Abstract
We conducted a randomized comparison of Dual Focus Schema Therapy with Individual Drug Counseling as enhancements to residential treatment for 105 substance dependent patients with versus without specific personality disorders. Both therapies were manual-guided and delivered for 6 months by experienced psychotherapists intensively trained and supervised with independent fidelity assessment. Using Cox Proportional Hazards, we found no psychotherapy differences in retention (days in treatment). Hierarchical Linear Modeling indicated that personality disordered participants started with higher psychiatric, interpersonal, and dysphoria symptoms, and both therapies reduced symptoms over 6 months. Contrary to predictions, Individual Drug Counseling resulted in more sustained reductions than Dual Focus Schema Therapy in several symptoms for several personality disorders. Our findings raised important questions about the added value of integrative or dual-focus therapies for co-occurring personality disorders and substance dependence relative to empirically supported therapies focused more specifically on addiction symptoms.
Keywords: Personality disorder, substance dependence, psychotherapy, schema therapy, drug counseling
INTRODUCTION
The co-occurrence of Axis I and II disorders is very common and associated with severe psychosocial impairment (Crouse et al, 2007; Mertens et al, 2003; Oldham et al, 2009). Although most clinicians and experts believe that these complex Axis I-II patients need intensive or integrative treatments, there is very little research that supports the efficacy of integrative or dual focus models in comparison to treatments that primarily target one of the disorders (Conrad & Stewart, 2005; Kienast & Foerster, 2008). There is substantial evidence that psychotherapy and intensive psychosocial treatments are effective for personality disorders (PDs), and many patients in the over 100 Axis II treatment outcome studies had co-occurring Axis I disorders (Leichsenring & Leibing, 2003; Perry et al 1999; Sanislow & McGlashan, 1998; Verheul & Hebrink, 2007). In addition, outcomes have been evaluated for subgroups of Axis II patients in treatment for an Axis I diagnosis such as mood, (Diguer et al, 1993; Hardy et al, 1995; Shea et al, 1990), eating (Fahy et al, 1993; Johnson et al, 1990), anxiety (Brown et al, 1995; Stravynksi et al, 1982), and substance use (Cacciola et al, 1996; Messina et al, 2003; Woody et al, 1995) disorders. Furthermore, many treatment outcome studies specifically targeting Borderline PD have included patients with Axis I diagnoses, most commonly mood disorders (Bateman & Fonagy, 1999, 2008; Blum et al, 2008; Clarkin et al, 2007; Davidson et al, 2006; Giesen-Bloo et al, 2006; Hoglend, 1993; Linehan et al, 1991, 2006; Ryle & Golynkina, 1990). However, very few randomized trials have been conducted on psychotherapy models that provide an integrative or dual focus on managing and ameliorating the symptoms of both Axis I and II disorders or included a broader range of PDs.
Dialectical behavior therapy (DBT; Linehan, 1993) for Borderline PD and schema therapy (Young, 1994) for the broader range of PDs have both been adapted and evaluated for substance dependent patients in small randomized trials and shown promising results (Ball et al, 2005; Ball, 2007; Linehan et al, 1999, 2002). In addition, Gregory and colleagues have developed and tested an integrative psychodynamic model for co-occurring Borderline PD and alcohol use disorders that has shown promising acute treatment (Gregory et al, 2008) and follow-up (Gregory et al, 2010) symptom improvement. An important question is whether the increased time, cost, and complexity of training, supervision, and delivery of integrative models for dual disorders is justified based on their superior outcome over existing evidenced based therapies focused mostly on the symptoms of one of the disorders. To date, there is limited support for the use of DBT in substance dependent patients with Borderline PD in comparison to an addiction-focused comparison therapy (Linehan et al, 2002; van den Bosch et al, 2002). A very small clinical trial suggested that DBT may be better for this population than an uncontrolled therapy-as-usual for which limited symptom change seemed best explained by poor retention and utilization (Linehan et al, 1999). Similar concerns about small sample size and differential intensity of an uncontrolled treatment-as-usual can be raised about Gregory and colleagues’ promising Dynamic Deconstructive Psychotherapy model (Gregory et al, 2008, 2010). The current study compared the efficacy of Dual Focus Schema Therapy (DFST; Ball, 1998, 2003; Ball & Young, 2000), which treats a broader range of PDs and substance dependence, versus Individual Drug Counseling (IDC; Mercer & Woody, 1999), which specifically targets addiction symptoms. Both DFST and IDC were manual guided weekly individual therapies delivered during the first 6 months of a residential therapeutic community.
We have focused on PDs and substance dependence because this is the most common form of co-occurring psychiatric disorders and are especially prevalent (70-90%) in inpatient or residential programs (Verheul et al, 1998). Numerous studies have found that PDs are associated with worse substance-related outcomes when provided routine or standard addiction treatment (Verheul et al, 2005), but that the poor prognosis of Antisocial and Borderline PD may be mitigated by adding psychotherapeutic (Cacciola et al, 1996; Woody et al, 1985), psychiatric (Nace & Davis, 1993), contingency management (Messina et al, 2003), or therapeutic community interventions (McKendrick et al, 2007; Ravndal et al, 2005). For this reason, we developed and tested DFST as the first integrative cognitive behavioral therapy for the full range of PDs found in substance dependent patients (Ball, 1998; 2004). DFST showed promise in two small randomized trials when tested against individual 12 Step Facilitation Therapy in methadone maintained patients (Ball, 2007) and group drug counseling with homeless substance abusing clients (Ball et al, 2005). However, both studies raised questions about the effectiveness of DFST to manage negative affect symptoms and its suitability for all PD patients relative to a professional counseling that more narrowly targeted addiction symptoms. The larger sample and residential setting of the current study allowed for an analysis of the more common PDs (paranoid, antisocial, borderline, avoidant) and a range of psychological symptom outcomes (while controlling for the confounding influence of ongoing substance use). We hypothesized that the presence of co-occurring PD and substance dependence would contribute to worse retention (days in treatment) and symptom (psychiatric, interpersonal, affect) management within a residential therapeutic community. We predicted that DFST would have better outcomes than IDC for residents with PDs, but that IDC would be better for those without PDs.
METHODS
PARTICIPANTS
The randomized, intent-to-treat sample consisted of 105 (54 DFST, 51 IDC) residents who were predominantly single (81%), male (79%), and self-identified as European American decent (53%; 27% African American; 15% Hispanic American; 5% Bi-racial). Their average age was 26.5 (SD=10.1), years of education was 10.9 (SD=1.8), and longest period of employment was 2.9 (SD=4.0) years. All participants had been referred for residential treatment with external pressure from State of Connecticut institutions (70% direct referrals from court, jail, or detention; 19% probation; 11% child protection services). Because many were referred directly from another controlled environment, relatively few (33%) had used substances in the 30 days (mean=2.7, SD=5.7) prior to admission, and only 29% had a current substance dependence diagnosis on the Structured Clinical Interview for DSM-IV (First, 1996). Lifetime substance dependence diagnoses included: alcohol (41%); cocaine (31%); cannabis (31%); opiates (20%). The average number of prior substance abuse treatments, excluding detoxification only programs, was 2.0 (SD=2.0). The average number of previous psychiatric treatments was 1.2 (SD=2.3). Participants had significant lifetime histories of criminal convictions (Mean=7.3, SD=11.9), arrests (Mean=13.7, SD=16.2), and months incarcerated (Mean=16.1, SD=24.0) (see Table 1 for demographic and clinical indicators for the two psychotherapy conditions).
Table 1.
Participant Characteristics in the Two Therapy Conditions
| Therapy Condition | ||||
|---|---|---|---|---|
| DFST (54) | IDC (51) | |||
| Variable | Mean or % | SD or (n) | Mean or % | SD or (n) |
| Gender (%male) | 80% | (43) | 78% | (40) |
| Race** | ||||
| Caucasian | 57% | (31) | 49% | (25) |
| African-American | 15% | (8) | 39% | (20) |
| Hispanic-American | 18% | (10) | 12% | (6) |
| Biracial | 9% | (5) | 0% | (0) |
| Marital Status | ||||
| Married | 4% | (2) | 2% | (1) |
| Separated | 7% | (4) | 6% | (3) |
| Divorced | 11% | (6) | 8% | (4) |
| Single, never married | 78% | (42) | 84% | (43) |
| Age (years) | 25.60 | 9.31 | 27.53 | 11.09 |
| Education (years) | 10.81 | 1.823 | 10.98 | 1.706 |
| High School Graduate | 46% | (24) | 46% | (22) |
| Longest Employment (years) | 2.43 | 2.92 | 3.39 | 4.80 |
| Primary Lifetime Substance Diagnosis | ||||
| Alcohol (%) | 7% | (4) | 8% | (4) |
| Cocaine (%) | 30% | (16) | 26% | (13) |
| Opioid (%) | 19% | (10) | 21% | (12) |
| Cannabis (%) | 41% | (22) | 41% | (21) |
| Hallucinogen (%) | 4% | (2) | 2% | (1) |
| Lifetime Alcohol Diagnosis | 74% | (40) | 63% | (32) |
| Past Month Diagnosis on Admission | 32% | (17) | 26% | (13) |
| Past Month Days Primary Substance Used | 2.46 | 5.04 | 2.96 | 6.41 |
| Lifetime Months Primary Substance Used | 73.74 | 84.65 | 74.16 | 72.44 |
| Lifetime Number of Substances Abused | 3.30 | 2.16 | 3.00 | 1.65 |
| Substance Use Diagnosis Age of Onset | 15.43 | 3.48 | 17.38 | 6.52 |
| Lifetime Arrests | 12.41 | 11.02 | 15.16 | 20.30 |
| Lifetime Months Incarcerated | 17.28 | 25.32 | 14.78 | 22.69 |
| # of PDQ-4R (interview) PD Diagnoses | 2.67 | 2.17 | 3.02 | 2.61 |
| # of PDQ-4R (self-report) PD Symptoms | 33.61 | 12.23 | 34.41 | 11.63 |
| Paranoid PD (%) | 52% | (28) | 57% | (29) |
| Antisocial PD (%) | 50% | (27) | 49% | (25) |
| Borderline PD (%) | 22% | (12) | 37% | (19) |
| Avoidant PD (%) | 30% | (16) | 28% | (14) |
| No PD Diagnosis | 19% | (10) | 20% | (10) |
| BSI Psychiatric Severity | 1.05 | .66 | 1.04 | .76 |
| IIP Interpersonal Problems | 1.14 | .70 | 1.22 | .69 |
| MAACL Dysphoria | 9.83 | 8.29 | 8.92 | 8.34 |
| Study Therapy Sessions Attended | 13.22 | 8.11 | 13.63 | 9.02 |
| Days in Study Therapy | 100.46 | 60.68 | 96.88 | 63.25 |
| Days in Residential Treatment Program | 189.88 | 148.24 | 205.04 | 170.27 |
| Study Therapy Completers | 41% | (22) | 43% | (22) |
| Early (first month) Residential Drop-outs | 19% | (10) | 28% | (14) |
Note:
Race was the only significant difference between therapy conditions at baseline (see text). All other t-test (for means) differences or Chi Square (for frequencies) associations were non-significant.
DFST=Dual Focus Schema Therapy; IDC=Individual Drug Counseling; PDQ-4R=Personality Diagnostic Questionnaire-4th edition, revised; PD=personality disorder; BSI-Brief Symptom Inventory; IIP=Inventory of Interpersonal Problems; MAACL=Multiple Affect Adjective Checklist
ASSESSMENTS
Personality Diagnostic Questionnaire-version 4 revised
The PDQ-4R (Hyler, 1994) is a structured assessment for DSM-IV PDs that incorporates a self-report instrument with an interview follow-up. The self-report consists of 106 true/false items corresponding to each diagnostic criterion for each PD. When there were a sufficient number of symptoms endorsed for a diagnosis, the research interviewer queried to determine whether each group of items had the necessary persistence, maladaptivity, and independence from Axis I disorders to constitute a PD diagnosis. Assessments were completed by bachelor's level research assistants who were systematically trained and supervisor by the second author, although formal reliability testing was not conducted. Most (81%) of the sample met PDQ-4R interview criteria for at least one disorder with the following rates: Paranoid 54%, Schizoid 21%, Schizotypal 25%, Antisocial 50%, Borderline 30%, Histrionic 11%, Narcissistic 18%, Avoidant 29%, Dependent 10%, Obsessive-Compulsive 37%. The reliability and validity of the PDQ-4 has been summarized by Bagby and Farvolden (2004) and evaluated in the substance abuse samples (Verheul et al, 1998). Of the more common PDs, we chose not to analyze Obsessive-Compulsive because our prior research (Ball et al, 2005) had found that the PDQ-4R over-diagnosed this in substance abusers.
Brief Symptom Inventory
The BSI (Derogatis, 1992) is a 53-item self-report inventory of psychiatric symptoms that asks participants to rate items on a 0-4 point scale of distress. It yields three general severity measures and nine primary symptom dimensions; we limited our analyses to the BSI Global Severity Index.
Multiple Affect Adjective Checklist-Revised
The MAACL-R (Zuckerman & Lubin, 1985) is a 132 adjective checklist providing state and trait affect measures; we limited our analyses to Dysphoria, a composite state affect indicator which combines anxiety, depression, and hostility subscales.
Inventory of Interpersonal Problems-Circumplex
The IIP (Alden et al, 1990) is a 64-item self-report measure of interpersonal problems in the past 30 days on a 0-4 point scale of distress; we analyzed the overall problem index which averages the eight interpersonal subscales.
Adherence/Competence Rating Scale
This 40-item measure was adapted from one used in our two prior trials comparing DFST with an addiction-focused therapy and used the format developed in the Yale Adherence Competence Scale (Carroll et al, 2000).Ten items assessed General Therapist Skills and session characteristics, 10 assessed DFST specific techniques, 10 assessed IDC specific techniques, and 10 assessed Other Therapy techniques not considered part of either approach. See Table 2 for an abbreviated listing of items for each scale. Each therapy technique was rated on two dimensions: 1) adherence (frequency and extensiveness with which technique was done); 2) competence (quality or skill with which technique was done).
Table 2.
Adherence and Competence Rating Differences for Two Therapy Conditions
| Therapy Conditions | ||||||
|---|---|---|---|---|---|---|
| DFST | IDC | t (341)= | p< | |||
| Mean | SD | Mean | SD | |||
| General Skillfulness | 5.79 | .46 | 5.25 | .50 | 10.34 | .001 |
| General Effectiveness and Skill | 5.73 | .58 | 4.95 | .63 | 11.72 | .001 |
| Maintaining Session Structure | 5.67 | .60 | 4.81 | .70 | 11.84 | .001 |
| Collaboration | 5.52 | .64 | 4.87 | .71 | 8.84 | .001 |
| Empathy | 5.52 | .67 | 4.98 | .64 | 7.51 | .001 |
| Spontaneity and Openness | 5.53 | .68 | 4.96 | .67 | 7.66 | .001 |
| Non-interference by Therapist Issues1 | 6.76 | .37 | 6.50 | .62 | 4.44 | .001 |
| Clarifying Misunderstandings1 | 6.41 | .61 | 6.28 | .82 | 1.51 | .132 |
| Alliance | 5.18 | .68 | 4.66 | .71 | 6.82 | .001 |
|
DFST Techniques A
C |
2.91 | .68 | 1.65 | .41 | 21.26 | .001 |
| 5.27 | .53 | 4.65 | .49 | 11.05 | .001 | |
| Schema Identification and Education | 3.46 | 1.95 | 1.09 | .33 | 17.04 | .001 |
| Functional Analysis of Current Problems | 3.39 | 1.65 | 1.82 | 1.13 | 10.43 | .001 |
| Linking Schema-Driven Situations | 3.02 | 1.81 | 1.23 | .63 | 13.03 | .001 |
| Empathic Confrontation and Validation | 2.15 | 1.07 | 1.79 | .95 | 3.28 | .001 |
| Maladaptive Schema Coping | 2.18 | 1.68 | 1.04 | .21 | 9.62 | .001 |
| Behavioral Pattern Breaking | 3.08 | 1.65 | 2.20 | 1.24 | 5.67 | .001 |
| Cognitive Techniques | 2.91 | 1.40 | 1.68 | .86 | 10.05 | .001 |
| Use of Therapeutic Relationship | 3.67 | 1.32 | 2.66 | 1.17 | 7.18 | .001 |
| Early Origins and Past Problems | 3.43 | 2.03 | 1.88 | 1.27 | 8.73 | .001 |
| Experiential or Emotive Techniques | 1.84 | 1.64 | 1.15 | .43 | 5.73 | .001 |
|
IDC Techniques A
C |
1.52 | .34 | 2.16 | .53 | -12.55 | .001 |
| 4.88 | .57 | 4.83 | .51 | .80 | .423 | |
| Maintains an Addiction Focus | 2.95 | 1.54 | 3.93 | 1.52 | -5.83 | .001 |
| Psychoeducation About Substance Abuse | 1.19 | .60 | 1.64 | 1.18 | -4.12 | .001 |
| Disease Concept of Addiction | 1.14 | .42 | 1.86 | 1.28 | -6.38 | .001 |
| Exploration or Confrontation of Denial | 1.18 | .53 | 1.58 | 1.12 | -3.92 | .001 |
| Reality Therapy Concepts | 1.73 | .97 | 2.11 | 1.08 | -3.40 | .001 |
| Healthy Lifestyle and Risk Reduction | 1.23 | .60 | 2.06 | 1.57 | -5.91 | .001 |
| Addressing Other Compulsive Behaviors | 1.13 | .50 | 1.54 | 1.12 | -3.97 | .001 |
| Self-Help Group Involvement | 1.22 | .66 | 2.78 | 1.83 | -9.62 | .001 |
| Codependent and Enabling Relationships | 1.22 | .54 | 1.28 | .85 | -.76 | .446 |
| Recovery-oriented Needs and Feelings | 2.21 | 1.08 | 2.88 | 1.65 | -4.22 | .001 |
|
Other Therapeutic Techniques A
C |
3.04 | .46 | 3.07 | .50 | -.56 | .579 |
| 5.20 | .45 | 4.80 | .46 | 8.03 | .001 | |
| Treatment Agenda, Goals, and Rationale | 4.57 | .97 | 4.00 | 1.07 | 5.16 | .001 |
| Motivational Interviewing Techniques | 6.06 | .71 | 5.62 | 1.10 | 4.14 | .001 |
| Problem Discussion and Feedback | 4.82 | 1.4 | 4.04 | 1.47 | 5.00 | .001 |
| Addressing Psychopathology | 1.32 | .79 | 1.36 | .96 | -.33 | .741 |
| Pros and Cons of Change | 1.61 | 1.01 | 1.36 | .75 | 2.56 | .016 |
| Authoritative Advice or Direction Giving | 2.02 | 1.24 | 2.67 | 1.55 | -4.10 | .001 |
| Relapse Prevention Skills | 1.61 | 1.03 | 2.92 | 1.74 | -8.73 | .001 |
| Involvement in Other Program Activities | 3.79 | 1.55 | 4.08 | 1.45 | -1.74 | .082 |
| Social Functioning and Support | 3.50 | 1.45 | 3.58 | 1.57 | -.53 | .598 |
| Psychodynamic Interventions | 1.08 | .31 | 1.05 | .23 | .84 | .399 |
Note: A=Adherence or the “frequency and extensiveness” with which a therapist performed techniques of particular approach. C=Competence or “skillfulness” with which therapist performed techniques of approach. Means (SDs) for each of the scale items refer to Adherence only. DFST=Dual Focus Schema Therapy. IDC=Individual Drug Counseling.
These items were reverse score with high scores indicating absence of this behavior.
PROCEDURES
Enrollment and Assessment
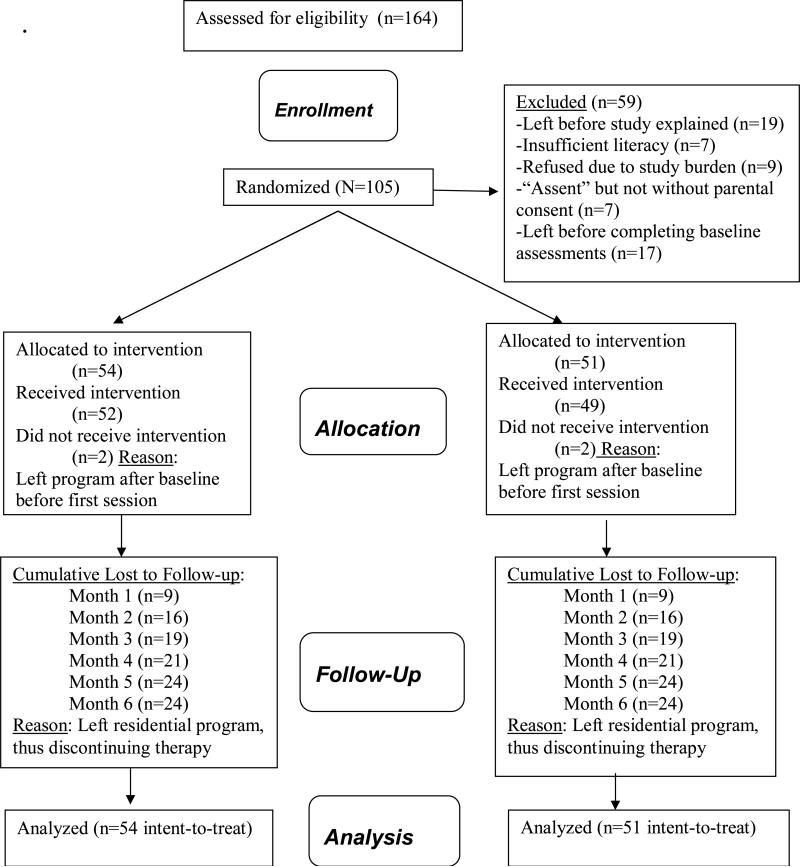
Participation in this study was voluntary and did not affect entrance or termination from the residential program. In addition to the exclusion criteria used by the residential program (current psychosis, suicidality, severe medical condition, need for detoxification), residents were excluded whose reading level was below 6th grade on the Slosson Oral Reading Test (Slosson & Nicholson, 1990) and Yale's Institutional Review Board would not allow enrollment of Department of Correction transfers because of their vulnerable legal status as “prisoners.” Over 1/3 of the 351 residential program admissions during the study recruitment period (August 2002 - September 2004) were ineligible for screening due to this prisoner exclusion. Of the remaining, 164 completed a research interest form indicating their permission to be approached by study staff for eligibility determination and informed consent. The Consort Diagram details the flow of subjects into the study and the rates of follow-up assessments.
Once enrolled, the 105 intent-to-treat participants completed baseline self-reports and interviews with a research assistant (who remained blind to the therapy conditions), were randomized by the project director, and scheduled for their first therapy appointment. Random assignment used a computerized urn allocation procedure that balanced groups with regard to gender and referral source. Participants met monthly with the research assistant to complete process and outcome measures during their 6 month therapy participation. The increasingly poor rates of follow-up (almost 50% left residential treatment before termination assessment) reflected the fact that when most participants left residential treatment prematurely, this triggered an arrest warrant which contributed to their unwillingness be located by research staff despite their earlier consent to be contacted through significant others. Participants received a $50 store gift card for completing the baseline, $10 for each of month 1-5, and $60 for month 6 assessments.
Treatments
All participants received either manual-guided individual DFST or IDC for 6 months as an enhancement to standard residential therapeutic community treatment which did not provide other individual psychotherapy.
Dual Focus Schema Therapy
(Ball, 1998, 2004; Ball & Young, 2000) integrated cognitive behavioral coping skills for substance use (Carroll, 1998) with targeted interventions for early maladaptive schemas (i.e., enduring negative themes about oneself, others, and events), affective reactions, relational problems, and maladaptive behavioral coping styles (Young et al, 2004). An important and distinct assumption of DFST, relative to other CBT models for PD (Beck et al, 1990; Linehan, 1993), was that a single integrative therapy can be used for diverse patients rather than separate approaches for each Axis II category. In the first 2 months of therapy, addiction coping skills were integrated with identification and education about personality, schemas, relationships, and coping. The remaining 4 months focused on cognitive, experiential, behavioral, and relational change strategies (Young et al, 2004) using events within the residential program as opportunities for practicing skills learned in each session.
Individual Drug Counseling
(Mercer & Woody, 1999) was specifically focused on addiction as a primary disease, and it addressed symptoms by providing exposure to various recovery topics and tools, especially admitting addiction, developing drug-free social supports, committing to abstinence, reviewing self-help philosophy, and encouraging meeting attendance. IDC was developed and found to be effective for outpatient cocaine abusers (Crits-Christoph et al, 1998), and can be adapted for other drug addicted clients and settings (Mercer & Woody, 1999). IDC did not target personality or other psychiatric disorders and had very little overlap with DFST. As an active therapy condition focused on one disorder, IDC controlled for general therapist factors such as time and attention. We also conceptualized it as a quantitative enhancement to the residential program because it provided content in individual sessions that was also being covered in standard groups.
Residential Therapeutic Community
treatment was provided to participants in both DFST and IDC through the Yale-affiliated APT Foundation Residential Services Division located in Bridgeport, CT. This intensive modality was chosen because professionally delivered weekly individual psychotherapy is not a part of standard care and because it is believed to be an appropriate modality for patients with severe addiction and PDs, especially Antisocial (Hesse & Pedersen, 2007; McKendrick et al, 2007). This program provided most of the core elements that define a modified therapeutic community (DeLeon, 1997) including highly organized staff-guided daily groups (therapeutic, behavior management) and activities (occupational, educational) designed to challenge and change attitudes, perceptions, and behaviors associated with substance dependence. There are strict, explicit, behavioral norms with contingencies to promote self-control, honesty, responsibility, and other pro-social behaviors necessary for the treatment milieu to promote recovery. Because of funding and contractual reporting, this program considered 6 months of treatment to be the minimum amount of time for completion which corresponded to the duration of study therapies provided. All participants were encouraged to continue in a second residential aftercare phase of treatment which could be an additional 6-18 months.
Therapist Training, Supervision, and Fidelity
Therapists were 10 (6 DFST, 4 IDC) masters- or doctoral-level clinicians with at least five years clinical experience with substance abuse and co-occurring patients. DFST therapists were trained by the developer of schema therapy (Jeffrey Young, Ph.D.) and the first author for DFST, and the last author provided training in IDC. Based on implementation and monitoring procedures developed in our prior clinical trials, training for both conditions involved didactic presentations, detailed review of treatment manual and training videotapes, and technical demonstrations and role plays. Therapists were assigned pilot cases (n=15), and each treated one participant for 24 weeks while videotapes were reviewed by the first author and respective supervisor for DFST (D.L.) or IDC (M.O.) to determine readiness based on the Adherence/Competence scale. During the training and randomized phases, weekly supervision for both conditions incorporated review of therapist's adherence self-checklists, session discussion, written participant assignments, and Adherence/Competence ratings of videotapes to facilitate feedback and coaching. Each therapist treated 6-15 randomized cases.
Following completion of the study, 14 substance abuse clinicians from two treatment programs in the area served as independent (i.e., blind to study conditions and aims) raters of Adherence and Competence. They attended an all-day training (by S.B. and L.M.) in the use of the rating scale which involved discussion of each rating item and joint rating of pilot case videotapes. All rated the same 10 tapes for practice and reliability calibration purposes, and a recalibration tape mid-way through the 3-month rating period to detect and correct any rater drift. Then, tapes were selected so that: 1) each participant had at least one session rated; 2) each session (weeks 1-24) for each condition had at least one session rated with a comparable number for each of the six month intervals; 3) comparable numbers of tapes were rated for each therapist; 4) each session was rated by two (47% of selected tapes) or three (53%) raters. This resulted in 343 separate sessions being jointly rated. Because there were two more DFST than IDC therapists, there were more DFST (205) than IDC (138) sessions ratings.
We analyzed the averaged Adherence and Competence item ratings across participants, therapists, sessions, and raters to test the discriminability and fidelity of IDC and DFST. As expected, Table 2 shows that DFST therapists had higher Adherence and Competence in the delivery of “DFST techniques” than did IDC therapists. Each of the ten DFST items was rated as occurring more frequently for DFST than IDC. IDC therapists scored higher than DFST therapists on Adherence but not Competence of delivering “IDC techniques.” Although there was no average Adherence difference in the delivery of “Other Therapeutic Techniques,” three items were delivered more frequently by DFST and two by IDC therapists. Overall, there was a higher level of Competence among DFST than IDC therapists for these Other techniques. In addition, all of the General Skillfulness item ratings were higher in DFST than IDC, indicating that independent clinicians judged DFST therapists as being more competent and skillful in their overall delivery of psychotherapy. These results make the outcome findings below surprising.
DATA ANALYSIS
Four PDs (Paranoid, Antisocial, Borderline, Avoidant) were tested based on literature reviews (Verheul et al, 1998, 2005) indicating that they are the most common PDs in substance dependence. These four PDs and the two treatment conditions were tested as main effects and as interactions to predict two groups of outcomes: 1) retention (days in 6-month therapy); 2) problem/symptom change (BSI psychiatric severity, IIP interpersonal problems, MAACL dysphoria). Retention was tested using survival analysis (Cox Proportional Hazards) with 6 months to define the censoring point to reflect the maximum duration of therapy and the minimum period of time to define positive residential outcome. Problem/symptom changes were tested using hierarchical linear modeling (to account for missing data) with SPSS version 16 (PROC MIXED) testing main and interaction effects for each PD and Therapy as well as their interaction with Time (baseline plus six monthly measures). All analyses involved the intent-to-treat sample. We chose to analyze the PDs separately; Chi squares found evidence of significant overlap (with the exceptions of Antisocial and Avoidant), but not redundancy among the PDs.
RESULTS
The therapy conditions were equivalent on all baseline measures (demographics, personality disorder, substance abuse, retention, symptoms) except ethnicity (see Table 1). African Americans were more commonly assigned to IDC than DFST with no significant differences for the other ethnic groups, X2(df=3; n=105) =11.71, p<.008. We analyzed Black vs. non-Black participants (excluding biracial) and found no differences between these groups on treatment retention, baseline symptoms, or prevalence of the four PDs. For this reason and because cell sizes would have precluded subgroup analyses, no further analyses were done.
SIX-MONTH RETENTION IN THERAPY
There were no differences between therapy conditions for the retention measure using Cox Proportional Hazards analysis. Participants averaged a total of 95.0 (SD=63.3) days in the study therapy and completed 13.4 (SD=8.5) individual sessions. The average total number of days in residential treatment was 207.9 (SD=161.8) for participants with no differences based on therapy assignment. Rates of discharge for different residential retention milestones were equivalent for the two therapies: less than 1 month (DFST=11% vs. IDC=12%); 1-3 months (20% vs. 26%); 3-6 months (20% vs. 18%); 6-12 months (30% vs. 26%); greater than 12 months (19% vs. 20%). Therapy completion (defined as completing 5 months or 20 sessions of psychotherapy) was achieved by 42% of the sample with no differences between conditions. Cox Regression analyses indicated no retention main effects for Paranoid, Antisocial, Borderline, or Avoidant and no PD X Therapy interactions. Chi square analysis of missing assessments by therapy condition for each of the six time points indicated no differences. Thus, no adjustments for differential attrition between conditions were needed for the symptom change analyses.
THERAPY AND TIME EFFECTS FOR SYMPTOMS
There were significant main effects for Time for BSI psychiatric symptom severity, F(1,417)=47.37,p<.001, IIP interpersonal problems, F(1,424)=34.79,p<.001, and MAACL dysphoria, F(1,417)=23.07, p<.001. Participants in both conditions reported decreased symptoms over the 6-month therapy period.
Although there were no main effects for Therapy condition, there was a significant Therapy X Time interaction for BSI severity, F(1,417)=4.78,p<.02. Although participants assigned to both therapy conditions showed significant and comparable reductions in psychiatric symptoms over the first three months of therapy, those assigned to DFST showed no further symptom reductions whereas those assigned to IDC had continued reduction over the last three months of therapy. Table 3 lists the observed and estimated means for each of the two therapy conditions for each of the three symptom outcomes for each of the seven assessment points.
Table 3.
Observed and HLM Estimated Means (SDs) for Two Therapy Conditions for Three Outcomes Over Six-Month Study Period
| Study | Observed Means | Estimated Means | ||||||
|---|---|---|---|---|---|---|---|---|
| Month | Therapy Conditions | Therapy Conditions | ||||||
| DFST | IDC | DFST | IDC | |||||
| BSI | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| 0 | 1.05 | .66 | 1.04 | .76 | 1.05 | .09 | 1.04 | .10 |
| 1 | .93 | .76 | .93 | .73 | .95 | .10 | .93 | .10 |
| 2 | .72 | .65 | .83 | .62 | .85 | .10 | .85 | .10 |
| 3 | .83 | .69 | .75 | .71 | .99 | .10 | .78 | .11 |
| 4 | .69 | .73 | .51 | .43 | .86 | .10 | .68 | .11 |
| 5 | .67 | .65 | .41 | .35 | .80 | .11 | .58 | .11 |
| 6 | .66 | .74 | .46 | .34 | .78 | .11 | .61 | .11 |
| IIP | ||||||||
| 0 | 1.14 | .70 | 1.22 | .69 | 1.14 | .09 | 1.22 | .09 |
| 1 | 1.15 | .68 | 1.05 | .59 | 1.16 | .10 | 1.09 | .10 |
| 2 | 1.03 | .66 | 1.08 | .69 | 1.15 | .10 | 1.10 | .10 |
| 3 | 1.05 | .72 | 1.05 | .72 | 1.20 | .10 | 1.09 | .11 |
| 4 | .94 | .59 | .85 | .59 | 1.07 | .10 | .95 | .11 |
| 5 | .88 | .71 | .70 | .53 | .97 | .11 | .80 | .11 |
| 6 | .78 | .61 | .75 | .50 | .87 | .11 | .80 | .12 |
| MAACL | ||||||||
| 0 | 9.83 | 8.29 | 8.92 | 8.34 | 9.70 | 1.06 | 8.89 | 1.09 |
| 1 | 8.71 | 8.88 | 6.45 | 6.04 | 9.34 | 1.11 | 6.77 | 1.15 |
| 2 | 6.66 | 7.73 | 5.19 | 6.37 | 7.57 | 1.16 | 6.19 | 1.19 |
| 3 | 7.00 | 7.28 | 6.75 | 8.58 | 8.13 | 1.19 | 7.72 | 1.24 |
| 4 | 6.91 | 8.94 | 3.50 | 3.80 | 7.98 | 1.21 | 5.96 | 1.31 |
| 5 | 4.87 | 7.18 | 2.58 | 3.26 | 5.79 | 1.23 | 5.04 | 1.31 |
| 6 | 6.00 | 7.34 | 2.75 | 4.30 | 6.92 | 1.24 | 5.24 | 1.34 |
NOTE: HLM=Hierarchical Linear Modeling; BSI=Brief Symptom Inventory; IIP=Inventory of Interpersonal Problems; MAACL = Multiple Affect Adjective Checklist; DFST=Dual Focus Schema Therapy; IDC=Individual Drug Counseling. Sample sizes for each month: 0 (105); 1 (87); 2 (75); 3 (67); 4 (59); 5 (56); 6 (54)
PDs AND SYMPTOM CHANGE
Paranoid PD
There were significant main effects for Paranoid PD for BSI symptoms, F(1,150)=29.91, p<.001, IIP problems, F(1,166)=12.95,p<.001, and MAACL dysphoria, F(1,152)=6.47,p<.012, indicating that participants with Paranoid PD were more symptomatic than those not diagnosed over the 6-month study period. However, significant two-way PD X Time interactions for BSI, F(1,420)=7.88,p<.002, IIP, F(1,420)=7.88,p<.002, and MAACL, F(1,417)=16.95, p<.001, indicated that the difference between Paranoid diagnosed and non-diagnosed participants was significantly larger at the start than at the end of therapy. Paranoid participants showed significant reductions in all three symptoms in comparison to the minimal change and lower severity of non-Paranoid participants over the 6 months.
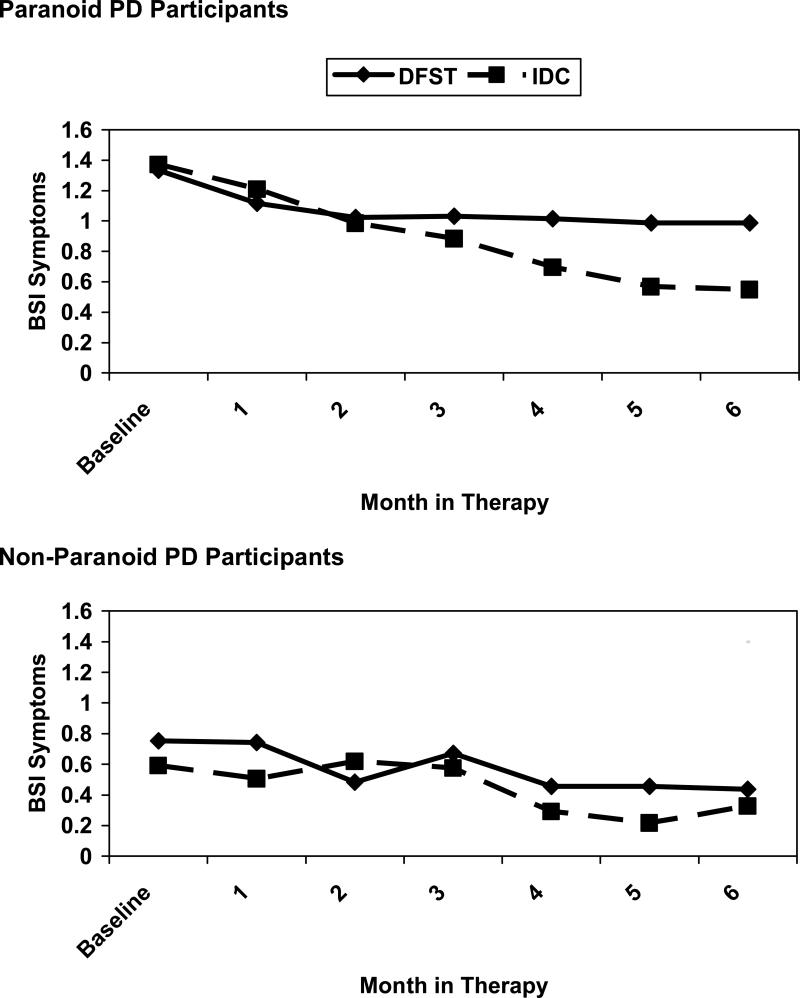
Although there were no 2-way interactions with Therapy condition, there was a significant PD X Therapy X Time interaction for BSI symptoms, F(1,420)=6.96,p<.009 (see Figure 1). Paranoid PD participants had significant symptom reductions over the first 2 months in both therapies. However, IDC showed continued reductions for those with Paranoid PD over the remaining 4 months whereas DFST showed no further improvement. Participants without Paranoid PD showed no differential treatment effect on their lower level symptoms.
Figure 1.
Personality Disorder (PD) X Therapy (DFST vs. IDC) X Time (Month in Therapy) interaction for BSI severity showing observed mean changes for Paranoid (top panel) and non-Paranoid (bottom panel) PD participants as a function of therapy condition
Antisocial PD
Similar to above, there were significant main effects for Antisocial PD for BSI symptoms, F(1,145)=7.51,p<.007, IIP problems, F(1,168)=7.32,p<.008, and MAACL dysphoria, F(1,161)=11.26,p<.001, indicating that Antisocial participants were more symptomatic than those not diagnosed over the 6-month study period. A significant two-way PD X Time interaction for MAACL dysphoria, F(1,417)=16.95,p<.001, indicated that the difference between diagnosed and non-diagnosed participants was significantly larger at the start than at the end of therapy. The PD X Therapy interaction for the MAACL, F(1,161)=4.64,p<.033, indicated that Antisocial participants reported less dysphoria when they received IDC than when they received DFST with no therapy condition differences between the non-diagnosed.
Borderline PD
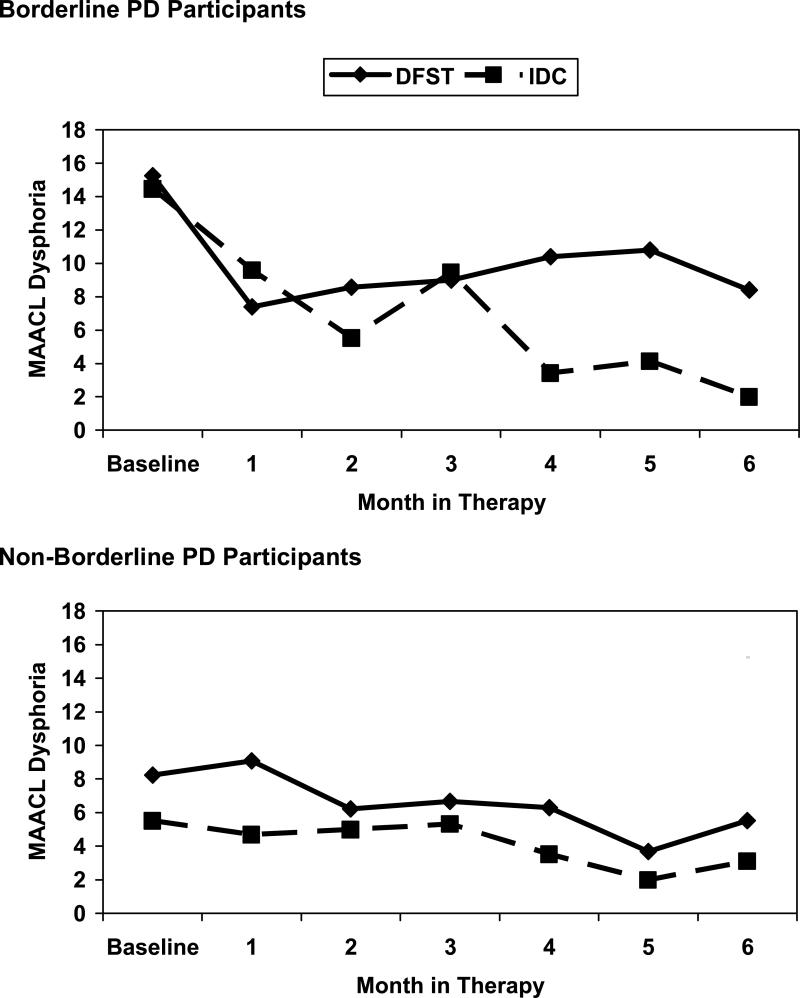
As above, there were significant main effects for Borderline PD for BSI symptoms, F(1,158)=35.28,p<.001, IIP problems, F(1,179)=23.12,p<.001, and MAACL dysphoria, F(1,163)=12.78,p<.001, indicating that Borderline participants were more symptomatic on average than those without Borderline over the 6-month study period. However, significant PD X Time interactions for BSI, F(1,429)=9.09,p<.003, and IIP, F(1,438)=7.16,p<.008, indicated that the difference between diagnosed and non-diagnosed participants was significantly larger at the start than at the end of therapy. Although there was no PD X Time interaction for MAACL, the three-way interaction with Therapy condition was significant, F(1,428)=7.01, p<.008 (see Figure 2). Although participants diagnosed with Borderline showed significant symptom reductions over the first 3 months in both therapy conditions, IDC had continued reductions over the remaining 3 months whereas DFST showed no further improvement. Non-borderline participants showed no differential treatment effect on their lower level symptoms.
Figure 2.
Personality Disorder (PD) X Therapy (DFST vs. IDC) X Time (Month in Therapy) interaction for MAACL dysphoria showing observed mean changes for Borderline (top panel) and non-Borderline (bottom panel) PD participants as a function of therapy condition
Avoidant PD
Consistent with the other three PDs, there were significant main effects for Avoidant for BSI symptoms, F(1,153)=47.93,p<.001, IIP problems, F(1,170)=14.26,p<.001, and MAACL dysphoria, F(1,156)=12.46,p<.001, indicating that diagnosed participants were more symptomatic than those without diagnoses over the 6-month study period. Also similarly, significant two-way interactions between PD and Time for BSI, F(1,423)=21.20, p<.001, MAACL, F(1,420)=4.58, p<.033, and a non-significant trend for IIP (p=.074) indicated that differences between Avoidant diagnosed and non-diagnosed participants were significantly larger at the start than at the end of therapy. There were no PD X Therapy interactions and two non-significant trends for PD X Therapy X Time interaction for IIP problems (p=.09) and MAACL dysphoria (p=.08) were similar in direction to those illustrated in Figures 1 and 2 (i.e., IDC showing better symptom reduction than DFST in the latter half of therapy for Avoidant PD).
DISCUSSION
Contrary to our hypotheses, we did not find that a therapy developed to provide a dual focus on a range of PDs and substance dependence retained or reduced symptoms better for this group of participants or that a therapy focused mostly on addiction was better for those without those PDs. Quite the opposite, we found that IDC provided more sustained reduction of psychiatric symptoms or dysphoric affect than did DFST for three of the four PDs evaluated. The superiority of IDC could not be attributed to differences in therapist skill between the conditions. In fact, PD participants receiving DFST improved less despite independent fidelity ratings that they were being treated by more competent psychotherapists.
Although our prior trial of DFST with methadone maintained PD patients (Ball, 2007) had promising substance use outcomes, it was less effective in reducing dysphoria than a 12-step facilitation therapy that has overlap with IDC. Our trial with homeless substance using PD clients (Ball et al, 2005) suggested that DFST was less effectively utilized by some clients with more severe PDs than group counseling using IDC topics. These two trials and our current findings suggest that PD patients with significant paranoia, affect instability, impulsivity, rigidity, and avoidance may find addiction-focused discussions more stabilizing than an insight- and change-oriented focus on their maladaptive schemas and coping styles. An alternative explanation is that the addiction-focused topics discussed in IDC were more similar to what patients had been exposed in prior treatments, the standard care in their current program, or self-help meetings. The greater familiarity of the IDC material may allow better consolidation of therapeutic content and skills. In contrast, the newness (and possibly anxiety provoking nature) of the schema material may interfere with the cognitive-affective integration necessary for symptom improvement.
This study had several limitations. First, the substance-free status of most participants on admission and the controlled residential environment made substance use an irrelevant outcome variable. This is important to note because this was the one outcome that DFST outperformed the standard addiction counseling approach in the first clinical trial involving methadone maintained patients (Ball, 2007). In addition, the three outcomes assessed in the current study were all self-report measures of personality-related symptoms or problems and did not involve more objective, expert, or observational behavior ratings. Finally, it should be noted that neither IDC nor DFST were particularly effective as once weekly individual psychotherapies in preventing the very high drop out that is seen in a challenging 24 hour/7 day residential addiction treatment environment.
Related to this issue, the most significant limitations related to treatment exposure, duration, and focus. Our low rates of successful treatment completion and research assessment follow-ups are common problems in PD clinical trials (Blum et al, 2008; Verheul et al, 2003). For reasons related to what happened (i.e., relapse, re-arrest) when most patients dropped out of residential treatment, significant symptom improvement can only be assumed for participants who completed most of their assigned therapy. On a related note, 6 months of weekly therapy is probably insufficient to result in sustained changes in maladaptive personality or psychological indicators. We chose this duration because: 1) 6-months is the minimum necessary for substance use and psychosocial improvements in long-term residential programs (Hubbard et al, 1997); 2) a meta-analysis of PD treatments (Perry et al, 1999) found a median of 28 weeks of intensive treatment was associated with significant symptom improvement; 3) both DFST and IDC manuals were designed as 6-month interventions. Given the above noted differences in familiarity with therapy content, acute psychiatric symptom reduction may be more achievable in 6 months of IDC than DFST. A clinical trial that found schema therapy more effective than transference focused therapy for Borderline PD (Geisen-Bloo et al, 2006) involved 2-year duration therapies, and the treatments for Borderline PD with the most empirical support (Bateman & Fonagy, 1999, 2008; Linehan et al, 1991, 2006) have durations exceeding one year, an intensive outpatient focus, and integrate different orientations or modalities. Finally with regard to therapeutic focus, the developers of schema therapy (Young et al, 2003) have argued that the original model may not be effective for Borderline and other PDs characterized by very high avoidance or rigidity, which may describe our sample of patients. A revised schema-based approach called mode therapy has been proposed and was found to be effective in a clinical trial with Borderline PD (Geisen-Bloo et al, 2006).
Clinicians and experts believe there is a the need for highly specialized, integrative, or dual focus therapies for substance abuse and PDs despite very limited empirical evidence (Conrod & Stewart, 2005; Ekleberry, 2009; Kienas & Foerster, 2008; van den Bosch & Verheul, 2007). Our findings do little to support such beliefs, at least for the severely compromised substance users we have tested in three service settings. The majority of evidence supporting the use of integrative or dual focus cognitive behavioral treatment models (Conrod & Stewart, 2005) has come either from studies involving no comparison group or an uncontrolled treatment-as-usual typically of unknown quality and variable quantity. The delivery of an evidence-based therapy by an experienced psychotherapist who specifically targets substance dependence may provide acute symptom management over which a dual focus model cannot improve significantly. Further research on both addiction-focused and dual-focused therapies is needed to improve outcomes for this challenging population and to determine if the increased time and cost for training and implementing a complex, integrative therapy model for Axis I-II patients is justified. In addition to the numerous treatment models tested for Borderline PD (Bateman & Fonagy, 1999, 2008; Blum et al, 2008; Clarkin et al, 2007; Davidson et al, 2006; Giesen-Bloo et al, 2006; Gregory et al, 2008; Hoglend, 1993; Linehan et al, 1991, 2006; Ryle & Golynkina, 1990), several randomized trials have suggested that once or twice weekly outpatient psychodynamic or cognitive behavioral models may be effective for the broader group of PDs (Arnevik et al, 2010; Leichsenring & Leibing, 2003; Svartberg et al, 2004; Verheul & Herbrink, 2007). It remains an empirical question whether these models can be adapted more effectively than schema therapy for use with substance dependent patients.
CONCLUSIONS
PD participants started with higher psychiatric, interpersonal, and dysphoria symptoms, and both therapies reduced symptoms over 6 months of residential treatment for substance dependence. IDC resulted in more sustained reductions than DFST in psychiatric and affective symptoms for Paranoid, Antisocial, Borderlines PD, but not for non-PD participants. We question the added value of dual-focus therapies for the a range of co-occurring personality disorders and substance dependence relative to empirically supported therapies more narrowly targeting addiction symptoms.
Figure 3.
Consort Diagram for study enrollment, randomization, and follow-up rates.
ACKNOWLEDGMENTS
Ever Linares, Michelle Altomare, Melanie McAlpine, Melissa Williams, and Lori Bellino served as research staff for this study. We gratefully acknowledge the support of all APT Foundation staff at the Residential Services Division and especially the contributions of Shelley Krysta, Brenda Davie, Nancy Legow, Wendy Levy, Douglas Gruber, Natalie DuMont, Nancy Moak, David Polio, Maria Sullivan, Gretchen Celestino, and the late Vincent Nuzzo. Several clinical staff from nearby treatment programs served as independent tape raters and we thank them and Linda Mosel from Connecticut Renaissance and Carey Ostrow from Liberation Programs for coordinating their involvement. This research occurred with the permission or institution review board approval from Yale University and State of Connecticut agencies that fund The APT Foundation, including the Court Support Services Division, Department of Mental Health and Addiction Services, and Department of Children and Families. This project was funded by a grant from the National Institute on Drug Abuse (R01DA14967) awarded to the first author. Portions of this study were presented previously at the annual conventions of the International Society for the Study of Personality Disorders in The Hague, Netherlands (November 2007) and the College on Problems of Drug Dependence in San Juan, Puerto Rico (June 2008).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Alden LE, Wiggins JS, Pincus AL. Construction of circumplex scales for the Inventory of Interpersonal Problems. J Pers Assess. 1990;55:521–536. doi: 10.1080/00223891.1990.9674088. [DOI] [PubMed] [Google Scholar]
- Arnevik E, Wilberg T, Urnes O, Johansen M, Monsen JT, Karterud S. Psychotherapy for personality disorders: 18 months’ follow-up of the Ulleval Personality Project. J Pers Disord. 2010;24:188–203. doi: 10.1521/pedi.2010.24.2.188. [DOI] [PubMed] [Google Scholar]
- Bagby RM, Farvolden P. The Personality Diagnostic Questionnaire-4 (PDQ-4). In: Hersen M, editor. Comprehensive handbook of psychological assessment: Personality assessment. John Wiley & Sons, Inc.; Hoboken, NJ: 2004. pp. 122–131. [Google Scholar]
- Ball SA. Manualized treatment for substance abusers with personality disorders: Dual focus schema therapy. Addict Behav. 1998;23:883–891. doi: 10.1016/s0306-4603(98)00067-7. [DOI] [PubMed] [Google Scholar]
- Ball SA. Treatment of personality disorders with co-occurring substance dependence: Dual focus schema therapy. In: Magnavita JJ, editor. Handbook of personality disorders: theory and practice. John Wiley & Sons, Inc.; New York: 2004. pp. 398–425. [Google Scholar]
- Ball SA. Comparing individual therapies for personality disordered opioid dependent patients. J Pers Disord. 2007;21:305–321. doi: 10.1521/pedi.2007.21.3.305. [DOI] [PubMed] [Google Scholar]
- Ball SA, Cobb-Richardson P, Connolly AJ, Bujosa CT, O'Neall TW. Substance abuse and personality disorders in homeless drop-in center clients: symptom severity and psychotherapy retention in a randomized clinical trial. Compr Psychiatry. 2005;46:371–379. doi: 10.1016/j.comppsych.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Ball SA, Young JE. Dual Focus Schema Therapy for personality disorders and substance dependence: case study results. Cogn Behav Pract. 2000;7:270–281. [Google Scholar]
- Bateman A, Fonagy P. Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. Am J Psychiatry. 1999;156:1563–1569. doi: 10.1176/ajp.156.10.1563. [DOI] [PubMed] [Google Scholar]
- Bateman A, Fonagy P. 8-year follow-up of patients treated for borderline personality disorder: Mentalization-based treatment versus treatment as usual. Am J Psychiatry. 2008;165:634–638. doi: 10.1176/appi.ajp.2007.07040636. [DOI] [PubMed] [Google Scholar]
- Beck AT, Freeman A, editors. Cognitive therapy of personality disorders. Guilford Press; NY: 1990. [Google Scholar]
- Blum N, St. John D, Pfohl B, Stuart S, McCormick B, Allen J, Arndt S, Black DW. Systems Training for Emotional Predictability and Problem Solving (STEPPS) for outpatients with borderline personality disorder: A randomized controlled trial and 1-year follow-up. Am J Psychiatry. 2008;165:468–478. doi: 10.1176/appi.ajp.2007.07071079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown EJ, Heimberg RG, Juster HR. Social phobia subtype and avoidant personality disorder: Effect of severity of social phobia, impairment, and outcome of cognitive-behavioral treatment. Behav Ther. 1995;26:467–486. [Google Scholar]
- Cacciola JS, Rutherford MJ, Alterman AI, McKay JR, Snider EC. Personality disorders and treatment outcome in methadone maintenance patients. J Nerv Ment Dis. 1996;184:234–239. doi: 10.1097/00005053-199604000-00006. [DOI] [PubMed] [Google Scholar]
- Carroll KM. A cognitive-behavioral approach: treating cocaine addiction: therapy manuals for drug addiction. National Institute on Drug Abuse, U.S. Department of Health and Human Services; Rockville, MD: 1998. [Google Scholar]
- Carroll KM, Nich C, Sifry RL, Nuro K, Frankforter TL, Ball SA, Fenton L, Rounsaville BJ. A general system for evaluating therapist adherence and competence in psychotherapy in the addictions. Drug Alcohol Depend. 2000;57:225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: A multiwave study. Am J Psychiatry. 2007;164:922–928. doi: 10.1176/ajp.2007.164.6.922. [DOI] [PubMed] [Google Scholar]
- Conrod PJ, Stewart SH. A critical look at dual-focused cognitive-behavioral treatments for comorbid substance use and psychiatric disorders: strengths, limitation, and future directions. J Cogn Psychother. 2005;19:261–284. [Google Scholar]
- Crits-Christoph P, Siqueland L, Blaine J, Frank A, Luborsky L, Onken LS, et al. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Arch Gen Psychiatry. 1999;57:493–502. doi: 10.1001/archpsyc.56.6.493. [DOI] [PubMed] [Google Scholar]
- Crouse EM, Drake KM, McGovern MP. Personality disorders and drug and alcohol problems. In: Baker A, Velleman R, editors. Clinical handbook of co-existing mental health and drug and alcohol problems. Routledge/Taylor & Francis Group; NY: 2007. pp. 309–328. [Google Scholar]
- Darke S, Ross J, Williamson A, Mills K, Havard A, Teesson M. Borderline personality disorder and persistently elevated levels of risk in 36-month outcomes for the treatment of heroin dependence. Addiction. 1997;102:1140–1146. doi: 10.1111/j.1360-0443.2007.01876.x. [DOI] [PubMed] [Google Scholar]
- Davidson K, Norrie J, Tyrer P, Gumley A, Tata P, Murray H, Palmer S. The effectiveness of cognitive behavior therapy for borderline personality disorder: Results from the Borderline Personality Disorder Study of Cognitive Therapy (BOSCOT) trial. J Pers Disord. 2006;20:450–465. doi: 10.1521/pedi.2006.20.5.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLeon G. Therapeutic communities: is there an essential model. In: DeLeon G, editor. Community as method: therapeutic communities for special populations and special settings. Praeger; Westport, CT: 1997. [Google Scholar]
- Derogatis L. Brief Symptom Inventory: administration, procedures, and scoring manual-II. Clinical Psychometric Research, Inc.; USA: 1992. [Google Scholar]
- Diguer L, Barber JP, Luborsky L. Three concomitants: personality disorders, psychiatric severity, and outcome of dynamic psychotherapy of major depression. Am J Psychiatry. 1993;150:1246–1248. doi: 10.1176/ajp.150.8.1246. [DOI] [PubMed] [Google Scholar]
- Ekleberry SC. Integrated treatment for co-occurring disorders: personality disorders and addiction. Routledge/Taylor & Francis Group; NY: 2009. [Google Scholar]
- Fahy TA, Eisler I, Russell GFM. Personality disorder and treatment response in bulimia nervosa. Br J Psychiatry. 1993;162:765–770. doi: 10.1192/bjp.162.6.765. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV) American Psychiatric Press; Washington, D.C.: 1996. [Google Scholar]
- Giesen-Bloo J, van Dyck R, Spinhoven P, van Tilburg W, Dirksen C, van Asselt T, Kremers I, Nadort M, Arntz A. Outpatient psychotherapy for borderline personality disorder-randomized trial of schema-focused therapy vs. transference-focused therapy. Arch Gen Psychiatry. 2006;63:649–658. doi: 10.1001/archpsyc.63.6.649. [DOI] [PubMed] [Google Scholar]
- Gregory RJ, Chlebowski S, Kang D, Remen AL, Soderberg MG, Stepkovich J. A controlled trial of psychodynamic psychotherapy for co-occurring borderline personality disorder and alcohol use disorder. Psychotherapy. 2008;45:28–41. doi: 10.1037/0033-3204.45.1.28. [DOI] [PubMed] [Google Scholar]
- Gregory RJ, DeLucia-Deranja E, Mogel JA. Dynamic deconstructive psychotherapy versus optimized community care for borderline personality disorder co-occurrring with alcohol use disoders: A 30-month follow-up. J Nerv Ment Dis. 2010;198:292–298. doi: 10.1097/NMD.0b013e3181d6172d. [DOI] [PubMed] [Google Scholar]
- Hardy GE, Barkham M, Shapiro DA, Stiles WB, Rees A, Reynolds S. Impact of cluster C personality disorders on outcomes of contrasting brief psychotherapies for depression. J Consult Clin Psychol. 1995;63:997–1004. doi: 10.1037//0022-006x.63.6.997. [DOI] [PubMed] [Google Scholar]
- Hesse M, Pedersen MU. Antisocial personality disorder and retention: a systematic review. Ther Communities. 2006;27:495–504. [Google Scholar]
- Hoglend P. Personality disorders and long-term outcome after brief psychodynamic therapy. J Pers Disord. 1993;7:168–181. [Google Scholar]
- Hubbard RL, Craddock SG, Flynn PM, Anderson J, Etheridge RM. Overview of 1-year follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS). Psychol Addict Behav. 1997;11:261–278. [Google Scholar]
- Hyler SE. Personality Diagnostic Questionnaire-4 (PDQ-4) New York State Psychiatric Institute; NY: 1994. Unpublished test. [Google Scholar]
- Johnson C, Tobin DL, Dennis A. Differences in treatment outcome between borderline and nonborderline bulimics at one-year follow-up. Int J Eat Disord. 1990;9:617–627. [Google Scholar]
- Kienast T, Foerster J. Psychotherapy of personality disorders and concomitant substance dependence. Curr Opin Psychiatry. 2008;21:619–624. doi: 10.1097/YCO.0b013e32830d365c. [DOI] [PubMed] [Google Scholar]
- Kosten TA, Kosten TR, Rounsaville BJ. Personality disorders in opiate addicts show prognostic specificity. J Subst Abuse Treat. 1989;6:163–168. doi: 10.1016/0740-5472(89)90003-2. [DOI] [PubMed] [Google Scholar]
- Leichsenring F, Leibing E. The effectiveness of psychodynamic therapy and cognitive-behavior therapy in the treatment of personality disorders: A meta-analysis. Am J Psychiatry. 2003;160:1223–1232. doi: 10.1176/appi.ajp.160.7.1223. [DOI] [PubMed] [Google Scholar]
- Linehan M. Cognitive behavior therapy for borderline personality disorder. Guilford; New York: 1993. [Google Scholar]
- Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard H. Cognitive behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991;48:1060–1064. doi: 10.1001/archpsyc.1991.01810360024003. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, Korslund KE, Tutek DA, Reynolds SK, Lindenboim N. Two year randomized controlled trial and follow up of dialectical behavior therapy vs. therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. 2006;63:757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welch SS, Heagerty P, Kivlahan DR. Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug Alcohol Depend. 2002;67:13–26. doi: 10.1016/s0376-8716(02)00011-x. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Schmidt H, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. Am J Addict. 1999;8:279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- McKendrick K, Sullivan C, Banks S, Sacks S. Modified therapeutic community treatment for offenders with MICA disorders: Antisocial personality disorder and treatment outcomes. J Offender Rehabil. 2007;44:133–159. doi: 10.1080/00952990701653800. [DOI] [PubMed] [Google Scholar]
- Mercer DE, Woody GE, editors. An individual counseling approach to treat cocaine addiction: the collaborative cocaine treatment study model: therapy manuals for addiction (manual 3) National Institute on Drug Abuse; Bethesda, MD: 1999. [Google Scholar]
- Mertens JR, Lu YW, Parthasarathy S, Moore C, Weisner CM. Medical and psychiatric conditions of alcohol and drug treatment patients in an HMO: Comparison with matched controls. Arch Gen Psychiatry. 2003;163:2511–2517. doi: 10.1001/archinte.163.20.2511. [DOI] [PubMed] [Google Scholar]
- Messina N, Farabee D, Rawson R. Treatment responsivity of cocaine-dependent patients with antisocial personality disorder to cognitive-behavioral and contingency management interventions. J Consult Clin Psychol. 2003;71:320–329. doi: 10.1037/0022-006x.71.2.320. [DOI] [PubMed] [Google Scholar]
- Nace EP, Davis CW. Treatment outcome in substance abusing patients with a personality disorder. Am J Addict. 1993;2:26–33. [Google Scholar]
- Oldham JM, Skodol AE, Bender DS, editors. Essentials of personality disorders. American Psychiatric Publishing, Inc.; Washington, DC: 2009. [Google Scholar]
- Perry JC, Banon E, Ianni F. Effectiveness of psychotherapy for personality disorders. Am J Psychiatry. 1999;156:1312–1321. doi: 10.1176/ajp.156.9.1312. [DOI] [PubMed] [Google Scholar]
- Ravndal E, Vaglum P, Lauritzen G. Completion of long-term inpatient treatment of drug abusers: A prospective study from 13 different units. Eur Addict Res. 2005;11:180–185. doi: 10.1159/000086399. [DOI] [PubMed] [Google Scholar]
- Ryle A, Golynkina K. Effectiveness of time-limited cognitive-analytic therapy for borderline personality disorders: factors associated with outcome. Br J Med Psychol. 2000;73:197–210. doi: 10.1348/000711200160426. [DOI] [PubMed] [Google Scholar]
- Sanislow CA, McGlashan TH. Treatment outcome of personality disorders. Can J Psychiatry. 1998;43:237–250. doi: 10.1177/070674379804300302. [DOI] [PubMed] [Google Scholar]
- Shea MT, Pilkonis PA, Beckham E, Collins JF, Elkin I, Sotsky SM, Docherty JP. Personality disorders and treatment outcome in the NIMH Treatment of Depression Collaborative Research Program. Am J Psychiatry. 1990;147:711–718. doi: 10.1176/ajp.147.6.711. [DOI] [PubMed] [Google Scholar]
- Slosson R, Nicholson C. Slosson Oral Reading Test (rev. ed.) SORT-R3. Slosson Educational Publications; East Aurora, NY: 1990. [Google Scholar]
- Stravynski A, Marks I, Yule W. Social skills problems in neurotic outpatients. Arch Gen Psychiatry. 1982;39:1378–1385. doi: 10.1001/archpsyc.1982.04290120014003. [DOI] [PubMed] [Google Scholar]
- Svartberg M, Stiles TC, Seltzer MH. Randomized, controlled trial of the effectiveness of short-term dynamic psychotherapy and cognitive therapy for cluster C personality disorders. Am J Psychiatry. 2004;161:810–817. doi: 10.1176/appi.ajp.161.5.810. [DOI] [PubMed] [Google Scholar]
- van den Bosch LM, Verheul R. Patients with addiction and personality disorder: Treatment outcomes and clinical implications. Curr Opin Psychiatry. 2007;20:67–71. doi: 10.1097/YCO.0b013e328011740c. [DOI] [PubMed] [Google Scholar]
- van den Bosch LMC, Verheul R, Schippers GM, van den Brink W. Dialectical behavior therapy of borderline patients with and without substance use problems: Implementation and long-term effects. Addict Behav. 2002;27:911–923. doi: 10.1016/s0306-4603(02)00293-9. [DOI] [PubMed] [Google Scholar]
- Verheul R, Ball S, van den Brink W. Substance abuse and personality disorders. In: Kranzler HR, Rounsaville BJ BJ, editors. Dual diagnosis and treatment: substance abuse and comorbid medical and psychiatric disorders. Marcel Dekker; NY: 1998. [Google Scholar]
- Verheul R, Hartgers C, van den Brink W, Koeter MWJ. The effect of sampling, diagnostic criteria and assessment procedures on the observed prevalence of DSM-III-R personality disorders among treated alcoholics. J Stud Alcohol. 1998;59:227–236. doi: 10.15288/jsa.1998.59.227. [DOI] [PubMed] [Google Scholar]
- Verheul R, Herbrink M. The efficacy of various modalities of psychotherapy for personality disorders: A systematic review of the evidence and clinical recommendations. Int Rev Psychiatry. 2007;19:25–38. doi: 10.1080/09540260601095399. [DOI] [PubMed] [Google Scholar]
- Verheul R, van den Bosch LMC, Ball SA. Substance abuse. In: Oldham JM, Skodol AE, Bender DS, editors. Textbook of personality disorders. American Psychiatric Publishing; Washington, DC: 2005. pp. 463–476. [Google Scholar]
- Verheul R, van den Bosch LMC, Koeter MWJ, De Ridder MAJ, Stijnen T, van den Brink W. Dialectical behavior therapy for women with borderline personality disorder: 12-month randomized clinical trial in the Netherlands. Br J Psychiatry. 2003;182:135–140. doi: 10.1192/bjp.182.2.135. [DOI] [PubMed] [Google Scholar]
- Woody G, McLellan AT, Luborsky L, O'Brien CP. Sociopathy and psychotherapy outcome. Arch Gen Psychiatry. 1985;42:1081–1086. doi: 10.1001/archpsyc.1985.01790340059009. [DOI] [PubMed] [Google Scholar]
- Young JE. Cognitive therapy for personality disorders: a schema-focused approach. Professional Resource Exchange, Inc.; Sarasota, Fl: 1994. [Google Scholar]
- Young JE, Klosko JS, Weishaar ME. Schema therapy: a practitioner's guide. Guilford Press; New York, NY: 2003. [Google Scholar]
- Zuckerman M, Lubin B. The Multiple Affect Adjective Checklist - Revised. Educational and Industrial Testing Service; San Diego, CA: 1985. [Google Scholar]