic. Science. 2003;301:1677. doi: 10.1126/science.1090270. [DOI] [PubMed] [Google Scholar]
- 52.Rieckmann P. Imatinib buys time for brain after stroke. Nat Med. 2008;14:712–3. doi: 10.1038/nm0708-712. [DOI] [PubMed] [Google Scholar]
- 53.Gupta YK, Briyal S, Sharma U, Jagannathan NR, Gulati A. Effect of endothelin antagonist (TAK-044) on cerebral ischaemic volume, oxidative stress markers and neurobehavioral parameters in the middle cerebral artery occlusion model of stroke in rats. Life Sci. 2005;77:15–27. doi: 10.1016/j.lfs.2004.11.025. [DOI] [PubMed] [Google Scholar]
- 54.Briyal S, Pant AB, Gupta YK. Protective effect of endothelin antagonist (TAK-044) on neuronal cell viability in in vitro oxygen-glucose deprivation model of stroke. Indian J Physiol Pharmacol. 2006;50:157–62. [PubMed] [Google Scholar]
- 55.Chaudhary G, Sinha K, Gupta YK. Protective effect of exogenous administration of alpha-tocopherol in middle cerebral artery occlusion model of cerebral ischemia in rats. Fundam Clin Pharmacol. 2003;17:703–7. doi: 10.1046/j.0767-3981.2003.00209.x. [DOI] [PubMed] [Google Scholar]
- 56.Sinha K, Chaudhary G, Gupta YK. Protective effect of resveratrol against oxidative stress in middle cerebral artery occlusion model of stroke in rats. Life Sci. 2002;71:655–65. doi: 10.1016/s0024-3205(02)01691-0. [DOI] [PubMed] [Google Scholar]
- 57.Sinha K, Degaonkar MN, Jagannathan NR, Gupta YK. Effect of melatonin on ischemia reperfusion injury induced by middle cerebral artery occlusion in rats. Eur J Pharmacol. 2001;428:185–92. doi: 10.1016/s0014-2999(01)01253-5. [DOI] [PubMed] [Google Scholar]
- 58.Vaughan CJ, Delanty N. Neuroprotective properties of statins in cerebral ischemia and stroke. Stroke. 1999;30:1969–73. doi: 10.1161/01.str.30.9.1969. [DOI] [PubMed] [Google Scholar]
- 59.Endres M, Laufs U, Huang Z, Nakamura T, Huang P, Moskowitz MA, et al. Stroke protection by 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase inhibitors mediated by endothelial nitric oxide synthase. Proc Natl Acad Sci USA. 1998;95:8880–5. doi: 10.1073/pnas.95.15.8880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Amin-Hanjani S, Stagliano NE, Yamada M, Huang PL, Liao JK, Moskowitz MA. Mevastatin, an HMG-CoA reductase inhibitor, reduces stroke damage and upregulates endothelial nitric oxide synthase in mice. Stroke. 2001;32:980–6. doi: 10.1161/01.str.32.4.980. [DOI] [PubMed] [Google Scholar]
- 61.Newcomb JD, Ajmo CT, Jr, Sanberg CD, Sanberg PR, Pennypacker KR, Willing AE. Timing of cord blood treatment after experimental stroke determines therapeutic efficacy. Cell Transplant. 2006;15:213–23. doi: 10.3727/000000006783982043. [DOI] [PubMed] [Google Scholar]
- 62.Vendrame M, Cassady J, Newcomb J, Butler T, Pennypacker KR, Zigova T, et al. Infusion of human umbilical cord blood cells in a rat model of stroke dose-dependently rescues behavioral deficits and reduces infarct volume. Stroke. 2004;35:2390–5. doi: 10.1161/01.STR.0000141681.06735.9b. [DOI] [PubMed] [Google Scholar]
- 63.Su EJ, Fredriksson L, Geyer M, Folestad E, Cale J, Andrae J, et al. Activation of PDGF-CC by tissue plasminogen activator impairs blood-brain barrier integrity during ischaemic stroke. Nat Med. 2008;14:731–7. doi: 10.1038/nm1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hailer NP. Immunosuppression after traumatic or ischaemic CNS damage: it is neuroprotective and illuminates the role of microglial cells. Prog Neurobiol. 2008;84:211–33. doi: 10.1016/j.pneurobio.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 65.Betz AL, Coester HC. Effect of steroids on edema and sodium uptake of the brain during focal ischemia in rats. Stroke. 1990;21:1199–204. doi: 10.1161/01.str.21.8.1199. [DOI] [PubMed] [Google Scholar]
- 66.Zhou Y, Ling EA, Dheen ST. Dexamethasone suppresses monocyte chemoattractant protein-1 production via mitogen activated protein kinase phosphatase-1 dependent inhibition of Jun N-terminal kinase and p38 mitogen-activated protein kinase in activated rat microglia. J Neurochem. 2007;102:667–78. doi: 10.1111/j.1471-4159.2007.04535.x. [DOI] [PubMed] [Google Scholar]
- 67.Schumacher M. Rapid membrane effects of steroid hormones: an emerging concept in neuroendocrinology. Trends Neurosci. 1990;13:359–62. doi: 10.1016/0166-2236(90)90016-4. [DOI] [PubMed] [Google Scholar]
- 68.Tanaka J, Fujita H, Matsuda S, Toku K, Sakanaka M, Maeda N. Glucocorticoid- and mineralocorticoid receptors in microglial cells: the two receptors mediate differential effects of corticosteroids. Glia. 1997;20:23–37. [PubMed] [Google Scholar]
- 69.Chao CC, Hu S, Close K, Choi CS, Molitor TW, Novick WJ, et al. Cytokine release from microglia: differential inhibition by pentoxifylline and dexamethasone. J Infect Dis. 1992;166:847–53. doi: 10.1093/infdis/166.4.847. [DOI] [PubMed] [Google Scholar]
- 70.Drew PD, Chavis JA. Inhibition of microglial cell activation by cortisol. Brain Res Bull. 2000;52:391–6. doi: 10.1016/s0361-9230(00)00275-6. [DOI] [PubMed] [Google Scholar]
- 71.Jacobsson J, Persson M, Hansson E, Ronnback L. Corticosterone inhibits expression of the microglial glutamate transporter GLT-1 in vitro. Neuroscience. 2006;139:475–83. doi: 10.1016/j.neuroscience.2005.12.046. [DOI] [PubMed] [Google Scholar]
- 72.Bertorelli R, Adami M, Di Santo E, Ghezzi P. MK 801 and dexamethasone reduce both tumor necrosis factor levels and infarct volume after focal cerebral ischemia in the rat brain. Neurosci Lett. 1998;246:41–4. doi: 10.1016/s0304-3940(98)00221-3. [DOI] [PubMed] [Google Scholar]
- 73.Fenske A, Fischer M, Regli F, Hase U. The response of focal ischaemic cerebral edema to dexamethasone. J Neurol. 1979;220:199–209. doi: 10.1007/BF00705537. [DOI] [PubMed] [Google Scholar]
- 74.de Courten-Myers GM, Kleinholz M, Wagner KR, Xi G, Myers RE. Efficacious experimental stroke treatment with high-dose methylprednisolone. Stroke. 1994;25:487–92. doi: 10.1161/01.str.25.2.487. [DOI] [PubMed] [Google Scholar]
- 75.De Reuck J, Vandekerckhove T, Bosma G, De Meulemeester K, Van Landegem W, De Waele J, et al. Steroid treatment in acute ischaemic stroke. A comparative retrospective study of 556 cases. Eur Neurol. 1988;28:70–2. doi: 10.1159/000116232. [DOI] [PubMed] [Google Scholar]
- 76.Norris JW. Steroid therapy in acute cerebral infarction. Arch Neurol. 1976;33:69–71. doi: 10.1001/archneur.1976.00500010071014. [DOI] [PubMed] [Google Scholar]
- 77.Butcher SP, Henshall DC, Teramura Y, Iwasaki K, Sharkey J. Neuroprotective actions of FK506 in experimental stroke: in vivo evidence against an antiexcitotoxic mechanism. J Neurosci. 1997;17:6939–46. doi: 10.1523/JNEUROSCI.17-18-06939.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mulkey RM, Endo S, Shenolikar S, Malenka RC. Involvement of a calcineurin/inhibitor-1 phosphatase cascade in hippocampal long-term depression. Nature. 1994;369:486–8. doi: 10.1038/369486a0. [DOI] [PubMed] [Google Scholar]
- 79.Nichols RA, Suplick GR, Brown JM. Calcineurin-mediated protein dephosphorylation in brain nerve terminals regulates the release of glutamate. J Biol Chem. 1994;269:23817–23. [PubMed] [Google Scholar]
- 80.Xin G, Dillman JF, Valina LD, Dawson TM. Neuroimmunophilins: novel neuroprotective and neuroregenerative targets. Ann Neurol. 2001;50:6–16. doi: 10.1002/ana.1030. [DOI] [PubMed] [Google Scholar]
- 81.Elliott JF, Lin Y, Mizel SB, Bleackley RC, Harnish DG, Paetkau V. Induction of interleukin 2 messenger RNA inhibited by cyclosporin A. Science. 1984;226:1439–41. doi: 10.1126/science.6334364. [DOI] [PubMed] [Google Scholar]
- 82.Reem GH, Cook LA, Vilcek J. Gamma interferon synthesis by human thymocytes and T lymphocytes inhibited by cyclosporin A. Science. 1983;221:63–5. doi: 10.1126/science.6407112. [DOI] [PubMed] [Google Scholar]
- 83.Soriano-Izquierdo A, Gironella M, Massaguer A, Salas A, Gil F, Piqué JM, et al. Effect of cyclosporin A on cell adhesion molecules and leukocyte-endothelial cell interactions in experimental colitis. Inflamm Bowel Dis. 2004;10:789–800. doi: 10.1097/00054725-200411000-00014. [DOI] [PubMed] [Google Scholar]
- 84.Sheehan J, Eischeid A, Saunders R, Pouratian N. Potentiation of neurite outgrowth and reduction of apoptosis by immunosuppressive agents: implications for neuronal injury and transplantation. Neurosurg Focus. 2006;20:E9. doi: 10.3171/foc.2006.20.5.10. [DOI] [PubMed] [Google Scholar]
- 85.Shiga Y, Onodera H, Matsuo Y, Kogure K. Cyclosporin A protects against ischemia-reperfusion injury in the brain. Brain Res. 1992;595:145–8. doi: 10.1016/0006-8993(92)91465-q. [DOI] [PubMed] [Google Scholar]
- 86.Uchino H, Elmer E, Uchino K, Lindvall O, Siesjo BK. Cyclosporine A dramatically ameliorates CA1 hippocampal damage following transient forebrain ischemia in the rat. Acta Physiol Scand. 1995;155:469–71. doi: 10.1111/j.1748-1716.1995.tb09999.x. [DOI] [PubMed] [Google Scholar]
- 87.Miyata K, Omori N, Uchino H, Yamaguchi T, Isshiki A, Shibasaki F. Involvement of the brain-derived neurotrophic factor/TrkB pathway in neuroprotecive effect of cyclosporin A in forebrain ischemia. Neuroscience. 2001;105:571–8. doi: 10.1016/s0306-4522(01)00225-1. [DOI] [PubMed] [Google Scholar]
- 88.Wakita H, Tomimoto H, Akiguchi I, Kimura J. Protective effect of cyclosporin A on white matter changes in the rat brain after chronic cerebral hypoperfusion. Stroke. 1995;26:1415–22. doi: 10.1161/01.str.26.8.1415. [DOI] [PubMed] [Google Scholar]
- 89.Drachman DB, Adams RN, McIntosh K, Pestronk A. Treatment of experimental myasthenia gravis with cyclosporin A. Clin Immunol Immunopathol. 1985;34:174–88. doi: 10.1016/0090-1229(85)90022-4. [DOI] [PubMed] [Google Scholar]
- 90.Mahattanakul W, Crawford TO, Griffin JW, Goldstein JM, Cornblath DR. Treatment of chronic inflammatory demyelinating polyneuropathy with cyclosporin-A. J Neurol Neurosurg Psychiatry. 1996;60:185–7. doi: 10.1136/jnnp.60.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rao A, Luo C, Hogan PG. Transcription factors of the NFAT family: regulation and function. Annu Rev Immunol. 1997;15:707–47. doi: 10.1146/annurev.immunol.15.1.707. [DOI] [PubMed] [Google Scholar]
- 92.Dawson TM, Steiner JP, Dawson VL, Dinerman JL, Uhl GR, Snyder SH. Immunosuppressant FK506 enhances phosphorylation of nitric oxide synthase and protects against glutamate neurotoxicity. Proc Natl Acad Sci USA. 1993;90:9808–12. doi: 10.1073/pnas.90.21.9808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Labrande C, Velly L, Canolle B, Guillet B, Masmejean F, Nieoullon A, et al. Neuroprotective effects of tacrolimus (FK506) in a model of ischaemic cortical cell cultures: role of glutamate uptake and FK506 binding protein 12 kDa. Neuroscience. 2006;137:231–9. doi: 10.1016/j.neuroscience.2005.08.080. [DOI] [PubMed] [Google Scholar]
- 94.Tokime T, Nozaki K, Kikuchi H. Neuroprotective effect of FK506, an immunosuppressant, on transient global ischemia in gerbil. Neurosci Lett. 1996;206:81–4. doi: 10.1016/s0304-3940(96)12438-1. [DOI] [PubMed] [Google Scholar]
- 95.Furuichi Y, Maeda M, Matsuoka N, Mutoh S, Yanagihara T. Therapeutic time window of tacrolimus (FK506) in a nonhuman primate stroke model: comparison with tissue plasminogen activator. Exp Neurol. 2006;204:138–46. doi: 10.1016/j.expneurol.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 96.Vignot S, Faivre S, Aguirre D, Raymond E. mTOR-targeted therapy of cancer with rapamycin derivatives. Ann Oncol. 2005;16:525–37. doi: 10.1093/annonc/mdi113. [DOI] [PubMed] [Google Scholar]
- 97.Guba M, von Breitenbuch P, Steinbauer M, Koehl G, Flegel S, Hornung M, et al. Rapamycin inhibits primary and metastatic tumor growth by antiangiogenesis: involvement of vascular endothelial growth factor. Nat Med. 2002;8:128–35. doi: 10.1038/nm0202-128. [DOI] [PubMed] [Google Scholar]
- 98.Kamada Y, Sekito T, Ohsumi Y. Autophagy in yeast: a TOR-mediated response to nutrient starvation. Curr Top Microbiol Immunol. 2004;279:73–84. doi: 10.1007/978-3-642-18930-2_5. [DOI] [PubMed] [Google Scholar]
- 99.Daoud D, Scheld HH, Speckmann EJ, Gorji A. Rapamycin: brain excitability studied in vitro. Epilepsia. 2007;48:834–6. doi: 10.1111/j.1528-1167.2006.00976.x. [DOI] [PubMed] [Google Scholar]
- 100.Lu DY, Liou HC, Tang CH, Fu WM. Hypoxia-induced iNOS expression in microglia is regulated by the PI3-kinase/Akt/mTOR signaling pathway and activation of hypoxia inducible factor-1alpha. Biochem Pharmacol. 2006;72:992–1000. doi: 10.1016/j.bcp.2006.06.038. [DOI] [PubMed] [Google Scholar]
- 101.Erlich S, Alexandrovich A, Shohami E, Pinkas-Kramarski R. Rapamycin is a neuroprotective treatment for traumatic brain injury. Neurobiol Dis. 2007;26:86–93. doi: 10.1016/j.nbd.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 102.Cleary C, Linde JA, Hiscock KM, Hadas I, Belmaker RH, Agam G, et al. Antidepressive-like effects of rapamycin in animal models: Implications for mTOR inhibition as a new target for treatment of affective disorders. Brain Res Bull. 2008;76:469–73. doi: 10.1016/j.brainresbull.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 103.Nagy SE, Andersson JP, Andersson UG. Effect of mycophenolate mofetil (RS-61443) on cytokine production: inhibition of super antigen induced cytokines. Immunopharmacology. 1993;26:11–20. doi: 10.1016/0162-3109(93)90062-u. [DOI] [PubMed] [Google Scholar]
- 104.Dehghani F, Hischebeth GT, Wirjatijasa F, Kohl A, Korf HW, Hailer NP. The immunosuppressant mycophenolate mofetil attenuates neuronal damage after excitotoxic injury in hippocampal slice cultures. Eur J Neurosci. 2003;18:1061–72. doi: 10.1046/j.1460-9568.2003.02821.x. [DOI] [PubMed] [Google Scholar]
- 105.Miljkovic D, Samardzic T, Cvetkovic I, Mostarica SM, Trajkovic V. Mycophenolic acid down regulates inducible nitric oxide synthase induction in astrocytes. Glia. 2002;39:247–55. doi: 10.1002/glia.10089. [DOI] [PubMed] [Google Scholar]
- 106.Yan J, Xu L, Welsh AM, Chen D, Hazel T, Johe K, et al. Combined immunosuppressive agents or CD4 antibodies prolong survival of human neural stem cell grafts and improve disease outcomes in amyotrophic lateral sclerosis transgenic mice. Stem Cells. 2006;24:1976–85. doi: 10.1634/stemcells.2005-0518. [DOI] [PubMed] [Google Scholar]
- 107.Janssen SP, Phernambucq M, Martinez-Martinez P, De Baets MH, Losen M. Immunosuppression of experimental autoimmune myasthenia gravis by mycophenolate mofetil. J Neuroimmunol. 2008;201-202:111–20. doi: 10.1016/j.jneuroim.2008.05.029. [DOI] [PubMed] [Google Scholar]
- 108.Chaudhry V, Cornblath DR, Griffin JW, O’Brien R, Drachman DB. Mycophenolate mofetil: a safe and promising immunosuppressant in neuromuscular diseases. Neurology. 2001;56:94–6. doi: 10.1212/wnl.56.1.94. [DOI] [PubMed] [Google Scholar]
- 109.Ryan ME, Greenwald RA, Golub LM. Potential of tetracyclines to modify cartilage breakdown in osteoarthritis. Curr Opin Rheumatol. 1996;8:238–47. doi: 10.1097/00002281-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 110.Golub LM, Lee HM, Ryan ME, Giannobile WV, Payne J, Sorsa T. Tetracyclines inhibit connective tissues breakdown by multiple non-antimicrobial mechanisms. Adv Dental Res. 1998;12:12–26. doi: 10.1177/08959374980120010501. [DOI] [PubMed] [Google Scholar]
- 111.Gabler WL, Creamer HR. Suppression of human neutrophil functions by tetracyclines. J Periodontal Res. 1991;26:52–8. doi: 10.1111/j.1600-0765.1991.tb01626.x. [DOI] [PubMed] [Google Scholar]
- 112.Tikka TM, Koistinaho JE. Minocycline provides neuroprotection against N-methyl-D-aspartate neurotoxicity by inhibiting microglia. J Immunol. 2001;166:7527–33. doi: 10.4049/jimmunol.166.12.7527. [DOI] [PubMed] [Google Scholar]
- 113.Tikka T, Fiebich BL, Goldsteins G, Keinanen R, Koistinaho J. Minocycline, a tetracycline derivative, is neuroprotective against excitotoxicity by inhibiting activation and proliferation of microglia. J Neurosci. 2001;21:2580–8. doi: 10.1523/JNEUROSCI.21-08-02580.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chen M, Ona VO, Li M, Ferrante RJ, Fink KB, Zhu S, et al. Minocycline inhibits caspase-1 and caspase-3 expression and delays mortality in a transgenic mouse model of Huntington disease. Nat Med. 2000;6:797–801. doi: 10.1038/77528. [DOI] [PubMed] [Google Scholar]
- 115.Du Y, Ma Z, Lin S, Dodel RC, Gao F, Bales KR, et al. Minocycline prevents nigrostriatal dopaminergic neurodegeneration in the MPTP model of Parkinson’s disease. PNAS. 2001;98:14669–74. doi: 10.1073/pnas.251341998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lampl Y, Boaz M, Gilad R, Lorberboym M, Dabby R, Rapoport A, et al. Minocycline treatment in acute stroke: an open-label, evaluator-blinded study. Neurology. 2007;69:1404–10. doi: 10.1212/01.wnl.0000277487.04281.db. [DOI] [PubMed] [Google Scholar]
- 117. www.clinicaltrials.gov, accessed on January 16, 2011.


